Abstract
Background
Injury in the home is common, accounting for approximately a third of all injuries. The majority of injuries to children under five and people aged 75 and older occur at home. Multifactorial injury prevention interventions have been shown to reduce injuries in the home. However, few studies have focused specifically on the impact of physical adaptations to the home environment and the effectiveness of such interventions needs to be ascertained.
Objectives
To determine the effect of modifications to the home environment on the reduction of injuries due to environmental hazards.
Search methods
We searched The Cochrane Library, MEDLINE, EMBASE and other specialised databases. We also scanned conference proceedings and reference lists. We contacted the first author of all included randomised controlled trials. The searches were last updated to the end of December 2009, and were not restricted by language or publication status.
Selection criteria
Randomised controlled trials.
Data collection and analysis
Two authors screened all abstracts for relevance, outcome and design. Two authors independently assessed methodological quality and extracted data from each eligible study. We performed meta‐analysis to combine effect measures, using a random‐effects model. We assessed heterogeneity using an I2 statistic and a Chi2 test.
Main results
We found 28 published studies and one unpublished study. Only two studies were sufficiently similar to allow pooling of data for statistical analyses. Studies were divided into three groups; children, older people and the general population/mixed age group. None of the studies focusing on children or older people demonstrated a reduction in injuries that were a direct result of environmental modification in the home. One study in older people demonstrated a reduction in falls and one a reduction in falls and injurious falls that may have been due to hazard reduction. One meta‐analysis was performed which examined the effects on falls of multifactorial interventions consisting of home hazard assessment and modification, medication review, health and bone assessment and exercise (RR 1.09, 95% CI 0.97 to 1.23).
Authors' conclusions
There is insufficient evidence to determine whether interventions focused on modifying environmental home hazards reduce injuries. Further interventions to reduce hazards in the home should be evaluated by adequately designed randomised controlled trials measuring injury outcomes. Recruitment of large study samples to measure effect must be a major consideration for future trials. Researchers should also consider using factorial designs to allow the evaluation of individual components of multifactorial interventions.
Plain language summary
More evidence is needed to show whether or not altering the physical home environment by removing potential hazards reduces injuries
Injuries in the home are very common. Most of the injuries to older people and children under five occur at home. Many people are encouraged to alter their home to try and reduce injury and injury risk. Common alterations include the fitting of locks on cupboards, installing stair gates, improvement of lighting in halls and stairways, and the removal of trip hazards. The review found that there is insufficient evidence from studies to show that such changes reduce the number of injuries in the home but does not conclude that these interventions are ineffective. Home alterations need to be evaluated by larger and better designed studies which include injuries in their outcomes.
Background
Injury in the home environment is an extremely common event, accounting for around a third of injuries in all age groups. The majority of injuries of children under five and people aged 75 and over occur in the home (DTI 1997; Lilley 1995; Lyons 2002). A European Union report (EU 2006) describes injury as the number one killer of children, adolescents and young adults; a major cause of disability, morbidity and healthcare costs; as detrimental to European Union production and unequal in its impact on social groups. The report cites children, adolescents and the elderly as priority groups for addressing safety issues. The World Health Organization (WHO 2006) estimated that within its Member States, 875,000 children and adolescents under the age of 18 died each year due to injury and approximately 70% of these deaths were due to accidental injury. One study reported that up to 44% of accidental injuries occur in the home (Scheidt 1995). It is unclear what proportion of these injuries are caused by hazards in the home. There is evidence from certain reviews to suggest that it is possible to reduce injuries in the home by using multifactorial, injury prevention interventions (Coleman 1996; Health Development Agency 2003; Lyons 1998; NHS CRD 1996; Towner 2001; Van Haastregt 2000a). Subsequently, this evidence has found its way into policy documents and strategies prepared to prevent injuries in the home.
In England, the National Service Framework for Older People sets as a standard the development of an integrated falls prevention service in every acute hospital (DoH 2001). National Institute of Health and Clinical Excellence (NICE) guidance (NICE 2004) states that all older people who experience recurrent falls or are at risk of falling should be considered for an individualised multifactorial intervention. This advice was based on non‐experimental, descriptive studies. This message was reiterated recently in UK government guidance to reduce falls and fractures with early intervention paramount (DH 2009). Research which examined the views of older people towards fall prevention strategies highlighted that interventions perceived as overbearing or restrictive were not popular and advice to be constantly vigilant for fall hazards could be disempowering (Yardley 2005). Older people favoured positive messages about benefits of interventions and the opportunity to choose strategies that suited them.
In setting up such services, a balance needs to be struck between the amount of resource spent on reducing intrinsic risk factors for falls (for example, excess or inappropriate medication, visual and balance problems) and extrinsic factors (for example, presence of environmental hazards). There appears to be a lack of similar guidelines in relation to injury prevention for children, although some guidance is currently being formulated, notably by NICE in the UK. This may reflect the lack of good quality scientific evidence available.
Existing reviews, however, have looked at any interventions that prevent falls and injuries and have not determined the relative importance of tackling intrinsic and extrinsic factors. The aim of this review, therefore, was to determine whether modification of the home environment reduces injuries in the home. It is hoped that the results of the review may inform and alert clinicians, practitioners and the public to gaps in the evidence and provide suggestions for the testing of future interventions. In addition, the conclusions will guide the research and policy development communities and government departments engaged in policy development. This is particularly important, given the development of cross‐disciplinary collaboration in the field of injury prevention and because government policy, strategy and implementation documents should now directly reflect the results of research evidence.
Objectives
To determine the effect of modifications to the home environment on the reduction of injuries, with the primary focus being interventions which reduce physical hazards in the home.
This review does not include interventions to promote smoke alarm ownership and function. These are the focus of an existing Cochrane review (DiGuiseppi 2001); interventions to prevent injuries caused by items brought into the home such as household chemicals and firearms; home‐based items unrelated to building structure such as hip protectors for the elderly, also the subject of an existing Cochrane review (Parker 2005); medicines, bottles or toys; or injuries related to chronic exposures such as environmental lead.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs).
Types of participants
People of all age groups who are at home (that is, in the place they would normally eat and sleep), in areas where housing is normally architect‐designed and always subject to housing regulations.
Types of interventions
Eligible interventions are those which focus on modifying physical hazards including the building fabric or 'fixtures and fittings' (that is, removable items within a property that are fastened or attached to the building fabric) in the domestic environment, and where modifications such as the installation of grab rails, stair gates, fireguards, cupboard locks, hot‐water tap adaptations and lighting adjustments, have been included.
We have included interventions which take a multifactorial approach (that is, have modification plus education or action on other risk factors). We have included studies which include the installation of smoke alarms alongside other physical interventions but not those where provision of smoke alarms was the sole intervention.
We excluded interventions which did not focus on reducing acute physical injuries (for example studies reducing chronic exposure to lead or nitrogen dioxide). We excluded any intervention where the focus has been to change the home environment solely for non‐injury benefits (for example, improved quality of life of disabled individuals).
Types of outcome measures
Change in injury rate or risk.
Change in prevalence of safety features.
Change in prevalence of hazards.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases:
ASSIA (1987 to December 2009)
British Nursing Index (BNI) (1985 to December 2009)
CINAHL (1994‐December 2009)
Cochrane Library (1996‐December 2009)
EMBASE (1947 to 2009 Week 50)
ICONDA (1976 to December 2009)
MEDLINE (1966 to November Week 3 2009)
MEDLINE In‐Process (1996 to November Week 3 2009)
OpenSIGLE (1980 to 2005)
Planex (formerly the IDOX Information Service) (2004 to December 2009)
RIBA‐British Architectural Library Catalogue (2004 to December 2009)
SafetyLit (2004 to December 2009)
Urbadisc (Acompline and Urbaline) (1970 to December 2004)
-
Web of Science
Science Citation Index and Social Sciences Citation Index (1970 to December 2009)
Conference Proceedings Citation Index (1990 to December 2009)
We searched the electronic databases to December 2009, with the exception of OpenSIGLE which we searched to 2005 when updating ceased. Electronic searches of 12 databases yielded 4509 hits in the most recent update (2004 to December 2009) (see Figure 1). We have provided the complete search strategies in Appendix 1.
1.
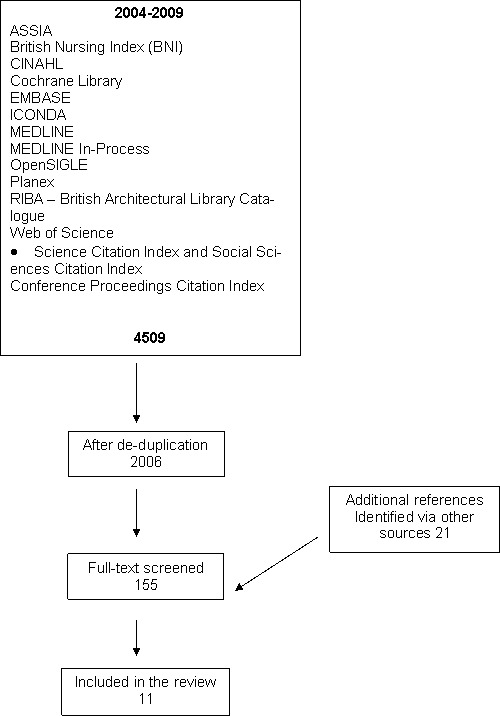
Flow chart of search process
Searching other resources
In addition, we contacted first authors of all included RCTs to ask if they were aware of any recently published, in‐press or unpublished studies on the topic. We carried out handsearching for the most recent 12 months, May 2009 to May 2010, of issues of journals appearing twice or more in the papers considered for inclusion.
Age and Ageing
BMC Public Health
British Medical Journal
Environmental Research
Injury Prevention
Journal of the American Geriatrics Society
Pediatrics
We also checked the reference lists of systematic reviews for further studies relevant to modification of the home environment with a focus on interventions to modify environmental hazards.
This resulted in 21 additional references not found via the electronic search (see Figure 1).
Data collection and analysis
Selection of studies
Two authors pre‐screened all abstracts for relevance, duplication, outcome and design. An expert assessor independently reviewed all abstracts considered not eligible. Where it was not possible to determine if a study met the inclusion/exclusion criteria on the basis of the title and/or abstract alone, we retrieved the full reference and two authors assessed the study according to the pre‐defined inclusion/exclusion criteria. We also screened the reference lists of review articles for any additional studies.
Data extraction and management
Eligible studies were separated into three categories for the purposes of data extraction: a) older people, b) children and c) the general population. Two expert authors independently extracted data from each study. We used EPOC (data collection checklists) guidelines for methodological quality for quality checking and assessed inter‐rater reliability by the kappa statistic. The kappa statistic for the older people category was 1 in the original review, 0.93 in the last update and 0.85 in the current update. It was 0.95 between raters for groups b) children and c) the general population in the original review, 1 in the update and 1 in the current update. We resolved any disagreements on data extraction by consensus discussion, following review by a third assessor.
Assessment of risk of bias in included studies
We considered allocation concealment to be adequate if the randomisation process was protected before and until allocation of treatment group (e.g. use of sealed opaque envelopes). Where a study reported randomisation, but did not describe the method of randomisation, or we judged the method described inadequate, we then deemed it to be a controlled clinical trial (CCT) and excluded it. We also assessed blinding of outcome assessment, method of analysis (e.g. Intention‐To‐Treat versus Per Protocol analysis), attrition rate and statistical power as indicators of study quality.
Measures of treatment effect
We performed meta‐analysis by combining outcome measures and presented results using risk ratios (RR) and 95% confidence intervals (CI).
Assessment of heterogeneity
We determined clinical and methodological heterogeneity by assessing the differences between study characteristics (e.g. variability in participants, interventions, outcomes, follow‐up length, biases). If two or more studies were considered to be sufficiently homogenous, we explored variability between effect size using both the Chi2 test and the I2 statistic. Chi2 tests with a P value ≤ 0.10 were taken as indicating significant statistical heterogeneity and I2 of ≥75% indicating a high level of heterogeneity.
Data synthesis
Although the studies included in this review reported a wide range of outcomes, we judged only two studies reporting falls as an outcome sufficiently methodologically and statistically homogenous to combine in a meta‐analysis.
We performed all analyses using Review Manager software (RevMan 2008). We used a random‐effects model to adjust for the observed statistical heterogeneity between studies.
Results
Description of studies
General findings
In the initial searches performed up to December 2004, we identified 44,717 unique citations through our electronic database searches. A stepped exclusion exercise was performed where references were excluded on the basis of title or title and abstract based on the pre‐defined inclusion/exclusion criteria. Where it was not possible to confirm inclusion/exclusion criteria on review of the abstract alone, we retrieved the full reference. At this stage, we identified 128 potentially relevant references. We identified three more studies through personal contact (Elkan 2000; Thomson 2001; Day 2002) and 13 additional citations by checking the reference lists of reviews (including one review article (Purdue 2003) which identified no new citations). Of the 144 studies reviewed in full, 19 met the inclusion criteria (Becker 2003; Carter unpublished; Clamp 1998; Close 1999; Cumming 1999; Day 2002; Gielen 2002; Hogan 2001; Jenson 2002; Kendrick 1999; King 2005; Nikolaus 2003; Pardessus 2002; Posner 2004; Shaw 2003; Stevens 2001; Tinetti 1994; Van Haastregt 2000b; Vetter 1992).
From our updated electronic searches, we found 2,006 unique citations, 155 of which we identified as potentially relevant citations. We retrieved only 152 studies in full, as one study was available only as an abstract (Rehmani 2005) and two studies were found to be duplications (Posner 2004; Watson 2005). In addition, we identified 21 more citations by checking the reference lists of systematic reviews. Of 173 studies reviewed in full, 10 additional studies met the inclusion criteria (Babul 2007; Campbell 2005; Elley 2008; Gitlin 2006; Hendrickson 2005; Hendriks 2008; Mahoney 2007; Salminen 2009; Sangvai 2007; Watson 2005). Therefore we have included 28 published studies and one unpublished study in this update.
Excluded studies
Initially, 87 studies appeared to meet the eligibility criteria, but after further inspection we excluded them as they did not meet all of the inclusion criteria. One (Ozanne‐Smith 2002) was an ecological study where the measures of changes to physical hazards were not reported at household level, one (Assantachai 2002) was similarly community‐based with no home hazard intervention, one (Duff 2002) included undefined access to home equipment with no measure of change to physical hazards and one (Swart 2008) did not meet the inclusion criteria definition for a home. Seventeen studies (Caplan 2004; Bouwen 2008; Ciaschini 2009; Fergusson 2005; Haynes 2003; Huang 2003; Kerse 2004; Lannin 2007; Llewellyn 2003; Minkovitz 2010; Nelson 2005; Neno 2008; Neyens 2009; Ramsey 2003; Vind 2009; Weatherall 2004; Wyman 2007) had no intervention which met the inclusion criteria and two (Pressley 2009; Tanner 2003) had no outcome.
A further 13 studies were observational studies with either cohort, case‐control or cross‐sectional designs. One was a German‐language paper that was found not to meet the inclusion criteria when it was translated. In another the environmental intervention was not taken up. Four studies were interrupted‐time series studies that did not have a sufficient number of gathering points to meet the EPOC guidelines. One was a non‐controlled before‐and‐after study, three were controlled before‐and‐after studies with no allocation concealment, one a PRECEDE‐PROCEED model with different subjects and methods (Durongritichai 2003). Twenty‐seven (including Huang 2004; Lightbody 2002; Lin 2007; Peel 2000; Robson 2003; Sznajder 2003; Xia 2009) were considered controlled clinical trials because the method of randomisation was not adequately described.
Three studies did not focus on reducing acute physical injuries (Binns 2004; Boreland 2006; Gillespie‐Bennett 2008), two were evaluation studies examining either a tool used in the study (Morgan 2005) or part of the methodology (Robertson 2005), three had smoke alarm installation as the sole intervention (Ginnelly 2005; Roberts 2004; Yang 2008), two were survey studies (Iwarsson 2009; Lamb 2008), two were protocols for studies (Kendrick 2008; Peeters 2007) and one was a Trial of Improved Practices (TIPs) methodology (Barnes 2004).
Included studies
We included 28 completed RCTs published between 1979 and the end of 2009 (Becker 2003; Babul 2007; Campbell 2005; Clamp 1998; Close 1999; Cumming 1999; Day 2002; Elley 2008; Gielen 2002; Gitlin 2006; Hendrickson 2005; Hendriks 2008; Hogan 2001; Jenson 2002; Kendrick 1999; King 2005; Mahoney 2007; Nikolaus 2003; Pardessus 2002; Posner 2004; Salminen 2009; Sangvai 2007; Shaw 2003; Stevens 2001; Tinetti 1994; Van Haastregt 2000b; Vetter 1992; Watson 2005) and one unpublished (Carter unpublished) study. Twenty studies were in older age groups and nine in child populations.
Participants
Study populations included: urban, suburban and rural families (including families in inner‐city, lower‐income areas) with children under five years; caregivers of children under five; parents of newborn infants; independent community‐dwelling older people; staff of nursing homes; venues for older people; nursing home residents and in‐patients of geriatric wards who had returned home; older people with visual acuity problems, cognitive impairment or functional vulnerability; emergency department patients; primary care patients; children from nursery and toddler groups; children attending secondary care paediatric clinics and specialist physicians in training. We also included census tracts and municipalities.
Cluster randomised trials included units based on general practices and residential care facilities for older people.
Type of intervention
Two of the 29 RCTs made an environmental modification to the domestic environment as the sole intervention (Cumming 1999; Pardessus 2002).
Seven studies used a combined approach of direct or recommended modification and educational strategy (Carter unpublished; Clamp 1998; Close 1999; Gielen 2002; Kendrick 1999; King 2005; Stevens 2001).
Three studies used a combined approach of recommended modification with free safety devices, which in some cases were only available to low‐income families, and an educational strategy (Hendrickson 2005; Posner 2004; Watson 2005).
One study used a combined approach of recommended modification with free safety devices (Babul 2007).
One study used a combined approach of free safety devices and safety counselling (Sangvai 2007).
Thirteen of the studies (Becker 2003; Elley 2008; Gitlin 2006; Hendriks 2008; Hogan 2001; Jenson 2002; Mahoney 2007; Nikolaus 2003; Salminen 2009; Shaw 2003; Tinetti 1994; Van Haastregt 2000b; Vetter 1992) were multifactorial and included home modification for injury prevention as well as interventions that did not fit the review protocol. The other interventions encompassed the targeting of nutritional deficiencies, balance and resistance training, psychosocial activities, energy conserving techniques, training in use of mobility aids, exercise, medication review, visual problems, hip protectors, post fall problem solving conferences and reviews of medical conditions.
Two of the studies (Campbell 2005; Day 2002) had a factorial design, which enabled the effect of each component to be evaluated separately, as well as any possible interactive effects between interventions to be examined.
All of the interventions, except two (Clamp 1998; Posner 2004), included a home assessment evaluation made by either a community nurse, trained researcher, project assistant, occupational therapist, health visitor or self‐report by participant. Environmental hazards were evaluated using standardised data collection forms, structured interviews, questionnaires and checklists. Modifications to the home environment included the installation of grab bars, stair gates, handrails, fire guards, blind cord wind‐ups, smoke alarms, cupboard locks, corner cushions for sharp‐edged furniture, electric outlet covers, the reduction of hot water temperatures, the repair of damaged flooring, improvement in lighting levels and the stabilisation of floor surfaces. Fourteen of the interventions (Babul 2007; Campbell 2005; Clamp 1998; Day 2002; Elley 2008; Gitlin 2006; Hendrickson 2005; Kendrick 1999; King 2005; Mahoney 2007; Posner 2004; Sangvai 2007; Stevens 2001; Watson 2005) provided or made available free or discounted safety equipment or devices.
Interventions were delivered in either a healthcare setting (Posner 2004), in the clinical setting as part of routine health surveillance (Clamp 1998; Kendrick 1999; Sangvai 2007), the home (Babul 2007; Becker 2003; Campbell 2005; Carter unpublished; Close 1999; Cumming 1999; Day 2002; Elley 2008; Gitlin 2006; Hendrickson 2005; Hogan 2001; Jenson 2002; King 2005; Mahoney 2007; Nikolaus 2003; Stevens 2001;Tinetti 1994; Van Haastregt 2000b) or in both a healthcare setting and the home (Day 2002; Gielen 2002; Hendriks 2008; Pardessus 2002; Salminen 2009; Shaw 2003; Vetter 1992; Watson 2005).
Outcomes
Sixteen of the 29 randomised controlled trials had an injury, or proxy for injury severity, such as seeking medical advice following a fall, as an outcome variable (Becker 2003; Campbell 2005; Carter unpublished; Close 1999; Elley 2008; Hendriks 2008; Jenson 2002; Kendrick 1999; King 2005; Salminen 2009; Sangvai 2007; Shaw 2003; Stevens 2001; Van Haastregt 2000b ; Vetter 1992; Watson 2005). Nineteen of the studies collected data on falls (Becker 2003; Campbell 2005; Carter unpublished; Close 1999; Cumming 1999; Day 2002; Elley 2008; Hendriks 2008; Hogan 2001; Jenson 2002; Mahoney 2007; Nikolaus 2003; Pardessus 2002; Salminen 2009; Shaw 2003; Stevens 2001; Tinetti 1994; Van Haastregt 2000b; Vetter 1992). Fourteen studies collected data on hazard modification, which included the collection of data on safety knowledge and or possession, use and compliance of safety equipment, as an outcome (Carter unpublished; Clamp 1998; Cumming 1999; Day 2002; Gielen 2002; Gitlin 2006; Hendrickson 2005; King 2005; Nikolaus 2003; Posner 2004; Sangvai 2007; Shaw 2003; Stevens 2001; Watson 2005).
Outcome measures were collected either via self report using fall diaries or calenders, health professional report for care facilities, or chart or medical record review.
Risk of bias in included studies
The adequacy of allocation concealment was evaluated for all studies using the EPOC checklist for RCTs. Where a study reported randomisation but did not describe the method of randomisation, or the method described was judged inadequate, it was then deemed to be a controlled clinical trial (CCT) and was excluded. Schulz 2000 argues that studies have shown that methodologically weak RCTs and inadequately reported RCTs yield biased results. Their earlier review (Schulz 1995) of 250 controlled trials from 33 meta‐analyses in pregnancy and childbirth found that RCTs with inadequate or unclear allocation concealment gave larger estimates of treatment effects, 41% and 33% respectively on average, than trials which reported adequate concealment. Similar results were found for trials in digestive diseases, circulatory diseases, mental health, and stroke (Moher 1998).They found that trials that used inadequate or unclear allocation concealment gave on average 37% larger estimates of effect, than those using adequate concealment.
Allocation concealment was judged adequate in all 29 included studies. Nine studies (Clamp 1998; Close 1999; Cumming 1999; Gielen 2002; Kendrick 1999; Pardessus 2002; Stevens 2001; Tinetti 1994; Vetter 1992) used a table of random numbers and nine (Campbell 2005; Carter unpublished; Day 2002; Elley 2008; Hendriks 2008; Hogan 2001; Shaw 2003; Van Haastregt 2000b; Watson 2005) computer generation. Nine studies (Babul 2007; Becker 2003; Gitlin 2006; Jenson 2002; Mahoney 2007; Nikolaus 2003; Posner 2004; Salminen 2009; Sangvai 2007) used sealed envelopes. One (King 2005) used sealed envelopes mixed in an opaque container, sequentially numbered when withdrawn and then distributed in aliquots to each study site, and one used a coin toss by the child's mother (Hendrickson 2005).
Nine studies had sufficient statistical power to detect important effects as statistically significant and recorded power (Elley 2008; Gitlin 2006; Hendriks 2008; Mahoney 2007; Nikolaus 2003; Posner 2004; Salminen 2009; Shaw 2003; Watson 2005). Two studies appeared slightly underpowered. In one (Day 2002) the power calculation was stated as requiring a sample size of 1143 and achieved a sample size of 1107 and in another (Hendrickson 2005), a sample size of 80 mothers was required and 78 was achieved. In three it was reported that the study was underpowered. Babul 2007 stated that their study was underpowered to detect injury outcomes and was limited to examining trends. Similarly another study (Becker 2003) was underpowered to detect a significant difference due to a lower than expected number of hip fractures. Pardessus 2002 did not report a power calculation but concluded that the number of participants in their study (n = 60) was perhaps too small to detect a significant difference between the intervention and control in terms of rate of falls. Campbell 2005 and Jenson 2002 reported that they had carried out power calculations but did not state the number required to achieve this.
One study had large losses to follow‐up (Sangvai 2007), thus results should be interpreted with caution.
Blinding of outcome assessment was stated in eight studies (Campbell 2005; Elley 2008; Gitlin 2006; Hendriks 2008; King 2005; Posner 2004; Salminen 2009; Sangvai 2007). Although allocation concealment was judged adequate in Jenson 2002 and Hendrickson 2005, they were non‐blinded. Outcomes were self‐reported by participants, except in the following eight studies (Becker 2003; Campbell 2005; Elley 2008; Gielen 2002; Hendrickson 2005; Hendriks 2008; Salminen 2009; Watson 2005). Loss to follow‐up ranged from 0% to 91.5%.
Effects of interventions
Falls
a) Older people
There were 19 studies in the older people category (Becker 2003; Campbell 2005; Carter unpublished; Close 1999; Cumming 1999; Day 2002; Elley 2008; Hendriks 2008; Hogan 2001; Jenson 2002; Mahoney 2007; Nikolaus 2003; Pardessus 2002; Salminen 2009; Shaw 2003; Stevens 2001; Tinetti 1994; Van Haastregt 2000b; Vetter 1992) reporting falls data.
Many of the studies involved multifactorial interventions: that is the intervention consisted of multiple components, not just a single intervention. In 11 studies (Carter unpublished; Elley 2008; Hendriks 2008; Hogan 2001; Mahoney 2007; Pardessus 2002; Salminen 2009; Shaw 2003; Stevens 2001; Van Haastregt 2000b; Vetter 1992), no significant effect of the intervention on falls was found. In Carter unpublished, the proportion of participants who reported falling did not differ significantly between the control group (CG) and either of the intervention groups (IG): brief intervention (odds ratio (OR) 0.6, 95% CI 0.3 to 1.1) and intensive intervention (OR 0.8, 95% CI 0.4 to 1.4). Hogan 2001 combined a home visit to record hazards and falls prevention classes, and found no significant differences between the CG and IG in the cumulative number of falls (311 versus 241, P = 0.34), having one or more falls (79.2% versus 72.0%, P = 0.30) or in the mean number of falls (4.0 versus 3.2, P = 0.43).
In Pardessus 2002, a home visit was performed post hospitalisation for a fall. The main intervention was the identification of environmental hazards and the recommendation of home modifications. Social support mechanisms were also addressed. There was no significant difference in fall recurrence between the IG and CG (mean number of fall recurrences IG 0.68 ± 0.16 vs CG 0.82 ± 0.16). However the study may have been underpowered to detect an effect. Shaw 2003 was a multifactorial intervention where intention‐to‐treat analysis showed no significant difference between IG and CG in proportion of patients who fell during one year of follow up (RR 0.92, 95% CI 0.81 to 1.05). Stevens 2001, which combined a home visit to assess hazards, free safety devices and an educational strategy, found that there was no significant reduction in the IG in the incidence rates of falls involving environmental hazards inside the home (adjusted rate ratio 1.11, 95% CI 0.82 to 1.50) or the rate of falls inside the home (adjusted rate ratio 1.17, 95% CI 0.85 to 1.60).
Van Haastregt 2000b reported no effect in the IG for those who experienced at least one fall (OR 1.3, 95% CI 0.7 to 2.1) while Vetter 1992 found that more falls without fracture occurred in the IG (23% versus 16%, no CI stated), although it is unclear if this is statistically significant.
Elley 2008's programme of falls and fracture risk assessment and referral to appropriate community interventions, such as an exercise programme, was not significant in reducing falls in older people (incidence rate ratio (IRR) = 0.96, CI 95% 0.70 to1.34). The authors suggested that low adherence to programme components and possible internal contamination may have reduced the effectiveness of this study. In addition, the study authors speculate whether multifactorial studies lessen the effectiveness of the individual components.
The multifactorial fall prevention programme in Hendriks 2008 was based on an earlier programme carried out in the UK (Close 1999). However, unlike the UK study, which found favourable effects on the number of people experiencing a fall, the Hendriks 2008 study carried out in the Netherlands, found no effect on falls (OR = 0.86, 95% CI 0.50 to 1.49). The study authors gave several possible explanations for this, including the suggestion that the extended implementation period of the fall prevention programme, in a Dutch healthcare as opposed to a UK healthcare setting, may have reduced the effectiveness of this programme.
Mahoney 2007's results demonstrated that a multifactorial model with referrals to existing medical care and services supported with monthly follow‐up calls to encourage adherence, did not decrease falls in community dwelling older adults (RR 0.81, P = 0.27). However, nursing home days were fewer in the IG (10.3 versus 20.5 days, P = 0.04). The study authors suggest their intermediate‐intensity model, which relied on recommendations and referrals, may not provide enough direct intervention to be effective.
Salminen 2009's multifactorial fall prevention programme, which was based on individual risk analysis, did not reduce the incidence of falls in community dwelling older people with at least one previous fall, during a 12‐month follow‐up (IRR 0.92, 95% CI = 0.72 to 1.19). However, in subgroup analysis, significant interactions between subgroups and groups, both in the IG and CG, were found for persons with depressive symptoms (P = 0.006), number of falls during previous 12 months (P = 0.003) and self‐perceived risk of falling (P = 0.045). The authors present several explanations for their results, including opportunistic recruitment; non‐stringent inclusion criteria; and the possibility that their study may have been underpowered to detect a reduction in the incidence of falls.
Two studies (Elley 2008 and Salminen 2009) were considered sufficiently methodologically and statistically homogenous to undertake a meta‐analysis (Analysis 1.1). Both studies included a multifactorial fall prevention intervention. The interventions comprised: home hazard assessment and modification; medication review and health and bone assessment; and exercise programme. Inclusion criteria and outcome assessment were also considered comparable and both control groups received basic guidance on fall prevention. Combining data from these two studies showed that a multifactorial fall prevention programme designed for older people who had fallen in the previous 12 months did not reduce the risk of falling (RR 1.09, 95% CI 0.97 to 1.23).
1.1. Analysis.
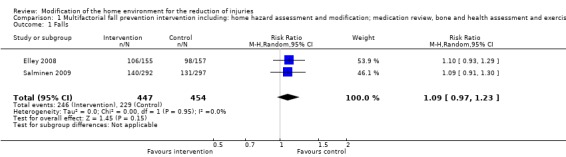
Comparison 1 Multifactorial fall prevention intervention including: home hazard assessment and modification; medication review, bone and health assessment and exercise program, versus control, Outcome 1 Falls.
In other multifactorial studies (Becker 2003; Jenson 2002; Nikolaus 2003; Tinetti 1994), although a significant reduction in falls was reported, the effect of environmental modifications was impossible to separate from other interventions. Although Becker 2003 reported the incidence density rate of falls per 1000 resident years was 2558 for the CG and 1399 for the IG, (RR 0.55, 95% CI 0.41 to 0.73), this was a multifactorial intervention targeting falls in nursing homes. The authors agreed on a list of environmental hazard removal and prosthetic supports but admitted that the lack of validated scoring system for environmental factors as well as time differences for corrections, made the reporting of adherence to environmental corrections unfeasible. Thus any contribution of home modification to the intervention effect was impossible to quantify. Additionally, it was argued that seeing the effects of environmental adaptations, such as installing new floor surfaces, would take more time than allowed in the study.
Jenson 2002 was a multifactorial fall prevention programme including staff education, environmental adjustment, exercise, medication review, aids, hip protectors and post fall problem‐solving conferences. Their intervention significantly reduced the number of residents who fell (RR 0.78, 95% CI 0.64 to 0.96), total number of falls (IRR 0.60 95% CI 0.5 to 0.73) adjusted for baseline factors), time to first fall (adjusted hazard ratio 0.66, 95% CI 0.54 to 0.79) and number of femoral fractures (adjusted OR 0.23, 95% CI 0.06 to 0.94). In Nikolaus 2003's study the interventions included modification to the home environment and training in the use of mobility and technical aids. The IG had 31% fewer falls than the CG (IRR 0.69, 95% CI 0.51 to 0.97). The intervention was most effective in a subgroup of participants who reported having had two or more falls during the year before recruitment into the study.
In Tinetti 1994, the adjusted IRR for falling in the IG compared with the CG was 0.69 (95% CI 0.52 to 0.90).
In one study (Cumming 1999), a reduction in falls was observed in an intervention subgroup only, participants with a history of falls (RR 0.64, 95% CI 0.50 to 0.83).
In Day 2002, the percentage estimated reduction in annual fall rate attributed to home hazard management was not significant (3.1%, 95% CI ‐2.0 to 9.7). However, there was a significant effect when the intervention included exercise (9.9%, 95% CI 2.4 to 17.9). The strongest effect was observed when all three interventions; exercise, home hazard management, vision correction, were combined together (14.0%, 95% CI 3.7 to 22.6), (RR 0.67, 95% CI 0.51 to 0.88). The study authors propose that the intervention may not have been intensive enough or the modifications may not have been sufficient or the right type to affect falls outcome.
Campbell 2005's study focused on older people with severe visual impairment. Due to the factorial design, each component of the study could be evaluated separately. They found that fewer falls occurred in the group randomised to receive only the home safety programme, compared to the social visits group (IRR 0.39, 95% CI 0.24 to 0.62).
There were no included studies which had falls data as an outcome measure in children or general population categories.
Injuries
a) Older people
There were 13 studies which included older people (Becker 2003; Campbell 2005; Carter unpublished; Close 1999; Elley 2008; Hendriks 2008; Jenson 2002; Nikolaus 2003; Salminen 2009; Shaw 2003; Stevens 2001; Van Haastregt 2000b; Vetter 1992) and reported injuries data, 11 of which found no significant reduction in the IG. In Becker 2003, no significant difference in hip fractures between the IG and CG (RR 1.11, 95% CI 0.49 to 2.51) was reported. There was also no significant difference between the incidence density rate of non‐hip fractures between the IG and the CG (RR 0.78, 95% CI 0.57 to 1.07). Similarly in Shaw 2003, the RR between the IG and CG was not significantly different for major injuries (RR 1.32, 95% CI 0.87 to 2.00) or fractured neck of femurs (RR 0.55, 95% CI 0.21 to 1.72). However in all of these studies the numbers of injuries were small. Nikolaus 2003 was not designed to examine fall‐related injuries and stated that numbers were too small for statistical comparisons. Stevens 2001 found no significant reduction in the rate of injurious falls in the IG (adjusted RR 0.92, 95% CI 0.73 to 1.14). Vetter 1992 reported a similar proportion of fractures in both the IG and CG (5% versus 4%, no CI stated). Van Haastregt 2000b reported OR 1.4 (95% CI 0.8 to 2.6) for injurious falls in the IG compared to the CG.
Five further studies (Carter unpublishedClose 1999Elley 2008; Hendriks 2008; Salminen 2009) found no significant reduction in the number of injurious falls or fracture rates. Carter unpublished found the proportion of participants who reported one or more falls requiring medical attention did not differ significantly between CG and either of the IGs: brief intervention (OR 0.7, 95% CI 0.2 to 2.2) and intensive intervention (OR 0.7, 95% CI 0.2 to 2.4). Close 1999 found no significant reductions in the percentage of patients reporting serious injury from falls (CG 8% versus IG 4%, P = 0.26). Elley 2008 reported no significant reduction in moderate injurious falls (IG 1.05 injurious falls per person‐year vs CG 1.00, no CI stated) or serious injurious falls (IG 0.09 injurious falls per person‐year vs CG 0.05, no CI stated). The study authors speculate whether multifactorial trials lessen the effectiveness of the individual components. Hendriks 2008's study reported no significant reduction in injurious falls between IG and CG (OR 0.77, 95% CI 0.35 to 1.73, P = 0.53). Salminen 2009's intervention did not reduce the incidence of falls requiring medical treatment at 12 months' follow‐up (IRR 1.04, 95% CI 0.64 to 1.69) or at three years follow‐up (IRR 0.87, 95% CI = 0.63 to 1.21).
The picture is only a little different in Jenson 2002. Although the authors report a reduction in injurious falls in the IG, no statistical comparison is reported. However, a significant reduction in femoral fractures is recorded, with only three residents in the IG suffering a femoral fracture compared to 12 in the CG (adjusted OR = 0.23, CI 0.06 to 0.94). In a later report, Jensen 2003 analysed the effect of this intervention in older people with differing levels of cognitive function. Fifty‐nine minor, moderate or serious injuries occurred in the higher cognitive group, giving a non‐significant crude IRR 0.90 (95% CI 0.50 to 1.50) compared with the control group and similarly in the lower cognitive group (crude IRR 0.90, 95% CI 0.50 to 1.30). However in the lower cognitive group the 171 participants sustained 10 femoral fractures, all of which were in the control group (result expressed as P = 0.006).
In Campbell 2005's study, which focused on older people with visual acuity problems, a significant reduction in injurious falls was reported in the home safety programme only group versus social visits group (IRR 0.56, 95% CI 0.36 to 0.87).
b) Children
Five studies (Babul 2007; Kendrick 1999; King 2005; Sangvai 2007; Watson 2005) reported data on injuries. Four of these studies found no significant difference in injury occurrence between IG and CG. Kendrick 1999 reported no significant change in the frequency of at least one medically attended injury (OR 0.97 95% CI 0.72 to 1.30), at least one attendance at an accident and emergency department for injury (OR 1.02, 95% CI 0.76 to 1.37), at least one primary care attendance for injury (OR 0.75, 95% CI 0.48 to 1.17) or at least one hospital admission for injury (OR 0.69, 95% CI 0.42 to 1.12). Sangvai 2007's multifactorial intervention showed no significant difference in medically attended injuries (19/160 IG and 22/159 CG). Watson 2005 reported a higher attendance rate for injury in primary care in the IG compared to the CG (IRR 1.37, 95% CI = 1.11 to 1.70, P = 0.003). Treatment arms did not differ significantly for other injury outcomes. Finally in Babul 2007 injury rates did not differ between the group provided with a safety kit and the CG (OR 1.03, 95% CI 0.49 to 2.18), or the safety kit plus home visit group and CG (OR 1.05, 95% CI 0.50 to 2.21).
King 2005's study showed a significant reduction in injury visits per patient at 12 months in the IG (RR 0.69, 95% CI = 0.54 to 0.88). However, they reported that between 12 and 36 months the effect appeared to diminish but did not cause harm (RR 0.8, 95% CI 0.64 to 1.00).
c) General population (mixed age groups)
There were no included studies in the general population group.
Hazards reduction (including safety knowledge, possession, compliance with and use of safety equipment)
a) Older people
Eight included studies (Campbell 2005; Carter unpublished; Cumming 1999; Day 2002; Gitlin 2006; Nikolaus 2003; Shaw 2003; Stevens 2001) reported data on hazard reduction in older people. All eight studies found a greater reduction in hazards in the IG compared to the CG, but only two studies reported a significant reduction (Carter unpublished; Stevens 2001). Five studies did not report whether their result were statistically significant, and Gitlin 2006's results appeared non‐effective. Only three studies (Campbell 2005; Cumming 1999; Nikolaus 2003) had an associated reduction in falls. In one other study (Day 2002), the reduction in falls could not be directly associated with the reduction in hazards.
In Nikolaus 2003, 222 home modifications were recommended. A minimum of one recommended change was implemented by 137 homes (75.7%). The most commonly recommended changes were elevation of the toilet seat in 43 homes, use of a rollator (walking frame with wheels) in 37 homes and fixing grab rails in the bathroom in 27 homes. Compliance with recommendations ranged from 33.3% to 82.6% at 12 months' follow‐up. Participants who made at least one of the recommendations experienced a significant reduction in the rate of falls (IRR 0.64, 95% CI 0.37 to 0.99, P = 0.047) at 12 months' follow up. The number of falls in participants in the IG with no home modifications was not significantly different from those in the CG (IRR 1.05, 95% CI 0.82 to 1.41). Therefore an intention‐to‐treat analysis would be likely to report no difference between the groups. Cumming 1999 observed a reduction in hazards in the IG but it is unclear if this was a significant reduction and falls were only reduced in the intervention sub‐group with a history of falls (RR 0.64, 95% CI 0.50 to 0.83). In Campbell 2005, 85% of participants in the home safety group were followed up at six months (169/198), and 90% of these (152/169) were reported as complying partially or completely with one or more of the home safety recommendations made by the occupational therapist, implying that the intervention was acceptable.
Carter unpublished observed a positive effect on making changes to improve home safety in both IGs with 35% in the brief intervention group and 49% in the intensive IG making changes in the home to improve safety, compared to 28% in the CG at 12 months' follow‐up. No test for statistical significance was reported. In Shaw 2003 there was no significant change in environmental risk factors score at three months in either the IG or CG, but there was a significant change in score between the two groups, P < 0.001. Stevens 2001 reported statistically significant improvements in a sample (n = 51) of the larger study in: unsafe steps (Mean 0.61, 95% CI 0.28 to 0.94), stabilisation of rugs and mats (Mean 1.27, 95% CI 0.91 to 2.24), rooms with trailing cords (Mean 0.43, 95% CI 0.10 to 0.76) and rooms with unsafe favourite chair (Mean 0.10 95% CI 0.02 to 0.18). Whilst the authors reported other results as significant, no statistical significance tests were reported.
Day 2002 reported that of the 543 participants receiving the home hazard management intervention, 478 were advised to have modifications to their homes. Help to carry out modifications was received by 363 participants which included 275 hand rails fitted, 72 modifications to floor coverings and 72 homes receiving contrast edging to steps. Modification of environmental hazards on their own did not reduce injuries but the strongest effect was found when all three interventions (exercise, medical review and home modification) were combined (RR 0.67, 95% CI 0.51 to 0.88).
In Gitlin 2006's study, the effect of their intervention on environmental home hazards at 12 months was reported as a difference of adjusted means of ‐1.38, 95% CI ‐3.17 to 0.41, P = 0.13, which is not statistically significant.
b) Children
Eight studies reported data on hazard reduction (Babul 2007; Clamp 1998; Gielen 2002; Hendrickson 2005; King 2005; Posner 2004; Sangvai 2007; Watson 2005) and seven reported either a significant reduction of hazards or significant increase in safety features in the IG. Clamp 1998 found that significantly more families in the IG used fireguards (RR 1.89, 95% CI 1.18 to 2.94), socket covers (RR 1.27, 95% CI 1.10 to 1.48), locks on cupboards for storing cleaning materials (RR 1.38, 95% CI 1.02 to 1.88), and door slam devices (RR 3.60, 95% CI 2.17 to 5.97) compared to the CG. In addition, significantly more families in the IG showed safe practice for windows (RR 1.30, 95% CI 1.06 to 1.58), fireplaces (RR 1.84, 95% CI 1.34 to 2.54) and door‐slam safety (RR 7.00, 95% CI 3.15 to 15.6). King 2005 found a significant reduction in the prevalence of homes with hot water above 54°C; (OR 1.31, 95% CI 1.14 to 1.50) and the presence of a fire extinguisher (OR 0.81, 95% CI 0.67 to 0.97) in the IGs (King 2001). In one study (Posner 2004), the IG received comprehensive home safety education and free safety devices and the CG received a focused injury‐specific emergency department discharge set of instructions. The IG demonstrated significantly higher average overall safety scores than the CG (73.3%, SD 8.4%, P ≦ 0.002), and significant improvements in prevention of the following hazards: poison (74.4%, SD 19.5, P ≦ 0.02), cut/piercing (81%, SD 18.2, P ≦ 0.001) and burn category scores (76.0%, SD 14.9, P = 0.03). Caregivers in the IG also demonstrated greater improvement in reported use of the distributed safety devices (65.4%, SD 20.5, P ≦ 0.001).
Three further studies (Babul 2007; Hendrickson 2005; Watson 2005) demonstrated a reduction in hazards. In Babul 2007, parents in both IG (home visit plus safety kit and just safety kit) were more likely to report having hot water at a safe temperature than CG participants: safety kit alone (OR 2.21, 95% CI 1.32 to 3.69); and safety kit plus home visit (OR 2.6, 95% CI 1.57 to 4.46), both adjusted for income and baseline measure of dependent values. Parents receiving the safety kit plus home visit were also more likely to report having used the hot water temperature‐testing card than those receiving the safety kit alone (OR 2.38, CI 1.42 to 3.97, adjusted for income), and compared to the CG, were more likely to report having plants placed out of reach of children (OR 1.90, 95% CI 1.03 to 3.52, adjusted for income and baseline measure of dependent values), as some houseplants are toxic.
In Hendrickson 2005 a statistically significant difference was found in controllable safety hazard scores between groups (F(1.77) 99.6, P ≦ 0.01). In Watson 2005, at both one‐year and two‐year follow‐up, families in the IG were significantly more likely to have implemented a range of safety practices. At 12 months' follow‐up the IG were significantly more likely to be safe in terms of smoke alarms (OR 1.83, CI 1.33 to 2.52, P = 0.0002), stairs (OR 1.46, CI 1.19 to 1.80, P = 0.0004), windows (OR 1.28, CI 1.02 to 1.59, P = 0.03), storage of cleaning products (OR 1.34, CI 1.09 to 1.66, P = 0.006) and sharp objects (OR 1.34, CI 1.09 to 1.65, P = 0.005) in the kitchen than families in the CG. At 24 months' follow‐up, families in the IG were also significantly more likely to be safe in terms of smoke alarms (OR 1.67, CI 1.21 to 2.32, P = 0.002), storage of medicines (OR 1.55, CI 1.00 to 2.40, P = 0.05), and cleaning products (OR 1.31, CI 1.07 to 1.60, P = 0.008) in the kitchen than families in the CG. However, absolute differences in the percentages of families with safety practices were small. For example in the case of fitted window locks, 71.7% of families in the IG were reported as having locks at follow‐up compared to 66.5% in the CG.
In Sangvai 2007, smoke detectors were functional in 16 of 17 intervention households compared with five of 10 control households (P = 0.015, fisher exact test), and hazardous substances were not found in low cabinets of 13 of 16 intervention households compared to three of 10 control households (P = 0.015, fishers exact test). However results should be interpreted cautiously due to large losses to follow‐up.
Gielen 2002 randomised participants to either a standard or an enhanced‐intervention group. Parents in the standard‐intervention group received safety counselling and referral to a childrens safety centre; parents in the enhanced‐intervention group received these standard services plus a home visit. No significant differences in safety practices were observed between study groups. However, a sub‐analysis, independent of study group, found that families who visited the safety centre were significantly more likely to have 3 or more home safety practices observed, compared to families who did not (34% vs 17% ≥3, OR 3.39, 95% CI 1.30 to 8.82). Although this analysis was adjusted for exposure to safety counselling and a home visit, and the authors found no socio‐demographic confounders; it was based on non‐randomised participants and is therefore susceptible to confounders and self selection bias.
c) General population (mixed age groups)
There were no included studies in this group.
We did not contact authors of included studies for further information or data.
We have included supplementary results data in the Additional tables (Table 2; Table 3).
1. Children.
| Study ID | Study Type | Intervention | Results | Reduction |
| Babul 2007 | RCT | Home visit plus safety kit or safety kit alone or control group | Parents in both intervention groups were more likely than those in the control group to report having their home hot water temperature adjusted to a safe level (safety kit alone (OR 2.21, 95% CI 1.32 to 3.69) & safety kit plus home visit (OR 2.6, 95% CI 1.57 to 4.46), both adjusted for income and baseline measure of dependent variable)). Parents receiving a safety kit plus home visit were more likely to report having used the hot water temperature‐testing card than those receiving the safety kit alone (OR 2.38, 95% CI 1.42‐3.97), adjusted for income)). Parents receiving a safety kit plus home visit were also more likely than those in the control group to report having plants placed out of reach of infants (OR 1.90, 95% CI 1.03 to 3.52), adjusted for income and baseline measure of dependent variable)). However, no differences were found in the levels of parent‐reported infant injuries. Difference in injury rates between kit group and control group was OR = 1.03, (95% CI 0.49 to 2.18), and difference between the kit plus home visit group compared to control group OR =1.05, (95% CI 0.50 to 2.21). |
Injury N Falls NA Hazards Y |
| Clamp 1998 | RCT | GP safety advice | Post intervention, intervention group families used fireguards (RR 1.89, 95% CI 1.18 to 2.94), smoke alarms (RR1.14, 95% CI 1.04 to 1.25), socket covers (RR 1.27, 95% CI 1.10 to 1.48), locks on cupboards for storing cleaning materials (RR 1.38, 95% CI 1.02 to 1.88), and door slam devices (RR 3.60, 95% CI 2.17 to 5.97). Intervention group families showed safe practice for: window (RR 1.30, 95% CI 1.06 to 1.58), fireplace (RR 1.84, 95% CI 1.34 to 2.54), socket (RR 1.77, 95% CI 1.37 to 2.28), smoke alarm (RR 1.11, 95% CI 1.01 to 1.22) and door slam safety (RR 7.00, 95% CI 3.15 to 15.6). Unadjusted results. |
Injury NA Falls NA Hazards Y |
| Gielen 2002 | RCT | Safety counselling by paediatric residents, referral to children's safety centre, plus home visit | No significant differences in safety practices were found observed between study groups. However, a sub‐analysis, independent of study group, found that families who visited the safety centre were significantly more likely to have 3 or more home safety practices observed compared to families who di not (34% vs 17% ≥3, 95% CI 1.30 to 8.82). Although this analysis was adjusted for exposure to safety councelling and a home visit, and the authors found no socio‐demographic confounders; it was based on non‐randomised participants and is therefore susceptible to confounders and self selection bias. |
Injury NA Falls NA Hazards N |
| Hendrickson 2005 | RCT | Counselling, assessment of maternal safety practices and provision of safety items. A researcher counselled mothers regarding hazards reported during the first visit based on Health Belief Model (HBM) constructs. | A statistically significant difference was found in controllable safety hazard (CHS) scores between groups F (1.77) = 99.6, P = 0.00. As well as having fewer observed hazards, mothers receiving the intervention indicated improved self efficacy for home safety behaviours. All significant ANCOVA findings occurred after the intervention. Unadjusted results. |
Injury NA Falls NA Hazards Y |
| Kendrick 1999 | RCT | Safety advice, low‐cost safety equipment and home visit | No significant difference was found in frequency of at least one medically attended injury (OR 0.97, 95% CI 0.72 to 1.30), at least one attendance at an accident and emergency department for injury (OR 1.02, 95% CI 0.76 to 1.37), at least one primary care attendance for injury (OR 0.75, 95% CI 0.48 to 1.17) or at least one hospital admission for injury (OR 0.69, 95% CI 0.42 to 1.12). Unadjusted results. |
Injury N Falls NA Hazards NA |
| King 2005 | RCT | Home hazards assessment, discount coupons for safety devices and information package | Significant reduction in injury visits per patient was shown in the intervention group at 12 months (RR 0.69, 95% CI 0.54 to 0.88). However between 12 and 36 months the effect appeared to diminish (RR 0.8, 95% CI 0.64 to 1.00). Significant reduction in the observed prevalence of homes without hot water (> 54%; OR 1.31, 95% CI 1.14 to 1.50) and the presence of a fire extinguisher (OR 0.81, 95% CI 0.67 to 0.97). Other changes were small and non‐significant. Self reported home safety modifications were reported in 62% of intervention and 23% of control homes (P < 0.05). Unadjusted results. |
Injury Y Falls NA Hazards Y |
| Posner 2004 | RCT | Home visit with structured home safety questionnaire caregivers of those < 5 years given comprehensive home safety education and free safety devices | At 2 months follow‐up the IG demonstrated significantly higher average overall safety scores than the CG (73.3%, SD 8.4%, P ≦ 0.002), and significant improvements in poison (74.4%, SD 19.5, P ≦ 0.02), cut/piercing (81%, SD18.2, P ≦ 0.001) and burn category scores (76.0%, SD 14.9, P = 0.03). Caregivers in the intervention group also demonstrated greater improvement in reported use of the distributed safety devices (65.4%, SD 20.5, P ≦ 0.001). Unadjusted results. |
Injury NA Falls NA Hazard reduction Y |
| Sangvai 2007 | RCT | Multicomponent intervention including focused counselling from a physician and health assistant, educational handouts, phone follow‐up, and access to free safety devices and automobile restraint evaluations. | At 6 months follow‐up smoke detectors were present and functional in 16/17 intervention households and 5/10 control (P = 0.015); hazardous substances not found in low cupboards in 13/16 intervention and 3/10 controls (P = 0.015). However the study was extremely underpowered with only 27 home assessments. No significant difference in medically attended injuries, 19/160 intervention, 22/159 control. Unadjusted results. |
Injury N Falls NA Hazards Y |
| Watson 2005 | RCT | Standardised safety consultation and provision of free safety equipment | At 24 months follow up the attendance rate for injury in primary care was higher (37%) for children in intervention than in the control arm (IRR 1.37, 95% CI 1.11 to 1.70, P = 0.003). Treatment arms did not differ significantly for other injury outcomes. At both one and two years’ follow up, families in the intervention arm were significantly more likely to have a range of safety practices. The intervention arm were significantly more likely to be safe in terms of stairs (OR 1.46, 95% CI 1.19 to 1.80, P = 0.0004), smoke alarms (OR 1.83, 95% CI 1.33 to 2.52, P = 0.0002), windows (OR 1.28, 95% CI 1.02 to 1.59, P = 0.03), and storage of cleaning products (OR 1.34, 95% CI 1.09 to 1.66, P = 0.006) and sharp objects (OR 1.34, 95% CI 1.09 to 1.65, P = 0.005) in the kitchen than families in the control arm. At two years, families in the intervention arm were significantly more likely to be safe in terms of smoke alarms (OD 1.67, 95% CI 1.21 to 2.32, P = 0.002), storage of medicines (OR1.55, CI 1.00 to 2.40, P = 0.05), and cleaning products (OR 1.31, 95% CI 1.07 to 1.60, P = 0.008) in the kitchen than families in the control arm. Absolute differences in the percentages of families with safety practices were, however, small. Unadjusted results. |
Injury N Falls NA Hazards Y |
2. Older people.
| Study ID | Study Type | Intervention | Results | Reduction |
| Becker 2003 | RCT | Staff and resident education on fall prevention, advice on environmental adaptations, progressive balance and resistance training and hip protectors. | Incidence density rate of falls was reduced (RR 0.55, 95% CI 0.41 to 0.73). No significant difference was seen for hip fractures. Lack of validated scoring meant no hazard reduction was recorded. Unadjusted results. |
Injury N Falls Y Hazards NA |
| Campbell 2005 | RCT | Home safety assessment and modification programme, home exercise programme plus vitamin D supplementation, both interventions, or social visits. | 90% of the home safety group participants (152/169) reported as complying partially or completely with one or more recommendations made by the occupational therapist. Fewer falls occurred in the group randomised to receive the home safety programme only, compared to the social visits group (IRR 0.39, 95% CI 0.24 to 0.62). Although a conservative analysis showed neither intervention was effective in reducing injuries from falls, when the home safety programme group was analysed in a single comparison against the social visit group, the home safety programme was shown to significantly reduce injurious falls (IRR 0.56, 95% CI 0.36 to 0.87). *Although a reduction in hazards was observed in the intervention group, no statistical significance test was reported. Unadjusted results. |
Injury Y Falls Y Hazards N* |
| Carter (unpublished) | RCT | Home visit to assess hazards followed by action plan. | The proportion of participants who reported falling did not differ significantly between control group (CG) and either of the intervention groups (IG): brief intervention (OR 0.6, 95%CI 0.3 to 1.1) and intensive intervention (OR 0.8, 95% CI 0.4 to 1.4). The proportion of participants who reported one or more falls resulting in medical attention did not differ significantly between control group (CG) and either of the intervention groups (IG): brief intervention, (OR 0.7, 95%CI 0.2 to 2.2) and intensive intervention (OR 0.7, 95% CI 0.2 to 2.4). The proportion of older people falling in and around their homes was not significantly different between the control group and either of the intervention groups. A significant association was found between intervention and control groups to improve home safety with the brief (35%) and the intensive intervention (49%) groups compared to the control group (28%) over a 12‐month follow‐up. *Although a significant reduction in hazards is reported, no statistical significance test was reported. Unadjusted results. |
Injury N Falls N Hazards Y* |
| Close 1999 | RCT | Home visit to identify hazards. | Risk of falling was significantly reduced in the intervention group (OR 0.39; 95% CI 0.23 to 0.66), as was risk of recurrent falls (OR 0.33; 95% CI 0.16 to 0.68). No significant reductions in the percentage of patients reporting serious injury from falls was found (CG 8% versus IG 4%, P = 0.26). Unadjusted results. |
Injury N Falls Y Hazards NA |
| Cumming 1999 | RCT | Home visit to record hazards and facilitate modifications. | Hazard percentage of homes with modifications recommended; compliance at 12 months:
Remove mats/rugs: 48%; 49%
Change footwear: 24%; 54%
Non‐slip mats: 21%; 75%
Change behaviour: 15%; 60%
Night light: 13%; 58%
Stair rails: 12%; 19%
Remove electrical cords: 12%; 67% Falls were reduced in the intervention subgroup with a history of falls (RR 0.64, 95% CI 0.50 to 0.83). *Although a reduction in hazards was observed in the intervention group, no statistical significance test was reported. Unadjusted results. |
Injury NA Falls Y Hazards N* |
| Day 2002 | RCT | Multifactorial intervention including home hazards management. | The percentage estimated reduction in annual fall rate attributed to home hazard management was not significant (3.1%, 95% CI ‐2.0 to 9.7). There was a significant effect when combined with exercise (9.9%, 95% CI 2.4 to 17.9) and the strongest effect was observed when all three interventions; exercise, home hazard management, vision correction, were combined together (14.0%, 95% CI 3.7 to 22.6) (RR 0.67, 95% CI 0.51 to 0.88). 543 participants receiving the home hazard management intervention 478 were advised to have modifications to their homes. 363 received help to do these modifications which included 275 hand rails fitted, 72 modifications to floor coverings and 72 homes receiving contrast edging to steps. Unadjusted results. * Although hazards were reduced in the intervention homes, no statistical significance test was reported. |
Injury NA Falls Y Hazards N* |
| Elley, 2008 | RCT | Multicomponent intervention. Home‐based nurse assessment of falls and fracture risk factors and home hazards, referral to appropriate community interventions, and strength and balance exercise programme. | The incidence rate ratio for falls for intervention group compared with the control group, over the 12 month follow‐up period, was 0.96 (95% CI 0.7‐1.34). There was no significant difference in secondary outcomes between the two groups. Unadjusted results. |
Injury N Falls N Hazards NA |
| Gitlin 2006 | RCT | Multicomponent intervention involving home modifications and training in their use, instruction in strategies of problem solving, energy conservation, safe performance, and fall recovery techniques; and balance and muscle strength training. | Fewer home hazards were observed in the intervention group than in the control group. The difference of adjusted means for environmental hazards at 6 months was ‐1.53 (P = 0.05) which appears non‐effective. The difference of adjusted means for environmental hazards at 12 months was ‐1.38, (95% CI ‐3.17 to 0.41, P = 0.13) which was non‐significant. In both, the difference of adjusted means were adjusted for race, living arrangements, number of recent fallers and near falls, and perceived ability to manage fall risks and control falling and health conditions. |
Injury NA Falls NA Hazards N |
| Hendricks 2008 | RCT | 333 community dwelling Dutch people aged 65 and over who were seen in an emergency department after a fall. Participants were also recruited from the GP Cooperative. | No significant differences between the two groups were observed in terms of falls. At least one fall: 4 months (OR 1.36, 95% CI 0.77 to 2.41, (P = 0.29)), 12 months (OR 0.86 (0.50 to 1.49) P = 0.59). More than 1 fall: 4 months (OR 0.91, 95% CI 0.39 to 2.11 (P = 0.83)), 12 months (OR 0.95, 95% CI 0.51 to 1.78 (P = 0.87)). injurious falls: 4 months (OR 0.79, 95% CI 0.31‐2.0, (P = 0.62)), 12 months (OR 0.77, 95% CI 0.35‐1.73, (P = 0.53)). Unadjusted results. |
Injury N Falls N Hazards NA |
| Hogan 2001 | RCT | Home visit to assess environmental risk factors followed by treatment plan. | No significant differences between the control and intervention groups in the cumulative number of falls (311 versus 241, P = 0.34), having one or more falls (79.2% versus 72.0%, P = 0.30) or in the mean number of falls (4.0 versus 3.2, P = 0.43). Unadjusted results. |
Injury NA Falls N Hazards NA |
| Jensen 2002 | RCT | Multifactorial fall prevention programme comparing staff education, environmental adjustment, exercise, drug reviews, aids, hip protectors and post fall problem solving conferences. | An interdisciplinary and multifactorial prevention programme targeting residents, staff and the environment may reduce falls and femoral fractures. During the 34‐week follow‐up period, 44% of residents in the intervention group sustained a fall compared with 56% in the control group (RR 0.78, 95% CI, 0.64 to 0.96). The odds ratio adjusted for baseline factors was 0.49 (95% CI 0.37 to 0.65), and the incidence rate ratio of falls adjusted for baseline factors was 0.60 (95% CI 0.50 to 0.73). Three people in the intervention group and 12 people in the control group had a fracture to the femur (adjusted odds ratio, 0.23 (CI 0.06 to 0.94)). In a later report (Jensen 2003) the effect of this intervention in older people with differing levels of cognitive function was investigated. 59 minor, moderate or serious injuries occurred in the higher cognitive group (IRR 0.9, 95% CI 0.5 to 1.5) compared with the control group and similarly in the lower cognitive group (IRR 0.9, 95% CI 0.5 to 1.3). However in the lower cognitive group the 171 participants sustained 10 femoral fractures, all of which were in the control group (P = 0.006). |
Injury Y Falls Y Hazard NA |
| Mahoney 2007 | RCT | Home visits to assess falls risk factors, recommendations to participant and physician, exercise plan, and 11 monthly telephone calls. | There was no difference in rate of falls between the intervention and control groups (RR 0.81, P = 0.27). Nursing home days were fewer in the intervention group (10.3 vs 20.5 days, P = 0.04). Intervention subjects with a Mini‐Mental State Examination (MMSE) score of 27 or less had a lower rate of falls (RR 0.55; P = 0.05) and, if they lived with someone, had fewer hospitalisations (RR 0.44, P = 0.05), nursing home admissions (RR 0.15, P = .003), and nursing home days (7.5 vs 58.2, P = .008). Unadjusted results. |
Injury NA Falls N Hazard NA |
| Nikolaus 2003 | RCT | Home visit with advice about environmental hazards, offer of facilities to change them and training in the use of mobility and technical aids. | Intervention group had 31% fewer falls than control group (IRR 0.69, 95% CI 0.51 to 0.97).
Study not designed to examine fall related injuries.
Compliance rate of 75.7% with at least one recommended hazard change.
Participants who made at least one recommendation experienced a significant reduction in the rate of falls (IRR 0.64; 95% CI 0.37 to 0.99).
The number of falls in those in the intervention group with no modifications was not significantly different from those in the control group (IRR, 1.05, 95% CI 0.82 to 1.41). Unadjusted results. * Although hazards were reduced in the intervention homes, no statistical significance test was reported. |
Injury NA Falls Y Hazards N* |
| Pardessus 2002 | RCT | Home visit that assessed environmental hazards and recommended modifications. | Rate of falls, hospitalisation for falls were not significantly different between the two groups. Unadjusted results. |
Injury N Falls N Hazards NA |
| Salminen 2009 | RCT | 12‐month fall prevention programme based on individual risk analysis; geriatric assessment, counselling and guidance in fall prevention, home hazard assessment, group physical exercise, home exercise, lectures in groups and psychosocial groups. | The intervention did not reduce the incidence of falls overall (IRR for I vs C 0.92, 95% CI = 0.72 to 1.19) or the incidence of falls requiring medical treatment (IRR 0.87, 95% CI 0.63 to 1.21). However in subgroup analysis, significant interactions between subgroups and groups (I and C) were found for depressive symptoms (P = .006), number of falls during previous 12 months (P = .003), and self‐perceived risk of falling (P = .045). Unadjusted results. |
Injury N Falls N Hazards NA |
| Shaw 2003 | RCT | Multifactorial intervention including medication review, vision, blood pressure, mobility, footwear and an assessment of home environmental fall hazards and modification using standard checklists. | No significant differences between two groups in proportion who fell after 1 year or in injuries sustained.
Compliance with hazard advice was 41/105 in intervention group and 8/111 in control. Unadjusted results. * Although hazards were reduced in the intervention homes, no statistical significance test was reported. |
Injury N Falls N Hazards N* |
| Stevens 2001 | RCT | Home visit to assess hazards, installation of free safety devices and educational strategy. | No significant reduction in the intervention group in the incidence rate of falls involving environmental hazards inside the home (adjusted rate ratio 1.11; 95% CI 0.82 to 1.50), or the rate of falls inside the home (adjusted rate ratio 1.17; 95% CI 0.85 to 1.60). There was no significant reduction in the rate of injurious falls in intervention subjects (adjusted rate ratio 0.92; 95% CI 0.73 to 1.14). Rate ratios were adjusted for the covariates of age, sex, history of falling, sole participation, recruitment method and use of walking aid. Two‐thirds of falls that occurred inside the home involved an environmental hazard ‐ most frequently implicated falls were caused by furniture (25%), steps (19%), wet and slippery floors (13%), objects on the floor (9%) and mats and rugs (7%). Statistically significant improvements in a sample (n = 51) of the larger study were reported in: unsafe steps (mean 0.61, 95% CI 0.28 to 0.94), stabilisation of rugs and mats (mean 1.27, 95% CI 0.91 to 2.24), rooms with trailing cords (mean 0.43, 95% CI 0.10 to 0.76) and rooms with an unsafe favourite chair (mean 0.10 95% CI 0.02 to 0.18). Whilst the authors reported other results as significant, no statistical significance test was reported. |
Injury N Falls N Hazards Y |
| Tinetti 1994 | RCT | Home visit assessment and changes made to environmental hazards. | The adjusted incidence ratio for falling in the intervention group as compared with the control group was 0.69; 95% CI 0.52 to 0.90. The incidence rate ratio was adjusted for the number of previous falls (0,1,2 or > 3) during the follow‐up and for the week of follow‐up in order to account for non‐independence of recurrent falls. Changes in physical hazards were not reported. | Injury NA Falls Y Hazards NA |
| van Haastregt 2000b | RCT | Home visit screening for environmental & behavioural factors. | Odds ratios for the intervention group for at least one fall was 1.3, 95% CI 0.7 to 2.1 and for an injurious fall 1.4, 95% CI 0.8 to 2.6. Changes in physical hazards were not reported. Unadjusted results. |
Injury N Falls N Hazards NA |
| Vetter 1992 | RCT | Home visit to provide environmental hazards check. | Similar proportions of fractures were observed in both groups (5% (I) versus 4% (C)). More falls without fracture occurred in the intervention group (23% (I) versus 16% (C)). Stratifying by disability there were more falls for all disability levels in the intervention group participants.
No results reported related to changes in environmental hazards and no indication of uptake/self reported falls and injurious falls implementation. Unadjusted results. |
Injury N Falls N Hazards NA |
Discussion
It is logical to presume that the presence of environmental risk factors must play some part in the cause of injuries in the home. However, despite the inclusion of 29 randomised trials, the findings of this review suggest that there is little high‐level scientific evidence for modification of the built home environment as a method of reducing the risk of injury. It should be remembered that only some home injuries are due to environmental hazards and that removal of such hazards or provision of safety equipment can only influence the occurrence or severity of these particular injuries. As most studies reported all injuries as their outcome, this will have the effect of reducing the power to detect changes in falls and injuries due to environmental hazards. Most studies did not provide enough detail in their results to ascertain the mechanism of injuries, probably as such information was not available to them and is difficult to systematically collect from participants or routine data sources.
Summary of the main findings
Thirteen of the studies in the older people group reported injuries as an outcome. However, only two of these studies reported a significant reduction in injuries (Campbell 2005; Jenson 2002). Campbell 2005 reported significantly fewer injurious falls in the intervention group (IG) compared to the control group (CG) (IRR 0.39, 95% CI 0.24 to 0.62) and Jenson 2002's study found a significant reduction in femoral fractures in the IG (adjusted OR 0.23, 95% CI 0.06 to 0.94) but no reductions in falls that resulted in minor or moderate injuries. Campbell 2005 used a 2×2 factorial study design, and specifically targeted interventions towards older people with severe visual impairment, which may mean the results from this study are not generalisable to other populations. The home safety intervention was delivered by an occupational therapist and included a home safety assessment and modifications to the home environment if indicated. In contrast, Jenson 2002's study was set in a residential care facility in Sweden, and used an 11‐week multifactorial programme which included general and individualised strategies focusing on: educating staff; modifying the environment; implementing exercise programmes; medication reviews and providing free hip protectors. Campbell 2005's factorial study design allowed the home safety programme to be evaluated in isolation and potentially permits a direct link to be made between the home safety programme and subsequent reduction in injuries. This is not possible in Jenson 2002's study due to their multifactorial study design. Jenson 2002 also stresses that no femoral fractures occurred in residents wearing hip protectors and suggest that their use may have contributed towards this result. When comparing results across studies, it should be considered that hazard prevalence and other risk factors for having a fall or injury vary by setting and hence variation in effect sizes of interventions is to be expected.
Out of the nine studies involving children, five reported injuries as an outcome. Only one of these studies reported significantly fewer self‐reported injuries in the IG (King 2005) at 12 months' follow‐up (RR 0.69, 95% CI 0.54 to 0.88) and a borderline result at 36 months' follow‐up (RR 0.8, 95% CI 0.64 to 1.00). None of the studies involving children reported a significant reduction in medically attended injuries. King 2005's study was aimed at children under eight years old, and intervention participants received a single home visit that included an information pack, discount coupons, and specific instructions regarding home safety measures. Interestingly, out of the 16 safety modifications, only hot water temperature was shown to be significantly lower in the intervention households (OR 1.31, 95% CI 1.14 to 1.50).
In an earlier report (King 2001), the actual observation of hazard changes was at variance with the self‐reported adoption of safety precautions. The authors conclude that it is unlikely that the intervention had an impact on the adoption of home safety measures and that other effects of the intervention, such as behavioural changes, might explain the reduction in injuries.
Key themes and relevance of evidence
Although the focus of this systematic review is on the prevention of injuries by modifications of the home environment, most of the studies focusing on older people used the incidence of falls rather than the rate of injuries as their main outcome measure. Although the majority of fractures in older people follow a fall, only around one in 20 falls leads to a fracture (Rubenstein 2001). A reduction in the proportion of people in an IG suffering a fall should lead to a similar reduction in the proportion suffering a fracture, but the absolute number of fractures prevented will be much smaller.
Studies using fracture incidence as their endpoint would need to be very much larger in scale, and this explains the literature's focus on fall prevention. There is no doubt that falls and the fear of falling are significant public health problems in themselves, but one cannot automatically assume that success in a falls prevention strategy will necessarily be reflected in reduced rates of injuries or fractures.
Additionally the vast majority of these studies were multifactorial and the effect of home modification on falls was either inseparable or insignificant. However this is a problem posed by the fact that falls, injuries or fractures in older people are commonly multifactorial in origin. A child may suffer a fracture that reflects the severity of the trauma, but over 95% of fractures in older people occur after only minor or moderate trauma (Johansen 1999). Factors underlying the causes of falls or the reduced ability to react and cushion the impact, and those affecting bone fragility are all relevant to the occurrence of injuries in older people.
Environmental modification cannot address all of these factors and injury prevention studies in older people therefore tend to be multifactorial in nature. This makes it more difficult to distinguish the contribution of environmental modification to the effectiveness of any strategy. An example of this is Nikolaus 2003 who found 31% fewer falls in the IG than in the CG however the intervention also included training in the use of technical and mobility aids. However, participants who made at least one of the home modifications at 12 months' follow‐up did experience a significant reduction in the rate of falls (IRR 0.64, 95% CI 0.37 to 0.99, P = 0.047). In contrast, Day 2002 used a rigorous factorial design where the separate and combined effects of exercise training, vision improvement and house hazards management on falls could be assessed. Although the study reported non‐significant reductions in falls following home hazard management as a sole intervention, when combined with both of the other interventions positive additive effects were reported. However, the beneficial effects were only significant when the combination of interventions contained an exercise component.
Studies in this review tended to be conducted in areas, countries or settings where the major environmental hazards have already been removed. Studies in low and/or middle income countries (LMICs) were largely absent from the literature and this may reflect issues in funding this type of study in these settings. Our selection criteria, which excluded housing which was not subject to housing regulations, also meant that studies conducted in potentially more hazardous environments were unlikely to be included. Given this, only modest changes may be possible in settings where the major environmental hazards have already been removed. Furthermore the fact that only a proportion of all falls or injuries can be addressed by additional environmental changes means that many studies which were powered to detect changes in all falls or injuries suffer from low statistical power when the outcome of interest is falls or injuries associated with hazards. Most trials with the prevention of injuries as an outcome require large numbers using all injuries as an outcome and it may not be feasible to fund or implement adequately powered studies to detect modest changes in injuries due to modification of specific environmental hazards.
Campbell 2005's study was the only study to demonstrate a direct association between the home safety component of the intervention and a significant reduction in falls. However, the authors reported that there was no significant difference between falls occurring inside and outside the home, where the home modification intervention could not have influenced the risk of falling. This result has also been reported in other studies (Cumming 1999 and Nikolaus 2003) and led Campbell 2005 to suggest that the reduction in falls may have been due to a combination of the occupational therapist's fall prevention advice as well as the environmental modifications in the home.
A number of studies involving older people reported a reduction in home hazards which did not translate into a reduction in falls or injuries (Carter unpublished; Shaw 2003; Stevens 2001). Further, several studies reported no significant reduction in injuries, falls or hazards (Elley 2008; Gitlin 2006; Hendriks 2008; Hogan 2001; Mahoney 2007; Pardessus 2002; Salminen 2009; Van Haastregt 2000b; Vetter 1992). The authors suggest several possible explanations for the ineffectiveness of their studies.
Mahoney 2007 speculated that low intensity interventions which rely upon recommendations and referrals may be too indirect to be effective, but that financial constraints may prevent the successful implementation of higher intensity fall prevention programmes. Mahoney 2007's study demonstrated that telephone follow‐up alone is not necessarily efficacious in increasing the effectiveness of an intermediate multifactorial study based upon recommendations and referrals.
There is also a debate as to whether multiple or single factor fall prevention programmes are more effective. Although meta‐analyses have shown that multifactorial fall prevention programmes reduce the number of falls (Chang 2004; Campbell 2007), a recent meta‐analysis found that the number of people having at least one fall did not reduce significantly in multifactorial interventions and that the benefit of multifactorial programmes may be less than first thought (Gates 2007). In addition, a meta‐analysis of two studies carried out in our review found a multifactorial fall prevention intervention including home assessment and modification, medication review and health and bone assessment, and an exercise programme to be ineffective at reducing falls in older people (RR 1.09, 95% CI 0.97 to 1.23). Many authors have proposed that multiple component interventions may act to lessen the impact of their individual components (Elley 2008; Salminen 2009) and Campbell 2007 has shown that multifactorial programmes may lead to lower adherence rates in some part or parts of the intervention.
Campbell 2005 found that participants who received a combined intervention of home safety and exercise were more likely to fall or suffer an injurious fall than those who received only the home safety programme. The fall rate was also found to be greater in participants who received the exercise programme compared to the CG, albeit not significantly. The results of this study are in stark contrast to the results of Day 2002 which found the exercise component of their factorial study to be the most effective at reducing falls. Campbell 2005 concluded that although the Otago exercise programme has been shown to be successful in other populations (Campbell 1997; Robertson 2001; Robertson 2001a), in a population of older people with severe visual impairment, the programme may be unsuitable and potentially harmful.
Hendriks 2008's study highlighted the potential impact a different health care setting can have on the outcomes of a fall prevention programme. Hendriks 2008 based their programme on a multifactorial fall prevention study that had been carried out in the UK (Close 1999). However, unlike the UK study which found the programme to have significantly beneficial effects on the number of participants experiencing a fall (Close 1999), the Hendriks 2008 study, which was carried out in a Dutch healthcare setting, reported no statistically significant effect on falls. Although the authors provide several possible theories for the ineffectiveness of their study, they emphasise that the adaptations to the protocol which were required to implement the programme into the Dutch healthcare setting may have been one of the main causes. By introducing two new professional disciplines into the study (rehabilitation physician and geriatric nurse) and by involving GPs, the implementation period was extended by approximately 3.5 months. The study authors suggest that the extended time period between fall and completion of the intervention, may have reduced the efficacy of the programme in this healthcare setting.
It is also possible that a number of the multifactorial studies were underpowered to detect a statistically significant difference. An earlier meta‐analysis suggested that a 30% relative reduction in falls was an attainable result for a multifactorial fall prevention programme (Chang 2004). However a more recent meta‐analysis reported that a smaller relative reduction, approximately 10 percent, might be expected (Gates 2007). A number of studies including Salminen 2009 calculated their sample size based on a 30% difference and therefore these studies may have been underpowered to detect a 10% reduction in falls.
Nonetheless multifactorial fall prevention programmes have demonstrated positive results. One of the first successful fall prevention studies used a multifactorial design (Tinetti 1994) and Jenson 2002, a multifactorial study set in a residential care home, reported significant reductions in falls and femoral fractures in the IG.
Overall there were nine included studies involving children (Babul 2007; Clamp 1998; Gielen 2002; Hendrickson 2005; Kendrick 1999; King 2005; Posner 2004; Sangvai 2007; Watson 2005). Although King 2005 reported a significant reduction in self‐reported injuries in the IG, they found that a single home visit was insufficient to encourage a lasting adoption of home safety measures. King 2005 concluded that a successful home visitation programme may require several home visits in order to develop a more therapeutic relationship with the participant, so that wider issues which may affect a child's safety can be addressed. Watson 2005 unexpectedly found a significant increase in primary care attendances in the IG, even though the prevalence of safety practices in this group was significantly increased compared to the CG. As well as proposing possible explanations for this result, Watson 2005's study highlights the difficulties in demonstrating a reduction in injuries using RCT's. As the prevalence of safety features is high and the incidence of injuries that could be prevented from these safety features is low, very large sample sizes are usually required. One alternative offered by Watson 2005's study is to conduct well designed case‐control or cohort studies to examine the effect of safety equipment followed by RCTs to investigate strategies for the increased uptake of effective safety equipment. Hewitt 2008 challenges this approach, arguing that observational studies are potentially biased and this is why we conduct randomised trials. Specifically they assert that Watson 2005's result indicates potential for harm caused by the intervention.
Five studies (Clamp 1998; Gielen 2002; Gitlin 2006; Hendrickson 2005; Posner 2004) in this review assess a change in safety features or hazards without reporting injury occurrence. Whilst it is logical to deduce that physical hazards in the home will contribute to a sequence of events culminating in an injury, it is not possible to conclude that the modification of such hazards will definitely reduce the number of injuries. However, even though a direct association can not be made between hazard reduction and injury reduction, the three studies which reported a significant reduction in hazards (Clamp 1998; Hendrickson 2005; Posner 2004) can be viewed encouragingly.
Although Sangvai 2007 reported significant reductions in hazards in the IG, the very large losses to follow‐up may have been a potential source of bias. The more enthusiastic participants who implemented the home safety intervention more effectively may have been more likely to agree to a follow‐up home visit. This may have led to an over‐estimation of the effectiveness of this intervention.
Although Gielen 2002 found no significant difference in safety practices between study groups, an adjusted sub‐analysis revealed families who visited the safety centre were significantly more likely to have 3 or more safety practices compared to families who did not (34% vs 17% ≥3). However these results should be interpreted with caution, given the analysis was based on non‐randomised participants. The study authors mentioned that during the home visit safety products were not installed due to concerns around liability. Other studies which have since obtained liability waivers and installed safety products have been shown to be more successful (King 2005).
It is worth noting that there are currently no RCTs included in the mixed age group. A controlled clinical trial by Petridou 1997 included only 172 households and 636 people in the IG. Significant improvement in the provision of automatic electricity cut off devices and better lighting in corridors as well as first aid kits were reported post intervention but there were no changes in structural or expensive interventions, for example, modification to stairs or balconies. A non‐significant 21% reduction in home injuries was reported (95% CI ‐40% to +6%).
Meta‐analysis issues
Attempting to carry out meta‐analyses with the studies included in this review proved to be problematic. The majority of studies included were too methodologically and statistically heterogenous to combine the results. Specifically, studies varied in terms of the characteristics of the population, inclusion and exclusion criteria and components of the intervention. Populations varied in terms of age, cognitive function and physical ability. Inclusion and exclusion criteria differed inasmuch as studies might include only those who had had a previous fall, attended the emergency department or been admitted to hospital after a fall. This may mean that populations in these studies could be considered at higher risk of falling and thus results might be less generalisable. Components of the interventions differed greatly. Participants might be visited at home or not, safety equipment might be free, means tested, directly supplied or referral made to a service where it could be obtained. Medication reviews were sometimes carried out, exercise programmes might be included and, if so, provided directly or referred to a programme. In some studies direct assistance with hazard modification might be provided or advice only given. Outcomes also differed. These included falls, injurious fall, fractures, self reported injuries and medically attended injuries. When studies appeared methodologically similar and combining data appeared plausible, we attempted meta‐analysis. In the end only one meta‐analysis was included in this review, as the other attempted analyses were too statistically heterogeneous.
Conclusion
The conclusion of this systematic review is that there is very little high‐grade evidence that interventions to modify the home physical environment affect the likelihood of sustaining an injury in the home.
The first version of this review included 28 studies (13 RCTs, 14 CCTs and one before‐and‐after study). The 2006 update identified six additional RCTs which allowed the inclusion criteria to be limited to higher quality randomised controlled studies. In this update we identified a further 10 RCTs. However this review still does not provide a clear, unequivocal evidence base that modification of the home environment reduces injuries. None of the studies focusing on children demonstrated a reduction in injuries that might have been due to environmental adaptation in the home; one study reported a reduction in injuries and hazards but the two could not be directly associated. Of the 20 included studies in the older people category, none demonstrated a reduction in injuries that could be directly linked to hazard reduction, although two demonstrated a reduction in falls that may have been due to environmental hazard reduction in the home. This is not the same as saying that such interventions are ineffective. It should be remembered that many of the studies in this review were powered to detect changes in all falls and injuries. Therefore it is likely that these studies were under‐powered to detect a change in falls and injuries that occurred specifically as a result of an environmental hazard in the home. In addition, it is often difficult to fund studies which focus on the prevention of injuries as an outcome, as large numbers of participants are often required for the study to be adequately powered. The studies in this review also tended to be conducted in areas where the major environmental home hazards had already been removed, making it possible for only modest changes in the environment to be observed. It is also important to highlight that, due to the stringent exclusion criteria for this review, studies may have been excluded where allocation concealment was carried out but not reported adequately in the methodology.
Although the debate surrounding the effectiveness of multifactorial interventions continues, they have been shown to be effective at reducing falls (Day 2002; Becker 2003; Jenson 2002; Nikolaus 2003; Tinetti 1994). It is important however to know the cost‐effectiveness of specific components of multifactorial interventions, so that scarce resources can be targeted to the most effective interventions. In order to answer these questions, future studies should adopt a factorial design and have sufficient power to detect modest, but important, changes in injury occurrence.
Limitations of the review
Publication bias can threaten the validity of systematic reviews if research which does not reach statistical significance or produces a counter‐intuitive result is not published. We searched a large number of electronic databases covering health, social science and architectural domains. Although we contacted first authors of all included studies, we did not contact lead researchers in this update to ask about unpublished material, as in the first review it had a very low yield and was resource intensive. We cannot rule out the possibility, therefore, of missing studies published in journals not indexed in the electronic databases and which have not been referenced in any of the included studies. This review is limited to interventions with primary outcomes of reductions in injuries, falls and the prevalence of home hazards. It does not comment on the effectiveness of physical modification of the home environment with the intention of influencing other outcome measures, for example, morbidity, satisfaction, independence or quality of life.
Authors' conclusions
Implications for practice.
The conclusion of this systematic review is that there is very little high‐grade evidence that interventions to modify the home physical environment affect the likelihood of sustaining an injury in the home.
Injuries occur as a result of complex interactions between individuals and the environment and can always be considered multifactorial in nature. The results of this systematic review of modifying the physical environment in the home to reduce injuries (with the exception of the provision and promotion of smoke alarm ownership, which was excluded from the review) demonstrate a paucity of evidence on which to base current practice. Whilst it is logical to deduce that physical hazards and poor design and layout contribute to a sequence of events culminating in an injury, it is not possible to conclude that the amelioration of such hazards will definitely reduce the number of injuries. Nor is it possible to determine which aspects of multifactorial interventions are most cost effective. In the absence of good quality evidence, it is human nature for individuals to use interventions in the hope that they might be effective. This review has not shown that such interventions do not work. Limitations within the studies meant it was difficult to reach definitive conclusions in most cases.
Implications for research.
RCTs provide the gold standard for the assessment of the effectiveness of interventions. This review shows the paucity of appropriately designed and sized studies to test the effectiveness of interventions to remove or reduce physical hazards in the home environment in reducing injury occurrence.
Studies were generally too small to have sufficient power to detect anything but a very large effect and rarely employed a factorial design that would allow an assessment of specific interventions as part of a multifactorial intervention. Most studies had very low uptake rates for interventions. The active involvement of participants in the design of studies might improve this. The challenge to the global injury research community is to collaborate to design and implement studies of a sufficient size, rigorous design and acceptability to participants to answer these important questions.
What's new
| Date | Event | Description |
|---|---|---|
| 3 October 2011 | Amended | Minor edits have been made to the text which provide additional information about the Gielen 2002 study. |
History
Protocol first published: Issue 3, 2002 Review first published: Issue 4, 2003
| Date | Event | Description |
|---|---|---|
| 30 September 2010 | New citation required but conclusions have not changed | This updated review includes 10 new studies identified in literature searches performed to December 2009.
There are 28 completed published randomised controlled trials and one unpublished study investigating the effect on injuries of modification of the home environment.
There are no randomised controlled trials that met the inclusion criteria in the mixed age group.
There is still insufficient evidence to determine the effects of interventions to modify environmental home hazards on injury occurrence. The authors of the review have changed. |
| 11 July 2008 | Amended | Converted to new review format. |
| 16 August 2006 | New search has been performed | August 2006 This update of the original review includes studies identified in literature searches performed to December 2004. Since the original study a further six randomised controlled trials have been indentified and the review is now limited to high quality randomised controlled trials, providing the best evidence available. There are 18 completed published randomised controlled trials and one unpublished study investigating the effect on injuries of modification of the home environment. There are no randomised controlled trials that met the inclusion criteria in the mixed age group. There is still insufficient evidence to determine the effects of interventions to modify environmental home hazards. |
Acknowledgements
The authors would like to thank Emma Sydenham from the Cochrane Injuries Group for her guidance and support during the review process.
The authors would also like to thank everyone who has contributed towards earlier versions of the review including: Lesley Victoria Sander, Sinead Brophy, Nikki Weaver, Sian King, Antony Johansen, Alison Kemp, Joanne Patterson and Ben Rolfe, Frances Bunn, Katherine Ker, Stephen Palmer & Sylvia Morgan.
Appendices
Appendix 1. Search strategy
The searches were based on the following strategy, developed in MEDLINE and adapted as appropriate to the specifications of each database. The strategy was deliberately designed to capture a broad range of references and the 'explode' feature was used wherever this was applicable to the database. There were no language restrictions.
ASSIA (2004 to December 2009)
Search Query #25 ((DE=("accommodation" or "cottages" or "flats" or "houses" or "local authority housing" or "sheltered housing" or "buildings")) or(home) or(DE="ergonomics") or(DE="home environment") or(stair or staircase or stairwell) or(DE=("local authority housing" or "local authorities")) or(bedsit) or(maisonette*) or(dwelling)) and((DE=("accidents" or "burns" or "fractured" or "injuries" or "lesions" or "suffocation")) or(falls) or(DE="falls") or(falling) or(accident*)) (Copy Query)
| 322 Published Works results found in Multiple Databases + 29,056 Scholars results found in COS Scholar Universe: Social Science 82 Web Sites results found in Web Resources Related to the Social Sciences/Humanities |
| Date Range: | 2004 to 2009 |
British Nursing Index (BNI) (1994 to December 2009)
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 (housing or house*).mp. (899) 2 (home or homes or abode*).mp. (6716) 3 accommodation*.mp. (163) 4 (residence* or residential).mp. (1180) 5 (apartment* or flat).mp. (23) 6 (building* or estate*).mp. (643) 7 (neighbourhood* or neighborhood*).mp. (82) 8 urban environment*.mp. (6) 9 buil* environment*.mp. (12) 10 ergonomic*.mp. (63) 11 local authorit*.mp. (141) 12 environment* design*.mp. (5) 13 living quarter*.mp. (3) 14 (staircase or stairs or stairwell).mp. (9) 15 exp housing/ (162) 16 exp Elderly Housing/ (158) 17 or/1‐16 (8852) 18 exp Elderly : Accidents/ (549) 19 exp Children : Accidents/ (408) 20 (injury or injuries).mp. (2172) 21 (accident* or wound*).mp. (7717) 22 (fall* or scald* or burn*).mp. (1424) 23 (suffocat* or poison*).mp. (320) 24 exp Burns/ (285) 25 exp poisoning/ (200) 26 or/18‐25 (10139) 27 17 and 26 (397) 28 limit 27 to yr="2004 ‐ 2009" (258)
CINAHL (2004‐December 2009)
| Search ID# | Search Terms |
| S17 | (S9 and S16) |
| S16 | (S10 or S11 or S12 or S13 or S14 or S15) |
| S15 | (MH "Accidental Falls") |
| S14 | (MH "Fractures") |
| S13 | (MH "Burns") |
| S12 | (MH "Poisons") |
| S11 | (MH "Accidents") |
| S10 | (MH "Wounds and Injuries") |
| S9 | (S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8) |
| S8 | ("ergonomics") or (MH "Ergonomics") |
| S7 | (MH "Home Environment") |
| S6 | "neighbourhood" |
| S5 | "apartment" |
| S4 | "accommodation" |
| S3 | "stairs" |
| S2 | (MH "Residence (Omaha)") |
| S1 | (MH "Housing for the Elderly") or (MH "Public Housing") or (MH "Housing") |
Cochrane Library (2004‐December 2009)
| ID | Search |
| #1 | MeSH descriptor Housing explode all trees |
| #2 | MeSH descriptor Homes for the Aged explode all trees |
| #3 | apartment |
| #4 | flat |
| #5 | accommodation |
| #6 | maisonette |
| #7 | home* |
| #8 | ergonomics |
| #9 | stairs |
| #10 | stairway |
| #11 | staircase |
| #12 | local authority |
| #13 | (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12), from 2004 to 2009 |
| #14 | MeSH descriptor Wounds and Injuries explode all trees |
| #15 | MeSH descriptor Accidents explode all trees |
| #16 | MeSH descriptor Accidental Falls explode all trees |
| #17 | MeSH descriptor Fractures, Bone explode all trees |
| #18 | MeSH descriptor Burns explode all trees |
| #19 | (#14 OR #15 OR #16 OR #17 OR #18), from 2004 to 2009 |
| #20 | (#13 AND #19), from 2004 to 2009 |
EMBASE (1996 to 2009 Week 50)
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 (housing or house*).mp. (51121) 2 (home or homes or abode*).mp. (63648) 3 accommodation*.mp. (5162) 4 (residence* or residential).mp. (23053) 5 (apartment* or flat).mp. (12495) 6 maisonette*.mp. (1) 7 (condo or condominium*).mp. (16) 8 (dwelling or domocil*).mp. (6732) 9 (menage or bedsit*).mp. (79) 10 (building* or estate*).mp. (24941) 11 (neighbourhood* or neighborhood*).mp. (5520) 12 urban environment*.mp. (1053) 13 buil* environment*.mp. (343) 14 ergonomic*.mp. (4700) 15 local authorit*.mp. (675) 16 environment* design*.mp. (193) 17 living quarter*.mp. (32) 18 (staircase or stairs or stairwell).mp. (1702) 19 exp housing/ (3259) 20 exp home/ (3652) 21 or/1‐20 (182349) 22 exp accident/ (42332) 23 exp accident prevention/ (4661) 24 exp accident proneness/ (333) 25 exp home accident/ (575) 26 (injury or injuries).mp. (336796) 27 (fall* or scald* or burn* or wound*).mp. (152114) 28 exp fracture/ (63681) 29 (suffocat* or poison*).mp. (22475) 30 poison/ (434) 31 exp fire/ (2195) 32 exp burn/ (15057) 33 or/22‐32 (537720) 34 random$.ti,ab. (314126) 35 factorial$.ti,ab. (6755) 36 (crossover$ or cross over$ or cross‐over$).ti,ab. (24439) 37 placebo$.ti,ab. (74183) 38 (doubl$ adj blind$).ti,ab. (51338) 39 (singl$ adj blind$).ti,ab. (4862) 40 assign$.ti,ab. (82683) 41 allocat$.ti,ab. (26205) 42 volunteer$.ti,ab. (62897) 43 crossover procedure/ (18016) 44 double blind procedure/ (55904) 45 randomized controlled trial/ (147415) 46 single blind procedure/ (7826) 47 or/34‐46 (491729) 48 limit 47 to human (391555) 49 21 and 33 and 48 (1956) 50 limit 49 to yr="2004 ‐ 2009" (1093)
ICONDA (1976 to December 2009)
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 "Housing and Houses".de. (445) 2 dwelling.de. (2941) 3 housing for the elderly.de. (1497) 4 urban design.de. (4245) 5 multiple dwelling.de. (3379) 6 ergonomics.de. (581) 7 Houses.de. (3413) 8 (housing or house*).mp. (74296) 9 (home or homes or abode).mp. (10034) 10 accommodation*.mp. (1932) 11 (residence* or residential).mp. (40396) 12 (apartment* or flat).mp. (15208) 13 (housing or house*).mp. (74296) 14 (condo or condominium*).mp. (237) 15 maisonette*.mp. (854) 16 living quarter*.mp. (75) 17 Neighbourhood.de. (842) 18 built environment.mp. (1559) 19 (staircase or stairs or stairwell).mp. (4154) 20 or/1‐19 (113286) 21 (injury or injuries).mp. (1210) 22 (accident* or wound*).mp. (7428) 23 (scald* or burn*).mp. (3217) 24 (suffocat* or poison*).mp. (219) 25 fire.de. (4862) 26 poison.mp. (81) 27 safety.de. (6334) 28 (fall or falling or fell).mp. (2880) 29 or/21‐28 (24079) 30 20 and 29 (2047) 31 limit 30 to yr="2004 ‐ 2009" (395)
MEDLINE (1996 to November Week 3 2009)
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 (housing or house*).mp. (60035) 2 (home or homes or abode*).mp. (81935) 3 accommodation*.mp. (4838) 4 (residence* or residential).mp. (29931) 5 (apartment* or flat).mp. (13317) 6 maisonette*.mp. (1) 7 (condo or condominium*).mp. (15) 8 (dwelling or domocil*).mp. (7671) 9 (menage or bedsit*).mp. (78) 10 (building* or estate*).mp. (24964) 11 (neighbourhood* or neighborhood*).mp. (6806) 12 urban environment*.mp. (1032) 13 buil* environment*.mp. (390) 14 ergonomic*.mp. (2779) 15 local authorit*.mp. (800) 16 environment* design*.mp. (1876) 17 living quarter*.mp. (47) 18 (staircase or stairs or stairwell).mp. (1742) 19 exp Housing/ (9771) 20 exp Public Housing/ (459) 21 exp Housing for the Elderly/ (949) 22 exp "Facility Design and Construction"/ (7407) 23 or/1‐22 (218709) 24 exp Accidents/ (61762) 25 exp Accidents, Home/ (1284) 26 exp Accidental Falls/ (8237) 27 exp Accident prevention/ (31735) 28 exp "Wounds and Injuries"/ (235238) 29 (injury or injuries).mp. (270239) 30 (accident* or wound*).mp. (145871) 31 (fall* or scald* or burn*).mp. (90653) 32 exp Fires/ (2801) 33 exp Burns/ (13774) 34 (suffocat* or poison*).mp. (27875) 35 Poisons/ (457) 36 or/24‐35 (555186) 37 randomized controlled trial.pt. (181189) 38 controlled clinical trial.pt. (34294) 39 randomized.ab. (142722) 40 placebo.ab. (71399) 41 clinical trials as topic.sh. (62839) 42 randomly.ab. (98005) 43 trial.ab. (137623) 44 or/37‐43 (452948) 45 exp animals/ not humans.sh. (1287604) 46 44 not 45 (412042) 47 23 and 36 and 46 (1773) 48 limit 47 to yr="2004 ‐ 2009" (927)
Planex
housing or house or home or homes or accommodation or residence* or residential or apartment* or flat or building AND Injury or injuries or accident* or wound* or fall* or scald* or hazards
RIBA‐British Architectural Library Catalogue
housing or house or home or homes or accommodation or residence* or residential or apartment* or flat or building AND Injury or injuries or accident* or wound* or fall* or scald* or hazards
SafetyLit
Within SafetyLit search ‐ Randomised controlled trial
Web of Science
| Search History |
WoK Conference Proceedings Citation Index
| Set | Results | Combine Sets AND OR |
Delete Sets | |
| # 28 | 49 | #21 or #27 Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 27 | 26 | #26 and #1 Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 26 | 332 | #22 or #23 or #24 or #25 Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 25 | 37 | TS=(injury SAME home) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 24 | 4 | TS=(injury SAME house) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 23 | 144 | TS=(hazard* and house*) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 22 | 172 | TS=(hazard* and home*) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 21 | 32 | #1 and #11 and #20 Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 20 | 6,163 | #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 19 | 10 | TS=("Thermal Burns") Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 18 | 4,060 | TS=(injuries) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 17 | 0 | TS=("accidental burn") Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 16 | 317 | TS=("home injur*" OR "burn injur*") Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 15 | 172 | TS=("injury prevention") Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 14 | 48 | TS=("accidental fall*" OR "accidental injur*") Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 13 | 4 | TS=("residential fire") Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 12 | 1,795 | TS=(scald* OR suffocat* OR poison*) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 11 | 58,747 | #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 10 | 720 | TS=(local authorit*) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 9 | 23 | TS=(condo OR condominium) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 8 | 30,369 | TS=(building) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 7 | 1,013 | TS=(ergonomic*) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 6 | 6,035 | TS=(neighbourhood* OR neighborhood*) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 5 | 553 | TS=(stairs OR staircase) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 4 | 226 | TS=(apartment) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 3 | 4,837 | TS=(accommodation* OR residence* OR homes) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 2 | 17,342 | TS=(housing or home or house) Databases=CPCI‐S Timespan=2004‐2009 |
||
| # 1 | 82,878 | TS=Randomized controlled trial* OR TS=Randomised controlled trial* OR TS= clinical trial* OR TS=random* OR TS= Random* allocat* OR TS=placebo* OR TS=single blind* OR TS=double blind* Databases=CPCI‐S Timespan=2004‐2009 |
||
Data and analyses
Comparison 1. Multifactorial fall prevention intervention including: home hazard assessment and modification; medication review, bone and health assessment and exercise program, versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Falls | 2 | 901 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.97, 1.23] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Babul 2007.
| Methods | 3 armed parallel, non‐blinded, RCT. | |
| Participants | Parents of newborn infants, recruited from single public health unit, with 82% of the population living in urban communities or suburban neighbourhoods and the balance in the rural hillsides and farming areas. n = 202 (I1). n = 206 (I2); n = 192 (C). |
|
| Interventions | (I1) A home visit and home safety kit. A 41‐item checklist was used to identify potential hazards in the home, and when identified parents were taught how to remove or modify these hazards. The nine home safety kit items included a smoke alarm, a coupon for 50% savings on a safety gate and cabinet locks. (I2) Home safety kit alone. (C) The control group received standard services provided by the community health unit for families with newborn infants. |
|
| Outcomes | Parent reported use of safety measures, attitudes toward safety and parent reported injury rates assessed by questionnaire. Outcomes evaluated using questionnaire completed at 2‐month (baseline), 6‐month and 12‐month immunisation visits with community health nurse. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | |
Becker 2003.
| Methods | Cluster RCT. | |
| Participants | Long‐stay residents ≥ 60 from 6 community nursing homes. Mean age 85; 79% female. n = 509 (I). n = 472 (C). |
|
| Interventions | Staff and resident education on fall prevention, advice on environmental adaptations, balance and resistance training, hip protectors. Participants could participate in any possible combination of intervention options for any time they wanted. | |
| Outcomes | Falls, injuries and fracture rates were documented for all facilities for 365 consecutive days from the same index date. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Campbell 2005.
| Methods | RCT. | |
| Participants | Study set in Dunedin and Auckland, New Zealand. Men and women aged ≥ 75 with visual acuity of 6/24 or worse who were living in the community. n = 100 (I1). n = 97 (I2). n = 98 (I3). n = 96 (C). |
|
| Interventions | Recruitment took place over a 12‐month period beginning in October 2002, and participants were followed up for 12 months. The study included 3 interventions: (I1) A home safety assessment and modification programme delivered by an occupational therapist. (I2) An exercise programme prescribed at home by a physiotherapist plus vitamin D supplementation. (I3) Both interventions. (C) Social visits. Environmental hazards were identified using the Westmead home safety assessment checklist to identify hazards and to initiate discussion with the participant about any items, behaviour or lack of equipment that could lead to falls. The therapist and participant agreed on which recommendations to implement, and the therapist facilitated the provision of equipment and evaluated adherence to the home safety programme. |
|
| Outcomes | Compliance to home safety recommendations measured by a 6‐month follow‐up telephone call. Falls and fall related injuries were monitored for 12 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Carter unpublished.
| Methods | RCT. | |
| Participants | Patients > 70 years of age identified from patient lists of 37 family physicians. n = 163 (I1). n = 133 (I2). n = 161 (C). | |
| Interventions | Brief intervention ‐ Home visit assessment of house/garden for hazards. Post‐home visit ‐ summary of hazards found and given pamphlet on home safety and use of medications. Intensive intervention ‐ Home assessment as above. Post‐assessment participant joint development of action plan including actions to be taken to modify hazards found. Phone prompts for action plan were provided after 3 and 6 months. 6‐month follow‐up advised to see family physician for medication review. Home hazards not specifically reported. Control group received no intervention. | |
| Outcomes | Falls and falls resulting in medical attention, hazard reduction. Fall related data was collected via phone interviews at 3, 6 and 12 months, and hazard reduction data was collected during the 12‐month interview. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Clamp 1998.
| Methods | RCT. | |
| Participants | Families with children < 5 years registered with a single‐handed general practice. n = 83 (I). n = 82 (C). | |
| Interventions | Intervention group families received GP safety advice and leaflets to promote the use of smoke alarms, stair gates, fireguards, cupboard locks, covers for electric sockets and door slam devices. Access to low‐cost safety equipment was made available for families receiving means tested state benefits. Control group families received usual care. | |
| Outcomes | Prevalence of safety devices and practices, collected 6 weeks after the intervention via a questionnaire. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Close 1999.
| Methods | RCT. | |
| Participants | All patients > 65 years living in the local community who attended A & E department with a primary diagnosis of a fall between Dec 1995 and June 1996. n = 184 (I). n = 213 (C). | |
| Interventions | Intervention group participants received a single home visit by an occupational therapist after medical assessment. Environmental hazards were identified using a checklist. Safety advice and education was given on completion of the assessment, and modifications such as removal of loose rugs were made with the patient's consent. Minor equipment was supplied directly by the occupational therapist and additional support was referred to social or hospital services. Control group patients received usual care. | |
| Outcomes | Primary diagnosis of a fall & hospital admissions, collected via postal questionnaire every 4 months for 1 year after the fall. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Cumming 1999.
| Methods | RCT. | |
| Participants | Inpatients, > 65 years of age, in 2 hospitals. Also recruitment from outpatient clinics at study hospitals and local day care centres for older people. n = 264 (I). n = 266 (C). | |
| Interventions | Intervention group participants received home visit by an occupational therapist who conducted a 1‐hour home assessment using a standardised form to record hazards and facilitated necessary home modifications. Modifications included: removal of mats and electrical cords, installation of non‐slip mats, night‐lights and stair rails and advice on footwear and activities. Control group participants received usual care. | |
| Outcomes | Falls, and modifications to the home. Fall data was collected over a 12‐month follow‐up period using monthly fall calendars and compliance with home modifications was recorded during a 12‐month follow‐up home visit. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Day 2002.
| Methods | RCT. | |
| Participants | Independent community‐dwelling elderly > 70 years of age registered on the Australian electoral roll for the area. n = 395 (I). n = 47 (C). | |
| Interventions | Factorial intervention trial of group‐based exercise including a balance component, home hazard management and vision improvement delivered separately or combined. Control participants received no intervention until after study end. Home hazards intervention consisted of a walk‐through checklist for rooms used in a normal week to review steps/stairs, floor surfaces, lighting, bathroom fittings and furniture and the removal/modification of home hazards either by participants or via the City's home maintenance staff. The control group received a home visit by a research nurse for baseline questionnaire and risk factor measurements before randomisation took place (as did intervention group), a falls calendar for monthly falls recording and other variables (as did intervention group), phone call if their calendar was more than 7‐10 days late in being returned each month (as did intervention group), a phone call if fall reported and a telephone interview regarding circumstances of the fall (as did intervention group), promise of being given most effective intervention at study end. About 50% of control group were re‐visited at study end for risk factor measurements & questionnaire (as did intervention group). There was, however, no placebo intervention for the control group, so they did not for example receive visits by a social worker etc. |
|
| Outcomes | Falls and hazard reduction. Fall data collected over 18‐month follow‐up period using monthly fall calendars and hazard data collected at 18 months also. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Elley 2008.
| Methods | RCT. | |
| Participants | 312 community‐living people aged 75 and older who had fallen in the previous year. n = 155 (I). n = 157 (C). |
|
| Interventions | Multicomponent intervention: Home‐based nurse assessment of falls‐and‐fracture risk factors and home hazards, referral to appropriate community interventions, and strength and balance exercise programme. | |
| Outcomes | Fall data collected over a 12‐month follow‐up period using monthly fall calendars. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | |
Gielen 2002.
| Methods | RCT. | |
| Participants | Paediatric residents in a large, urban teaching hospital in Maryland. Parents/guardians of infants 6 months of age. n = 19 (I1). n = 94 (I2). n = 20 (C1). n = 93 (C2). | |
| Interventions | Intervention group parents received safety counselling and referral to Children's Safety Centre (providing safety products such as, safety gates, smoke alarms, and hot water thermometers) from paediatric residents plus a home safety visit by community health worker between patient's 6‐ and 9‐month well‐infant clinic visit. Paediatric residents received 2‐part training programme. (Physical hazards assessed during home visit unspecified.) Control group families received the same as above without the home visit. | |
| Outcomes | Prevalence of safety practices collected at 12‐18 months follow‐up during home visit. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Gitlin 2006.
| Methods | Two‐group randomised design with survivorship followed for 14 months. | |
| Participants | Urban community living adults aged 70 and older, who reported having difficulty with one or more activities of daily living. n = 160 (I). n = 159 (C). |
|
| Interventions | Multicomponent intervention. Occupational and physical therapy sessions involving home modifications and training in their use, instruction in strategies of problem solving, energy conservation, safe performance, and fall recovery techniques; and balance and muscle strength training. The six‐month intervention consisted of five occupational therapy contacts and one physical therapy visit. OT's identified and prioritised priority areas, and for each targeted area an OT observed participants' performance for safety, efficiency and difficulty and presence of environmental barriers. Before the sixth contact, home modifications were ordered and installed (grab bars, rails, raised toilet seats) which were paid for through grant funds. Over the following six months OTs conducted three telephone calls to reinforce use of intervention derived strategies. |
|
| Outcomes | Presence of 106 potential tripping and falling hazards (torn carpets, glare, lack of grab rails). The home hazard index represented the total number of potentially unsafe conditions. Data collected at 6 and 12 months follow‐up. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | |
Hendrickson 2005.
| Methods | RCT: Pre‐ and post‐test experimental design | |
| Participants | Mothers of 1‐4 year old children, English‐ or Spanish‐speaking and agency qualified at or below 185% of the US Federal poverty level, were recruited from a non‐urban area in Texas where migrant Hispanics represent the majority of residents. n = 41 (I). n = 41 (C). |
|
| Interventions | The intervention was carried out 1 week after the baseline visit and included counselling, assessment of maternal safety practices and provision of safety items. A researcher counselled mothers regarding hazards reported during the first visit based on Health Belief Model (HBM) constructs. One construct ‐ behaviour accomplishment ‐ involved mothers placing free safety items and correcting hazards such as putting a working battery in a smoke detector. Mothers were also offered the option of having a photograph taken as they corrected a hazard. Another construct ‐ persuasion ‐ was targeted towards individuals, but built around a SafeKids brochure to stress the prevention of injuries. | |
| Outcomes | Maternal childhood injury health beliefs (MCIHB) and observed controllable safety hazards (CSH) scores collected 6 weeks after baseline visit via a home visit. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | |
Hendriks 2008.
| Methods | Two group RCT. | |
| Participants | 333 community dwelling Dutch people aged 65 and over who were seen in an emergency department after a fall. Participants were also recruited from the GP Cooperative. n = 166 (I). n = 167 (C). |
|
| Interventions | Multidisciplinary fall prevention programme. Intervention participants underwent a detailed medical and occupational therapy assessment to evaluate and address risk factors for recurrent falls, followed by recommendations and referral if indicated. Environmental hazards were identified and recorded using a home safety checklist, and modifications were referred to and delivered by social and community services. | |
| Outcomes | Falls and injurious falls collected over a 12‐month follow‐up period using monthly fall calendars. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | |
Hogan 2001.
| Methods | RCT. | |
| Participants | Ambulatory, community‐dwelling residents, > 65 years of age, of Calgary, Alberta. n = 79 (I). n = 84 (C). | |
| Interventions | Intervention subjects received in‐home assessments to identify both host and environmental risk factors in conjunction with the development of an individualised treatment plan, including an exercise programme for those deemed likely to benefit. Environmental risk factors identified by example only. Examples include: no grab bars on bath/shower and the removal of floor rugs. Control group participants received a home visit from a recreational therapist who performed a leisure assessment following which a letter was sent to each participant's GP. | |
| Outcomes | Falls collected over a 12‐month follow‐up period via monthly fall calendars, 3‐ and 6‐month home visits and telephone contact at 12 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Jenson 2002.
| Methods | Cluster RCT. | |
| Participants | Living in residential care facilities, > 65 years. n = 194 (I). n = 208 (C). |
|
| Interventions | Staff education, environmental adjustment, exercise, drug review, aids, hip protectors, post‐fall problem‐solving conferences, guiding staff. | |
| Outcomes | Falls and injuries collected over a 34‐week follow‐up period using a structured report form. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Kendrick 1999.
| Methods | Cluster RCT. | |
| Participants | All children aged 3‐12 months registered with 36 participating general practices in Nottingham. All health visitors in Nottingham. n = 1100 (I). n = 1019 (C). | |
| Interventions | Intervention group participants received: age‐specific safety advice at child health surveillance consultations at 6‐9, 12‐15 and 18‐24 months, provision of low‐cost safety equipment (stair gates, fireguards, cupboard locks and smoke alarms) to families on means tested state benefits and home safety checks by a health visitor. Physical hazards checked during home visit unspecified. Control group participants received usual care. | |
| Outcomes | Frequency and severity of medically attended injuries, ascertained from a search of the secondary and primary care records, at 25 months follow‐up. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
King 2005.
| Methods | RCT. | |
| Participants | Participants < 8 years old presenting to the Emergency Departments at 5 hospitals in 4 urban centres. n = 601 (I). n = 571 (C). | |
| Interventions | Study research assistant conducted home visits to observe home safety hazards for both control and intervention groups. Intervention group participants received an information package on injury prevention, discount coupons for safety devices, specific instruction regarding home safety measures and a letter from site project directors on need to maintain preventive behaviours. Hazards measured were: access to small and dangerous objects, absence of child resistant medicine containers, tap water greater than 54oC, functioning smoke detectors, fire extinguishers, stair gates, infant walkers, ease of opening basement door, absence of bicycle helmets and car restraints. Control group participants received a general pamphlet on safety and notification if a non‐functioning smoke detector was found. All participants were contacted at 4 and 8 months after the initial visit to reinforce the intervention. | |
| Outcomes | Injuries and hazard reduction recorded at 4, 8 and 12 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Mahoney 2007.
| Methods | RCT. | |
| Participants | 65 years and older, with two falls in the previous year or one fall in the previous 2 years with injury or balance problems. n = 174 (I). n = 175 (C). |
|
| Interventions | The intervention used an algorithm based on the University of Wisconsin Falls Prevention Clinic, designed to identify predisposing factors for falls; induce risk reduction changes in medical conditions, medications, behaviour, physical status, and home environment through recommendations to participants and their physicians, referrals to physical therapy and other providers, 11 monthly telephone calls, and a balance exercise plan. Control subjects received a home safety assessment. | |
| Outcomes | Falls were followed for 12 months using monthly fall calendars and telephone contact. All hospitalisation and nursing home reports were verified using medical records. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | |
Nikolaus 2003.
| Methods | RCT with follow‐up of subjects for 1 year. | |
| Participants | Patients with functional decline, admitted from home to a geriatric clinic in southern Germany. n = 181 assigned to geriatric assessment and home intervention team (I). n = 179 assigned to geriatric assessment and usual care (C). |
|
| Interventions | Geriatric assessment and home intervention. Home intervention included an assessment of the home for environmental hazards, advice about possible changes, offer of facilities to modify the home environment, and training in the use of mobility and technical aids. | |
| Outcomes | Falls and compliance with home safety recommendations, measured at 12‐month follow‐up. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Pardessus 2002.
| Methods | RCT. | |
| Participants | Patients admitted to a geriatric hospital following a fall. Study set in Lille, France and mean age 83.5 years. n = 30 (I). n = 30 (C). |
|
| Interventions | A home visit to assess environmental hazards and recommend modifications. Environmental hazards were identified using a check list and where possible modifications such as the removal of loose carpets were made with the patient's consent. When a hazard could not be removed the occupational therapist provided safety advice instead. | |
| Outcomes | Falls collected by contacting each patient every month during 6‐month follow‐up and at 12 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Posner 2004.
| Methods | RCT. | |
| Participants | Caregivers of < 5 year olds who presented to casualty with acute unintentional injury sustained at home. n = 69 (I). n = 67 (C). |
|
| Interventions | Comprehensive home safety education and free home safety kit which included: cabinet latches, drawer latches, electrical outlet covers, tub spout covers, non‐slip bath decals, bath water thermometer, small parts tester (choking tube), poison control telephone number stickers, and literature related to fire and window safety. | |
| Outcomes | Degree of improvement in safety practices assessed by improvement in safety scores, collected by telephone contact at 6‐8 weeks after the initial ED visit. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Salminen 2009.
| Methods | RCT. | |
| Participants | 591 community dwelling 65+ year olds, self selected between 2003 and 2005, via news articles and mail‐shots. n = 293 (I). n = 298 (C). |
|
| Interventions | 12‐month fall prevention programme based on individual risk analysis; geriatric assessment, counselling and guidance in fall prevention, home hazard assessment, group physical exercise, home exercise, lectures in groups and psychosocial groups. | |
| Outcomes | Falls were followed for 12 months using monthly fall calendars. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | |
Sangvai 2007.
| Methods | Prospective RCT. | |
| Participants | Trial conducted at 3 paediatric sites. Recruitment occurred from December 2002 to January 2004 and included parents of children aged 0 to 5 years who were with their child at a health maintenance visit. n = 160 (I). n = 159 (C). |
|
| Interventions | Multicomponent intervention including focused counselling from a physician and health assistant, educational handouts, phone follow‐up, and access to free safety devices and automobile restraint evaluations. Intervention focused on 5 safety issues: use of automobile restraints, use of smoke detectors, safe storage of hazardous materials (household cleaners and medications), setting of appropriate tap water temperature (< 120oF), and safe storage of guns. | |
| Outcomes | Prevalence of safety features collected by home visit and medically attended injuries collected by chart review, both at 6‐month follow‐up. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | |
Shaw 2003.
| Methods | Prospective single centre RCT. | |
| Participants | Older people aged ≥ 65 years, cognitively impaired and dementia, presenting to casualty following a fall. Study set in Newcatle upon Tyne. n = 130 (I). n = 144 (C). |
|
| Interventions | Multifactorial intervention involving a medical, cardiovascular, physiotherapy and occupational therapy assessment and intervention. Occupational therapy assessment identified environmental fall hazards using a standard checklist, and home hazard modification was carried out using a standard protocol. | |
| Outcomes | Falls, injury rates, objective effect on environmental risk factors. Fall and injury data collected over a 12‐month follow‐up period, using weekly diaries and A&E department records. Environmental risk factor data collected at 3 months' follow‐up. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Stevens 2001.
| Methods | RCT. | |
| Participants | Residents, aged ≥ 70 years of age, living independently in the Perth metropolitan area and listed on the State Electoral Roll and the White Pages telephone directory. n = 570 (I). n = 1167 (C). Recruited and randomly allocated by household. | |
| Interventions | All members of both the intervention and the control groups received a home visit from a nurse. Intervention consisted of 3 strategies: a home hazard assessment, the installation of free safety devices and an educational strategy to empower seniors to remove or modify home hazards. Modifications included: installation of grab bars, removal of obstacles, removal/stabilisation of rugs and mats, repair of damaged flooring, improving the height of chairs and improving poor lighting. Control subjects received no safety devices or information on home hazard reduction. | |
| Outcomes | Falls, injurious falls, hazard reduction. Fall and injury data collected over a 12‐month follow‐up period using daily calendars and hazard reduction data was collected at 11 months' follow‐up by postal questionnaire (51 homes received a second home hazard assessment to evaluate change in hazard prevalence). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Tinetti 1994.
| Methods | RCT. | |
| Participants | ≥ 70 years of age, members of a Health Maintenance Organisation (HMO) with one of the following risk factors for falling: postural hypotension; use of sedatives; use at least four prescription medications; and impairment in arm or leg strength or range of motion, balance, ability to move safely from bed to chair or to the bathtub or toilet, or gait. n = 153 (I). n = 148 (C). | |
| Interventions | Multifactorial intervention. Intervention group received home assessment visit by a nurse followed 1‐week later by physical therapist. Nurse assessment included: postural hypotension, medication review and use, transfer and gait training skills, balance exercises and exercises with resistive tools. Appropriate changes to environmental hazards for falls or tripping were made such as removal of hazards, safer furniture (correct height, more stable), installation of structures such as grab bars or handrails on stairs determined by room‐by‐room assessment. Control group received home visits from social‐work students where structured interviews were conducted. | |
| Outcomes | Falls, collected over a 12‐month follow‐up period. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Van Haastregt 2000b.
| Methods | RCT. | |
| Participants | Participants, ≥ 70 years of age, from 6 general practices in Hoensbroek, who had reported two or more falls in the previous 6 months or had scored 3 or more on the mobility control scale of the short version of the sickness impact profile. n = 159 (I). (n = 138 received standard intervention programme; n = 21 did not receive standard intervention programme). n = 157 (C). | |
| Interventions | Multifactorial intervention. Intervention group received 5 home visits by community nurse over a period of 1 year. During home visits participants were screened for medical, environmental and behavioural factors potentially influencing falls and mobility and followed by advice, referrals and other actions aimed at dealing with observed hazards. The control group did not receive any special attention or intervention on prevention of falls and impairments in mobility. No details of any home modification given. | |
| Outcomes | Falls & injurious falls, collected at 12 and 18 months' follow‐up. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Vetter 1992.
| Methods | RCT. | |
| Participants | 70 years of age patients registered at a group practice of 5 general practitioners in a Welsh market town. n = 350 (I). n = 324 (C). | |
| Interventions | Intervention participants received intensive health visiting, over 4 years, to provide nutrition advice and make medical and environmental checks environmental hazards included: trailing wires, loose carpets, outside toilets, lighting levels and slippery slopes. Muscle tone and fitness levels were addressed at physiotherapist‐led classes. Health visitor visited as often as believed to be necessary, carrying out referrals. Details concerning the control group are not available. | |
| Outcomes | Change in fracture rates, falls over a 4‐year follow‐up period. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate. |
Watson 2005.
| Methods | RCT. | |
| Participants | Families with one or more children younger than 5 years, from the caseloads of participating health visitors. Health visitors were recruited from working practices located in deprived areas in the Nottingham Health Authority. n = 1711 families (I). n = 1717 families (C). |
|
| Interventions | Standardised safety consultation and provision of free safety equipment. Intervention comprised of a standard consultation on safety that had been adapted to conform to educational principles to increase the effectiveness. Consultation was individualised and specific to children's ages in each family and took about 20 minutes. The health visitor offered stair gates, fire guards, smoke alarms, cupboard locks and window locks free of charge to low income families and these were fitted free of charge. Families not on a low income were offered equipment at cost price and a delivery service to their home. |
|
| Outcomes | Medically attended injury over a two year follow‐up period, and possession of safety equipment collected at 12 and 24 months by postal questionnaire. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Assantachai 2002 | Community based with no home hazard intervention. |
| Barnes 2004 | Trials of Improved Practices (TIPs) methodology. |
| Binns 2004 | Study focused on reducing injuries related to chronic exposures. |
| Boreland 2006 | Study focused on reducing injuries related to chronic exposures. |
| Bouwen 2008 | No intervention that met inclusion criteria. |
| Caplan 2004 | No intervention that met inclusion criteria. |
| Carman 2006 | Evaluation study. |
| Casteel 2004 | Controlled clinical trial. Allocation concealment unclear. |
| Ciaschini 2009 | No intervention that met inclusion criteria. |
| Clemson 1996 | Case‐control study. |
| Colver 1982 | Controlled clinical trial. Allocation concealment unclear. |
| Conn 2005 | Non‐controlled before and after study. Allocation concealment not used. |
| Dershewitz 1979 | Controlled clinical trial. Allocation concealment unclear. |
| Diener 2005 | Controlled clinical trial. Allocation concealment unclear. |
| Dixon 2009 | Controlled clinical trial. Allocation concealment unclear. |
| Duff 2002 | Undefined access to home equipment with no measure of change to physical hazards. |
| Durongritichai 2003 | PRECEDE‐PROCEED methodology with randomisation not described. |
| Fergusson 2005 | No intervention that met inclusion criteria. |
| Filiatrault 2007 | Controlled clinical trial. Allocation concealment unclear. |
| Gerson 2005 | Controlled clinical trial. Allocation concealment unclear. |
| Gillespie‐Bennett 2008 | Study focused on reducing injuries related to chronic exposures. |
| Ginnelly 2005 | Installation of smoke alarm sole intervention. |
| Haynes 2003 | No intervention that met inclusion criteria. |
| Hermann 1999 | German‐language paper translated does not meet inclusion criteria. |
| Hornbrook 1994 | Controlled clinical trial. Allocation concealment unclear. |
| Huang 2003 | No intervention to meet inclusion criteria. |
| Huang 2004 | Controlled clinical trial. Allocation concealment unclear. |
| Iwarsson 2009 | Survey study. |
| Johnston 2000 | Controlled clinical trial. Allocation concealment unclear. |
| Katcher 1989 | Controlled clinical trial. Allocation concealment unclear. |
| Kelly 1987 | Controlled clinical trial. Allocation concealment unclear. |
| Kendrick 2008 | Study protocol. |
| Kerse 2004 | No intervention that met inclusion criteria. |
| Laffoy 1997 | Case‐control. |
| Lamb 2008 | Survey study. |
| Lannin 2007 | No intervention that met inclusion criteria. |
| Lightbody 2002 | Controlled clinical trial. Allocation concealment unclear. |
| Lin 2007 | Controlled clinical trial. Allocation concealment unclear. |
| Llewellyn 2003 | No intervention that met inclusion criteria. |
| McLean 1996 | Case‐control. |
| McMurdo 2000 | Environmental intervention was not undertaken. |
| Minkovitz 2010 | No intervention that met inclusion criteria. |
| Morgan 2005 | Evaluation study. |
| Morgenstern 2000 | Stage 1: cohort. Stage 2: case‐control. |
| Nelson 2005 | No intervention that met inclusion criteria. |
| Neno 2008 | No intervention that met inclusion criteria. |
| Neyens 2009 | No intervention that met inclusion criteria. |
| Northridge 1995 | Cohort. |
| Odendaal 2009 | Controlled clinical trial. Allocation concealment unclear. |
| Ozanne‐Smith 2002 | Ecological study. Changes to hazards not reported at a household level. |
| Paul 1994 | Controlled clinical trial. Allocation concealment unclear. |
| Peel 2000 | Controlled clinical trial. Allocation concealment unclear. |
| Peeters 2007 | Study protocol. |
| Petridou 1996 | Case‐control. |
| Petridou 1997 | Controlled clinical trial. Allocation concealment not used. |
| Plautz 1996 | Interrupted time‐series. Insufficient data gathering points. |
| Poulstrop 2000 | Controlled before and after study. |
| Pressley 2009 | No outcome that met inclusion criteria. |
| Ramsey 2003 | No intervention that meets inclusion criteria. |
| Rizawati 2008 | Cross‐sectional study. |
| Roberts 2004 | Installation of smoke alarm sole intervention. |
| Robertson 2005 | Evaluation study. |
| Robson 2003 | Controlled clinical trial. Allocation concealment unclear. |
| Runyan 1992 | Case‐control. |
| Sattin 1998 | Case‐control study. |
| Schwarz 1993 | Controlled clinical trial. Allocation concealment not used. |
| Schwebel 2009 | Observational study. |
| Spiegel 1977 | Interrupted time‐series. Insufficient data gathering points. |
| Steinberg 2000 | Controlled clinical trial. Allocation concealment unclear. |
| Stone 2007 | Controlled before and after study. Allocation concealment not used. |
| Studenski 1994 | Cohort study. |
| Swart 2008 | Housing was not architect‐designed or subject to housing regulations. |
| Sznajder 2003 | Controlled clinical trial. Allocation concealment unclear. |
| Tanner 2003 | No outcome that met inclusion criteria. |
| Thomas 1984 | Controlled clinical trial. Allocation concealment unclear. |
| Thompson 1996 | Interrupted time series. Insufficient data gathering points. |
| Tideiksaar 1990 | Interrupted time‐series. No control group. |
| Van Rijn 1991 | Case‐control. |
| Vind 2009 | No intervention that meets inclusion criteria. |
| Wagner 1994 | Controlled clinical trial. Allocation concealment not used. |
| Waller 1993 | Controlled clinical trial. Allocation concealment unclear. |
| Weatherall 2004 | No intervention that meets inclusion criteria. |
| Wyman 2007 | No intervention that meets inclusion criteria. |
| Xia 2009 | Controlled clinical trial. Allocation concealment not used. |
| Yang 2008 | Installation of smoke alarm sole intervention. |
| Yates 2001 | Controlled clinical trial. Allocation concealment not used. |
| Ytterstad 1996 | Controlled before and after study. Allocation concealment not used. |
Contributions of authors
ST screened abstracts, critically appraised included studies, wrote updated sections and made review amendments as recommended by the peer referees.
GA screened abstracts, critically appraised included studies, wrote updated sections and made review amendments as recommended by the peer referees.
RL helped to write and edit the protocol, critically appraise included studies, edit updated sections, and suggest review amendments.
AW and MM developed the search strategy, ran electronic database searches, contacted experts, carried out handsearching and reference list follow up, screened records and commented on the review. SJ critically appraised included studies and updated included studies tables and commented on the review.
AJ critically appraised included studies and updated included studies tables and commented on the review.
SL critically appraised included studies and updated included studies tables and commented on the review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
NIHR 2009 Cochrane Review Incentive Scheme, UK.
£5000
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Babul 2007 {published data only}
- Babul S, Olsen L, Janssen P, McIntee P, Raina P, Babul S, et al. A randomized trial to assess the effectiveness of an infant home safety programme. International Journal of Injury Control & Safety Promotion 2007;14(2):109‐17. [DOI] [PubMed] [Google Scholar]
Becker 2003 {published data only}
- Becker C, Kron M, Lindemann U, Sturm E, Eichner B, Walter‐Jung B. Effectiveness of a multifaceted intervention on falls in nursing home residents. Journal of the American Geriatrics Society 2003;51:306‐13. [DOI] [PubMed] [Google Scholar]
Campbell 2005 {published data only}
- Campbell AJ, Robertson MC, Grow SJ, Kerse NM, Sanderson GF, Jacobs RJ, et al. Randomised controlled trial of prevention of falls in people aged greater than or equal to 75 with severe visual impairment: the VIP trial. BMJ 2005;331(7520):817‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grow SJ, Robertson MC, Cambell AJ, Clarke GA, Kerse NM. Reducing hazard related falls in people 75 years and older with significant visual impairment: how did a successful program work?. Injury Prevention 2006;12:296‐301. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carter unpublished {unpublished data only}
- Carter S, Campbell E, Sanson‐Fisher R, Corkrey R, Gillespie W. A trial of two strategies aimed at reducing falls through home hazard modification and medication review. Unpublished (permission to quote granted).
Clamp 1998 {published data only}
- Clamp M, Kendrick D. A randomised controlled trial of general practitioner safety advice for families with children under 5 years. BMJ 1998;316:1576‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Close 1999 {published data only}
- Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET):a randomised controlled trial. Lancet 1999;353:93‐7. [DOI] [PubMed] [Google Scholar]
Cumming 1999 {published data only}
- Cumming RG, Thomas M, Szonyi G, Salkeld G, O'Neill E, Westbury C, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards:a randomized trial of falls prevention. Journal of the American Geriatrics Society 1999;47:1397‐402. [DOI] [PubMed] [Google Scholar]
Day 2002 {published data only}
- Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 2002;325:128‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elley 2008 {published data only}
- Elley CR, Robertson MC, Garrett S, Kerse NM, McKinlay E, Lawton B, et al. Effectiveness of a falls‐and‐fracture nurse coordinator to reduce falls: a randomized, controlled trial of at‐risk older adults. Journal of the American Geriatrics Society 2008;56(8):1383‐9. [DOI] [PubMed] [Google Scholar]
Gielen 2002 {published data only}
- Gielen AC, McDonald EM, Wilson MEH, Hwang WT, Serwint J, Andrews JS, et al. Effects of improved access to safety counselling, products and home visits on parents' safety practices: Results of a randomized trial. Archives of Pediatrics & Adolescent Medicine 2002;156:33‐40. [DOI] [PubMed] [Google Scholar]
- Gielen AC, Wilson ME, McDonald EM, Serwint JR, Andrews JS, Hwang WT, et al. Randomized trial of enhanced anticipatory guidance for injury prevention. Archives of Pediatrics and Adolescent Medicine 2001;155:42‐9. [DOI] [PubMed] [Google Scholar]
Gitlin 2006 {published data only}
- Gitlin LN, Winter L, Dennis MP, Corcoran M, Schinfeld S, Hauck WW. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. Journal of the American Geriatrics Society 2006;54:809‐16. [DOI] [PubMed] [Google Scholar]
Hendrickson 2005 {published data only}
- Hendrickson SG. Reaching an underserved population with a randomly assigned home safety intervention. Injury Prevention 2005;11(5):313‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hendriks 2008 {published data only}
- Hendriks MR, Bleijlevens MH, Haastregt JC, Crebolder HF, Diederiks JP, Evers SM, et al. Lack of effectiveness of a multidisciplinary fall‐prevention program in elderly people at risk: a randomized, controlled trial. Journal of the American Geriatrics Society 2008;56(8):1390‐7. [DOI] [PubMed] [Google Scholar]
Hogan 2001 {published data only}
- Hogan DB, MacDonald FA, Betts J, Bricker S, Ebly EM, Delarue B, et al. A randomized controlled trial of a community‐based consultation service to prevent falls. Canadian Medical Association Journal 2001;165(5):537‐43. [PMC free article] [PubMed] [Google Scholar]
Jenson 2002 {published data only}
- Jensen J, Lundin ‐Olsson L, Nyberg L, Gustafson Y. Fall and injury prevention in older people living in residential care facilities. Annals of Internal Medicine 2002;136:733‐41. [DOI] [PubMed] [Google Scholar]
- Jensen J, Nyberg L, Gustafson Y, Lundin‐Olsson L. Fall and injury prevention in residential care ‐ effects in residents with higher and lower levels of cognition. Journal of the American Geriatrics Society 2003;51:627‐35. [DOI] [PubMed] [Google Scholar]
Kendrick 1999 {published data only}
- Kendrick D, Marsh P, Fielding K, Miller P. Preventing injuries in children:cluster randomised controlled trial in primary care. BMJ 1999;318:980‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
King 2005 {published data only}
- King WJ, Klassen TP, LeBlanc J, Bernard‐Bonnin AC, Robitaille Y, Pham B, et al. The effectiveness of a home visit to prevent childhood injury. Pediatrics 2001;108(2):382‐8. [DOI] [PubMed] [Google Scholar]
- King WJ, LeBlanc JC, Barrowman NJ, Klassen TP, Bernard‐Bonnin A‐C, Robitaille Y, et al. Long term effects of a home visit to prevent childhood injury: three year follow up of a randomized trial. Injury Prevention 2005;11:106‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mahoney 2007 {published data only}
- Mahoney JE, Shea TA, Przybelski R, Jaros L, Gangnon R, Cech S, et al. Kenosha County falls prevention study: a randomized, controlled trial of an intermediate‐intensity, community‐based multifactorial falls intervention. Journal of the American Geriatrics Society 2007;55(4):489‐98. [DOI] [PubMed] [Google Scholar]
Nikolaus 2003 {published data only}
- Nikolaus T, Bach M. Preventing falls in community‐dwelling frail older people using a home intervention team (HIT): results from the randomized Falls‐HIT trial. Journal of the American Geriatrics Society 2003;51(3):300‐5. [DOI] [PubMed] [Google Scholar]
Pardessus 2002 {published data only}
- Pardessus V, Parieux F, Di P, Gaudefroy C, Thevenon A, Dewailly P. Benifits of home visits for falls and autonomy in the elderly: a randomised study. American Journal of Physical Medicine and Rehabilitation 2002;81(4):247‐52. [DOI] [PubMed] [Google Scholar]
Posner 2004 {published data only}
- Posner JC, Hawkins LA, Garcia‐Espana F, Durbin DR. A randomized, clinical trial of a home safety intervention based in an emergency department setting. Pediatrics 2004;113:1603‐8. [DOI] [PubMed] [Google Scholar]
Salminen 2009 {published data only}
- Salminen M, Vahlberg T, Kivela SL. The long‐term effect of a multifactorial fall prevention programme on the incidence of falls requiring medical treatment. Public Health 2009;123(12):809‐13. [DOI] [PubMed] [Google Scholar]
- Salminen MJ, Vahlberg TJ, Salonoja MT, Aarnio PT, Kivela SL, Salminen Marika J, et al. Effect of a risk‐based multifactorial fall prevention program on the incidence of falls. Journal of the American Geriatrics Society 2009;57(4):612‐9. [DOI] [PubMed] [Google Scholar]
- Sjosten NM, Salonoja M, Piirtola M, Vahlberg T, Isoaho R, Hyttinen H, et al. A multifactorial fall prevention programme in home‐dwelling elderly people: A randomized‐controlled trial. Public Health 2007;121:308‐18. [DOI] [PubMed] [Google Scholar]
Sangvai 2007 {published data only}
- Sangvai S, Cipriani L, Colborn DK, Wald ER, et al. Studying injury prevention: practices, problems, and pitfalls in implementation. Clinical Pediatrics 2007;46(3):228‐35. [DOI] [PubMed] [Google Scholar]
Shaw 2003 {published data only}
- Shaw FE, Bond J, Richardson DA, Dawson P, Steen IN, McKeith IG. Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: randomised controlled trial. BMJ 2003;326:73‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stevens 2001 {published data only}
- Stevens M, D'Arcy C, Holman J, Bennett N, Klerk N. Preventing falls in older people:outcome evaluation of a randomized controlled trial. Journal of the American Geriatrics Society 2001;49:1448‐55. [DOI] [PubMed] [Google Scholar]
Tinetti 1994 {published data only}
- Tinetti ME, Baker DI, McAvay G, Blaus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. New England Journal of Medicine 1994;331(13):821‐7. [DOI] [PubMed] [Google Scholar]
Van Haastregt 2000b {published data only}
- Haastregt JCM, Diederiks JPM, Rossum E, Witte LP, Woorhoeve PM, Crebolder HF. Effects of a programme of multifactorial home visits on falls and mobility impairments in elderly people at risk: randomised controlled trial. BMJ 2000;321:994‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vetter 1992 {published data only}
- Vetter N, Lewis P, Ford D. Can health visitors prevent fractures in elderly people?. BMJ 1992;304:888‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Watson 2005 {published data only}
- Watson M, Kendrick D, Coupland C, Woods A, Futers D, Robinson J. Providing child safety equipment to prevent injuries: randomised controlled trial. BMJ 2005;330:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Assantachai 2002 {published data only}
- Assantachi P, Chatthanaearee W, Thamlikitkul V, Praditsuwan R, Pisalsarakij D. Strategy to prevent falls in the Thai elderly: a controlled study integrated health research program for the Thai elderly. Journal of the Medical Association of Thailand 2002;85:215‐22. [PubMed] [Google Scholar]
Barnes 2004 {published data only}
- Barnes BR, Mathee A, Krieger L, Shafritz L, Favin M, Sherburne L, et al. Testing selected behaviors to reduce indoor air pollution exposure in young children. Health Education Research 2004;19(5):543‐50. [DOI] [PubMed] [Google Scholar]
Binns 2004 {published data only}
- Binns HJ, Gray KA, Chen T, Finster ME, Peneff N, Schaefer P, et al. Evaluation of landscape coverings to reduce soil lead hazards in urban residential yards: The Safer Yards Project. Environmental Research 2004;96(2):127‐38. [DOI] [PubMed] [Google Scholar]
Boreland 2006 {published data only}
- Boreland F, Lyle DM, Boreland F, Lyle DM. Lead dust in Broken Hill homes: effect of remediation on indoor lead levels. Environmental Research 2006;100(2):276‐83. [DOI] [PubMed] [Google Scholar]
Bouwen 2008 {published data only}
- Bouwen A, Lepeleire J, Buntinx F, Bouwen A, Lepeleire J, Buntinx F. Rate of accidental falls in institutionalised older people with and without cognitive impairment halved as a result of a staff‐oriented intervention. Age & Ageing 2008;37(3):306‐10. [DOI] [PubMed] [Google Scholar]
Caplan 2004 {published data only}
- Caplan GA, Williams AJ, Daly B, Abraham K. A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department ‐ the DEED II study. Journal of the American Geriatrics Society 2004;52(9):1417‐23. [DOI] [PubMed] [Google Scholar]
Carman 2006 {published data only}
- Carman J, Friedman E, Lamb D, Lennon K. Evaluating the impact of a child injury prevention project. Community Practitioner 2006;79(6):188‐92. [PubMed] [Google Scholar]
Casteel 2004 {published data only}
- Casteel C, Peek‐Asa C, Lacsamana C, Vazquez L, Kraus JF. Evaluation of a falls prevention program for independent elderly. American Journal of Health Behavior 2004;28:S51‐60. [DOI] [PubMed] [Google Scholar]
Ciaschini 2009 {published data only}
- Ciaschini PM, Straus SE, Dolovich LR, Goeree RA, Leung KM, Woods CR, et al. Community‐based intervention to optimise falls risk management: a randomised controlled trial. Age & Ageing 2009;38(6):724‐30. [DOI] [PubMed] [Google Scholar]
Clemson 1996 {published data only}
- Clemson L. Case‐control study of hazards in the home. Age and Aging 1996;25:97‐101. [DOI] [PubMed] [Google Scholar]
Colver 1982 {published data only}
- Colver AF, Hutchinson PJ, Judson EC. Promoting children's home safety. BMJ 1982;285:1177‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Conn 2005 {published data only}
- Conn L. Mind your Step! A falls prevention programme designed to reduce falls in those over 75 years. Quality in Ageing 2005;8(1):10‐22. [Google Scholar]
Dershewitz 1979 {published data only}
- Dershewtiz RA. Will mothers use free household safety devices?. American Journal of Diseases in Childhood 1979;133:61‐4. [DOI] [PubMed] [Google Scholar]
Diener 2005 {published data only}
- Diener DD, Mitchel JM. Impact of a multifactorial fall prevention program upon falls of older frail adults attending an adult health day care center. Topics in Geriatric Rehabilitation 2005;21(3):247‐57. [Google Scholar]
Dixon 2009 {published data only}
- Dixon SL, Fowler C, Harris J, Moffat S, Martinez Y, Walton H, et al. An examination of interventions to reduce respiratory health and injury hazards in homes of low‐income families. Environmental Research 2009;109(1):123‐30. [DOI] [PubMed] [Google Scholar]
Duff 2002 {published data only}
- Duff S, Ryan M, Mullan C, O'Keefe B, Nicholson AJ. The use of local accident and emergency injury surveillance to monitor the impact of a lay safety community programme. Irish Medical Journal 2002;95(5):143‐5. [PubMed] [Google Scholar]
Durongritichai 2003 {published data only}
- Durogritichai V, Tongvichean S, Silapasuwan P, Plitponkarnpim A, Nontapatamadul K. Caregiver self‐help group development for preschooler home injury prevention: community‐action research perspective. Thai Journal of Nursing Research 2003;7(1):23‐36. [Google Scholar]
Fergusson 2005 {published data only}
- Fergusson DM, Grant H, Horwood LJ, Ridder EM. Randomized trial of the Early Start program of home visitation. Pediatrics 2005;116(6):e803‐9. [DOI] [PubMed] [Google Scholar]
Filiatrault 2007 {published data only}
- Filiatrault J, Parisien M, Laforest S, Genest C, Gauvin L, Fournier M, et al. Implementing a community‐based falls‐prevention program: from drawing board to reality. Canadian Journal on Aging 2007;26(3):213‐25. [DOI] [PubMed] [Google Scholar]
Gerson 2005 {published data only}
- Gerson LW, Camargo CA Jr, Wilber ST. Home modification to prevent falls by older ED patients. American Journal of Emergency Medicine 2005;23(3):295‐8. [DOI] [PubMed] [Google Scholar]
Gillespie‐Bennett 2008 {published data only}
- Gillespie‐Bennett J, Pierse N, Wickens K, Crane J, Nicholls S, Shields D, et al. Sources of nitrogen dioxide (NO2) in New Zealand homes: findings from a community randomized controlled trial of heater substitutions. Indoor Air 2008;18(6):521‐8. [DOI] [PubMed] [Google Scholar]
Ginnelly 2005 {published data only}
- Ginnelly L, Sculpher M, Bojke C, Roberts I, Wade A, Diguiseppi C, et al. Determining the cost effectiveness of a smoke alarm give‐away program using data from a randomized controlled trial. European Journal of Public Health 2005;15(5):448‐53. [DOI] [PubMed] [Google Scholar]
Haynes 2003 {published data only}
- Haynes R, Reading R, Gale S. Household and neighbourhood risks for injury to 5‐14 year old children. Social Science & Medicine 2003;57(4):625‐36. [DOI] [PubMed] [Google Scholar]
Hermann 1999 {published data only}
- Hermann R, Meier‐Baumgartner HP. Hip‐fracture in the elderly caused by a fall ‐ etiology and rehabilitation [Die sturzbedingte, proximale Femurfraktur alterer Menschen ‐ Atiologie und Rehabilitation]. Zeitschrift fur Gerontologie und Geriatrie 1999;32:52‐7. [DOI] [PubMed] [Google Scholar]
Hornbrook 1994 {published data only}
- Hornbrook MC, Stevens VJ, Wingfield DJ, Hollis JF, Greenlick MR, Ory MG. Preventing falls among community‐dwelling older persons: results from a randomized trial. Gerontologist 1994;34(1):16‐23. [DOI] [PubMed] [Google Scholar]
Huang 2003 {published data only}
- Huang H, Gau M, Lin W. Assessing risk of falling in older adults. Public Health Nursing 2003;20(5):399‐411. [DOI] [PubMed] [Google Scholar]
Huang 2004 {published data only}
- Huang T, Acton G. Effectiveness of home visit falls prevention strategy for Taiwanese community‐dwelling elders: a randomized trial. Public Health Nursing 2004;21(3):247‐56. [DOI] [PubMed] [Google Scholar]
Iwarsson 2009 {published data only}
- Iwarsson S, Horstmann V, Carlsson G, Oswald F, Wahl H. Person‐environment fit predicts falls in older adults better than the consideration of environmental hazards only. Clinical Rehabilitation 2009;23(6):558‐67. [DOI] [PubMed] [Google Scholar]
Johnston 2000 {published data only}
- Johnston BD, Britt J, D'Ambrosio L, Mueller BA, Rivara FP. A preschool program for safety ad injury prevention delivered by home visitors. Injury Prevention 2000;6:305‐09. [DOI] [PMC free article] [PubMed] [Google Scholar]
Katcher 1989 {published data only}
- Katcher ML, Landry GL, Shapiro MM. Liquid‐crystal thermometer use in pediatric office counseling about tap water burn prevention. Pediatrics 1989;83(5):766‐71. [PubMed] [Google Scholar]
Kelly 1987 {published data only}
- Kelly B, Sein C, McCarthy PL. Safety education in a pediatric primary care setting. Pediatrics 1987;79(5):818‐24. [PubMed] [Google Scholar]
Kendrick 2008 {published data only}
- Kendrick D, Stewart J, Coupland C, Hayes M, Hopkins N, McCabe D, et al. Randomised controlled trial of thermostatic mixer valves in reducing bath hot tap water temperature in families with young children in social housing: a protocol. Trials [Electronic Resource] 2008;9:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kerse 2004 {published data only}
- Kerse N, Butler M, Robinson E, Todd M, Kerse Ngaire, Butler Meg, et al. Fall prevention in residential care: a cluster, randomized, controlled trial. Journal of the American Geriatrics Society 2004;52(4):524‐31. [DOI] [PubMed] [Google Scholar]
Laffoy 1997 {published data only}
- Laffoy M. Childhood accidents in the home. Irish Medical Journal 1997;90(1):26‐7. [PubMed] [Google Scholar]
Lamb 2008 {published data only}
- Lamb SE, Fisher JD, Gates S, Potter R, Cooke MW, Carter YH. A national survey of services for the prevention and management of falls in the UK. BMC Health Services Research 2008;8:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lannin 2007 {published data only}
- Lannin NA, Clemson L, McCluskey A, Lin CW, Cameron ID, Barras S, et al. Feasibility and results of a randomised pilot‐study of pre‐discharge occupational therapy home visits. BMC Health Services Research 2007;7:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lightbody 2002 {published data only}
- Lightbody E, Watkins C, Leathley M, Sharma A, Lye M. Evaluation of a nurse‐led falls prevention programme versus usual care: a randomized controlled trial. Age and Aging 2002;31(3):203‐10. [DOI] [PubMed] [Google Scholar]
Lin 2007 {published data only}
- Lin MR, Wolf SL, Hwang HF, Gong SY, Chen CY. A randomized, controlled trial of fall prevention programs and quality of life in older fallers. Journal of the American Geriatrics Society 2007;55(4):499‐506. [DOI] [PubMed] [Google Scholar]
Llewellyn 2003 {published data only}
- Llewellyn G, McConnell D, Honey A, Mayes R, Russo D. Promoting health and home safety for children of parents with intellectual disability: a randomized control trial.. Research in Developmental Disabilities 2003;24:405‐31. [DOI] [PubMed] [Google Scholar]
McLean 1996 {published data only}
- McLean D, Lord S. Falling in older people at home: transfer limitations and environmental risk factors. Australian Occupational Therapy Journal 1996;43:13‐8. [Google Scholar]
McMurdo 2000 {published data only}
- McMurdo ET, Millar AM, Daly F. A randomized controlled trial of fall prevention strategies in old peoples' homes. Gerontology 2000;46:83‐7. [DOI] [PubMed] [Google Scholar]
Minkovitz 2010 {published data only}
- Minkovitz MD, Hughart N, Strobino D, Scharfstein D, Grason H, Hou W, et al. A practice‐based intervention to enhance quality of care in the first 3 years of life. JAMA 2003;290(23):3081‐91. [DOI] [PubMed] [Google Scholar]
Morgan 2005 {published data only}
- Morgan RO, Devito CA, Stevens JA, Branche CM, Virnig BA, Wingo PA, et al. A self‐assessment tool was reliable in identifying hazards in the homes of elders. Journal of Clinical Epidemiology 2005;58(12):1252‐9. [DOI] [PubMed] [Google Scholar]
Morgenstern 2000 {published data only}
- Morgenstern H, Bingham T, Reza A. Effects of pool‐fencing ordinances and other factors. American Journal of Public Health 2000;90(4):595‐601. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nelson 2005 {published data only}
- Nelson CS, Higman SM, Sia C, McFarlane E, Fuddy L, Duggan AK, et al. Medical homes for at‐risk children: parental reports of clinician‐parent relationships, anticipatory guidance, and behavior changes. Pediatrics 2005;115(1):48‐56. [DOI] [PubMed] [Google Scholar]
Neno 2008 {published data only}
- Neno R. The rise of falls research. Nursing Older People 2008;20(6):8‐9. [DOI] [PubMed] [Google Scholar]
Neyens 2009 {published data only}
- Neyens JC, Dijcks BP, Twisk J, Schols JM, Haastregt JC, Heuvel WJ, et al. A multifactorial intervention for the prevention of falls in psychogeriatric nursing home patients, a randomised controlled trial (RCT). Age & Ageing 2009;38(2):194‐9. [DOI] [PubMed] [Google Scholar]
Northridge 1995 {published data only}
- Northridge ME, Nevitt MC, Kelsey JL, Link B. Home hazards and falls in the elderly: the role of health and functional status. American Journal of Public Health 1995;85(4):509‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Odendaal 2009 {published data only}
- Odendaal W, Niekerk A, Jordaan E, Seedat M. The impact of a home visitation programme on household hazards associated with unintentional childhood injuries: a randomised controlled trial. Accident Analysis & Prevention 2009;41(1):183‐90. [DOI] [PubMed] [Google Scholar]
Ozanne‐Smith 2002 {published data only}
- Ozanne‐Smith J, Day L, Stathakis V, Sherrard J. Controlled evaluation of a community based injury prevention program in Australia. Injury Prevention 2002;8(1):18‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Paul 1994 {published data only}
- Paul CL, Sanson‐Fisher RW, Redman S. Preventing accidental injury to young children in the home using volunteers. Health Promotion International 1994;9(4):241‐9. [Google Scholar]
Peel 2000 {published data only}
- Peel N, Steinberg M, Williams G. Home safety assessment in the prevention of falls among older people. Australian and New Zealand Journal of Public Health 2000;24:536‐9. [DOI] [PubMed] [Google Scholar]
Peeters 2007 {published data only}
- Peeters GM, Vries OJ, Elders PJ, Pluijm SM, Bouter LM, Lips P, et al. Prevention of fall incidents in patients with a high risk of falling: design of a randomised controlled trial with an economic evaluation of the effect of multidisciplinary transmural care. BMC Geriatrics 2007;7:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Petridou 1996 {published data only}
- Petridou E, Polychronopoulou A, Dounis E, Tsampira P, Revinthi K, Trichopoulos D. Risk factors for injuries among the elderly in Greece. Accident Analysis and Prevention 1996;28(3):333‐8. [DOI] [PubMed] [Google Scholar]
Petridou 1997 {published data only}
- Petridou E, Tolma E, Dessypris N, Trichopoulos D. A controlled evaluation of a community injury prevention project in two Greek islands. International Journal of Epidemiology 1997;26(1):173‐9. [DOI] [PubMed] [Google Scholar]
Plautz 1996 {published data only}
- Plautz B, Beck DE, Selmar C, Radetsky M. Modifying the environment: a community‐based injury‐reduction program for elderly residents. American Journal of Preventive Medicine 1996;12(suppl.1):33‐8. [PubMed] [Google Scholar]
Poulstrop 2000 {published data only}
- Poulstrop A, Jeune B. Prevention of fall injuries requiring hospital treatment among community‐dwelling elderly. European Journal of Public Health 2000;10:45‐50. [Google Scholar]
Pressley 2009 {published data only}
- Pressley JC, Kiragu A, Lapidus G, Pomerantz WJ, Ford H, Barlow B, et al. Race and ethnic differences in a multicenter study of home safety with vouchers redeemable for free safety devices. Journal of Trauma‐Injury Infection & Critical Care 2009;67(1 Suppl):S3‐11. [DOI] [PubMed] [Google Scholar]
Ramsey 2003 {published data only}
- Ramsay LJ, Moreton G, Gorman DR, Blake E, Goh D, Elton RA, et al. Unintentional home injury in preschool‐aged children: Looking for the key ‐ an exploration of the inter‐relationship and relative importance of potential risk factors. Public Health 2003;117(6):404‐11. [DOI] [PubMed] [Google Scholar]
Rizawati 2008 {published data only}
- Rizawati M Mas Ayu. Home environment and fall at home among the elderly in Masjid Tanah Province. Journal of the University of Malaya Medical Centre 2008;11(2):72‐82. [Google Scholar]
Roberts 2004 {published data only}
- Roberts H, Curtis K, Liabo K, Rowland D, Diguiseppi C, Roberts I, et al. Putting public health evidence into practice: increasing the prevalence of working smoke alarms in disadvantaged inner city housing. Journal of Epidemiology & Community Health 2004;58(4):280‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robertson 2005 {published data only}
- Robertson AS, Rivara FP, Ebel BE, Lymp JF, Christakis DA, Robertson AS, et al. Validation of parent self‐reported home safety practices. Injury Prevention 2005;11(4):209‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robson 2003 {published data only}
- Robson E, Edwards J, Gallagher E, Baker D. Steady as you go (SAYGO): A falls‐prevention program for seniors living in the community. Canadian Journal on Aging 2003;22(2):207‐16. [Google Scholar]
Runyan 1992 {published data only}
- Runyan CW, Bangdiwala SI, Linzer MA, Sacks JJ, Butts J. Risk factors for fatal residential fires. New England Journal of Medicine 1992;327(12):859‐63. [DOI] [PubMed] [Google Scholar]
Sattin 1998 {published data only}
- Sattin RW, Rodriguez JG, DeVito CA, Wingo PA. Home environmental hazards and the risk of fall injury events among community‐dwelling older persons. Journal of the American Geriatrics Society 1998;46:669‐76. [DOI] [PubMed] [Google Scholar]
Schwarz 1993 {published data only}
- Schwarz DF, Grisso JA, Miles C, Holmes JH, Sutton RL. An injury prevention program in an urban African‐American community. American Journal of Public Health 1993;83:675‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schwebel 2009 {published data only}
- Schwebel DC, Swart D, Hui SK, Simpson J, Hobe P. Paraffin‐related injury in low‐income South African communities: knowledge, practice and perceived risk. Bulletin of the World Health Organization 2009;87(9):700‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spiegel 1977 {published data only}
- Spiegel CN, Lindaman FC. Children can't fly: a program to prevent childhood morbidity and mortality from window falls. American Journal of Public Health 1977;67:1143‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steinberg 2000 {published data only}
- Steinberg M, Cartwright C, Peel N, Williams G. A sustainable programme to prevent falls and near falls in community dwelling older people: results of a randomised trial. Journal of Epidemiology and Community Health 2000;54:227‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stone 2007 {published data only}
- Stone KE, Eastman EM, Gielen AC, Squires B, Hicks G, Kaplin D, et al. Home safety in inner cities: prevalence and feasibility of home safety‐product use in inner‐city housing. Pediatrics 2007;120(2):E346‐53. [DOI] [PubMed] [Google Scholar]
Studenski 1994 {published data only}
- Studenski S, Duncan PW, Chandler J, Samsa G, Prescott B, Hogue C, et al. Predicting falls: the role of mobility and nonphysical factors. Journal of the American Geriatrics Society 1994;42:297‐302. [DOI] [PubMed] [Google Scholar]
Swart 2008 {published data only}
- Swart L, Niekerk A, Seedat M, Jordaan E. Paraprofessional home visitation program to prevent childhood unintentional injuries in low‐income communities: a cluster randomized controlled trial. Injury Prevention 2008;14(3):164‐9. [DOI] [PubMed] [Google Scholar]
Sznajder 2003 {published data only}
- Sznajder M, Leduc S, Janvrin MP, Bonnin MH, Aegerter P, Baudier F, et al. Home delivery of an injury prevention kit for children in four French cities: a controlled randomized trial. Injury Prevention 2003;9(3):261‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tanner 2003 {published data only}
- Tanner E. Assessing home safety in homebound older adults. Geriatric Nursing 2003;24(4):250‐4. [DOI] [PubMed] [Google Scholar]
Thomas 1984 {published data only}
- Thomas KA, Hassanein RS, Christophersen ER. Evaluation of group well‐child care for improving burn prevention practices in the home. Pediatrics 1984;74(5):879‐82. [PubMed] [Google Scholar]
Thompson 1996 {published data only}
- Thompson PG. Preventing falls in the elderly at home: a community‐based program. Medical Journal of Australia 1996;164:530‐2. [PubMed] [Google Scholar]
Tideiksaar 1990 {published data only}
- Tideiksaar R. The biomedical and environmental characteristics of slips, stumbles and falls in the elderly. In: Gray, BE editor(s). Slips, Stumbles and Falls: pedestrian footwear and surfaces. Philadelphia: American Society for Testing and Materials, 1990:17‐27. [Google Scholar]
Van Rijn 1991 {published data only}
- Rijn OJ, Bouter LM, Kester AD, Knipschild PG, Meertens RM. Aetiology of burn injuries among children aged 0‐4 years: results of a case‐control study. Burns 1991;17(3):213‐9. [DOI] [PubMed] [Google Scholar]
Vind 2009 {published data only}
- Vind ABA. An outpatient multifactorial falls prevention intervention does not reduce falls in high‐risk elderly Danes. Journal of the American Geriatrics Society 2009;57(6):June. [DOI] [PubMed] [Google Scholar]
Wagner 1994 {published data only}
- Wagner EH, LaCroix AZ, Grothaus L, Leveille SG, Hecht JA, Artz K, et al. Preventing disability and falls in older adults:a population‐based randomized trial. American Journal of Public Health 1994;84(11):1800‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Waller 1993 {published data only}
- Waller AE, Clarke JA, Langley JD. An evaluation of a program to reduce home hot tap water temperatures. Australian Journal of Public Health 1993;17(2):116‐23. [PubMed] [Google Scholar]
Weatherall 2004 {published data only}
- Weatherall M. A targeted falls prevention programme plus usual care significantly reduces falls in elderly people during hospital stays. Evidence‐Based Healthcare and Public Health 2004;8(5):Oct. [Google Scholar]
Wyman 2007 {published data only}
- Wyman JF, Croghan CF, Nachreiner NM, Gross CR, Stock HH, Talley K, et al. Effectiveness of education and individualized counseling in reducing environmental hazards in the homes of community‐dwelling older women. Journal of the American Geriatrics Society 2007;55(10):1548‐56. [DOI] [PubMed] [Google Scholar]
Xia 2009 {published data only}
- Xia QH, Jiang Y, Niu CJ, Tang CX, Xia ZL, Xia QH, et al. Effectiveness of a community‐based multifaceted fall‐prevention intervention in active and independent older Chinese adults. Injury Prevention 2009;15(4):248‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yang 2008 {published data only}
- Yang J, Peek‐Asa C, Jones MP, Nordstrom DL, Taylor C, Young TL, et al. Smoke alarms by type and battery life in rural households: a randomized controlled trial. American Journal of Preventive Medicine 2008;35(1):20‐4. [DOI] [PubMed] [Google Scholar]
Yates 2001 {published data only}
- Yates SM, Dunnagan TA. Evaluating the effectiveness of a home‐based fall risk reduction program for rural community‐dwelling older adults. Journal of Gerontology 2001;56A(4):M226‐30. [DOI] [PubMed] [Google Scholar]
Ytterstad 1996 {published data only}
- Ytterstad B. The Harstad injury prevention study:community based prevention of fall‐fractures in the elderly evaluated by means of a hospital based injury recording system in Norway. Journal of Epidemiology and Community Health 1996;50:551‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Campbell 1997
- Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 1997;315(7115):1065‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2007
- Campbell AJ, Robertson MC. Rethinking individual and community fall prevention strategies: a meta‐regression comparing single and multifactorial interventions. Age Ageing 2007;36(6):656‐62. [DOI] [PubMed] [Google Scholar]
Chang 2004
- Chang JT, Morton SC, Rubenstein LZ, Mojica WA, Maglione M, Suttorp MJ, et al. Interventions for the prevention of falls in older adults: systematic review and meta‐analysis of randomised clinical trials. BMJ 2004;328(7441):680‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coleman 1996
- Munro J, Coleman P, Nicholl J, Harper R. The effectiveness of interventions to prevent accidental injury to young persons aged 15‐24 years: a review of the evidence. Sheffield: University of Sheffield Medical Care Research Unit, 1996. [Google Scholar]
DH 2009
- Department of Health. Effective interventions in health and social care. London: DH, 2009. [Google Scholar]
DiGuiseppi 2001
- DiGuiseppi C, Higgins JPT. Interventions for promoting smoke alarm ownership and function. Cochrane Database of Systematic Reviews 2001, Issue 2. [DOI: 10.1002/14651858.CD002246] [DOI] [PMC free article] [PubMed] [Google Scholar]
DoH 2001
- Department of Health. National Service Framework for older people. London: Department of Health, 2001. [Google Scholar]
DTI 1997
- Department of Trade and Industry. Home accident surveillance system. Accident data and safety research ‐ home, garden and leisure. Vol. Annual Report 21, London: DTI, 1997. [Google Scholar]
Elkan 2000
- Elkan R, Kendrick D, Hewitt M, National Coordinating Centre for HTA. The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature. Vol. 4(13), Alton: Core Research, 2000. [PubMed] [Google Scholar]
EU 2006
- Council of the European Union. Communication from the Commission to the European Parliament and the Council on Actions for a Safer Europe. Brussels: Council of the European Union, 2006. [Google Scholar]
Gates 2007
- Gates S, Lamb SE, Fisher JD, Cooke MW, Carter YH. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: systematic review and meta‐analysis. BMJ 2007;336:130‐3. [bmj.39412.525243.BE] [DOI] [PMC free article] [PubMed] [Google Scholar]
Health Development Agency 2003
- Health Development Agency. Prevention and reduction of accidental injury in children and older people. London, 2003. [Google Scholar]
Hewitt 2008
- Hewitt CE, Mitchell N, Torgerson DJ. Listen to the data when results are not significant. BMJ 2008;336(7634):23‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jensen 2003
- Jensen J, Nyberg L, Gustafson Y, Lundin‐Olsson L. Fall and injury prevention in residential care ‐ effects in residents with higher and lower levels of cognition. Journal of the American Geriatrics Society 2003;51:627‐35. [DOI] [PubMed] [Google Scholar]
Johansen 1999
- Johansen A, Harding K, Evans R, Stone M. Trauma in elderly people:what proportion of fractures are a consequence of bone fragility?. Archives of Gerontology and Geriatrics 1999;29:215‐21. [DOI] [PubMed] [Google Scholar]
King 2001
- King WJ, Klassen TP, LeBlanc J, Bernard‐Bonnin AC, Robitaille Y, Pham B, et al. The effectiveness of a home visit to prevent childhood injury. Pediatrics 2001;108(2):382‐8. [DOI] [PubMed] [Google Scholar]
Lilley 1995
- Lilley J, Arie T, Chivers C. Special reviews. Accidents involving older people: a review of the literature. Age and Ageing 1995;24:336‐45. [DOI] [PubMed] [Google Scholar]
Lyons 1998
- Lyons R, Payne C, Sheppard S, Tomlinson J. Health Evidence Bulletins ‐ Wales: Injury Prevention. Cardiff: Welsh Office, 1998. [Google Scholar]
Lyons 2002
- Lyons RA, Jones S, Palmer SR, Kemp A, Sibert JR, Shepherd J, et al. Data from All Wales Injury Surveillance System. The development and use of a low‐cost injury surveillance system: the All Wales Injury Surveillance System (AWISS). Injury Prevention 2002;8:83‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 1998
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta‐analyses?. Lancet 1998;352(9128):609‐13. [DOI] [PubMed] [Google Scholar]
NHS CRD 1996
- NHS Centre for Reviews & Dissemination. Preventing falls and subsequent injury in older people. Effective Health Care 1996;2(4):1‐16. [Google Scholar]
NICE 2004
- National Institute for Health and Clinical Excellence. The assessment and prevention of falls in older people. London: NICE, 2004. [PubMed] [Google Scholar]
Parker 2005
- Parker MJ, Gillespie WJ, Gillespie LD. Hip protectors for preventing hip fractures in older people. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD001255.pub3] [DOI] [PubMed] [Google Scholar]
Purdue 2003
- Perdue C. Falls in older people ‐ taking a multi‐disciplinary approach. Nursing Times 2003;99:28‐30. [PubMed] [Google Scholar]
Rehmani 2005
- Rehmani R. Reduction of home injury hazards by home visiting program: a randomized controlled trial. Annals of Emergency Medicine 2005;46(3):S86. [Google Scholar]
RevMan 2008 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008; Vol. 5.0.
Robertson 2001
- Robertson MC, Devlin N, Gardner MM, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: Randomised controlled trial. BMJ 2001;322(7288):697. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robertson 2001a
- Robertson MC, Gardner MM, Devlin N, McGee R, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 2: Controlled trial in multiple centres. BMJ 2001;322(7288):701. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rubenstein 2001
- Rubenstein LZ, Powers CM, MacLean CH. Quality indicators for the management and prevention of falls and mobility problems in vulnerable elders. Annals of Internal Medicine 2001;135(8 Part 2):686‐93. [DOI] [PubMed] [Google Scholar]
Scheidt 1995
- Scheidt PC, Harel Y, Trumble AC, Jones DH, Overpeck MD, Bijur PE. The epidemiology of nonfatal injuries among US children and youth. American Journal of Public Health 1995;85(7):932‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273(5):408‐12. [DOI] [PubMed] [Google Scholar]
Schulz 2000
- Schulz KF. Assessing allocation concealment and blinding in randomised controlled trials: why bother?. Evidence Based Medicine 2000;5(2):36‐8. [DOI] [PubMed] [Google Scholar]
Thomson 2001
- Thomson H, Petticrew M, Morrison D. Health effects of housing improvement:systematic review of intervention studies. BMJ 2001;323:187‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Towner 2001
- Towner E, Dowswell T, Mackereth C, Jarvis S. What works in preventing unintentional injuries in children and young adolescents? An updated systematic review. London: Health Development Agency 2001.
Van Haastregt 2000a
- Haastregt JCM, Diedericks JPM, Rossum E, Witte LP, Crebolder HF. Effects of preventive home visits to elderly people living in the community: a systematic review. BMJ 2000;320:754‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2006
- World Health Organization. Child and adolescent injury prevention: A WHO plan of action 2006‐2015. Geneva, Switzerland: WHO, 2006. [Google Scholar]
Yardley 2005
- Yardley L, Todd C. Encouraging positive attitudes to falls prevention in later life. London: Help the Aged, 2005. [Google Scholar]


