Abstract
As we move from a disease-specific care model toward comprehensive eye care (CEC), there is a need for a more holistic and integrated approach involving the health system. It should encompass not only treatment, but also prevention, promotion, and rehabilitation of incurable blindness. Although a few models already exist, the majority of health systems still face the challenges in the implementation of CEC, mainly due to political, economic, and logistic barriers. Shortage of eye care human resources, lack of educational skills, paucity of funds, limited access to instrumentation and treatment modalities, poor outreach, lack of transportation, and fear of surgery represent the major barriers to its large-scale diffusion. In most low- and middle-income countries, primary eye care services are defective and are inadequately integrated into primary health care and national health systems. Social, economic, and demographic factors such as age, gender, place of residence, personal incomes, ethnicity, political status, and health status also reduce the potential of success of any intervention. This article highlights these issues and demonstrates the way forward to address them by strengthening the health system as well as leveraging technological innovations to facilitate further care.
Keywords: Blindness, comprehensive eye care, eye care coverage, primary eye care
Vision impairment (VI) is a major global health concern, as it is associated with a diminished quality of life[1] and decreased survival expectancy in the middle-aged and elderly population.[2] Recent global data shows that there are 36 million blinds and 217 million moderately and severely visually impaired people.[3] Compared to 1990, though the prevalence of blindness and moderate and severe VI has decreased, the absolute number of blind persons has increased by 17.6% and moderate to severe VI has increased by 35%.[3,4] The economic burden of blindness, due to both direct and indirect costs, makes it extremely important to allocate adequate resources and invest in prevention, treatment, and rehabilitation programmes.[5] A significant shift in prevalence and causes of VI since the beginning of the 21st century has occurred, from relatively easy and cost-effective treatable conditions like cataract, uncorrected refractive error (URE), trachoma, onchocerciasis, to chronic diseases, globally termed as noncommunicable eye diseases (NCEDs).[6] The consequences of global eye health planning are straightforward: vertically running, stand-alone programs focusing on a specific disease rather than addressing the person as a whole cannot be effective any longer. The solution is to provide a comprehensive eye care (CEC) strategy,[7] based on integrated, multilevel models of eye care delivery (from primary to advanced tertiary levels of care), using the Health System approach and addressing all causes of blindness.[8] A comprehensive approach to eye care involves not only treatment, but also encompasses prevention, promotion, and rehabilitation for the incurable blindness as well as integrating with other stakeholders in the community. According to WHO, CEC is indented as the strategy which “aims to ensure that people have access to eye care services that meet their needs at every stage of life. This includes not only prevention and treatment services, but also vision rehabilitation. CEC care also aims to address the full spectrum of eye diseases.”[9]
Starting from this definition, the aim of this review is to illustrate the main features of CEC models, illustrate certain case studies, and to analyze the major challenges that have to be faced to ensure its global diffusion. A PubMed engine search was carried out using the terms “comprehensive eye care”, “primary eye care”, and “comprehensive ophthalmology”. All studies published in English up to December 2018, irrespective of their online publication status, were included in this review. These data were integrated with personal knowledge and peer communications and reports available on dedicated websites.
The Demographic Transition and Non-communicable Eye Diseases (NCED)
Since the launch of VISION 2020: The Right to Sight initiative in 1999, the achievements in terms of elimination of preventable blindness have been encouraging.[10,11] During the last decades, most of the global prevention programmes have focused on public health conditions, such as trachoma, onchocerciasis, and vitamin A deficiency, which have been addressed with specific control measures.[12] Specifically, onchocerciasis was eliminated in Africa and Latin America thanks to three major programmes: the Onchocerciasis Control Program (OCP), the African Program for Onchocerciasis Control (APOC), and the Onchocerciasis Elimination Program of America (OEPA). The WHO established the Alliance for Global Elimination of Trachoma (GET) by year 2020 in 1997, while the World Health Assembly (WHA) adopted a resolution in 1998 to eliminate trachoma by 2020 through the SAFE (Surgery, Antibiotics, Facial cleanliness and Environmental change) strategy. Thanks to these projects, elimination of trachoma has been achieved in many areas where the disease was endemic. Sustained political commitment of national governments, global partnerships, private–public philanthropy, non-governmental organizations (NGOs), and community support were the major reasons for success of these programs. Outstanding examples of philanthropic support include the donation of medicines like ivermectin by Merck and of azithromycin by Pfizer that were pivotal for effective control of onchocerciasis and trachoma.[12] Apart from these cases, the most visible partnership is the joint global initiative of the World Health Organization (WHO) and International Agency for the Prevention of Blindness (IAPB) for the elimination of avoidable blindness, VISION 2020: The Right to Sight.[11]
Large-scale cataract surgical programs in developing countries have been another successful step in the fight against world blindness in the period 1990–2010.[13] Wang et al. demonstrated the direct relationship between the cataract surgical rates (CSR) of a country and its per capita gross domestic product (GDP) and gross national income (GNI),[14] illustrating the impact of resource availability on the delivery of eye care. In India and Nepal, success has been achieved thanks to a combination of involvement of the ophthalmology leadership coupled with international funding, as well as the collaborative efforts between the government, NGOs, and the private sector. The formation of the District Blindness Control Society (DBCS) was one initiative that led to decentralization of planning and program implementation, resulting in increased output. A total of 15.3 million cataract operations were performed between 1995 and 2002, through the World Bank–supported Cataract Blindness Control Project, considerably reducing the burden of this condition in India.[15]
All the above examples for controlling diseases like trachoma, onchocerciasis, and cataract highlight the critical factors involved in the control of blindness and VI from a specific disease. Some of these conditions might be cleared with a one-time intervention (surgery for cataract and systemic antibiotics for trachoma); however, they need a periodic follow-up for longer community health measures. Conversely, NCEDs like glaucoma, age-related macular degeneration (AMD), and diabetic retinopathy (DR), as well as emerging ocular conditions, such as childhood blindness (pediatric cataract, congenital glaucoma, tumors, retinopathy of prematurity [ROP]), myopic degeneration, macular hole, and optic neuritis, need not only more competent diagnostic skills, but also lifelong follow-up care as well as referral across different specialties. The same holds true for many other non-blinding diseases, like dry eye, allergic conjunctivitis, uveitis, and oculoplastic and orbital conditions. These conditions also require ongoing follow-up care as well as compliance to therapy.
The relative prevalence of NCEDs and the above listed emerging conditions has been increasing in the last decade. As age is the main risk factor for many NCEDs, especially glaucoma, AMD and cataract, these changes can be relatively well-explained by the global population growth and the increased life expectancy. In addition, the nutritional and lifestyle transformations have led to a demographic and epidemiologic transition toward a less-active and more urbanized generation, with completely different health demands. For instance, the reduction in the global amount of time spent outdoor and the shift towards new highly caloric food regimens have been linked to an a raising prevalence of myopia and increased rate of obesity (and therefore type 2 diabetes and DR).[16] These changes have already taken place in high-income countries, and now are progressively becoming more frequent in low- and middle-income countries (LMICs).[17] Projections for these chronic NCEDs are alarming and can have devastating consequences on health if not identified and controlled at the earlier stage. For example, there were 382 million people with diabetes in 2013 and projections for 2035 were 592 million.[18] This will have implications on DR too. Similarly, there were approximately 65 million people with glaucoma in 2013 with projections being more than 110 million by 2040,[19] and 196 million people with ARMD in 2020 with projections for 2040 being 288 million.[20] At the same time, there is also increase in the global prevalence of conditions like myopia. There are approximately, 1.5 billion people with myopia and 163 million people with high myopia. Projections for 2050 is approximately 5 billion with 1 billion having high myopia.[16] Intervention for myopia again needs an integrated approach and should also involve other sectors in health as well as education. Similarly, there are 1.8 billion people with presbyopia, with nearly 50% of these people without appropriate spectacle near correction.[21]
The Comprehensive Eye Care
Dealing with chronic conditions is challenging: a single medical intervention (either medical, with antibiotics or spectacles; or surgical, with cataract extraction) is not enough to restore vision in these scenarios. There is a need for repeated follow-up as well as life-long therapies. There is also the need to integrate with other stakeholders in the health system. At times, NCEDs are incurable, and the response to available treatment is often unpredictable and unsatisfactory. Considering the challenges related to high treatment costs, need for regular follow-up, interaction with other healthcare sectors and patients' cooperation and compliance, it is not difficult to understand how NCEDs often result in permanent and severe visual loss.[22,23] Currently, a significant proportion of these problems are treated at the tertiary level and guidelines for their management using public health approaches at primary level is limited.[24] However, recently, these services are also being offered at primary and secondary level of care.[25,26] Most of these models are using teleophthalmology for screening, consulting, and triage for conditions like DR and glaucoma.[27]
CEC models are critical to face NCEDs; this strategy of providing eye care is based on an integrated multilevel structure [Fig. 1].[28] They include:
Figure 1.
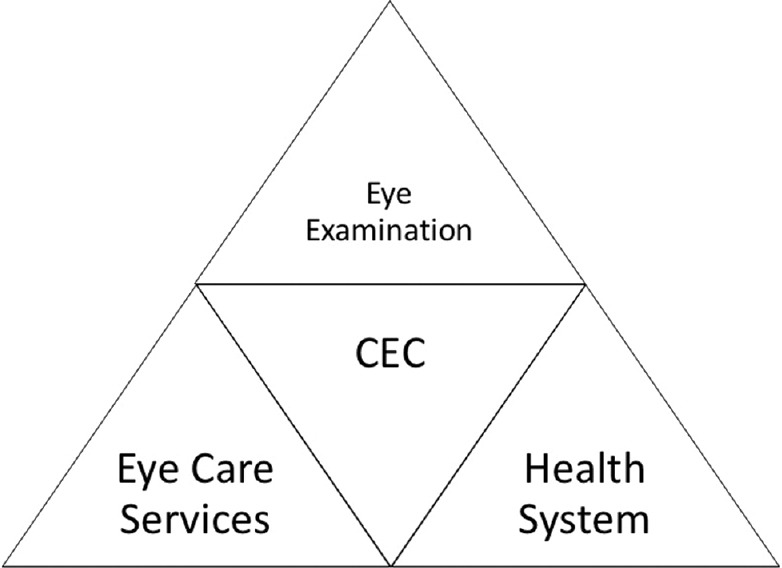
The pyramidal structure of comprehensive eye care (CEC)
Comprehensive eye examination, which refers to a relevant series of evaluations (visual acuity, anterior segment, and posterior segment) conducted for a patient with an eye problem
Comprehensive eye care services, which include eye health promotion; prevention, diagnosis, and treatment of eye diseases (primary eye care, PEC) and rehabilitation of those with irreversible blindness and low vision
Comprehensive eye care system, designed to provide the services as mentioned above equally to different groups (related to age, sex, location, genetic tract, and economic status) irrespectively to the complexity and cost of care.
The chances of success of CEC depend on the combination of six building blocks proposed by WHO as frameworks for health systems strengthening [Fig. 2].[7]
Figure 2.
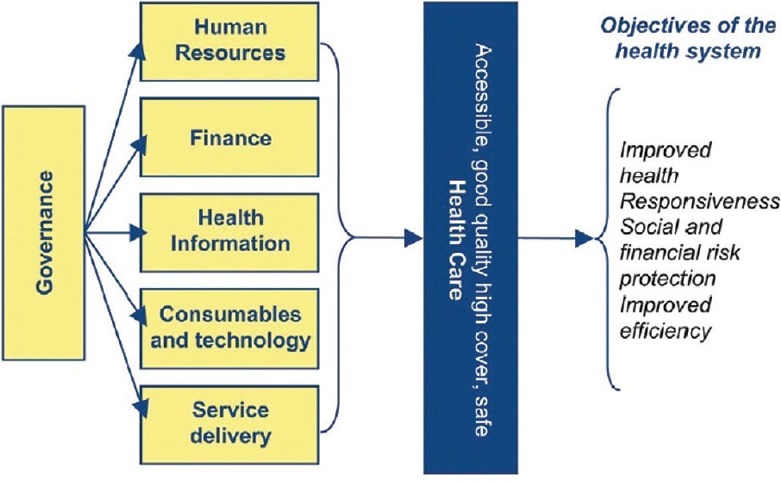
Building blocks of comprehensive eye care (CEC). Source: Blanchet K, Patel D. Indian J Ophthalmol. 2012 Sep-Oct; 60 (5):470-4
Human resources: An “Eye Care Team” approach needs to be adapted. It is necessary to have ophthalmologists well-trained to perform comprehensive eye examinations, provide or initiate medical treatment for the majority of diseases, and conduct surgical procedures up to secondary-level services, including cataract, glaucoma, and some corneal and oculoplastic procedures. He/she is supported by a range of mid-level ophthalmic personnel including nurses, optometrists, technicians, and administrative staff who aid with surgery, rehabilitation, PEC, and management planning. Respectively there are also systems for continuous professional development (CPD) for the staff. The eye care providers are able to judge appropriately those cases which should be referred for advanced care and are oriented towards long-term care and support; there is also need of provision for a two-way referral, so that those referred to tertiary care centers or higher level of care can be followed-up back. Moreover, they adopt a patient-centered approach, including patient training to increase adherence to treatment regimens (this is especially important when managing diseases like DR and glaucoma and other chronic eye conditions, where patients need to comply with life-long treatments and follow-up)
Service delivery: The CEC services are comprehensive in disease control, population coverage and referrals; they are also of high-quality, equitable, accessible, and affordable. Eye care providers offer the entire spectrum of eye services, from promotion to treatment, in a continuous manner across levels of care, settings, and providers, rather than as a one-time activity. They also deliver rehabilitation programs to irreversibly blind people, empowering them to continue to live independently and maintain their accustomed quality of life. Low vision rehabilitation services are provided at all levels of eye care, to guarantee complete fruition; if not, an efficient referral pathway is established within the hospital system. Finally, CEC systems run both vertically and horizontally: they are imbricated with other medical facilities to guarantee prompt referral of patients who need multidisciplinary management and are also vertically integrated across the primary, secondary, and tertiary levels of care
-
Consumables and technology: Infrastructure are designed to match the needs of care, thus eliminating needless expenditure on items not appropriate for that particular level of care. Physical spaces are organized to create a patient-centered ambience and involve family and community members as partners in eye care
CEC services require equitable access to essential medical products and technologies of assured quality, safety, efficacy, and cost-effectiveness. Basic equipment, including a slit lamp, applanation tonometer, direct and indirect ophthalmoscopes etc., should be available for delivery of CEC. There is also an operating microscope with adequate number of instrument sets for performing any procedure. There are systems in place for the ongoing supply of consumables. Further resources vary based on the service level where eye care is delivered
Health information: An eye health information system allows to register (systematically tracking all patients), relay (facilitate information sharing), and recall (timely review and reassessment) medical data. This permits the production, analysis, and dissemination of reliable information on eye health determinants, eye health status, and eye health system performance. An electronic medical record (EMR) / Electronic Health Record (EHR) or a manual collection of data needs to be in place
Finance: An eye health financing system, which raises adequate funds for eye care, and ensures that patients with chronic eye conditions do not suffer from unaffordable expenses due to protracted illness and extended treatment. Appropriate health insurance-based financing methods should be available to cover the CEC costs. India is a classic example of how financing for cataract surgery has increased the CSR from 1342/million in 1995 to 3620/million in 2002, and it is continuing to do so.[29] A recently published analysis has shown that many developing countries have experienced an increase in CSR in the last years, with the greatest increase observed for Iran (from 1331/million in 2005 to 6328/million in 2011) and Argentina (from 1769/million in 2005 to 5515/million in 2011)[14]
Governance: CEC relies on solid leadership and governance to guarantee universal eye health coverage and integration within the national health system; and to maintain strong links between government organizations, NGOs, and private local service providers. Finally, adequate advocacy is needed to increase awareness among stakeholders and ensure resources and environment for the treatment of major eye conditions.[30]
Implementation of Comprehensive Eye Care
Several solutions have been proposed so far to strengthen the different aspects of the CEC building blocks, including vertical and horizontal integration, PEC services in the community, formal and informal training to enable task shifting, and competence and funding buildup.[31] In addition, commitment from political leadership coordinated with voluntary associations, NGOs, and public–private partnerships is critical to raising adequate funding.[32]
-
Human resources: The recognition of new figures of eye care personnel is necessary to address the shortage in human resources and service delivery. Primary health workers in local and rural African districts have been effectively trained and basically equipped to identify and refer patients with latent eye conditions and to treat common simple eye conditions, such as conjunctivitis or minor trauma at the primary level. Both general health care and lay persons including traditional healers,[33] school teachers,[34] and community members can be effectively recruited to perform PEC tasks in cases of lack of resources; in Malawi, the collaboration with traditional healers has resulted in an 80% increase in cataract blind patients presenting to secondary level of eye care. In Gambia, community-based rehabilitation workers, teachers, and village health workers work as nyateros or “friends of the eye” provide connection between the population and the eye care personnel, helping to reduce fear of modern eye care, to fight traditional medicine practices or self-medication, and to generate awareness about eye diseases. Another example of a successful strategy to increase human resources in Africa is the WHO-AFRO Primary Eye Care training package, aimed to instruct health personnel such as nurses and clinical officers working at primary-level health facilities in eye care[35]
These services at a community level have been implemented with specialist eye health outreach visits to remote settings,[36] which has been associated with more efficient care in rural African districts.[37] Moreover, the training of the mid-level and third level eye care personnel is addressed to perform comprehensive eye examination instead of disease-specific assessment (like cataract or trachoma); this has shown the potential to reduce the global burden of blindness from all causes in the long-term.[38] When focusing on a single condition, all the aspect of the disease, from screening to visual rehabilitation should be covered. The ophthalmologist and the mid-level ophthalmic personnel must work altogether as a team. Every single member of the team should have clearly defined skills and responsibilities, and they should be motivated with new career opportunities, good financial and professional rewards, and continuous professional development programs for a more efficient delivery of eye care[39]
Service delivery: Different approaches to delivery of eye care services range from integration into the existing primary health services, to creating new models such as the rural family health system in Pakistan or the pyramidal structure of vision centres in India. A positive example of aligning national eye health strategies and low vision services with health system strengthening has been effectively provided in Pakistan[40] and by many countries in sub-Saharan Africa, where the integration of PEC services into the existing primary health services has led to an increasing access of the population to eye care initiatives throughout the continent.[41,42] Fruition of eye care services can be also supported by outreach activities; example is given by the Swiss Red Cross in Ghana, Togo, and Mali, where outreach consultations are conducted in areas not supplied by mid- and tertiary level eye care
Consumables and technology: A recent study on the types of facilities caring for DR in India, the India 11-city 9-state study, has shown that positive results have been reached towards a comprehensive management of the disease, even though additional steps are needed. Technologic innovations, like teleophthalmology, non-mydriatic retinal cameras, and automated perimeters, will facilitate the referral system, enabling direct sharing of clinical information between PEC and secondary centers.[26] It has been proved that the addition of frequency doubling perimeter examination at the PEC level increases the sensitivity for glaucoma detection by 20%.[43] Teleophthalmology has been successfully used for eye screening for DR and ROP and in teaching and training new technicians performing photographs[25]
Health information: Information systems such as electronic health records (EHRs) have been demonstrated to be useful tools in comprehensive data management. As instance, a pilot project providing computers with health information registration software and Internet connectivity via mobile phones has been set in three eye units in Kenya, offering also training for eye health personnel, at a total cost of around $3 a month. After initial reluctance, the project has been accepted, allowing easy and direct access to data and generation of medical reports.[41] Similarly, the study “Reorganizing the Approach to Diabetes through the Application of Registries” (RADAR) in Canada has been set up with the aim to combine innovative EHRs technology with national diabetes registers to deliver organized care in remote First Nations Canadian communities[44]
Finance: The experiences of the integrated multilevel system of L V Prasad Eye Institute (LVPEI) in India has demonstrated that a CEC system can achieve financial self-sustainability, providing high-quality and low-cost eye care in rural areas with more than 50% of services free of cost.[8] Several other organizations have also demonstrated this, in other parts of India and in different countries, like Australia, sub-Saharan Africa, Middle East, and Latin America[45]
Governance: As example of successful governance, Sri Lanka has launched from 2007 a two-phase National Program for the Prevention and Control of Avoidable Blindness (NPPCAB) thanks to the collaboration of the College of Ophthalmologists and the Ministry of Health. A Vision 2020 Secretariat was established at the Health Ministry Head Office with a dedicated and competent team for coordination of the activities, infrastructure, and human resources. The control of five major ophthalmic conditions (cataract, primary eye care and childhood blindness, glaucoma, diabetic retinopathy (DR), refractive errors, and low vision) and the implementation of control programmes in most of the districts of the country were their main tasks. A population survey for evidence-based eye care resources planning was set in place. Free cataract operations were conducted in large numbers especially in the areas affected by the war. Children were screened in the primary school for refractive errors, and free spectacles were provided across the country. PEC was incorporated into the primary health care system in 13 out of the 25 districts, and a referral system was established from the primary level to tertiary level of eye care. Finally, awareness programmes for DR[46] and glaucoma were carried out at both a national and a local level[47]
Human resource planning must be effectively supported by the knowledge of the current prevalence and future projections of ocular diseases in a given country. Epidemiologic cross-sectional surveys and rapid assessment studies are indispensable tools in the assessment of public health needs and monitoring interventions[48]
Finally, to ensure equity in eye care access, several countries have included eye services in the national health coverage schemes. Thailand, for instance, achieved universal health coverage through the implementation of the Universal Coverage Scheme, the main social health insurance program in the country, which currently covers approximately 75% (47 million people) of the entire population. Some successful factors of Thailand's universal health care system have been a strong political leadership, community engagement, and stiff budget control.[49] In the same period, Ghana has established a National Health Insurance Scheme in 2003, including cataract and eyelid surgery, biometry, visual fields, refraction, and basic ophthalmic preparations, which nowadays covers more than 60% of the population.[50] Burkina Faso has introduced user fees waivers for public eye care facilities for children under five, with a six-fold increase in the number of children attending at health facilities.[51] In Chile, where 70% of the population is not covered by private insurance, the government guarantees universal eye health coverage by paying the fees in full if the patients unable to afford. In India, the Pradhan Mantri Jan Arogya Yojana (PMJAY) or National Health Protection Scheme has been launched in 2018 providing interventions in primary, secondary, and tertiary care, including eye care, covering both preventive, therapeutic, and promotive actions.[52] Finally, Saudi Arabia has incorporated prevention of blindness into its new primary health care policy with a dedicated budget line and training schedule.[53]
Issues and Challenges in Providing CEC
Data from several population-based surveys and from the IAPB country chairs regarding the national health policy, the national health expenditure, the insurance systems, the expenses for eye health care, the strength of eye health personnel, the training programmes, human resources planning, and the presence of the international NGOs in different Asian countries in 2015 have been published.[54] The eye care service profile in the Southeast Asia region turned out to be encouraging: the blindness prevalence was low in Bhutan (0.33%), Nepal (0.35%), Myanmar (0.58%) and Thailand (0.59%), but still high in Timor-Leste (4.2% for people over 40). Five out of the 11 countries analyzed have an established national eye health plan, namely Bangladesh, with the Bangladesh National Control of the Blind (BNCB); India, with the National Program for Control of Blindness (NPCB); Indonesia, with the Ministry of Health, National Eye Committee; Nepal, with the Apex Body of eye health; and Thailand, with the National Committee of Eye Care services. Free primary eye care delivery is still not uniform and eye health care insurance coverage is highest in Thailand, compared to the other countries. As per capacity and resource building, the number of ophthalmologists has been increasing since 2010, even though the availability of auxiliary ophthalmic personnel is still insufficient. Cataract surgery coverage is as high as 96% in certain countries, including Thailand, Sri Lanka, and Nepal. Finally, strong links between international NGOs and eye care provision is established in many countries, including Bangladesh, India, Nepal, Indonesia, and Timor Leste.
Despite efforts at global, regional, country, and district levels in terms of political and financial commitment, most of the LMICs in the rest of the World have still unmet needs and insufficient budgets for health care. Shortage of eye care human resources, lack of educational skills, paucity of funds, limited access to instrumentation and treatment modalities, poor outreach, lack of transportation, and fear of surgery may still represent the major barriers to CEC large-scale diffusion.[53] Each of the requirements listed above needed for health system strengthening represents a serious issue for LMICs, due to consistent political, economic, and logistic barriers. The issues in providing CEC can be assessed with the same combination of the WHO six building blocks proposed above:
Human resources: Consistent gaps in the medical coverage characterize LMICs, though there are more than 200,000 eye care practitioners in the World.[55] A recent study has shown that only five countries in sub-Saharan Africa, out of 21 included in the review, are currently meeting WHO standards for ophthalmic personnel, and that is not expected to change by 2020;[56] the rest of the 21 countries had fewer ophthalmologists than recommended (i.e. four per one million), while no country in sub-Saharan Africa had the appropriate number of optometrists.[57] Inappropriate human resources coupled with inadequate level of technology and lack of equipment and medications have been identified as the major causes of low CSR and trichiasis surgery[58,59]
Service delivery: For eye care especially, population coverage is inadequate, and treatment resources are unevenly distributed. Along with international differences, local inequities should be addressed to fulfill universal coverage of the CEC system. Social, economic, and demographic factors, such as age, gender, place of residence (state or district), personal incomes, ethnicity, political and health status, also reduce the potential of success of any intervention.[53] As a result, a large percentage of “neglected population” receive very little health care of appropriate quality.[12,60] Neglected population constitutes people living in urban slums or rural and tribal areas, illiterates from lower socioeconomic groups, women and children, people with disabilities, and migrants and refugees[61]
Consumables and technology: Service delivery, including transportation to care centers, distribution logistics, surgical consumables and technology, and dispensing treatment represent the main challenges in establishing CEC systems. Outreach camps usually help in filling these gaps, but this approach is often not sufficient to cover all the needs of the population, especially in the poor and rural areas. Equipment maintenance should also be planned to provide quality services efficiently and effectively. A questionnaire on the key issues and challenges faced by eye health providers with regard to eye care equipment published in 2010 revealed that 60% of government eye units had equipment that did not work and 20% of all the eye units reported that they had equipment left unrepaired for more than 12 months.[62] The impact of breakdowns resulted in frustrating delay in proper treatment and referral. In addition, the inability to conduct a proper assessment (due to non-functioning instrumentation) increases the risk of disease progression and poor outcomes
Health information: Medical record systems are often lacking, resulting in fragmented healthcare data; if such systems are in place, there is no review or feedback on the information collected to make evidence-based decisions. At the same time, the quality of the records may also be questionable
Finance and Governance: Growing evidence shows that early diagnosis and treatment of many chronic diseases can significantly modify their natural history.[63,64,65] Only a few countries have planned for defined public health approaches in terms of awareness, health education, and prevention. Screening programmes have been proposed for DR,[66] AMD,[67] glaucoma,[68] refractive errors in children,[69] and ROP.[70] However, there is a severe limitation of access and affordability in most parts of the World.[71,72] Advocacy is needed to encourage governments to set up training programmes, professional standards, careers and salaries for ophthalmic workers; however, only ophthalmologists, ophthalmic nurses, optometrists, opticians, and orthoptists are currently recognized in the International Standard Classification of Occupations (ISCO-08). Recognition of new figures of eye care allied personnel is necessary to ensure to address the lacks and inequality in service delivery.
Apart from these major themes, there are issues with compliance to treatment, especially for chronic conditions as well as having a robust two-way referral mechanism in place. In most LMICs, PEC services are defective and inadequately integrated into primary health care and national health systems.[73] A recent analysis in two districts in Tanzania has shown that despite successful and satisfying training of primary health workers in primary eye care, there was still a strong limitation in service provision and fruition by the population due to poor integration in the local health system. Major flaws recognized were absence of an agreed and defined system of supervision of the trained workers; inability of the health management information system to collect information on a full spectrum of eye conditions treated in primary facilities; inadequateness of the referral systems to ensure continuity of care between primary and secondary level facilities; and excessive costs for many patients to uptake the referral. As a result, many primary health workers felt abandoned, frustrated, and demotivated in providing eye care.[74]
The referral organization is also poor. This leads to delay in treatment, increase in the possibility of self-medication, approaching pharmacies directly or using traditional remedies, or the compulsion to seek primary care directly at secondary and tertiary levels, using resources required for more complex cases.[75] Finally, coverage by low vision programs is often inadequate with respect to the demand. In LMICs, it is estimated that only 5–10% of the people needing low vision services have access to it.[76] Finally, it must be kept in mind that many LMICs still have to tackle infectious diseases, such as trachoma and onchocerciasis, as well as cataract and uncorrected refractive errors, along with rapidly emerging NCEDs.
Conclusion
In conclusion, while a vertical model of eye care has been working efficiently for diseases like onchocerciasis, trachoma, and cataract, a comprehensive eye care approach should be advocated whenever possible to address the rapidly growing burden of NCEDs. Developing a robust, sustainable, and good-quality CEC system throughout the world, with focus on areas of the highest need, is the first step toward eliminating avoidable blindness. Strengthening the components of health system would be the approach as we move forward.
The recognition of new figures of eye care personnel is necessary to address the shortage in human resources and service delivery. Involvement of primary health workers, clinical officers, and non-ophthalmic personnel help in assuring eye health continuity and service delivery. For appropriate delivery of eye care services, integration into the existing primary health services is pivotal. Modern technologies and standardized data collection tools are necessary, but also need an even distribution, initial training, and regular maintenance services. Advocacy and recognition of new figures of eye care allied personnel is necessary to ensure to address the lacks and inequalities in service delivery and to persuade governance to invest in eye care. Moreover, CEC should be necessarily integrated in the health system of each country. The specific approach, the composition of personnel teams, and the territorial organization of CEC services should be tailored according to the specific disease/socioeconomical context/demographical setting. Other, but not less important, concerns relate to the proper development of rehabilitation services for the irreversible visually impaired. Further work is needed to implement these programmes both in the central and the peripheral centers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Crewe JM, Morlet N, Morgan WH, Spilsbury K, Mukhtar A, Clark A, et al. Quality of life of the most severely vision-impaired. Clin Exp Ophthalmol. 2011;39:336–43. doi: 10.1111/j.1442-9071.2010.02466.x. [DOI] [PubMed] [Google Scholar]
- 2.Khanna RC, Murthy GV, Giridhar P, Krishnaiah S, Pant HB, Palamaner Subash Shantha G, et al. Cataract, visual impairment and long-term mortality in a rural cohort in India: The Andhra Pradesh eye disease study. PLoS One. 2013;8:e78002. doi: 10.1371/journal.pone.0078002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourne RRA, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: A systematic review and meta-analysis. Lancet Glob Health. 2017;5:e888–97. doi: 10.1016/S2214-109X(17)30293-0. [DOI] [PubMed] [Google Scholar]
- 4.Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990-2020: A systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–34. doi: 10.1016/S2214-109X(17)30393-5. [DOI] [PubMed] [Google Scholar]
- 5.Frick KD. What the comprehensive economics of blindness and visual impairment can help us understand. Indian J Ophthalmol. 2012;60:406–10. doi: 10.4103/0301-4738.100535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Resnikoff S, Kocur I. Non-communicable eye diseases: Facing the future. Community Eye Health. 2014;27:41–3. [PMC free article] [PubMed] [Google Scholar]
- 7.Khanna RC, Marmamula S, Rao GN. International vision care: Issues and approaches. Annu Rev Vis Sci. 2017;3:53–68. doi: 10.1146/annurev-vision-102016-061407. [DOI] [PubMed] [Google Scholar]
- 8.Rao GN, Khanna RC, Athota SM, Rajshekar V, Rani PK. Integrated model of primary and secondary eye care for underserved rural areas: The L V Prasad Eye Institute experience. Indian J Ophthalmol. 2012;60:396–400. doi: 10.4103/0301-4738.100533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Organization WH. Comprehensive eye care. 2018. [Last accessed on 2019 Apr 24]. Available from: https://www.who.int/blindness/comprehensive-eye-care/en/
- 10.Ackland P. The accomplishments of the global initiative VISION 2020: The right to sight and the focus for the next 8 years of the campaign. Indian J Ophthalmol. 2012;60:380–6. doi: 10.4103/0301-4738.100531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pizzarello L, Abiose A, Ffytche T, Duerksen R, Thulasiraj R, Taylor H, et al. VISION 2020: The right to sight: A global initiative to eliminate avoidable blindness. Arch Ophthalmol. 2004;122:615–20. doi: 10.1001/archopht.122.4.615. [DOI] [PubMed] [Google Scholar]
- 12.Rao GN. The Barrie Jones lecture-eye care for the neglected population: Challenges and solutions. Eye (Lond) 2015;29:30–45. doi: 10.1038/eye.2014.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khairallah M, Kahloun R, Bourne R, Limburg H, Flaxman SR, Jonas JB, et al. Number of people blind or visually impaired by cataract worldwide and in world regions, 1990 to 2010. Invest Ophthalmol Vis Sci. 2015;56:6762–9. doi: 10.1167/iovs.15-17201. [DOI] [PubMed] [Google Scholar]
- 14.Wang W, Yan W, Fotis K, Prasad NM, Lansingh VC, Taylor HR, et al. Cataract surgical rate and socioeconomics: A global study. Invest Ophthalmol Vis Sci. 2016;57:5872–81. doi: 10.1167/iovs.16-19894. [DOI] [PubMed] [Google Scholar]
- 15.India: Cataract Blindness Control Project. [Last accessed on 2019 Apr 24]. Available from: http://web.worldbank.org/archive/website01291/WEB/0__CO-86.HTM .
- 16.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 17.Atiim GA, Elliott SJ. The global epidemiologic transition: Noncommunicable diseases and emerging health risk of allergic disease in Sub-Saharan Africa. Health Educ Behav. 2016;43(1 Suppl):37S–55S. doi: 10.1177/1090198115606918. [DOI] [PubMed] [Google Scholar]
- 18.Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103:137–49. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90. doi: 10.1016/j.ophtha.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 20.Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob Health. 2014;2:e106–16. doi: 10.1016/S2214-109X(13)70145-1. [DOI] [PubMed] [Google Scholar]
- 21.Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: Systematic review, meta-analysis, and modelling. Ophthalmology. 2018;125:1492–9. doi: 10.1016/j.ophtha.2018.04.013. [DOI] [PubMed] [Google Scholar]
- 22.Taylor HR, Pezzullo ML, Keeffe JE. The economic impact and cost of visual impairment in Australia. Br J Ophthalmol. 2006;90:272–5. doi: 10.1136/bjo.2005.080986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Velez-Gomez MC, Vasquez-Trespalacios EM. Adherence to topical treatment of glaucoma, risk and protective factors: A review. Arch Soc Esp Oftalmol. 2018;93:87–92. doi: 10.1016/j.oftal.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 24.Rao GN. Ophthalmology and opportunities. Indian J Ophthalmol. 2017;65:335–6. doi: 10.4103/ijo.IJO_319_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prathiba V, Rema M. Teleophthalmology: A model for eye care delivery in rural and underserved areas of India. Int J Family Med. 2011;2011:683267. doi: 10.1155/2011/683267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sreelatha OK, Ramesh SV. Teleophthalmology: Improving patient outcomes? Clin Ophthalmol. 2016;10:285–95. doi: 10.2147/OPTH.S80487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caffery LJ, Taylor M, Gole G, Smith AC. Models of care in tele-ophthalmology: A scoping review. J Telemed Telecare. 2019;25:106–22. doi: 10.1177/1357633X17742182. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. Everybody's Business: Strengthening Health Systems to Improve Health Outcomes: WHO's Framework for Action. Geneva: World Health Organization; 2007. [Google Scholar]
- 29.Jose R, Bachani D. World Bank-assisted cataract blindness control project. Indian J Ophthalmol. 1995;43:35–43. [PubMed] [Google Scholar]
- 30.Ravilla TD, Ramasamy D. Advocacy for eye care. Indian J Ophthalmol. 2012;60:376–9. doi: 10.4103/0301-4738.100530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blanchet K, Patel D. Applying principles of health system strengthening to eye care. Indian J Ophthalmol. 2012;60:470–4. doi: 10.4103/0301-4738.100553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McIntyre D, Ranson MK, Aulakh BK, Honda A. Promoting universal financial protection: Evidence from seven low- and middle-income countries on factors facilitating or hindering progress. Health Res Policy Syst. 2013;11:36. doi: 10.1186/1478-4505-11-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lewallen S, Courtright P. Role for traditional healers in eye care. Lancet. 1995;345:456. doi: 10.1016/s0140-6736(95)90440-9. [DOI] [PubMed] [Google Scholar]
- 34.Wedner SH, Ross DA, Balira R, Kaji L, Foster A. Prevalence of eye diseases in primary school children in a rural area of Tanzania. Br J Ophthalmol. 2000;84:1291–7. doi: 10.1136/bjo.84.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Graham R. Facing the crisis in human resources for eye health in sub-Saharan Africa. Community Eye Health. 2017;30:85–7. [PMC free article] [PubMed] [Google Scholar]
- 36.Gruen R, Weeramanthri T, Knight S, Bailie R. Specialist outreach clinics in primary care and rural hospital settings (Cochrane Review) Community Eye Health. 2006;19:31. [PMC free article] [PubMed] [Google Scholar]
- 37.Courtright P, Murenzi J, Mathenge W, Munana J, Muller A. Reaching rural Africans with eye care services: Findings from primary eye care approaches in Rubavu District, Rwanda. Trop Med Int Health. 2010;15:692–6. doi: 10.1111/j.1365-3156.2010.02530.x. [DOI] [PubMed] [Google Scholar]
- 38.Lawlor M, Thomas R. Addressing glaucoma in the developing countries of the Asia Pacific region: An opportunity to transition from disease-specific responses to integration of eye care. Asia Pac J Ophthalmol (Phila) 2014;3:4–8. doi: 10.1097/APO.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 39.Shamanna BR, Nirmalan PK, Saravanan S. Roles and responsibilities in the secondary level eye care model. Community Eye Health. 2005;18:120–1. [PMC free article] [PubMed] [Google Scholar]
- 40.Khan AA, Khan NU, Bile KM, Awan H. Creating synergies for health systems strengthening through partnerships in Pakistan--A case study of the national eye health programme. East Mediterr Health J. 2010;16(Suppl):S61–8. [PubMed] [Google Scholar]
- 41.du Toit R, Faal HB, Etya’ale D, Wiafe B, Mason I, Graham R, et al. Evidence for integrating eye health into primary health care in Africa: A health systems strengthening approach. BMC Health Serv Res. 2013;13:102. doi: 10.1186/1472-6963-13-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lilian RR, Railton J, Schaftenaar E, Mabitsi M, Grobbelaar CJ, Khosa NS, et al. Strengthening primary eye care in South Africa: An assessment of services and prospective evaluation of a health systems support package. PLoS One. 2018;13:e0197432. doi: 10.1371/journal.pone.0197432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomas R, Naveen S, Nirmalan PK, Parikh R. Detection of ocular disease by a vision-centre technician and the role of frequency-doubling technology perimetry in this setting. Br J Ophthalmol. 2010;94:214–8. doi: 10.1136/bjo.2008.152165. [DOI] [PubMed] [Google Scholar]
- 44.Eurich DT, Majumdar SR, Wozniak LA, Soprovich A, Meneen K, Johnson JA, et al. Addressing the gaps in diabetes care in first nations communities with the reorganizing the approach to diabetes through the application of registries (RADAR): The project protocol. BMC Health Serv Res. 2017;17:117. doi: 10.1186/s12913-017-2049-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Qureshi BM, Mansur R, Al-Rajhi A, Lansingh V, Eckert K, Hassan K, et al. Best practice eye care models. Indian J Ophthalmol. 2012;60:351–7. doi: 10.4103/0301-4738.100526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Piyasena PN, Murthy GV. A situation analysis of diabetic eye care service delivery in health care institutions of the Western Province of Sri Lanka. Ceylon Med J. 2017;62:205–6. doi: 10.4038/cmj.v62i3.8527. [DOI] [PubMed] [Google Scholar]
- 47.Yasmin S. An integrated low vision service: Sri Lanka. Community Eye Health. 2012;25:16. [PMC free article] [PubMed] [Google Scholar]
- 48.Marmamula S, Keeffe JE, Rao GN. Rapid assessment methods in eye care: An overview. Indian J Ophthalmol. 2012;60:416–22. doi: 10.4103/0301-4738.100539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Limwattananon S, Tangcharoensathien V, Tisayaticom K, Boonyapaisarncharoen T, Prakongsai P. Why has the universal coverage scheme in Thailand achieved a pro-poor public subsidy for health care? BMC Public Health. 2012;12(Suppl 1):S6. doi: 10.1186/1471-2458-12-S1-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jehu-Appiah C, Aryeetey G, Spaan E, de Hoop T, Agyepong I, Baltussen R. Equity aspects of the National Health Insurance Scheme in Ghana: Who is enrolling, who is not and why? Soc Sci Med. 2011;72:157–65. doi: 10.1016/j.socscimed.2010.10.025. [DOI] [PubMed] [Google Scholar]
- 51.Yaya Bocoum F, Grimm M, Hartwig R. The health care burden in rural Burkina Faso: Consequences and implications for insurance design. SSM Popul Health. 2018;6:309–16. doi: 10.1016/j.ssmph.2018.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Angell BJ, Prinja S, Gupt A, Jha V, Jan S. The Ayushman Bharat Pradhan Mantri Jan Arogya Yojana and the path to universal health coverage in India: Overcoming the challenges of stewardship and governance. PLoS Med. 2019;16:e1002759. doi: 10.1371/journal.pmed.1002759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ellison EW. Universal eye health: Increasing access for the poorest. Community Eye Health. 2013;26:s3. [PMC free article] [PubMed] [Google Scholar]
- 54.Das T, Ackland P, Correia M, Hanutsaha P, Mahipala P, Nukella PB, et al. Is the 2015 eye care service delivery profile in Southeast Asia closer to universal eye health need! Int Ophthalmol. 2018;38:469–80. doi: 10.1007/s10792-017-0481-y. [DOI] [PubMed] [Google Scholar]
- 55.Resnikoff S, Felch W, Gauthier TM, Spivey B. The number of ophthalmologists in practice and training worldwide: A growing gap despite more than 200,000 practitioners. Br J Ophthalmol. 2012;96:783–7. doi: 10.1136/bjophthalmol-2011-301378. [DOI] [PubMed] [Google Scholar]
- 56.Palmer JJ, Chinanayi F, Gilbert A, Pillay D, Fox S, Jaggernath J, et al. Trends and implications for achieving VISION 2020 human resources for eye health targets in 16 countries of sub-Saharan Africa by the year 2020. Hum Resour Health. 2014;12:45. doi: 10.1186/1478-4491-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Palmer JJ, Chinanayi F, Gilbert A, Pillay D, Fox S, Jaggernath J, et al. Mapping human resources for eye health in 21 countries of sub-Saharan Africa: Current progress towards VISION 2020. Hum Resour Health. 2014;12:44. doi: 10.1186/1478-4491-12-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Courtright P, Ndegwa L, Msosa J, Banzi J. Use of our existing eye care human resources: Assessment of the productivity of cataract surgeons trained in eastern Africa. Arch Ophthalmol. 2007;125:684–7. doi: 10.1001/archopht.125.5.684. [DOI] [PubMed] [Google Scholar]
- 59.Habtamu E, Rajak SN, Gebre T, Zerihun M, Genet A, Emerson PM, et al. Clearing the backlog: Trichiasis surgeon retention and productivity in northern Ethiopia. PLoS Negl Trop Dis. 2011;5:e1014. doi: 10.1371/journal.pntd.0001014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Galambos CM. Health care disparities among rural populations: A neglected frontier. Health Soc Work. 2005;30:179–81. doi: 10.1093/hsw/30.3.179. [DOI] [PubMed] [Google Scholar]
- 61.Joseph S, Ravilla T, Bassett K. Gender issues in a cataract surgical population in South India. Ophthalmic Epidemiol. 2013;20:96–101. doi: 10.3109/09286586.2013.766756. [DOI] [PubMed] [Google Scholar]
- 62.Patel D, Mercer E, Mason I. Ophthalmic equipment survey 2010: Preliminary results. Community Eye Health. 2010;23:22–5. [PMC free article] [PubMed] [Google Scholar]
- 63.Olafsdottir E, Andersson DK, Dedorsson I, Svardsudd K, Jansson SP, Stefansson E. Early detection of type 2 diabetes mellitus and screening for retinopathy are associated with reduced prevalence and severity of retinopathy. Acta Ophthalmol. 2016;94:232–9. doi: 10.1111/aos.12954. [DOI] [PubMed] [Google Scholar]
- 64.Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E, et al. Factors for glaucoma progression and the effect of treatment: The early manifest glaucoma trial. Arch Ophthalmol. 2003;121:48–56. doi: 10.1001/archopht.121.1.48. [DOI] [PubMed] [Google Scholar]
- 65.Bressler NM. Early detection and treatment of neovascular age-related macular degeneration. J Am Board Fam Pract. 2002;15:142–52. [PubMed] [Google Scholar]
- 66.Murthy KR, Murthy PR, Kapur A, Owens DR. Mobile diabetes eye care: Experience in developing countries. Diabetes Res Clin Pract. 2012;97:343–9. doi: 10.1016/j.diabres.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 67.Heraghty J, Cummins R. A layered approach to raising public awareness of macular degeneration in Australia. Am J Public Health. 2012;102:1655–9. doi: 10.2105/AJPH.2012.300657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Thapa SS, Kelley KH, Rens GV, Paudyal I, Chang L. A novel approach to glaucoma screening and education in Nepal. BMC Ophthalmol. 2008;8:21. doi: 10.1186/1471-2415-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kaur G, Koshy J, Thomas S, Kapoor H, Zachariah JG, Bedi S. Vision screening of school children by teachers as a community based strategy to address the challenges of childhood blindness. J Clin Diagn Res. 2016;10:NC09–14. doi: 10.7860/JCDR/2016/18939.7628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Akman A, Yilmaz E, Mutlu H, Ozdogan M. Complete remission of psoriasis following bevacizumab therapy for colon cancer. Clin Exp Dermatol. 2009;34:e202–4. doi: 10.1111/j.1365-2230.2008.02991.x. [DOI] [PubMed] [Google Scholar]
- 71.Butt NH, Ayub MH, Ali MH. Challenges in the management of glaucoma in developing countries. Taiwan J Ophthalmol. 2016;6:119–22. doi: 10.1016/j.tjo.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ezegwui IR, Aghaji AE, Uche NJ, Onwasigwe EN. Challenges in the management of paediatric cataract in a developing country. Int J Ophthalmol. 2011;4:66–8. doi: 10.3980/j.issn.2222-3959.2011.01.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Woo GC, Woo SY. The need for full scope primary eye care in every country. Clin Exp Optom. 2013;96:1–3. doi: 10.1111/j.1444-0938.2012.00774.x. [DOI] [PubMed] [Google Scholar]
- 74.Jolley E, Mafwiri M, Hunter J, Schmidt E. Integration of eye health into primary care services in Tanzania: A qualitative investigation of experiences in two districts. BMC Health Serv Res. 2017;17:823. doi: 10.1186/s12913-017-2787-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Al-Attas AH, Williams CD, Pitchforth EL, O’Callaghan CO, Lewallen S. Understanding delay in accessing specialist emergency eye care in a developing country: Eye trauma in Tanzania. Ophthalmic Epidemiol. 2010;17:103–12. doi: 10.3109/09286580903453522. [DOI] [PubMed] [Google Scholar]
- 76.Ryan B. Models of low vision care: Past, present and future. Clin Exp Optom. 2014;97:209–13. doi: 10.1111/cxo.12157. [DOI] [PubMed] [Google Scholar]


