Abstract
Childhood blindness is one of the priority targets of Vision 2020—Right To Sight due to its impact on the psychological and social growth of the child. An extensive search was performed to locate research papers on childhood blindness prevalence and its causes in the community based and blind schools, respectively, conducted from 1990 onward up to the present. Cross references were also manually searched along with expert consultation to enlarge the reference data. A total of five community-based studies on the prevalence including two refractive error studies conducted all over India in children less than 16 years were found. The causes of childhood blindness from the available blind school studies revealed that causes of childhood blindness have mainly shifted from corneal causes to whole globe abnormalities. This article highlights that though with the availability of proper healthcare facilities, the trend is changing for the causes but still a lot of effort in the form of timely neonatal eye care facilities, pediatric surgical services and proper refraction strategies is required.
Keywords: Childhood blindness, ocular morbidity, prevalence, visual impairment
Childhood blindness (CHB) is a public health concern across the world. Global estimates on childhood blindness show that there are around 1.42 million and 17.52 million children suffering from blindness and moderate to severe visual impairment, respectively.[1] Almost three quarters of these live in low–middle income countries where the prevalence is reported to be as high as 1.5 per 1000 children in contrast to high-income countries where the prevalence is 0.3 per 1000.[1,2]
Blindness in children leads to deep impact on psychological, emotional, and socioeconomic growth to the family. A child with blindness is more likely to have delays in developmental milestones, to be more frequently hospitalized, and die during childhood than a sighted child. Such severe vision loss also adversely effects the educational activities, orientation, and mobility from the early stage of life resulting in lack of employment privilege. These differential characteristics between a sighted and nonsighted child is more obvious in developing countries. Moreover, the disability adjusted life years (DALY) loss in a blind child is far more than that of adults with blindness.[3] For example, childhood blindness results in 11.2 million blind person years resulting in longer DALY loss as compared to 5.5 million blind person years of glaucoma in India. Therefore, the control of childhood blindness is one of the overarching priorities of Vision 2020 - Right to Sight initiative. Quite recently, the WHO has fixed the target to reduce the burden of avoidable visual impairment by 25% by the year 2019 from the baseline established by WHO in 2010.[4,5,6] It has been observed that unlike adult blindness that is 80% avoidable (either preventable or treatable), in children, less than 50% of the causes are avoidable.[7]
The Indian perspective on childhood blindness
As the prevalence of blindness in children is relatively lower than that in adults, a larger sample size of children is required to provide accurate data on the prevalence and causes of childhood blindness. Hence, population-based surveys on childhood blindness are few. The current prevalence of blindness in children is known to be around 0.8/1000.[3,4] The prevalence is likely to be affected by the methodology used to estimate the blindness such as community-based surveys and locations like rural or urban settings.
Despite various intervention programs, CHB remains a challenge, as much as for the epidemiologist as for the care provider. There are various difficulties associated with tackling CHB in India like diverse cultural practices and beliefs due to socioeconomic barriers. Besides this, the major challenges faced are due to inequitable distribution of healthcare services, with most of the advanced eye care centers being located in the urban areas, and remote rural villages getting ignored.
Therefore, prevalence and causes of CHB must be reviewed in order to ascertain the success of current interventions in India, and to judiciously allocate future resources, tailored to the needs of the community. Such a review will certainly highlight the need for a paradigm shift in the context of childhood intervention program in India. In fact, with population-based studies being few and far apart, and blind schools–based surveys not being representative and robust enough, it is important that data from both the sources be reviewed in cohesion to establish a holistic overview of the challenges facing us with respect to childhood blindness.
Methods
A systematic review was performed as the database gathering method for the study and in order to determine the prevalence and causes of childhood blindness in India.
Search strategy
The database search was based on the Preferred Reporting of Items for Systematic Review and Meta Analysis (PRISMA) guidelines. The search was conducted from January to June 2018. The search engines used included the Pubmed, Medline, OVID, Cochrane Library, and Google Scholar.
The search was conducted based on medical subject heading (MeSH) and keywords to search in the title and abtsract: [childhood], [child], and [blindness] or blind AND [causes] AND [Prevalence] AND [Blind schools] OR [Community] OR [Field] OR [Epidemiology], while limiting the search to English.
From initial MeSH searches, original articles and review articles that were published after January 1990 were analyzed. Citations and cross references from relevant key articles were used to identify additional publications.
The inclusion criteria for various articles were: setting: country, India, community, blind schools, community based rehabilitation (CBR) Participants: Age and number of participants Outcomes: anatomical and etiological causes of childhood blindness using WHO/PBL form. There was no restriction based on number of participants.
The studies that did not follow WHO standard guidelines/methodologies and not using the anatomical and etiological causes were excluded.[5]
Only primary sources of publication were included while the secondary publications reviewing different causes of blindness were excluded. The studies on causes of childhood blindness were divided into two time frames: those from 1990 to 2007 were compared with the studies in the next that were conducted from 2007 to 2018. A total of 30 articles were thus found to be suitable for inclusion in this review. For estimating the prevalence, data from blind schools was excluded and only community-based studies were used; only the studies from India were included finally for the systematic review [Fig. 1].
Figure 1.
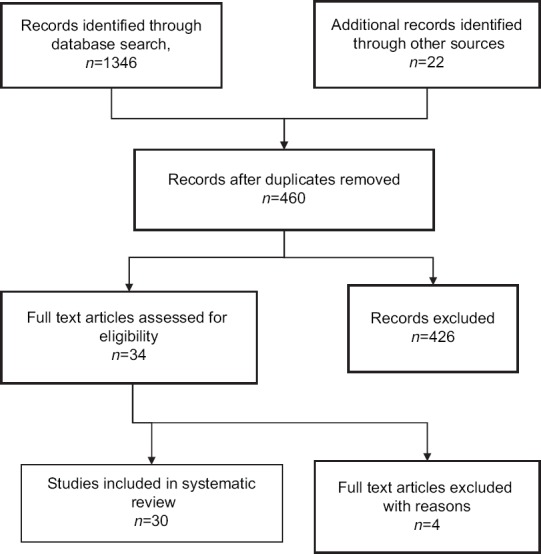
Summary of the review strategy-Flow diagram
Results
Available methods to determine the prevalence and causes of childhood blindness
Prevalence
Prevalence of CHB and VI can be determined by conducting community-based surveys. Besides this, another proxy method for evaluating CHB is Under 5 mortality rate, data from CBR or using key informants[8,9] from the community to conduct case findings. The community-based studies[1,10,11,12] have an advantage in that they depict the accurate picture of prevalence, but are resource intensive and time consuming requiring a coverage of large sample size of minimum 100,000 children.
Another important method to determine the causes of CHB is blind school–based studies as they have the advantage of using one examiner (ophthalmologist) to screen the whole school (decreasing fallacies of interobserver variation), being more cost effective and less time consuming. However, these studies have a distinct disadvantage over community-based surveys: these involve children with multiple disabilities, and are often biased because of nonrandom sampling, location, type, clustering, and population.
Under 5 mortality rate is an indirect proxy method to determine the prevalence of childhood blindness by reflecting Vitamin A deficiency and measles (nutritional deficiency)-related corneal blindness. It is estimated that a childhood blindness of 0.8 is associated with an under 5 mortality rate of 100–120 whereas a CHB of 0.3/1000 is associated with under 5 mortality rate of <20.[13]
The involvement of key informants (KI) to identify blind children is another successful novel methodology. Key informants (KIs) are local volunteers who live and/or work in their communities and are already involved in doing health-related surveys in their local areas and are familiar with the people living in these areas.[8]
Causes of CHB
Over the last few years, most of the information on blindness in children has been recorded on a specialized form designed by the WHO.[14] In this form, the causes are divided according to etiological (Hereditary, intrauterine, perinatal, childhood, and unknown) and anatomical (cornea, lens, retina, cortical, whole globe, uvea, glaucoma, and others) classification. The main advantage is that in most of the children the anatomical causes are easy to determine as compared to the etiological classifications. In developing countries, 30–72% of pediatric blindness is avoidable with most in fact being preventable.[3,7,15]
Community - based prevalence studies
As per the available information from community-based studies, the prevalence of childhood blindness varied between 0.6 per thousand to 1.06 per thousand and prevalence of visual impairment varied between 2.05 per thousand to 13.6 per thousand.[4,7,12] This variation could be attributed to the difference in definition of blindness used in these studies [Table 1].
Table 1.
Population based studies on Childhood Visual Impairment and Blindness in India (Community based)
| Author, Year | Number of examined participants, age group | Location | Study setting | Blindness prevalence Va criteria | Visual Impairment prevalence Va criteria |
|---|---|---|---|---|---|
| Dandona, 1998[4] | 1,13,514* | West Godavari, Andhra Pradesh | R & SU | 0.65/1000$ | - |
| Murthy, 2002[16] | 5950** | Delhi | U | 2.2/1000$$ | 13.6/1000# |
| Dandona, 2002[1] | 3994*** | Mahabubnagar, Andhra Pradesh | R | 2/1000$$ | 7.3/1000# |
| Nirmalan, 2003[11] | 9035* | Kariapatti, Tamil Nadu | R | 0.62/1000$ | 2.05/1000## |
| Dorairaj, 2008[10] | 8684* | Hobli, Bangalore | R | 1.06/1000$ | 3.34/1000## |
| Kemannu, 2016[12] | 23,087* | Tumkur, Karnataka | R | 0.8/1000$ | - |
Study setting- R rural, SU-Semiurban, U urban, Age group-*≤15 years of age, **5-15 years of age,***7-15 years of age, Va Criteria for blindness- $BCVA <20/400 in better eye, $$PVA <20/200 in better eye, Va Criteria for visual impairment- #PVA ≤20/60 in better eye, ##BCVA <20/60 in better eye
Blind school–based studies-causes
On reviewing the data from various blind schools for the causes of blindness between 1990 to 2007, corneal causes were mainly responsible for ocular morbidity as mentioned in the majority of studies.[15,17] On comparing this with the studies conducted after 2000 but between 2007 to 2018, whole globe was the major culprit.[7,10,11,17,18,19,20,21,22,23] Hence, the focus has shifted from preventable causes to irreversible causes. The major difference in causes in these blind school–based studies in these two decades is due to the improvement in healthcare facilities and the socioeconomic status of various countries over a period of time.
Also, there is a major difference in the causes of ocular morbidity in blind school studies[18,19,20,21,22,23] as compared to community-based studies and that could be attributed to the fact that blind school–based studies were mainly restricted to North India as compared to community-based studies that were restricted to South India where the provision of social, economic, and healthcare services is better as compared to North India [Table 2].[10,11,12]
Table 2.
Classification of blindness and proportion of visual impairment according to anatomical categories in different studies
| Year | Author (Va Criteria for BL) (Number of examined children) | Area of study, Type of study | Total No. of blind Children | Whole globe | Cornea | Lens | Retina | Cortical | Optic Nerve | Uvea | Glaucoma | Others (CNS abnormality) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1995 | Rahi[15],$$ (1411) | India* | 1318 | 25.3 | 26.4 | 12.3 | 20.7 | - | 5.9 | 5.8 | 2.6 | 0.9 |
| 2003 | Nirmalan[11],$ (1441) | Kariapatti, Tamil Nadu** | 7 | - | - | 14.3 | 14.3 | - | 28.6 | 14.3 | - | 28.6 |
| 2006 | Titiyal[7],$$$ (703) | Delhi* | 650 | 27.4 | 21.7 | 10.9 | 15.1 | - | 10.6 | 8.8 | 4.9 | 0.8 |
| 2007 | Gogate[18],$ (1985) | India, Maharashtra* | 1778 | 41.3 | 22.2 | 6.0 | 11.2 | - | - | - | - | 19.3 |
| 2008 | Dorairaj[10],$ (8684) | Hobli, Bangalore** | 14 | 35.7 | - | 42.9 | 7.1 | - | 14.2 | - | - | - |
| 2008 | Bhattacharya et al.[19],$$ (376) | North East* | 258 | 36.1 | 36.4 | 10.9 | 5.8 | - | 5.4 | 2.3 | - | 3.1 |
| 2012 | Krishnaiah[20],$ (119) | South India** | 113 | 41.4 | 8.1 | 9.9 | 18.6 | - | 6.3 | 4.5 | - | 10.8 |
| 2014 | Israfil[21],$ (460) | Pune* | 460 | 30.9 | 13.0 | 17.0 | 9.4 | - | - | - | - | - |
| 2015 | Bhalerao[22],$ (90) | Allahabad* | 90 | 54.4 | 24.4 | 10.0 | 3.3 | - | 6.7 | 1.1 | - | - |
| 2015 | Danayak et al.[23],$ (179) | Gujarat* | 179 | 42.5 | 24.0 | 7.3 | 11.7 | - | 10.6 | 3.9 | 29.6 | 40.2 |
| 2016 | Kemannu et al.[12],$ (1538) | Tumkur, Karnataka** | 18 | 16.7 | - | 27.8 | 44.4 | 5.6 | - | 5.6 | - | - |
Va Criteria for blindness SVI/BL, $$BCVA <6/60 in better eye, $BCVA <3/60 in better eye, $$$PVA <6/60 in better eye
Does a trend exists
On reviewing the data from various blind schools for the causes of visual impairment and blindness, it was found that there is a paradigm shift in the anatomical causes of CHB from corneal causes as mentioned in the studies conducted between 1990 to 2007 to causes related to whole globe after 2007 as depicted by the study done by Rahi et al. in 1995[15] that revealed the major cause of blindness to be corneal abnormalities. In another study conducted in 1995 by Thylefores et al,[17] xerophthalmia and ophthalmia neonatorum were found to be responsible for CHB and VI in six WHO regions.
In the studies conducted between 2007 and 2018 in blind schools,[18,19,20,21,22] the major anatomical cause of CHB was whole globe. The reason that could be attributed to the difference in causes in these blind school studies reflects the improvement in healthcare facilities and socioeconomic status of various countries [Table 2].[10,11,12,20
Possible causes for paradigm shift in causes of childhood blindness
In anatomical causes of blindness that include various parts of the eye, there is a newer trend in the shift of causes of blindness to whole globe that includes microphthalmos and anophthalmos; the major reason for this shift is the genetic abnormalities related to PAX 2, PAX 6, use of alcohol and drugs, and also exposure to pesticides or fertilizers during pregnancy.[24] However, one hypothesis also holds the interaction between genes controlling retinal acid signalling and maternal Vitamin A deficiency (VAD) during early fetal development similar to spina bifida and folate deficiency for the genetic abnormalities.[25,26]
The etiological causes include hereditary, intrauterine, prenatal, and postnatal. In various studies, the hereditary causes include iridofundal coloboma as a very important cause of ocular morbidity.[24,25] Also, in intrauterine causes, it was found that an improvement has been noted after covering Rubella immunization under universal immunization coverage.[27] The incidence of rubella-related ocular morbidity has decreased though it requires a strict rubella vaccination coverage and coverage in teenage girls.[28,29] Regarding postnatal causes, there is a shift towards retinal causes including retinal dystrophies and retinopathy of prematurity (ROP).[30,31,32] The reasons for emergence of ROP as a new cause is due to the availability of neonatal services (NICU) and saving low birth weight babies (LBW) and premature babies as previously most of these babies suffering from ROP did not survive due to unavailability of neonatal services.[32] A major important issue is that till now lenticular opacities were a common cause of ocular morbidity with most of them being identified as unoperated cataract, the etiology for these could be unknown or rubella. These lenticular causes like untreated cataract and uncorrected aphakia should be treated as an emergency with an important concern for avoiding complications like amblyopia and strabismus.[1,7,16]
Discussion
Impact of blindness control programs and policies
This change in the trend for causes of CHB indicates the successful implementation of various programs related to health care, immunization, and vitamin A supplementation which have made a positive impact by decreasing the burden of CHB. This trend is supported by the evidence that there has been a significant reduction in vitamin A deficiency in India over the past two decades as indicated by reduction in prevalence of bitots spots from 1.8% among preschool children in 1975 to 0.2% in 2012.[26,33] This reflects a positive response to the action taken by the Ministry of Health and Family Welfare that have changed the Vitamin A supplementation and included it as an essential component of reproductive and child health programs from 2006.[34] In a recent study (CORE) conducted by Noopur et al. on prevalence of corneal opacities, a total of 3 (0.08%) children under 15 years were found to be having corneal opacities due to ocular morbidity.[35] In India, there is a shift in the cause of CHB from the corneal diseases toward globe abnormalities.[4,10,12,15]
Besides blindness, the most important cause of VI in Indian children is refractive error.[1,16,24] The failure of correction of underlying refractive error is the most important contributory factor to VI in India;[3,16] as most of the studies done in India have taken best corrected visual acuity as the criteria therefore, uncorrected refractive error gets underrepresented. This problem can further be resolved by using modified WHO, definition for blindness and VI that uses presenting visual acuity instead of best corrected.[36] Hence, this will diagnose refractive errors that can be corrected and timely correction of refractive error can lead to further prevention of amblyopia in future years.[16,37] Also in the past, there has been a reduction in the Under 5 mortality rate by 67% between 2005 and 2015, which also serves as another supportive evidence for successful implementation of various policies (Child survival and safe motherhood programmes [CSSM] and Rashtriya Bal Swathaya programme [RBSK]) related to health care.[34]
Future interventions and strategies related to improve blindness
The change in prevalence and causes of blindness between the studies compared is very encouraging, reflecting a response to socioeconomic development and the implementation and utilization of public health programs for child health. The control of blindness in children, especially in India and similar developing countries, requires not only robust strategies but also a well-designed and functional integrated healthcare delivery system. This integrated health system, for both screening and referral services, has to be tailored for both geographical accessibility and sociocultural acceptance.
A major recommendation to combat CHB would be effective referrals to eye surgeons and especially pediatric ophthalmologists. A lot of school screenings are done by state governments but this strategy falls flat as no followups are taken and affected children are not referred further to specialists and therefore no interventions are done. A major hinderance is lack of recognition of pediatric eye care as an speciality by state governments or the Government of India. Since the government fails to recognize this, only school screenings are possible and no preschool screens are done or are effectively taken up.
A strong case regarding pediatric eye services as a distinct speciality should be made by this particular publication and followed up which would make a difference in childhood blindness. The children found deficient should be promptly referred to pediatric ophthalmologists. If the government hospitals do not have a pediatric eye care provider, they should get someone honorary for the sake of the future of these children. The impact of adult ophthalmologists does not seem to be effective in tackling the problem.
Conclusion
It should be a comprehensive eye care approach in which the provision of a continuum of health promotion, disease prevention, diagnosis, treatment, and rehabilitation that addresses the full spectrum of eye diseases is coordinated across and integrated within the community, primary, secondary, and tertiary levels within and beyond the health sector, and according to people's needs throughout the life course. To tackle with the current causes of ocular morbidity due to whole globe and retinal abnormalities, a careful genetic counselling of parents before child birth, especially in the cases of consanguineous marriage, and teleophthalmology to diagnose the preventable and potentially blinding diseases like ROP timely should be emphasized to prevent these children from becoming blind in future years.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Dandona R, Dandona L, Srinivas M, Sahare P. Refractive error in children in an rural population in India. Invest Ophthalmol Vis Sci. 2002;43:615–22. [PubMed] [Google Scholar]
- 2.World Health Organization. Cummulative official updates to ICD–Feb 2009. [Last accessed 2015 Jul]. Available from: http://www.Who.int/clasificationd/icd/Official updates Combined 1996-2008 VOLUME1.pdf .
- 3.Murthy GVS. Magnitude and temporal trends in avoidable blindness in Children (ABC) in India. Indian J Pediatr. 2017;84:924–9. doi: 10.1007/s12098-017-2405-2. [DOI] [PubMed] [Google Scholar]
- 4.Dandona L, Williams JD, Williams BC, Rao GN. Population based assessment of childhood blindness in Southern India. Arch Ophthalmol. 1998;116:545–6. [PubMed] [Google Scholar]
- 5.Dandona R, Dandona L. Childhood blindness in India: A population based perspective. Br J Ophthalmol. 2003;87:263–5. doi: 10.1136/bjo.87.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Universal Eye Health, A global action plan, 2014-2019. doi: 10.1016/j.jcjo.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 7.Titiyal JS, Pal N, Murthy GV, Gupta SK, Tandon R, Vajpayee RB. Causes and temporal trends of blindness and severe visual impairment in children in schools for the blind in North India. Br J Ophthalmol. 2003;87:941–5. doi: 10.1136/bjo.87.8.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murthy GVS, Mactaggart I, Muhit M, Islam J, Noe C, Khan AI, et al. Assessing the prevalence of sensory and motor impairment in childhood in Bangladesh using key informants. Arch Dis Child. 2014;99:1103–8. doi: 10.1136/archdischild-2014-305937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gilbert C. Changing challenges in the control of blindness in children. Eye. 2007;21:1338–43. doi: 10.1038/sj.eye.6702841. [DOI] [PubMed] [Google Scholar]
- 10.Dorairaj SK, Bandrakalli P, Shetty C, Vathsala R, Misquith D, Ritch R. Childhood blindness in a rural population of Southern India: Prevalence and etiology. Ophthalmic Epidemiol. 2008;15:176–82. doi: 10.1080/09286580801977668. [DOI] [PubMed] [Google Scholar]
- 11.Nirmalan PK, Vijayalakshmi P, Sheeladevi S, Kothari MB, Sundaresan K, Rahmathullah L. The Kariapatti pediatric eye evaluation project: Baseline ophthalmic data of children aged 15 years or younger in southern India. Am J Ophthalmol. 2003;136:703–9. doi: 10.1016/s0002-9394(03)00421-5. [DOI] [PubMed] [Google Scholar]
- 12.Kemmanu V, Hegde K, Giliyar SK, Shetty BK, Kumaramanickavel G, McCarty CA. Prevalence of childhood blindness and ocular morbidity in a rural pediatric population in Southern India. The Pavagadapediatric Eye Disease study 1. Ophthalmic Epidemiol. 2016:23:3:185–92. doi: 10.3109/09286586.2015.1090003. [DOI] [PubMed] [Google Scholar]
- 13.Imdad A, Herzer K, Mayo-Wilson E, Yakoob MY, Bhutta ZA. Vitamin A supplementation for preventing morbidity and mortality in children from 6 months to 5 years of age (Review) Cochrane Library 2011 Internet. [Last accessed on 2016]. Available from: http://onlinelibrarywileycom/doi/101002/14651858CD008524pub2/pdf . [DOI] [PubMed]
- 14.Gilbert C, Foster A, Negrel D, Thylefors B. Childhood blindness: A new form for recording causes of visual loss in children. Bull World Health Organ. 1993;71:485–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Rahi JS, Sripathi S, Gilbert CE, Foster A. Childhood blindness in India: Causes in 1318 blind school studies in nine states. Eye. 1995;9:545–50. doi: 10.1038/eye.1995.137. [DOI] [PubMed] [Google Scholar]
- 16.Murthy GV, Gupta SK, Ellwein LB, Muñoz SR, Pokharel GP, Sanga L, et al. Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci. 2002;43:623–31. [PubMed] [Google Scholar]
- 17.Thylefores B, Negrel AD, Parajasegaram R, Dadzie KY. Global data on blindness. Bull World Health Organ. 1995;73:115–21. [PMC free article] [PubMed] [Google Scholar]
- 18.Gogate P, Deshpande M, Sudrik S, Taras S, Kishore H, Gilbert C. Changing patterns of childhood blindness in Maharashtra, India. Br J Ophthalmol. 2007;91:8–12. doi: 10.1136/bjo.2006.094433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhattacharya H, Das K, Borah RR, Guha K, Gogate P, Purukayastha S, et al. Causes of childhood blindness in northeastern states of India. Indian J Ophthalmol. 2008;56:495–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Krishnaiah S, Subba Rao B, Narasamma KL, Amit G. A survey of severe visual impairment in children attending schools for the blind in a coastal district of Andhra Pradesh in South India. Eye. 2012;26:1065–70. doi: 10.1038/eye.2012.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Israfil AT, Gogate PM, Kulkarni V, Shinde M. Improving functional vision in schools for the blind students with low vision aids in Pune, India. J Clin Ophthalmol Res. 2014;2:99–101. [Google Scholar]
- 22.Bhalerao SA, Tandon M, Singh S, Dwivedi S, Kumar S, Rana J. Visual impairment and blindness among the students of blind schools in Allahabad and its vicinity: A causal assessment. Indian J Ophthalmol. 2015;63:254–8. doi: 10.4103/0301-4738.156930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Danayak PM, Patel RB. Avoidable blindness and its correction in schools for the blind in Gujarat. Int J Adv Med. 2015;2:370–2. [Google Scholar]
- 24.Fujiki K, Nakajima A, Yasuda N, Tanabe U, Kabasawa K. Genetic analysis of microphthalmos. Ophthalmic Paediatr Genet. 1992;1:139–49. [Google Scholar]
- 25.Kapil U, Gupta A. Low quality evidence for the continuation of universal vitamin A supplementation among under 5 children in India. India J Public Health. 2016;60:176–80. doi: 10.4103/0019-557X.188999. [DOI] [PubMed] [Google Scholar]
- 26.Rahi JS, Tripathi S, Gilbert CE, Foster A. Childhood blindness due to vitamin A deficiency in India: Regional variations. Arch Dis Child. 1995;72:330–3. doi: 10.1136/adc.72.4.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gilbert C, Foster A. Blindness in children: Control priorities and research opportunities. Br J Ophthalmol. 2001;85:1025–7. doi: 10.1136/bjo.85.9.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eckstein MB, Brown DWG, Foster A, Richards AF, Gilbrt CE, Vijayalakshmi P. Congental rubella in South India: Diagnosis using saliva in infants with cataract. Br Med J. 1996;312:161. doi: 10.1136/bmj.312.7024.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Special advisory group of experts of the children's vaccine initiative and the global programme for vaccines and immunisation. New vaccines, New vaccination approaches and the vaccination target groups. Weekly Epidem Rec WHO [Google Scholar]
- 30.Deorari A, Gilbert C. Controlling visual loss from retinopathy of prematurity in India. Indian Pediatr. 2016:53:S73–5. [PubMed] [Google Scholar]
- 31.Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P, et al. Characteristics of babies with severe retinopathy of prematurity in countries with low, moderate and high levels of development: Implications for screening programmes. Pediatrics. 2005;115:e518–25. doi: 10.1542/peds.2004-1180. [DOI] [PubMed] [Google Scholar]
- 32.Vinekar A, Dogra MR, Sangtam T, Narang A, Gupta A. Retinopathy of prematurity in Asian Indian babies weighing greater than 1250 grams at birth: Ten year data from a tertiary care center in a developing country. Indian J Ophthalmol. 2007;55:331–6. doi: 10.4103/0301-4738.33817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sil AK, Gilbert CE. Childhood blindness in India. J Indian Med Assoc. 2001;99:10–15. [PubMed] [Google Scholar]
- 34.International Institute for population Sciences. National Family Health Survey-4 2015-16: India Fact Sheet. Government of India. New Delhi: Ministry of Health and family welfare; 2016. [Last accessed on 2017 20 Mar]. pp. 1–6. Available from: http://rchips.org/nfhs/pdf/NHFS4/Indiapdf . [Google Scholar]
- 35.Gupta N, Vashist P, Tandon R, Gupta SK, Dwivedi S, Mani K. Prevalence of corneal opacities in the rural Indian population. The corneal opacity rural epidemiological (CORE) study. Br J Ophthalmol. 2015;99:147–52. doi: 10.1136/bjophthalmol-2014-305945. [DOI] [PubMed] [Google Scholar]
- 36.Vashist P, Senjam SS, Gupta V, Gupta N, Kumar A. Definition of blindness under national program for control of blindness Do we need to revise it. Indian J Ophthalmol. 2017:6592–6. doi: 10.4103/ijo.IJO_869_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jose R, Sachdeva S. School eye screening and the national program for control of blindness. Indian Pediatr. 2009;46:205–8. [PubMed] [Google Scholar]


