Abstract
Hepatocellular carcinoma or Liver cancer (LC) is the sixth most common cancer and the fourth cause of death worldwide in 2018. There has not been a comprehensive study on the survival rate of patients with LC in Asia yet. Therefore, the present study was conducted to evaluate the survival rate of patients with LC in Asian countries. The methodology of the present study is based on the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement. The researchers searched five international databases including Medline/PubMed, Scopus, Embase, Web of Knowledge and ProQuest until July 1, 2018. We also searched Google Scholar for detecting grey literature. The Newcastle-Ottawa Quality Assessment Form was used to evaluate the quality of selected papers. A total of 1425 titles were retrieved. 63 studies met the inclusion criteria. Based on the random-effect model one-year, three-year and five-year survival rate of LC were 34.8 % (95 % CI; 30.3-39.3), 19 % (95 % CI ; 18.2-21.8) and 18.1 % (95 % CI ;16.1-20.1) respectively. According to the results of our study, the LC survival rate in Asian countries is relatively lower than in Europe and North America.
Keywords: survival rate, hepatocellular carcinoma, systematic review, meta-analysis, Asia
Introduction
Cancer is one of the major health problems today and is currently one of the leading causes of death in many countries (Bray et al., 2018[9]). Among malignancies, liver cancer (LC) is one of the most common one, of which more than 85 % of cases of LC has been observed in developing countries (Global Burden of Disease Cancer Collaboration et al., 2017[31]). The highest incidence of this cancer is in Asian and sub-Saharan Africa (Ladep et al., 2014[61]). Evidence suggests that the incidence of this cancer is soaring (McGlynn et al., 2015[77]), which has been observed in Europe, the Pacific, as well as Asian countries (La Vecchia et al., 2000[60]; Mirzaei et al., 2016[78]; Mohammadian et al., 2016[80]; Hassanipour et al., 2019[34]). In terms of mortality, the standardized mortality rate of LC is 5.9 per 100,000. Due to the very poor prognosis of LC, the mortality rate is 95 % (Torre et al., 2016[106]; Nikbakht et al., 2019[84]). Global variation in LC rates can be explained by the distribution of viral hepatitis B and C infection, that should be mentioned here, the two viruses alone account for 78 % of the total mortality rate of LC in the world (Zamor et al., 2017[122]; Jakupi et al., 2018[38]). There is also evidence that the incidence of LC in Asia is declining in many Asian countries as a result of hepatitis B vaccination (Mansour-Ghanaei et al., 2007[71]; Yeo et al., 2013[119]; Joukar et al., 2018[44]; Aniaku et al., 2019[5]). Liver cirrhosis is another major risk factor, of which 80-90 % of these patients have hepatocellular carcinoma (Gao et al., 2012[28]). LC is one of the malignancies that have been studied by genetics, and in this case the relative risk for a person with family history is 6.2 (Fernandez et al., 1994[27]; Turati et al., 2012[109]) and also it is significantly higher in males than in women (Naugler et al., 2007[83]).
The main affecting factors for long-term survival in these patients are, early diagnosis of tumors, and treatment of patients with effective therapies (Wang et al., 2008[110]). Patients diagnosed at an early stage will be more likely to respond to treatment and have long-term survival (Yuen et al., 2000[120]) Also, in order to diagnose these patients at an early-stage, monitoring high risk people is a key and important factor (Zhang et al., 2004[125]).
Survival rate is one of the most important health indicators that is essential in evaluating diagnostic and therapeutic programs. The first step to control the burden of disease related to cancers in any population, is to understand its status in the population, as well as to collect information about the incidence, survival, type and location of cancers. It is necessary to record effective indicators on the process and survival of cancers in a monitoring area and patients' information in order to perform the correct and appropriate treatment and to apply effective therapeutic methods and prevention strategies. In spite of increasing cancer treatment costs in developing countries, a few researches that were hospital-centered and population-based information have been conducted. Studies on the survival of LC in Asian countries have achieved various results, and the studied population in these surveys has also been different. Familiarity with the various years of survival rate of this cancer in different countries as well as different population groups can provide valuable information on the control, prevention, and treatment outcomes of patients with LC. There has not been a comprehensive study on the survival rate of patients with LC in Asia yet. Therefore, according to the mentioned points, the present study was conducted to evaluate the survival rate of patients with LC in Asian countries.
Methods
The present study is a systematic review and meta-analysis study of LC survival rate in Asian countries. This study was designed and conducted in 2018. The methodology of the present study is based on the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement (Moher et al., 2015[81]).
Search strategy
The researchers searched five international databases including Medline/PubMed, Scopus, Embase, web of knowledge and ProQuest until July 1, 2018. We also searched the Google Scholar for detecting grey literature. Selected keywords for international databases included: (“neoplasm”, “cancer”, “carcinoma”, “malignancy”, “liver cancer”, “hepatocellular neoplasms”, “hepatocellular carcinoma”, “liver tumor”, “cancer of liver”, “neoplasms of liver”, “survival, “survival analysis”, “survival rate”, “Afghanistan”, “Armenia” ,“Azerbaijan”, “Bahrain” “Bangladesh”, “Bhutan”, “Brunei”, “Myanmar”, “Cambodia”, “China” “Georgia”, “Hong Kong”, “India”, “Indonesia”, “Iran”, “Iraq”, “Israel”, “Japan”, “Jordan”, “Kazakhstan” “North Korea”, “South Korea”, “Kuwait”, “Kyrgyzstan”, “Laos”, “Lebanon”, “Macau”, “Malaysia” “Maldives”, “Mongolia”, “Nepal”, “Oman”, “Pakistan”, ”Philippines”, “Qatar”, “Saudi Arabia”, “Singapore”, “Sri Lanka”, “Syria”, “Taiwan”, “Tajikistan”, “Thailand”, “Timor-Leste”, “Turkmenistan”, “United Arab Emirates”, “Uzbekistan” , ”Vietnam”, and “Yemen”).
The initial search was conducted by two researchers (S.H and M.V). The searched record entered the EndNote X7 software, and duplicate articles were deleted. The search strategy of this study is presented in Supplementary Appendix 1.
Inclusion and exclusion criteria
All observational studies (cross-sectional, case-control, and cohort) stated the survival rate of Localize LC in Asian countries were included in the study. Articles of other cancers reported survival in people who reported regional, metastatic, as well as review and meta-analysis studies were excluded. It should be noted that studies that did not report the sample size or confidence interval of survival rate were not included into the meta-analysis.
Quality assessment
The Newcastle-Ottawa Quality Assessment Form was used to evaluate the quality of selected papers. This tool has 3 different parts including Selection (4 questions), Comparability (1 question) and Outcome (3 questions) and is based on the final scores divided into 3 categories Good (3 or 4 stars in selection domain and 1 or 2 stars in comparability domain and 2 or 3 stars in outcome/exposure domain), Fair (2 stars in selection domain and 1 or 2 stars in comparability domain and 2 or 3 stars in outcome/exposure domain) and Poor (0 or 1 star in selection domain or 0 stars in comparability domain or 0 or 1 stars in outcome/exposure domain) (Penson et al., 2012[89]). Result of quality assessment is presented in Suppplementary Appendix 2.
Screening of studies
Screening of studies, extraction of results, and evaluation of quality control of articles were performed separately undependably by two authors (M.V and E.A). If there was no agreement between the two, the supervisor (F.M) would announce the final comment on that article.
Data extraction form
All final articles entered into the study process were provided by a checklist that was previously prepared, and were arranged to extract the data. This checklist includes the name of the author, the year of publication, the period of the study, the country of origin, the survival rate by year for each survival period.
Statistical analysis
The heterogeneity of the studies was assessed by Cochran test (with significance less than 0.1) and its composition using I2 statistics. In the case of heterogeneity, the random effects model was utilized with the inverse-variance method, and in the absence of heterogeneity, the fixed effects model was applied. In the case of a heterogeneity in the studies, methods such as subgroup analysis were used and factors like the geographical area and the HDI considered in the analysis of subgroups. All analyzes were performed by the STATA (version 13) software.
Additional analysis
Due to the heterogeneity of the studies, the subgroups analysis was used. The indicator applied for this purpose is Human Development Indices and Indicators (HDI). The HDI is a relative measure of life expectancy, education, quality and education level, and in general, it is the living standards in human societies. This Index is estimated using the measure of welfare, especially among children and people of low age. These statistics can be used to measure the development of countries, the impact of economic policies on living standards, and the survival of LC in each of the countries was reported to provide a clear indication of the LC survival status in each country (Human Development Indices and Indicators, 2018[35]).
Results
Study selection
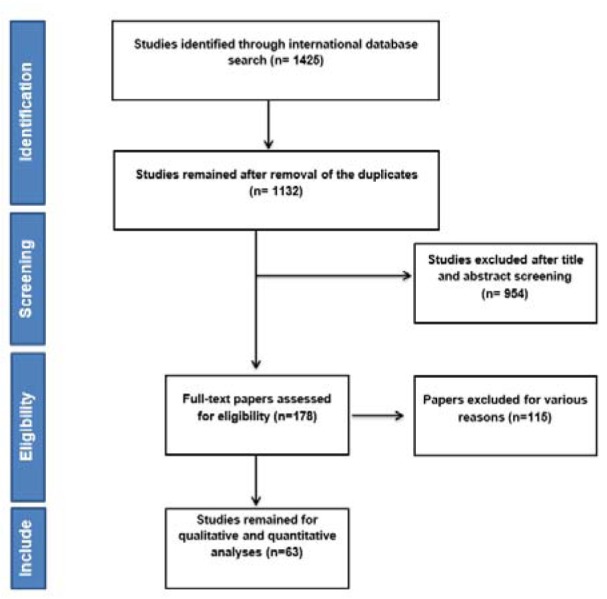
After searching the named international databases 1425 articles were selected and after removing duplicate articles 1132 remained. After reviewing the titles and abstract articles, the number of 178 articles entered the next stage, at which point the full text was examined and the 63 articles entered the final analysis. It should be noted that the referenced articles were also reviewed to add related studies. In the screening stages of studies, some articles were excluded for a variety of reasons, which included the unrelated topic (N=921), the unrelated population (N=133), inadequate information such as sample size, confidence interval and not reported overall survival in both sexes (N=12) and the repeated results (N=3). The study selection process is outlined in Figure 1(Fig. 1).
Figure 1. Flowchart of the included studies in systematic review.
Results of quality assessment
Based on our result, 30 studies had good quality and 33 studies had fair quality. The result of Quality Assessment is presented in Supplementary Appendix 1.
Description of studies
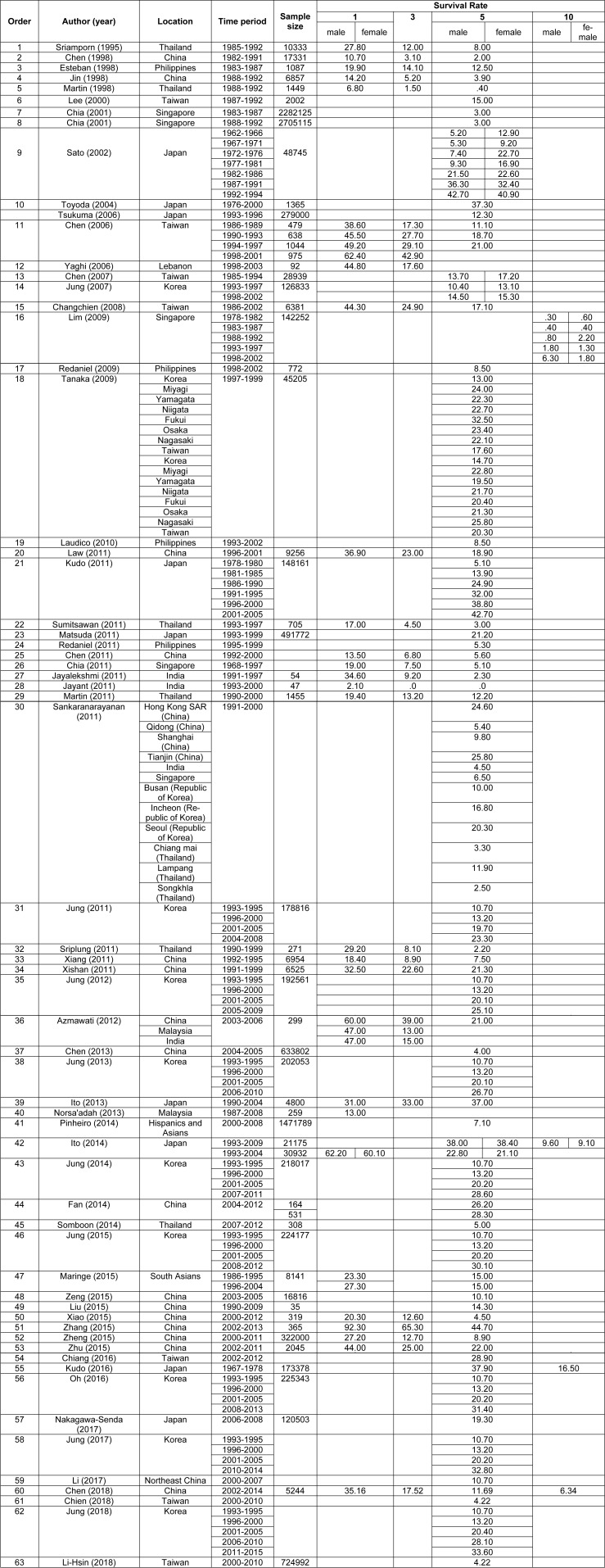
Based on the geographical location of 63 included studies (Sriamporn et al., 1995[99]; Chen et al., 1998[14]; Esteban et al., 1998[24]; Jin et al., 1998[43]; Martin et al., 1998[74]; Lee et al., 2000[64]; Chia et al., 2001[19]; Sato et al., 2002[95]; Toyoda et al., 2004[107]; Chen et al., 2006[12]; Tsukuma et al., 2006[108]; Yaghi et al., 2006[118]; Chen et al., 2007[16]; Jung et al., 2007[53]; Changchien et al., 2008[11]; Lim et al., 2009[68]; Redaniel et al., 2009[93]; Tanaka et al., 2009[104]; Laudico et al., 2010[62]; Chen et al., 2011[15]; Chia, 2011[18]; Jayalekshmi et al., 2011[40]; Jayant et al., 2011[41]; Jung et al., 2011[47]; Kudo et al., 2011[58]; Law and Mang, 2011[63]; Martin et al., 2011[73]; Matsuda et al., 2011[75]; Redaniel et al., 2011[92]; Sankaranarayanan, 2011[94]; Sriplung and Prechavittayakul, 2011[100]; Sumitsawan et al., 2011[101]; Xiang et al., 2011[114]; Xishan et al., 2011[116]; Azmawati and Krisnan, 2012[6]; Jung et al., 2012[48]; Chen et al., 2013[17]; Ito et al., 2013[37]; Jung et al., 2013[51]; Norsa'adah and Nurhazalini-Zayani, 2013[86]; Fan et al., 2014[26]; Ito et al., 2014[36]; Jung et al., 2014[46]; Pinheiro et al., 2014[90]; Somboon et al., 2014[98]; Jung et al., 2015[50]; Liu et al., 2015[69]; Maringe et al., 2015[72]; Xiao et al., 2015[115]; Zeng et al., 2015[124]; Zhang et al., 2015[126]; Zheng et al., 2015[129]; Zhu et al., 2015[131]; Chiang et al., 2016[20]; Kudo et al., 2016[59]; Oh et al., 2016[87]; Jung et al., 2017[52]; Li et al., 2017[66]; Nakagawa-Senda et al., 2017[82]; Chen et al., 2018[13]; Chien et al., 2018[21]; Jung et al., 2018[49]; Li-Hsin et al., 2018[67]), twenty-one studies were conducted in China, fourteen in Korea, nine in Japan, nine in Thailand, nine in Taiwan, four in Philippines, four in Singapore, four in India, two in Malaysia, one in Hong-Kong and one study in south Asian countries. The summary characteristics of the included studies were shown in Table 1(Tab. 1) (References in Table 1: Azmawati, 2012[6]; Changchien, 2008[11]; Chen, 1998[14]; Chen, 2006[12]; Chen, 2007[16]; Chen, 2011[15]; Chen, 2013[17]; Chen, 2018[13]; Chia, 2001[19]; Chia, 2011[18]; Chiang, 2016[20]; Chien, 2018[21]; Esteban, 1998[24]; Fan, 2014[26]; Ito, 2013[37]; Ito, 2014[36]; Jayalekshmi, 2011[40]; Jayant, 2011[41]; Jin, 1998[43]; Jung, 2007[53]; Jung, 2011[47]; Jung, 2012[48]; Jung, 2013[51]; Jung, 2014[46]; Jung, 2015[50]; Jung, 2017[52]; Jung, 2018[49]; Kudo, 2011[58]; Kudo, 2016[59]; Laudico, 2010[62]; Law, 2011[63]; Lee, 2000[64]; Li, 2017[66]; Li-Hsin, 2018[67]; Lim, 2009[68]; Liu, 2015[69]; Maringe, 2015[72]; Martin, 1998[74]; Martin, 2011[73]; Matsuda, 2011[75]; Nakagawa-Senda, 2017[82]; Norsa'adah, 2013[86]; Oh, 2016[87]; Pinheiro, 2014[90]; Redaniel, 2009[93]; Redaniel, 2011[92]; Sankaranarayanan, 2011[94]; Sato, 2002[95]; Somboon, 2014[98]; Sriamporn, 1995[99]; Sriplung, 2011[100]; Sumitsawan, 2011[101]; Tanaka, 2009[104]; Toyoda, 2004[107]; Tsukuma, 2006[108]; Xiang, 2011[114]; Xiao, 2015[115]; Xishan, 2011[116]; Yaghi, 2006[118]; Zeng, 2015[124]; Zhang, 2015[126]; Zheng, 2015[129]; Zhu, 2015[131]).
Table 1. Basic information of included studies.
Heterogeneity
The result of chi-squared test and the I2 index indicated that there was a considerable between-study heterogeneity. For one (I2= 99.8 %, P<0.001), three (I2= 99.8 %, P<0.001), five (I2= 99.9 %, P<0.001) and ten- year survival rate (I2= 99.6 %, P<0.001).
Synthesis of results
The articles were sorted according to the year of publication, and then analyzed by survival analysis of 1, 3, 5 and 10 years survival rate based on random effect model.
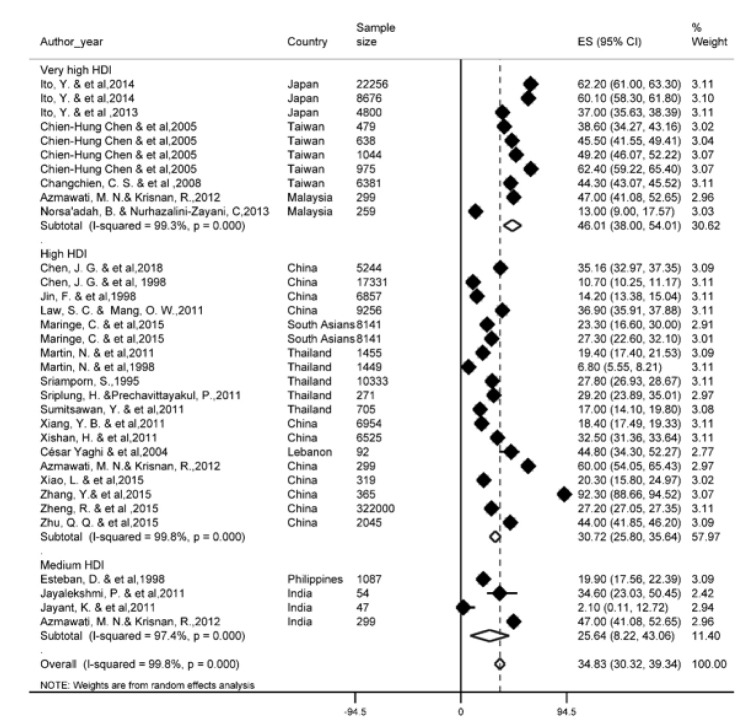
One-year survival rate
Of the most recent papers, 27 studies reported a one-year survival rate. The results of the study showed that one-year survival rate in Asian countries was 34.8 % (95 % CI; 30.3- 39.3). One-year survival rate of LC based on HDI has been shown in Figure 2(Fig. 2) (References in Figure 2: Azmawati, 2012[6]; Changchien, 2008[11]; Chen, 1998[14]; Chen, 2018[13]; Esteban, 1998[24]; Ito, 2013[37]; Ito, 2014[36]; Jayalekshmi, 2011[40]; Jayant, 2011[41]; Jin, 1998[43]; Law, 2011[63]; Maringe, 2015[72]; Martin, 1998[74]; Martin, 2011[73]; Norsa'adah, 2013[86]; Sriamporn, 1995[99]; Sriplung, 2011[100]; Sumitsawan, 2011[101]; Xiang, 2011[114]; Xiao, 2015[115]; Xishan, 2011[116]; Zhang, 2015[126]; Zheng, 2015[129]; Zhu, 2015[131]). Regarding the results, the highest one-year survival rate in countries with a very high HDI level (46 %, 95 % CI; 38-54) and the lowest was observed among countries with medium HDI level (25.6 %, 95 % CI; 8.2-43.6).
Figure 2. Forest plot of one-year survival rate of liver cancer in Asian countries.
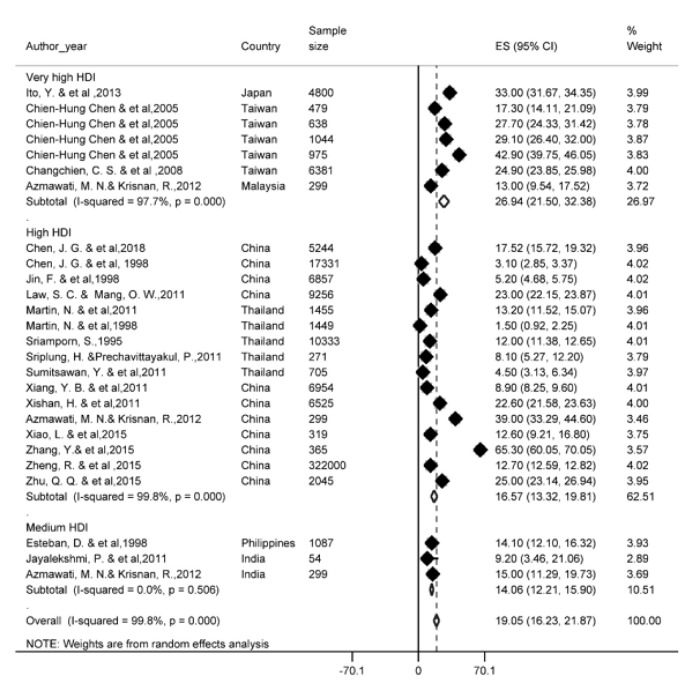
Three-year survival rate
There were 22 studies that reported 3-year survival rate. Based on the results of our study, the 3-year survival rate in Asian countries was 19 %, (95 % CI; 16.2-21.8). The three-year survival rate of LC based on HDI is presented in Figure 3(Fig. 3) (References in Figure 3: Azmawati, 2012[6]; Changchien, 2008[11]; Chen, 1998[14]; Chen, 2018[13]; Esteban, 1998[24]; Ito, 2013[37]; Jayalekshmi, 2011[40]; Jin, 1998[43]; Law, 2011[63]; Martin, 1998[74]; Martin, 2011[73]; Sriamporn, 1995[99]; Sriplung, 2011[100]; Sumitsawan, 2011[101]; Xiang, 2011[114]; Xiao, 2015[115]; Xishan, 2011[116]; Zhang, 2015[126]; Zheng, 2015[129]; Zhu, 2015[131]). According to the results, the highest three-year survival rate for countries with a high HDI level (26.9 %, 95 % CI; 32.3-21.5) and the lowest for countries with the medium HDI levels was 14 % (95 % CI; 18.2-12.29).
Figure 3. Forest plot of three-year survival rate of liver cancer in Asian countries.
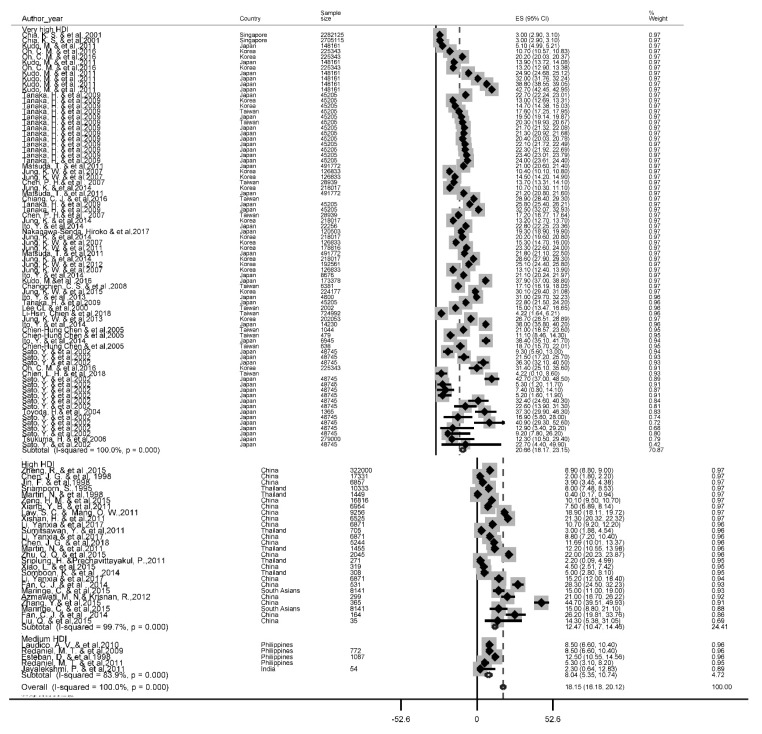
Five-year survival rate
A total of 56 studies reported this survival rate. The 5 years rate of LC was 18.1 % (95 % CI, 16.2-20.1). The results of the 5-year survival by the HDI is depicted in Figure 4(Fig. 4) (References in Figure 4: Azmawati, 2012[6]; Changchien, 2008[11]; Chen, 1998[14]; Chen, 2007[16]; Chen, 2018[13]; Chia, 2001[18]; Chiang, 2016[20]; Chien, 2018[21]; Esteban, 1998[24]; Fan, 2014[26]; Ito, 2013[37]; Ito, 2014[36]; Jayalekshmi, 2011[40]; Jin, 1998[43]; Jung, 2007[53]; Jung, 2011[47]; Jung, 2012[48]; Jung, 2013[51]; Jung, 2014[46]; Jung, 2015[50]; Kudo, 2011[58]; Laudico, 2010[62]; Law, 2011[63]; Lee, 2000[64]; Li, 2017[66]; Li-Hsin, 2018[67]; Liu, 2015[69]; Maringe, 2015[72]; Martin, 1998[74]; Matsuda, 2011[75]; Nakagawa-Senda, 2017[82]; Oh, 2016[87]; Redaniel, 2009[93]; Redaniel, 2011[92]; Sato, 2002[95]; Somboon, 2014[98]; Sriamporn, 1995[99]; Sriplung, 2011[100]; Sumitsawan, 2011[101]; Tanaka, 2009[104]; Toyoda, 2004[107]; Tsukuma, 2006[108]; Xiang, 2011[114]; Xiao, 2015[115]; Xishan, 2011[116]; Zeng, 2015[124]; Zhang, 2015[126]; Zheng, 2015[129]; Zhu, 2015[131]). Based on the findings of our study, the highest five-year survival rate for countries with very high HDI levels (20.7 %, 95 % CI; 18.2-23.2) and the lowest was for the countries with the medium HDI level 8 %, 95 % CI; 5.3-10.7).
Figure 4. Forest plot of five-year survival rate of liver cancer in Asian countries.
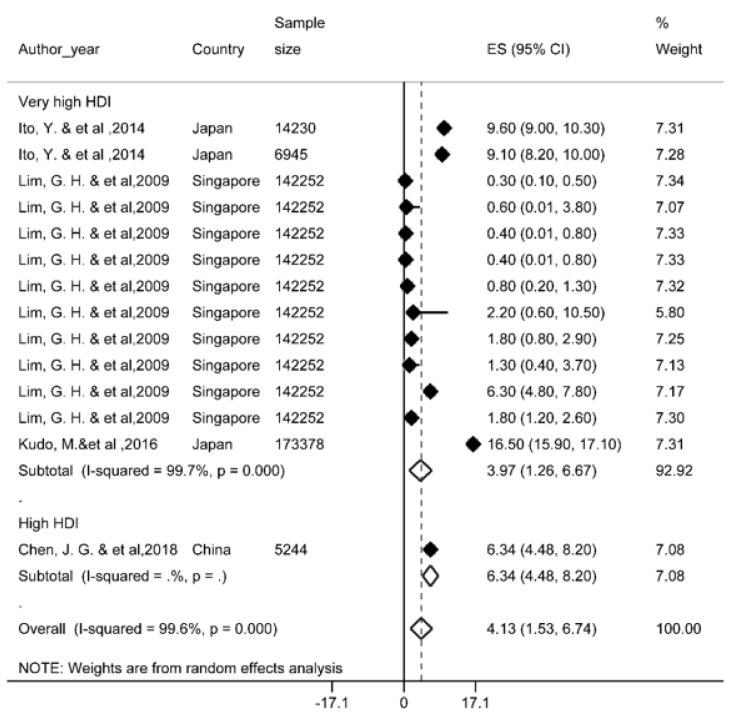
Ten-year survival rate
Four studies reported this survival rate and based on the results, the ten-year survival rate was 4.1 % (95 % CI; 1.5-6.7). Ten-year survival of LC by HDI has been shown in Figure 5(Fig. 5) (References in Figure 5: Ito, 2014[36]; Lim, 2009[68]; Kudo, 2016[59]; Chen, 2018[13]). Given the limited number of studies conducted for 10-year survival rate, data on countries with medium HDI levels was not available.
Figure 5. Forest plot of ten-year survival rate of liver cancer in Asian countries.
Analysis of Subgroups
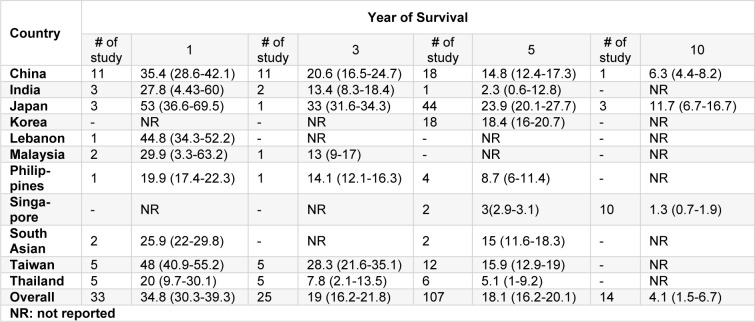
Survival rate of liver cancer in each country
Overall, the results of the survival of the LC in ten countries and another region has been reported in Table 2(Tab. 2). The highest survival rates of one, three, five, and ten years were reported in Japan and the lowest survival rates for these years were observed in countries such as the Philippines, Thailand, India and Singapore.
Table 2. Result of meta-analysis of survival rate of liver cancer in Asia based on each country and year of survival.
Meta-regression
Results of meta-regression showed a significant association between publication year and survival rate. Thus, year of study is a cause of variability in results of one (Reg Coef= 0.041, p=0.002), three (Reg Coef= 0.049, p=0.017) and five year survival rate (Reg Coef= 0.036, p<0.001). According to results, an increasing survival rate across the study period was observed. Results of meta-regression has been shown in Supplementary Appendix 3.
Discussion
LC is the sixth most common cancer and the fourth cause of death worldwide in 2018, with 841,000 new cases and 782,000 deaths annually (Bray et al., 2018[9]). The incidence and mortality of men are two to three times higher than women in most parts of the world (Altekruse et al., 2014[3]).
The results of our study showed that one, three, five and ten-year survival rate of LC in Asian countries was 34.8 %, 19 %, 18.1 %, and 4.1 % respectively. Significant heterogeneity was seen in the between studies. The present study was conducted in identifying high-risk individuals, diagnosis and early treatment of LC. The most important treatment for hepatocellular carcinoma is hepatic resection, trans-arterial embolization, percutaneous ethanol injection therapy, regional chemotherapy, and liver transplantation (Takano et al., 2000[102]; Fakhar et al., 2016[25]; Zhao et al., 2019[127]). For instance, 84.5 % of patients in Pakistan (Yusuf et al., 2007[121]) did not receive any treatment interventions, which was 30.5 % in China (Zhou et al., 2000[130]). Mortality rate for all cancers are 50 % more common in men than in women. Mortality rate in men were 171 per 100,000 in East Africa to 67.4 in Central America, ranging from 7.1 in Melanesia to 2.6 in Central and East Asia (except China) (Ghoncheh and Salehiniya, 2016[30]). The cumulative mortality risk from cancer among women in East Africa (11.4 %) in 2018 was higher than the estimated risk in North Africa (8.6 %), Northern Europe (9.1 %), and Australia / New Zealand (1.8 %) (Allemani et al., 2018[2]; Bray et al., 2018[9]). In one study which is conducted on localized staged patients treated with invasive methods, blacks have a 12 percent higher mortality rate, while Asian or Pacific islanders have a 16 percent lower mortality rate compared to whites (Wong and Corley, 2009[112]).
The statistics show that about half of the cases of death from primary LC occurred in China (Zheng et al., 2018[128]). The variety of survival rates in Asian countries includes the range of medical and pharmaceutical care and coverage of insurance services, socioeconomic status, ethnicity and lifestyle (Williams et al., 2010[111]). Medical advances have been made in detecting small tumors with a variety of scanning techniques (Takayasu et al., 1995[103]).
In our analysis, the one-year survival rate in Asian countries was 34.8 %. The one-year survival rate is related to factors such as age older than 50 years, CLIP score <3, ALP <120 U/l, LDH <450 IU/l, CRP <0.8 mg/dl, tumor size less than 6 cm, disease stage, and Child-Pugh less than 7 that is associated with increased mortality (Toyoda et al., 2004[107]; Georgiades et al., 2006[29]; Jun et al., 2013[45]; Agarwal et al., 2015[1]). A meta-analysis study concluded that Transarterial chemoembolization (TACE) in patients with portal vein thrombosis significantly increased the 6 months survival rate (Xue et al., 2013[117]). However, haptoglobin (Hp) serum could be a potential and alternative contributor to alpha-fetoprotein. Contradiction in predicting one year rate in various geographic regions can be due to the selecting patients with demographic and clinical characteristics, diagnostic criteria, severity of the cirrhosis, number and size of the tumor (Shu et al., 2010[97]; Moayedi et al., 2019[79]). Despite the limited number of HCTs available for HCC, one-year survival rates for HCC have almost doubled over the period of 1992-1993 to 2003-2004 in the United States (Altekruse et al., 2009[4]). Of course, this increase in survival is limited to short-term follow-up. In addition, with aggressive treatments including liver transplantation and resection for localized-stage tumors, they are effective in boosting survival rates (Schwarz and Smith, 2008[96]). It is also associated with the expansion of public health and oncology care (Bai et al., 2018[7]).
Based on the results, the five-year survival rate was 18.1 %. The 5-year survival rate of all cancers in Korea in each sex, reached to 7.70 % (2011-2015) from 2.41 % (1995-1993) (Jung et al., 2018[49]). Besides, the five-year survival rate of LC in Shanghai in 1990 was 0.9 percent, reaching 0.1 percent in the last decade (Xiang et al., 2011[114]; Han et al., 2012[32]). Uninodular tumors and non-vascular invasion were associated with a 5-year survival (Jeong et al., 2017[42]). Liver transplant increases 5-year survival to 75 %, which is the best treatment option (Zamora-Valdes et al., 2017[123]). A meta-analysis study of 19 researches illustrated that the median survival rate for 436 patients with liver resection for hepatocyte metastasis to gastric was 17 months and a 5-year survival of 26.5 % (Kerkar et al., 2010[54]). An overall improvement in community health and the use of anti-viral therapies is effective in extending patient survival. Liver transplantation is an appropriate option (Omata et al., 2010[88]; Zhu et al., 2015[131]). However, the high cost of transplantation and the low number of donors of liver transplantation in most cases make it impractical (Llovet et al., 2005[70]). Resection surgery is recommended as a treatment for BCLC (Barcelona Clinic Liver Cancer) in very early and primary phases without portal hypertension and abnormal bilirubin. However, resection surgery is now the first line of therapy and leads to better patient survival (Dimitroulis et al., 2017[22]).
The gender variable is an independent predictor in the prognostic primary liver cancer (PLC), regardless of the death of the PLC and all causes of death (Chen et al., 2007[16]). However, in other studies, the gender variable was not a predictor of survival due to PLC (Tangkijvanich et al., 2004[105]; Jarnagin et al., 2009[39]). Previous studies have shown that women have a higher rate of survival after surgery. Differences in aspects of medical interventions are attributed to gender disparity in survival rates (Wu et al., 2018[113]). The high alcohol intake in men increases cirrhosis of the liver towards the PLC (Nordenstedt et al., 2010[85]; Kröner et al., 2015[57]).
Analysis of subgroups based on the geographic region show that, the highest survival rates of one, three, five, and ten years are reported in Japan and the lowest survival rates for these years were observed in the Philippines, Thailand, India and Singapore, respectively. The only areas with a high prevalence rate in the past include Japan, Korea and China, which have witnessed a sharp decline in outbreaks in recent years (Bertuccio et al., 2017[8]).
According to the latest global release, the highest incidence has taken place in lower HDI settings, and LC in 13 countries was one of the most common malignancies, including several countries in North and West Africa (Egypt, Gambia, Guinea) and the East and South East Asia (Mongolia, Cambodia and Vietnam) (Hashim et al., 2016[33]). Also, over the most recent years, the mortality rate of HCC is 2 to 5 times higher in Japan, Hong Kong and Korea than in European and American countries (McGlynn and London, 2011[76]; Zhu et al., 2016[132]). In the case of China, the proportion of Child A was less prevalent, while this proportion was more prevalent in the case of the Italian Child B type (Pons et al., 2005[91]; Azmawati and Krisnan, 2012[6]; Kew, 2014[55]). In addition, Asians have lower survival rates than non-Asians (Chang et al., 2007[10]). Advances have been made in HCC management and treatment, through local ablation, hepatic resection and liver transplantation. The impact of such improvements on HCC mortality was limited, as its 5-year survival rate was about 10 % (Lepage et al., 2015[65]). The five-year survival rate of the cancer in the US rose from 3 % over the 1975-1977 period to 11 % in the period of 2001-2007. While this survival rate ranged from 10.7 % in 1975-1977 to 18.9 % in the period 2001-2005. Approximately 62 % of HCC patients in Japan have undergone resection or ablation as primary care (Korean Liver Cancer Study Group and National Cancer Center Korea, 2015[56]). By comparing these proportions, only 30 % of these patients in the Western countries by the initial diagnosis were under these treatment interventions. Perhaps the care of high-risk patients will cause early detection and early diagnosis in countries such as Japan and Korea (El-Serag and Davila, 2011[23]).
Study limitations
There are certain limitations in systematic review studies, most notably in the absence of access to some of the information that attempts were made to contact the authors of the study to resolve the problem, which in several cases did not receive an adequate response. One of the main limitation in our study was the failure to report sample size and the inability to calculate the confidence interval for survival, which did not allow the study to include the meta-analysis stage. Other limitations included a survival report of less than one year (6 and 9 months), which, given the low level of these, had no significant effect on our results. Ultimately, due to the lack of studies reporting 10-year survival, the correct estimate of survival requires more robust studies.
Recommendations for future research
According to the results of this study, estimating the survival rate of LC requires more extensive studies at the level of other Asian countries, especially in the West and Central Asia, as most studies in this study were conducted in South and Southeast of Asia, and estimates are somewhat incorrect. Another suggestion could be a study of the survival of LC in patients who metastasized, which was not our study goal, and is an important issue in clinical decision-making and the continuation of treatment.
Conclusion
According to the results of our study, the LC survival rate in Asian countries is relatively lower than in Europe and North America, which may be due to less access to diagnostic facilities and higher age at recognition of disease than to advanced countries. Another result of our study was the higher survival rate of LC in countries with very high HDI (such as South Korea and Japan), with similar survival rates within advanced countries such as Europe and North America.
Author contributions
Conceived and designed the experiments: S.H and F.M
Collected the data: M.V, H.N and E.A
Analyzed the data: S.H, F.J, M.A and H.S.
Wrote the paper: S.G, H.N, A.P and A.S.
Revised the paper: S.H, F.M and F.J.
Funding
This study was supported financially by Guilan University of Medical Sciences, Rasht, Iran.
Conflict of interests
The authors have no conflict of interest to disclose.
Supplementary Material
References
- 1.Agarwal A, Yadav AK, Kumar A, Gupta S, Panwala HK, Redhu N, et al. Transarterial chemoembolization in unresectable hepatocellular carcinoma--assessing the factors affecting the survival: An audit from a tertiary care center in northern india. Indian J Gastroenterol. 2015;34:117–126. doi: 10.1007/s12664-015-0544-9. [DOI] [PubMed] [Google Scholar]
- 2.Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, et al. Global surveillance of trends in cancer survival 2000-14 (concord-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altekruse SF, Henley SJ, Cucinelli JE, McGlynn KA. Changing hepatocellular carcinoma incidence and liver cancer mortality rates in the united states. Am J Gastroenterol. 2014;109:542–553. doi: 10.1038/ajg.2014.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the united states from 1975 to 2005. J Clin Oncol. 2009;27:1485–1491. doi: 10.1200/JCO.2008.20.7753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aniaku JK, Amedonu EK, Fusheini A. Assessment of knowledge, attitude and vaccination status of hepatitis b among nursing training students in ho, ghana. Ann Global Health. 2019;85(1) doi: 10.5334/aogh.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Azmawati M, Krisnan R. Roles of ethnicity in survival of hepatocellular carcinoma patients in malaysia. Asian Pac J Cancer Prev. 2012;13:6023–6026. doi: 10.7314/apjcp.2012.13.12.6023. [DOI] [PubMed] [Google Scholar]
- 7.Bai L, Liu Z, Fang Q, Yan Q, Shi O, Bao P, et al. The trends and projections in the incidence and mortality of liver cancer in urban shanghai: A population-based study from 1973 to 2020. Clin Epidemiol. 2018;10:277–288. doi: 10.2147/CLEP.S153951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bertuccio P, Turati F, Carioli G, Rodriguez T, La Vecchia C, Malvezzi M, et al. Global trends and predictions in hepatocellular carcinoma mortality. J Hepatol. 2017;67:302–309. doi: 10.1016/j.jhep.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 9.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 10.Chang ET, Keegan THM, Gomez SL, Le GM, Clarke CA, So SKS, et al. The burden of liver cancer in asians and pacific islanders in the greater san francisco bay area, 1990 through 2004. Cancer. 2007;109:2100–2108. doi: 10.1002/cncr.22642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Changchien CS, Chen CL, Yen YH, Wang JH, Hu TH, Lee CM, et al. Analysis of 6381 hepatocellular carcinoma patients in southern taiwan: Prognostic features, treatment outcome, and survival. J Gastroenterol. 2008;43:159–170. doi: 10.1007/s00535-007-2134-9. [DOI] [PubMed] [Google Scholar]
- 12.Chen CH, Su WW, Yang SS, Chang TT, Cheng KS, Lin HHH, et al. Long-term trends and geographic variations in the survival of patients with hepatocellular carcinoma: Analysis of 11 312 patients in taiwan. J Gastroenterol Hepatol. 2006;21:1561–1566. doi: 10.1111/j.1440-1746.2006.04425.x. [DOI] [PubMed] [Google Scholar]
- 13.Chen JG, Chen HZ, Zhu J, Yang YL, Zhang YH, Huang PX, et al. Cancer survival in patients from a hospital-based cancer registry, china. J Cancer. 2018;9:851–860. doi: 10.7150/jca.23039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen JG, Li WG, Shen ZC, Yao HY, Zhang BC, Zhu YR. Population-based cancer survival in qidong, people's republic of china. IARC Sci Publ. 1998;145:27–35. [PubMed] [Google Scholar]
- 15.Chen JG, Zhu J, Zhang YH, Lu JH. Cancer survival in qidong, china, 1992-2000. IARC Sci Publ. 2011;162:43–53. [PubMed] [Google Scholar]
- 16.Chen PH, Lin YC, Tu HP, Chiang SL, Ko AM, Hsu CL, et al. Important prognostic factors for the long-term survival of subjects with primary liver cancer in taiwan: A hyperendemic area. Eur J Cancer. 2007;43:1076–1084. doi: 10.1016/j.ejca.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 17.Chen W, Armstrong BK, Rahman B, Zheng R, Zhang S, Clements M. Relationship between cancer survival and ambient ultraviolet b irradiance in china. Cancer Causes Control. 2013;24:1323–1330. doi: 10.1007/s10552-013-0210-4. [DOI] [PubMed] [Google Scholar]
- 18.Chia KS. Cancer survival in Singapore, 1993-1997. IARC Sci Publ. 2011;162:183–198. [PubMed] [Google Scholar]
- 19.Chia KS, Du WB, Sankaranarayanan R, Sankila R, Seow A, Lee HP. Population-based cancer survival in singapore, 1968 to 1992: An overview. Int J Cancer. 2001;93:142–147. doi: 10.1002/ijc.1293. [DOI] [PubMed] [Google Scholar]
- 20.Chiang CJ, Lo WC, Yang YW, You SL, Chen CJ, Lai MS. Incidence and survival of adult cancer patients in taiwan, 2002-2012. J Formosan Med Assoc. 2016;115:1076–1088. doi: 10.1016/j.jfma.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 21.Chien LH, Tseng TJ, Tsai FY, Wang JH, Hsiung CA, Liu TW, et al. Patterns of age-specific socioeconomic inequalities in net survival for common cancers in taiwan, a country with universal health coverage. Cancer Epidemiol. 2018;53:42–48. doi: 10.1016/j.canep.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 22.Dimitroulis D, Damaskos C, Valsami S, Davakis S, Garmpis N, Spartalis E, et al. From diagnosis to treatment of hepatocellular carcinoma: An epidemic problem for both developed and developing world. World J Gastroenterol. 2017;23:5282–5294. doi: 10.3748/wjg.v23.i29.5282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.El-Serag HB, Davila JA. Surveillance for hepatocellular carcinoma: In whom and how? Therap Adv Gastroenterol. 2011;4:5–10. doi: 10.1177/1756283X10385964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Esteban D, Ngelangel C, Lacaya L, Robles E, Monson M. Cancer survival in rizal, philippines. IARC Sci Publ. 1998;145:101–108. [PubMed] [Google Scholar]
- 25.Fakhar N, Nikeghbalian S, Kazemi K, Shamsayeefar AR, Gholami S, Kasraianfard A, et al. Transplantation of deceased donor livers with elevated levels of serum transaminases at shiraz transplant center. Hepat Mon. 2016;16(10):e40140. doi: 10.5812/hepatmon.40140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fan CJ, Jin GX, Sun C, Ma DL, Chen CY, Qiao PF, et al. Clinical characteristics, treatment patterns and survival outcome of hepatocellular carcinoma patients aged 70 years or older: A single-center retrospective study from china. Aging Clin Exp Res. 2014;26:123–130. doi: 10.1007/s40520-013-0142-6. [DOI] [PubMed] [Google Scholar]
- 27.Fernandez E, La Vecchia C, D'Avanzo B, Negri E, Franceschi S. Family history and the risk of liver, gallbladder, and pancreatic cancer. Cancer Epidemiol Biomarkers Prev. 1994;3:209–212. [PubMed] [Google Scholar]
- 28.Gao J, Xie L, Yang WS, Zhang W, Gao S, Wang J, et al. Risk factors of hepatocellular carcinoma--current status and perspectives. Asian Pac J Cancer Prev. 2012;13:743–752. doi: 10.7314/apjcp.2012.13.3.743. [DOI] [PubMed] [Google Scholar]
- 29.Georgiades CS, Liapi E, Frangakis C, Park JU, Kim HW, Hong K, et al. Prognostic accuracy of 12 liver staging systems in patients with unresectable hepatocellular carcinoma treated with transarterial chemoembolization. J Vasc Interv Radiol. 2006;17:1619–1624. doi: 10.1097/01.RVI.0000236608.91960.34. [DOI] [PubMed] [Google Scholar]
- 30.Ghoncheh M, Salehiniya H. Inequality in the incidence and mortality of all cancers in the world. Iran J Public Health. 2016;45:1675–1677. [PMC free article] [PubMed] [Google Scholar]
- 31.Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: A systematic analysis for the global burden of disease study. JAMA Oncol. 2017;3:524–528. doi: 10.1001/jamaoncol.2016.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Han X, Huang CX, Zhang HW, Qiao P, Xie M, Zhang R, et al. [The occurrence and survival condition of primary liver cancer among residents in yangpu district of shanghai between year 2002 and 2010]. Zhonghua Yu Fang Yi Xue Za Zhi. 2012;46:119–124. (Ger). [PubMed] [Google Scholar]
- 33.Hashim D, Boffetta P, La Vecchia C, Rota M, Bertuccio P, Malvezzi M, et al. The global decrease in cancer mortality: Trends and disparities. Ann Oncol. 2016;27:926–933. doi: 10.1093/annonc/mdw027. [DOI] [PubMed] [Google Scholar]
- 34.Hassanipour S, Mohammadzadeh M, Mansour-Ghanaei F, Fathalipour M, Joukar F, Salehiniya H, et al. The incidence of hepatocellular carcinoma in iran from 1996 to 2016: A systematic review and meta-analysis. J Gastrointest Cancer. 2019;50:193–200. doi: 10.1007/s12029-019-00207-y. [DOI] [PubMed] [Google Scholar]
- 35.Human Development Indices and Indicators. 2018. Available from: http://hdr.undp.org/sites/default/files/2018_human_development_statistical_update.pdf.
- 36.Ito Y, Nakaya T, Nakayama T, Miyashiro I, Ioka A, Tsukuma H, et al. Socioeconomic inequalities in cancer survival: A population-based study of adult patients diagnosed in Osaka, Japan, during the period 1993-2004. Acta Oncol. 2014;53:1423–1433. doi: 10.3109/0284186X.2014.912350. [DOI] [PubMed] [Google Scholar]
- 37.Ito Y, Nakayama T, Miyashiro I, Ioka A, Tsukuma H. Conditional survival for longer-term survivors from 2000-2004 using population-based cancer registry data in osaka, Japan. BMC Cancer. 2013;13:304. doi: 10.1186/1471-2407-13-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jakupi X, Lunar MM, Mlakar J, Matković I, Tavakoli NP, Ivanovska BZ, et al. Hcv infection among injecting drug users in Prishtina, Kosovo. Hepat Mon. 2018;18 [Google Scholar]
- 39.Jarnagin WR, Schwartz LH, Gultekin DH, Gönen M, Haviland D, Shia J, et al. Regional chemotherapy for unresectable primary liver cancer: Results of a phase ii clinical trial and assessment of dce-mri as a biomarker of survival. Ann Oncol. 2009;20:1589–1595. doi: 10.1093/annonc/mdp029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jayalekshmi P, Gangadharan P, Sebastian P. Cancer survival in Karunagappally, India, 1991-1997. IARC Sci Publ. 2011;162:125–132. [PubMed] [Google Scholar]
- 41.Jayant K, Nene BM, Dinshaw KA, Badwe RA, Panse NS, Thorat RV. Cancer survival in Barshi, India, 1993-2000. IARC Sci Publ. 2011;162:101–106. [PubMed] [Google Scholar]
- 42.Jeong SO, Kim EB, Jeong SW, Jang JY, Lee SH, Kim SG, et al. Predictive factors for complete response and recurrence after transarterial chemoembolization in hepatocellular carcinoma. Gut Liver. 2017;11:409–416. doi: 10.5009/gnl16001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jin F, Xiang YB, Gao YT. Cancer survival in Shanghai, People's Republic of China. IARC Sci Publ. 1998;145:37–50. [PubMed] [Google Scholar]
- 44.Joukar F, Mansour-Ghanaei F, Naghipour MR, Hassanipour S. Knowledge, distribution and risk factors of hepatitis b and c infection in high-risk groups in Guilan province, Iran. Hepat Mon. 2018;18 [Google Scholar]
- 45.Jun CH, Sim DW, Kim SH, Hong HJ, Chung MW, Myoung E, et al. Predictive factors for recurrence and survival in hepatocellular carcinoma in South Korea. Anticancer Res. 2013;33:4129–4134. [PubMed] [Google Scholar]
- 46.Jung K, Won Y, Kong H, Oh C, Lee DH, Lee JS. Cancer statistics in Korea: Incidence, mortality, survival and prevalence in 2011. Cancer Res Treat. 2014;46:109–123. doi: 10.4143/crt.2014.46.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Park EC, et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011;43:1–11. doi: 10.4143/crt.2011.43.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Seo HG, et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat. 2012;44:11–24. doi: 10.4143/crt.2012.44.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jung KW, Won YJ, Kong HJ, Lee ES, Kim CH, Yoo CI, et al. Cancer statistics in Korea: Incidence, mortality, survival,and prevalence in 2015. Cancer Res Treat. 2018;50:303–316. doi: 10.4143/crt.2018.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015;47:127–141. doi: 10.4143/crt.2015.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics inKkorea: Incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013;45:1–14. doi: 10.4143/crt.2013.45.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jung KW, Won YJ, Oh CM, Kong HJ, Lee DH, Lee KH, et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2014. Cancer Res Treat. 2017;49:292–305. doi: 10.4143/crt.2017.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jung K-W, Yim S-H, Kong H-J, Hwang S-Y, Won Y-J, Lee J-K, et al. Cancer survival in Korea 1993-2002: A population-based study. J Korean Med Sci. 2007;22:S5–S10. doi: 10.3346/jkms.2007.22.S.S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kerkar SP, Kemp CD, Avital I. Liver resections in metastatic gastric cancer. HPB (Oxford) 2010;12:589–596. doi: 10.1111/j.1477-2574.2010.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kew MC. Hepatocellular carcinoma: Epidemiology and risk factors. J Hepatocell Carcinoma. 2014;1:115–125. doi: 10.2147/JHC.S44381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Korean Liver Cancer Study Group (KLCSG), National Cancer Center Korea (NCC) 2014 Korean Liver Cancer Study Group, National Cancer Center Korea practice guideline for the management of hepatocellular carcinoma. Korean J Radiol. 2015;16:465–522. doi: 10.3348/kjr.2015.16.3.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kröner PT, Mankal PK, Dalapathi V, Shroff K, Abed J, Kotler DP. Alcohol-attributable fraction in liver disease: Does gdp per capita matter? Ann Global Health. 2015;81:711–717. doi: 10.1016/j.aogh.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 58.Kudo M, Izumi N, Kokudo N, Sakamoto M, Matsuyama Y, Ichida T, et al. Improved survival in patients with hepatocellular carcinoma over 30 years in Japan: Analysis of nationwide prospective registry of 148,161 patients. J Clin Oncol. 2011;29 [Google Scholar]
- 59.Kudo M, Izumi N, Sakamoto M, Matsuyama Y, Ichida T, Nakashima O, et al. Survival analysis over 28 years of 173,378 patients with hepatocellular carcinoma in japan. Liver Cancer. 2016;5:190–197. doi: 10.1159/000367775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.La Vecchia C, Lucchini F, Franceschi S, Negri E, Levi F. Trends in mortality from primary liver cancer in Europe. Eur J Cancer. 2000;36:909–915. doi: 10.1016/s0959-8049(00)00052-6. [DOI] [PubMed] [Google Scholar]
- 61.Ladep NG, Lesi OA, Mark P, Lemoine M, Onyekwere C, Afihene M, et al. Problem of hepatocellular carcinoma in West Africa. World J Hepatol. 2014;6:783–792. doi: 10.4254/wjh.v6.i11.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Laudico AV, Mirasol-Lumague MR, Mapua CA, Uy GB, Toral JAB, Medina VM, et al. Cancer incidence and survival in Metro Manila and Rizal province, Philippines. Jpn J Clin Oncol. 2010;40:603–612. doi: 10.1093/jjco/hyq034. [DOI] [PubMed] [Google Scholar]
- 63.Law SC, Mang OW. Cancer survival in Hong Kong SAR, China, 1996-2001. IARC Sci Publ. 2011;162:33–41. [PubMed] [Google Scholar]
- 64.Lee CL, Ko YC, Choong CS. Survival rate for liver cancer in Taiwan. Chin Med J (Taipei) 2000;63:16–20. [PubMed] [Google Scholar]
- 65.Lepage C, Capocaccia R, Hackl M, Lemmens V, Molina E, Pierannunzio D, et al. Survival in patients with primary liver cancer, gallbladder and extrahepatic biliary tract cancer and pancreatic cancer in Europe 1999-2007: Results of Eurocare-5. Eur J Cancer. 2015;51:2169–2178. doi: 10.1016/j.ejca.2015.07.034. [DOI] [PubMed] [Google Scholar]
- 66.Li Y, Yu L, Na J, Li S, Liu L, Mu H, et al. Survival of cancer patients in Northeast China: Analysis of sampled cancers from population-based cancer registries. Cancer Res Treat. 2017;49:1106–1113. doi: 10.4143/crt.2016.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li-Hsin C, Tseng T-J, Fang-Yu T, Wang J-H, Hsiung CA, Tsang-Wu L, et al. Patterns of age-specific socioeconomic inequalities in net survival for common cancers in Taiwan, a country with universal health coverage. Cancer Epidemiol. 2018;53:42–48. doi: 10.1016/j.canep.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 68.Lim GH, Wong CS, Chow KY, Bhalla V, Chia KS. Trends in long-term cancer survival in Singapore: 1968-2002. Ann Acad Med Singapore. 2009;38:99–105. [PubMed] [Google Scholar]
- 69.Liu Q, Bi JJ, Tian YT, Feng Q, Zheng ZX, Wang Z. Outcome after simultaneous resection of gastric primary tumour and synchronous liver metastases: Survival analysis of a single-center experience in China. Asian Pac J Cancer Prev. 2015;16:1665–1669. doi: 10.7314/apjcp.2015.16.4.1665. [DOI] [PubMed] [Google Scholar]
- 70.Llovet JM, Schwartz M, Mazzaferro V. Resection and liver transplantation for hepatocellular carcinoma. Semin Liver Dis. 2005;25:181–200. doi: 10.1055/s-2005-871198. [DOI] [PubMed] [Google Scholar]
- 71.Mansour-Ghanaei F, Fallah M-S, Jafarshad R, Joukar F, Salari A, Tavafzadeh R. Prevalence of hepatitis b surface antigen and hepatitis c virus antibody and their risk factors among Guilan’s volunteer blood donors (1998-2003) Hepat Mon. 2007;7:239–241. [Google Scholar]
- 72.Maringe C, Li R, Mangtani P, Coleman MP, Rachet B. Cancer survival differences between South Asians and non-South Asians of England in 1986-2004, accounting for age at diagnosis and deprivation. Brit J Cancer. 2015;113:173–181. doi: 10.1038/bjc.2015.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Martin N, Pongnikorn S, Patel N, Daoprasert K. Cancer survival in Lampang, Thailand, 1990-2000. IARC Sci Publ. 2011;162:217–226. [PubMed] [Google Scholar]
- 74.Martin N, Srisukho S, Kunpradist O, Suttajit M. Cancer survival in Chiang Mai, Thailand. IARC Sci Publ. 1998;145:109–121. [PubMed] [Google Scholar]
- 75.Matsuda T, Ajiki W, Marugame T, Ioka A, Tsukuma H, Sobue T, et al. Population-based survival of cancer patients diagnosed between 1993 and 1999 in Japan: A chronological and international comparative study. Jpn J Clin Oncol. 2011;41:40–51. doi: 10.1093/jjco/hyq167. [DOI] [PubMed] [Google Scholar]
- 76.McGlynn KA, London WT. The global epidemiology of hepatocellular carcinoma: Present and future. Clin Liver Dis. 2011;15:223–43, vii. doi: 10.1016/j.cld.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.McGlynn KA, Petrick JL, London WT. Global epidemiology of hepatocellular carcinoma: An emphasis on demographic and regional variability. Clin Liver Dis. 2015;19:223–238. doi: 10.1016/j.cld.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mirzaei M, Ghoncheh M, Pournamdar Z, Soheilipour F, Salehiniya H. Incidence and trend of liver cancer in Iran. J Coll Physicians Surg Pak. 2016;26:306–309. [PubMed] [Google Scholar]
- 79.Moayedi J, Moini M, Geramizadeh B, Malekhosseini SA, Yaghobi R. Seropositive form of occult hepatitis b virus infection in Iranian patients with cryptogenic liver cirrhosis. Hepat Mon. 2019;19. [Google Scholar]
- 80.Mohammadian M, Soroush A, Mohammadian-Hafshejani A, Towhidi F, Hadadian F, Salehiniya H. Incidence and mortality of liver cancer and their relationship with development in Asia. Asian Pac J Cancer Prev. 2016;17:2041–2047. doi: 10.7314/apjcp.2016.17.4.2041. [DOI] [PubMed] [Google Scholar]
- 81.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nakagawa-Senda H, Yamaguchi M, Matsuda T, Koide K, Kondo Y, Tanaka H, et al. Cancer prevalence in Aichi, Japan for 2012: Estimates based on incidence and survival data from population-based cancer registry. Asian Pac J Cancer Prev. 2017;18:2151–2156. doi: 10.22034/APJCP.2017.18.8.2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Naugler WE, Sakurai T, Kim S, Maeda S, Kim K, Elsharkawy AM, et al. Gender disparity in liver cancer due to sex differences in myd88-dependent il-6 production. Science. 2007;317:121–124. doi: 10.1126/science.1140485. [DOI] [PubMed] [Google Scholar]
- 84.Nikbakht HA, Sahraian S, Ghaem H, Javadi A, Janfada M, Hassanipour S, et al. Trends in mortality rates for gastrointestinal cancers in Fars Province, Iran (2005–2015) J Gastrointest Cancer. 2019;epub ahead of print. doi: 10.1007/s12029-019-00204-1. [DOI] [PubMed] [Google Scholar]
- 85.Nordenstedt H, White DL, El-Serag HB. The changing pattern of epidemiology in hepatocellular carcinoma. Dig Liver Dis. 2010;42(Suppl 3):S206–S214. doi: 10.1016/S1590-8658(10)60507-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Norsa'adah B, Nurhazalini-Zayani CGC. Epidemiology and survival of hepatocellular carcinoma in North-East Peninsular Malaysia. Asian Pac J Cancer Prev. 2013;14:6955–6959. doi: 10.7314/apjcp.2013.14.11.6955. [DOI] [PubMed] [Google Scholar]
- 87.Oh CM, Won YJ, Jung KW, Kong HJ, Cho H, Lee JK, et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2013. Cancer Res Treat. 2016;48:436–450. doi: 10.4143/crt.2016.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, et al. Asian pacific association for the study of the liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010;4:439–474. doi: 10.1007/s12072-010-9165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Penson DF, Krishnaswami S, Jules A, Seroogy JC, McPheeters ML. Evaluation and treatment of cryptorchidism. Rockville, MD: Agency for Healthcare Research and Quality (US); 2012. (Report No.: 13-EHC001-EF.2012). [PubMed] [Google Scholar]
- 90.Pinheiro PS, Morris CR, Liu L, Bungum TJ, Altekruse SF. The impact of follow-up type and missed deaths on population-based cancer survival studies for hispanics and asians. J Natl Cancer Inst Monogr. 2014;49:210–217. doi: 10.1093/jncimonographs/lgu016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pons F, Varela M, Llovet JM. Staging systems in hepatocellular carcinoma. HPB (Oxford) 2005;7:35–41. doi: 10.1080/13651820410024058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Redaniel MT, Laudico A, Mirasol-Lumague MR, Gondos A, Brenner H. Cancer survival differences between European countries and an urban population from the Philippines. Eur J Public Health. 2011;21:221–228. doi: 10.1093/eurpub/ckq031. [DOI] [PubMed] [Google Scholar]
- 93.Redaniel MT, Laudico A, Mirasol-Lumague MR, Gondos A, Pulte D, Mapua C, et al. Cancer survival discrepancies in developed and developing countries: Comparisons between the Philippines and the United States. Brit J Cancer. 2009;100:858–862. doi: 10.1038/sj.bjc.6604945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sankaranarayanan R. Cancer survival in Africa, Asia, the Caribbean and Central America. Introduction. IARC Sci Publ. 2011;162:1–5. [PubMed] [Google Scholar]
- 95.Sato Y, Arimoto H, Ishikawa KB, Yoshimura K, Kaneko S, Koshiji M, et al. Survival trends of patients treated at the national cancer center hospital, Japan, from 1962 to 1994. Jpn J Clin Oncol. 2002;32:181–186. doi: 10.1093/jjco/hyf037. [DOI] [PubMed] [Google Scholar]
- 96.Schwarz RE, Smith DD. Trends in local therapy for hepatocellular carcinoma and survival outcomes in the US population. Am J Surg. 2008;195:829–836. doi: 10.1016/j.amjsurg.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 97.Shu H, Kang X, Guo K, Li S, Li M, Sun L, et al. Diagnostic value of serum haptoglobin protein as hepatocellular carcinoma candidate marker complementary to alpha fetoprotein. Oncol Rep. 2010;24:1271–1276. doi: 10.3892/or_00000982. [DOI] [PubMed] [Google Scholar]
- 98.Somboon K, Siramolpiwat S, Vilaichone RK. Epidemiology and survival of hepatocellular carcinoma in the central region of Thailand. Asian Pac J Cancer Prev. 2014;15:3567–3570. doi: 10.7314/apjcp.2014.15.8.3567. [DOI] [PubMed] [Google Scholar]
- 99.Sriamporn S, Black RJ, Sankaranarayanan R, Kamsa-ad S, Parkin DM, Vatanasapt V. Cancer survival in Khon Kaen Province, Thailand. Int J Cancer. 1995;61:296–300. doi: 10.1002/ijc.2910610303. [DOI] [PubMed] [Google Scholar]
- 100.Sriplung H, Prechavittayakul P. Cancer survival in Songkhla, Thailand, 1990-1999. IARC Sci Publ. 2011;162:227–235. [PubMed] [Google Scholar]
- 101.Sumitsawan Y, Srisukho S, Sastraruji A, Chaisaengkhum U, Maneesai P, Waisri N. Cancer survival in Chiang Mai, Thailand, 1993-1997. IARC Sci Publ. 2011;162:199–209. [PubMed] [Google Scholar]
- 102.Takano S, Watanabe Y, Ohishi H, Kono S, Nakamura M, Kubota N, et al. Multimodality treatment for patients with hepatocellular carcinoma: A single institution retrospective series. Eur J Surg Oncol. 2000;26:67–72. doi: 10.1053/ejso.1999.0743. [DOI] [PubMed] [Google Scholar]
- 103.Takayasu K, Furukawa H, Wakao F, Muramatsu Y, Abe H, Terauchi T, et al. CT diagnosis of early hepatocellular carcinoma: Sensitivity, findings, and CT-pathologic correlation. AJR Am J Roentgenol. 1995;164:885–890. doi: 10.2214/ajr.164.4.7726041. [DOI] [PubMed] [Google Scholar]
- 104.Tanaka H, Tanaka M, Chen WQ, Park S, Jung KW, Chiang CJ, et al. Proposal for a cooperative study on population-based cancer survival in selected registries in East Asia. Asian Pac J Cancer Prev. 2009;10:1191–1198. [PubMed] [Google Scholar]
- 105.Tangkijvanich P, Mahachai V, Suwangool P, Poovorawan Y. Gender difference in clinicopathologic features and survival of patients with hepatocellular carcinoma. World J Gastroenterol. 2004;10:1547–1550. doi: 10.3748/wjg.v10.i11.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends - an update. Cancer Epidemiol Biomarkers Prev. 2016;25:16–27. doi: 10.1158/1055-9965.EPI-15-0578. [DOI] [PubMed] [Google Scholar]
- 107.Toyoda H, Kumada T, Kiriyama S, Sone Y, Tanikawa M, Hisanaga Y, et al. Changes in the characteristics and survival rate of hepatocellular carcinoma from 1976 to 2000 - analysis of 1365 patients in a single institution in Japan. Cancer. 2004;100:2415–2421. doi: 10.1002/cncr.20289. [DOI] [PubMed] [Google Scholar]
- 108.Tsukuma H, Ajiki W, Ioka A, Oshima A, Research Group of Population-Based Cancer Registries of Japan. Survival of cancer patients diagnosed between 1993 and 1996: A collaborative study of population-based cancer registries in japan. Jpn J Clin Oncol. 2006;36:602–607. doi: 10.1093/jjco/hyl068. [DOI] [PubMed] [Google Scholar]
- 109.Turati F, Edefonti V, Talamini R, Ferraroni M, Malvezzi M, Bravi F, et al. Family history of liver cancer and hepatocellular carcinoma. Hepatology. 2012;55:1416–1425. doi: 10.1002/hep.24794. [DOI] [PubMed] [Google Scholar]
- 110.Wang JH, Changchien CS, Hu TH, Lee CM, Kee KM, Lin CY, et al. The efficacy of treatment schedules according to Barcelona clinic liver cancer staging for hepatocellular carcinoma - survival analysis of 3892 patients. Eur J Cancer. 2008;44:1000–1006. doi: 10.1016/j.ejca.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 111.Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Ann NY Acad Sci. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wong RJ, Corley DA. Survival differences by race/ethnicity and treatment for localized hepatocellular carcinoma within the United States. Dig Dis Sci. 2009;54:2031–2039. doi: 10.1007/s10620-008-0661-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wu EM, Wong LL, Hernandez BY, Ji J-F, Jia W, Kwee SA, et al. Gender differences in hepatocellular cancer: Disparities in nonalcoholic fatty liver disease/steatohepatitis and liver transplantation. Hepatoma Res. 2018;4:66. doi: 10.20517/2394-5079.2018.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Xiang YB, Jin F, Gao YT. Cancer survival in Shanghai, China, 1992-1995. IARC Sci Publ. 2011;162:55–68. [PubMed] [Google Scholar]
- 115.Xiao L, Zhang RL, Zhang H, Tulahong A, Zhang YF, Wen H, et al. Comparison of the clinical characteristics and survival between Uyghur patients with hepatitis virus-related and non-b, non-c hepatocellular carcinoma in Xinjiang, China. Chin J Cancer Res. 2015;27:279–287. doi: 10.3978/j.issn.1000-9604.2015.01.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Xishan H, Chen K, Min H, Shufen D, Jifang W. Cancer survival in Tianjin, China, 1991-1999. IARC Sci Publ. 2011;162:69–84. [PubMed] [Google Scholar]
- 117.Xue TC, Xie XY, Zhang L, Yin X, Zhang BH, Ren ZG. Transarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombus: A meta-analysis. BMC Gastroenterol. 2013;13:60. doi: 10.1186/1471-230X-13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Yaghi C, Sharara AI, Rassam P, Moucari R, Honein K, BouJaoude J, et al. Hepatocellular carcinoma in Lebanon: Etiology and prognostic factors associated with short-term survival. World J Gastroenterol. 2006;12:3575–3580. doi: 10.3748/wjg.v12.i22.3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yeo Y, Gwack J, Kang S, Koo B, Jung SJ, Dhamala P, et al. Viral hepatitis and liver cancer in Korea: An epidemiological perspective. Asian Pac J Cancer Prev. 2013;14:6227–6231. doi: 10.7314/apjcp.2013.14.11.6227. [DOI] [PubMed] [Google Scholar]
- 120.Yuen MF, Cheng CC, Lauder IJ, Lam SK, Ooi CG, Lai CL. Early detection of hepatocellular carcinoma increases the chance of treatment: Hong Kong experience. Hepatology. 2000;31:330–335. doi: 10.1002/hep.510310211. [DOI] [PubMed] [Google Scholar]
- 121.Yusuf MA, Badar F, Meerza F, Khokhar RA, Ali FA, Sarwar S, et al. Survival from hepatocellular carcinoma at a cancer hospital in Pakistan. Asian Pac J Cancer Prev. 2007;8:272–274. [PubMed] [Google Scholar]
- 122.Zamor PJ, deLemos AS, Russo MW. Viral hepatitis and hepatocellular carcinoma: Etiology and management. J Gastrointest Oncol. 2017;8:229–242. doi: 10.21037/jgo.2017.03.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zamora-Valdes D, Taner T, Nagorney DM. Surgical treatment of hepatocellular carcinoma. Cancer Control. 2017;24:1073274817729258. doi: 10.1177/1073274817729258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zeng HM, Zheng RS, Guo YM, Zhang SW, Zou XN, Wang N, et al. Cancer survival in China, 2003-2005: A population-based study. Int J Cancer. 2015;136:1921–1930. doi: 10.1002/ijc.29227. [DOI] [PubMed] [Google Scholar]
- 125.Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004;130:417–422. doi: 10.1007/s00432-004-0552-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Zhang Y, Li Y, Cai J. Surgical management of patients with BCLC b hepatocellular carcinoma and survival analysis - a single center experience in China. Eur J Cancer. 2015;51:S425. [Google Scholar]
- 127.Zhao Y, Zhan X, Zhang Y. Outcomes of non-alcoholic steatohepatitis patients after liver transplantation: A systematic review and meta-analysis. Hepat Mon. 2019;19 [Google Scholar]
- 128.Zheng R, Qu C, Zhang S, Zeng H, Sun K, Gu X, et al. Liver cancer incidence and mortality in China: Temporal trends and projections to 2030. Chin J Cancer Res. 2018;30:571–579. doi: 10.21147/j.issn.1000-9604.2018.06.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zheng R, Zuo T, Zeng H, Zhang S, Chen W. Mortality and survival analysis of liver cancer in China. Zhonghua zhong liu za zhi [Chinese journal of oncology] 2015;37:697–702. [PubMed] [Google Scholar]
- 130.Zhou XD, Tang ZY, Yang BH, Zhang BH. Hepatocellular carcinoma: The role of screening. Asian Pac J Cancer Prev. 2000;1:121–126. [PubMed] [Google Scholar]
- 131.Zhu Q, Li N, Zeng X, Han Q, Li F, Yang C, et al. Hepatocellular carcinoma in a large medical center of China over a 10-year period: Evolving therapeutic option and improving survival. Oncotarget. 2015;6:4440–4450. doi: 10.18632/oncotarget.2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhu RX, Seto W-K, Lai C-L, Yuen M-F. Epidemiology of hepatocellular carcinoma in the Asia-Pacific region. Gut Liver. 2016;10:332–339. doi: 10.5009/gnl15257. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.