Abstract
Background
Many patients visit their general practitioner (GP) because of problems that are psychosocial in origin. However, for many of these problems there is no evidence‐based treatment available in primary care, and these patients place time‐consuming demands on their GP. Therefore, GPs could benefit from tools to help these patients more effectively and efficiently. In this light, it is important to assess whether structured psychosocial interventions might be an appropriate tool for GPs. Previous reviews have shown that psychosocial interventions in primary care seem more effective than usual care. However, these interventions were mostly performed by health professionals other than the GP.
Objectives
To examine the effectiveness of psychosocial interventions by general practitioners by assessing the clinical outcomes and the methodological quality of selected studies.
Search methods
The search was conducted using the CCDANCTR‐Studies and CCDANCTR‐References on 20/10/2005, The Cochrane Library, reference lists of relevant studies for citation tracking and personal communication with experts.
Selection criteria
Randomised controlled trials, controlled clinical trials and controlled patient preference trials addressing the effectiveness of psychosocial interventions by GPs for any problem or disorder. Studies published before November 2005 were eligible for entry.
Data collection and analysis
Methodological quality was independently assessed by two review authors using the Maastricht‐Amsterdam Criteria List. The qualitative and quantitative characteristics of selected trials were independently extracted by two review authors using a standardised data extraction form. Levels of evidence were used to determine the strength of the evidence available. Results from studies that reported similar interventions and outcome measures were meta‐analysed.
Main results
Ten studies were included in the review. Selected studies addressed different psychosocial interventions for five distinct disorders or health complaints. There is good evidence that problem‐solving treatment by general practitioners is effective for major depression. The evidence concerning the remaining interventions for other health complaints (reattribution or cognitive behavioural group therapy for somatisation, cognitive behavioural therapy for unexplained fatigue, counselling for smoking cessation, behavioural interventions to reduce alcohol reduction) is either limited or conflicting.
Authors' conclusions
In general, there is little available evidence on the use of psychosocial interventions by general practitioners. Of the psychosocial interventions reviewed, problem‐solving treatment for depression may offer promise, although a stronger evidence‐base is required and the effectiveness in routine practice remains to be demonstrated. More research is required to improve the evidence‐base on this subject.
Plain language summary
Psychosocial interventions delivered by GPs
Many patients visit their general practitioner (GP) because of psychosocial problems. Consequently, GPs could benefit from tools to help these patients. The reviewers found no strong evidence for the effectiveness (or ineffectiveness) of psychosocial interventions by general practitioners. Of the psychosocial interventions reviewed, problem‐solving treatment for depression seems the most promising tool for GPs, although its effectiveness in daily practice remains to be demonstrated.
Background
Many patients visit their general practitioner (GP) because of problems that are psychosocial in origin. The reported prevalence of psychological or psychosocial disorders (e.g. depression, anxiety, stress, somatisation, unexplained or functional symptoms in primary care ranges from 30% to 70% (Chocron Bentata 1995; Tiemens 1996). However, the extent of mental health disorders in general practice is difficult to estimate due to problems of classification (Gray 1988).
There is an increasing awareness among GPs that responsibility for managing these patients falls mainly to them (Terluin 1999). However, for many of these complaints, there is no evidence‐based treatment available. Immediate referral to specialist care is often not an option, because of waiting lists or the vague nature of complaints. These patients often visit their GP frequently without being offered an appropriate treatment and place time‐consuming demands on already overloaded primary care services. Therefore, GPs need the tools to help these patients in a way that is not only effective but also cost‐effective, considering that the GP's time is expensive.
Several previous reviews have addressed the efficacy or effectiveness of psychosocial interventions (e.g. counselling, problem solving therapy, cognitive behavioural interventions, psychotherapy) in primary care (Corney 1992; Brown 1995; Friedli 1996; Rowland 2000; Bower 2002). A general characteristic of psychosocial interventions is that some sort of psychological process comprises the central dynamic in the treatment of the patient. The overall conclusion in these reviews was that psychosocial interventions seem more effective than the usual care that is given by the GP, but that clear clinical evidence is lacking. Rowland (2000) points out in her systematic review (an updated version in The Cochrane Library was headed by Bower) on counselling for depression that the four studies she was able to include had many methodological deficiencies, which makes the effectiveness of these studies harder to interpret. Friedli 1996 states that despite some supporting evidence for the effectiveness of counselling in primary care, it is still unknown which type of psychosocial intervention is helpful for which patient in primary care. These reviews also demonstrated how difficult it is to define 'psychosocial interventions'.
However, the psychosocial interventions addressed in the aforementioned reviews were mostly performed by primary care workers other than the GP (e.g. nurses, counsellors, psychologists, psychiatrists, internists), leaving the question of whether psychosocial interventions performed by GPs might be effective. In a narrative review of psychological management approaches by general practitioners, Cape 2000 came to the conclusion that the preliminary evidence for the clinical effectiveness of GP psychological management in routine consultations is scarce but encouraging.
There are several reasons why GPs could use the knowledge and skills to perform psychosocial interventions in primary care. As patients come to their GP first with their health concerns, it is desirable that all potential treatment options in primary care are considered before a patient is referred to specialist care. This approach is known as the 'stepped‐care principle' (Davison 2000; Von Korff 2000). Secondly, many GPs already take the time to support their distressed patients without adequate tools to structure these extended visits. Although these visits can be helpful, the contribution to the overall improvement often seems small against the investment of time. Therefore, many GPs would benefit from psychosocial skills that enable them to use their time more efficiently. Thirdly, the degree of success of any kind of psychosocial intervention depends largely on the trust one places in the care‐provider. Since patients and GPs already maintain a relationship, it can be assumed that the familiarity of the doctor's office is preferred to visiting an unknown non‐GP primary care worker. Finally, it is recommendable to take a holistic approach to patient care (Richardson 1989) in which physicians care not only about the somatic aspects of care but rather try to improve the well‐being of patients in all aspects related to health.
Objectives
In this review, we aimed to present a systematic review of all the available literature addressing the effectiveness of psychosocial interventions by general practitioners. An important underlying objective was to assess whether it is (more) effective to have GPs delivering psychosocial interventions in the first place, for the reasons mentioned previously. In most instances, psychosocial interventions are performed by psychologists and psychiatrists, not by general practitioners. We might have started with assessing the effects of training GPs in applying psychosocial interventions and focus on the feasibility. Instead, we chose to investigate the effects of psychosocial interventions by GPs on patients' well‐being, regardless of the anticipated diversity (and therefore incomparability) in type of interventions, participants and outcomes among studies eligible for inclusion.
The objectives of this review were:
1) To identify all randomised controlled trials (RCTs) controlled clinical trials (CCTs) and controlled patient preference trials (CPPTs) of psychosocial interventions delivered by general practitioners.
2) To assess the methodological quality and the relevant characteristics of the selected studies.
3) To assess the effectiveness of psychosocial interventions by general practitioners compared to the reference treatment (whether 'usual care' or another experimental intervention) by reviewing the clinical outcomes of the selected studies.
Methods
Criteria for considering studies for this review
Types of studies
Studies published before January 2002 were eligible for entry in the review. Identified trials in all languages were considered eligible. If necessary, assistance was going to be sought from the Cochrane Collaboration Depression Anxiety and Neurosis group (CCDAN) for translation purposes. An update was performed in November 2005, aimed at identifying studies that were published after 2002.
All RCTs, CCTs and CPPTs addressing the effectiveness of psychosocial interventions by GPs were considered eligible for inclusion. Patient preference for a certain treatment option is a strong predictor for patient compliance and thus for the effectiveness of the intervention. CPPTs, in which patients with a strong preference for a particular treatment are not randomised, but are allocated to the treatment of their choice, were therefore included.
Bower 2002 discussed the different objectives and designs of pragmatic versus explanatory trials. Explanatory trials aim to isolate the active elements of an intervention in order to determine the relative potential of the treatment under highly controlled circumstances, whereas pragmatic trials aim to determine the relative value of the treatment in the routine practice settings. Although explanatory studies serve the objective of this review best, pragmatic trials were also eligible for entry in the review as long as the psychosocial intervention was standardised to some degree (see section 'types of intervention').
Types of participants
There were no restrictions on the type of participants in studies to be selected.
Types of interventions
All trials reporting the effectiveness of psychosocial interventions delivered by GPs were eligible for inclusion. A methodological difficulty was choosing a clear and objective definition for a psychosocial intervention. Rowland (Rowland 2000) and Bower (Bower 2002) present the British Association for Counselling definition of counselling as appropriate for use in their systematic reviews. However, counselling is "a broadly non‐directive approach" (Rowland 2000) while we chose to also include other, more structured approaches, like cognitive behavioural interventions or problem solving therapy.
In this review, a GP‐administered psychosocial intervention should meet the following criteria: 1) the intervention is explicitly delivered by a GP (or family physician or family doctor), although the GP intervention may be compared with a similar intervention administered by a different health professional. The GP can be the regular GP of patients or a research GP who is assigned to patients for the purpose of the study. 2) the intervention is a systematic treatment in which a psychological process is the central dynamic. 3) the intervention consists of a standardised number of at least two face‐to‐face contacts between patient and GP. Single session interventions are excluded, so that psychosocial interventions are distinguished from the brief psychosocial advice that is commonly given by GPs, but that cannot be accounted as a systematic treatment.
Studies were excluded if: 1) the intervention was a (psycho) pharmacological intervention. 2) the GP was only one of many interventionists and the results were not presented for every discipline (e.g. GP, nurse, counsellor) separately. 3) psychosocial interventions were only delivered in combination with other types of treatment (e.g. (placebo) pharmacotherapy, physiotherapy) and the effectiveness of the psychosocial intervention alone could not be evaluated.
Types of outcome measures
We did not restrict ourselves to one disorder, say depression, since this would result in a scope that was too narrow for our purposes. Since there were no restrictions on type of participant, type of disorder, problem or complaint, or type of psychosocial intervention, all outcome measures were reviewed and evaluated on their relevance. If more than one outcome measure was reported, we analysed the outcome measures that were believed to be the main outcome measures. To be included in the review, studies had to report at least one of two types of outcome: 1) (clinical) improvement rates or numbers (e.g. % patients who are clinically recovered) 2) scores on relevant validated scales (e.g. Beck Depression Inventory, Hamilton Rating Scale for Depression, SCL‐90)
Search methods for identification of studies
The search strategy included the following sources:
1) The Cochrane Collaboration Depression Anxiety and Neurosis group Controlled Trials Registers (CCDANCTR‐Studies and CCDANCTR‐References) were searched on 20/20/2005. These are specialised registers tof studies and reference of trials comparing treatment options within the scope of the CCDAN. The register is updated quarterly, adding the results on searches of The Cochrane Library, CINAHL, EMBASE, LILACS, MEDLINE, NRR, PSYCLIT, PSYCINFO, PSYNDEX and SIGLE. Also, quarterly systematic screening of relevant journals and conference proceedings takes place. For information on the full search strategies, visit www.iop.kcl.ac.uk/iop/ccdan.index.htm.
CCDANCTR‐Studies Intervention = Therapy and Setting = General Practice or Primary Care or Family Practice
CCDANCTR‐References Free‐text = *Therapy and Free‐text = General Practi* or Primary Care or Family Practice
The original CCDANCTR search strategy can be found in Table 2
1. Original CCDAN search strategy.
| terms |
| (#30 = BEHAVIOR‐THERAPY or #30 = BIOFEEDBACK or #30 = CASE‐MANAGEMENT or #30 = COGNITIVE‐ANALYTIC‐THERAPY or #30 = COGNITIVE‐BEHAVIOR‐THERAPY or #30 = COGNITIVE‐THERAPY or #30 = COUNSELLING or #30 = FAMILY‐THERAPY or #30 = MARITAL‐THERAPY or #30 = PSYCHOANALYTIC‐THERAPY or #30 = PSYCHOTHERAPY or #30 = RELAXATION‐THERAPY or #30 = SOCIAL‐INTERVENTION) AND (#11 = PRIMARY‐CARE or "general practitioner*" or "family physician*" or "family doctor*") |
2) The Cochrane Library. It became apparent that some studies identified earlier through screening of journals did not appear in the first CCDAN‐CTR search. Trials Search Co‐ordinator, Hugh McGuire therefore performed additional searches in The Cochrane Library (Issues 2001‐2 to 2002‐1) using the following search strategy:
(GENERAL and PRACT*) (FAMILY and PRACT*) (PRIMARY and CARE) (PRIMARY and (HEALTH and CARE)) (FAMILY and DOCTOR*) (FAMILY and PHYSIC*) GP*((((((#1 or #2) or #3) or #4) or #5) or #6) or#7) PSYCHOTHERAPY COGNITIV* BEHAVIOR BEHAVIOUR PSYCHOANALYTIC MARITAL COUNSELLING THERAP* PSYCHO* (((((#10 or #11) or #12) or #13) or #14) or #17) (#18 and #16) ((#15 or #19) or #9) (#8 and #20)
3) Reference lists of relevant studies were scanned to retrieve additional studies that were not identified in the aforementioned database searches. This process is known as citation tracking.
4) Personal communication with experts in the field (CCDAN and otherwise) took place.
5) An updated search was performed in November 2005.
Data collection and analysis
Selection of studies Two authors (MH and AB) independently screened the abstracts of the studies that were retrieved by the computer assisted searches. Studies that were identified by citation tracking or personal communication were also screened by both MH and AB. Eligibility criteria were used to select relevant studies. Disagreement between MH and AB about the selection of a trial was resolved by discussion between MH, AB and a third review author (GB). Thus, a final selection of studies was established. Since the review authors were familiar with some of the studies beforehand, it was decided that studies were not blinded for assessment.
Methodological quality Methodological quality of the studies was independently assessed by two review authors, AB and GB, using the Maastricht‐Amsterdam Criteria List (MACL) (Van Tulder 1997). A third review author (MH) was involved in rating methodological quality if disagreement occured between AB and GB. Review authors were thus allowed to adjust their score assignments. If additional information on study characteristics was provided by authors on request, this information was used in the scoring of the items of the MACL.
The Maastricht‐Amsterdam Criteria List (MACL) was originally developed in the field of musculo‐skeletal disorders, but is known to produce disease‐nonspecific quality ratings. Also, the MACL includes all criteria of other prominent quality scales like the Jadad List (Jadad 1996) and the Delphi List (Verhagen 1998). The MACL contains 17 items to assess internal validity (e.g. selection bias, performance bias, attrition bias and detection bias, 10 items), external validity (descriptive criteria, five items) and statistical aspects (two items). The total score on the MACL can range from 0‐17. To prevent different interpretations between reviewers of study characteristics, each item of the MACL is explained in a separate appendix that provides uniform operationalisations of criteria. Despite this appendix, two items on the acceptability of compliance and withdrawal still raised questions about the appropriate interpretation among the reviewers. Therefore, we defined acceptable compliance as 75% of the patients in all treatment groups attending all treatment sessions and acceptable withdrawal/dropout as 80% of all patients in all study groups completing all study assessments, in addition to the original appendix.
Data extraction The study characteristics (i.e. qualitative and quantitative characteristics) of selected trials were extracted with the use of a specially designed data extraction form by two reviewers independently (AB and GB). Disagreement between AB and GB was resolved by discussion between AB, GB and MH. Missing information was obtained from the investigators when possible. The following study characteristics were extracted: study size (total, group), number of active GPs, number of practices, inclusion criteria, type of intervention (content, number of sessions, duration of sessions), type of control condition, training of GPs (content, number of sessions, duration of sessions), supervision of GPs (content, number of sessions, duration of sessions), integrity check (content), study outcome (main effects, compliance with treatment by patients, withdrawal from study assessments) and overall conclusion of authors. Statisical analysis Although selected studies were very heterogeneous in types of interventions, types of complaints, study population and outcome measures, meta‐analyses were performed if at least two studies reported data on a particular outcome of a clinically comparable intervention and a similar follow‐up period.
Analyses were performed using Review Manager software. Relative risks were calculated for dichotomous outcomes and weighted mean differences for continuous outcomes. If standard deviations were not available, we calculated imputations in accordance with the Cochrane Handbook for Systematic Reviews (section 8.5.2.). The random‐effect model was used as default method of analysis because of the potential statistical heterogeneity among studies. Heterogeneity was investigated by evaluating whether confidence intervals around the individual effect sizes of pooled studies overlapped sufficiently and were described accordingly in the results.
In addition to meta‐analyses, number needed to treat to benefit or harm were calculated for the last available endpoint if outcomes were presented as dichotomous data. We used the denotation as suggested by Altman (Altman 1998): number of patients needed to be treated for one additional patient to benefit or be harmed are denoted as NNTB (benefit, positive score) or NNTH (harm, negative score), with confidence intervals that include 'infinity' if necessary (for example, NNTB 10, CI = NNTH 20 to infinity to NNTB 4). If the confidence interval is limited to positive scores (e.g. CI = NNTB 5 to NNTB 15) or negative scores and therefore does not include infinity, the number needed to treat to benefit is statistically significant.
Levels of evidence For a more qualitative approach, so‐called 'levels of evidence' were used (Van Tulder 1997; Van Tulder 2001; Ostelo 2002). This rating scale enables reviewers to summarize the strength of scientific evidence by classifying results of studies with comparable interventions and more or less comparable outcome measures under one of four levels: 1. good evidence: provided by generally consistent findings in two or more high‐quality studies. 2. moderate evidence: provided by generally consistent findings in one high‐quality study and one or more low‐quality studies or by generally consistent findings in two or more low‐quality studies. 3. limited or conflicting evidence: only one study (either high‐ or low‐quality) or inconsistent findings in two or more studies. 4. no evidence: no studies. High quality studies were defined as studies that fulfilled five or more of the 10 MACL items on internal validity (range 0‐10). Generally consistent findings were defined as 75% or more of the studies having statistically significant findings in the same direction.
Results
Description of studies
Selection of studies Computer‐assisted searches of databases yielded 179 references in the CCDAN Trials Register and 436 references in the Cochrane Library. Of these, 42 full‐text articles were retrieved based on title and abstract and screened for eligibility. In addition, nine articles were identified through citation tracking or personal communication and retrieved for further screening. Of these 51 full‐text papers, 19 articles were selected for additional reading. Eight authors were contacted for additional information or unpublished data and seven authors responded to our requests. This process resulted in eight studies that met eligibility criteria and that were included in the review (table included studies). The remaining 36 studies (43 articles) were excluded from the review (Characteristics of excluded studies). In one included study (Mynors‐Wallis 1995), therapists were two research GPs and one psychiatrist. Since the effects were no different for the two GPs compared to the psychiatrist, we decided to include the study in the review, despite the fact that effects were not presented for GPs separately. In a second included study (Lidbeck 1997), the therapist performing all interventions was a physician trained in family medicine as well as internal and social medicine who worked in a preventive medicine unit in primary care, which raised our doubts whether this therapist could be classified as a typical general practitioner. However, since the study formally met our inclusion criteria, we decided to include the study in the review.
The updated search in 2005 yielded 97 references, and 4 full‐text articles were retrieved and selected for additional reading. One author was contacted for additional information. Two studies published after 2002 met eligibility criteria and were included in the review.
Excluded studies Of the 36 studies that were initially retrieved but finally excluded from the review, 11 studies were excluded because the intervention was not performed by a GP (Barkham 1989; Issakidis 1999; McLeod 1997; Ockene I 1999; Ockene J 1991; Peveler 1999; Scott 1997; Skinner 1984; Swinson 1992; Wadden 1997; White 1990). Seven studies were excluded because the intervention was not a psychosocial intervention in our definition (Beusterien 2000; Bowman 2000; Durand 2002; Katzelnick 2000; King 1998; Kottke 1989; Wallace 1988). Another seven studies were excluded because the intervention was administered by a group of GPs and other health professionals (e.g. nurse practitioners, general internists, psychiatrists), without separate analyses for each discipline being presented (Blomhoff 2001; Fleming 1997; Fleming 1999; Goldstein 1999; Patel 1988; Pill 1998; Simkin 1997). In one of these studies, the intervention consisted of two parts administered by a GP and a nurse (Patel 1988). In six studies, the selection criterion of at least two standardised intervention sessions was not met: in four studies, the intervention studies consisted of only one session (Anderson 1992; Brody 1990; Calfas 1996; Horst 1997) while in two other studies, no required number of standardised intervention sessions was formulated (Catalan 1984; King 2002). In these last two studies, the training of GPs in applying a psychosocial intervention was the focus of attention, rather than the application of the intervention itself. As a consequence, number of intervention sessions were not explicitly monitored, and it was often unknown if GPs even applied their new skills, as one of the authors stated. Three studies were excluded because the study design was not a RCT, CCT or CPPT (Baillargeon 1998; Gask 1992; Morriss 1999). In two studies, the effects of 'isolated' psychosocial intervention could not be assessed since the intervention was only administered in combination with another treatment (nicotine gum and (placebo‐)antidepressant treatment) (Malt 1999; Wilson 1988).
Of the two studies excluded in 2005, one study only assessed outcomes on the level of the participating GPs (Heatley 2005), while the second study assessed an intervention that did not require at least two standardised sessions (Whitehead 2002).
Study Characteristics The most important characteristics and outcomes of included studies were summarized in table 'characteristics of included studies'. In the section 'notes' of this table, additional information is presented on non‐compliance of patients with treatment (e.g. session attendance), withdrawal by patients from study assessments (i.e. drop‐out, loss‐to‐follow‐up) and the use of integrity checks (assessment of GP compliance with the treatment protocol).
The ten included studies reported the effectiveness of psychosocial interventions by general practitioners for the following health complaints or disorders: depression (Mynors‐Wallis 1995; Mynors‐Wallis 2000), somatisation (Blankenstein 2001; Lidbeck 1997; Larisch 2004), smoking addiction (Richmond 1985; Segnan 1991) excessive alcohol consumption (McIntosh 1997; Richmond 1995), and unexplained fatigue (Huibers 2004).
Risk of bias in included studies
For the qualification of methodological quality (high or low), the 10 MACL items on internal validity were used. In total seven studies (Blankenstein 2001; Lidbeck 1997; McIntosh 1997; Mynors‐Wallis 1995; Mynors‐Wallis 2000; Segnan 1991; Huibers 2004) had a high methodological quality (five points or more) and three studies (Richmond 1985; Richmond 1995; Larisch 2004) had a low methodological quality (less than five points). Details on the individual scores on the MACL will not be presented here, but are available from the first author.
Effects of interventions
Depression studies In two high‐quality RCTs by the same research group (Mynors‐Wallis 1995, Mynors‐Wallis 2000), the effects of six‐session problem solving treatment (PST) by a GP on major depression were compared to PST by a practice nurse, antidepressant treatment, placebo treatment or combination treatment (PST and antidepressant medication).
In the 1995 study, PST administered by one of two GPs (and a psychiatrist) was superior to placebo treatment combined with general support on depression and social functioning, but not on psychological symptoms at 12 week follow‐up. The NNTB of PST compared to placebo treatment was 3 (95% CI NNTB 1.75 to NNTB 10.29). There were no differences in effect between PST and antidepressant treatment (amitriptyline) combined with general support at 12 week follow‐up. The NNTB of PST compared to antidepressant treatment was 11.92 (95% CI NNTH 6.08 to infinity to NNTB 3.01).
In the 2000 study, the effects of PST administered by one of three GPs on depression, psychological symptoms or social functioning were no different compared to the effects of PST by a practice nurse, antidepressant treatment or combination treatment at 52 week follow‐up. The NNTB of PST by a GP was 18.38 (95% CI NNTH 6.21 to infinity to NNTB 3.71) compared to PST by a practice nurse and 16.71(95% CI NNTH 6.13 to infinity to NNTB 3.53) compared to antidepressant medication. The NNTH of PST by a GP compared to combination treatment was 23.95 (95% CI NNTH 3.83 to infinity to NNTB 5.63).
Both studies reported equivalent outcome measures for PST by a GP and antidepressant treatment at 12 weeks and several data were meta‐analysed. There were no differences between PST by a GP and antidepressant treatment in recovery (Hamilton Rating Scale score of 7 or lower), depression (Hamilton Rating Scale and Beck Depression Inventory) or social functioning (Social Adjustment Scale). The pooled relative risk for recovery of PST by a GP compared to antidepressant treatment was 0.93 (95% CI 0.62 to 1.39). The weighted mean difference between PST by a GP and antidepressant treatment was 0.77 (95% CI ‐2.45 to 4) on the Hamilton Rating scale, ‐1.12 (95% CI ‐4.75 to 2.51) on the Beck Depression Inventory. Evaluation of the confidence intervals around the weighted mean differences on the social adjustment scale revealed statistical heterogeneity between the two studies. Therefore, it was decided that scores on this scale should not be pooled.
There is good evidence (level 1) that problem‐solving treatment by a GP is no less effective than antidepressant treatment on depression, psychological symptoms and social functioning. There is limited evidence (level 3) that problem‐solving treatment by a GP is more effective than placebo treatment on depression and social functioning. Finally, there is limited evidence (level 3) that problem‐solving by a GP is no less effective than problem‐solving by a practice nurse or combination treatment on depression, psychological symptoms or social functioning.
Somatisation studies In two high‐quality RCTs and one low‐quality study, the effectiveness of a psychosocial intervention by a GP on somatisation was assessed.
In one study (Blankenstein 2001), the effects of a tailored and modified reattribution intervention of two to three sessions by one of 10 GPs were compared to the effects of care as usual. At two year follow‐up, the reattribution intervention was superior to usual care on all primary outcomes (consumption of medical resources, subjective health and sick leave) and on secondary outcome somatisation, although none of the patients had recovered completely (no data presented).
In a second study (Lidbeck 1997), the effects of cognitive behavioural group therapy of eight sessions administered by the author were compared to a waiting list condition. At 6 month follow‐up, group therapy was superior to the waiting list condition on illness behaviour, hypochondriasis and medication use but not on social problems, anxiety, depression or sleep.
In a third study (Larisch 2004), the effects of additional reattribution training combined with standard psychosocial primary care of six sessions (PPC) by one of 20 GPs were compared to the effects of standard PPC alone. At 6 month follow‐up, there were no significant differences between the treatment groups in anxiety, depression, quality of life or mental health, except for a small difference in number of physical symptoms.
In none of these studies, data concerning recovery were presented. Calculations of NNT were therefore not possible. Since interventions, outcome measures and timing of assessment were not comparable for the two studies, meta‐analyses were not performed.
There is limited evidence (level 3) that reattribution intervention by a GP is more effective than usual care on consumption of medical resources, subjective health, sick leave and somatisation. There is limited evidence (level 3) that adding reattribution training to psychosocial primary care is no more effective than PPC alone. There is also limited evidence (level 3) that cognitive behavioural group therapy by a GP is more effective on illness behaviour, hypochondriasis and medication use.
Smoking cessation studies In one high‐quality RCT and one low‐quality CCT the effects of counselling by a GP on smoking cessation were assessed.
In the high‐quality study (Segnan 1991), the effects of five‐session 'repeated counselling' (RC) delivered by one of 44 GPs were no different compared to the effects of a one‐session minimal intervention (MI), repeated counselling plus nicotine gum (RC+gum) or repeated counselling plus spirometry (RC+spiro): biochemically validated smoking abstinence rates at 12 month follow‐up were respectively 4.8%, 5.5%, 7.5%, and 6.5%. The NNTB of RC compared to MI was 162.38 (95% CI NNTH 18.64 to infinity to NNTB 15.16). The NNTH of RC was 49.29 (95% CI NNTH 16.51 to infinity to NNTB 49.93) compared to RC+gum and 95.02 (95% CI NNTH 20.19 to infinity to NNTB 35.11) compared to RC+spiro.
In the low‐quality study (Richmond 1985), six‐session smoking cessation counselling delivered by one of three GPs was superior to a minimal intervention (usual care and use of a diary) consisting of two sessions: at 6 month follow‐up, 33% of the patients in the counselling group were biochemically validated as abstinent from smoking versus 3% in the minimal intervention group. The NNTB of counselling compared to minimal intervention was 3.33 (95% CI NNTB 2.51 to NNTB 4.95).
Evaluation of the confidence intervals around the effect sizes revealed statistical heterogeneity between the two studies, possibly due to differences in methodological quality since the interventions appear to be quite similar. It was therefore decided that abstinence rates from both studies should not be pooled.
There is conflicting evidence (level 3) that counselling by a GP is more or no less effective than minimal intervention on smoking behaviour. There is limited evidence (level 3) that counselling by a GP is no less effective than counselling plus nicotine gum or counselling plus spirometry by a GP on smoking behaviour.
Alcohol reduction studies In one high‐quality RCT and one low‐quality CCT the effectiveness of a psychosocial intervention by a GP on alcohol consumption was assessed. In the high‐quality study (McIntosh 1997), the effects of a two‐session cognitive behavioural intervention (CBI) administered by one research GP were compared to a CBI by a nurse practitioner and one‐session brief advice by one of 12 regular GPs. At 12 month follow‐up, there were no differences between the groups in alcohol consumption (quantity‐frequency) or alcohol‐related problems, although there was an overall reduction on these outcomes in all groups.
In the low‐quality study (Richmond 1995), the effects of a five‐session behavioural change programme (Alcoholscreen) by one of 119 GPs were compared to one‐session brief advice to stop drinking, assessment of drinking behaviour only and follow‐up measurement only. At 12 month follow‐up, there were no differences between the groups in alcohol consumption (% patients drinking above predefined consumption level) or alcohol‐related problems, although Alcoholscreen was superior to other treatment conditions if only those patients were analysed who had attended two sessions or more.
No data concerning recovery were presented, therefore, calculations of NNTB and NNTH were not possible. Since interventions and outcome measures were (partially) incomparable for the two studies, meta‐analyses were not performed.
There is limited evidence (level 3) that a cognitive behavioural intervention by a GP is no more effective than a cognitive behavioural intervention by a nurse practitioner or brief advice on alcohol consumption or alcohol‐related problems. Furthermore, there is limited evidence (level 3) that a behavioural change programme is no more effective than brief advice, assessment of drinking behaviour only or follow‐up measurement only on alcohol consumption or alcohol‐related problems.
Unexplained fatigue studies In a high‐quality RCT (Huibers 2004), the effects of five to seven sessions of cognitve behavioural therapy by one of nine GPs were compared to the effects of no treatment or usual care in a group of employees absent from work suffering from unexplained fatigue. There were no signficant differences between the groups in fatigue, absenteeism or clinical recovery, at 12 month follow‐up or at any other time point. The NNTH of cognitive behavioural therapy compared to usual care was 11.89 (95% CI NNTH 4.25 to infinity to NNTB 14.92).
There is limited evidence (level 3) that cognitive behavioural therapy is no more effective than no treatment or usual care on unexplained fatigue among employees.
Discussion
Effectiveness of psychosocial interventions by general practitioners In this review, the main objective was to provide a systematic overview of the available evidence on the effects of psychosocial interventions that are delivered by general practitioners in primary care. Not surprisingly, we found it impossible to draw an overall conclusion concerning the effectiveness of "psychosocial interventions by general practitioners" since the ten selected studies were not comparable in numerous aspects (e.g. intervention, outcome, patient population). Under these circumstances, the classification of the available results into a single 'level of evidence' is inappropriate.
Rather, we found that the available evidence addressed different psychosocial interventions for five distinct disorders or health complaints (depression, somatisation, smoking addiction, excessive alcohol consumption and fatigue). There is some evidence that problem‐solving treatment (PST) by a GP is effective in the treatment of major depression: there is good evidence (level 1) provided by two studies that PST is no less effective than antidepressant treatment, while there is limited evidence (level 3) that PST is more effective than placebo treatment and no less effective than PST by a nurse practitioner or combination therapy. These findings should be interpreted with considerable caution: the two studies on PST were conducted by the same research team and groups consisting of only 30 to 40 patients were treated by a small number of experienced and highly trained research GPs, which limits the translation to routine general practice.
As for the treatment of somatisation, there is limited evidence (level 3) that a reattribution intervention by a GP and cognitive behavioural group therapy by a GP are more effective than usual care by a GP, while there is also limited evidence that adding reattribution training to standard psychosocial primary care (PPC) is no more effective than PPC alone. There is conflicting evidence (level 3) provided by two studies that counselling by a GP is more or no less effective than a minimal intervention in helping patients to stop smoking, while there is limited evidence (level 3) that counselling by a GP is no less effective than counselling plus the prescription of nicotine gum or the use of spirometry. It is noted that the findings from another review indicate a small benefit obtained through brief advice from physicians, with an additional small benefit from more intensive advice (Silagy 2003). Behavioural interventions by a GP to reduce alcohol consumption seem no more effective than other, more simple interventions: there is limited evidence (level 3) that a cognitive behavioural intervention (CBI) by a GP is no more effective than a CBI by a nurse practitioner or brief advice and there is limited evidence that a behavioural change programme is no more effective than brief advice, assessment of drinking or follow‐up assessments only. Finally, there is limited evidence (level 3) that cognitive behavioural therapy by a GP is no more effective than no treatment or usual care for unexplained fatigue among employees.
In summary, despite fairly good methodological quality and positive findings of some studies, evidence for the effectiveness of psychosocial interventions by general practitioners does not exceed level 3 (limited or conflicting evidence), except for good evidence that problem‐solving treatment is no less effective than antidepressant treatment for depression.
Methodological quality In line with previous studies (Van Tulder 1997; Van Tulder 2001; Ostelo 2002), we used internal validity criteria of the MACL to classify methodological quality since internal validity best reflects the most essential methodological aspects that are required for good quality (and lack of bias). The MACL is accompanied by an explanatory appendix that proved to be helpful but not always sufficient. Especially the items on the acceptability of compliance and withdrawal posed reviewers for a problem since 'acceptability' was not defined in any quantum or measure. We therefore chose to define acceptable compliance as 75% of the patients in all treatment groups attending all treatment sessions and acceptable withdrawal/drop‐out as 80% of all patients in all study groups completing all study assessments.
Seven out of ten selected studies had a satisfactory methodological quality. Although controlled patient preference trials were eligible as well, only randomised controlled trials (seven high‐quality and one low‐quality study) and controlled clinical trials (two low‐quality studies) met eligibility criteria for the review. As was to be expected, none of the selected studies reported blinding of patients or GPs. Information on the avoidance or comparability of co‐interventions was poor in all but one study: six studies did not even mention this subject (Blankenstein 2001; Lidbeck 1997; Richmond 1985; Richmond 1995; McIntosh 1997; Larisch 2004) and three (Mynors‐Wallis 1995; Mynors‐Wallis 2000; Segnan 1991) provided very little information on these aspects. Acceptable compliance of patients with treatment, which is an indication of the acceptability of the treatment to patients, was achieved in only three studies (Lidbeck 1997; McIntosh 1997; Huibers 2004), while withdrawal rates were acceptable in only half of the studies (Blankenstein 2001; Lidbeck 1997; McIntosh 1997; Segnan 1991; Huibers 2004). The latter is of particular concern since unacceptable withdrawal/dropout rates, especially due to selective withdrawal, represent a major threat to the validity of results.
In general, it should be noted that many studies reported poorly on the supervision and training of GPs during the trial, the use of treatment protocols, the performance of integrity checks, the compliance of patients apart from the attendance of sessions, the nature of usual care (what care exactly did patients receive?), co‐interventions received, subgroup analyses or prognostic analyses (which patients benefit most?). Only two studies reported that GPs were supervised throughout the trial (Mynors‐Wallis 2000; Huibers 2004). In eight studies it was mentioned that GPs were trained (Blankenstein 2001; Lidbeck 1997; Mynors‐Wallis 1995; Mynors‐Wallis 2000; Richmond 1995; Segnan 1991; Huibers 2004; Larisch 2004), but only four studies elaborated to some extent on the specific content of the training (Blankenstein 2001; Mynors‐Wallis 1995; Mynors‐Wallis 2000; Larisch 2004). Two studies reported the use of a treatment protocol (Larisch 2004; Huibers 2004). Two studies reported the performance of integrity checks (Segnan 1991; Huibers 2004). Details on other aspects (compliance, nature of usual care, co‐interventions, subgroup/prognostic analyses) were generally insufficient, if mentioned at all. This lack of vital information makes it difficult to interpret the results of studies. A similar conclusion was drawn in the review by Rowland and Bower (Rowland 2000; Bower 2002). Especially in this field of research, in which the blinding of patients and caregivers is virtually impossible, a thorough description of all factors that might introduce bias is of paramount importance.
Methodological aspects of this review We stated before that is difficult to define 'psychosocial interventions'. We deliberately chose a rather conservative definition, and this has affected the inclusion of studies. For example, several studies we identified initially were not included because interventions did not consist of at least two standardised treatment sessions. However, we feel this is appropriate since we were interested psychosocial interventions that are not limited to brief advice. In other excluded studies, psychosocial interventions were delivered by general practitioners and other health professionals (in the United States, it is customary that both 'family physicians' and general internists work in primary care). We are confident though that these restrictions enabled us to make clear assessments of the available evidence: a broader inclusion of studies would have resulted in even more incomparability among studies, adding no information or biased information to the evidence gathered in this review.
Another important issue has been addressed by Van Tulder (Van Tulder 2001) when he argued that "it is questionable whether the criteria list [...] evaluates the quality of the study or the quality of the publication". We used any additional information that was provided by authors on request to score quality criteria. Since we mostly addressed authors in case additional information on the intervention was needed to determine eligibility, the use of unpublished information might have been in favour of those studies in which descriptions of the intervention were less clear. This illustrates the need for clear guidelines as proposed in the CONSORT statement. Or, as members of the CONSORT group have stated it: "Despite several decades of educational efforts, the reporting of RCTs needs improvement" (Moher 2001).
Summary The results of this review do not allow an overall conclusion concerning the effectiveness of "psychosocial interventions by general practitioners". The available evidence addressed different psychosocial interventions for five distinct disorders or health complaints. The results of problem‐solving treatment by general practitioners seem promising for major depression, although the effectiveness in routine practice settings remains to be seen. The evidence for the remaining interventions (reattribution or cognitive behavioural group therapy for somatisation, counselling for smoking cessation, behavioural interventions to reduce alcohol reduction, cognitive behavioural therapy for unexplained fatigue) is either limited or conflicting. This finding can partly be explained by the incomparability of interventions and the small number of included studies. Therefore, the evidence has to be interpreted with caution: there is no strong evidence for the effectiveness of these interventions nor for the lack of effectiveness. The methodological quality of studies was fairly satisfactory, although most studies reported poorly on relevant study characteristics that are likely to influence the validity of results.
Authors' conclusions
Implications for practice.
The research question in this review was: "are psychosocial interventions delivered by general practitioners effective?". The underlying question for daily practice was: "is it commendable to have general practitioners deliver psychosocial interventions?". The answer to both questions is that it remains to be seen. There is a void of evidence‐based knowledge: due to a small number of available studies and incomparability among psychosocial interventions, the evidence for the use of such interventions is mostly limited and does not allow general conclusions concerning the effectiveness, or ineffectiveness, of psychosocial interventions by general practitioners. Problem‐solving treatment by highly experienced GPs seems a promising tool in the treatment of depressed patients, although the effectiveness of this intervention by regular GPs in routine care remains to be demonstrated.
Most psychological or psychosocial problems in primary care are vague and diffuse by nature, as opposed to the well‐defined and often diagnosed problems that are treated in specialist care. The moderate or limited evidence for psychosocial interventions presented here is restricted to a handful of well‐defined health complaints. Evidence on the effectiveness of psychosocial tools that are more suitable for the broad range of psychosocial complaints typically observed in primary care was not identified in this review. This too should be considered a void of knowledge.
In our view, the lack of evidence does not imply that GPs should be discouraged from delivering psychosocial interventions. One way to improve 'medicine‐based‐evidence' (Knottnerus 1997) is to promote the use of psychosocial interventions by general practitioners and collect the experiences from daily practice. However, the time consumption and related costs of these interventions might be a problem in general practice, especially if interventions turn out to be ineffective. Also, little is known about the potential harm GP‐delivered psychosocial interventions might cause. From a common sense standpoint, the answer to whether or not GPs should experiment with psychosocial interventions depends largely on the time available in the daily practice of GPs, the costs involved, the personal interest and competence of GPs and the prevalence of psychosocial complaints in primary care.
Implications for research.
Based on the findings in this review, several recommendations for future research can be made:
A possible explanation for the limited number of available studies in this review could be that psychosocial interventions are not considered to be helpful tools in general practice. A first step in future research should be to assess the need for GPs to have the use of psychosocial interventions at their disposal in the first place. If so, more empirical studies are needed. Secondly, results from a recent systematic review suggested that nurse practitioners can provide care equivalent to the care of GPs (Horrocks 2002). Since nurse practitioners emerged as possible counterparts of GPs in this review, future studies could investigate who is most suited to be the provider of psychosocial interventions in primary care.
Although a comparison between studies in this review is not justified, it seems that psychosocial interventions are most promising in the treatment of psychological problems like depression and somatisation. Future research that will contribute to a higher level of evidence for the effectiveness of problem‐solving treatment for depression and cognitive behavioural interventions for somatisation is helpful in that respect.
It is the reviewers' opinion that future research should also concentrate on more general psychosocial interventions or "tools" that are applicable for a wide range of problems observed in primary care (e.g. depressive symptoms, generalised anxiety, functional or unexplained symptoms). Highly specialised interventions such as cognitive behavioural therapy might be too time‐consuming and complicated to be delivered by GPs in routine practice.
A prerequisite for the building of evidence for any intervention is that articles reporting the effectiveness of studies contain high‐quality descriptions of all aspects that are relevant for the interpretation of results. As has been stated earlier, this prerequisite applies to this particular field of research especially. Future RCTs should especially assess and describe the supervision, training and monitoring of GPs, all aspects concerning patient compliance and the actual care received in all conditions (content of usual care, co‐interventions). Furthermore, future RCTs should ideally contain study samples large enough to include several subgroups of primary care patients.
What's new
| Date | Event | Description |
|---|---|---|
| 15 December 2008 | Amended | Author name amended |
History
Protocol first published: Issue 1, 2002 Review first published: Issue 2, 2003
| Date | Event | Description |
|---|---|---|
| 5 November 2008 | Amended | Converted to new review format. |
| 8 May 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
The reviewers would like to thank the following persons:
The CCDAN Editorial Team, Nancy Rowland (UK), Peter Bower (UK) and Raymond Ostelo (Netherlands) for their support, information and advice on how to conduct a review properly.
Nettie Blankenstein (Netherlands), Michael King (UK), Marta Buszewicz (UK), Oliver Davidson (UK), Ingrid Arnold (Netherlands), Ulrik Malt (Norway) and Jose Catalan (UK) for responding to our requests for (additional) information and study data.
This study was funded by the Health Research and Development Council (ZorgOnderzoek Nederland), The Netherlands.
Data and analyses
Comparison 1. problem solving versus antidepressant treatment at 12‐week follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 recovered cases (hamilton rating scale =< 7) | 2 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.62, 1.39] |
| 2 hamilton rating scale (depression) | 2 | 131 | Mean Difference (IV, Random, 95% CI) | 0.77 [‐2.45, 4.00] |
| 3 beck depression inventory (depression) | 2 | 131 | Mean Difference (IV, Random, 95% CI) | ‐1.12 [‐4.75, 2.51] |
1.1. Analysis.
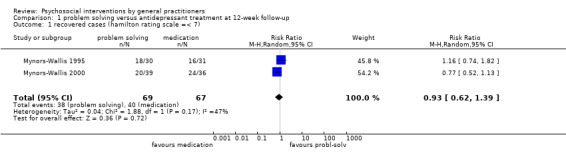
Comparison 1 problem solving versus antidepressant treatment at 12‐week follow‐up, Outcome 1 recovered cases (hamilton rating scale =< 7).
1.2. Analysis.
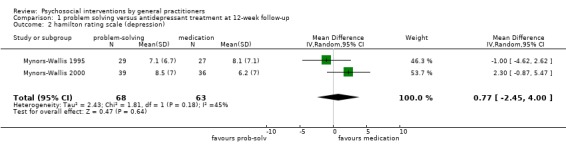
Comparison 1 problem solving versus antidepressant treatment at 12‐week follow‐up, Outcome 2 hamilton rating scale (depression).
1.3. Analysis.
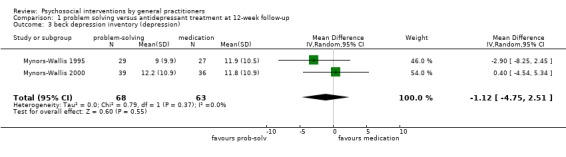
Comparison 1 problem solving versus antidepressant treatment at 12‐week follow‐up, Outcome 3 beck depression inventory (depression).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Blankenstein 2001.
| Methods | RCT to compare two conditions. Randomisation performed on practice level. Assessments on three occasions: baseline, 1 and 2 years. | |
| Participants | 162 patients (aged 20‐45) who were true or part somatisers (frequent GP attenders, 15 visits or more in 3 years and 5 or more somatisation symptoms) recruited from 20 GPs in 17 practices. Therapists: 10 GPs. | |
| Interventions | T (n:75) = tailored and modified reattribution intervention (dealing with illness worry, feeling understood, broadening the agenda, making the link) and care as usual, 2‐3 10‐30‐min sessions. C (n:87)= care as usual. Therapists received 20‐hr training programme (application intervention, feedback on audiotaped consultations) and booster sessions in first year. Supervision of therapists unknown. | |
| Outcomes | Two year follow‐up: complete attribution achieved in 33 of 51 patients. T superior to C on all primary outcomes: medical consumption, subjective health (VAS), sick leave. No complete recovery in either groups (not supported by data). | |
| Notes | non‐compliance: T=24/75. withdrawal: T=7/75, C=6/87. no integrity check. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Huibers 2004.
| Methods | RCT to compare two conditions. Randomisation on patient level according to randomised consent design. Assessments on four occasions: baseline, 4, 8 and 12 months. | |
| Participants | 151 patients (aged 18‐65) with severe fatigue (CIS =>35) and complete absenteeism (6‐26 weeks), recruited from an occupational health service. Therapists: 9 research GPs. | |
| Interventions | T (n:76) = brief ‐cognitive behavioural therapy, 5‐7 30‐min sessions in 4 months. C (n:75) = no treatment or usual care by own GP. Therapists (GPs) received 10‐h training in CBT (workshops, role playing), use of training manual, 2‐monthly supervision by experienced behaviour therapist throughout trial. | |
| Outcomes | At all time points (4,8, and 12 months): no sign. differences between groups on fatigue (CIS), absenteeism, clinical recovery (reduced fatigue plus work resumption) or any other outcome. Recovered cases (CIS <35 plus work resumption): T=23/76, C=29/75 (no significant differences). | |
| Notes | non‐compliance: T=20/76 withdrawal: T=6/76, C=7/76 (12 months) integrity check performed and published. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Larisch 2004.
| Methods | RCT to compare two conditions. Randomisation on GP level. Assessments on four occasions: baseline, 3, 6 and 12 months. | |
| Participants | 127 somatizing patients (aged 18‐65) (symptoms om SOMS 4=>; GHQ =>2), recruited from 37 practices. Therapists: 20 experimental GPs, 17 control GPs . | |
| Interventions | T (n:73) = routine ppc plus additional training in reattribution. C (n:75) = routine psychosocial primary care (ppc), based on 80‐h training for GPs aimed at psychosocial problems. Both groups: 6 20‐min sessions in 3 months. Therapists (GPs) in T received 12‐h additional training in reattribution (video feedback, role playing, modeling). Use of training manual, no supervision throughout trial. | |
| Outcomes | 3 month follow‐up: no sign. differences on physical symptoms (SOMS), anxiety and depression (HADS), quality‐of‐life (SF‐12) or mental health (GHQ). 6 month follow‐up: no sign. differences, except in number of physical symptoms (SOMS). 12 month follow‐up: results not accurately described. | |
| Notes | non‐compliance: unknown. withdrawal: T=29/73, C=20/54 (12 months). no integrity check. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Lidbeck 1997.
| Methods | RCT to compare two conditions. Randomisation biased towards more patients in experimental group. Assessments on three occasions: baseline, 2 and 6 months. | |
| Participants | 50 patients (aged 30‐60) with somatisation disorder (unexplained somatic symptoms and 1 or more symptoms meeting ICHPPC criteria for specific functional disorders) recruited from GPs and other physicians in an out‐patient clinic. Therapist: 1 research GP. | |
| Interventions | T (n:33) = group cognitive behavioural therapy (focus on reducing dread, physical examination, patient education, cognitive restructuring, relaxation training), 8 3‐hr sessions in 2 months. C (n:17) = waiting list. Therapist received training in stress relaxation. Supervision of therapist unknown. | |
| Outcomes | 6 month follow‐up: T superior to C on illness behaviour (IBQ), hypochondriasis (Whitley index), and medication use. No sign. differences on social problems (SPQ), anxiety (HAD), depression (HAD), sleep (SDI). | |
| Notes | non‐compliance: T=1/32. withdrawal: T=1/32,C=unknown. no integrity check. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
McIntosh 1997.
| Methods | RCT to compare three conditions. Assessments on four occasions: baseline, 3, 6 and 12 months. | |
| Participants | 159 patients (aged 15 or older) with high alcohol consumption (one or more CAGE items or 4 or more standard drinks each day in 28 days) recruited by nurse in family practice centre. Therapists: 1 research GP (and 1 nurse practitioner). | |
| Interventions | T1 (n:40) = cognitive behavioural intervention (CBI) by research GP (basic information, help understanding function alcohol, plan of action, moderation strategies, use of daily drinking records and self‐help manual), 2 30‐min sessions over 2 weeks. T2 (n:66) = CBI by research nurse practitioner, 2 30‐min sessions over 2 weeks. C (n:53) = brief advice by own GP (1 of 12) on drinking, 1 5‐min session. Training or supervision of therapists unclear. | |
| Outcomes | 12 month follow‐up: no sign. differences between groups (overall reduction in drinking and alcohol‐related problems in all groups). | |
| Notes | non‐compliance: T1&T2=27/106. withdrawal: T1&T2&C=16/159. no integrity check. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Mynors‐Wallis 1995.
| Methods | RCT to compare three conditions. Randomisation is stratified (severity of depression). Assessments on three occasions: baseline, 6 and 12 weeks. | |
| Participants | 91 patients (aged 18‐65) with major depression (research criteria for major depression and Hamilton rating scale score 13 or more) recruited from 26 GPs in 15 practices . Therapists: 2 research GPs (and 1 psychiatrist). | |
| Interventions | T1 (n:30) = problem solving treatment (PST) (explanation rationale, emotional symptoms are caused by problems in living that can be dealt with; identification problems; stages of PST explained). T2 (n:31) = amitriptyline (50 mg‐150 mg) and general support. C (n:30) = placebo and general support. All groups: 6 30‐60‐min sessions in 12 weeks. Therapists received training in PST( theory, role playing, treating five patients under supervision) and drug administration. Supervision of therapists unknown. | |
| Outcomes | 12 week follow‐up: T1 superior to C on depression (BDI and Hamilton) and social functioning (SAS). No sign. difference on psychological symptoms (PSE). No sign. differences between T1 and T2. Recovered cases (Hamilton <8): T1=18/30, T2=16/31, C=8/30 (difference T1 and C significant). Patient satisfaction ("T is (very) helpful"): T1=28/30, T2=21/31. | |
| Notes | non‐compliance: T1=2/30, T2=6/31, C=18/30. withdrawal (82 patients included in analysis): T1=1/29, T2=2/27, C=14/26. no integrity check. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Mynors‐Wallis 2000.
| Methods | RCT to compare four conditions. Randomisation is stratified (severity of depression). Assessments on four occasions: baseline, 6, 12 and 52 weeks. | |
| Participants | 151 patients (aged 18‐65) with major depression (research criteria for major depression, Hamilton rating scale score 13 or more, minimum illness duration 4 weeks) referred by 24 GPs. Therapists: 3 research GPs (and 2 practice nurses). | |
| Interventions | T1 (n:39) = problem solving treatment (PST) by GP (stages: clarification of problems, choice of goals, generation of solutions, choice of solutions, implementation of solutions, evaluation). T2 (n:41) = PST by practice nurse. T3 (n:36) = fluvoxamine (100 mg) or paroxetine (20 mg) and general support. T4 (n:35) = combination treatment (medication by GP and PST by nurse). All groups: 6 30‐60‐min sessions in 12 weeks (except T4=12 sessions). Therapists (GPs) received training in PST (theory, treating five patients under supervision), training manual and were supervised throughout trial. | |
| Outcomes | 52 week follow‐up: no sign. differences between groups on depression (BDI, Hamilton), psychological symptoms (clinical interview schedule) or social functioning (SAS). Recovered cases (Hamilton <8): T1=24/39, T2=23/41, T3=20/36, T4=23/35 (no significant differences). | |
| Notes | non‐compliance: T1=14/39, T2=9/41, T3=6/36, T4=6/35. withdrawal: T1=14/39, T2=13/41, T3=6/36, T4=5/35. no integrity check. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Richmond 1985.
| Methods | CCT to compare two conditions. Group allocation according to day of entry in study. Assessments on two occasions: baseline and 6 months. | |
| Participants | 200 patients (aged 16‐65) who smoked recruited from 4 GPs in one practice. Therapists: three GPs. | |
| Interventions | T (n:100) = smoking cessation counselling (use of 1 wk diary of smoking habits and self‐help manual, information on effects of smoking, strategy for maintaining abstinent, discussing alternatives, withdrawal symptoms, weight management, risks of smoking, benefits of abstinence, problems encountered), 6 sessions (duration?) in 6 months. C (n:100) = usual care and use of 1 wk diary of smoking habits, 2 sessions (duration?) in 6 months. Training or supervision of therapists unknown. | |
| Outcomes | 6 month follow‐up: abstinence T=33/100, C=3/100 | |
| Notes | non‐compliance: T=25/100, C=23/100. withdrawal (non‐compliers analysed as smokers): T=25/100, C=23/100. no integrity check. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Richmond 1995.
| Methods | CCT to compare four conditions. Group allocation according to weekly blocks. Assessments on three occasions: baseline, 6 and 12 months. | |
| Participants | 378 patients (aged 18‐70) with high weekly alcohol consumption (men > 35 drinks, women > 21) recruited from 119 GPs in 40 practices. Therapists: 119 GPs. | |
| Interventions | T1 (n:96) = behavioural change programme 'Alcoholscreen' (use of self‐help manual and diary, education, counselling, advice on changing drinking behaviour, supporting new drinking habits), 5 5‐25‐min sessions in 5 months. T2 (n:96) = brief advice to reduce drinking, 1 5‐min session. C1(n:93) = assessment of drinking behaviour and follow‐up only. C2 (n:93) = follow‐up only. All GPs received training, supervision unknown. | |
| Outcomes | 12 month follow‐up (not available for C2): No sign. differences between groups in % patients reporting drinking above predefined weekly level (men < 28 drinks, women < 14) or alcohol‐related problems (MAST). T1 superior to other treatments on alcohol consumption below level for patients who attended 2 sessions or more. | |
| Notes | non‐compliance: T1=49/96 2nd visit, 92/96 5th visit. withdrawal: T1=30/96, T2=26/96, C1=32/93 (C2 unavailable). no integrity check. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Segnan 1991.
| Methods | RCT to compare four conditions. Assessments on three occasions: baseline, 6 and 12 months. | |
| Participants | 923 patients (aged 20‐60) who were smokers free of a life‐threatening disease recruited by 44 GPs. Therapists: 44 GPs. | |
| Interventions | T1 (n:275) = repeated counselling (RC) (use of brochure, reinforcement antismoking message), 5 sessions (duration?) in 9 months. T2 (n:294) = RC plus prescription of nicotine gum. T3 (n:292) = RC plus spirometric test, results discussed by GP. C (n:62) = minimal intervention (counselling and use of brochure), 1 session. Therapists received 2 3‐hr training sessions (introduction counselling techniques), 40% of GPs attended both sessions. Supervision of therapists unknown. | |
| Outcomes | 12 month follow‐up: No sign. differences between groups on % biochemically verified quitters, overall low quit rates (4.8‐7.5%). | |
| Notes | non‐compliance: approx. 66% attended less than 4 sessions. withdrawal: total N=129/923. integrity check: GP compliance with treatment protocol: RC=67.3%; RC+gum=92.5%; RC+spiro=83.7%; MI=75%. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Anderson 1992 | intervention only one session |
| Baillargeon 1998 | no RCT, CCT, or CPPT (single‐case experimental design) |
| Barkham 1989 | intervention not performed by GP |
| Beusterien 2000 | no psychosocial intervention (information only) |
| Blomhoff 2001 | intervention performed by GPs, non‐specialist physicians and psychiatrists (no separate analysis) |
| Bowman 2000 | no psychosocial intervention (telephone assessment) |
| Brody 1990 | intervention only one session |
| Calfas 1996 | intervention only one session |
| Catalan 1984 | less than two standardised face‐to‐face contacts |
| Durand 2002 | no psychosocial intervention (self‐help manual) |
| Fleming 1997 | intervention performed by GPs and general internists (no separate analysis) |
| Fleming 1999 | intervention performed by GPs and general internists (no separate analysis) |
| Gask 1992 | no RCT, CCT or CPPT (narrative review) |
| Goldstein 1999 | intervention performed by GPs and general internists (no separate analysis) |
| Heatley 2005 | no data on outcomes in patients |
| Horst 1997 | less than two standardised face‐to‐face contacts (second contact merely optional) |
| Issakidis 1999 | intervention not performed by GP |
| Katzelnick 2000 | no psychosocial intervention (pharmacotherapy) |
| King 1998 | no psychosocial intervention (education of GPs) |
| King 2002 | no standardised number of face‐to‐face contacts (effects of training rather than effects of applying intervention) |
| Kottke 1989 | no psychosocial intervention (advice and information only) |
| Malt 1999 | intervention only in combination with (placebo) pharmacotherapy |
| McLeod 1997 | intervention not performed by GP |
| Morriss 1999 | no RCT, CCT or CPPT (before‐ and after‐training study) |
| Ockene I 1999 | intervention not performed by GP |
| Ockene J 1991 | intervention not performed by GP |
| Patel 1988 | intervention performed by GP in combination with intervention by nurse (no separate analysis) |
| Peveler 1999 | intervention not performed by GP |
| Pill 1998 | intervention performed by GPs and nurses (no separate analysis) |
| Scott 1997 | intervention not performed by GP |
| Simkin 1997 | intervention performed by GPs and general internists (no separate analysis) |
| Skinner 1984 | intervention not performed by GP |
| Swinson 1992 | intervention not performed by GP (not even in primary care) |
| Wadden 1997 | intervention not performed by GP |
| Wallace 1988 | no psychosocial intervention (advice and information only) |
| White 1990 | intervention not performed by GP |
| Whitehead 2002 | no standardised face‐to‐face contacts required |
| Wilson 1988 | intervention only in combination with nicotine gum |
Characteristics of ongoing studies [ordered by study ID]
Arnold 2006.
| Trial name or title | Treatment of somatoform disorders with cognitive behaviour therapy by general practitioners |
| Methods | |
| Participants | 100 patients who apply to criteria for somatoform disorder and who report severe functional impairment and complaints for more than six months. |
| Interventions | T (n:50) = cognitive behaviour therapy (5 45‐min sessions in 5 months) by 8 research GPs who treat 5‐8 patients. GPs are trained and supervised. C (n:50) = usual care. |
| Outcomes | main outcomes: frequency and intensity of main complaint, functional impairment and medical consumption assessed on three occasions (baseline, 6 and 12 months). |
| Starting date | January 2000 (expected finishing date = July 2004). |
| Contact information | I. Arnold, UMC Leiden, The Netherlands (I.A.Arnold@lumc.nl) |
| Notes |
Contributions of authors
Marcus Huibers (MH) and Anna Beurskens (AB) identified and selected all studies. In case of doubt, they consulted Gijs Bleijenberg (GB) for advice on the selection of studies. AB and GB assessed the methodological quality of selected studies and performed the data extraction. Aim was to reach consensus on methodological quality and the results from the data extraction. MH was involved as a third reviewer when lack of consensus persisted between AB and GB. MH performed the data analysis and reported the results. Onno van Schayck acted as advisor throughout the entire process. All authors are responsible for the results of this review and contributed to the final manuscript.
Sources of support
Internal sources
No sources of support supplied
External sources
Health Research and Development Council (ZorgOnderzoek Nederland), Netherlands.
Declarations of interest
There is no potential conflict of interest.
Edited (no change to conclusions)
References
References to studies included in this review
Blankenstein 2001 {published data only}
- Blankenstein AH, Horst van der HE, Schilte AF, Portegijs PJM, Knottnerus JA, Eijk van JTM ET AL. Effectiveness of reattribution for somatisation in general practice, a randomised controlled trial. Somatising patients in general practice (PhD thesis). Amsterdam: AH Blankenstein, 2001:49‐65. [Google Scholar]
Huibers 2004 {published data only}
- Bazelmans E, Huibers MJH, Bleijenberg G. Did cognitive behaviour therapy by general practitioners for unexplained fatigue among employees not work because of the delivery of the intervention?. Behavioural and Cognitive Psychotherapy 2005;33:225‐35. [Google Scholar]
- Huibers MJH, Beurskens AJHM, Schayck CP, Bazelmans E, Metsemakers JFM, Knottnerus JA, et al. Efficacy of cognitive‐behavioural therapy by general practitioners for unexplained fatigue among employees. British Journal of Psychiatry 2004;184:240‐6. [DOI] [PubMed] [Google Scholar]
Larisch 2004 {published data only}
- Larisch A, Schweickhardt A, Wirsching M, Fritzsche K. Psychosocial interventions for somatizing patients by the general practitioners: a randomized controlled trial. Journal of Psychosomatic Research 2004;57:507‐14. [DOI] [PubMed] [Google Scholar]
Lidbeck 1997 {published data only}
- Lidbeck J. Group therapy somatization disorders in general practice: effectiveness of a short cognitive‐behavioural treatment model. Acta Psychiatrica Scandinavia 1997;96:14‐24. [DOI] [PubMed] [Google Scholar]
McIntosh 1997 {published data only}
- McIntosh MC, Leigh G, Baldwin NJ, Marmulak J. Reducing alcohol consumption: comparing three brief methods in family practice. Canadian Family Physician 1997;43:1959‐67. [PMC free article] [PubMed] [Google Scholar]
Mynors‐Wallis 1995 {published data only}
- Mynors‐Wallis LM, Gath DH, Lloyd‐Thomas AR, Tomlinson D. Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. BMJ 1995;310:441‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mynors‐Wallis 2000 {published data only}
- Mynors‐Wallis LM, Gath DH, Day A, Baker F. Randomised controlled trial of problem solving treatment, antidepressant medication and combined treatment for major depression in primary care. BMJ 2000;320:26‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Richmond 1985 {published data only}
- Richmond RL, Webster IW. A smoking cessation programme for use in general practice. Medical Journal of Australia 1985;142:190‐4. [PubMed] [Google Scholar]
Richmond 1995 {published data only}
- Richmond R, Heather N, Wodak A, Kehoe L, Webster I. Controlled evaluation of a general practice‐based brief intervention for excessive drinking. Addiction 1995;90:119‐32. [DOI] [PubMed] [Google Scholar]
Segnan 1991 {published data only}
- Segnan N, Pont A, Battista RN, Senore C, Rosso S, Shapiro SH, Aimar D. A randomized trial of smoking cessation interventions in general practice in Italy. Cancer Causes and Control 1991;2:239‐46. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Anderson 1992 {published data only}
- Anderson P, Scott E. The effect general practitioners' advice to heavy drinking men. British Journal of Addiction 1992;87:891‐900. [DOI] [PubMed] [Google Scholar]
Baillargeon 1998 {published data only}
- Baillargeon L, Demers M, Ladouceur R. Stimulus‐control: nonpharmacologic treatment for insomnia. Canadian Family Physician 1998;44:73‐9. [PMC free article] [PubMed] [Google Scholar]
Barkham 1989 {published data only}
- Barkham M. Brief prescriptive therapy in two‐plus‐one sessions: initial cases from the clinic. Behavioural Psychotherapy 1989;17:161‐75. [Google Scholar]
Beusterien 2000 {published data only}
- Beusterien K, Buesching D, Robison R, Keats M, Tomlinson J, Cofran K, et al. Evaluation of an information exchange program for primary care patients with depression. Disease Management 2000;3:1‐9. [Google Scholar]
Blomhoff 2001 {published data only}
- Blomhoff S, Haug TT, Hellström K, Holme I, Humble M, Madsbu H, et al. Randomised controlled general practice trial of sertraline, exposure therapy and combined treatment in generalised social phobia. British Journal of Psychiatry 2001;179:23‐30. [DOI] [PubMed] [Google Scholar]
- Haug TT, Blomhoff S, Hellstrom K, Holme I, Humble M, Madsbu HP, et al. Exposure therapy and sertraline in social phobia: 1‐year follow‐up of a randomised controlled trial. British Journal of Psychiatry 2003;182:312‐8. [DOI] [PubMed] [Google Scholar]
- Haug TT, Hellström K, Blomhoff S, Humble M, Madsbu HP, Wold JE. The treatment of social phobia in general practice: is exposure therapy feasible. Family Practice 2000;17:114‐8. [DOI] [PubMed] [Google Scholar]
Bowman 2000 {published data only}
- Bowman M, Dignan M, Crandall S, Baier M. Changes in functional status related to health maintenance visits to family physicians. Journal of Family Practice 2000;49:428‐33. [PubMed] [Google Scholar]
Brody 1990 {published data only}
- Brody D, Lerman C, Wolfson H, Caputo G. Improvement in physician's counseling of patients. Archives of Internal Medicine 1990;150:993‐998. [PubMed] [Google Scholar]
Calfas 1996 {published data only}
- Calfas K, Long B, Sallis J, Wooten W, Pratt M, Patrick K. A controlled trial of physician counseling to promote the adoption of physical activity. Preventive Medicine 1996;25:225‐33. [DOI] [PubMed] [Google Scholar]
Catalan 1984 {published data only}
- Catalan J, Gath D, Bond A, Martin P. The effects of non‐prescribing anxiolytics in general practice II. Factors associated with outcome. British Journal of Psychiatry 1984;144:603‐10. [DOI] [PubMed] [Google Scholar]
- Catalan J, Gath D, Edmonds G, Ennis J. The effects of non‐prescribing of anxiolytics in general practice: I. controlled evaluation of psychiatric and social outcome. British Journal of Psychiatry 1984;144:593‐602. [DOI] [PubMed] [Google Scholar]
Durand 2002 {published data only (unpublished sought but not used)}
- Durand M, King M. Specialist treatment versus self‐help for bulimia nervosa: a randomised controlled trial in general practice. personal communication 2002. [PMC free article] [PubMed]
Fleming 1997 {published data only}
- Fleming M, Lawton Barry K, Baier Manwell L, Johnson K, London R. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community‐based primary care practices. JAMA 1997;277:1039‐45. [PubMed] [Google Scholar]
Fleming 1999 {published data only}
- Fleming M, Baier Manwell L, Lawton Barry K, Adams W, Stauffacher E. Brief physician advice for alcohol problems in older adults: a randomized community‐based trial. Journal of Family Practice 1999;48:378‐84. [PubMed] [Google Scholar]
Gask 1992 {published data only}
- Gask L. Training general practitioners to detect and manage emotional disorders. International Review of Psychiatry 1992;4:293‐300. [Google Scholar]
Goldstein 1999 {published data only}
- Goldstein M, Pinto, Marcus B, Lynn H, Jette A, Rakowski W. Physician‐based physical activity counseling for middle‐aged and older adults: a randomized trial. Annals of Behavioural Medicine 1999;21:40‐7. [DOI] [PubMed] [Google Scholar]
- Marcus B, Goldstein M, Jette A, Simkin‐Silverman L, Pinto B, Milan F, et al. Training physicians to conduct physical activity counseling. Preventive Medicine 1997;26:382‐8. [DOI] [PubMed] [Google Scholar]
- Pinto B, Goldstein M, DePue J, Milan F. Acceptability and feasibility of physician‐based activity counseling. American Journal of Preventive Medicine 1998;15:95‐102. [DOI] [PubMed] [Google Scholar]
Heatley 2005 {published data only}
- Heatley C, Ricketts T, Forrest J. Training general practitioners in cognitive behavioural therapy for panic disorder: randomized‐controlled trial. Journal of Mental Health 2005;14:73‐82. [Google Scholar]
Horst 1997 {published data only}
- Horst HE van der, Eijk JTM van, Schellevis FG, Devillé WLJM. The effectiveness of patient education and promotion of self‐care for patients with irritable bowel syndrome in primary care. Irritable bowel syndrome in general practice: how effective is patient education and counselling? (PhD thesis). Amsterdam: HE van der Horst, 1997. [Google Scholar]
Issakidis 1999 {published data only}
- Issakidis C, Sanderson K, Teesson M, Johnston S, Buhrich N. Intensive case management in Australia: a randomized controlled trial. Acta Psychiatrica Scandinavia 1999;99:360‐7. [DOI] [PubMed] [Google Scholar]
Katzelnick 2000 {published data only}
- Katzelnick D, Simon G, Pearson S, Manning W, Helstad C, Henk H, et al. Randomized trial of a depression management program in high utilzers of medical care. Archives of Family Medicine 2000;9:345‐51. [DOI] [PubMed] [Google Scholar]
King 1998 {published data only}
- King M, Hindler C, Nazareth I, Farmer R, Gerada C, Cohen J. A controlled evaluation of small group education of general practitioners in the management of drug users. British Journal of General Practice 1998;48:1159‐60. [PMC free article] [PubMed] [Google Scholar]
King 2002 {published data only}
- Davidson O, King M, Sharpe D, Taylor F. A pilot randomized trial evaluating GP registrar management of major depression following brief training in cognitive behaviour therapy. Education for General Practice 1999;10:485‐8. [Google Scholar]
- King M, Davidson O, Taylor F, Haines A, Sharp D, Turner R. Effectiveness of teaching general practitioners skills in brief cognitive behaviour therapy to treat patients with depression: randomised controlled trial. BMJ 2002;324:947‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kottke 1989 {published data only}
- Kottke T, Brekke M, Solberg L, Hughes J. A randomized trial to increase smoking intervention by physicians: doctors helping smokers, round I. JAMA 1989;261:2101‐6. [PubMed] [Google Scholar]
Malt 1999 {published data only}
- Malt UF. The antidepressant debate. British Journal of Psychiatry 2002. [DOI] [PubMed]
- Malt UF, Robak OH, Madsbu HP, Bakke O, Loeb M. The Norwegian naturalistic treatment study of depression in general practice (NORDEP)‐I: randomised double blind study. BMJ 1999;318:1180‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
McLeod 1997 {published data only}
- McLeod C, Budd M, McClelland. Treatment of somatization in primary care. General Hospital Psychiatry 1997;19:251‐8. [DOI] [PubMed] [Google Scholar]
Morriss 1999 {published data only}
- Morriss R, Gask L, Ronalds C, Downes‐Grainger E, Thompson H, Leese B, et al. Clinical and patient satisfaction outcomes of a new treatment for somatized mental disorders taught to general practitioners. British Journal of General Practice 1999;49:263‐7. [PMC free article] [PubMed] [Google Scholar]
- Morriss R, Gask L, Ronalds C, Downes‐Grainger E, Thompson H, Leese B, et al. Cost‐effectiveness of new treatment for somatized mental disorder taught to GPs. Family Practice 1998;15:119‐25. [DOI] [PubMed] [Google Scholar]
Ockene I 1999 {published data only}
- Ockene I, Hebert J, Ockene J, Merriam P, Hurley T, Saperia G. Effect of training and a structured office practice on physician‐delivered nutrition counseling: the Worcester Area Trial for Counseling in Hyperlipidemia (WATCH). American Journal of Preventive Medicine 1996;12:252‐8. [PubMed] [Google Scholar]
- Ockene I, Hebert J, Ockene J, Saperia G, Stanek E, Nicolosi R. Effect of physician‐delivered nutrition counseling training and an office‐support program on saturated fat intake, weight, serum lipid measurements in a hyperlipidemic population: Worcester Area Trial for Counseling in Hyperlipidemia (WATCH). Archives of Internal Medicine 1999;159:725‐31. [DOI] [PubMed] [Google Scholar]
- Ockene J, Ockene I, Quirk M, Hebert J, Saperia G, Luippold R, et al. Physician training for patient‐centered nutrition counseling in a lipid intervention trial. Preventive Medicine 1995;24:563‐70. [DOI] [PubMed] [Google Scholar]
Ockene J 1991 {published data only}
- Ockene J, Kristeller J, Goldberg R, Amick T, Pekow P, Hosmer D, et al. Increasing the efficacy of physician‐delivered smoking interventions: a randomized clinical trial. Journal of General Internal Medicine 1991;6:1‐8. [DOI] [PubMed] [Google Scholar]
- Ockene J, Kristeller J, Pbert L, Hebert J, Luippold R, Goldberg R, et al. The physician‐delivered smoking intervention project: can short‐term interventions produce long‐term effects for a general outpatient population?. Health Psychology 1994;13:278‐81. [DOI] [PubMed] [Google Scholar]
Patel 1988 {published data only}
- Patel C, Marmot M. Can general practitioners use training in relaxation and management of stress to reduce mild hypertension. BMJ 1988;296:21‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peveler 1999 {published data only}
- Peveler R, George C, Kinmonth A, Campbell M, Thompson C. Effect of antidepressant drug counselling and information leaflets on adherence to drug treatment in primary care: randomised controlled trial. BMJ 1999;319:612‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pill 1998 {published data only}
- Pill R, Stott NCH, Rollnick SR, Rees M. A randomized controlled trial of an intervention designed to improve the care given in general practice to type II diabetic patients: patient outcomes and professional ability to change behaviour. Family Practice 1998;15:229‐35. [DOI] [PubMed] [Google Scholar]
- Stott NCH, Rollnick S, Rees MR, Pill RM. Innovation in clinical method: diabetes care and negotiating skills. Family Practice 1995;12:413‐8. [DOI] [PubMed] [Google Scholar]
Scott 1997 {published data only}
- Scott C, Tacchi M, Jones R, Scott J. Acute and one‐year outcome of a randomised controlled trial of brief cognitive therapy for major depressive disorder in primary care. British Journal of Psychiatry 1997;171:131‐4. [DOI] [PubMed] [Google Scholar]
Simkin 1997 {published data only}
- Simkin‐Silverman L, Wing R. Management of obesity in primary care. Obesity Research 1997;5:603‐12. [DOI] [PubMed] [Google Scholar]
Skinner 1984 {published data only}
- Skinner P. Skills not pills: learning to cope with anxiety symptoms. Journal of the Royal College of General Practitioners 1984;34:258‐60. [PMC free article] [PubMed] [Google Scholar]
Swinson 1992 {published data only}
- Swinson R, Soulios C, Cox B, Kuch K. Brief treatment of emergency room patients with panic attacks. American Journal of Psychiatry 1992;7:944‐6. [DOI] [PubMed] [Google Scholar]
Wadden 1997 {published data only}
- Wadden T, Berkowitz R, Vogt R, Steen S, Stunkard A, Foster G. Lifestyle modification in the pharmacologic treatment of obesity: a pilot investigation of a potential primary care approach. Obesity Research 1997;5:218‐26. [DOI] [PubMed] [Google Scholar]
Wallace 1988 {published data only}
- Wallace P, Cutler S, Haines A. Randomised controlled trial of general practitioner intervention in patients with excessive alcohol consumption. BMJ 1988;297:663‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
White 1990 {published data only}
- White J, Keenan M. Stress control: a pilot study of large group therapy for generalized anxiety disorder. Behavioural Psychotherapy 1990;18:143‐6. [Google Scholar]
Whitehead 2002 {published data only}
- Whitehead L, Campion P. Can general practitioners manage chronic fatigue syndrome? A controlled trial. Journal of Chronic Fatigue Syndrome 2002;10:55‐64. [Google Scholar]
Wilson 1988 {published data only}
- Wilson DM, Taylor W, Gilbert JR, Best A, Lindsay EA, Wilms DG, Singer J. A randomized trial of a family physician intervention for smoking cessation. JAMA 1988;260:1570‐4. [PubMed] [Google Scholar]
References to ongoing studies
Arnold 2006 {unpublished data only}
- Treatment of somatoform disorders with cognitive behaviour therapy by general practitioners. Ongoing study January 2000 (expected finishing date = July 2004)..
Additional references
Altman 1998
- Altman D. Confidence intervals for the number needed to treat. BMJ 1998;317:1309‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bower 2002
- Bower P, Rowland N, Mellor Clark J, Heywood P, Godfrey C, Hardy R. Effectiveness and cost effectiveness of counselling in primary care. Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI] [PubMed] [Google Scholar]
Brown 1995
- Brown C, Schulberg HC. The efficacy of psychosocial treatments in primary care: a review of randomised clinical trials. General Hospital Psychiatry 1995;17:414‐24. [DOI] [PubMed] [Google Scholar]
Cape 2000
- Cape J, Barker C, Buszewicz M, Pistrang N. General practitioner psychological management of common emotional problems (I): definitions and literature review. British Journal of General Practice 2000;50:313‐8. [PMC free article] [PubMed] [Google Scholar]
Chocron Bentata 1995
- Chocron Bentata L, Vilalta Franch J, Legazpi Rodriguez I, Auquer K, Franch L. Prevalence of psychopathology at a primary care center. Atencion Primaria 1995;16:586‐90, 592‐3. [PubMed] [Google Scholar]
Corney 1992
- Corney R. The effectiveness of counselling in general practice. International Review of Psychiatry 1992;4:331‐8. [Google Scholar]
Davison 2000
- Davison GC. Stepped care: doing more with less?. Journal of Consulting and Clinical Psychology 2000;68:580‐5. [PubMed] [Google Scholar]
Friedli 1996
- Friedli K, King M. Counselling in general practice, a review. Primary Care Psychiatry 1996;2:205‐16. [Google Scholar]
Gray 1988
- Gray DP. Counsellors in general practice. Journal of the Royal College of General Practitioners 1988;38:50‐1. [PMC free article] [PubMed] [Google Scholar]
Horrocks 2002
- Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 2002;324:819‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jadad 1996
- Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Controlled Clinical Trials 1996;17:1‐12. [DOI] [PubMed] [Google Scholar]
Knottnerus 1997
- Knottnerus JA, Dinant GJ. Medicine based evidence, a prerequisite for evidence based medicine. BMJ 1997;315:1109‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman DG, for the CONSORT Group. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomised trials. Lancet 2001;357:1191‐4. [PubMed] [Google Scholar]
Moncreiff 2001
- Moncreiff J, et al. Quality rating scale for RCT. International Journal of Methods in Psychiatric Research 2001;10:3. [Google Scholar]
Ostelo 2002
- Ostelo RWJG, Vet HCW de, Waddell G, Kerckhoffs MR, Leffers P, Tulder MW van. Rehabilitation following lumbar disc surgery. Cochrane Database of Systematic Reviews 2002, Issue 2. [DOI] [PubMed] [Google Scholar]
Richardson 1989
- Richardson JD. Sexual difficulties. A general practice specialty. Australian Family Physician 1989;18:200‐4. [PubMed] [Google Scholar]
Rowland 2000
- Rowland N, Godfrey C, Bower P, Mellor Clark J, Heywood P, Hardy R. Counselling for depression in primary care: a systematic review of the research evidence.. British Journal of Guidance and Counselling 2000;28(2):215‐31. [Google Scholar]
Silagy 2003
- Silagy C, Stead LF. Physician advice for smoking cessation. Cochrane Database of Systematic Reviews 2003, Issue 2. [DOI] [PubMed] [Google Scholar]
Terluin 1999
- Terluin B, Meijman FJ. What do Dutch GP's do when patients have psychosocial problems? [Wat doen Nederlandse huisartsen bij psychosociale problemen van hun patiënten?]. Huisarts en Wetenschap 1999;42:151‐2. [Google Scholar]
Tiemens 1996
- Tiemens BG, Ormel J, Simon GE. Occurence, recognition and outcome of pyschological disorders in primary care. American Journal of Psychiatry 1996;153:636‐44. [DOI] [PubMed] [Google Scholar]
Van Tulder 1997
- Tulder MW van, Assendelft WJ, Koes BW, Bouter LM. Method guidelines for systematic reviews in the cochrane collaboration back review group for spinal disorders. Spine 1997;22:2323‐30. [DOI] [PubMed] [Google Scholar]
Van Tulder 2001
- Tulder MW van, Ostelo RWJG, Vlaeyen JWS, Linton SJ, Morley SJ, Assendelft WJJ van. Behavioral treatment for chronic low back pain. Spine 2001;26:270‐81. [DOI] [PubMed] [Google Scholar]
Verhagen 1998
- Verhagen AP, Vet HC de, Bie RA de, Kessels AG, Boers M, Bouter LM, et al. The delphi list: a criteria list for quality asessment of randomized clinical trials for conducting systematic reviews developed by delphi consensus. Journal of Clinical Epidemiology 1998;51:1235‐41. [DOI] [PubMed] [Google Scholar]
Von Korff 2000
- Korff M, Tiemens BG. Individualized stepped care of chronic illness. Western Journal of Medicine 2000;172:133‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wessely 1999
- Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many?. Lancet 1999;354:936‐9. [DOI] [PubMed] [Google Scholar]


