Abstract
The availability of social support is associated with health outcomes after acute myocardial infarction (AMI), yet previous studies have largely considered social support as a single entity, rather than examining its discrete domains. Furthermore, few studies have investigated the impact of social support in older AMI patients, in whom it may be especially important. We aimed to determine the associations between 5 discrete domains of social support – emotional support, informational support, tangible support, positive social interaction, and affectionate support – with 6-month readmission and mortality in older patients hospitalized for AMI, adjusting for known predictors of post-AMI outcomes. 3006 participants 75 years and older were recruited from a network of 94 hospitals across the United States. A 5-item version of the Medical Outcomes Study Social Support Survey was used to measure perceived social support, and readmission and mortality were ascertained 6 months after initial hospitalization. Independent associations were determined using multivariable regression. Among 3006 participants, mean age was 82 years, 44% were female, and 11% non-white. Participants who were female, non-white, less educated, and lived alone tended to report lower social support. In multivariable analyses, low informational support was associated with readmission (odds ratio [OR], 1.22; 95% CI, 1.01-1.47), and low emotional support with mortality (OR, 1.43; 95% CI, 1.04-1.97). In conclusion, individual domains of social support had distinct, independent associations with post-AMI outcomes, lending a more nuanced and precise understanding of this important social determinant of health. Understanding these distinct associations can inform the development of interventions and policies to improve post-AMI outcomes.
Keywords: Social Support, Acute Myocardial Infarction, Older Adults, Hospitalization, Outcomes
Introduction
The availability of social support — the care and companionship one receives from others — has a well-documented effect on a variety health outcomes.1 Although social support is often considered a single entity, it may be informative to categorize social support into discrete components, since different forms of social support confer distinct benefits.1,2 One such categorization identifies 5 domains: emotional support; informational support; tangible support; positive social interaction; and affectionate support.3 Social support has an important influence on the recovery of patients following acute myocardial infarction (AMI), yet to our knowledge, no prior studies have compared the effects of multiple different domains of social support.4-14 Additionally, there are no contemporary large-scale studies that have explored this association in older adults. Our objective was to examine the associations between the aforementioned 5 domains of social support – emotional support, informational support, tangible support, positive social interaction, and affectionate support – with readmission and mortality in a large, contemporary cohort of older adult AMI survivors using data from the SILVER-AMI study.15 By elucidating the impact of social support on recovery from AMI, this study can inform the implementation of interventions to improve post-AMI outcomes.
Methods
The design of the Comprehensive Evaluation of Risk Factors in Older Patients with Acute Myocardial Infarction (SILVER-AMI) study [NHLBI: R01HL115295] has been previously described.15 The study received approval from the Yale Institutional Review Board (IRB), as well as IRBs at each of the participating study sites. Participants were recruited between January 2013 and October 2016 from a network of 94 community and academic hospitals across the United States. Inclusion criteria were age of 75 years and older and a diagnosis of AMI in accordance with the Third Universal Definition of Myocardial Infarction.16 Local site coordinators consecutively screened hospitalized older adults with elevated troponins and reviewed medical records to confirm the AMI diagnosis. Participants in this study were excluded if: their AMI was the result of an inpatient procedure or surgery; they were unable to complete the baseline or follow-up interview; they were transferred >48 hours from an outside hospital; they did not speak English or Spanish; or if they died during the index hospitalization, resulting in a sample size of 3006 participants. Written informed consent was obtained from each participant, or a proxy in the instance of diminished capacity to consent.
Site coordinators administered an interview and physical assessment during the participants’ hospitalization, including information on participant race, education, and cohabitation status. A research nurse at the Yale coordinating center abstracted medical record data on participant age, sex, comorbidities, and AMI characteristics. Yale investigators reviewed the admission records and electrocardiograms to confirm eligibility and classify the index AMI. These covariates were selected because of their recognized associations with post-AMI outcomes in the contemporary literature.17,18
We assessed perceived social support, the amount of social support an individual subjectively feels he/she receives from others, since it is easily measured and has a recognized association with positive health outcomes.19 We used an abridged 5-item version20 of the Medical Outcomes Study Social Support Survey (MOS-SSS),3 to measure 5 domains of social support: emotional support (empathy); informational support (information and guidance); tangible support (physical assistance); positive social interaction (spending time with others); and affectionate support (love and affection). Its breadth and brevity, as well as its demonstrated internal consistency and validity20 informed our use of this survey. The questionnaire assessed each domain of social support by asking about the presence of someone who provides each type of support on a scale from 1 (lowest) to 5 (See Supplementary Figure 1). Low support was defined as responses of 1-3. Participants completed the survey during their initial AMI hospitalization.
All-cause readmission and all-cause mortality were assessed 6-months after hospital discharge. Site coordinators collected records on medical events that occurred within 6 months of hospital discharge as well as death certificates. A physician panel reviewed and double-adjudicated the medical records to verify the event and primary diagnosis.
The associations between low social support in each domain and mortality and readmission were determined using multivariable logistic regression, adjusting for the covariates shown in Table 1 and assigning significance to findings with a p-value of < 0.05. Missing data were accounted for using multiple imputation. All variables were missing <5% of values, except for left ventricular ejection fraction (LVEF) which was missing in 9.2% of participants. All analyses were performed with SAS, version 9.4 (SAS Institute).
Table 1.
Baseline Characteristics of Study Population (n = 3006)
| DEMOGRAPHIC | |
| Mean Age (SD) | 81.56 (5.0) |
| Women | 1335 (44.4%) |
| Non-White | 317 (10.6%) |
| Education <= 12 Years | 1707 (56.8%) |
| Married or Living with Partner | 1514 (50.4%) |
| COMORBIDITIES AND PRIOR MEDICAL HISTORY | |
| Chronic Kidney Disease [Estimated Glomerular Filtration Rate < 60 ml/min/1.73m2] | 1804 (60.0%) |
| Coronary Artery Disease | 1603 (53.3%) |
| Revascularization | 1220 (40.6%) |
| Diabetes Mellitus | 1116 (37.1%) |
| Myocardial Infarction | 819 (27.3%) |
| Arrhythmias | 749 (24.9%) |
| Cancer | 646 (21.5%) |
| Congestive Heart Failure | 563 (18.7%) |
| Cerebrovascular Disease | 468 (15.6%) |
| Chronic Obstructive Pulmonary Disease | 426 (14.2%) |
| Peripheral Arterial Disease | 363 (12.1%) |
| Valvular Heart Disease | 349 (11.6%) |
| PRESENTATION AND HOSPITALIZATION CHARACTERISTICS | |
| Time from Symptom Onset to Presentation (Hours) | |
| < 6 | 1719 (57.2%) |
| >= 6 to < 12 | 346 (11.5%) |
| >= 12 | 925 (30.8%) |
| Mean Length of Stay [Days] (SD) | 5.93 (5.32) |
| Mean Heart Rate [bpm] [First Available] (SD) | 83.57 (22.66) |
| Mean Systolic Blood Pressure [mmHg] [First Available] (SD) | 145.88 (30.81) |
| Mean Hemoglobin Initial Value [First Available] (SD) | 12.82 (2.07) |
| Killip Class | |
| I | 2614 (87.0%) |
| II, III or IV | 392 (13.0%) |
| ST-Elevation Myocardial Infarction | 791 (26.3%) |
| Revascularization Status | |
| No Cardiac Catheterization | 458 (15.2%) |
| Cardiac Catheterization Without Revascularization | 494 (16.4%) |
| Percutaneous Coronary Intervention Only | 1700 (56.6%) |
| Coronary Artery Bypass Graft | 354 (11.8%) |
| In-hospital Complications | |
| Bleeding | 773 (25.7%) |
| Arrhythmia | 538 (17.9%) |
| Heart Failure | 414 (13.8%) |
| In-hospital Left Ventricular Ejection Fraction >= 50% | 1527 (50.8%) |
| Discharge Location - Home | 2417 (80.4%) |
| SOCIAL SUPPORT | |
| Participants Reporting Low Support | |
| Emotional Support | 584 (19.4%) |
| Informational Support | 633 (21.1%) |
| Tangible Support | 566 (18.8%) |
| Positive Social Interaction | 739 (24.6%) |
| Affectionate Support | 339 (11.3%) |
Results
Participant characteristics are shown in Table 1. The mean age was 81.6 years and 44.4% of participants were female. Most participants had AMI Killip class I (87.0%) and had an NSTEMI (73.7%). Approximately 80.4% of participants were discharged to their home. Rates of low social support in each domain ranged from 11.3% to 24.6%.
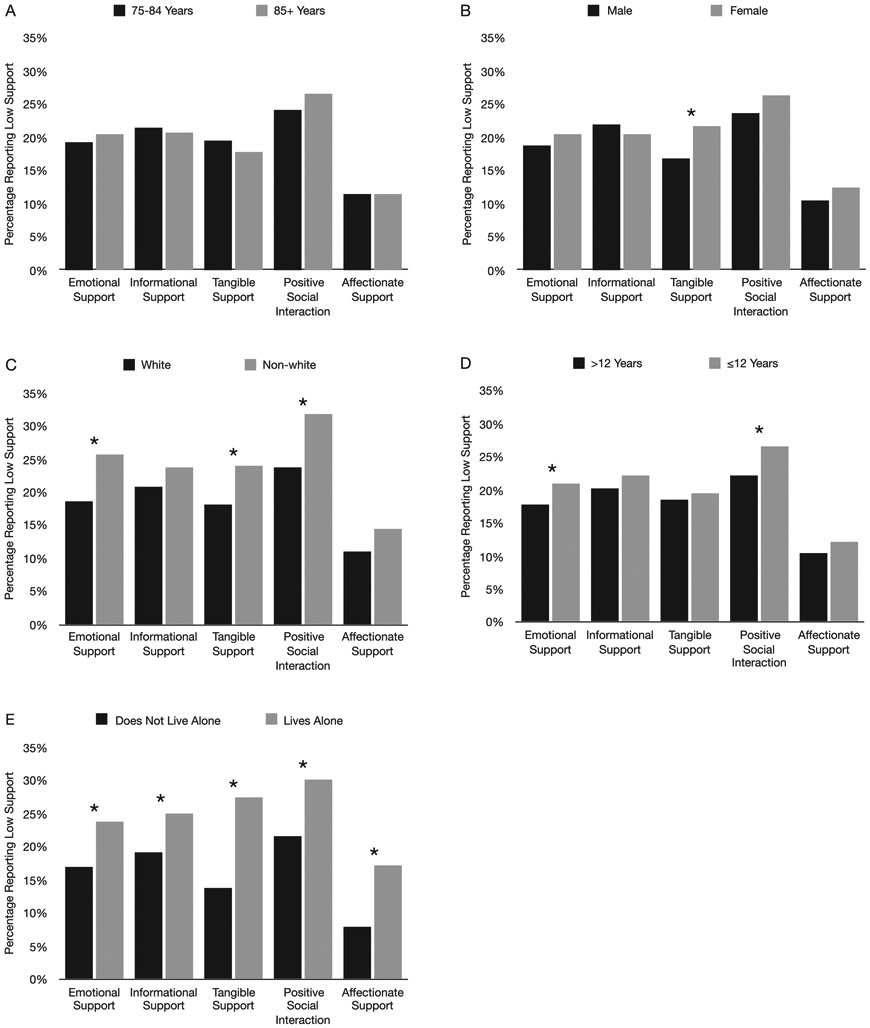
Shown in Figure 1 are the rates of low social support according to select sociodemographic characteristics, including age, sex, race, education, and cohabitation status. Female participants reported lower tangible support than males (21.7% vs. 16.9% reporting low support; P = 0.001). Non-white participants reported lower emotional support (25.6% vs. 18.6%; P = 0.003), tangible support (24.0% vs. 18%; P = 0.012), and positive social interaction (31.7% vs. 23.8%; P = 0.002) than white participants. Participants with <12 years of education reported lower emotional support (21.0% vs. 17.7%; P = 0.029) and positive social interaction (26.7% vs. 22.1%; P = 0.004) than those ≥12 years of education. Participants who lived alone reported lower social support in all 5 domains than those living with others (23.7% vs. 17.0% emotional; 25.0% vs. 19.0% informational; 27.4% vs. 13.8% tangible; 30.1% vs. 21.5% positive social interaction; 17.2% vs. 7.9% affectionate; all P < 0.001).
Figure 1. Percentage of participants reporting low support in each domain.
Data presented by a) age, b) sex, c) race, d) education level, and e) cohabitation status. Asterisks indicate statistically significant differences between groups (p<0.05). N=3006.
There were 1222 participants (40.7%) who experienced a readmission within 6 months of discharge from the index hospitalization. Results of the multivariable models for 6-month readmission are shown in Figure 2. After adjustment for all covariates shown in Table 1, participants who reported low informational support had higher odds of readmission in the 6 months following hospitalization (odds ratio [OR] = 1.22; 95% confidence interval [CI] = 1.01-1.47; P = 0.040). All other domains of social support showed no statistically significant association with 6-month readmission.
Figure 2. Multivariable-adjusted association of low social support with all-cause readmission.
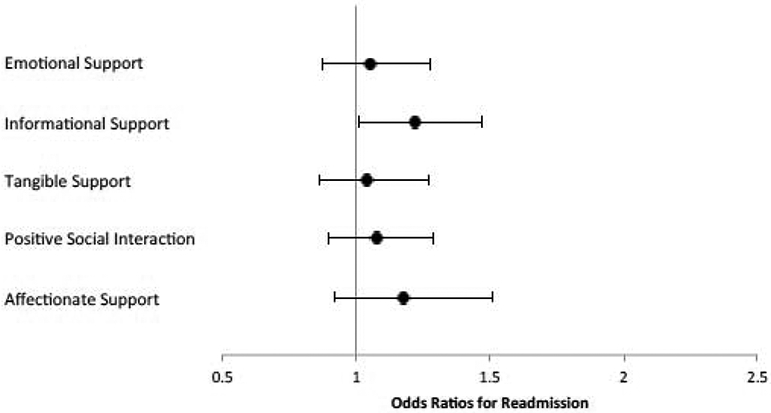
Low social support defined as a response of “none of the time,” “a little of the time,” or “some of the time” on the 5-item MOS-SSS. Adjusted for: sociodemographic characteristics (age, sex, race, education, cohabitation status); comorbidities (prior coronary artery disease, AMI, revascularization, arrhythmia, or heart failure; peripheral vascular disease, valvular disease, cerebrovascular accident, chronic obstructive pulmonary disease, chronic kidney disease, cancer, diabetes mellitus); as well as AMI and hospitalization characteristics (Killip class, presenting heart rate, presenting systolic blood pressure, time to presentation, AMI classification, length of admission, initial hemoglobin value, in-hospital revascularization, in-hospital complications [arrhythmia, bleeding, heart failure], left ventricular ejection fraction, and discharge location). Odds ratios (circles) are shown with 95% confidence intervals (bars). N=3006.
There were 266 participants (8.9%) who died within 6 months of discharge from the index hospitalization. Shown in Figure 3 are results for 6-month mortality. After adjustment for all covariates shown in Table 1, participants who reported low emotional support had greater odds of mortality in the 6 months following hospitalization (OR = 1.43; 95% CI = 1.04-1.97; P = 0.026), whereas other domains of social support showed no statistically significant association.
Figure 3. Multivariable-adjusted association of low social support with all-cause mortality.
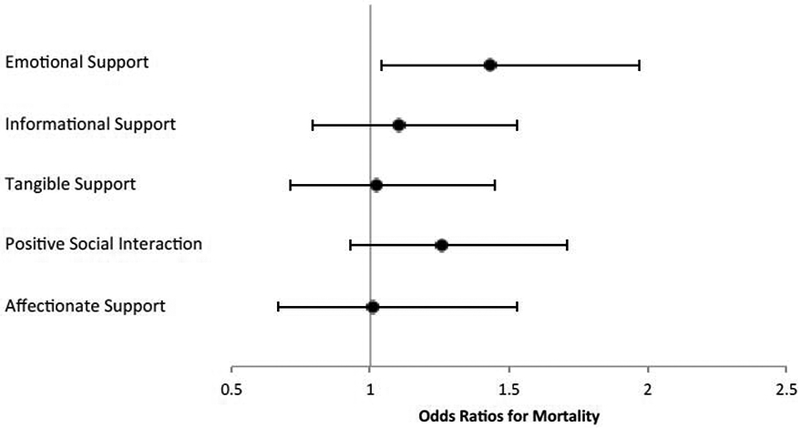
Low social support defined as a response of “none of the time,” “a little of the time,” or “some of the time” on the 5-item MOS-SSS. Adjusted for: sociodemographic characteristics (age, sex, race, education, cohabitation status); comorbidities (prior coronary artery disease, AMI, revascularization, arrhythmia, or heart failure; peripheral vascular disease, valvular disease, cerebrovascular accident, chronic obstructive pulmonary disease, chronic kidney disease, cancer, diabetes mellitus); as well as AMI and hospitalization characteristics (Killip class, presenting heart rate, presenting systolic blood pressure, time to presentation, AMI classification, length of admission, initial hemoglobin value, in-hospital revascularization, in-hospital complications [arrhythmia, bleeding, heart failure], left ventricular ejection fraction, and discharge location). Odds ratios (circles) are shown with 95% confidence intervals (bars). N=3006.
Discussion
Using data from a contemporary cohort of older adults hospitalized for AMI, we found that participants who reported low informational support were more likely to be readmitted, and that participants who reported low emotional support were more likely to die within 6 months of discharge. These findings demonstrate heterogeneity in the predictive value of the domains of social support. They further show that even after adjustment for demographics, past medical history, and characteristics of the AMI and hospitalization, perceived social support remains an independent and robust predictor of post-discharge outcomes among older patients.
Our study extends previous literature on the effects of social support on post-AMI health outcomes in 3 important ways. First, our study focuses specifically on older patients, in whom social support may play an especially important role.21 To our knowledge, the few studies that have investigated this association in older adults were published over 25 years ago and used samples of fewer than 500 participants.12,13 Second, while there have been numerous studies on the impact of social support on outcomes after AMI,4-14 the vast majority4-10 have considered social support in its totality, rather than examining its discrete domains, despite the utility of doing so.1,2 Some studies have reported associations between components of social support and outcomes, however, these did not investigate the effects of any greater than 2 domains, precluding comparisons across multiple domains.11-14 Third, our study rigorously adjusts for predictors of post-AMI outcomes based on contemporary evidence.17,18 The majority of prior studies examining social support after AMI were published over 10 years ago,4,5,10-14 and did not adjust for many of the factors currently known to affect post-AMI outcomes, factors such as comorbidities, length of hospital stay, and in-hospital complications. Our methodology therefore enables more rigorous conclusions about the associations between social support and outcomes in older patients hospitalized for AMI than has previously been available.
Low informational support — operationalized as lacking “someone to turn to for suggestions about how to deal with a personal problem” — was the only domain of social support associated with readmission. This may be related to lack of advice for the complex self-care required after an AMI, such as obtaining medications or transportation to appointments. Indeed, it is well-recognized that social relationships promote healthy decisions and behaviors.22 The association between low informational support and readmission can inform interventions to facilitate patients’ transitions out of the hospital. There is growing consensus that the experience of hospitalization itself can leave patients in a state of heightened vulnerability and therefore less able to navigate complex self-care tasks on their own upon discharge.23 Including family, friends, and caregivers in discharge planning can help patients obtain the guidance needed to support self-care and recovery. Notably, this is an intent of the American Association of Retired Persons’ (AARP’s) “CARE Act,” which requires hospitals to provide family caregivers with relevant instruction upon discharge.24 Despite having been enacted into law in most states, the requirements of the CARE Act are rarely addressed by providers.24 Our study provides rationale for more consistent implementation of this legislation, as well as assessment of social support upon discharge. Our findings also support the provision of greater access to patient and caregiver education within communities through institutions such as federally-funded Aging and Disability Resource Centers.25
Low emotional support — operationalized as lacking “someone to confide in or talk to about your problems” — was the only domain associated with mortality. This is consistent with evidence that supportive social interactions are associated with reduced cardiovascular, inflammatory, and neuroendocrine reactivity as well as improved immune function.21,22 Similarly, low emotional support may specifically contribute to or represent feelings of loneliness, which is increasingly being shown as an independent risk factor for mortality.26 The relationship between low emotional support and mortality has broad implications for how the needs of the geriatric cardiac population should be addressed. Nearly 70% of Americans age 60-79, and 85% age 80 and over suffer from cardiovascular disease, totaling to millions of Americans.27 The significance of emotional support in reducing mortality, as demonstrated by our study and others,12,13 underscores the importance of providing services that enable seniors to live socially well-connected lives. This may include bolstering funding for the creation of community-based services, such as senior centers and home care. This may also include increasing funding for retirement and assisted living facilities, so that they can better provide their residents with socially enriching environments. Indeed, more robust investment in social services has been associated with reduced mortality, including amongst AMI survivors.28
There are several issues to be considered in the interpretation of our findings. First, our cohort had a relatively low percentage of racial minorities, with only 11% of participants being non-white. This is consistent with population estimates of minorities in older patients with AMI.29 Second, our study only included individuals who spoke English or Spanish, yet social support may be of particular importance for individuals who speak other languages. Third, our measure of social support was based on self-report. As such, it is subject to “desirability bias” and participants may have been reticent to report poor support.30 However, there is evidence that this bias does not significantly influence the self-reporting of social support.30 Furthermore, perceived social support is easily attainable in clinical settings and has recognized associations with health outcomes.19 Fourth, our study focused only on patients with AMI. Despite this, the prevalence and burden of the disease make the implications of this study impactful nevertheless. Moreover, we believe that the recovery from AMI, and the psychosocial factors underlying it, may be applicable to other diseases for which geriatric patients are hospitalized.
In conclusion, in a large, contemporary cohort of older patients hospitalized for AMI, low informational support was associated with readmission, and low emotional support with mortality within 6 months of discharge from their index hospitalization. By examining the individual associations of domains of social support with outcomes, our findings provide rationale for more precise design and delivery of social interventions, such as targeting informational support in discharge planning and emotional support through community-based services. Furthermore, our study adds to a large body of literature on the importance of social support amongst older adults and emphasizes the need for more robust public services to better meet the needs of our aging population.
Supplementary Material
Acknowledgement
Data Access, Responsibility, and Analysis
Dr. Chaudhry had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Grant Support
Funding from the National Heart, Lung, and Blood Institute (NHLBI) of the NIH (R01HL115295) as well as from the National Institute on Aging of the NIH through the Yale Program on Aging/Claude D. Pepper Older Americans Independence Center (P30AG21342) supported the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Funding from the National Institute on Aging of the NIH (T35AG049685) supported Mr. Green’s efforts for this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lyyra TM, Heikkinen RL. Perceived social support and mortality in older people. J Gerontol B - Psychol 2006;61(3):S147–S152. [DOI] [PubMed] [Google Scholar]
- 2.Lett HS, Blumenthal JA, Babyak MA, Catellier DJ, Carney RM, Berkman LF, Burg MM, Mitchell P, Jaffe AS, Schneiderman N. Dimensions of social support and depression in patients at increased psychosocial risk recovering from myocardial infarction. Int J Behav Med 2009; 16(3):248–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991;32(6):705–714. [DOI] [PubMed] [Google Scholar]
- 4.Welin C, Lappas G, Wilhelmsen L. Independent importance of psychosocial factors for prognosis after myocardial infarction. J Intern Med 2000;247(6):629–639. [DOI] [PubMed] [Google Scholar]
- 5.Burg MM, Barefoot J, Berkman L, Catellier DJ, Czajkowski S, Saab P, Huber M, DeLillo V, Mitchell P, Skala J. Low perceived social support and post-myocardial infarction prognosis in the enhancing recovery in coronary heart disease clinical trial: the effects of treatment. Psychosom Med 2005;67(6):879–888. [DOI] [PubMed] [Google Scholar]
- 6.Bucholz EM, Rathore SS, Gosch K, Schoenfeld A, Jones PG, Buchanan DM, Spertus JA, Krumholz HM. Effect of living alone on patient outcomes after hospitalization for acute myocardial infarction. Am J Cardiol 2011;108(7):943–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leifheit-Limson EC, Reid KJ, Kasl SV, Lin H, Buchanan DM, Jones PG, Peterson PN, Parashar S, Spertus JA, Lichtman JH. Changes in social support within the early recovery period and outcomes after acute myocardial infarction. J Psychosom Res 2012;73(1):35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bucholz EM, Strait KM, Dreyer RP, Geda M, Lichtman JH, D'Onofrio G, Spertus JA, Krumholz HM. Effect of low perceived social support on health outcomes in young patients with acute myocardial infarction: results from the VIRGO study. J Am Heart Assoc 2014;3(5):e001252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lei S, Dayihu, Liwang, Rongjingding. The influence of social support on health outcomes in patients with acute coronary syndrome: A prospective study from China. J Am Coll Cardiol 2017;70 (16 Supplement 1):C75–C76. [Google Scholar]
- 10.Frasure-Smith N, Lesperance F, Gravel G, Masson A, Juneau M, Talajic M, Bourassa MG. Social support, depression, and mortality during the first year after myocardial infarction. Circulation 2000; 101 (16): 1919–1924. [DOI] [PubMed] [Google Scholar]
- 11.Woloshin S, Schwartz LM, Tosteson AN, Chang CH, Wright B, Plohman J, Fisher ES. Perceived adequacy of tangible social support and health outcomes in patients with coronary artery disease. J Gen Intern Med 1997;12(10):613–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berkman LF, Leo-Summers L, Horwitz RI. Emotional support and survival after myocardial infarction. A prospective, population-based study of the elderly. Ann Intern Med 1992; 117(12): 1003–1009. [DOI] [PubMed] [Google Scholar]
- 13.Hedblad B, Ostergren PO, Hanson BS, Janzon L, Johansson BW, Juul-Moller S. Influence of social support on cardiac event rate in men with ischaemic type ST segment depression during ambulatory 24-h long-term ECG recording. The prospective population study 'Men born in 1914', Malmo, Sweden.[Erratum appears in Eur Heart J 1993 Aug; 14(8): 1152]. Eur Heart J 1992; 13(4):433–439. [DOI] [PubMed] [Google Scholar]
- 14.Molloy GJ, Perkins-Porras L, Bhattacharyya MR, Strike PC, Steptoe A. Practical support predicts medication adherence and attendance at cardiac rehabilitation following acute coronary syndrome. J of Psychosom Res 2008;65(6):581–586. [DOI] [PubMed] [Google Scholar]
- 15.Dodson JA, Geda M, Krumholz HM, Lorenze N, Murphy TE, Allore HG, Charpentier P, Tsang SW, Acampora D, Tinetti ME. Design and rationale of the comprehensive evaluation of risk factors in older patients with AMI (SILVER-AMI) study. BMC Health Serv Res 2014;14(1):506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K, Alpert JS, White HD, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Chaitman BA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S. Third universal definition of myocardial infarction. Eur Heart J 2012;33(20):2551–2567. [DOI] [PubMed] [Google Scholar]
- 17.Krumholz HM, Lin Z, Drye EE, Desai MM, Han LF, Rapp MT, Mattera JA, Normand SL. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ-Cardiovasc Qua 2011. ;4(2):243–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith LN, Makam AN, Darden D, Mayo H, Das SR, Halm EA, Nguyen OK. Acute Myocardial Infarction Readmission Risk Prediction Models: A Systematic Review of Model Performance. Circ-Cardiovasc Qual 2018; 11(1):e003885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norris FH, Kaniasty K. Received and perceived social support in times of stress: A test of the social support deterioration deterrence model. J Pers Soc Psychol 1996;71(3):498. [DOI] [PubMed] [Google Scholar]
- 20.McCarrier K, Bushnell D, Martin M, Paczkowski R, Nelson D, Buesching D. PRM16 validation and psychometric evaluation of a 5-item measure of perceived social support. Value Health 2011. ;14(3):A148. [Google Scholar]
- 21.Seeman TE. Health promoting effects of friends and family on health outcomes in older adults. Am J Health Promot 2000;14(6):362–370. [DOI] [PubMed] [Google Scholar]
- 22.Reblin M, Uchino BN. Social and Emotional Support and its Implication for Health. Curr Opin Psychiatr 2008;21 (2):201–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krumholz HM. Post-Hospital Syndrome — An Acquired, Transient Condition of Generalized Risk. N Engl J Med 2013;368(2): 100–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coleman EA. Family caregivers as partners in care transitions: The caregiver advise record and enable act. J Hosp Med 2016; 11(12):883–885. [DOI] [PubMed] [Google Scholar]
- 25.O'Shaughnessy C Aging and Disability Resource Centers (ADRCs): Federal and state efforts to guide consumers through the long-term services and supports maze. 2010.
- 26.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and Social Isolation as Risk Factors for Mortality:A Meta-Analytic Review. Perspect Psychol Sci 2015; 10(2):227–237. [DOI] [PubMed] [Google Scholar]
- 27.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation 2018;137(12):e67–e492. [DOI] [PubMed] [Google Scholar]
- 28.Bradley EH, Canavan M, Rogan E, Talbert-Slagle K, Ndumele C, Taylor L, Curry LA. Variation in health outcomes: the role of spending on social services, public health, and health care, 2000–09. Health Aff (Millwood) 2016;35(5):760–768. [DOI] [PubMed] [Google Scholar]
- 29.Canto JG, Rogers WJ, Goldberg RJ, Peterson ED, Wenger NK, Vaccarino V, Kiefe Cl, Frederick PD, Sopko G, Zheng ZJ, NRMI Investigators. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. Jama 2012;307(8):813–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dahlem NW, Zimet GD, Walker RR. The Multidimensional Scale of Perceived Social Support: A confirmation study. J Clin Psychol 1991. ;47(6):756–761. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.