ABSTRACT
BACKGROUND AND PURPOSE
To identify and evaluate diagnostic magnetic resonance imaging (MRI) features in patients with suspicion of discoligamentous cervical injury after hyperextension trauma of the cervical spine.
METHODS
MR images with a standard protocol (1.5 T, including sagittal T2‐weighted images and short tau inversion recovery [STIR]) in 21 patients without any sign of fracture or instability on multidetector computed tomography of the cervical spine were assessed. Among other structures we evaluated the following: prevertebral hematoma, anterior longitudinal ligament (ALL), intervertebral disc, and spinal cord. Presence and the anatomic level of injury were identified and recorded. Results were then compared with intraoperative findings as a reference standard. Simple descriptive statistical analysis, agreement coefficients (given by calculating the percent agreement), and the determination of Gwet's AC1 coefficient were used to analyze our results.
RESULTS
The overall percent agreement between STIR and intraoperative findings was 90.9% (AC1 = .881) and for T2 69.7% (AC1 = .498). For the ALL, the overall agreement was 87.9% (AC1 = .808) and for the intervertebral disc 78.8% (AC1 = .673), in which STIR always showed a higher agreement. Prevertebral hematoma was found in 20 of 21 patients with the maximum thickness at the same anatomic level as the intraoperatively proven lesion in 12 of 18 patients (67%). Edema and/or hemorrhage of the spinal cord was shown in 16 of 21 being at the same anatomic level as the intraoperatively confirmed pathology in 16 of 16 patients (100%).
CONCLUSIONS
MRI is a reliable tool for the evaluation of discoligamentous injuries in the cervical spine, with ancillary features proven as helpful information.
Keywords: cervical spine, injury, MRI
Introduction
Injuries of the cervical spine in major trauma usually present with neurological impairment. Symptoms can vary from upper extremity paresthesia to complete and incomplete tetraplegia.1, 2, 3 Therefore, these injuries are approached with much caution by clinicians. Traumatic injury to the cervical spine and associated soft‐tissue structures occurs when the physiologic ranges are rapidly exceeded, as in trauma from high‐speed motor vehicle accidents, high‐speed sports injuries or falls.4 The severity of the injury depends on whether the mechanical stability of the spine or the integrity of the spinal cord has been compromised.2 Instability can lead to further injury, pain, or deformity and often requires surgical stabilization.5
Fast imaging plays a crucial role in the treatment of these patients. The initial modality to evaluate the cervical spine in major trauma patients is multidetector computed tomography (MDCT).6 While MDCT is excellent for the timely assessment of osseous injuries, only magnetic resonance imaging (MRI) provides evaluation of ligamentous or other soft tissue injuries, disc, spinal cord, occult osseous lesions, and even small haematomas.1, 2, 3, 7, 8, 9 Although the prevalence of acute cervical spine injury in the absence of fracture is low, fast imaging can help to mitigate possibly life‐threatening complications and to plan the operative procedure.10, 11, 12 Due to its increased availability in the emergency settings and its high sensitivity for soft‐tissue structures, MRI nowadays plays an important role and has the potential to revolutionize the management of spinal trauma patients.2, 3, 4, 5, 8, 13 MRI is the modality of choice in patients who present with neurological symptoms referable to the cervical spine and in cases of persistent neck pain with or without osseous abnormalities at radiography or MDCT, but with a high index of suspicion of injury.
Imaging of patients with suspected cervical spine injury has been extensively debated in the literature.2, 14 Many studies have indirectly compared MRI with CT or radiography and determined its benefit as compared to conventional imaging.14 Few have attempted direct comparison between surgical findings and imaging findings for patients who underwent surgery based on imaging findings but the information on sensitivity and specificity in the evaluation of various structures varies widely.14, 15, 16 So far, only a few studies have aimed at a comparison of different MR sequences or possible ancillary features to improve the diagnosis.15, 17
The purpose of this study was to identify and evaluate diagnostic MRI features in patients with suspicion of discoligamentous cervical injury after hyperextension trauma of the cervical spine. Therefore, we assessed MR images with a standard protocol in patients without any sign of fracture or instability on MDCT of the cervical spine and compared results with intraoperative findings as a reference standard.
Methods
Patients
A total of 21 patients (3 women and 18 men, mean age 62 years, range 38‐87 years) were included in this retrospective study. All patients were referred to the Department of Radiology at the Medical University of *blinded* between January 2008 and July 2016 for a standard MRI of the cervical spine after major trauma. Further inclusion criteria were: (1) trauma patients with a history of hyperextension injury of the cervical spine, (2) MDCT with no signs of a fracture or instability, (3) neurologic deficits up to tetraplegia, (4) subsequent anterior stabilization of cervical disc and/or ligamentous injury with corresponding documentation of the intraoperative findings, (5) MDCT, MRI and operation performed within 72 hours after the trauma.
MRI Protocol, Interpretation, and Correlation
All MRI scans were obtained on a 1.5 T MR scanner (Magnetom Avanto or AvantoFit, Siemens Healthineers, Erlangen, Germany) using a dedicated head and neck phased array surface coil. Our routine trauma cervical spine imaging protocol is provided in Table 1.
Table 1.
Imaging Parameters of our Routine MR Protocol for Imaging the Cervical Spine after Trauma
| TR (ms) | TE (ms) | Matrix | FOV (mm) | Slice thickness (mm) | |
|---|---|---|---|---|---|
| Sagittal T1‐weighted turbo spin echo | 514‐760 | 9.4‐12 | 320 × 320 or 384 × 384 | 220 × 220 or 250 × 250 or 270 × 270 | 3 |
| Sagittal T2‐weigthed turbo spin echo | 2,370‐4,110 | 82‐117 | 320 × 320 or 384 × 384 | 220 × 220, or 250 × 250, or 270 × 270 | 3 |
| Sagittal short tau inversion recovery | 2,660‐5,170 | 13‐92 | 256 × 256, or 320 × 320, or 384 × 384 | 220 × 220, or 250 × 250, or 270 × 270 | 3 |
| Axial T1‐weighted turbo spin echo1 | 505‐806 | 9.5‐14 | 256 × 204 or 256 × 256 | 159 × 200, or 150 × 200, or 150 × 200 | 4 |
| Axial T2‐weighted turbo spin echo1 | 2,480‐8,660 | 82‐99 | 320 × 256 or 320 × 240 | 160 × 200 or 160 × 160 | 4 |
TR = repetition time; TE = echo time; FOV = field‐of‐view.
1At the height of the pathological changes, defined by the attending radiologist.
MR scans were re‐evaluated separately in retrospect by two radiologists (rater 1 *blinded* with 9 years and rater 2 *blinded* with 3 years’ experience in reading MRI) on an IMPAX EE workstation (Agfa HealthCare, Bonn, Germany). Both readers were blinded to the results of the intraoperative findings and for any clinical information. They also had no access to any other patient imaging studies. First, the anatomic level of the pathology with respect to the vertebrae was determined, separately for the sagittal T2‐weighted sequence and sagittal short tau inversion recovery (STIR) and in total regardless of the sequence used.
We evaluated the following structures and possible pathologies with regard to the presence of a pathology on a simple yes/no decision: prevertebral hematoma, anterior longitudinal ligament (ALL), intervertebral disc, posterior longitudinal ligament (PLL), spinal cord, facet joints, and hematoma of the paravertebral muscles. Presence and the anatomic level of injury were identified and recorded. Tearing of the ALL or PLL was defined by interruption or absence of the normal linear band of hypointense signal of the ligament visualized on sagittal T2‐weighted images and/or STIR. The intervertebral disc was considered abnormal if it demonstrated high T2 and/or STIR signal intensity or complete disruption or if a herniation could be identified, also on sagittal T2‐weighted images and/or STIR. In relation to the intervertebral disc and the ligament, the lesions were also documented in several locations, if these were present. Similarly, the spinal cord was considered abnormal if it showed any focus of hyperintense signal in T2/STIR due to cord edema and/or hemorrhage or, in the acute stage, hypointense signal on T2‐weighted images indicating intraparenchymal cord hemorrhage. The anatomic level of the respective change in the spinal cord was documented. Finally, the presence of prevertebral hematoma, pathology of the facet joints (eg, edema, widening of joint space, or injury to the facet capsule) and posterior hematoma of the neck muscles were documented. For the prevertebral hematoma, the anatomic level of the maximum thickness of the hematoma on the sagittal STIR sequence was indicated. The sagittal T1‐weighted images and the axial T1‐ and T2‐weighted images were used for further orientation or anatomic assignment. For these three sequences, no separate assessment was made.
The findings of the ALL, the intervertebral disc, and the anatomic level of the pathology were then correlated with intraoperative findings (= “gold standard”). The anterior surgical approach prevented intraoperative assessment of the PLL and the facet joints. Therefore, a comparison with the intraoperative findings was not possible for these two structures. The surgical information was provided by written surgical reports for each patient.
Finally, the results of the two radiologists were compared with each other and with respect to the intraoperative results. In a second meeting, a common consensus was formed between the two radiologists for all findings.
Statistical Analysis
The results are presented as patient‐based and segment‐based, depending on the structure to be examined. Simple descriptive statistical analysis was used to quantitatively describe the results. Intraoperative findings were classified as lesion or nonlesion and correlated with MRI findings. Interrater agreement was only calculated for the height of the pathology (affected segment), ALL, and intervertebral disc because in all the other structures/pathologies both readers had 100% agreement. Statistical analysis was performed using R Project for Statistical Computing 3.4.1.18 Agreement coefficients were on one hand given by calculating the percent agreement and to avoid paradoxical values19 by determining Gwet's AC1 coefficient20 using the rel‐package for R.21 Assuming intraoperative findings as gold standard, sensitivity and specificity were calculated and a χ2 test for independence was performed. Results were considered significant for P‐values less than .05.
Results
In total, 30 segments were affected by a discoligamentous injury in 21 patients. Intraoperatively, the most frequent lesions were found at segments C 3/4 (n = 10) and C5/6 (n = 10).
For all patients (100%), sagittal STIR images identified a lesion at the same spinal segment as identified intraoperatively. There were only 3 patients where STIR indicated a further pathology at one additional spinal segment, resulting in an overall percent agreement between STIR and intraoperative findings of 90.9% and an AC1 agreement coefficient of .881. For sagittal T2‐weighted images only in 16 of 21 (76.2%) patients, a pathology was detected at the intraoperatively identified spinal sites. In 5 patients, T2‐weighted images showed no conspicuities at all, in 3 patients a segment with pathology was missed, and in 1 patient a pathology was detected at an additional segment.
Considering the agreement between T2w and intraoperative findings for individual spinal segments, an overall percent agreement of 69.7% was obtained with an AC1 of .498. For the final MRI finding, 27 segments were true positive, three true negative, three false positive, and 0 false negative. This results in a percent agreement of 90.9%, a total sensitivity of 100% and a specificity of 50% (P < .05).
Intraoperatively, the ALL was found to be injured in 18 of 21 patients (at 23/33 segments). In four segments, the ALL was considered as torn in MRI, but intraoperative findings showed an intact ligament (overall agreement = 87.9%; AC1 = .808). Agreement between sagittal STIR images and intraoperative findings was the same as for the overall MR result, but markedly lower for T2w images (overall agreement: 60.6%; AC1 = .224). In 3 patients (four segments) no tearing of the ALL was found intraoperatively; the reason for the clinical symptoms was a spinal cord compression caused by the hyperextension with underlying pre‐existing cervical canal stenosis due to degenerative disease.
In 19 of 21 patients (at 24 spinal segments), lesions of the intervertebral disc were identified intraoperatively. At five segments, a intervertebral disc lesion was identified by MRI but not intraoperatively, and at two segments with intraoperative intervertebral disc findings no lesion was identified by MRI (overall agreement: 78.8%; AC1 = .673). Sagittal STIR sequences revealed a higher overall agreement ( = 81.8%; AC1 = .727) than T2‐weighted sequences (overall agreement = 60.6%, AC1 = .278).
Due to the anterior surgical approach, the PLL was evaluated intraoperatively only in 5 of 21 patients (seven segments) and a lesion was found for 2 patients (at one segment each). Only in one of these patients, MRI was able to detect the PLL lesion correctly and detected a lesion for 1 patient where none was identified intraoperatively.
Results of the agreement coefficients between intraoperative findings and MRI are summarized in Table 2. Interrater agreement is provided in Table 3.
Table 2.
Agreement Coefficients between Intraoperative Findings and MRI
| MRI in total | STIR only | T2w only | |
|---|---|---|---|
| Agreement with intraoperative findings for the affected segments | 90.9% (AC1 .881 [SE: .071, 95% CI: .737‐1.0]) | 90.9% (AC1 .881 [SE: .071, 95% CI: .737‐1.0]) | 69.7% (AC1 .498 [SE: .158, 95% CI: .176‐.82]) |
| Agreement with intraoperative findings for the ALL | 87.9% (AC1 .808 [SE: .097, 95% CI: .61‐1.0]) | 87.9% (AC1 .808 [SE: .097, 95% CI: .61‐1.0]) | 60.6% (AC1 .224 [SE: .173, 95% CI: −.13‐.58)] |
| Agreement with intraoperative findings for the disc | 78.8% (AC1 .673 [SE: .127, 95% CI: −.414‐ .932]) | 81.8% (AC1 .727 [SE: .115, 95% CI: .49‐.96]) | 60.6% (AC1 .278 [SE: .179, 95% CI: −.08‐.64]) |
STIR = short tau inversion recovery; T2w = T2‐weighted imaging; AC1 = Gwet's AC1 coefficient; CI = confidence interval; SE = standard error.
Table 3.
Interrater Agreement
| MRI in total | STIR only | T2w only | |
|---|---|---|---|
| Interrater agreement between both raters for the affected segments | 84.8% (AC1 .813 [SE: .088, 95% CI: .633‐.99]) | 75.8% (AC1 .692 [SE: .117, 95% CI: .454‐.93]) | 84.8% (AC 1 .732 [SE: .118, 95% CI: .493‐.972]) |
| Interrater agreement between both raters for the ALL | 78.8% (AC1 .673 [SE: .127, 95% CI: .414‐.932]) | 78.8% (AC1 .673 [SE: .127, 95% CI: .414‐.932]) | 90.9% (AC1 = .824 [SE: .098, 95% CI: .624 ‐1.0]) |
| Interrater agreement between both raters for the disc | 72.7% (AC1 .58 [SE: .144, 95% CI: .286‐.874]) | 69.7% (AC1 .521 [SE: .154, 95% CI: .207‐.835]) | 72.7% (AC1 .455 [SE: .155, 95% CI: .139‐.77]) |
STIR = short tau inversion recovery; T2w = T2‐weighted imaging; AC1 = Gwet's AC1 coefficient; CI = confidence interval; SE = standard error.
Prevertebral hematomas were found in 20 of 21 patients. The 1 patient without hematoma had a lesion of the intervertebral disc without any sign of an ALL tear intraoperatively. Two patients with no lesion of the ALL, PLL, or intervertebral disc intraoperatively nonetheless showed a prevertebral hematoma (and spinal cord edema)—degenerative changes with pre‐exisitng degenerative disease were noted. The maximum thickness of the prevertebral hematoma was at the same anatomic level as the intraoperatively proven lesion in 12 of 18 patients (67%), in the adjacent segment in 4 of 18 (22%) and more than one segment away in 2 of 18 (11%).
Edema and/or hemorrhage of the spinal cord was shown in 16 of 21 patients, whereas the 5 patients without a visible pathology of the spinal cord on MRI revealed lesions of the ALL and/or the intervertebral disc, both intraoperatively and with MRI. The edema and/or hemorrhage was at the same anatomic level as the intraoperatively confirmed pathology in 16 of 16 patients (100%).
In MRI, facet joints were evaluated as injured in 10 of 21 patients (47.6%) and in 16 of 21 patients (84.2%) a posterior hematoma of the neck muscles was described.
Figures 1, 2, 3, 4 provide clinical examples.
Figure 1.
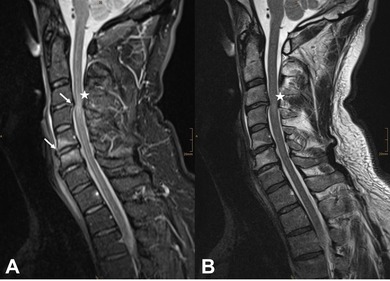
A 53‐year‐old patient after a ski accident with hyperextension injury of the cervical spine. The patient had initial tetraplegia emphasizing both upper extremities with partial remission of the lower extremities 2 hours after the accident. Sagittal short tau inversion recovery (STIR) (A) and T2‐weighted (B) images show an edema of spinal cord at C3/4 (white asterisk). The intervertebral disc at C3/4 and at C5/6 was reported with a lesion on STIR images and the anterior longitudinal ligament (ALL) was further reported as torn at C5/6 (white arrows in A). Intraoperatively neither the lesion of the intervertebral disc nor the ALL tear could be detected. The tetraplegia was due to a contusion of the spinal cord at C3/4 with pre‐existing vertebrostenosis.
Figure 2.
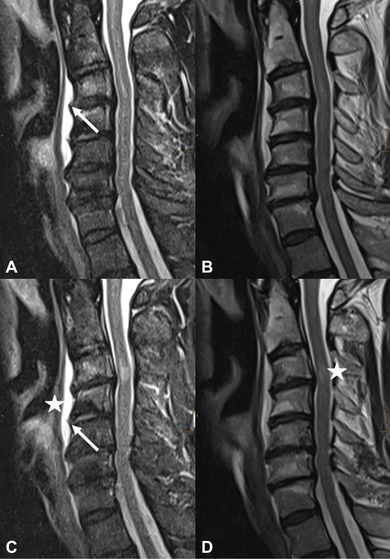
Sagittal short tau inversion recovery images on the left (A + C) were able to depict tearing of the anterior longitudinal ligament (ALL) at C3/4 and C4/5 (white arrows). With T2‐weighted images (B + D), the discontinuity is not visual. Prevertebral hematoma with the maximum thickness at this anatomic level and edema of the spinal cord is also present (white asterisks in C + D), no tearing of the posterior longitudinal ligament. Tear of the ALL at C3/4 and C4/5 was confirmed intraoperatively (images are zoomed for better visualization).
Figure 3.
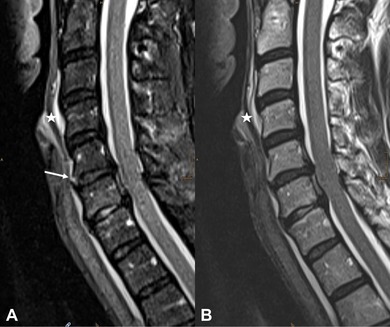
Complete tear of the anterior longitudinal ligament (ALL) at C5/6 only depicted with short tau inversion recovery (white arrow in A). There is no indication of tearing or direct evidence of a tear with T2‐weighted images (B). Prevertebral hematoma, as an ancillary finding, is present (asterisk in A + B). The tear of the ALL at C5/6 was confirmed intraoperatively.
Figure 4.
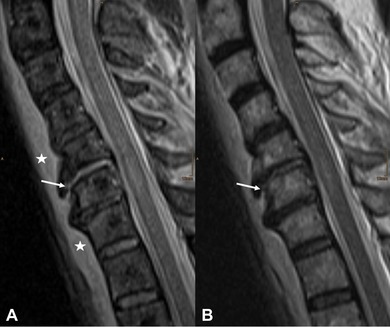
A 70‐year‐old male patient after a heavy fall. Sagittal short tau inversion recovery (A) shows a clear interruption (white arrow) of the anterior longitudinal ligament (ALL) at C5/6. T2‐weighted images (B) do not show this interruption so clearly (white arrow), with poor demarcation of liquid accumulation in the area of interruption. Prevertebral hematoma can be depicted with both sequences with the maximum thickness in the segment directly adjacent to the pathological findings (asterisks in A).
Discussion
Sagittal STIR reached a higher overall agreement with intraoperative findings in all pathologies compared to sagittal T2‐weighted images. The reason for this can be seen in its high contrast between fluid and nonfluid tissue. Surprisingly, a fat‐saturated image depicted small lesion better, for example, discontinuity of the ALL than the conventional T2‐weighted image with its higher signal‐to noise ratio (due to the presence of fat). The resolution of both used sequences was comparable. Concerning the ALL, T2‐weighted images are probably in disadvantage because the distinction between the ligament and the underlying disc annulus is not possible.22 In this context, T2‐weighted images have been described as inherently difficult for the evaluation of integrity.15, 22 STIR has already been recommended as the best sequence for the evaluation of the ALL by Kumar et al in a pictorial review, however, our study is the first that confirms this fact in a clinical study.8
Malham et al found a reasonable sensitivity of 81% for the detection of disc disruption with MRI but only a poor sensitivity concerning lesion of the ALL (48%) and PLL (50%).16 The specificity for ALL/PLL disruption was 100/87%, respectively, but 0% for disc disruption. This study led us to look at the results in more detail and, above all, to take into account different sequences to possibly increase the sensitivity or specificity. In contrast to nearly all so far published studies concerning MRI and trauma of the cervical spine, our study is the first that provides a closer look at different sequences, the approach of interpreting them and integrating the secondary signs of injury as hematoma or edema into the report.
Haris et al assessed the sensitivity of MRI in identifying injuries to the soft‐tissue structures of the spine.14 This study evaluated nearly all relevant structures but did not focus on different sequence types or the presence of any hematoma. They found that MRI was ineffective for the interpretation of the ALL with a high number of false negative results (3/9 false negative), but injuries of the PLL and the spinal cord could be detected with high sensitivity (94.4/ 93%). The specificity for the ALL was high with only one false positive result (1/6 false positive). An important reason for the low sensitivity in evaluating the ALL can be seen in the low field strength of the used scanner (.4 T). Furthermore, in particular lesions of the ALL can, according to our experience, be very subtle, and secondary findings as prevertebral haematoma can lead the radiologist on the right track. Goradia et al found similar results concerning the ALL (sensitivity 71%) with fat‐saturated T2‐weighted and STIR sequences.15 Also Zhuge et al showed comparable results to our study (using a 1.5 T scanner) and found a sensitivity and specificity of 100% in detecting injury to the ALL with MRI.17 They concluded that caution should be exercised when using MRI for operative decision making due to its less predictable specificity for detecting injuries of paraspinal muscles, intervertebral disc, and interspinous ligament.
In patients with pre‐existing cervical canal stenosis caused by degenerative disease, hyperextension injuries may lead to relevant cord compression.23 In this type of injury, a discoligamentous lesion may be absent. MRI is then the only modality to show a pathology to the spinal cord. In our study, in 3 patients no tearing of the ALL was found intraoperatively, whereas 2 of 3 also did not show any traumatic lesion to the intervertebral disc (beside edema of the spinal cord), only degenerative changes with pre‐existing degenerative disease were noted. In our study, edema and/or hemorrhage of the spinal cord was present in 16 of 21 patients, whereas 16 of 16 had an intraoperatively confirmed pathology. This suggests that in this patient group, the sheer presence of spinal cord edema and/or hemorrhage is usually associated with a lesion of the ALL and/or intervertebral disc.
The presence of a prevertebral hematoma also showed a relevant correlation: only 1 patient without a hematoma had a lesion of the intervertebral disc without any intraoperative sign of an ALL tear; 2 patients with no intraoperative lesion of the ALL, PLL or intervertebral disc showed a prevertebral hematoma. Therefore, the prevertebral hematoma is a good indicator and should be used as a relevant ancillary feature in discoligamentous injury, which is also supported by the study of Maeda et al.23 We hypothesize that a missing prevertebral hematoma can rule out injury of the ALL for nearly 100%. In addition, the maximum thickness of the prevertebral hematoma can serve as an orientation for a possibly better detection of the correct anatomic level (based on the segment) of the lesion.
In general, from a practical point of view, when reviewing cases with suspected cervical injury we strongly recommend to zoom into the MR images, because pathological changes can sometimes be very subtle and, therefore, easily missed when reviewing images on small views. The STIR sequence is again the workhorse sequence and should be reviewed first. Finally, hematoma prevertebral or in the dorsal soft tissue can give important information and serve as an indirect sign. The spinal cord should be reviewed with all available sequences, also on the axial plane in order to minimize misinterpretation due to artifacts. In cases of an edema of the spinal cord and narrowing of the spinal canal, a degenerative reason for the clinical appearance should be considered.
It has to be noted that sagittal T1‐weighted images were not included in our assessment, because due to its poor rendering of fluid, which is always present in the case of an acute injury, this sequence does not help in the evaluation of the ALL and the intervertebral disc.22 Nevertheless, we suggest to include the assessment of T1‐weighted images for the reporting, especially with respect to bony changes and for surveying the anatomy and caliber of the spinal cord.8
The number of patients for our study is rather small in relation to a timeframe of 8 years. One reason for this is that we based our study on patients without any sign of fracture or instability on MDCT. At our department, patients with clear fractures or conspicuousness on MDCT are also operated without a MR examination. MRI is mainly used in patients without osseous abnormalities at MDCT but with a high index of suspicion of injury. The major limitation of our study is that the two reviewers were aware that all reviewed patients underwent surgery of the cervical spine. This can be seen as an inherent verification bias as the reviewers expected lesions and, thus, more carefully inspected the MR images. However, subsequently this also reveals an important fact: the evaluation of the cervical spine after a major trauma can sometimes bring up only subtle changes and the radiologist has to carefully search for such changes. Furthermore, our study is limited because the PLL was not assessed intraoperatively in all patients and, therefore, no general correlation was possible. Nevertheless, high sensitivity and specificity for the MRI evaluation of the PLL have already been reported in literature.14, 17 Although MRI could not reach a 100% correlation with intraoperative findings, it can still be considered as a reliable and important tool for the evaluation of discoligamentous injuries in the cervical spine. Overinterpretation is still a problem, but ancillary features can help to minimize this.
Conflict of Interest: The authors declare no conflict of interest.
References
- 1. Utz M, Khan S, O'Connor D, Meyers S. MDCT and MRI evaluation of cervical spine trauma. Insights Imaging 2014;5:67‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rao SK, Wasyliw C, Nunez DB, Jr. Spectrum of imaging findings in hyperextension injuries of the neck. Radiographics 2005;25:1239‐54. [DOI] [PubMed] [Google Scholar]
- 3. Dundamadappa SK, Cauley KA. MR imaging of acute cervical spinal ligamentous and soft tissue trauma. Emerg Radiol 2012;19:277‐86. [DOI] [PubMed] [Google Scholar]
- 4. Jackson AB, Dijkers M, Devivo MJ, Poczatek RB. A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehabil 2004;85:1740‐8. [DOI] [PubMed] [Google Scholar]
- 5. Benedetti PF, Fahr LM, Kuhns LR, Hayman LA. MR imaging findings in spinal ligamentous injury. AJR Am J Roentgenol 2000;175:661‐5. [DOI] [PubMed] [Google Scholar]
- 6. Munera F, Rivas LA, Nunez DB, Jr. , Quencer RM. Imaging evaluation of adult spinal injuries: emphasis on multidetector CT in cervical spine trauma. Radiology 2012;263:645‐60. [DOI] [PubMed] [Google Scholar]
- 7. Morais DF, de Melo Neto JS, Meguins LC, Mussi SE, Filho JR, Tognola WA. Clinical applicability of magnetic resonance imaging in acute spinal cord trauma. Eur Spine J 2014;23:1457‐63. [DOI] [PubMed] [Google Scholar]
- 8. Kumar Y, Hayashi D. Role of magnetic resonance imaging in acute spinal trauma: a pictorial review. BMC Musculoskelet Disord 2016;1:310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin JL, Samuel S, Gray R, et al. Occult subaxial cervical disco‐ligamentous injuries in computer tomography negative trauma patients. Eur Spine J 2017;26:1277‐83. [DOI] [PubMed] [Google Scholar]
- 10. Chiu WC, Haan JM, Cushing BM, Kramer ME, Scalea TM. Ligamentous injuries of the cervical spine in unreliable blunt trauma patients: incidence, evaluation, and outcome. J Trauma 2001;50:457‐63. [DOI] [PubMed] [Google Scholar]
- 11. Demetriades D, Charalambides K, Chahwan S, et al. Nonskeletal cervical spine injuries: epidemiology and diagnostic pitfalls. J Trauma 2000;48:724‐7. [DOI] [PubMed] [Google Scholar]
- 12. Hendey GW, Wolfson AB, Mower WR, Hoffman JR, National Emergency XRUSG . Spinal cord injury without radiographic abnormality: results of the National Emergency X‐Radiography Utilization Study in blunt cervical trauma. J Trauma 2002;53:1‐4. [DOI] [PubMed] [Google Scholar]
- 13. Harris JH, Yeakley JW. Hyperextension‐dislocation of the cervical spine. Ligament injuries demonstrated by magnetic resonance imaging. J Bone Joint Surg Br 1992;74:567‐70. [DOI] [PubMed] [Google Scholar]
- 14. Haris AM, Vasu C, Kanthila M, Ravichandra G, Acharya KD, Hussain MM. Assessment of MRI as a modality for evaluation of soft tissue injuries of the spine as compared to intraoperative assessment. J Clin Diagn Res 2016;10:TC01‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goradia D, Linnau KF, Cohen WA, Mirza S, Hallam DK, Blackmore CC. Correlation of MR imaging findings with intraoperative findings after cervical spine trauma. AJNR Am J Neuroradiol 2007;28:209‐15. [PMC free article] [PubMed] [Google Scholar]
- 16. Malham GM, Ackland HM, Varma DK, Williamson OD. Traumatic cervical discoligamentous injuries: correlation of magnetic resonance imaging and operative findings. Spine (Phila Pa 1976) 2009;34:2754‐9. [DOI] [PubMed] [Google Scholar]
- 17. Zhuge W, Ben‐Galim P, Hipp JA, Reitman CA. Efficacy of MRI for assessment of spinal trauma: correlation with intraoperative findings. J Spinal Disord Tech 2015;28:147‐51. [DOI] [PubMed] [Google Scholar]
- 18. R Development Core Team . The R project for statistical computing, Version 3.2.5, Vienna, Austria. Available at: http://www.R-project.org. Accessed March 12, 2019.
- 19. Zec S, Soriani N, Comoretto R, Baldi I. High agreement and high prevalence: The paradox of Cohen's kappa. Open Nurs J 2017;11:211‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gwet KL. Computing inter‐rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol 2008;61:29‐48. [DOI] [PubMed] [Google Scholar]
- 21. Martire RL. Reliability Coefficients . R package version 1.3.1. Available at: https://CRAN.R-project.org/package=rel. Accessed March 12, 2019.
- 22. Saifuddin A, Green R, White J. Magnetic resonance imaging of the cervical ligaments in the absence of trauma. Spine (Phila Pa 1976) 2003;28:1686‐91. [DOI] [PubMed] [Google Scholar]
- 23. Maeda T, Ueta T, Mori E, et al. Soft‐tissue damage and segmental instability in adult patients with cervical spinal cord injury without major bone injury. Spine (Phila Pa 1976) 2012;37:E1560‐6. [DOI] [PubMed] [Google Scholar]


