Abstract
Objectives
The well‐being of doctors is at risk, as evidenced by high burnout rates amongst doctors around the world. Alarmingly, burned‐out doctors are more likely to exhibit low levels of professionalism and provide suboptimal patient care. Research suggests that burnout and the well‐being of doctors can be improved by mindfulness‐based interventions (MBIs). Furthermore, MBIs may improve doctors’ performance (eg in empathy). However, there are no published systematic reviews that clarify the effects of MBIs on doctor well‐being or performance to inform future research and professional development programmes. We therefore systematically reviewed and narratively synthesised findings on the impacts of MBIs on doctors’ well‐being and performance.
Methods
We searched PubMed and PsycINFO from inception to 9 May 2018 and independently reviewed studies investigating the effects of MBIs on doctor well‐being or performance. We systematically extracted data and assessed study quality according to the Medical Education Research Study Quality Instrument (MERSQI), and narratively reported study findings.
Results
We retrieved a total of 934 articles, of which 24 studies met our criteria; these included randomised, (un)controlled or qualitative studies of average quality. Effects varied across MBIs with different training contents or formats: MBIs including essential mindfulness training elements, or employing group‐based training, mostly showed positive effects on the well‐being or performance of doctors across different educational and hospital settings. Doctors perceived both benefits (enhanced self‐ and other‐understanding) and challenges (time limitations and feasibility) associated with MBIs. Findings were subject to the methodological limitations of studies (eg the use of self‐selected participants, lack of placebo interventions, use of self‐reported outcomes).
Conclusions
This review indicates that doctors can perceive positive impacts of MBIs on their well‐being and performance. However, the evidence was subject to methodological limitations and does not yet support the standardisation of MBIs in professional development programmes. Rather, health care organisations could consider including group‐based MBIs as voluntary modules for doctors with specific well‐being needs or ambitions regarding professional development.
Short abstract
Mindfulness is often promoted as a means to facilitate well‐being and performance. This review offers guidance regarding the essential interventional elements that determine perceptions of impact.
1. INTRODUCTION
The medical community has increasingly acknowledged that competent professionals are committed not only to the well‐being of patients, but also to their own well‐being.1, 2 In medical education, the CanMEDS framework has included commitment to personal well‐being as a key competency of professionalism.3 However, translating this competency into daily medical practice can be challenging.4, 5 Medical practice involves working in a dynamic and stressful practice environment, in which doctors have limited time and resources available to nurture their own well‐being.6 Doctor well‐being is reflected by a combination of a doctor's physical, psychological and occupational health, which, overall, are vital for doctors to thrive and achieve success in various areas of personal and professional life.6, 7 Hence well‐being involves more than the absence of distress,7 and is reflected by a variety of both positive (eg job satisfaction) and negative (eg burnout) indicators.8, 9
Alarmingly, doctors increasingly report poor well‐being, evidenced by high burnout rates amongst doctors worldwide.10, 11, 12, 13, 14 Doctor burnout has been related to the various demands of modern practice (eg workload and administrative burden).7, 15, 16 These demands decrease autonomy and interfere in relationships with patients, thereby eroding doctors’ energy levels and their sense of meaning in their work.17, 18, 19, 20 Research has suggested that the process of reconnecting and enhancing meaning could benefit from mindfulness: awareness that arises through the paying of purposeful and non‐judgemental attention to the present moment in a stressful practice environment.21, 22, 23, 24 In times of stress, doctors often respond by working harder. Mindfulness offers an alternative: increasing doctors’ awareness of stress and of their own emotions and needs, promoting self‐regulation, and facilitating self‐reflection on their behaviours and clinical practice.25
A qualitative study has shown that residents experience mindfulness as helping them to become more aware of stress, proactively set priorities and limits, and develop a healthier relationship to work in a stressful practice environment.25 Ultimately, residents and specialists who practise mindfulness report lower levels of burnout, as indicated by reviews.26, 27, 28, 29 Therefore, mindfulness‐based interventions (MBIs) are increasingly implemented in medical education and practice.27, 28 Such interventions employ mindfulness meditation and other approaches to promote awareness and attentiveness, such as those adopted by the widely used Mindfulness‐Based Stress Reduction (MBSR) programme.30, 31, 32, 33 Some studies have suggested that MBIs could promote positive well‐being (eg positive mental health).31, 34 However, this evidence has not yet been systematically reviewed; previous reviews on MBIs exclusively investigated negative well‐being outcomes.26, 27, 28, 29
In addition to their potential benefits for well‐being, studies have suggested that MBIs could facilitate doctors’ performance in relation to doctors’ activities in providing patient care.35, 36, 37 In providing patient care, mindful doctors may be more likely to perform better in interpersonal domains: they are trained to have a non‐judgemental attitude towards thoughts and feelings, and therefore may more openly listen and empathically respond to patients’ worries and emotions.38, 39, 40 As MBIs enhance attention and awareness, they may also facilitate performance in safety domains (eg with reference to medical error).41, 42 However, previous reviews have not clarified whether or how the interpersonal or safety domains of doctor performance are affected by MBIs.
Mindfulness‐based interventions are most effective when embedded in an organisational approach that promotes a culture of wellness to doctors in various educational phases (ie from postgraduate to continuing medical education) when also addressing system‐related demands (eg workloads).28, 43, 44 Adequate design of this approach is facilitated by insights into the effects of MBIs as these could, for example, guide medical educators and faculty developers to effectively tailor MBIs to meet doctors’ diverse well‐being and professional development needs. However, previous research has not systematically reviewed how mindfulness is trained in postgraduate and continuing medical education, and how residents and specialists perceive the impact of MBIs on their well‐being and performance. Therefore, we conducted a systematic review of the impact of MBIs on well‐being and performance in residents and specialists.
2. METHODS
Starting the review, the authors (RAS, HE, RME and KMJMHL) agreed upon the eligibility criteria, search strategy, study selection, data extraction and quality assessment. The review process was reported according to the PRISMA (preferred reporting items for systematic reviews and meta‐analyses) standards.45
2.1. Eligibility criteria
Studies were eligible when they examined the effects of MBIs on indicators of well‐being or performance in medical practice. The MBIs included interventions that adopted a mindfulness approach to train ‘purposeful and non‐judgemental attention to present experiences, thoughts and feelings.’22 We included studies in which doctor well‐being or performance were main outcomes and were reported for doctors as the entire sample or as a subgroup. We excluded non‐empirical articles (including letters, comments and editorials) and articles in languages other than English or Dutch.
2.2. Data sources and searches
We searched the electronic databases PubMed and PsycINFO from inception to 9 May 2018. To prevent the omission of relevant articles, we developed a broad search strategy that included the use of index terms and free text on the subjects’ ‘mindfulness’ and ‘doctors’ (Appendix S1 gives the full search string). As well‐being and performance can be measured by various indicators and this review was the first to map these, we did not include predefined search terms; we systematically assessed the issue of whether studies included indicators of well‐being or performance based on full‐text review (see study selection). Furthermore, we performed a manual search in the references of eligible studies and related reviews on this topic.
2.3. Study selection
One researcher (RAS) performed the search and then reviewed it with members of the research team. In the first stage, two researchers (HE and RAS) independently screened both titles and abstracts and excluded non‐empirical studies and studies that did not include the subjects ‘mindfulness’ and ‘doctors’. When abstracts were unavailable, two researchers (HE and RAS) independently reviewed the titles to exclude obviously non‐relevant articles. In the second stage, two researchers (HE and RAS) independently reviewed the full‐text articles. Disagreements were discussed and resolved by consensus between the researchers.
2.4. Data extraction and analysis
The articles were distributed to two researchers (HE and RAS), who independently extracted data on the study design, participants and setting, intervention type, measurements and study findings. To reach a uniform extraction procedure, the first five articles were checked and discussed within the research team. The researchers then assessed the completeness and accuracy of extracted data for all articles.
We used the Medical Education Research Study Quality Instrument (MERSQI) to assess study quality on 10 criteria: study design; number of institutions; response rate; type of data; internal structure; content validity; criterion validity; appropriateness of data analyses; sophistication of data analyses, and outcome level. The possible total MERSQI score can range from 5 to 18. Evidence for the validity of the MERSQI has been shown to be strong.46, 47 Two researchers independently assessed study quality; in the event of disagreement, the researchers discussed the issue and reached a decision by consensus.
Because of great heterogeneity in well‐being and performance outcomes, we did not conduct a meta‐analysis. Studies were also heterogeneous in intervention characteristics (training content or format) and the educational settings under study, and participating doctors reported various benefits and challenges in the context of MBIs. Given this heterogeneity, reporting the outcomes of MBIs at an aggregated level was not meaningful. Therefore, we reviewed findings in the context of the heterogeneous study characteristics with regard to the intervention (training content or format), study setting (postgraduate or continuing medical education), and benefits and challenges of MBIs. Systematic comparisons across studies allowed the research team to report varying findings of heterogeneous studies in a narrative manner, when also considering study quality and methodological limitations.48
3. RESULTS
3.1. Search results
The search yielded 934 unique hits (Figure 1). The screening of titles and abstracts resulted in 79 potentially eligible articles. Full‐text screening resulted in the retaining of 25 articles; two articles reported different outcomes of the same study and were analysed as representing one study.49, 50 This resulted in the inclusion of 24 studies (Table S1).
Figure 1.
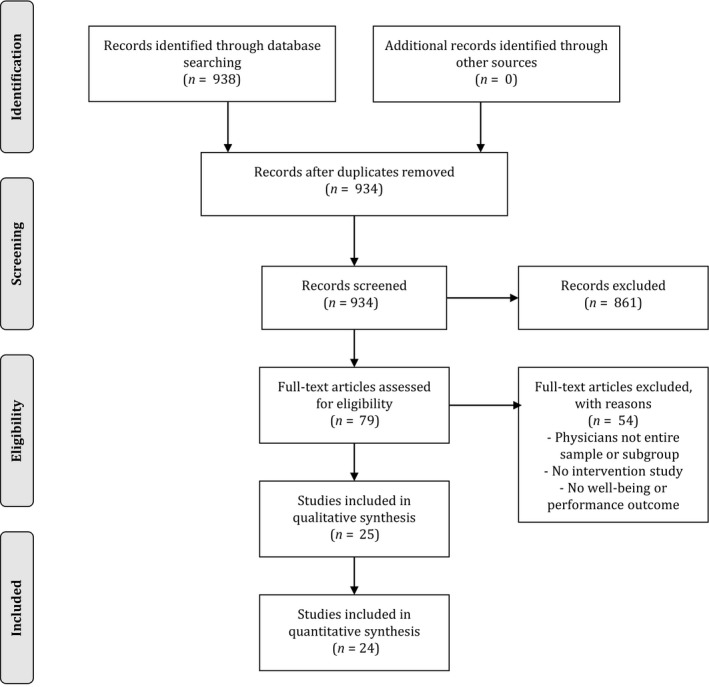
PRISMA (preferred reporting items for systematic reviews and meta‐analyses) flow chart of the review process
3.2. Study quality
Scores for the quality of the studies ranged between 6.5 and 14.5 on the MERSQI scale; the mean score was 9.9, reflecting average quality (Table S2).47 The eligible studies included seven randomised controlled trials (RCTs),49, 50, 51, 52, 53, 54, 55, 56 three non‐randomised controlled trials (CTs),57, 58, 59 12 pre‐post studies,60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71 and two qualitative interview studies25, 72 (Table S1). Of the RCTs and CTs, four studies employed a waitlist control condition,51, 55, 56, 57 four studies employed a passive control condition,49, 53, 58, 59 and two studies exposed controls to protected free time during the intervention period.52, 54 In all but one study,66 participation in the MBI was voluntary and based on self‐selection. Response rates for survey completion were between 75% and 100% in seven studies,54, 56, 58, 62, 67, 68, 72 between 50% and 74% in three studies,25, 51, 71 and below 50% (or were not reported) in 14 studies.49, 50, 52, 53, 55, 57, 59, 60, 61, 63, 64, 65, 66, 69, 70 Eight were multicentre studies.57, 58, 61, 62, 63, 67, 69, 72 Indicators of instrument validity (eg internal consistency, content or criterion validity) were inconsistently reported (Table S2).
3.3. Study characteristics
The eligible studies had been conducted in Europe, the USA and Australia, and included residents or licensed doctors from diverse specialties (emergency medicine, general practice, internal medicine, paediatrics, psychiatry, radiology, surgery and mixed specialty samples) (Table S1). All studies measured the outcomes of an MBI immediately after the intervention, and four studies also measured outcomes after 2 months64 or 3 months.52, 62, 67
Outcomes regarding doctor well‐being specifically targeted physical, psychological and occupational domains. Studies on physical well‐being measured heart rate and blood pressure,49, 50 and self‐reported physical health.61 Psychological well‐being was studied by questionnaires on anxiety,51, 56 depression,52, 60 mental health,55, 61 mood,62 negative affect,49, 69, 71 perceived stress,51, 52, 54, 58, 63, 64, 67, 68 positive affect,69, 71 relaxation states,50 resilience56 and quality of life.51, 52, 56 Occupational well‐being was measured by questionnaires on burnout,49, 52, 54, 55, 57, 59, 60, 61, 62, 64, 65, 66, 67, 69, 70 empowerment at work,52 job satisfaction,52, 58 specialty satisfaction58 and work engagement.57, 58 Self‐perceived physical and mental health52 or fatigue56 reflected both physical and psychological well‐being.
Outcomes regarding doctors’ performance focused on both interpersonal and safety indicators. Interpersonal indicators of performance involved empathy52, 55, 57, 58, 62, 66, 68 and psychosocial orientation.62 Safety indicators of performance were investigated by observed hand hygiene adherence,53 and self‐reported medical errors55 or cognitive failures.60
3.4. Study findings
The study findings showed effects of MBIs on well‐being and performance to vary based on training content, training format and across educational settings (ie postgraduate or continuing medical education). Furthermore, the effects of MBIs varied following specific benefits and challenges of MBIs, which were based on doctors’ perceptions of why these MBIs were (not) effective (see below).
3.5. Training content of MBIs
Based on the conceptual framework on mindfulness interventions of Crane et al, the training content of MBIs can be defined by five different elements: (i) integration of mindfulness theory; (ii) provision of didactic information on mindfulness; (iii) development of self‐awareness about thoughts, feelings and bodily sensations; (iv) promotion of attentive and behavioural self‐regulation and positive qualities (curiosity, joy, compassion), and (v) training of meditation practice (Box 1).73 The studies included in this review showed variability in the specific elements adopted and ranged from studies that consistently included all elements of MBIs, to studies that included only one element (Table S3). Mindfulness‐based interventions with different elements showed variable effects on the well‐being or performance of participants (see below).
BOX 1. Elements of training content of mindfulness‐based interventions* .
1.
| Mindfulness theory | Is informed by theories that follow from a combination of contemplative traditions and science (medicine, psychology, education) |
| Didactic information on mindfulness | Addresses how distress is created and maintained, and how mindfulness deals with alleviating distress |
| Self‐awareness | Develops self‐awareness of experience characterised by present moment focus, decentring and an approach orientation |
| Self‐regulation | Supports attentional, emotional and behavioural self‐regulation, as well as positive qualities (eg compassion, wisdom, equanimity) |
| Meditation practice | Involves participants in training of mindfulness meditation practice |
Based on the framework of Crane et al.73
3.5.1. Effects of MBIs with all mindfulness intervention elements
Nine studies included all mindfulness elements as defined by Crane et al73 (Table S3). These studies employed MBIs that were based on validated mindfulness programmes (ie MBSR or Mindfulness‐Based Cognitive Therapy [MBCT]). The MBSR programme, designed by Jon Kabat‐Zinn, involves group‐based discussions and practices focused on applying mindfulness in daily life; MBCT is an adapted version of MBSR that specifically focuses on cognitive self‐regulation.74 Studies on MBSR and MBCT reported positive effects on well‐being or performance.49, 50, 54, 55, 57, 61, 66, 67, 68 Positive effects on performance were particularly found for interpersonal domains (ie empathy towards patients).55, 58, 66, 68 By contrast, no effect was reported on safety domains of performance (ie self‐reporting of medical errors).55 Well‐being specifically improved on psychological (stress, worry, relaxation) or occupational (burnout, dedication) domains.49, 50, 54, 55, 57, 61, 67, 68
However, not all well‐being outcomes were affected (ie positive mental health or work engagement).55, 58 Furthermore, not all studies on MBSR reported the same effects on well‐being or performance, which was, in part, the result of heterogeneous outcome measures across studies (Table S1). For example, two studies on MBSR investigated different indicators of physical well‐being, resulting in different effects: self‐reported physical well‐being did not improve,61 whereas heart rate and blood pressure did.49 In addition, variable findings were subject to the variable quality of the studies, which ranged from RCTs49, 55 to qualitative evaluations,25, 57 and small (underpowered) uncontrolled pre‐post studies.66, 68 Even the studies of higher quality did not employ placebo‐based interventions, and included self‐selected participants, all of which limited the robustness of evidence on the effects of MBSR and MBCT.
3.5.2. Effects of MBIs with variable mindfulness intervention elements
A total of 15 studies included multiple but fewer than five of the elements defined by Crane et al73 (Table S3). The majority of these studies included elements involving didactic information on mindfulness (10 studies) or meditation practice (11 studies). However, fewer studies integrated mindfulness theory (six studies), or addressed self‐awareness or self‐regulation (seven studies for each). Studies that adopted a multi‐faceted MBI with multiple (four of five) mindfulness elements mostly reported positive effects on well‐being. These effects were reported for diverse indicators of psychological (anxiety, stress, quality of life, mood, positive affect) or occupational (burnout, job satisfaction) well‐being.51, 56, 58, 62, 69 However, not all indicators of well‐being (negative affect, burnout) improved when mindfulness training elements were specifically incorporated in web‐based rather than group‐based programmes (see Training approaches of MBIs).69
Mindfulness‐based interventions that included only one or two training elements purposefully targeted and improved specific, rather than diverse, well‐being or performance outcomes.53, 59, 63, 71 This was reflected in the training content; an MBI that promoted collegiality and community at work specifically targeted occupational well‐being (burnout, empowerment at work).52 Other MBIs used meditation or mental silence to specifically alleviate stress,59, 63, 64 or promoted mindful awareness to target safety performance (hand hygiene adherence).53 It is unknown whether target outcomes were presented to participants in advance (this was not reported in the studies), and thus, whether the findings were subject to overestimation bias as outcomes were in all (but one53) studies self‐reported.
3.6. Training format of MBIs
Effects on well‐being or performance also differed amongst MBIs with varying training formats, including the MBI trainers, training delivery (web‐based or group‐based), and length of the MBI. Firstly, MBI trainers varied from certified trainers to trained doctors (from the same or another department). The use of certified, independent trainers is considered best practice by validated MBSR and MBCT programmes73 and such trainers were indeed most often selected by the included studies.25, 49, 50, 55, 57, 61 By contrast, independently trained doctors were specifically appointed in MBIs that also focused on shared experiences with the implementing of mindfulness in daily clinical practice. In such cases, the trainer's own medical experience may be helpful in guiding the discussion.52, 65, 67, 68 However, in one study the trainer was also the programme director of participating residents, which may have potentially introduced social desirability into the training process and residents’ reported outcomes.68 Trainers were specially appointed in studies on group‐based MBIs (21 studies), but not in studies focusing on web‐based MBIs (three studies). Web‐ and group‐based MBIs showed different effects on well‐being and performance.
3.6.1. Effects of web‐ and group‐based MBIs
Web‐based MBIs adopted an individual approach in teaching mindfulness using smartphone‐ or Internet‐based exercises. These MBIs showed mixed effects on well‐being.69, 70, 71 Specifically, negative indicators of well‐being (negative affect, burnout) were not affected, whereas improvements in well‐being based on positive indicators (positive affect) were reported, although these were based exclusively on non‐randomised and uncontrolled studies that made no qualitative evaluation of participants’ experiences with MBIs.
Group‐based MBIs included mindfulness training sessions in combination with mindfulness exercises carried out at home. These MBIs were employed by studies that showed high variability in quality and ranged from larger RCTs with qualitative evaluations, to small non‐randomised and uncontrolled studies (Table S1). Despite this variability in study quality, studies were consistent in showing positive effects on well‐being or performance. Performance improved in interpersonal domains (empathy or psychosocial orientation),55, 57, 58, 62, 66, 68 although these findings were based on self‐reported outcomes. Well‐being improved on psychological (anxiety, mental health, mood, relaxation, resilience, stress, worry, quality of life) and occupational (burnout, empowerment at work, specialty satisfaction, dedication) domains.50, 51, 54, 55, 56, 57, 58, 59, 61, 62, 64, 67 Although the diverse study designs, and the different outcomes under study, precluded the interpretation of findings at an aggregated level, the mixed (quantitative and qualitative) methods did contribute to the triangulation of the research. Effects of group‐based MBIs did, however, differ for training approaches of different lengths. The programme length of MBIs varied from short‐term (one to two sessions)51, 53, 56, 60, 63, 65 to medium‐term (2‐3 months)25, 49, 50, 54, 55, 57, 58, 59, 61, 62, 66, 67, 68, 72 and long‐term (9 months)52 training approaches.
3.6.2. Effects of short‐, medium‐ and long‐term MBIs
Short‐term MBIs ranged from single‐session MBIs51, 53, 56, 63 to two‐session MBIs60 or a 2‐day mindfulness retreat.65 Short‐term MBIs resulted in effects on well‐being (stress, anxiety, burnout) in the context of explicit discussions of strategies for persevering in mindfulness practice,53, 63, 65 or following participants up after the intervention.51, 56 These training components may be of particular relevance for short‐term MBIs, although the long‐term effectiveness of these MBIs was unclear.
Medium‐term MBIs employed programmes of 2‐3 months in length, with weekly classes. These MBIs were more consistent in both training approach and effects: medium‐term MBIs positively affected well‐being (stress, burnout or job satisfaction) or performance (empathy or psychosocial orientation),50, 54, 55, 57, 58, 59, 61, 62, 64, 66, 67, 68 as was also evident at 2‐ or 3‐month follow‐ups.62, 64, 67 Two medium‐term MBIs also included a maintenance phase after the main intervention programme, involving monthly training sessions during 10 months; these studies showed well‐being improvement to be sustained during the maintenance phase.50, 62
Long‐term MBIs were investigated in only one study involving a 9‐month, small‐group learning programme on mindfulness.52 The programme promoted well‐being in work through collegiality, community and shared experience, which improved occupational well‐being (burnout, empowerment at work), but not psychological well‐being (depression, stress) or interpersonal performance (empathy).
3.7. Settings of MBIs
Studies were conducted in the settings of postgraduate or continuing medical education, focusing on either residents or specialists (Table S1).
3.7.1. Effects of MBIs in postgraduate medical education
In postgraduate medical education, departments or hospitals presented MBIs as opportunities for residents to invest in their professional development on a voluntary basis. Occasionally, MBIs might be included in training portfolios.55 Residents from diverse specialties (mixed specialties, or emergency medicine, paediatrics, psychiatry or surgery) participated (Table S1). In psychiatry in particular, no effects on well‐being were reported, although these findings were reported by uncontrolled studies with power limitations.66, 68 In other specialties, randomised and controlled studies showed positive effects on psychological (stress, worry) or occupational (burnout, specialty satisfaction) domains of well‐being, specifically following medium‐term, group‐based MBIs.25, 54, 55, 58, 59 However, these positive effects may not apply equally to all residents.55 Specifically, residents with poor well‐being at baseline (ie high levels of exhaustion) were more likely to benefit from MBIs than residents with high levels of well‐being at baseline (ie low levels of exhaustion).55 This finding aligned with residents’ recommendations that participation in MBIs should be especially promoted amongst residents in need of better well‐being.58
3.7.2. Effects of MBIs in continuing medical education
In the setting of continuing medical education, departments or hospitals, or regional or national medical associations organised MBIs for medical specialists who wished to invest in their professional development (on a voluntary basis). Some studies reported that specialists could receive education credits61 or include the MBI in their portfolio.57 Studies focused on general practice or the hospital‐based context (mixed specialty samples or internal medicine, psychiatry, radiology) (Table S1). Specialists in the hospital‐based context reported positive effects of group‐based MBIs on their well‐being with respect to psychological (anxiety, stress, relaxation) or occupational (burnout, empowerment at work) domains.50, 51, 52, 56, 64 General practitioners also reported positive effects on psychological (stress, mood) or occupational (burnout, work engagement) well‐being.57, 62, 67
Qualitative findings related positive effects to specific mindfulness elements: self‐awareness of stress and self‐regulation of behaviours facilitated self‐care of well‐being.57 However, the group‐based setting of an MBI, which promoted shared experience and peer support, also appeared beneficial for well‐being.57, 72 Specifically, general practitioners noticed that sharing experiences with peers helped them to deal with stressful events by providing reassurance that they were not alone in their feelings. This was particularly relevant to general practitioners working in solo practices as they reported that participation in an MBI reduced their sense of professional isolation.72
3.8. Benefits and challenges of MBIs
Both qualitative interview studies and mixed‐method studies provided insight into specific benefits and challenges that clarified why MBIs did or did not affect well‐being or performance.
3.8.1. Benefits of MBIs
The reported benefits of MBIs were related to enhanced self‐understanding or understanding of others (ie patients or peers).25, 53, 57, 58, 65, 66, 72 Self‐understanding increased in response to better self‐awareness of stress following an MBI, as well as greater reflection on one's own behaviours that were (un)helpful in dealing with stress.25, 57, 66 Ultimately, enhanced self‐understanding helped participants to change automatic patterns in order to make more deliberate choices and take better care of their own well‐being.25, 57 This process of better self‐understanding, in combination with a less judgemental attitude towards emotions and uncertainties, also stimulated participants to set priorities and limits more clearly, and to ask peers for help more easily. These benefits of MBIs supported participants in their goals to continuously nurture and enhance their own well‐being.
Understanding of others was specifically facilitated by acceptance of one's own as well as others’ emotions following mindfulness practice.25, 57 Specifically, participants reported that their more open and curious focus on feelings present in themselves and others improved their reflective listening and their ability to see patients’ perspectives.65, 66 Furthermore, participants noted that they became more accepting of and compassionate towards patients as they recognised their shared humanity.25, 57 Ultimately, participants perceived mindfulness as improving the doctor‐patient relationship,53 in line with quantitative effects of MBIs on interpersonal domains of performance.55, 57, 58, 62, 66, 68 Both the quantitative and qualitative findings were, however, subject to selection bias (given the self‐selection of participants) and overestimation bias (given the self‐reporting of empathy).
3.8.2. Challenges of MBI
In addition to benefits, studies also reported challenges associated with MBIs; these specifically included limitations to time and feasibility in daily practice.25, 53, 57, 58, 65, 66, 72 Time was one of the major challenges as practising mindfulness required an investment of time, but participants felt guilty about taking time for their own professional development and, consequently, spending less time on work or home responsibilities.72 Mindfulness‐based interventions differed in the degree of time investment required as some MBIs were organised during protected work time,53, 54, 57 whereas others were organised in the evenings.49, 55, 67 Many MBIs prescribed that participants should practise mindfulness at home (eg for 45 minutes per day).49, 55, 57, 61, 68, 69 Although these time investments in the evenings or at home could put further pressure on the work‐home balance, findings also showed that mindfulness helped participants to protect their work‐home balance: awareness of stress and self‐reflection on values facilitated participants in setting priorities and limits to work demands.25
The feasibility of practising mindfulness was considered challenging as participants reported that exercising mindfulness was difficult to sustain in daily life.58 In daily practice, high workloads or patient volumes were a barrier to being and staying mindful.66 To enhance the feasibility of daily practice, participants recommended engaging in brief moments of mindfulness with the whole team, for example before doing rounds.53 In addition, different MBIs provided room for discussion and the sharing of experiences of how to apply mindfulness in daily life.58, 65 For example, residents reported that brief exercises, such as mindful breathing, were applicable in daily practice as they could be purposefully used in advance of a stressful situation (eg before performing an operation).58 Overall, doctors recognised that practising mindfulness met unfulfilled needs to reflect and care for themselves and were motivated to explore its feasibility in the long term.72
4. DISCUSSION
4.1. Main findings
This systematic review found the effects of MBIs to vary across programmes with different training contents or formats, and across educational and hospital settings, when participating doctors perceived both benefits and challenges of MBIs. Mindfulness‐based interventions that included multiple essential mindfulness elements in their training content, or that employed a group‐based training format, mostly showed positive effects.49, 50, 57, 61, 62, 64, 67, 72 These positive effects particularly applied to psychological and occupational domains of well‐being, and to interpersonal performance of residents or specialists in the setting of postgraduate or continuing medical education.49, 50, 54, 55, 57, 61, 66, 67, 68 However, this evidence was subject to the methodological limitations (ie participants were self‐selected, placebo interventions were lacking, outcomes were self‐reported) of randomised, controlled or uncontrolled studies. Mixed‐method or qualitative studies nonetheless reported that residents and specialists perceived benefits of MBIs in the form of enhanced self‐understanding or understanding of others (ie patients).25, 53, 57, 58, 65, 66, 72 However, challenges relating to time and feasibility could hinder the application of mindfulness in daily medical practice, especially in the long term.
4.2. Explanation of findings
Most studies in this review (19 of 24) were published between 2014 and 2018, illustrating the emerging popularity of MBIs in medical practice and education.25, 49, 50, 51, 52, 53, 54, 55, 57, 58, 59, 60, 64, 65, 66, 67, 68, 69, 70, 71 However, this popularity did not result in consensus on the most adequate training design of an MBI: the studies included employed MBIs with variable training content (Table S3). Despite this variability, many studies adopted essential elements of mindfulness, which were most consistently adopted by MBSR or MBCT, both well‐validated forms of MBIs that have been shown to be effective in various professional settings outside medicine.74 In medical practice, MBSR also showed mostly positive effects, although this evidence was subject to methodological limitations (see Limitations).49, 50, 54, 55, 57, 61, 66, 67, 68
Mindfulness‐based interventions other than MBSR and MBCT less consistently adopted essential mindfulness intervention elements, or did not specifically provide training in meditation or contemplative practice. This was surprising as contemplative practice is traditionally considered the core of mindfulness.73, 75 However, in the modern scientific literature mindfulness is also viewed as a sociocognitive concept, involving a mindset of openness to novelty in which individuals give new meaning to their social context.76, 77, 78 This approach was also adopted by some MBIs, for example by stimulating participants to give new meaning to daily routines in clinical practice.53 Specifically, hand hygiene routines were reframed as mindful moments in which to briefly pause and reflect on internal experiences, which was considered valuable and feasible by specialists and residents.53 Another study found that small moments between clinical encounters were experienced as suitable for the brief practice of mindfulness.58 Participants found it valuable to exchange these and other strategies with peers, which, in part, clarified why group‐based MBIs specifically were positively evaluated by participants.25, 72 By contrast, web‐based MBIs did not include the benefits of shared experience or peer support, and showed limited effects on well‐being or performance.69, 70, 71
Group‐based MBIs, in which weekly training sessions took place over the course of 2‐3 months, were designed to allow participants to gradually learn mindfulness and implement it in daily routines. Nonetheless, doctors reported that persevering in mindfulness practice was challenging.53, 58 In this event, a completed MBI could be followed with a maintenance phase, such as by providing participants with a monthly session in which they can refresh their skills and share maintenance strategies with peers.49, 62 Two studies in this review adopted such a maintenance phase and both showed sustained effects on well‐being after the training.50, 62 Other than in these instances, there was limited insight into the sustained effects of an MBI: only four studies measured outcomes at follow‐up, showing improved well‐being (stress or burnout) at 2 months64 or 3 months.52, 62, 67
In other settings, sustained effects of MBIs were shown to last up to 6 years, as demonstrated by a recent RCT conducted in medical students.79 These long‐lasting effects were attributed to an approach‐focused (rather than avoidance‐focused) coping strategy in response to improved self‐awareness and attentive, emotional and behavioural self‐regulation following an MBI. These findings can be explained by the mindfulness to meaning theory, which outlines that mindfulness benefits the ability to cope with poor well‐being by de‐automatising unhelpful negative thoughts, emotions and behaviours.80 This effect of mindfulness on coping also raises the question of whether MBIs should be recommended to all doctors, or only to those who could benefit specifically from more approach‐focused coping in the context of poor well‐being. Indeed, particularly residents with poor well‐being were shown to benefit from MBIs, rather than their peers with high levels of well‐being.55 This finding resonates with residents’ own recommendations that MBIs should be promoted particularly amongst residents or doctors in need of better well‐being.58
However, MBIs may be relevant not only to doctors’ well‐being, but also to their attentiveness and ability to be fully present with patients.25, 72 These capacities have been more strongly associated with finding meaning in work than with diagnostic and therapeutic achievements.81 Therefore, MBIs may be able to address, in part, doctors’ current challenges in finding meaning in their work and connecting with patients in stressful practice environments.18 Indeed, doctors exposed to MBIs reported enhanced connection with patients manifested as a better ability to listen deeply, be attentive to patients’ concerns and effectively respond to patients.25, 55, 58, 62, 66, 68, 72 Patients recognised this as they reported that mindful clinicians (doctors, nurse practitioners and doctor assistants) communicated in a more patient‐centred way, and engaged in rapport building and psychosocial issues to a greater degree.39 Mindfulness‐based interventions may therefore be valuable in enhancing doctors’ empathic and patient‐centred care, although the standardised implementation of MBIs would first require enhanced robustness of evidence.
4.3. Limitations
Like all reviews, this systematic review may have suffered from publication bias, which may lead to an overestimation of the positive impact of MBIs.82 Furthermore, the included studies were of highly variable methodological quality, as found by MERSQI evaluations.46 The eligible studies showed diverse strengths (multicentre designs and randomised or controlled designs), as well as limitations, such as in outcome measures. Specifically, outcome measures were often based on doctors’ self‐reports. However, self‐reports of well‐being are widely accepted in research as well‐being involves a subjective experience that inherently requires evaluation by the respondent.83, 84 The studies in this review employed validated measures of self‐reported well‐being.
Notwithstanding this, performance involves behaviours in clinical practice, and in this case patient or peer reports are generally considered more reliable than self‐reports.85 Research has nonetheless shown that self‐ and patient reports can provide comparable insights into doctors’ performance on empathy.86 One study in this review included observer reports of performance, showing positive effects of an MBI on doctor performance in safety domains (ie hand hygiene adherence). These observer reports, as well as patient‐ or peer‐reported measures, should be employed more often to provide further clarification of the effects of MBIs on doctors’ performance.
Additionally, it is important to be aware that mindfulness studies are often conducted by researchers who are experienced mindfulness practitioners themselves. These experiences may both help and hinder in analysing the effectiveness of an MBI, and therefore the rigorous investigation of the effects of MBIs by both RCTs49, 51, 52, 53, 55 and doctors’ own reports of the effectiveness of MBIs25, 58, 65, 72 represents a positive development. The effects of MBIs are systematically mapped by this review, the findings of which resonate with those of other RCT‐focused reviews on MBIs in non‐medical settings.74
Randomised controlled trials have generally been considered suitable for the study of effectiveness as they can account for possible placebo effects and selection bias.87 However, the RCTs in this review employed waitlist or passive control conditions rather than placebo interventions, and the participation of respondents was voluntary, which may have resulted in selection bias. However, involuntary or obligatory participation would be unfeasible or even unethical. Therefore, future RCTs might report on the characteristics of non‐participants (including their scores on outcome measures) to estimate selection bias. Future RCTs should also employ suitable placebo interventions to enhance the robustness of evidence.88, 89 Furthermore, a combination of RCTs and in‐depth pre‐post and qualitative studies is required to not only evaluate but also clarify the effectiveness of MBIs, as well as to provide insights into doctors’ strategies to translate mindfulness or other self‐care strategies into daily practice.
4.4. Implications
This systematic review indicates that doctors perceive the impacts of MBIs as positive: doctors exposed to MBIs reported lower levels of negative well‐being (burnout, stress and anxiety) and higher levels of positive well‐being (empowerment, dedication and satisfaction).49, 50, 52, 57, 58, 61, 62, 64, 67, 72 However, these positive effects did not necessarily apply to all types of MBI as effects varied across MBIs with different training contents and formats. Hospitals that would like to offer MBIs might consider employing validated mindfulness programmes (MBSR or MBCT) or consistently adopting essential mindfulness elements.73 Furthermore, group‐based training formats that provide space for shared experience and peer support will be more likely to result in positive participant experiences. Individual, web‐based approaches may, in particular cases, be considered when these meet individual preferences or feasibility challenges. Further research should also clarify how and when an MBI should be tailored to meet the needs of doctors with differing levels of well‐being and support, and different coping styles.44, 90, 91
Mindfulness‐based interventions should be combined with organisational changes to promote a supportive work environment that reinforces and does not undermine the effects of an MBI.28 Furthermore, promising findings on the long‐term effects of MBIs79 advocate for intensified research on the effectiveness of incorporating MBIs into medical school curricula in order to equip graduates with mindfulness skills that can be sustained throughout their medical careers. Future studies should also address the effects of MBIs on doctors’ physical well‐being, patient‐reported outcomes and safety indicators of doctors’ performance. Very few studies have addressed these outcomes to date.49, 53 Furthermore, future research would benefit from international collaborations on MBIs with planned variations in training content, format, intensity and length of programme, and systematic investigation of selected (rather than heterogeneous) outcomes, when combining quantitative and qualitative study methods.92 These efforts could help researchers to identify the most optimal training design, and to determine the feasibility and cost benefits of different MBIs for large‐scale implementation.92
5. CONCLUSIONS
The findings of this review showed mostly positive effects of MBIs that included multiple essential mindfulness elements in their training content, or employed a group‐based training format.49, 50, 57, 61, 62, 64, 67, 72 These effects were reported to apply to the well‐being of residents and specialists across different educational or hospital settings, although findings were subject to methodological limitations involving the self‐selection of participants and lack of active control conditions. This level of evidence does not yet support the standardised implementation of MBIs; rather MBIs could be promoted as voluntary modules to doctors in need of better well‐being. These modules should address time and feasibility challenges associated with MBIs. The present findings furthermore indicate that patients may, indirectly, benefit from MBIs: doctors who had undertaken an MBI were reported to provide more empathic and patient‐centred care.25, 55, 58, 62, 66, 68, 72 Yet, as these findings were based on doctor self‐reports, future research should clarify the degree to which MBIs have positive effects on empathic care from the patient perspective.
CONFLICTS OF INTEREST
None.
ETHICAL APPROVAL
Not applicable.
AUTHOR CONTRIBUTION
RAS designed the study, conducted the search, selected the eligible articles, extracted the data and assessed study quality, analysed the results and drafted the article. HE co‐designed the study, selected the eligible articles, analysed the results and critically revised all the sections of the article. RME and KMJMHL co‐designed the study, co‐analysed the results and critically revised all the sections of the article. All authors (RAS, HE, RME and KMJMHL) approved the final manuscript for publication.
Supporting information
ACKNOWLEDGEMENTS
We would like to thank our colleagues of the Professional Performance and Compassionate Care research group for their stimulating feedback on the study.
Scheepers RA, Emke H, Epstein RM, Lombarts KMJMH. The impact of mindfulness‐based interventions on doctors’ well‐being and performance: A systematic review. Med Educ. 2020;54:138‐149. 10.1111/medu.14020
REFERENCES
- 1. Dobkin PL, Hutchinson TA. Primary prevention for future doctors: promoting well‐being in trainees. Med Educ. 2010;44:224‐226. [DOI] [PubMed] [Google Scholar]
- 2. West CP. Empathy, distress and a new understanding of doctor professionalism. Med Educ. 2012;46:243‐244. [DOI] [PubMed] [Google Scholar]
- 3. Frank JR, Snell L, Sherbino J. CanMEDS Physician Competency Framework. Ottawa, ON: Royal College of Physicians and Surgeons of Canada, 2015. [Google Scholar]
- 4. Lases S, Slootweg IA, Pierik E, Heineman E, Lombarts M. Efforts, rewards and professional autonomy determine residents’ experienced well‐being. Adv Health Sci Educ Theory Pract. 2018;23:977‐993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sanchez‐Reilly S, Morrison LJ, Carey E, et al. Caring for oneself to care for others: physicians and their self‐care. J Support Oncol. 2013;11:75‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714‐1721. [DOI] [PubMed] [Google Scholar]
- 7. Shanafelt TD, Sloan JA, Habermann TM. The well‐being of physicians. Am J Med. 2003;114:513‐519. [DOI] [PubMed] [Google Scholar]
- 8. Epstein RM. What's the opposite of burnout? J Gen Intern Med. 2017;32:723‐724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ratanawongsa N, Wright SM, Carrese JA. Well‐being in residency: a time for temporary imbalance? Med Educ. 2007;41:273‐280. [DOI] [PubMed] [Google Scholar]
- 10. Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50:132‐149. [DOI] [PubMed] [Google Scholar]
- 11. Prins JT, Gazendam‐Donofrio SM, Tubben BJ, van der Heijden FM, van d Wiel H, Hoekstra‐Weebers JE. Burnout in medical residents: a review. Med Educ. 2007;41:788‐800. [DOI] [PubMed] [Google Scholar]
- 12. Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88:1358‐1367. [DOI] [PubMed] [Google Scholar]
- 13. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work–life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600‐1613. [DOI] [PubMed] [Google Scholar]
- 14. Prins JT, Hoekstra‐Weebers JEHM, Gazendam‐Donofrio SM, et al. Burnout and engagement among resident doctors in the Netherlands: a national study. Med Educ. 2010;44:236‐247. [DOI] [PubMed] [Google Scholar]
- 15. Rao SK, Kimball AB, Lehrhoff SR, et al. The impact of administrative burden on academic physicians: results of a hospital‐wide physician survey. Acad Med. 2017;92:237‐243. [DOI] [PubMed] [Google Scholar]
- 16. Boerjan M, Bluyssen SJM, Bleichrodt RP, van Weel‐Baumgarten EM, van Goor H. Work‐related health complaints in surgical residents and the influence of social support and job‐related autonomy. Med Educ. 2010;44:835‐844. [DOI] [PubMed] [Google Scholar]
- 17. Slavin SJ, Chibnall JT. Finding the why, changing the how: improving the mental health of medical students, residents, and physicians. Acad Med. 2016;91:1194‐1196. [DOI] [PubMed] [Google Scholar]
- 18. Shanafelt TD. Enhancing meaning in work: a prescription for preventing physician burnout and promoting patient‐centered care. JAMA. 2009;302:1338‐1340. [DOI] [PubMed] [Google Scholar]
- 19. Schifferdecker KE, Reed VA. Using mixed methods research in medical education: basic guidelines for researchers. Med Educ. 2009;43:637‐644. [DOI] [PubMed] [Google Scholar]
- 20. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397‐422. [DOI] [PubMed] [Google Scholar]
- 21. Epstein RM. Mindful practice. JAMA. 1999;282:833‐839. [DOI] [PubMed] [Google Scholar]
- 22. Kabat‐Zinn J, Hanh TN. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. 15th ed New York, NY: Delta; 2009. [Google Scholar]
- 23. Connelly J. Being in the present moment: developing the capacity for mindfulness in medicine. Acad Med. 1999;74:420‐424. [DOI] [PubMed] [Google Scholar]
- 24. Gaufberg E, Hodges B. Humanism, compassion and the call to caring. Med Educ. 2016;50:264‐266. [DOI] [PubMed] [Google Scholar]
- 25. Verweij H, van Ravesteijn H, van Hooff MLM, Lagro‐Janssen ALM, Speckens AEM. Does mindfulness training enhance the professional development of residents? A qualitative study. Acad Med. 2018;93:1335‐1340. [DOI] [PubMed] [Google Scholar]
- 26. Regehr C, Glancy D, Pitts A, LeBlanc VR. Interventions to reduce the consequences of stress in physicians: a review and meta‐analysis. J Nerv Ment Dis. 2014;202:353‐359. [DOI] [PubMed] [Google Scholar]
- 27. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta‐analysis. Lancet. 2016; 388:2272‐2281. [DOI] [PubMed] [Google Scholar]
- 28. Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta‐analysis. JAMA Intern Med. 2017; 177:195‐205. [DOI] [PubMed] [Google Scholar]
- 29. Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ. 2017;9:294‐301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Warnecke E, Quinn S, Ogden K, Towle N, Nelson MR. A randomised controlled trial of the effects of mindfulness practice on medical student stress levels. Med Educ. 2011;45:381‐388. [DOI] [PubMed] [Google Scholar]
- 31. Van Dijk I, Lucassen P, Akkermans RP, van Engelen BGM, van Weel C, Speckens AEM. Effects of mindfulness‐based stress reduction on the mental health of clinical clerkship students: a cluster‐randomized controlled trial. Acad Med. 2017;92:1012‐1021. [DOI] [PubMed] [Google Scholar]
- 32. Rosenzweig S, Reibel DK, Greeson JM, Brainard GC, Hojat M. Mindfulness‐based stress reduction lowers psychological distress in medical students. Teach Learn Med. 2003;15:88‐92. [DOI] [PubMed] [Google Scholar]
- 33. Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness‐based stress reduction for health care professionals: results from a randomized trial. Int J Stress Manag. 2005;12:164‐176. [Google Scholar]
- 34. Aherne D, Farrant K, Hickey L, Hickey E, McGrath L, McGrath D. Mindfulness based stress reduction for medical students: optimising student satisfaction and engagement. BMC Med Educ. 2016;16:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rethans J‐J, Norcini JJ, Barón‐Maldonado M, et al. The relationship between competence and performance: implications for assessing practice performance. Med Educ. 2002;36:901‐909. [DOI] [PubMed] [Google Scholar]
- 36. Daouk‐Öyry L, Zaatari G, Sahakian T, Rahal Alameh B, Mansour N. Developing a competency framework for academic physicians. Med Teach. 2017;39:269‐277. [DOI] [PubMed] [Google Scholar]
- 37. Van der Meulen MW, Smirnova A, Heeneman S, Oude Egbrink MG, van der Vleuten CP, Lombarts KM. Exploring validity evidence associated with questionnaire‐based tools for assessing the professional performance of physicians: a systematic review. Acad Med. 2019;94:1384‐1397. [DOI] [PubMed] [Google Scholar]
- 38. Dekeyser M, Raes F, Leijssen M, Leysen S, Dewulf D. Mindfulness skills and interpersonal behaviour. Pers Indiv Diff. 2008;44:1235‐1245. [Google Scholar]
- 39. Beach MC, Roter D, Korthuis PT, et al. A multicenter study of physician mindfulness and health care quality. Ann Fam Med. 2013;11:421‐428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Burgess DJ, Beach MC, Saha S. Mindfulness practice: a promising approach to reducing the effects of clinician implicit bias on patients. Patient Educ Couns. 2017;100:372‐376. [DOI] [PubMed] [Google Scholar]
- 41. Sibinga EM, Wu AW. Clinician mindfulness and patient safety. JAMA. 2010;304:2532‐2533. [DOI] [PubMed] [Google Scholar]
- 42. Berner ES. Mind wandering and medical errors. Med Educ. 2011;45:1068‐1069. [DOI] [PubMed] [Google Scholar]
- 43. Panagopoulou E, Montgomery A. From burnout to resilient practice: is it a matter of the individual or the context? Med Educ. 2019;53:112‐114. [DOI] [PubMed] [Google Scholar]
- 44. Shanafelt TD, Noseworthy JH. Executive leadership and physician well‐being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92:129‐146. [DOI] [PubMed] [Google Scholar]
- 45. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM. Association between funding and quality of published medical education research. JAMA. 2007;298:1002‐1009. [DOI] [PubMed] [Google Scholar]
- 47. Reed DA, Beckman TJ, Wright SM, Levine RB, Kern DE, Cook DA. Predictive validity evidence for Medical Education Research Study Quality Instrument scores: quality of submissions to JGIM's Medical Education Special Issue. J Gen Intern Med. 2008;23:903‐907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Dixon‐Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy. 2005;10:45‐53. [DOI] [PubMed] [Google Scholar]
- 49. Amutio A, Martinez‐Taboada C, Delgado LC, Hermosilla D, Mozaz MJ. Acceptability and effectiveness of a long‐term educational intervention to reduce physicians' stress‐related conditions. J Contin Educ Health Prof. 2015;35:255‐260. [DOI] [PubMed] [Google Scholar]
- 50. Amutio A, Martinez‐Taboada C, Hermosilla D, Delgado LC. Enhancing relaxation states and positive emotions in physicians through a mindfulness training program: a one‐year study. Psychol Health Med. 2015;20:720‐731. [DOI] [PubMed] [Google Scholar]
- 51. Sood A, Sharma V, Schroeder DR, Gorman B. Stress Management and Resiliency Training (SMART) program among Department of Radiology faculty: a pilot randomized clinical trial. Explore (NY). 2014;10:358‐363. [DOI] [PubMed] [Google Scholar]
- 52. West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well‐being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174:527‐533. [DOI] [PubMed] [Google Scholar]
- 53. Gilmartin H, Saint S, Rogers M, et al. Pilot randomised controlled trial to improve hand hygiene through mindful moments. BMJ Qual Saf. 2018;27:799‐806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ireland MJ, Clough B, Gill K, Langan F, O'Connor A, Spencer L. A randomized controlled trial of mindfulness to reduce stress and burnout among intern medical practitioners. Med Teach. 2017;39:409‐414. [DOI] [PubMed] [Google Scholar]
- 55. Verweij H, van Ravesteijn H, van Hooff MLM, Lagro‐Janssen ALM, Speckens AEM. Mindfulness‐based stress reduction for residents: a randomized controlled trial. J Gen Intern Med. 2018;33:429‐436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sood A, Prasad K, Schroeder D, Varkey P. Stress management and resilience training among Department of Medicine faculty: a pilot randomized clinical trial. J Gen Intern Med. 2011;26:858‐861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Verweij H, Waumans RC, Smeijers D, et al. Mindfulness‐based stress reduction for GPs: results of a controlled mixed methods pilot study in Dutch primary care. Br J Gen Pract. 2016;66:e99‐e105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lases S, Lombarts M, Slootweg IA, Arah OA, Pierik E, Heineman E. Evaluating mind fitness training and its potential effects on surgical residents' well‐being: a mixed methods pilot study. World J Surg. 2016;40:29‐37. [DOI] [PubMed] [Google Scholar]
- 59. Thimmapuram J, Pargament R, Sibliss K, Grim R, Risques R, Toorens E. Effect of heartfulness meditation on burnout, emotional wellness, and telomere length in health care professionals. J Community Hosp Intern Med Perspect. 2017;7:21‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Goldhagen BE, Kingsolver K, Stinnett SS, Rosdahl JA. Stress and burnout in residents: impact of mindfulness‐based resilience training. Adv Med Educ Pract. 2015;6:525‐532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Goodman MJ, Schorling JB. A mindfulness course decreases burnout and improves well‐being among healthcare providers. Int J Psychol Med. 2012;43:119‐128. [DOI] [PubMed] [Google Scholar]
- 62. Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302:1284‐1293. [DOI] [PubMed] [Google Scholar]
- 63. Manoch R, Gordon A, Black D, Malhi G, Seidler R. Using meditation for less stress and better wellbeing – a seminar for GPs. Aust Fam Physician. 2009;38:454‐458. [PubMed] [Google Scholar]
- 64. Pflugeisen BM, Drummond D, Ebersole D, Mundell K, Chen D. Brief video‐module administered mindfulness program for physicians: a pilot study. Explore (NY). 2016;12:50‐54. [DOI] [PubMed] [Google Scholar]
- 65. Razzaque R, Wood L. Exploration of the effectiveness and acceptability of a professional mindfulness retreat for psychiatrists. Mindfulness. 2016;7:340‐348. [Google Scholar]
- 66. Bentley PG, Kaplan SG, Mokonogho J. Relational mindfulness for psychiatry residents: a pilot course in empathy development and burnout prevention. Acad Psychiatry. 2018;42:668‐673. [DOI] [PubMed] [Google Scholar]
- 67. Hamilton‐West K, Pellatt‐Higgins T, Pillai N. Does a modified mindfulness‐based cognitive therapy (MBCT) course have the potential to reduce stress and burnout in NHS GPs? Feasibility study. Prim Health Care Res Dev. 2018;19:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Hoenders HJ, Booij SH, Knegtering H, van den Brink H. Mindfulness training for psychiatrists in residency: a pilot study. Tijdschr Psychiatr. 2016;58:809‐813. [PubMed] [Google Scholar]
- 69. Montero‐Marin J, Gaete J, Araya R, et al. Impact of a blended web‐based mindfulness programme for general practitioners: a pilot study. Mindfulness. 2018;9:129‐139. [Google Scholar]
- 70. Taylor M, Hageman JR, Brown M. A mindfulness intervention for residents: relevance for pediatricians. Pediatr Ann. 2016;45:e373‐e376. [DOI] [PubMed] [Google Scholar]
- 71. Wen L, Sweeney TE, Welton L, Trockel M, Katznelson L. Encouraging mindfulness in medical house staff via smartphone app: a pilot study. Acad Psychiatry. 2017;41:646‐650. [DOI] [PubMed] [Google Scholar]
- 72. Beckman HB, Wendland M, Mooney C, et al. The impact of a program in mindful communication on primary care physicians. Acad Med. 2012;87:815‐819. [DOI] [PubMed] [Google Scholar]
- 73. Crane R, Brewer J, Feldman C, et al. What defines mindfulness‐based programs? The warp and the weft. Psychol Med. 2017;47:990‐999. [DOI] [PubMed] [Google Scholar]
- 74. Fjorback LO, Arendt M, Ørnbøl E, Fink P, Walach H. Mindfulness‐based stress reduction and mindfulness‐based cognitive therapy – a systematic review of randomized controlled trials. Acta Psychiatr Scand. 2011;124:102‐119. [DOI] [PubMed] [Google Scholar]
- 75. Davidson RJ, Kaszniak AW. Conceptual and methodological issues in research on mindfulness and meditation. Am Psychol. 2015;70:581‐592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Pirson M, Langer EJ, Bodner T, Zilcha‐Mano S. The development and validation of the Langer Mindfulness Scale – enabling a socio‐cognitive perspective of mindfulness in organizational contexts. SSRN Electronic J 2012; 10.2139/ssrn.2158921. [DOI]
- 77. Khoury B, Knäuper B, Pagnini F, Trent N, Chiesa A, Carrière K. Embodied mindfulness. Mindfulness. 2017;8:1160‐1171. [Google Scholar]
- 78. Langer EJ, Moldoveanu M. The construct of mindfulness. J Soc Issues. 2000;56:1‐9. [Google Scholar]
- 79. de Vibe M, Solhaug I, Rosenvinge JH, Tyssen R, Hanley A, Garland E. Six‐year positive effects of a mindfulness‐based intervention on mindfulness, coping and well‐being in medical and psychology students: results from a randomized controlled trial. PLoS ONE. 2018;13:e0196053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Garland EL, Farb NA, Goldin P, Fredrickson BL. Mindfulness broadens awareness and builds eudaimonic meaning: a process model of mindful positive emotion regulation. Psychol Inq. 2015;26:293‐314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Firth‐Cozens J, Greenhalgh J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017‐1022. [DOI] [PubMed] [Google Scholar]
- 82. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Int J Surg. 2010;8:336‐341. [DOI] [PubMed] [Google Scholar]
- 83. Veenhoven R. Subjective measures of well‐being In: McGillivray M, ed. Human Well‐Being: Concept and Measurement. London: Palgrave Macmillan; 2007;214‐239. [Google Scholar]
- 84. Diener E. Guidelines for national indicators of subjective well‐being and ill‐being. Appl Res Qual Life. 2006;1:151‐157. [Google Scholar]
- 85. Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self‐assessment compared with observed measures of competence: a systematic review. JAMA. 2006;296:1094‐1102. [DOI] [PubMed] [Google Scholar]
- 86. Glaser KM, Markham FW, Adler HM, McManus PR, Hojat M. Relationships between scores on the Jefferson Scale of Physician Empathy, patient perceptions of physician empathy, and humanistic approaches to patient care: a validity study. Med Sci Monit. 2007;13:CR291‐CR294. [PubMed] [Google Scholar]
- 87. Bothwell LE, Greene JA, Podolsky SH, Jones DS. Assessing the gold standard – lessons from the history of RCTs. N Engl J Med. 2016;374:2175‐2181. [DOI] [PubMed] [Google Scholar]
- 88. Pandis N, Chung B, Scherer RW, Elbourne D, Altman DG. CONSORT 2010 statement: extension checklist for reporting within person randomised trials. BMJ. 2017;357:j2835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Creswell JD. Mindfulness interventions. Annu Rev Psychol. 2017;68:491‐516. [DOI] [PubMed] [Google Scholar]
- 90. Ruitenburg MM, Frings‐Dresen MHW, Sluiter JK. How to define the content of a job‐specific worker's health surveillance for hospital physicians? Saf Health Work. 2016;7:18‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Linzer M, Levine R, Meltzer D, Poplau S, Warde C, West CP. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. 2014;29:18‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Van Dam NT, van Vugt MK, Vago DR, et al. Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect Psychol Sci 2018;13:36‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


