Abstract
Objectives
To understand whether interventions are effective, we need to know whether the interventions are delivered as planned (with fidelity) and engaged with. To measure fidelity and engagement effectively, high‐quality measures are needed. We outline a five‐step method which can be used to develop quality measures of fidelity and engagement for complex health interventions. We provide examples from a fidelity study conducted within an evaluation of an intervention aimed to increase independence in dementia.
Methods
We propose five steps that can be systematically used to develop fidelity checklists for researchers, providers, and participants to measure fidelity and engagement. These steps include the following: (1) reviewing previous measures, (2) analysing intervention components and developing a framework outlining the content of the intervention, (3) developing fidelity checklists and coding guidelines, (4) obtaining feedback about the content and wording of checklists and guidelines, and (5) piloting and refining checklists and coding guidelines to assess and improve reliability.
Results
Three fidelity checklists that can be used reliably were developed to measure fidelity of and engagement with, the Promoting Independence in Dementia (PRIDE) intervention. As these measures were designed to be used by researchers, providers, and participants, we developed two versions of the checklists: one for participants and one for researchers and providers.
Conclusions
The five steps that we propose can be used to develop psychometrically robust and implementable measures of fidelity and engagement for complex health interventions that can be used by different target audiences. By considering quality when developing measures, we can be more confident in the interpretation of intervention outcomes drawn from fidelity and engagement studies.
Statement of contribution.
What is already known on the subject?
Fidelity and engagement can be measured using a range of methods, such as observation and self‐report.
Studies seldom report psychometric and implementation qualities of fidelity measures.
What does this study add?
A method for developing fidelity and engagement measures for complex health interventions.
Guidance on how to consider quality when developing fidelity and engagement measures.
Keywords: complex health intervention, dementia, engagement, fidelity of delivery, implementation, measures, psychometric, quality
Background
Measuring fidelity of delivery and engagement alongside the delivery of a trial helps us to understand whether planned interventions were effective (Borrelli, 2011). Fidelity of delivery is the extent to which interventions are delivered as planned (Borrelli, 2011). Consistent with previous research (Walton, Spector, Tombor, & Michie, 2017), engagement is used as an umbrella term to refer to whether a participant understands and can perform the required skills (receipt) and whether they can put plans into practice in daily life (enactment) (Borrelli, 2011). In this manuscript, we collectively refer to receipt and enactment as engagement to distinguish between provider behaviours (fidelity of delivery) and participant behaviours (engagement) (Walton et al., 2017). The definitions used in this article are based on the National Institutes of Health Behaviour Change Consortium framework for fidelity of delivery, intervention receipt, and intervention enactment (Bellg et al., 2004).
Without understanding whether interventions are delivered as planned and engaged with, it is difficult to fully understand whether or not an intervention is effective. Therefore, measuring fidelity and engagement as part of a process evaluation is essential for understanding how and whether an intervention works (Moore et al., 2015; Oakley, Strange, Bonell, Allen, & Stephenson, 2006). This is particularly important for complex interventions, which have many components.
Despite the importance of fidelity and engagement, fewer than half of the studies (24/66) included in a review of complex health behaviour change interventions measured both fidelity and engagement (Walton et al., 2017). To measure fidelity, observational, self‐report, and multiple measures have been used (Breitenstein et al., 2010; Lorencatto, West, Christopherson, & Michie, 2013; Toomey, Matthews, & Hurley, 2017; Walton et al., 2017). Audio‐recording all sessions and using multiple researchers to reliably rate a percentage for fidelity is the current gold standard (Lorencatto et al., 2013). To measure engagement, self‐report, attendance records, and multiple measures have been used (Gearing et al., 2011; Hankonen et al., 2015; Rixon et al., 2016; Walton et al., 2017). There is currently no consensus regarding the gold standard method to measure engagement in face‐to‐face interventions (Walton et al., 2017). Different aspects of engagement can be measured in different ways. For example, receipt has been measured most commonly using quantitative measures (Rixon et al., 2016). Enactment is difficult to measure as, researchers propose that in order to distinguish between outcomes and enactment, measures for enactment need to be specific to intervention skills rather than the target behaviour (Resnick et al., 2005). To overcome limitations of individual measures, multiple measures of fidelity and engagement are recommended (Keller‐Margulis, 2012; McKenna, Flower, & Ciullo, 2014; Munafo & Smith, 2018).
To ensure that fidelity measurements are trustworthy, psychometric and implementation qualities of measures should be reported (Walton et al., 2017). Psychometric qualities include the following: reliability (consistency of results in different situations; e.g., inter‐rater agreement) and validity (measures assessing what they aim to; e.g., sampling across different providers, sites, and time points) (Roberts, Priest, & Traynor, 2006; Walton et al., 2017). Implementation qualities include the following: acceptability of measures in relation to the needs of the intended audience (e.g., providers’ attitudes towards measurements) and practicality of the measures in relation to ease of completion and minimizing burden (e.g., availability of resources) (Lohr, 2002; Walton et al., 2017).
Despite the importance of high‐quality measures, considerations of quality are seldom reported in fidelity studies (Rixon et al., 2016; Walton et al., 2017). A review of fidelity and engagement measures used in complex health behaviour change interventions found that 74.2% of studies report at least one ‘psychometric quality’ (the quality of the measures) whereas only 25.8% report at least one ‘implementation quality’ (how the measures were used in practice) (Walton et al., 2017). This highlights the need to consider and report quality when measuring fidelity and engagement in complex health interventions. Consideration of these qualities is particularly pertinent in complex interventions, in which measuring fidelity and/or engagement may not be straightforward. For example, previous research found that agreement was difficult to achieve when measuring fidelity of the Community Occupational Therapy in Dementia‐UK (COTiD‐UK) intervention (Walton et al., submitted). To improve the quality of fidelity and engagement measures for complex interventions, guidance on how to develop high‐quality fidelity and engagement measures is needed.
To the authors’ knowledge, there is a lack of practical guidance on how to consider the quality of the measures and how they are used in practice when developing fidelity and engagement measures for complex health interventions. This manuscript builds on the findings from an earlier review (Walton et al., 2017) and provides recommendations on how to develop measures of fidelity and engagement for complex health interventions, with consideration around psychometric and implementation qualities. These measures of fidelity and engagement can be used by researchers, intervention providers (those that deliver the intervention to participants), and participants. This five‐step method will be illustrated using examples from the fidelity assessment conducted within an intervention aimed to increase independence in dementia (Promoting Independence in Dementia: PRIDE; See Csipke et al., 2018 and Box 1 for further details about PRIDE).
Box 1. Description of the PRIDE intervention (Csipke et al., 2018).
PRIDE intervention
Aimed to improve independence for people living with mild dementia.
Complex, tailored, manual‐based feasibility trial.
Delivered by dementia advice workers (DAWs) – termed ‘providers’ in this manuscript (n = 12).
Delivered to people living with mild dementia and their supporters (e.g., family members/friends) (n = 34) across four sites.
Delivered over three sessions.
Participants chose up to three tailored topics from a choice of seven topics: (1) keeping mentally active, (2) keeping physically active, (3) keeping socially active, (4) making decisions, (5) getting your message across, (6) receiving a diagnosis, (7) keeping healthy.
Participants chose activities to work on, reviewed plans and identified barriers, facilitators and solutions.
In this fidelity assessment, a longitudinal observational design was used and fidelity was measured using observation (researcher ratings of transcribed, audio‐recorded intervention sessions) and provider and participant self‐report measures. Fidelity ratings from researchers, providers, and participants were compared. Engagement, including participants’ receipt (whether participants understood the information) and enactment (whether participants’ put their plans into practice between sessions), was measured using participant self‐report, which is consistent with previous research. Further details about the results of the fidelity assessment are reported elsewhere (see Walton, 2018).
This study is part of a larger mixed‐methods process evaluation which also included interviews with providers, participants, and supporters to qualitatively explore barriers and facilitators to fidelity and engagement and to develop recommendations to improve fidelity and engagement (see Walton, 2018).
Methods
Ethical approval
Ethical and research governance requirements were followed. Data were transcribed professionally and all transcripts were fully anonymized. Individuals were unidentifiable from data or resulting outputs. Ethical approval was obtained from the NHS East Midlands – Nottingham 1 Research Ethics committee (REC reference number: 16/EM/0044). Data were accessed by authorized study members and stored securely in a central location.
Proposed methodology for developing fidelity measures
Fidelity checklists, which can be used to measure both fidelity and engagement, were iteratively developed using five steps. The process for applying these five steps to develop fidelity and engagement measures is outlined in Table 1.
Table 1.
The five steps used to develop quality fidelity and engagement measures
| Step | Proposed procedure | How to apply this step |
|---|---|---|
| 1) Review previous measures | 1a) Review measures used in fidelity assessments within your field and/or related fields |
|
| 2) Analyse intervention components and develop an intervention framework | 2a) Analyse intervention components |
|
| 2b) Group the list of components into categories |
|
|
| 2c) Develop a comprehensive intervention framework |
|
|
| 2d) Remove redundant components from framework |
|
|
| 3) Develop fidelity checklists | 3a) Identify which components from the framework take place in which of the intervention sessions |
|
| 3b) Develop one checklist for each of your intervention sessions, based on your framework |
|
|
| 3c) Tailor checklists for use by your intended audiences |
|
|
| 3d) Review the checklists |
|
|
| 3e) Develop simple guidelines for all target users which explain how to complete the checklists |
|
|
| 4) Obtain feedback about the content and wording of the checklists and guidelines | 4a) Ask relevant stakeholders to give feedback on the content and wording of checklists and coding guidelines |
|
| 4b) Edit checklists and guidelines to take this feedback into account |
|
|
|
5) Pilot and refine checklists and coding guidelines to assess and improve reliability Note. This step is only necessary if researchers will be carrying out the fidelity assessment (i.e., not if only using provider/participant self‐ report) |
5a) Use multiple researchers to test coding guidelines and checklists against some initial intervention transcripts (initial piloting) |
|
| 5b) Discuss discrepancies and amend coding guidelines |
|
|
| 5c) Pilot and amend coding guidelines until selected agreement threshold is achieved |
|
Below, we briefly outline how these five steps were applied to develop fidelity and engagement measures for the PRIDE intervention. Due to time constraints associated with using these checklists in the feasibility trial, these checklists were iteratively developed alongside the intervention manual.
Step 1: Review previous measures
After developing the PRIDE fidelity checklists, many of these steps were also followed to develop fidelity checklists for use in another complex intervention for people with dementia: The Community Occupational Therapy in Dementia – UK intervention (COTiD‐UK; see Walton et al., submitted). The fidelity checklists for PRIDE were developed prior to the development of COTiD‐UK checklists, but the fidelity assessment for COTiD‐UK took place at the same time as PRIDE.
Prior to the development of the PRIDE checklists, we were not aware of any fidelity checklists that had been used in similar dementia interventions. Instead, to inform the development of our checklists, we reviewed fidelity measures that were known to our team: checklists used in the Prediction and Management of Cardiovascular Risk for people with severe mental illnesses (PRIMROSE) project (Osborn et al., 2016).
Step 2: Analyse intervention components and develop a framework outlining the content of the intervention
The framework described in this step is separate from the process of PRIDE intervention development (see Yates et al., 2019). The framework described in this manuscript should instead be considered as a tool to facilitate the development of fidelity checklists by clearly outlining the intervention content. To ensure that the intervention content matched the fidelity checklist content, we developed this framework from the intervention manual that was developed by the PRIDE intervention team. This framework was used to facilitate understanding of the PRIDE intervention manual and what should be delivered by providers.
2a) Analyse intervention components
The PRIDE intervention manual was read and coded. This coding was used to identify key components of PRIDE (i.e., aspects of the intervention that need to be delivered to participants). We used the Behaviour Change Technique (BCT) Taxonomy Version 1 to identify BCTs (Michie et al., 2013).
2b) Group the list of components into categories
Components were grouped into three categories by identifying similarities across components: necessary basic information, tailoring and assessment and PRIDE activities.
2c) Develop a comprehensive intervention framework
Categories were used to develop an intervention framework which included the following: (1) key targets of the intervention, (2) key intervention components, (3) PRIDE session number that the component is delivered in, (4) target behaviour, (5) BCTs, and (6) PRIDE objectives (see Appendix S1 for the PRIDE intervention framework).
2d) Review the framework
A team of behavioural scientists (the first, fourth, and last author) reviewed the intervention framework and removed redundant components.
Step 3: Develop fidelity checklists
3a) Identify which components from the framework take place in which of the intervention sessions
The PRIDE intervention framework was used to identify key components which should be delivered for each of the three PRIDE sessions.
3b) Develop one checklist for each of the intervention sessions, based on the intervention framework
Three PRIDE fidelity checklists were developed (one for each session). These checklists all contained standardized components which all participants should receive. Components were put in order of delivery. Intervention components were worded in everyday appointment activities rather than BCTs so that delivery of components could be measured by all intended audiences (researchers, providers, and participants).
If components were tailored to participants’ individual choices (e.g., providing relevant resources), these were referred to as the ‘chosen topic’ in the checklist. To identify which tailored components were delivered for participants’ chosen topics, an additional grid was included in the researcher and provider checklists.
Participant checklists also contained questions on whether participants understood the information, knew how to put their plan into action, and practised and used these skills between sessions. Questions were developed based on the definitions of ‘receipt’ and ‘enactment’ (Bellg et al., 2004; Borrelli, 2011). Engagement questions were not included on the researcher/provider checklists as providers and researchers would be unable to answer questions on participants’ understanding. Similarly, providers and researchers were not present between sessions when enactment of plans would take place.
3c) Tailor the checklists for use by the intended audiences
Two versions of these checklists were developed: one for providers and researchers, and one for participants (people living with dementia). Checklists were tailored and worded for the target audience. One checklist was developed to be used by both providers and researchers as the wording of the checklists applied to both groups. Participant checklists were worded in relation to receipt and provider checklists were worded in relation to delivery. For the provider checklists, we added a ‘brief reason’ column for them to add notes to explain why components were not delivered/partially delivered.
3d) Review the checklists
The team of behavioural scientists reviewed the checklists to identify and remove redundant components and jargon.
3e) Develop simple coding guidelines for all target users which explain how to complete the checklists
Simple guidelines were developed for all intended users (researchers, providers, and participants). The guidelines explained how to complete these checklists. In‐depth coding guidelines were developed for researchers (see Appendix S2). Researcher coding guidelines included definitions for each component and illustrative examples of ‘done’, ‘done to some extent’, and ‘not done’. Simple guidelines for providers and participants were also developed. Provider and participant guidelines provided information on what the checklists are for, how to complete and return the checklists, and an example checklist.
Step 4: Obtain feedback about the content and wording of the checklists and guidelines from relevant stakeholders
4a) Ask relevant stakeholders to give feedback on the content and wording of checklists and coding guidelines
This step ensured that the checklist and guideline items were relevant, accurate, and worded appropriately for use by providers and people living with dementia. Six members of the intervention development team provided feedback. We also asked for feedback from the intervention's Public Patient Involvement (PPI) group, providers, and a person living with dementia working in a PPI type role.
4b) Edit checklists and coding guidelines to take feedback into account
Feedback from the intervention team and PPI group was used to refine the checklists. To enhance accessibility of the checklists for people living with dementia, condition‐specific guidance was used (Dementia Empowerment and Engagement Project; DEEP Guide, 2013). To determine whether checklists were easy to read, Flesch readability statistics (Flesch, 1948) were reviewed following feedback.
Step 5: Pilot and refine checklists and coding guidelines to assess and improve reliability of researcher ratings
5a) Use multiple researchers to test coding guidelines and checklists against some intervention transcripts (initial piloting)
To test coding guidelines and pilot the coding task, two researchers (independent researcher and 1st author) transcribed and coded an initial set of three transcripts (Session one, Session two and Session three).
5b) Discuss discrepancies and amend coding guidelines
Discrepancies between coders were identified. Reliability was calculated using Cohen's weighted kappa and percentage agreement (Cohen, 1968; Gwet, 2014). Feedback from this process was used to amend the coding guidelines.
5c) Pilot and amend coding guidelines until selected agreement threshold is achieved
After initial piloting, 17 further sets of transcripts were coded independently by two researchers (1st and 3rd author) until good agreement was achieved. To ensure that instructions were clear, coders discussed guidelines before coding. Missing responses were clarified with the coder prior to agreement calculations where possible. If responses were not clarified, these were included as missing responses.
Agreement was measured using Cohen's weighted kappa and percentage agreement (Cohen, 1968; Gwet, 2014). For standardized components, agreement was assessed using weighted kappa. For tailored components and individual topics, agreement was assessed using percentage agreement. To account for the ordinal nature of data and partial agreements, we used weighted kappa (Gwet, 2014). For example, a disagreement of ‘done’ and ‘done to some extent’ would be more of a partial agreement than one of ‘done’ and ‘not done’. Linear weights (agreements = 1.0, partial agreements = 0.5, disagreements = 0.0) were selected instead of quadratic weights. Linear weights were chosen as they provide equal spacing between options and do not overestimate reliability as much as quadratic weights (Gwet, 2014).
Higher kappa scores indicate better agreement (<0.00 is poor, 0–0.2 is slight, 0.21–0.40 is fair, 0.41–0.60 is moderate, 0.61–0.80 is good and 0.81–1 is excellent agreement; Gisev, Bell, & Chen, 2013; Landis & Koch, 1977; Viera & Garrett, 2005). To ensure high agreement, a threshold of >.60 kappa (good) was selected. A threshold of >.60 kappa (good) was selected and deemed to be appropriate. This is because kappa is a conservative estimate of reliability which ensures that chance agreements are accounted for (Lombard, Snyder‐Duch, & Bracken, 2002). To ensure that a high level of agreement was achieved and maintained, coders needed to achieve κ > 0.61 for three consecutive transcripts per session. This threshold was also consistent with the level of agreement used due to difficulties achieving excellent agreement within a fidelity evaluation of the COTiD‐UK intervention (Walton et al., submitted).
Coding guidelines were finalized once no further changes were necessary. We then re‐applied these finalized coding guidelines to all intervention transcripts to measure fidelity of, and engagement with PRIDE (not reported here, see Walton, 2018; Walton et al., in preparation).
Results
Development of fidelity checklists
We developed three fidelity checklists (Session one, Session two, and Session three), each containing standardized intervention components (Session one: n = 22, Session two: n = 18, Session three: n = 12). Provider checklists also contained an additional grid for tailored components. See Figure 1 for an example of the provider and researcher checklists and Figure 2 for an example of the participant ‘your experience checklists’ (See Appendices S3 and S4 for full copies of both sets of checklists).
Figure 1.
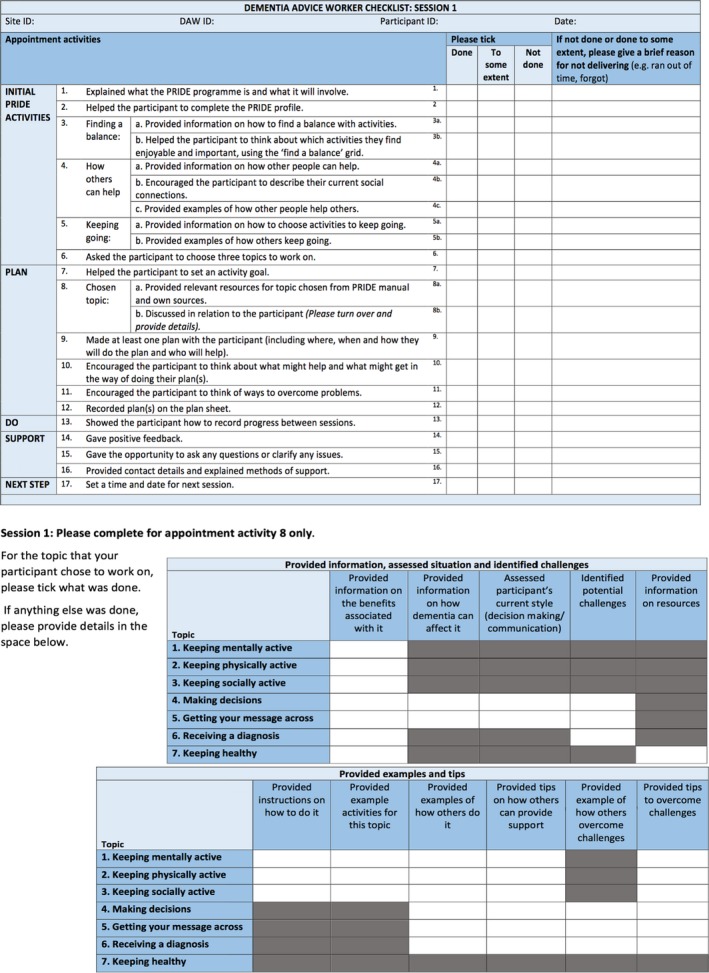
An example provider checklist (Session one). [Colour figure can be viewed at http://www.wileyonlinelibrary.com]
Figure 2.

An example participant ‘your experience’ checklist (Session one). [Colour figure can be viewed at http://www.wileyonlinelibrary.com]
In the provider/researcher checklists, three response options were offered: ‘done’, ‘done to some extent’, and ‘not done’. A ‘reason’ column was added to the PRIDE provider checklists so that providers could add details or context to indicate a reason for why a component was not delivered. In the participant checklists, three response options were available for the questions on fidelity: ‘definitely happened’, ‘possibly happened’ and ‘didn't happen’, and three response options were available for the questions on engagement: ‘yes’, ‘to some extent’, and ‘no’.
Based on feedback, we amended the checklists to minimize jargon (e.g., replacing ‘facilitators’ with ‘things that will help with my plan’). To enhance accessibility of the checklists for people with dementia, the Dementia Empowerment and Engagement Project (DEEP) guidance (DEEP Guide, 2013) was used. This included enlarging the font size to 16pt, using a clear font style, using colour, avoiding jargon and academic terminology, removing passive voice, and explaining terms.
Finalized participant checklists had a Flesch score of 71.4 and a grade of 6.2, and the provider checklists had a Flesch score of 62.0 and a grade of 7.5. This is within the recommendations for the general population (Vahabi & Ferris, 1995); thus, the readability of the checklists was suitable.
Response rates
To indicate how acceptable and practical the checklists were for use by providers and people with dementia, response rates were calculated. Ninety‐three sessions were delivered. Of these, 72 audio‐recordings (77.4%), 75 provider checklists (80.7%), and 59 participant checklists (63.4%) were returned. Reasons for not returning the audio‐recordings were as follows: technical failures during or after recording, the audio‐recording being wiped from the device before uploading, or a corrupt file. Of the 24 sets (n = 72 transcripts) sampled for the fidelity assessment, 17 recordings were missing, resulting in 55 transcripts.
For the researcher ratings, no components were missing, 13 components were scored ‘not applicable’, and no responses were unclear. Across the provider checklists, 30 individual components were missing, 11 components were scored ‘not applicable’ and one component was ‘unclear’. Across the participant checklists, 20 individual fidelity components were missing, one fidelity component was scored ‘not applicable’, and six fidelity components and two engagement components were ‘unclear’. ‘Missing’ components refer to components which participants did not complete a rating for.
Inter‐rater agreement for researcher ratings (piloting stage)
For the standardized components, good inter‐rater agreement (κ > .61) was achieved after coding 12 Session one transcripts (κ = 0.8–0.9), 14 Session two transcripts (κ = 0.7–0.8), and 14 Session three transcripts (κ = 0.6–1.00) (initial pilot coding not included) (See Table 2). For Session one, inter‐rater agreement of >. 61 kappa was not achieved three times in a row due to an unequal distribution of responses (Feinstein & Cicchetti, 1990), which meant that kappa was moderate (κ = 0.4) but percentage agreement was very high (86.4%).
Table 2.
Weighted kappa and percentage agreement for standardized components across PRIDE Sessions one, two, and three in both the piloting stage and main assessment stage
| Set of transcripts | Weighted kappa (%) | |||
|---|---|---|---|---|
| Session 1 | Session 2 | Session 3 | ||
| Piloting coding guidelines and checklists to achieve agreement | ||||
| 1 | Coding pair 1 (pilot) | 0.21 (59.1) | 0.26 (55.6) | −0.33 (50) |
| Coding pair 2 | 0.38 (54.6) | 0.4 (66.66) | −0.11 (66.66) | |
| 3 | −0.2 (36.4) | 0.48 (61.1) | −0.25 (41.66) | |
| 4 | 0.47 (63.6) | 0.65 (72.2)a | 0.49 (66.66) | |
| 5 | 0.55 (59.1) | 0.62 (77.7)a | 0.29 (58.33) | |
| 6 | 0.62 (77.3)a | 0.69 (77.7)a | 0.31 (50) | |
| 7 | 0.28 (68.2) | 0.16 (50) | 0.59 (66.6) | |
| 11b | 0.56 (77.3) | 0.54 (66.7) | 0.00 (33.3) | |
| 2 | 0.83 (90.9)a | 0.71 (77.7)a | No session | |
| 8 | No transcript | No transcript | 0.31 (58.3) | |
| 9 | 0.07 (72.7) | 0.41 (61.1) | No transcript | |
| 10 | 0.85 (90.9)a | 0.83 (83.3)a | No transcript | |
| 13 | 0.81 (86.4)a | No transcript | 0.61 (66.66)a | |
| 12 | No transcript | 0.45 (55.6) | 0.46 (58.33) | |
| 14 | 0.42 (86.4)a,c | No transcript | 0.57 (66.66) | |
| 15 | No transcript | No transcript | 1.00 (100)a | |
| 16 | No transcript | No transcript | 0.68 (75)a | |
| 17 | – | 0.83 (83.3)a | No transcript | |
| 18 | – | 0.77 (83.3)a | 0.64 (83.33)a | |
| 1 (re‐coded new guidelines) | – | 0.68 (88.9)a | – | |
| Main fidelity assessment | ||||
| 5 (*) | 0.7 (72.7) | 0.5 (72.2) | 0.3 (66.7) | |
| 6 | – | 0.4 (66.7) | 0.8 (83.3) | |
| 7 | – | 0.4 (72.2) | – | |
| 18 (*Session 1) | 0.4 (68.2) | Pre‐coded | Pre‐coded | |
| 19 (*Session 2) | 0.6 (77.3) | 0.5 (66.7) | 0.4 (50) | |
| 20 | 0.8 (90.9) | 0.7 (77.7) | 0.6 (75) | |
| 23 (*) | 0.8 (90.9) | 0.5 (55.5) | No transcript | |
| 24 | – | 0.7 (83.3) | 0.8 (91.7) | |
This was used when agreement had already been reached, and no further sessions needed to be coded until the next sampled set.
No transcript – refers to sessions where transcripts were not available to code.
(*) Sets in the main fidelity assessment that were selected for double coding.
Pre‐coded refers to sets that were coded during the piloting phase.
Indicates agreement >0.61 was reached.
Coding guidelines not changed after coding this set.
Weighted kappa did not reach >0.61 however >85% agreement achieved three times in a row and >0.8 kappa 3 times in last five sets. Kappa low due to lots of ‘not done’ responses, despite only three disagreements.
Table 3 reports percentage agreement for tailored topics and components. Good agreement (average means: 54.6–87.8%) was achieved for tailored components in both sessions.
Table 3.
Percentage agreement for delivery of tailored topics and topic components (scored out of 11) in PRIDE Sessions one and two in both the piloting stage and main assessment stage
| Topic (number of sets delivered in Session 1 and 2) | Mean number of components agreed on (range) (%) | |
|---|---|---|
| Session 1 | Session 2 | |
| Piloting coding guidelines and checklists to achieve agreement | ||
| Keeping mentally active (S1: 9, S2: 2) | 75.7 (54.6–90.9) | 86.4 (81.8–90.9) |
| Keeping physically active (S1: 3, S2: 0) | 84.8 (72.7–90.9) | N/A |
| Keeping socially active (S1: 4, S2: 3) | 86.4 (72.7–90.9) | 87.8 (81.8–90.9) |
| Making decisions (S1: 2, S2: 1) | 86.4 (81.8–90.9) | 81.8 |
| Getting your message across (S1: 4, S2: 1) | 75 (27.3–90.9) | 81.8 |
| Receiving a diagnosis (S1: 1, S2: 2) | 54.6 | 72.7 (63.6–81.8) |
| Keeping healthy (S1: 0, S2: 0) | N/A | 81.8 (63.6–90.9) |
| No topics delivered (S1: 2, S2: 3) | N/A | N/A |
| Main fidelity assessment | ||
| 1 Keeping mentally active (S1: 4, S2: 1) | 93.6 (81.8–100) | 100 |
| 2 Keeping physically active (S1: 2, S2: 2) | 90.9 | 90.9 |
| 3 Keeping socially active (S1: 2, S2: 2) | 90.9 (81.8–100) | 86.4 (81.8–90.9) |
| 4 Making decisions (S1: 2, S2: 1) | 81.8 | 63.6 |
| 5 Getting your message across (S1: 2, S2: 1) | 81.8 (72.7–90.9) | 81.8 |
| 6 Receiving a diagnosis (S1: 2, S2: 0) | 95.5 (90.9–100) | N/A |
| 7 Keeping healthy (S1: 0, S2: 2) | N/A | 77.3 (63.6–90.9) |
| No topic delivered (S1: 0, S2: 3) | N/A | N/A |
N/A = not applicable: Topic not delivered.
11 components = 100%.
Discussion
Key findings
We have developed a systematic method consisting of five steps that can be used to develop measures of fidelity and engagement that consider both psychometric and implementation qualities. These measures can be used by different audiences including providers, participants, and researchers. The consideration of quality when developing fidelity and engagement measurements for the PRIDE intervention provides confidence in fidelity and engagement results obtained using these measures.
Findings in relation to previous research
Findings from these studies extend previous work in this area by demonstrating that researchers can use these five steps to consider reliability, validity, practicality, and acceptability when developing measures of fidelity and engagement. These psychometric and implementation qualities have been recommended (Gearing et al., 2011; Glasgow et al., 2005; Holmbeck & Devine, 2009; Lohr, 2002; Stufflebeam, 2000), yet reported infrequently (Walton et al., 2017). These qualities were considered when developing PRIDE checklists.
To improve the consistency of fidelity coding, the checklists and coding guidelines were piloted until good inter‐rater agreement was achieved (Lorencatto, West, Bruguera, & Michie, 2014). The finding that good agreement was difficult to achieve highlights that while it is possible to achieve reliability, piloting checklists and coding guidelines is a necessary step when developing fidelity and engagement measures. This finding is consistent with previous fidelity research (Harting, van Assema, van der Molen, Ambergen, & de Vries, 2004; Thyrian et al., 2010; Walton et al., submitted). This may be due to the complexity of the intervention, which has been suggested to make it harder to achieve good agreement (Harting et al., 2004). To enhance agreement, clear definitions of components were provided in the researcher coding guidelines to make coding easier and limit individual judgement and subjectivity, as recommended by previous research (French et al., 2015; Hardeman et al., 2008; Harting et al., 2004; Keith, Hopp, Subramanian, Wiitala, & Lowery, 2010; Lorencatto et al., 2014).
The development of fidelity measures for use by multiple people (researchers, providers, and participants) contributes towards validity by ensuring that findings can be triangulated and that individual limitations are overcome by multiple measurements (Keller‐Margulis, 2012; McKenna et al., 2014; Munafo & Smith, 2018. In the PRIDE fidelity assessment, we found discrepancies between fidelity ratings, with researcher ratings indicating moderate fidelity and provider and participant ratings indicating high fidelity (see Walton et al., [Link]; Walton, 2018 for more details). In this study, the differences in measurement tools may lead to differences in fidelity ratings, as researchers had thorough coding guidelines to base their decisions on whereas providers and participants received simple guidelines to base their decisions on. Providing more thorough guidelines to providers and participants would have increased the time taken to complete checklists and complexity of the task, therefore this would not have been acceptable or practical to implement in this study.
This method highlights strategies that can be taken to enhance acceptability and practicality when developing measures of fidelity and engagement. To enhance acceptability and practicality, different versions of the checklists were created in the PRIDE study for different audiences (Glasgow et al., 2005; Holmbeck & Devine, 2009; Lohr, 2002). Providing a ‘reason’ column in the provider checklist aimed to provide an expectation that it is acceptable to not deliver all components, which may have enhanced acceptability. Feedback was sought on the content and wording of these checklists from PPI members and interventionists. This feedback, together with condition‐specific guidance (The Dementia Engagement and Empowerment Project (DEEP Guide), 2013), informed adaptations to improve ease of use and acceptability for participants and providers. Simple guidelines were developed to help participants and providers to try to enhance practicality (Lohr, 2002; Walton et al., 2017). While acceptability and practicality were not formally assessed, high response rates for audio‐recordings, participant and provider checklists offer an indication of acceptability and practicality (Walton, 2018).
Limitations
Although feedback was sought from the fidelity and intervention development teams, only one researcher coded the intervention content and developed the framework of intervention components. Although BCTs (Michie et al., 2013) were highlighted from the PRIDE manual, these were used to develop an intervention framework but not the checklist components. Therefore, components in the checklists were not specifically measured using BCTs. Using everyday language to describe components enabled the PRIDE checklists to be accessible for all audiences, including providers and people with dementia.
A further limitation of the checklist development process was that only one previous measure of fidelity was formally reviewed in step 1 of checklist development. Future research should consider reviewing a wider range of fidelity checklists prior to steps 2–5.
While we gained feedback on the checklists from the PRIDE PPI group, we only received feedback on the checklist wording from one person living with dementia. However, alongside this feedback, we also reviewed guidance which was co‐produced with people living with dementia (DEEP, 2013), to ensure that checklists were as accessible as possible for people living with dementia to use.
One limitation of this study is that we used participant self‐report to measure engagement (receipt and engagement). Objective measures of participant engagement may have helped to overcome limitations of self‐report such as social desirability bias. Furthermore, participants were asked to complete checklists as soon as possible after each session but in some cases this may not have happened. Therefore, there may have been some difficulties for participants remembering the extent to which they engaged or the extent to which the intervention was delivered as planned. Asking participants to complete a couple of extra questions was practical as participants only had to complete one measure which included both fidelity and engagement. We also triangulated findings with more in‐depth qualitative findings on barriers and facilitators to engagement from perspectives of participants and supporters. These findings are reported along with the engagement outcomes to develop recommendations for improving engagement (see Walton et al., in preparation).
This study only focused on fidelity and engagement and did not develop measures to evaluate therapeutic alliance or the relationship between the patient and provider. However, the relationship between participants and providers was explored when conducting interviews to identify barriers and facilitators to engagement, as part of the wider project.
Implications
These five steps can inform the development of quality fidelity and engagement measures that can be implemented by researchers, providers, and participants for complex health interventions for different populations and is not limited to dementia interventions. Developing high‐quality measures with good psychometric and implementation qualities can advance our understanding of fidelity and engagement outcomes and help us interpret intervention effectiveness more accurately.
The checklists developed from these five steps can be used to measure fidelity of delivery and engagement. Findings from fidelity and engagement assessments can help researchers to understand which components of an intervention were not delivered. From this, difficult to deliver components can be identified and together with interviews exploring barriers and facilitators to delivery; recommendations to improve fidelity of delivery, and training for providers can be developed. Similarly, by understanding participants’ levels of engagement with an intervention, recommendations to improve engagement can be developed.
Future research
Future research could consider how best to formally measure validity, acceptability, and practicality of fidelity and engagement measures. This would help to determine whether measures are in fact high‐quality.
The development of these checklists was part of a larger process evaluation of PRIDE, in which we assessed fidelity and engagement and qualitatively explored barriers and facilitators to fidelity of delivery and engagement (Walton, 2018). These findings will be used to develop recommendations to improve fidelity of delivery and engagement.
Conclusions
Researchers can follow these five steps to develop psychometrically robust and implementable fidelity and engagement measures for complex health interventions that can be used by different audiences, including researchers, providers, and participants. By considering quality when developing measures, we can be more confident in the interpretation of intervention outcomes drawn from fidelity and engagement studies.
The checklists developed in this study were used to measure fidelity of delivery of, and engagement with PRIDE. Together with findings from a qualitative exploration of fidelity and engagement, the findings from fidelity assessments can be used to develop recommendations to improve fidelity of delivery and engagement.
Compliance with ethical standards
The PRIDE programme of research received Health Research Authority approval and NHS ethical approval as part of the feasibility trials intervention ethics application (NHS East Midlands–Nottingham 1 Research Ethics Committee, REC reference number: 16/EM/0044).
Conflicts of interest
The authors declare no conflicts of interest.
Supporting information
Appendix S1. PRIDE Intervention framework.
Appendix S2. PRIDE coding guidelines for researchers.
Appendix S3. Provider/researcher fidelity checklists, Sessions 1–3.
Appendix S4. Participant ‘your experience’ fidelity checklists, Sessions 1–3.
Acknowledgements
Thank you to the wider PRIDE team for providing feedback on draft checklists and helping to gain feedback from PRIDE Public Patient Involvement members. Thank you to the PRIDE Public Patient Involvement members for providing feedback on the PRIDE checklists and coding guidelines. Thank you to Jem Bhatt for piloting the coding guidelines in the first instance. Thank you to Nelli Hankonen, Danielle D'Lima, Niall Anderson, Jo Hale, Ailbhe Finnerty, Catherine Lawrence, and Silje Zink for providing feedback on an earlier version of this manuscript. Holly Walton's PhD research was funded by the Economic and Social Research Council (ESRC) Doctoral Training Centre (Grant reference: ES/J500185/1), as part of the Promoting Independence in Dementia programme (Grant references: 2014‐2015 ES/L001802/1; 2015‐2019 ES/L001802/2). The funding bodies played no role in designing, conducting, analysing, interpreting, or reporting the results of the review.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Bellg, A. J. , Borrelli, B. , Resnick, B. , Hecht, J. , Minicucci, D. S. , Ory, M. , … Treatment Fidelity Workgroup of the NIH Behavior Change Consortium (2004). Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH Behavior Change Consortium. Health Psychology, 23, 443–451. 10.1037/0278-6133.23.5.443 [DOI] [PubMed] [Google Scholar]
- Borrelli, B. (2011). The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. Journal of Public Health Dentistry, 71(Suppl 1), S52–S63. 10.1111/j.1752-7325.2011.00233.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitenstein, S. M. , Gross, D. , Garvey, C. A. , Hill, C. , Fogg, L. , & Resnick, B. (2010). Implementation fidelity in community‐based interventions. Research in Nursing and Health, 33, 164–173. 10.1002/nur.20373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1968). Weighted kappa: Nominal scale agreement provision for scaled disagreement or partial credit. Psychological Bulletin, 70(4), 213–220. 10.1037/h0026256 [DOI] [PubMed] [Google Scholar]
- Csipke, E. , Yates, L. , Cook, E. M. , Leung, P. , Charlesworth, G. , Walton, H. , … Orrell, M. (2018). Promoting independence in dementia: Protocol for a feasibility trial of the PRIDE intervention for living well with dementia. International Journal, 5(4), 177 10.18203/2349-3259.ijct20184399 [DOI] [Google Scholar]
- Feinstein, A. R. , & Cicchetti, D. V. (1990). High agreement but low kappa: I. The problems of two paradoxes. Journal of Clinical Epidemiology, 43, 543–549. 10.1016/0895-4356(90)90158-L [DOI] [PubMed] [Google Scholar]
- Flesch, R. (1948). A new readability yardstick. Journal of Applied Psychology, 32, 221–233. 10.1037/h0057532 [DOI] [PubMed] [Google Scholar]
- French, S. D. , Green, S. E. , Francis, J. J. , Buchbinder, R. , O'Connor, D. A. , Grimshaw, J. M. , & Michie, S. (2015). Evaluation of the fidelity of an interactive face‐to‐face educational intervention to improve general practitioner management of back pain. British Medical Journal Open, 5(7), e007886 10.1136/bmjopen-2015-007886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gearing, R. E. , El‐Bassel, N. , Ghesquiere, A. , Baldwin, S. , Gillies, J. , & Ngeow, E. (2011). Major ingredients of fidelity: A review and scientific guide to improving quality of intervention research implementation. Clinical Psychology Review, 31(1), 79–88. 10.1016/j.cpr.2010.09.007 [DOI] [PubMed] [Google Scholar]
- Gisev, N. , Bell, J. S. , & Chen, T. F. (2013). Interrater agreement and interrater reliability: Key concepts, approaches, and applications. Research in Social and Administrative Pharmacy, 9, 330–338. 10.1016/j.sapharm.2012.04.004 [DOI] [PubMed] [Google Scholar]
- Glasgow, R. E. , Ory, M. G. , Klesges, L. M. , Cifuentes, M. , Fernald, D. H. , & Green, L. A. (2005). Practical and relevant self‐report measures of patient health behaviors for primary care research. The Annals of Family Medicine, 3(1), 73–81. 10.1370/afm.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwet, K. L. (2014). Handbook of inter‐rater reliability (4th ed.). Gaithersburg, MD: Advanced Analytics. [Google Scholar]
- Hankonen, N. , Sutton, S. , Prevost, A. T. , Simmons, R. K. , Griffin, S. J. , Kinmonth, A. L. , & Hardeman, W. (2015). Which behavior change techniques are associated with changes in physical activity, diet and body mass index in people with recently diagnosed diabetes? Annals of Behavioral Medicine, 49(1), 7–17. 10.1007/s12160-014-9624-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardeman, W. , Michie, S. , Fanshawe, T. , Prevost, A. T. , Mcloughlin, K. , & Kinmonth, A. L. (2008). Fidelity of delivery of a physical activity intervention: Predictors and consequences. Psychology and Health, 23(1), 11–24. 10.1080/08870440701615948 [DOI] [PubMed] [Google Scholar]
- Harting, J. , van Assema, P. , van der Molen, H. T. , Ambergen, T. , & de Vries, N. K. (2004). Quality assessment of health counseling: Performance of health advisors in cardiovascular prevention. Patient Education and Counseling, 54(1), 107–118. 10.1016/S0738-3991(03)00194-0 [DOI] [PubMed] [Google Scholar]
- Holmbeck, G. N. , & Devine, K. A. (2009). Editorial: An author's checklist for measure development and validation manuscripts. Journal of Pediatric Psychology, 34, 691–696. 10.1093/jpepsy/jsp046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keith, R. , Hopp, F. , Subramanian, U. , Wiitala, W. , & Lowery, J. (2010). Fidelity of implementation: Development and testing of a measure. Implementation Science, 5(1), 99 10.1186/1748-5908-5-99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller‐Margulis, M. A. (2012). Fidelity of implementation framework: A critical need for response to intervention models. Psychology in the Schools, 1–11. 10.1002/pits.21602 [DOI] [Google Scholar]
- Landis, J. R. , & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174. 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- Lohr, K. N. (2002). Assessing health status and quality‐of‐life instruments: Attributes and review criteria. Quality of Life Research, 11(3), 193–205. 10.1023/A:1015291021312 [DOI] [PubMed] [Google Scholar]
- Lombard, M. , Snyder‐Duch, J. , Bracken, C. C. (2002). Content analysis in mass communication: Assessment and reporting of intercoder reliability. Human Communication Research, 28, 587–604. [Google Scholar]
- Lorencatto, F. , West, R. , Bruguera, C. , & Michie, S. (2014). A method for assessing fidelity of delivery of telephone behavioral support for smoking cessation. Journal of Consulting and Clinical Psychology, 82, 482–491. 10.1037/a0035149 [DOI] [PubMed] [Google Scholar]
- Lorencatto, F. , West, R. , Christopherson, C. , & Michie, S. (2013). Assessing fidelity of delivery of smoking cessation behavioural support in practice. Implementation Science, 8, 40 10.1186/1748-5908-8-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenna, J. W. , Flower, A. , & Ciullo, S. (2014). Measuring fidelity to improve intervention effectiveness. Intervention in School and Clinic, 50(1), 15–21. 10.1177/1053451214532348 [DOI] [Google Scholar]
- Michie, S. , Richardson, M. , Johnston, M. , Abraham, C. , Francis, J. , Hardeman, W. , … Wood, C. E. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46(1), 81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- Moore, G. F. , Audrey, S. , Barker, M. , Bond, L. , Bonell, C. , Hardeman, W. , … Baird, J. (2015). Process evaluation of complex interventions: Medical Research Council guidance. British Medical Journal, 350, h1258 10.1136/bmj.h1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munafo, M. R. , & Smith, G. D. (2018). Repeating experiments is not enough. Nature, 553, 399–401.29368721 [Google Scholar]
- Oakley, A. , Strange, V. , Bonell, C. , Allen, E. , & Stephenson, J. (2006). Process evaluation in randomised controlled trials of complex interventions. British Medical Journal, 332, 413–416. 10.1136/bmj.332.7538.413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn, D. , Burton, A. , Walters, K. , Nazareth, I. , Heinkel, S. , Atkins, L. , … Robinson, V. (2016). Evaluating the clinical and cost effectiveness of a behaviour change intervention for lowering cardiovascular disease risk for people with severe mental illnesses in primary care (PRIMROSE study): Study protocol for a cluster randomised controlled trial. Trials, 17(1), 80 10.1186/s13063-016-1176-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick, B. , Inguito, P. , Orwig, D. , Yahiro, J. Y. , Hawkes, W. , Werner, M. , … Magaziner, J. (2005). Treatment fidelity in behavior change research: A case example. Nursing Research, 54, 139–143. [DOI] [PubMed] [Google Scholar]
- Rixon, L. , Baron, J. , McGale, N. , Lorencatto, F. , Francis, J. , & Davies, A. (2016). Methods used to address fidelity of receipt in health intervention research: A citation analysis and systematic review. BMC Health Services Research, 16(1), 663 10.1186/s12913-016-1904-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts, P. , Priest, H. , & Traynor, M. (2006). Reliability and validity in research. Nursing Standard, 20(44), 41–45. 10.7748/ns2006.07.20.44.41.c6560 [DOI] [PubMed] [Google Scholar]
- Stufflebeam, D. L. (2000). Guidelines for developing evaluation checklists: The checklists development checklist (CDC). Kalamazoo, MI: The Evaluation Center. [Google Scholar]
- The Dementia Engagement and Empowerment Project (DEEP Guide) (2013). Writing dementia friendly information. Retrieved from http://dementiavoices.org.uk/wp-content/uploads/2013/11/DEEP-Guide-Writing-dementia-friendly-information.pdf
- Thyrian, J. R. , Freyer‐Adam, J. , Hannöver, W. , Röske, K. , Mentzel, F. , Kufeld, C. , … Hapke, U. (2010). Population‐based smoking cessation in women post partum: Adherence to motivational interviewing in relation to client characteristics and behavioural outcomes. Midwifery, 26, 202–210. 10.1016/j.midw.2008.04.004 [DOI] [PubMed] [Google Scholar]
- Toomey, E. , Matthews, J. , & Hurley, D. A. (2017). Using mixed methods to assess fidelity of delivery and its influencing factors in a complex self‐management intervention for people with osteoarthritis and low back pain. British Medical Journal Open, 7(8), e015452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahabi, M. , & Ferris, L. (1995). Improving written patient education materials: A review of the evidence. Health Education Journal, 54(1), 99–106. [Google Scholar]
- Viera, A. J. , & Garrett, J. M. (2005). Understanding interobserver agreement: The kappa statistic. Family Medicine, 37, 360–363. [PubMed] [Google Scholar]
- Walton, H. J. (2018). Evaluating the implementation of social interventions to improve independence in dementia. Doctoral Thesis (Ph.D). Retrieved from UCL Discovery: http://discovery.ucl.ac.uk/10064480/
- Walton, H. , Spector, A. , Tombor, I. , & Michie, S. (2017). Measures of fidelity of delivery of, and engagement with, complex, face‐to‐face health behaviour change interventions: A systematic review of measure quality. British Journal of Health Psychology, 22, 872–903. 10.1111/bjhp.12260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton, H. , Tombor, I. , Burgess, J. , Groarke, H. , Swinson, T. , … Michie, S. (submitted). Measuring fidelity of delivery of the community occupational therapy in dementia‐UK intervention. [DOI] [PMC free article] [PubMed]
- Yates, L. , Csipke, E. , Moniz-Cook, E. , Leung, P. , Walton, H. , Charlesworth, G. , … Orrell, M. (2019). The development of the Promoting Independence in Dementia (PRIDE) intervention to enhance independence in dementia. Clinical interventions in aging, 14, 1615 10.2147/CIA.S214367. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. PRIDE Intervention framework.
Appendix S2. PRIDE coding guidelines for researchers.
Appendix S3. Provider/researcher fidelity checklists, Sessions 1–3.
Appendix S4. Participant ‘your experience’ fidelity checklists, Sessions 1–3.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


