Burning mouth syndrome (BMS), also known as glossodynia and stomatodynia, is a chronic oral mucosal pain disorder, without any organic dysfunction. An intense burning or stinging sensation, typically on the tongue or other areas of the oral mucosa, is a characteristic subjective symptom. As with any chronic pain condition, hypersensitivity, depression, and loss of sociality are commonly reported in BMS patients. However, to the best of our knowledge, no case of cutting the tongue for the purpose of alleviating tongue pain has been reported. Here, we report a rare case of BMS leading to death by hanging 10 days after self‐cutting of the tongue.
The patient was a woman in her early 80s who had had a clinical history of depression for about 15 years. In 2014, the patient visited our department and complained of chronic tingling pain localized around tip of her tongue. Abnormal statement was not seen in her mouth, and the pain disappeared during meals. Blood examination (e.g. serum zinc level, serum iron level, and vitamin level) and an oral bacteria test were performed, but there were no abnormal findings. We diagnosed the patient as having glossodynia and prescribed amitriptyline (30 mg/day), sulpiride (150 mg/day), and some herbal medicines along with general psychotherapy. However, the tongue pain did not disappear. As the tongue pain became relentless, paroxetine hydrochloride hydrate (20 mg/day) was added by a psychiatrist, but there was still no improvement.
In January 2016, the patient visited our department with bleeding from the tongue. She had cut off the tip of her tongue with a scissors with the hope of relieving her tongue pain. An approximately 10‐mm wide part of the tongue tip had been amputated, and continued bleeding was observed (Fig. S1). We diagnosed the patient with tongue laceration, and the wound was immediately sutured under local anaesthesia (Fig. S2). Bleeding from the cut surface of the tongue was easily stopped. We referred the patient to a psychiatrist, and she was diagnosed with a somatic symptoms disorder. As her tongue pain was out of control, we hospitalized her for removing pain and watching the wound 2 days after self‐cutting. Several types of injections were used to alleviate tongue pain. During hospitalization, magnetic resonance imaging and single‐photon emission computed tomography of the brain were performed. These exams showed decreased blood flow in both sides of the frontal lobe, parietal cortex, precuneus, and posterior cingulate cortex (Fig. 1). Wound healing of the tongue was fine, but the tongue pain did not disappear (Fig. S3). When the patient missed a follow‐up appointment on day 15, we phoned her at home. We were informed by the patient's family that she had hung herself 3 days after discharge (10 days after self‐cutting).
Figure 1.
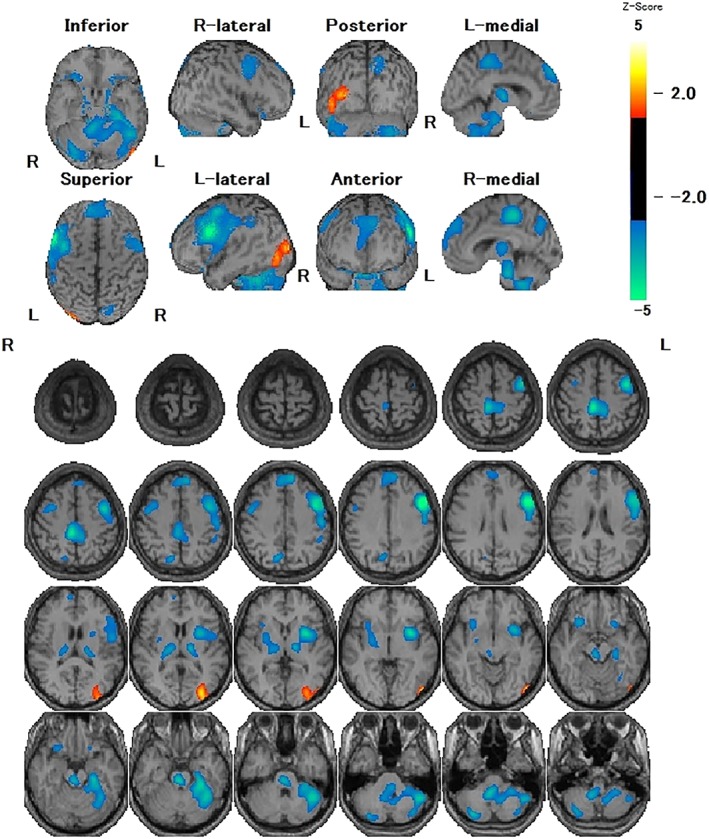
Cerebral blood flow single‐photon emission computed tomography images. Decreased blood flow was observed in both sides of the frontal lobe, parietal cortex, precuneus, and posterior cingulate cortex.
In this case, about 10 mm of the tongue was cut off. Given that this part of the tongue is highly sensitive, it is believed that the purpose of self‐injury was not suicide but pain relief, which was also the explanation given by the patient. Psychoanalytically, the self‐injurious behaviour in this case was an impulsive action based on the patient's delusion that tongue pain might disappear by cutting off the painful part of tongue. According to Simeon and Hollander, self‐injurious behaviour can be organized into four categories: (i) stereotypic; (ii) major; (iii) compulsive; and (iv) impulsive.1 Impulsivity is strongly related to the prefrontal cortex, specifically the orbital part, ventral inner part, and anterior cingulate gyrus. This association was first identified in the famous case of Phineas Gage and subsequently verified by using computer images at the University of Iowa and brain damage studies.2 Interestingly, brain magnetic resonance imaging of our patient revealed localized blood‐flow reduction in the frontal lobe.
Although tongue cutting was a self‐injurious behaviour based on delusions, the patient ultimately killed herself. Suicide is strongly linked to psychiatric disorders. Bertolote and Fleischmann reported that over 90% of suicide attempt cases have a psychiatric disorder.3 In the present case, the patient had had depression for more than 10 years.
Cognitive impairment is often cited as a reason that suicide occurs with depression because cognitive impairment generates pessimistic thoughts and suicidal Ideation. Recent reviews have reported that chronic pain is also associated with an increased risk of suicide mortality and that the rate of suicidal ideation is higher in individuals with pain. Edwards et al. reported that over 30% of patients seeking treatment for chronic pain have thought about suicide in the past.4 Shneidman reported that a common motive for suicide is unbearable mental pain; suicide offers an escape from such pain and occurs when distraction is needed from that pain.5 Beck et al. highlighted the importance of feelings of hopelessness as a psychological state leading to suicide.6 In this case, suicide may have been induced by a feeling of hopeless related to residual tongue pain after tongue cutting and pain relief during hospitalization.
DISCLOSURE
The authors have no potential conflicts of interest to disclosure.
Supporting information
Figure S1 Intraoral photograph at first visit. A portion of the tongue had been cut off, and persistent bleeding was observed.
Figure S2 Sutured tongue.
Figure S3 Tongue 7 days after self‐injury. Epithelialization without bleeding was observed.
ACKNOWLEDGMENTS
The authors thank Enago (http://www.enago.jp/) for the English language review.
REFERENCES
- 1. Simeon D, Hollander E. Self‐Injurious Behaviors: Assessment and Treatment. Washington, DC: American Psychiatric Press, 2001. 10.1176/appi.ajp.159.4.692. [DOI] [Google Scholar]
- 2. The return of Phineas Gage: clues about the brain from the skull of a famous patient . Science 1994; 264: 1102–1105. [DOI] [PubMed] [Google Scholar]
- 3. Bertolote JM, Fleischmann A. Suicide and psychiatric diagnosis: a worldwide perspective. World Psychiatry 2002; 1: 181–185. [PMC free article] [PubMed] [Google Scholar]
- 4. Edwards RR, Smith MT, Kudel I, Haythornthwaite J. Pain‐related catastrophizing as a risk factor for suicidal ideation in chronic pain. Pain 2006; 126: 272–279. [DOI] [PubMed] [Google Scholar]
- 5. Shneidman ES. The Suicidal Mind. New York: Oxford University Press, 1996. [Google Scholar]
- 6. Beck AT, Kovacs M, Weissman A. Hopelessness and suicidal behavior. An overview. JMMA 1975; 234: 146–149. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Intraoral photograph at first visit. A portion of the tongue had been cut off, and persistent bleeding was observed.
Figure S2 Sutured tongue.
Figure S3 Tongue 7 days after self‐injury. Epithelialization without bleeding was observed.


