Abstract
Objective
Internet‐delivered interventions may alleviate distress in cancer survivors with limited access to psychological face‐to‐face treatment. In collaboration with a group of cancer survivors, we developed and tested the efficacy of a therapist‐assisted internet‐delivered mindfulness‐based cognitive therapy (iMBCT) program for anxiety and depression in cancer survivors.
Methods
A total of 1282 cancer survivors were screened for anxiety and depression during their routine oncology follow‐up; eligible breast (n = 137) and prostate cancer (n = 13) survivors were randomized to iMBCT or care‐as‐usual (CAU) wait‐list. Primary outcomes of anxiety and depression were assessed at baseline, 5 weeks, 10 weeks (post intervention), and 6 months.
Results
Significant effects were found for both anxiety (Cohen's d = 0.45; P = .017) and depressive symptoms (d = 0.42; P = .024) post intervention. The effects were maintained at follow‐up for anxiety (d = 0.40; P = .029), but not for depressive symptoms (d = 0.28; P = .131).
Conclusions
Our preliminary findings suggest iMBCT to be a helpful intervention for cancer survivors suffering from symptoms of anxiety. Further studies on the efficacy for symptoms of depression are needed.
Keywords: anxiety, breast cancer, cancer, cancer survivors, cognitive therapy, depressive symptoms, internet, mindfulness, oncology, prostate cancer
1. BACKGROUND
The number of cancer survivors is increasing because of improved diagnosis and treatment. In North America and Europe combined, almost 1 500 000 new cases of breast and prostate cancer were diagnosed in 2018.1, 2 Since 5‐year survival rates for these cancer types are above 85%,3 a significant number of former breast and prostate cancer patients must cope with cancer survivorship. Anxiety and depression are prevalent among cancer survivors, even several years after successful treatment,4, 5, 6 with 2 to 4 times higher prevalence of mood disorders compared with the general population.5, 7 High levels of distress are associated with impaired quality of life, poorer daily function, and—possibly—poorer cancer prognosis.8, 9
Meta‐analyses have shown mindfulness‐based interventions (MBIs) to be efficacious for anxiety and depression with effect sizes (Hedges's g) up to 0.97 and 0.95 in patients with mood disorders10 and 0.39 and 0.44 with cancer patients and survivors.11 Despite documented efficacy, challenges remain to make MBIs available to patients in need because of limited number of trained therapists, costs, and restricted mobility and time constraints among cancer patients and survivors.12, 13, 14, 15
Delivering interventions over the internet is an increasingly popular approach to overcome these challenges. A systematic review of eHealth interventions aimed at breast cancer patients and survivors supports the general feasibility and acceptability of internet‐delivered interventions within this group,16 and two previous studies of internet‐delivered MBIs for psychological distress in cancer patients show promising results.17, 18 One study of cancer patients participating in an online “Mindfulness‐Based Cancer Recovery program” found an effect at post intervention on mood disturbance (d = 0.44) when compared with a wait‐list control.17 The second study explored mindfulness‐based cognitive therapy (MBCT) for psychological distress in cancer patients and found relatively comparable post‐intervention effects of internet‐delivered (d = 0.71) and face‐to‐face–delivered MBCT (d = 0.45) compared with care‐as‐usual (CAU).18 However, in both studies, long‐term effects went uninvestigated and participants were recruited through self‐referral, possibly introducing self‐selection bias. Offering the intervention to patients identified through a systematic screening for distress during follow‐up will add knowledge about the need for intervention and acceptability of internet delivery of such interventions.
Our aim was therefore to evaluate the efficacy of internet‐delivered MBCT (iMBCT) offered as part of routine follow‐up care to breast and prostate cancer survivors experiencing symptoms of anxiety and depression. Breast and prostate cancer were chosen as they are prevalent cancer types with high long‐term survival rates.19 We chose iMBCT as our group has previously found MBCT to be well‐accepted and efficacious for treating persistent pain in breast cancer survivors.20, 21 We compared iMBCT with waitlist CAU controls at post intervention and 6 months follow‐up.
2. METHODS
2.1. Participants
A total of 150 breast and prostate cancer survivors were randomized to iMBCT (70%) or wait‐list control (30%). Inclusion criteria were as follows: scoring greater than or equal to 3 when screened for symptoms of anxiety or depression on a 0‐ to 10‐point numeric rating scale, more than or equal to 3 months and less than or equal to 5 years after completed primary treatment for primary breast or prostate cancer, age 18 years and older, ability to understand and read Danish, internet access, and mobile phone ownership. Exclusion criteria are as follows: cancer recurrence or active cancer treatment (except adjuvant endocrine treatment), insufficient IT skills (self‐reported), and severe mental illness. The study was approved by the regional Science Ethics Committee (registration no: 1‐10‐72‐16‐16) and registered at http://ClinicalTrials.gov (NCT03100981).
2.2. Sample size and randomization
The study was designed to include 155 participants. Randomization was conducted in blocks of 10, with seven blocks allocated to intervention and three to control. The unbalanced allocation aimed at increasing power for subsequent mediation analyses. On the basis of previous reports, we expected an uneven attrition rate of 25% in the intervention group and 15% in the control group,22 leading to a final 80 and 41 participants in intervention and control, respectively. This would allow the detection of a statistical significant (P < .05) Time × Group interaction corresponding to an effect size (Hedge's g) of 0.60 with a statistical power of 83%. While larger than previously found for cancer patients and survivors,11 the effect size is more conservative than those found for face‐to‐face MBIs with patients screened for mood disorders.10 Because of resource and time constraints, recruitment was terminated after inclusion of 150 participants. Expecting an uneven number of eligible breast and prostate cancer survivors, computerized randomization was stratified according to cancer type.23 The allocation sequence was generated by the primary investigator. Research assistants handling recruitment were unaware of group allocation until after the participant was included.
2.3. Procedure
Participants were recruited between February 24, 2016 and August 28, 2017 at the Departments of Oncology and Urology, Aarhus University Hospital. Oncologists or nurses screened all breast and prostate cancer patients for anxiety and depressive symptoms during routine control visits after primary treatment. Eligible interested patients were contacted by telephone for further information about the study. After completing a consent form and online baseline questionnaires (T1), participants were randomly assigned to intervention or wait‐list control. Additional online questionnaires were completed after 5 (T2/midway), 10 (T3/post treatment), and 34 weeks (T4/6 months follow‐up). Follow‐up data collection was finalized on June 27, 2018.
The iMBCT program was developed in collaboration with cancer survivor representatives who recommended program adjustments to meet cancer survivorship needs. For details on this process, see Nissen et al.24 Program content, including the incorporation of cancer‐specific adjustments,20 was adapted from the original face‐to‐face MBCT manual25 by clinical psychologists (M.O.C. and E.R.N.) trained at Oxford Mindfulness Centre with experience of MBCT with cancer survivors.26 Each of the eight 1 week modules included written material, audio exercises, writing tasks, cancer‐specific patient examples, and videos with patients and experts. Participants completed a weekly training diary and mailed it to their therapist who gave written, asynchronous feedback on a prearranged day of the week. Participants were given access to the next module after submitting the tasks of the week (See Data S1 for an overview of intervention content). After completing the program, which included an optional 1 week break, participants had access to treatment materials for 6 months. The secure and encrypted intervention platform was provided by the Department of Internet Psychiatry, Karolinska Institutet, Stockholm, Sweden27 (See Data S2 for screen dump examples). A smartphone‐compliant website with login provided access to daily exercises to participants. Nine therapists, including eight Master's level psychology students trained in MBCT,28 and one experienced psychologist trained in MBCT (E.R.N.) provided the therapist feedback. The student therapists, supervised by two authors (M.O.C., E.R.N.), based their written feedback to participants on a manual‐consistent guide developed for the present study.
Wait‐list controls received auto generated emails asking them to complete online questionnaires at times T2, T3, and T4. If questionnaires were not completed within 1 week, participants received up to three reminder emails. If participants did not respond to reminders, they received a telephone call from a research assistant. The reminder procedures were identical for the intervention and control group. After completing the T4 follow‐up questionnaire, controls were offered iMBCT.
2.4. Measures
2.4.1. Screening
Eligible participants were screened for symptoms of depression and anxiety. Because routine care only allowed a brief screening procedure, a short two‐item measure was used. Patients indicated on 11‐point numerical rating scales (0 = not at all, 10 = very much) “Within the past week, how depressed and sad have you been?” and “Within the past week, how worried and anxious have you been?”. The 3‐point cut‐off was based on our experiences with similar recruitment procedures.21
2.4.2. Participant characteristics
At T1, participants provided sociodemographic and clinical information on gender, date of birth, marital status, educational level, occupation, cancer type, time of diagnosis, and comorbidities.29
2.4.3. Outcomes
The primary outcomes of anxiety and depression were assessed at T1, T2, T3, and T4 with the state subscale of the State‐Trait Anxiety Inventory Y‐Form (STAI‐Y)30 and the Beck Depression Inventory (BDI‐II).31 Internal consistencies (Cronbach's α) in the present sample were .94 and .85, respectively. Secondary outcomes included perceived stress measured at T1, T2, T3, and T4 with the Perceived Stress Scale (PSS‐10)32; well‐being assessed at T1, T3, and T4 with the World Health Organization Well‐Being Index (WHO‐5)33; and sleep disturbance measured at T1, T3, and T4 with the Insomnia Severity Index (ISI).34 Internal consistencies in the present sample ranged from 0.85 to 0.87. Therapist time spent was recorded for each module and participant adherence to the intervention was assessed as total login times for the intervention platform and training website and the number of completed modules. A module was considered completed if the participant had returned a completed “tasks of the week” working sheet to the therapist. Additional variables, not reported on in the present paper, included measures of mindfulness, self‐compassion, weekly distress, and therapeutic alliance.
2.5. Statistical methods
Data were analysed using IBM SPSS Statistics, version 25. Baseline differences were explored with t‐ and chi2 tests. Main intention‐to‐treat analyses were conducted with two‐level multilevel modelling (MLM), with assessments at time points at level 1 nested within individuals at level 2. To compare endpoint effects between groups, a linear function of time was estimated from T1 (baseline) through T3 (post‐assessment) and from T1 through T4 (6‐month follow‐up). Effect sizes (Cohen's d) were derived from the Group × Time F test and calculated as ,35 with magnitudes of 0.2, 0.5, and 0.8 considered small, medium, and large, respectively. MLMs were furthermore employed to evaluate the best fit of time (T1‐T4), including a linear effect (continued improvement), a log‐linear effect (improvement and then maintenance of effect), and a quadratic effect (worsening). This evaluation was based on log likelihood fit statistics (‐2LL), taking into account the number of parameters in the model. The moderating effect of cancer type was analysed with the three‐way MLM interaction term (Time × Group × Cancer type). Because of uneven attrition in the intervention and control group, sensitivity analyses were conducted by repeating analyses for primary outcomes with imputed data for missing responses with the “zero‐effect from baseline”(ZEFB) method, which assumes that participants with missing data do not experience any change during the study period. Adherence‐related effects for participants in the intervention group were explored with two‐way MLM interaction terms (Time × Moderator).
3. RESULTS
3.1. Participant characteristics
A total of 1282 cancer survivors were screened to obtain the final sample of 150 participants (Figure 1). Of these, 137 had been treated for breast cancer (mean age 54.55) and 13 for prostate cancer (mean age = 64.94). The screened patients (n = 1282) had an average score of 1.64 (SD = 2.39) on the depression screening item and 1.85 (SD = 2.55) on the anxiety screening item. Among the included participants, 21 (14.0%) scored greater than or equal to 3 on the anxiety item only, 10 (6.7%) scored greater than or equal to 3 on the depression item only, and 119 (79.3%) scored greater than or equal to 3 on both items. The mean scores of the included participants were 5.5 (SD = 2.1) for anxiety and 4.9 (SD = 2.2) for depression. No baseline differences between the intervention and control groups were found for any sociodemographic, clinical, or outcome variables (Table S3).
Figure 1.
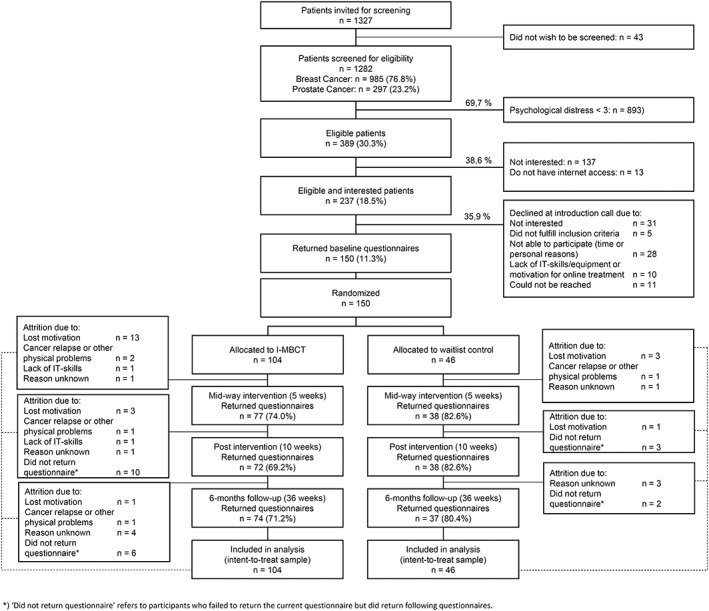
Participant flow diagram
Participants treated for prostate cancer were significantly older, had shorter time since diagnosis, and used less prescription medication than participants treated for breast cancer. Breast cancer survivors had higher baseline scores on stress (P = .015) and well‐being (P = .033) compared with prostate cancer survivors. Attrition rates were higher in the intervention group (26.0% [T2], 30.8% [T3], and 28.8% [T4]) compared with controls (17.4% [T2 and T3] and 19.6%[T4]). Attrition was associated with older age (P = .025) and being a woman/breast cancer survivor (P = .028). When comparing adherent (more than four completed modules) and non‐adherent participants (less than or equal to four completed modules), no statistically significant differences were found for any of the participant characteristics assessed.
3.2. Primary outcomes
Statistically significant Time × Group interactions corresponding to small‐to‐medium effect sizes were found for both anxiety and depression at post intervention (T3). At follow‐up (T4), the Time × Group interaction reached statistical significance for anxiety, but not for depression (Table 1) (separate results for cancer type are shown in Table S4). Model‐fit analyses revealed that for anxiety linear and log‐linear models showed comparable fits, whereas a log‐linear model provided the best fit of the data for depression (Figure S5).
Table 1.
Anxiety, depression, stress, well‐being, and insomnia severity at baseline, mid‐intervention, post‐intervention, and follow‐up
| Outcome | T1: Baseline | T2: Mid‐Intervention | T3: Post‐Intervention | T4: 6 Month Follow‐Up | Effects Time × Group | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| iMBCT | Control | iMBCT | Control | iMBCT | Control | iMBCT | Control | T1‐T3: Baseline–post intervention, Cohen d (95%CI); P | T1‐T4: Baseline–follow‐up (6 months), Cohen d (95% CI); P | |
| N | 104 | 46 | 77 | 38 | 73 | 38 | 74 | 37 | ||
| Primary outcomes (means and SDs) | ||||||||||
| STAI‐Y | 41.7 (10.2) | 42.7 (9.8) | 40.2 (9.2) | 42.7 (9.6) | 37.5 (8.9) | 41.8 (11.9) | 36.3 (9.9) | 40.5 (11.9) | 0.45 (0.26‐0.64); .017 | 0.40 (0.00‐0.80); .029 |
| BDI‐II | 15.1 (7.4) | 17.6 (7.5) | 11.9 (8.3) | 15.0 (8.4) | 10.7 (6.6) | 15.6 (9.2) | 10.2 (7.9) | 14.2 (9.7) | 0.42 (0.23‐0.61); .024 | 0.28 (0.09‐0.47); .131 |
| Secondary outcomes (means and SDs) | ||||||||||
| PSS | 18.5 (5.7) | 18.9 (6.2) | 16.7 (6.0) | 17.5 (6.1) | 15.7 (5.9) | 17.0 (6.3) | 15.0 (6.6) | 17.1 (6.8) | 0.18 (−0.21 to 0.57); .331 | 0.29 (−0.11 to 0.69); .125 |
| WHO‐5 | 17.6 (4.8) | 17.8 (5.4) | N/A | 15.6 (4.7) | 16.5 (5.0) | 15.0 (5.2) | 17.1 (5.6) | 0.25 (−0.14 to 0.64); .173 | 0.48 (0.08‐0.88); .010 | |
| ISI | 11.7 (5.5) | 11.8 (6.3) | N/A | 10.3 (6.0) | 10.1 (6.9) | 10.1 (6.3) | 10.0 (6.3) | 0.06 (−0.33 to 0.45); .759 | 0.04 (−0.36 to 0.44); .847 | |
Note. N = number of participants who filled out questionnaires at the given time point.
No moderating effects of cancer type were found for anxiety or depression at any time point (d = 0.07‐0.15; P = .393‐.697). The ZEFB sensitivity analyses showed that the effects remained statistically significant for anxiety at both post intervention (T3) (d = 0.39; P = .019) and follow‐up (T4) (d = 0.35; P = .033), whereas the post‐intervention (T3) effect for depression no longer reached statistical significance (d = 0.29, P = .073).
3.3. Secondary outcomes
A statistically significant Time × Group interaction corresponding to a medium effect size was found for changes in well‐being (d = 0.48) from baseline to follow‐up (T4). The effect on well‐being at post intervention (T3) failed to reach statistical significance. Likewise, no Time × Group interactions for perceived stress and insomnia severity reached statistical significance at any time point (Table 1).
3.4. Treatment adherence
Of the 104 participants randomized to intervention, 82 (79%) started iMBCT. Participants completed an average of 5.7 out of eight modules, with 46 (56%) completing all eight modules. The reported reasons for not starting or discontinuing iMBCT during the first 4 weeks (n = 51, 49.0%) were lack of motivation (n = 30, 28.8%), insufficient IT skills(n = 13, 12.5%), and cancer relapse or other physical problems (n = 3, 2.9%). Reasons are unknown for four participants (3.8%). Reasons for discontinuing treatment later than module four (n = 7, 6.7%) were lack of motivation (n = 6, 5.8%) and cancer relapse or other physical problems (n = 1, 1.0%). Login data showed that participants spent on average 39 hours and 15 minutes using the program, corresponding to 6 hours and 38 minutes per completed module. Therapists used an average of 117.7 minutes per participant providing feedback, corresponding to 20.3 minutes per completed module. No statistically significant associations were found between improvements in anxiety or depression and number of modules completed, total login time, or therapist time spent (d = 0.06‐0.16; P > .2).
4. DISCUSSION
The present study adds to the few available studies of effects of internet‐delivered MBIs in cancer survivors17, 18 and is the first to evaluate longer‐term effects. The primary outcomes of anxiety and depression were improved immediately after the intervention with between‐group effects largely maintained at the 6‐month follow‐up for anxiety, but not depression. Model fit analyses showed that the depression data fitted a log‐linear curve, suggesting that the improvement in the intervention group occurred in the beginning of the study period and was maintained over time. However, as controls also experienced improvement over time, the between‐group difference diminished at follow‐up. Significant between‐group effects were found for well‐being at the 6‐month follow‐up assessment (d = 0.48). No effects were found for any of the remaining secondary outcomes (stress and insomnia) at any time point.
The effect on symptoms of anxiety remained statistically significant in the sensitivity analysis, suggesting that iMBCT may have a robust, durable effect on anxiety symptoms in breast and prostate cancer survivors. The effect on depression, however, appeared less robust. One possible reason for this could be that the baseline scores were within the range of “mild depression,”36 and could thus indicate a floor effect. One solution for including the patients most likely to benefit could be a more comprehensive screening procedure or a higher cut‐off when screening patients.
While the post‐intervention effect sizes for anxiety and depression found in our study (0.45 and 0.42) are within the same range as those reported in a meta‐analysis of face‐to‐face group MBIs with cancer patients (0.37 and 0.44)11, 18 and the effect found on mood disturbance in the feasibility study of online mindfulness‐based cancer recovery (0.44),17 they are smaller than the effect found on distress in another previous study of iMBCT in cancer patients (0.71). When comparing the results, between‐study differences in participant selection procedures should be noted. While relatively high distress level cut‐offs were applied in the previous studies, ie, HADS scores greater than or equal to 1118 and distress thermometer scores greater than or equal to 4,17 the present study used a lower cut‐off, which could have introduced floor effects. In addition, the previous studies recruited patients through self‐referral, yielding higher inclusion rates, ie, 56%18 and 48%.17 In the present study, only 39% of eligible patients were enrolled, and one third of those who gave consent to be contacted about the study declined after receiving oral information. Thus, while many cancer survivors experience distress, all eligible patients may not find iMBCT equally attractive, and providing iMBCT as a routine offer based on a screening procedure may have included less motivated participants in the present study compared with studies with self‐referral.
Older age emerged a significant predictor of study attrition, i.e., failing to return questionnaires. Age was, however, not associated with intervention drop‐out, i.e., discontinuation of the iMBCT program. This result may be important to consider when offering internet‐delivered therapy to an ageing population in a study setting. Self‐reported reasons for dropping out of the intervention were lack of motivation and insufficient IT skills, and it has previously been found that cancer patients prefer face‐to‐face therapy when asked about preferences.37
With respect to intervention adherence, the number of modules completed did not appear to be associated with the magnitude of effects. One possible explanation for this somewhat counter‐intuitive result could be that adherence to mindfulness is not necessarily reflected in the number of modules completed or time spent on the platform. Furthermore, dropouts may have different reasons for discontinuing the intervention. Some may discontinue because they dislike the intervention, whereas others may discontinue when they have reached what they experience as sufficient improvement. Such reasons are consistent with reports of adherence‐related effects of internet‐delivered interventions in various clinical populations.38, 39, 40 Participants spent on average 6 hours and 38 minutes on each completed module, which would correspond to 2 hours for the session and 39 minutes of practice per day. This is comparable with face‐to‐face MBCT with weekly 2‐hour sessions and the required 45 daily minutes of practice.
The present study has several strengths, including the involvement of patient representatives in the study development, a relatively large sample, a randomized design, and 6 months follow‐up data. In addition, participant recruitment was based on systematic screening of breast and prostate cancer survivors in routine follow‐up care settings.
4.1.1. Study limitations
The present study has a number of limitations that should be noted. First, although the sample size was relatively large, we only nearly achieved the intended inclusion rate. Second, the control condition was a wait‐list CAU condition, which enables the initial evaluation of the relevance of the intervention in the clinical setting. This may be insufficient when assessing the efficacy of the intervention, where an active control condition could have been relevant. Likewise, evaluating non‐inferiority by directly comparing iMBCT with face‐to‐face MBCT, as discussed in Compen et al,18 is highly relevant. We had originally planned to include a third face‐to‐face MBCT arm, but were forced to abandon this approach because of insufficient resources and too few patients available for the study. Third, the distribution of breast and prostate cancer participants in our study sample was uneven. Between‐cancer type differences in follow‐up procedures provided fewer eligible prostate cancer survivors. The follow‐up period for breast cancer is 5 years compared with only 1 year for prostate cancer. Because of the nature of their disease, the two patient groups also differ on several parameters, including gender, age, late effects, and prescription medicine used. While it appears that both breast and prostate cancer survivors may benefit from iMBCT (Table S4), our study is likely underpowered to discern to which degree such cancer type‐related differences influence acceptance and efficacy of iMBCT. Finally, a high attrition rate was observed in the intervention group, especially at the beginning of intervention, which could indicate insufficient recruitment and information procedures. It could be that this type of intervention does not fully meet the needs, expectations, and skills of the target population. Participants completed online questionnaires covering these aspects prior to randomization, but additional in‐depth assessment of motivation and computer literacy prior to intervention start could have been relevant.
4.1.2. Clinical implications
iMBCT appears to be a feasible and flexible intervention for cancer survivors experiencing distress, with promising effects on anxiety and possibly depressive symptoms. Participants attend the programme from their homes, which may be attractive to groups of patients who do not typically seek psychological treatment. We find, in particular, the completion rate and effect among older men treated for prostate cancer encouraging.
5. CONCLUSION
Taken together, iMBCT showed positive effects for anxiety and depression immediately after treatment and for anxiety and well‐being at the 6‐month follow‐up. Despite our intention of maximizing access to treatment by reducing practical barriers for attending face‐to‐face treatment, a substantial percentage of distressed cancer survivors were not interested in an iMBCT intervention when offered as a part of routine follow‐up care.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
Supporting information
Data S1: Intervention content in iMBCT§
Data S2: Screendumps from the program (translated from Danish)
Table S3: Participant characteristics
Table S4: Mean scores for anxiety, depression, stress, well‐being, and insomnia severity at baseline, mid‐intervention, post‐intervention, and follow‐up for intervention and control group, specified for cancer types
Figure S5: Raw outcome scores on primary outcomes over the study period
ACKNOWLEDGEMENTS
We wish to thank the participating patients, the staff at the Departments of Oncology and Urology at Aarhus University Hospital, the student‐therapists, Nina Bennet Kjær Boisen for helping develop the program, and Mia Skytte O'Toole for statistical advice.
TrygFonden (Grant: 7‐12.0736) and the Danish Cancer Society (Grant: R113‐A7015‐14‐S34) funded the study.
Nissen ER, O'Connor M, Kaldo V, et al. Internet‐delivered mindfulness‐based cognitive therapy for anxiety and depression in cancer survivors: A randomized controlled trial. Psycho‐Oncology. 2020;29:68‐75. 10.1002/pon.5237
DATA AVAILABILITY STATEMENT
The data on which the present results are based are available upon request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. International Agency for Research on Cancer . Population Fact Sheet: Europe. Vol 513. 2018.
- 2. International Agency for Research on Cancer . Population Fact Sheet: North America. Vol. 347. 2018.
- 3. Danish Cancer Society [Internet] . [cited 2019. Aug 10]. Available from: http://www.cancer.dk
- 4. Honda K, Goodwin RD. Cancer and mental disorders in a national community sample: findings from the national comorbidity survey. Psychother Psychosom. 2004;73(4):235‐242. [DOI] [PubMed] [Google Scholar]
- 5. Mitchell AJ, Ferguson DW, Gill J, Paul J, Symonds P. Depression and anxiety in long‐term cancer survivors compared with spouses and healthy controls: a systematic review and meta‐analysis. Lancet Oncol. 2013;14(8):721‐732. [DOI] [PubMed] [Google Scholar]
- 6. Dalton SO, Laursen TM, Ross L, Mortensen PB, Johansen C. Risk for hospitalization with depression after a cancer diagnosis: a nationwide, population‐based study of cancer patients in Denmark from 1973 to 2003. J Clin Oncol. 2009;27(9):1440‐1445. [DOI] [PubMed] [Google Scholar]
- 7. Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative‐care settings: a meta‐analysis of 94 interview‐based studies. Lancet Oncol. 2011;12(2):160‐174. [DOI] [PubMed] [Google Scholar]
- 8. Reich M, Lesur A, Perdrizet‐Chevallier C. Depression, quality of life and breast cancer: a review of the literature. Breast Cancer Res Treat. 2008;110(1):9‐17. [DOI] [PubMed] [Google Scholar]
- 9. Prieto JM, Blanch J, Atala J, et al. Psychiatric morbidity and impact on hospital length of stay among hematologic cancer patients receiving stem‐cell transplantation. J Clin Oncol. 2002;20(7):1907‐1917. [DOI] [PubMed] [Google Scholar]
- 10. Hofmann SG, Sawyer AT, Witt A, Oh D. The effect of mindfulness‐based therapy on anxiety and depression: a meta‐analytic review. J Consult Clin Psychol. 2010;78(2):169‐183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Piet J, Würtzen H, Zachariae R. The effect of mindfulness‐based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: a systematic review and meta‐analysis. J Consult Clin Psychol. 2012;80(6):1007‐1020. [DOI] [PubMed] [Google Scholar]
- 12. Holm LV, Hansen DG, Johansen C, et al. Participation in cancer rehabilitation and unmet needs: a population‐based cohort study. Support Care Cancer. 2012/03/15. 2012;20(11):2913‐2924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Barak A, Hen L, Boniel‐nissim M, Shapira NA. Comprehensive review and a meta‐analysis of the effectiveness of internet‐based psychotherapeutic interventions a comprehensive review and a meta‐analysis of the effectiveness of internet‐based psychotherapeutic interventions. J Technol Hum Serv. 2008;26(2–4):109‐160. [Google Scholar]
- 14. Griffiths KM, Christensen H. Review article internet‐based mental health programs: a powerful tool in the rural medical kit. Aust J Rural Health. 2007;15:81‐87. [DOI] [PubMed] [Google Scholar]
- 15. Stanton AL. Psychosocial concerns and interventions for cancer survivors. J Clin Oncol. 2006;24(32):5132‐5137. [DOI] [PubMed] [Google Scholar]
- 16. Triberti S, Savioni L, Sebri V, Pravettoni G. eHealth for improving quality of life in breast cancer patients: a systematic review. Cancer Treat Rev. 2019;74(2018):1‐14. [DOI] [PubMed] [Google Scholar]
- 17. Zernicke KA, Campbell TS, Speca M, McCabe‐Ruff K, Flowers S, Carlson LE. A randomized wait‐list controlled trial of feasibility and efficacy of an online mindfulness‐based cancer recovery program: the eTherapy for cancer applying mindfulness trial. Psychosom Med. 2014;76(4):257‐267. [DOI] [PubMed] [Google Scholar]
- 18. Compen F, Bisseling E, Schellekens M, et al. Face‐to‐face and internet‐based mindfulness‐based cognitive therapy compared with treatment as usual in reducing psychological distress in patients with cancer: a multicenter randomized controlled trial. J Clin Oncol. 2018;36(23):2413‐2421. [DOI] [PubMed] [Google Scholar]
- 19. National Cancer Institute . Cancer Stat Facts. Surveillance, Epidemiology, and End Results Program. 2019.
- 20. Johannsen M, O'Connor M, O'Toole MS, Jensen AB, Højris I, Zachariae R. Efficacy of mindfulness‐based cognitive therapy on late post‐treatment pain in women treated for primary breast cancer: a randomized controlled trial. J Clin Oncol. 2016;34(28):3390‐3399. [DOI] [PubMed] [Google Scholar]
- 21. Johannsen M, O'Connor M, O'Toole MS, Jensen AB, Zachariae R. Mindfulness‐based cognitive therapy and persistent pain in women treated for primary breast cancer. Clin J Pain. 2018;34(1):59‐67. [DOI] [PubMed] [Google Scholar]
- 22. Cuijpers P, van Straten A, Andersson G. Internet‐administered cognitive behavior therapy for health problems: a systematic review. J Behav Med. 2008;31(2):169‐177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Haahr M, Haahr S. https://www.random.org. 2015.
- 24. Nissen ER, Bregnballe V, Mehlsen MY, et al. Patient involvement in the development of a psychosocial cancer rehabilitation intervention: evaluation of a shared working group with patients and researchers. Res Involv Engagem. 2018;4(24):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Segal ZV, Williams JMG, Teasdale JD. Mindfulness‐Based Cognitive Therapy for Depression. 2nd ed. New York: The Guilford Press; 2013:449. [Google Scholar]
- 26. Bartley T. Mindfulness‐Based Cognitive Therapy for Cancer. 1st ed. Oxford: Wiley‐Blackwell; 2012:400. [Google Scholar]
- 27. Titov N, Dear B, Nielssen O, et al. ICBT in routine care: a descriptive analysis of successful clinics in five countries. Internet Interv. 2018;13:108‐115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Farver‐Vestergaard I, Johannsen M, Nissen ER, O'Connor M. Mindfulness‐Baseret Kognitiv Terapi i en sundhedspsykologisk kontekst: Effektstudier og kliniske betragtninger fra Enhed for Psykoonkologi og Sundhedspsykologi. Psyke & Logos. 2016;37:12‐29. [Google Scholar]
- 29. Katz J, Chang L, Sangha O. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34(1):73‐84. [DOI] [PubMed] [Google Scholar]
- 30. Spielberger D, Gorsuch RL, Lushene PR, Vagg PR, Jacobs GA. State‐trait anxiety inventory for adults 1983;76.
- 31. Beck AT, Steere RA, Brown GK. Manual for the Beck Depression Inventory‐II. San Antonio. TX: The Psychological Corporation; 1996. [Google Scholar]
- 32. Cohen S, Williamson G. Perceived stress in a probability sample of the United States In: Spacapan S, Oskamp S, eds. The Social Psychology of Health. Newbury Park, CA: Sage; 1988:31‐67. [Google Scholar]
- 33. Bonsignore M, Barkow K, Jessen F, Heun R. Validity of the five‐item WHO Well‐Being Index (WHO‐5) in an elderly population. Eur Arch Psychiatry Clin Neurosci. 2001;251(Suppl):II27‐II31. [DOI] [PubMed] [Google Scholar]
- 34. Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297‐307. [DOI] [PubMed] [Google Scholar]
- 35. Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. New York: Springer; 2000. [Google Scholar]
- 36. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561‐571. [DOI] [PubMed] [Google Scholar]
- 37. Wallin EEK, Mattsson S, Olsson EMG. The preference for internet‐based psychological interventions by individuals without past or current use of mental health treatment delivered online: a survey study with mixed‐methods analysis. JMIR Ment Heal. 2016;3(2):e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Donkin L, Christensen H, Naismith SL, Neal B, Hickie IB, Glozier N. A systematic review of the impact of adherence on the effectiveness of e‐therapies. J Med Internet Res. 2011;13(3):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Donkin L, Hickie IB, Christensen H, et al. Rethinking the dose‐response relationship between usage and outcome in an online intervention for depression: randomized controlled trial. J Med Internet Res. 2013;15(10):e231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Arndt A, Lutz W, Rubel J, et al. Identifying change‐dropout patterns during an internet‐based intervention for depression by applying the Muthen‐Roy model. Cogn Behav Ther. 2019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1: Intervention content in iMBCT§
Data S2: Screendumps from the program (translated from Danish)
Table S3: Participant characteristics
Table S4: Mean scores for anxiety, depression, stress, well‐being, and insomnia severity at baseline, mid‐intervention, post‐intervention, and follow‐up for intervention and control group, specified for cancer types
Figure S5: Raw outcome scores on primary outcomes over the study period
Data Availability Statement
The data on which the present results are based are available upon request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


