Abstract
Background
Given the major changes in internet use for health communication, the objective of the current study was to compare the internet use and wishes of cancer survivors between 2005 and 2017.
Methods
The authors drew a sample of 390 patients in 2005 and 539 patients in 2017 who were diagnosed with breast (128 patients in 2005 and 143 patients in 2017), prostate (96 patients in 2005 and 126 patients in 2017), or gynecologic (89 patients in 2005 and 188 patients in 2017) cancer or lymphoma (77 patients in 2005 and 82 patients in 2017) in 4 different hospitals for the periods 2002 through 2004 and 2014 through 2016. These patients were sent a paper‐based questionnaire that contained 45 questions regarding demographics and 4 functions of internet use: content, communication, community, and e‐health.
Results
The response in 2017 (53%) was lower than that in 2005 (75%). Survivors browsed the internet most frequently to search for information regarding cancer shortly after being diagnosed and while waiting for treatment. There was little change noted with regard to the relative importance attached to the various subjects. In 2017, significant increases were evident with regard to finances (+33%), health care insurance (+29%), and genetics and/or heritability (+27%). The wishes expressed in 2005 by patients were realized in part in 2017.
Conclusions
A significant sample of cancer survivors in the Netherlands have indicated that the internet is an important source of information regarding their illness. However, little change was evident over the past 15 years with regard to patients' priorities regarding their wishes for internet use. The wishes of users in 2005 were found to accurately reflect the internet use of the majority of patients in 2017. The results of the current study support the belief that health care professionals should expand their online services and tailor them toward the needs and wishes of their patients.
Keywords: breast cancer, cancer survivors, gynecologic cancer, internet, lymphoma, prostate cancer
Short abstract
The internet wishes of patients with cancer reported in 2005 accurately reflect the internet use of the majority of patients in 2017. The current study supports the belief that health care professionals should expand their online services and tailor them toward the needs and desires of their patients.
Introduction
Over the past 15 years, major changes in internet use have occurred. Increasing numbers of individuals are using the internet, often daily, through broadband connections as well as mobile devices. This is especially true in the Netherlands, where the availability of the internet is very high.1 Next to the increase in use, an enormous expansion in internet‐based applications and internet‐based communication options such as Skype, FaceTime, Facebook, Instagram, and WhatsApp are available. It has become relatively simple to maintain remote contact with loved ones and colleagues. In addition to text, messages increasingly are received with still or moving images.1, 2
These new options also frequently are used in the health care sector. Patients are not only searching the internet for information regarding their illness but also to establish online contact with caregivers. Other frequently used internet options are reading or posting content in health communities. Moreover, when available, patients get access to their electronic health record (EHR) or obtain online treatment. The number of individuals with cancer using the internet in relation to their illness also has increased, although to our knowledge studies differ greatly with regard to the number.3, 4, 5
Although internet use has drastically changed in recent years, in our opinion the most comprehensive description of how internet use can influence cancer survivors still is the model that Eysenbach outlined in 2003.6 According to this model, patients use the internet for: 1) content; 2) communication; 3) communities; and 4) e‐commerce. This currently is referred to as e‐health.7, 8
Given these major changes in internet use, both in general and for health communication in particular, an important question is to what extent use of the internet by cancer survivors and their wishes for online modalities have changed in recent years. The current study has addressed this question by repeating and extending a study by van de Poll‐Franse and van Eenbergen3 published in 2005, which presented the future wishes regarding the internet of patients with cancer. In 2017, we hypothesized that approximately 75% of cancer survivors would search online for content, that approximately 20% would be active within a community, that approximately 45% would communicate with their caregiver, and that approximately 70% would access their own EHR.
Materials and Methods
A population‐based, cross‐sectional survey regarding internet use was conducted through the Netherlands Cancer Registry (NCR). In 2005, we drew a random sample of 390 patients with breast (128 patients in 1 hospital), prostate (96 patients in 1 hospital), or gynecologic (89 patients in 2 hospitals) cancer or lymphoma (77 patients in 2 hospitals) who were diagnosed between 2002 and 2004 and who were aged ≤65 years at the time of diagnosis. In October 2016, we again drew a random sample of 523 patients with breast (138 patients), prostate (125 patients), or gynecologic (184 patients) cancer or lymphoma (76 patients) who were diagnosed in the same hospitals between 2014 and 2016 and who were aged ≤70 years at the time of diagnosis. We thought that the elderly of 2017 would be more internet‐confident compared with the elderly of 2005. For that reason, we increased the age range by 5 years.
To exclude all deceased patients, the patient samples were linked with the Dutch municipal records database, which contains mortality and residential data from all citizens through municipal registries. Addresses were checked for correctness and all surviving patients (349 patients and 496 patients, respectively) then were sent an information letter together with a paper‐and‐pencil questionnaire by their oncologist (Fig. 1). By replying, the patients explicitly agreed to participate and consented to the linkage of their questionnaire data with their disease history as registered in the NCR. The returned questionnaires were identifiable only by a study number, which guaranteed patient anonymity. A declaration of no objection was granted by the Medical Ethics Review Committee Midden Brabant (NW2016‐47).
Figure 1.
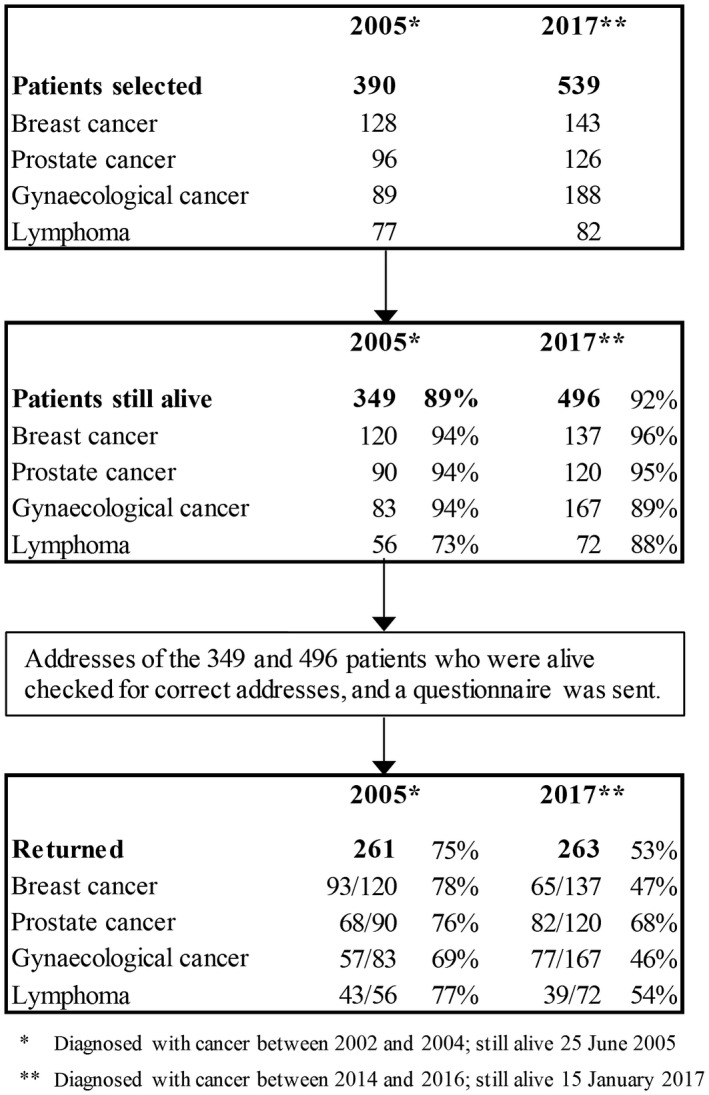
Flowchart of the data collection process.
The NCR routinely collects data regarding tumor characteristics such as date of diagnosis, subsite, histology, stage (using the TNM clinical classification), and primary treatment and patient characteristics including sex and date of birth.
Because to our knowledge no validated Dutch questionnaire regarding internet use by patients with cancer existed, we developed such a questionnaire in 2004. This questionnaire was based on a literature study and the 4 areas defined by Eysenbach.6 In 2017, we used the same questionnaire but updated some questions because of internet developments in the intervening years, including increased access to e‐health, social media, and blended care. In both questionnaires, patients were asked about their use of the internet and other sources of information for health care–related purposes and about their wishes regarding future internet use for health care–related purposes.
Statistical Analyses
All statistical analyses were performed using SPSS statistical software (version 24.0; IBM Corporation, Armonk, New York). Data regarding patient and tumor characteristics were compared between internet users and nonusers (both within and between the 2005 and 2017 cohorts) using chi‐square analyses for categorical variables and Student t tests for continuous variables. Tests were 2‐sided and considered statistically significant at P < .05.
Results
The questionnaire response in 2017 (53%) was lower than that in 2005 (75%). We did not measure significant differences between respondents and nonrespondents in 2005, but did so in 2017. Respondents in 2017 were older (aged 62.5 years vs 58.5 years; P = .001), were less often female (62% vs 74%; P = .005), and differed with regard to tumor type (P < .001) (see Supporting Table 1). In both years, we asked respondents in the survey not to answer a subitem when it was not applicable to them. In the 2008 article,3 we calculated the percentage based on the respondents of that question, mostly between 90 and 110 of the 153 internet users. In the current study, we calculated the results based on the number of respondents who used the internet (153 respondents and 223 respondents, respectively, in 2005 and 2017). This adaptation was necessary to enable a meaningful comparison with the earlier results to establish trends.
Characteristics of Patients Who Use the Internet
General daily use of the internet by patients with cancer increased from 49% in 2005 (153 patients) to 85% in 2017 (223 patients) whereas illness‐related daily internet use increased from 60% in 2005 to 85% in 2017 (Table 1). Patients were asked when as well as how often they browsed the internet for information regarding cancer: never (0), several times a year/month (1), several times a week (2), or daily (3). In both years, the mean search frequency varied from 2.5 right after diagnosis, 2.3 during treatment, 2.0 just before diagnosis, and 1.8 during follow‐up.
Table 1.
Patient Characteristics by Internet Use, Separated by Year of Study
| Characteristics | 2005 N = 254a | 2017 N = 263 | Internet Use 2005 Versus 2017 | ||||
|---|---|---|---|---|---|---|---|
| Yes Internet use n (%) | No Internet use n (%) | P | Yes Internet use n (%) | No Internet use n (%) | P | P | |
| Internet use | 153 (60) | 101 (40) | 223 (85) | 40 (15) | <.001 | ||
| Sex | |||||||
| Female | 86 (53) | 77 (47) | 140 (85) | 24 (15) | |||
| Male | 67 (74) | 24 (26) | .001 | 83 (84) | 16 (16) | .738 | .201 |
| Mean age at survey, y time: | 54.6 | 59.5 | <.001 | 60.9 | 71.3 | <.001 | <.001 |
| <50 years | 44 (80) | 11 (20) | 39 (100) | 0 (0) | |||
| 50‐65 years | 96 (57) | 72 (43) | 98 (91) | 10 (9) | |||
| >65 | 13 (42) | 18 (58) | .001 | 86 (74) | 30 (26) | <.001 | <.001 |
| Tumor | |||||||
| Breast | 45 (49) | 47 (51) | 61 (94) | 4 (6) | |||
| Prostate | 46 (77) | 20 (23) | 70 (85) | 12 (15) | |||
| Gynecologic | 30 (56) | 24 (44) | 64 (83) | 13 (17) | |||
| Lymphoma | 32 (76) | 10 (24) | .006 | 28 (72) | 11 (28) | .024 | .067 |
| Months since diagnosisb | |||||||
| 10‐18 | 34 (65) | 18 (35) | 6 (100) | 0 (0) | |||
| 19‐24 | 38 (60) | 25 (40) | 48 (92) | 4 (8) | |||
| 25‐30 | 32 (64) | 18 (36) | 73 (83) | 15 (17) | |||
| 31‐42 | 49 (55) | 40 (45) | .600 | 96 (83) | 20 (17) | .261 | <.001 |
| Educational levelc | |||||||
| Primary school | 19 (27) | 52 (73) | 40 (57) | 30 (43) | |||
| Secondary school | 66 (62) | 40 (38) | 108 (93) | 8 (7) | |||
| College/university | 67 (89) | 8 (11) | <.001 | 74 (100) | 0 (0) | <.001 | .081 |
| Employment statusd | |||||||
| Employed | 72 (69) | 32 (31) | 94 (95) | 5 (5) | |||
| Unemployed | 77 (54) | 65 (46) | .017 | 119 (79) | 31 (21) | .001 | .431 |
| Marital statusc | |||||||
| Married/living together | 122 (58) | 87 (42) | 183 (85) | 32 (15) | |||
| Partner, not living together | 8 (80) | 2 (20) | 13 (93) | 1 (7) | |||
| No partner | 22 (67) | 11 (33) | .286 | 26 (84) | 5 (16) | .706 | .724 |
| Childrene | |||||||
| No | 35 (71) | 14 (29) | 33 (97) | 1 (3) | |||
| Yes, living with | 36 (78) | 10 (22) | 40 (100) | 0 (0) | |||
| Yes, living somewhere else | 82 (52) | 76 (48) | .001 | 149 (79) | 39 (21) | <.001 | .027 |
Seven patients did not complete this question.
Missing data for 1 patient in 2017.
Missing data for 2 patients in 2005 and 3 patients in 2017.
Missing data for 5 patients in 2017.
Missing data for 1 patient in 2005.
In 2005, men were more likely to use the internet compared with women, whereas in 2017 this difference was no longer significant. The mean age of the participants in 2017 was higher compared with in 2005 (62.5 years vs 56.7 years), and more patients in 2017 had reached retirement age compared with in 2005 (41% vs 25%). In addition, in 2017, fewer patients were unemployed compared with in 2005 (24% vs 45%), and retired patients in both 2005 and 2017 used the internet less frequently than patients who were younger than retirement age.
The results of the 2 studies closely corresponded in terms of how patients ranked the importance of various information sources (Table 2). Patients rated caregivers, especially medical oncologists and oncology nurses, as their most important sources of information (90%). Significant changes (>10%) between 2005 and 2017 were evident for oncology nurses (from 60% to 70%) and general practitioners (from 58% to 45%). The greatest increase was noted for the internet (from 34% to 47%), whereas the greatest decrease was observed for books (from 29% to 15%).
Table 2.
Important Sources of Information Among All Respondents
| Ranking 2017/2015 | 2017 N = 263 No. (%) | 2005 N = 261 No. (%) | |
|---|---|---|---|
| Medical oncologist | 1/1 | 235 (90) | 229 (88) |
| Oncology nurse | 2/2 | 184 (70) | 156 (60) |
| Family | 3/3 | 145 (55) | 158 (61) |
| Friends | 4/5 | 133 (51) | 141 (54) |
| Internet for information | 5/7 | 124 (47) | 88 (34) |
| Children | 6/6 | 121 (46) | 136 (52) |
| General practitioner | 7/4 | 118 (45) | 151 (58) |
| Other patients | 8/10 | 64 (24) | 72 (28) |
| Pharmacist | 9/12 | 56 (21) | 42 (16) |
| Newspapers and/or television | 10/9 | 47 (18) | 73 (28) |
| Colleagues | 11/11 | 45 (17) | 52 (20) |
| Books | 12/8 | 40 (15) | 75 (29) |
| Second‐opinion physician | 13/13 | 25 (10) | 34 (13) |
Internet for Content, Communication, Community, and e‐Health
Content
Approximately 34% of respondents in 2005 and approximately 47% of respondents in 2017 regarded the internet as an important source of information concerning their illness. A larger percentage (61% and 79%, respectively) searched for information on their own type of cancer (Table 3). Between 2005 and 2017, there was little change observed in the relative importance attached to the various subjects. The most frequently browsed topics were cancer type, consequences of treatment, and cancer treatment. In 2017, significant increases were evident in finances (+33%), health care insurance (+29%), and genetics and/or heritability (+27%). Additional analyses among respondents who considered the internet to be an important source of information (88 respondents in 2005 and 124 respondents in 2017) demonstrated similar findings.
Table 3.
Types of Information Searched for on Internet by Patients (%)
| All Internet Users | |||
|---|---|---|---|
| 2017/2005 Ranking | 2017 N = 223 % | 2005 N = 153 % | |
| Type of cancer | 1/1 | 79 | 61 |
| Consequences of treatment in general | 2/3 | 72 | 58 |
| Treatment | 3/2 | 70 | 59 |
| Cancer genetics and/or heritability | 4/7 | 57 | 30 |
| Treatment guidelines | 5/4 | 48 | 37 |
| What I can do myself | 6/5 | 42 | 35 |
| Consequences for sexuality | 6/6 | 42 | 33 |
| Health care insurance coverage | 8/12 | 41 | 12 |
| Fatigue | 9/8 | 39 | 28 |
| Financial consequences | 9/18 | 39 | 6 |
| Which hospital is best | 11/16 | 20 | 7 |
| Cancer support groups | 12/9 | 18 | 20 |
| Trials and/or research | 12/10 | 18 | 18 |
| Patient activities in region | 12/12 | 18 | 12 |
| Alternative medicine | 15/11 | 14 | 17 |
| Where to find a good oncologist | 15/16 | 14 | 7 |
| End of life | 17/14 | 12 | 8 |
| Consequences for future parenthood | 18/14 | 5 | 8 |
Communication
In 2017, approximately 66% of patients maintained online contact with colleagues, friends, and family members. There was an increase compared with 2005 that ranged from 18% (friends) to 30% (children). In 2017, there also was greater online contact with caregivers reported compared with in 2005. Contact with oncology nurses increased from 3% to 32%, and with medical oncologists from 7% to 27%. Communication with other patients was similar between the 2 studies (12% and 13%, respectively, in 2005 and 2017).
Communities
From 2005 to 2017, the number of patients who visited online health communities for content (Table 3) demonstrated a slight decrease (20% to 18%). In 2015, approximately 6% of patients maintained online contact via such options as chat, bulletin boards, and online chats. In 2017, the percentage of patients who actively participated in an online community was 24% (Table 4).
Table 4.
Patients' Wishes for Future Internet Possibilities in 2005 and 2017 and Patients' Current Use
| Ranking 2017/2005 | Wishes 2017 N = 223 Yes, % | Wishes 2005 N = 153 Yes, % | Current Use 2017 N = 223 Yes, % | |
|---|---|---|---|---|
| Aspects in 2005 and 2017 | ||||
| Accessing own test results | 1/1 | 75 | 70 | 31 |
| Accessing own medical file | 2/2 | 72 | 69 | 33 |
| Making an appointment | 3/3 | 71 | 60 | 24 |
| Requesting prescriptions | 4/4 | 69 | 59 | 32 |
| Emailing with oncologist | 5/6 | 61 | 44 | 25 |
| Receiving reminders | 6/9 | 55 | 36 | 24 |
| Making complaints | 7/5 | 54 | 48 | 26 |
| Emailing with nurse | 8/14 | 53 | 26 | 35 |
| Requesting tests | 9/8 | 46 | 37 | 40 |
| Suggesting ideas | 10/7 | 42 | 39 | 14 |
| Requesting referral | 10/9 | 42 | 36 | 9 |
| Performing test/self‐diagnoses | 12/12 | 27 | 27 | 2 |
| Requesting oncologist via forum | 13/11 | 20 | 29 | 4 |
| Chatting with others | 14/15 | 18 | 17 | 24 |
| Questioning oncologist in patient forum | 15/13 | 15 | 27 | 2 |
| New issues in 2017 | ||||
| Receiving personal advice on symptoms | 63 | — | — | |
| Receiving advice on additional care | 56 | — | — | |
| Self‐monitoring of consequences of treatment | 49 | — | — | |
| Rating of caregivers/hospitals | 42 | — | — | |
| Participating in online self‐management class | 20 | — | — |
E‐health
In 2005, approximately 69% of patients wanted online access to their EHR. In 2017, approximately 33% of the patients actually accessed their EHR. The 2 studies demonstrated only a slight increase in the patient's wish to access their EHR from 69% to 72%.
Differences in Wishes and Possibilities
In 2005 and 2017, patients with cancer were asked which internet possibilities they would like to use if their caregivers offered them. In 2017, 5 new possibilities were added as a result of technological developments (Table 4). For all possibilities, the wish to use them was higher in 2017 compared with 2005, with the exception of forum‐related topics. Of the 5 possibilities added in 2017, “personal advice on symptoms” (63%) and “advice on additional care” (56%) were found to be at the top of the ranking.
The wishes expressed in 2005 were realized in part in 2017 (see the “Current Use” column in Table 4). “Accessing own medical file,” “accessing own test results,” and “requesting prescriptions” were in the top 5 of wished possibilities in 2005 and realized possibilities in 2017.
Discussion
Of the 2 samples of Dutch cancer survivors in 2005 (261 survivors) and 2017 (263 survivors) that we compared in the current study, approximately 60% and 85%, respectively, had internet access. Of those who used the internet in 2017, approximately 85% did so daily. This suggests that, similar to the general population, patients with cancer increasingly are often online (78% of patients in 2005 and 98% of patients in 2017 had internet access9).
Although internet use among patients has increased dramatically over the past 12 years, to our knowledge the relative importance they attach to various types of information appears to have hardly changed. The behavior of “early adopters” in 2005 reflects the behavior of the majority of cancer survivors in 2017. The personal characteristics of educational level and age group continue to influence patients' internet use and appear to contribute toward a type of “digital divide.”10, 11, 12 In the current study, patients in the group of internet users and the subgroup of “internet‐important” users were significantly younger and more highly educated compared with patients who did not use the internet. The relation between internet use and being unemployed and “having children who live on their own” was strongly related to age. In our 2017 study, it was interesting to note that the “lag” in internet use by females had completely disappeared. Because these characteristics are fixed for all participants, it is advisable that caregivers pay extra attention to the group of patients who do not use internet to ensure that they are not disadvantaged.
During a period of illness, the information need (content) is influenced by personal and disease characteristics13, 14 and is largest during the diagnosis and treatment phases.15, 16 Although the physician is the most important source of information,5, 17 over the past 10 years the importance of the internet as a source of information has increased.11, 12 We hypothesized that in 2017, approximately 75% of cancer survivors would search online for content. In 2017, we found that approximately 79% of the respondents searched the internet for content related to their cancer type, which was somewhat more than expected and an increase of 18% compared with 2005. The majority of respondents searched the internet after being diagnosed with cancer and just before initiating treatment. It reasonably can be assumed that patients in the early phases of their disease trajectory have many unanswered questions.15, 16, 18 It can be difficult for patients to assess the reliability of the content they have found, especially in the early phases. Therefore, one wish of patients is that their caregivers recommend suitable websites for them to consult.19, 20
Between 2005 and 2017, there was a striking increase in the wish for information regarding finances and insurance. Societal changes (eg, in the area of employment status) may have driven this change.21 The data from the current study demonstrate that this aspect has become especially important for young respondents.
Online contact between patients demonstrated little change over the period from 2005 through 2017. Irrespective of the function, approximately 20% of the patients found some form of contact with other patients to be important. Among online communities, including those regarding health care–related topics, it is known that approximately 1% of the visitors actively post content, whereas 9% react to it and 90% read it.22 That would suggest that of every 100,000 patients newly diagnosed with cancer, only 200 actively post. Online cancer‐related communities have been established by patient groups, health care providers, on social media, and on focused websites. This fragmentation is not in the best interests of patients. To create a coherent, effective, and active community, bundling of forces appears to be advisable.
Communities of patients with cancer provide mutual emotional and informational support, which can positively influence quality of life.7, 8 Ziebland and Wyke concluded that this community opportunity was the greatest internet‐driven change: “Patients learning to tell the story and visualizing disease.”23 Based on wishes reported in the 2005 study, we hypothesized that approximately 20% of patients with cancer wished to participate in communities. In 2017, the rate of participation was 24%. Over the past 10 years, the power of social media has become increasingly evident.2 This may have influenced the recognition by increasing numbers of survivors of the added value of the online sharing of knowledge and experiences.23
Communication often takes the form of emailing with the caregiver, relatives, and other patients.6 A recent study in several countries in the European Union found that email contact with caregivers has greatly increased in recent years, varying between 19% and 51% of patients.20 In 2005, nearly one‐half of patients wanted to be able to communicate with their caregivers, although in 2017 only 1 in 4 patients was able to communicate digitally (by email) with their oncologist and only 1 in 3 patients was able to do so with their oncology nurse. For this internet function as for others, it is mainly those individuals with a higher educational level, young people, and males who communicate with a caregiver.20, 24
E‐health applications of various types are used in cancer care, although to our knowledge little is known regarding their use and impact on patients.25, 26 For the purposes of the current study, we measured e‐health as patients' access, via a portal, to their EHR. We hypothesized, based on wishes expressed in the 2005 study, that approximately 70% of the internet‐using respondents wished to be able to have access to their EHR. In 2017, only 33% of respondents actually had such access. The health care sector appears to respond slowly to patients' wishes. Hospitals in the Netherlands currently are investing in the implementation of these systems. The information present in EHRs does strengthen the position of patients with respect to, as an example, shared decision making.27, 28 We expect that the possibilities will increase in coming years as a result of societal and technological developments.26
Interesting additional wishes since 2005 are the ability of patients to self‐monitor the impact of their disease and treatment, including the wish for personalized advice regarding how to deal with symptoms and the search for complementary care. This is consistent with recent studies suggesting that self‐monitoring of the side effects of chemotherapy and/or radiotherapy has positive effects, including fewer hospital admissions, an enhanced quality of life, and even improved survival.29, 30 Due to the general increase in cancer incidence and prevalence31 and the greater knowledge among patients,32 increasing numbers of patients are aware of the possibilities to reduce the damaging side effects resulting from chemotherapy and radiotherapy. As more e‐health services become available, it will become increasingly necessary to conduct supplementary research into patient use of those services according to educational level and age group to tailor the service provision to the wishes of patients.14, 33
Limitations
The current study had several limitations. The response rate in 2017 was lower than that in 2005 (53% vs 75%) and the respondents in 2017 were somewhat older than those in the 2005 study (mean age, 62.5 years vs 56.7 years). For >10 years, the Patient Reported Outcomes Following Initial treatment and Long‐term Evaluation of Survivorship (PROFILES) research group has been studying cancer survivors. They also have observed a general decline in response rates.34 The design of the current study yielded more female respondents than males, although in 2017 the 2 sexes appeared to access the internet to a similar extent.
Another limitation of the current study approach was the influence of changes in internet use over the time period of the study. Patients with cancer may have used different devices to consult the internet in 2017 compared with in 2005. Individuals who were aged 65 years in 2017 were aged 53 years in 2005, and they likely have had more exposure to the internet compared with a 65‐year‐old patient in 2005. Nevertheless, we also included patients aged ≥65 years in the 2017 cohort.
Conclusions
Internet use by cancer survivors has increased by approximately 25% over the past 15 years, but little change is evident with regard to the wishes of these individuals concerning the internet.
For internet functions that patients can easily access themselves, internet use appears to correspond fairly closely with their wishes. However, in situations in which patients are dependent on caregivers, the possibilities for internet use have been found to be more limited compared with the wishes.
Higher educational level and younger age continue to be important positive indicators of access to and use of the internet. These personal characteristics are impossible to influence and may have resulted in a “digital divide” between different types of patients.
We believe the results of the current study support the need for health care professionals to expand their online communication possibilities and e‐health services and tailor them to the wishes of their patients. It appears that future patients will be not only health care consumers but also health care partners. Future research should focus on specific e‐health needs and the effect of their active participation on treatment. To limit the disadvantages of the “digital divide,” research also should focus on how caregivers can involve less educated and older patients in treatment and decision making.
Funding Support
No specific funding was disclosed.
Conflict of Interest Disclosures
The authors made no disclosures.
Author Contributions
Mies C. H. J. van Eenbergen: Conceptualization, data curation, formal analysis, methodology, writing–original draft, and writing–review and editing. Ruben D. Vromans: Data curation, formal analysis, and writing–review and editing. Dorry Boll: Data curation and writing–review and editing. Paul J. M. Kil: Data curation and writing–review and editing. Caroline M. Vos: Data curation and writing–review and editing. Emiel J. Krahmer: Formal analysis, methodology, supervision, and writing–review and editing. Floortje Mols: Formal analysis, methodology, supervision, and writing–review and editing. Lonneke V. van de Poll‐Franse: Formal analysis, methodology, supervision, and writing–review and editing. All authors have read and approved the contents of this article.
Supporting information
We wish to thank the patients and their physicians at the following Dutch hospitals for their participation in this study: Catharina Hospital (Eindhoven), Elisabeth‐TweeSteden Hospital (Tilburg), and Maxima Medical Center (Veldhoven).
References
- 1. Centraal Bureau voor de Statistiek . Households–connection to the internet. Accessed October 31, 2018. https://opendata.cbs.nl/statline/#/CBS/nl/dataset/83291NED/table?ts=1560934345782.
- 2. Poushter J. Smartphone ownership and internet usage continues to climb in emerging economies. But advanced economies still have higher rates of technology use. Pew Research Center; 2016. Accessed September 17, 2019. https://www.pewresearch.org/wp-content/uploads/sites/2/2016/02/pew_research_center_global_technology_report_final_february_22__2016.pdf [Google Scholar]
- 3. van de Poll‐Franse LV, van Eenbergen MC. Internet use by cancer survivors: current use and future wishes. Support Care Cancer. 2008;16:1189‐1195. [DOI] [PubMed] [Google Scholar]
- 4. An LC, Wallner L, Kirch MA. Online social engagement by cancer patients: a clinic‐based patient survey. JMIR Cancer. 2016;2:e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nagler RH, Gray SW, Romantan A, et al. Differences in information seeking among breast, prostate, and colorectal cancer patients: results from a population‐based survey. Patient Educ Couns. 2010;81(suppl):S54‐S62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eysenbach G. The impact of the Internet on cancer outcomes. CA Cancer J Clin. 2003;53:356‐371. [DOI] [PubMed] [Google Scholar]
- 7. van Eenbergen MC, van de Poll‐Franse LV, Krahmer E, Verberne S, Mols F. Analysis of content shared in online cancer communities: systematic review. JMIR Cancer. 2018;4:e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. van Eenbergen MC, van de Poll‐Franse LV, Heine P, Mols F. The impact of participation in online cancer communities on patient reported outcomes: systematic review. JMIR Cancer. 2017;3:e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eurostat . Households – level of internet access. Accessed June 19, 2019. https://ec.europa.eu/eurostat/web/products-datasets/-/isoc_ci_in_h
- 10. Xie B, Wang M, Feldman R, Zhou L. Internet use frequency and patient‐centered care: measuring patient preferences for participation using the health information wants questionnaire. J Med Internet Res. 2013;15:e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kowalski C, Kahana E, Kuhr K, Ansmann L, Pfaff H. Changes over time in the utilization of disease‐related Internet information in newly diagnosed breast cancer patients 2007 to 2013. J Med Internet Res. 2014;16:e195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Greenberg‐Worisek AJ, Kurani S, Finney Rutten LJ, Blake KD, Moser RP, Hesse BW. Tracking Healthy People 2020 internet, broadband, and mobile device access goals: an update using data from the Health Information National Trends Survey. J Med Internet Res. 2019;21:e13300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Warren E, Footman K, Tinelli M, McKee M, Knai C. Do cancer‐specific websites meet patient's information needs? Patient Educ Couns. 2014;95:126‐136. [DOI] [PubMed] [Google Scholar]
- 14. Miller SM. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Implications for cancer screening and management. Cancer. 1995;76:167‐177. [DOI] [PubMed] [Google Scholar]
- 15. Finney Rutten LJ, Agunwamba AA, Wilson P, et al. Cancer‐related information seeking among cancer survivors: trends over a decade (2003‐2013). J Cancer Educ. 2016;31:348‐357. [DOI] [PubMed] [Google Scholar]
- 16. Fletcher C, Flight I, Chapman J, Fennell K, Wilson C. The information needs of adult cancer survivors across the cancer continuum: a scoping review. Patient Educ Couns. 2017;100:383‐410. [DOI] [PubMed] [Google Scholar]
- 17. Ankem K. Use of information sources by cancer patients: results of a systematic review of the research literature. Inform Res. 2006;11:254 http://www.informationr.net/ir/11-3/paper254.html [Google Scholar]
- 18. Hall LK, Kunz BF, Davis EV, Dawson RI, Powers RS. The cancer experience map: an approach to including the patient voice in supportive care solutions. J Med Internet Res. 2015;17:e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Laugesen J, Hassanein K, Yuan Y. The impact of internet health information on patient compliance: a research model and an empirical study. J Med Internet Res. 2015;17:e143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McMullan M. Patients using the Internet to obtain health information: how this affects the patient–health professional relationship. Patient Educ Couns. 2006;63:24‐28. [DOI] [PubMed] [Google Scholar]
- 21. Pearce A, Tomalin B, Kaambwa B, et al. Financial toxicity is more than costs of care: the relationship between employment and financial toxicity in long‐term cancer survivors. J Cancer Surviv. 2019;13:10‐20. [DOI] [PubMed] [Google Scholar]
- 22. van Mierlo T. The 1% rule in four digital health social networks: an observational study. J Med Internet Res. 2014;16:e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ziebland S, Wyke S. Health and illness in a connected world: how might sharing experiences on the internet affect people's health? Milbank Q. 2012;90:219‐249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Newhouse N, Lupianez‐Villanueva F, Codagnone C, Atherton H. Patient use of email for health care communication purposes across 14 European countries: an analysis of users according to demographic and health‐related factors. J Med Internet Res. 2015;17:e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jiang Y, West BT, Barton DL, Harris MR. Acceptance and use of eHealth/mHealth applications for self‐management among cancer survivors. Stud Health Technol Inform. 2017;245:131‐135. [PMC free article] [PubMed] [Google Scholar]
- 26. Powell KR. Patient‐perceived facilitators of and barriers to electronic portal use: a systematic review. Comput Inform Nurs. 2017;35:565‐573. https://www.ncbi.nlm.nih.gov/pubmed/28723832 [DOI] [PubMed] [Google Scholar]
- 27. Bass SB, Ruzek SB, Gordon TF, Fleisher L, McKeown‐Conn N, Moore D. Relationship of Internet health information use with patient behavior and self‐efficacy: experiences of newly diagnosed cancer patients who contact the National Cancer Institute's Cancer Information Service. J Health Commun. 2006;11:219‐236. [DOI] [PubMed] [Google Scholar]
- 28. Girault A, Ferrua M, Lalloue B, et al. Internet‐based technologies to improve cancer care coordination: current use and attitudes among cancer patients. Eur J Cancer. 2015;51:551‐557. [DOI] [PubMed] [Google Scholar]
- 29. Basch E, Deal AM, Kris MG, et al. Symptom monitoring with patient‐reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol. 2016;34:557‐565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Denis F, Lethrosne C, Pourel N, et al. Randomized trial comparing a web‐mediated follow‐up with routine surveillance in lung cancer patients. J Natl Cancer Inst. 2017;109(9). [DOI] [PubMed] [Google Scholar]
- 31. Netherlands Cancer Registry . Dutch cancer figures. Accessed May 13, 2019. https://www.cijfersoverkanker.nl/2018
- 32. Grando MA, Rozenblum R, Bates DW. Information Technology for Patient Empowerment in Healthcare. Walter de Gruyter GmbH; 2015. [Google Scholar]
- 33. de Rooij BH, Ezendam NPM, Vos MC, et al. Patients' information coping styles influence the benefit of a survivorship care plan in the ROGY Care Trial: new insights for tailored delivery. Cancer. 2019;125:788‐797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. de Rooij BH, Ezendam NPM, Mols F, et al. Cancer survivors not participating in observational patient‐reported outcome studies have a lower survival compared to participants: the population‐based PROFILES registry. Qual Life Res. 2018;27:3313‐3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


