Abstract
Background
Colorectal cancer screening uptake is low, particularly among individuals enrolled in Medicaid. To the authors' knowledge, little is known regarding the effectiveness of direct‐to‐member outreach by Medicaid health insurance plans to raise colorectal cancer screening use, nor how best to deliver such outreach.
Methods
BeneFIT is a hybrid implementation‐effectiveness study of 2 program models that health plans developed for a mailed fecal immunochemical test (FIT) intervention. The programs differed with regard to whether they used a centralized approach (Health Plan Washington) or collaborated with health centers (Health Plan Oregon). The primary implementation outcome of the current study was the percentage of eligible enrollees to whom the plans delivered each intervention component. The primary effectiveness outcome was the rate of FIT completion within 6 months of mailing of the introductory letter.
Results
The health plans identified 12,000 eligible enrollees (8551 in Health Plan Washington and 3449 in Health Plan Oregon). Health Plan Washington mailed an introductory letter and FIT kit to 8551 enrollees (100%) and delivered a reminder call to 839 (10.3% of the 8132 attempted). Health Plan Oregon mailed an introductory letter, and a letter and FIT kit plus a reminder postcard to 2812 enrollees (81.5%) and 2650 enrollees (76.8%), respectively. FIT completion rates were 18.2% (1557 of 8551 enrollees) in Health Plan Washington. In Health Plan Oregon, completion rates were 17.4% (488 of 2812 enrollees) among enrollees who were mailed an introductory letter and 18.3% (484 of 2650 enrollees) among enrollees who also were mailed a FIT kit plus reminder postcard.
Conclusions
The implementation of mailed FIT outreach by health plans may be effective and could reach many individuals at risk of developing colorectal cancer.
Keywords: colorectal cancer screening, direct mail, fecal immunochemical test, health plans, Medicaid
Short abstract
Colorectal cancer screening uptake is low, particularly among individuals enrolled in Medicaid. The implementation of mailed fecal immunochemical test outreach among health plans may be effective and could reach many individuals at risk of developing colorectal cancer.
Introduction
Directly mailing fecal immunochemical tests (FITs) to patients who are due for colorectal cancer (CRC) screening has been shown to improve CRC screening rates in several health care settings, with meta‐analyses demonstrating a 22% increase in FIT completion rates.1 Our previous research has demonstrated both the benefits of mailed FIT interventions and the implementation challenges faced by health centers when conducting such programs, including a high burden on staff, competing clinical demands, and a lack of continuity due to leadership and staff turnover.2 One possible solution to these challenges is for implementation to be spearheaded by health insurance plans rather than health centers or clinics.
Innovation in encouraging CRC screening could be particularly valuable for health plans that serve US Medicaid populations. In 2016, Medicaid provided health insurance to 82 million individuals, including 1.8 million in Washington state and 1 million in Oregon, some of whom also are covered through Medicare.3 Nationally, the Medicaid population includes approximately 1.8 million adults who are overdue for CRC screening.3 Medicaid can reduce financial barriers to screening, and several studies have reported higher screening uptake and more favorable CRC outcomes among Medicaid enrollees compared with uninsured individuals.4, 5 Nevertheless, compared with individuals with commercial insurance or Medicare, Medicaid enrollees are less likely to be screened for CRC.3 National data from 2015 demonstrated that only approximately 47% of Medicaid‐insured adults aged 50 to 64 years were up to date with CRC screening recommendations compared with at least 60% of privately or Medicare disability–insured adults.4 Medicaid enrollees have a >40% increased risk of mortality from CRC compared with commercially insured adults,6 and a 2‐fold higher risk of late‐stage CRC compared with non–Medicaid‐enrolled adults.7
Recently, Medicaid Managed Care plans and Medicare Advantage plans have started using direct‐to‐member outreach to promote the uptake of CRC screening and other preventive health screenings.8 This health plan–level outreach can offer many advantages over clinic‐level efforts. Burden on the clinics is minimized, cost‐sharing is facilitated between health plans and clinics, and efficiencies are created by standardizing processes across clinics.
To the best of our knowledge, few previous investigations have assessed the effectiveness of a health insurance plan–based mailed FIT outreach program, nor have any assessed how best to implement such a program. Brenner et al reported a FIT completion rate of 21% for a centralized FIT program that mailed to >1000 Medicaid enrollees in a large county health department.9 This study, however, was designed to determine efficacy under ideal circumstances (eg, programs designed and delivered by researchers rather than health plan staff). To our knowledge, little is known regarding the effectiveness of mailed FIT outreach interventions designed and initiated by health plans.
To address this literature gap, we conducted an observational study, the Pilot Program of Mailed Fecal Immunochemical Tests to Increase Colorectal Cancer Screening Rates: BeneFIT (herein referred to as BeneFIT), to evaluate the implementation and effectiveness of a mailed FIT outreach program initiated by health plans serving Medicaid Managed Care, Medicare Advantage, and dual Medicare‐Medicaid populations. The findings of the current study may aid health plan decision makers in developing mailed FIT outreach programs best suited for their unique populations and organizations.
Materials and Methods
Study Setting
BeneFIT was a study of 2 mailed FIT outreach programs initiated by 2 health plans operating in Washington State and Oregon. The Washington plan, which we will call Health Plan Washington, is a for‐profit organization that operates in multiple states and provides Medicaid and dual Medicaid‐Medicare coverage for approximately 650,000 members in the state of Washington. The Oregon plan, which we will call Health Plan Oregon, is a nonprofit organization that provides Medicaid and Medicare (with the majority of Medicare patients dually eligible for Medicaid) coverage for approximately 220,000 enrollees in Oregon. Our processes for health plan and health center recruitment have been described elsewhere.10 Health Plan Washington passively involved 504 health centers, allowing an opt‐out option. Health Plan Oregon involved 6 selected health centers that agreed to share patient FIT results with researchers. Both programs were offered in addition to any existing CRC screening efforts taking place in the health centers.
Member Selection
Medicaid and Medicare enrollees from both health plans were considered eligible for the mailed outreach program based on 2015 Healthcare Effectiveness Data and Information Set (HEDIS) criteria (based on claims data only): that is, they were aged 50 to 75 years with claims records demonstrating no evidence of having undergone a colonoscopy within the past 9 years, or a fecal test within the past 11 months (for Health Plan Oregon) or within that calendar year (for Health Plan Washington), and no sigmoidoscopy within the past 4 years. Each health plan excluded enrollees who had a prior history of CRC or total colectomy, or who currently had an invalid address. Lists of initially eligible enrollees were pulled in August 2016 for Health Plan Washington and between August and October 2016, depending on the health center, for Health Plan Oregon.
Health Plan Intervention Models
The research team met regularly with representatives from each health plan, supporting their development of an implementation model for a mailed FIT program. The mailed FIT programs were based in part on our STOP CRC study11 and the Washington plan's previous experience offering mailed FITs to Medicare enrollees. The intervention spanned 2 years; herein, we have reported on the first‐year mailings, which took place between August and November 2016.
Centralized model
Health Plan Washington used a “centralized” program model whose workflow involved minimal collaboration with health centers; the majority of activities were conducted by an outside vendor. Health plan staff generated a list of initially eligible enrollees and provided the list to an outside vendor, which mailed introductory letters (in English and Spanish) and, approximately 3 weeks later, FIT kits (2‐sample Insure; Clinical Genomics, Bridgewater, New Jersey) to enrollees on the list. All FITs were mailed on November 9, 2016. One to 2 months later, vendor outreach staff attempted to deliver live reminder telephone calls to 8132 enrollees (95%) who were mailed a FIT and had not yet returned it. Up to 6 attempts were made; calls were delivered in English. Completed kits were sent to a centralized laboratory for processing. Test results were sent to the health plan and to the enrollee's health care provider. Enrollees whose mailed FIT results were found to be positive were referred to a health plan care coordinator who telephoned enrollees and recommended they contact their primary care provider to discuss results (care coordinators could not inform enrollees of their results). Primary care providers were expected to follow their usual process of contacting their patients with positive FIT results and assisting them in getting a follow‐up colonoscopy.
Collaborative model
Health Plan Oregon used a “collaborative” model in which the health plan and participating health centers worked together to deliver mailed FIT outreach. Health plan staff generated and distributed lists of initially eligible enrollees to each health center, whose staff had the option to update the list by removing the names of anyone who was not a current patient or who, based on electronic health record data, was not a candidate for CRC screening (eg, recently had been screened). Three of the 6 health centers chose to review lists. Health plan staff provided the updated list and FIT kits selected by the health center (2‐sample Insure or 1‐sample OC‐Auto [PolyMedco, Cortland Manor, New York]) to a mail vendor, who mailed an introductory letter to enrollees on the list and a FIT kit approximately 3 to 4 weeks later, followed approximately 2 weeks later by a postcard reminder. Three health centers delivered additional telephone call reminders, and 2 other health centers offered patient incentives for returning the FIT kit. The program used bilingual (English and Spanish) materials containing the logos of both the health plan and the participating health center. Enrollees mailed or dropped off completed FITs to their assigned health center, where staff placed laboratory orders and processed kits according to their center's standard procedures (ie, external laboratory). FIT results were transferred to primary care providers through electronic laboratory interfaces, and health center staff communicated test results and assisted enrollees who screened positive in completing follow‐up colonoscopies, according to standard health center procedures.
Implementation Measures
Implementation was measured as the percentage of eligible enrollees to whom the health plans delivered each intervention component (mailed letter introducing the program, mailed FIT, reminders, and care coordination). For each health plan, we have reported the number of enrollees excluded at each step, and the reason for the exclusion.
Effectiveness Measures
Our primary effectiveness outcome was the FIT completion rate, and the secondary outcome was any CRC screening completion (including FIT, colonoscopy, and flexible sigmoidoscopy) within 6 months of mailing of the introductory letter, as reported in claims data. FIT‐DNA testing or computed tomography colonography were not included in the secondary outcome because they were not part of the 2015 HEDIS measure set. We assessed variability in FIT and any CRC screening completion by enrollees' demographic characteristics and health care use. We also reported FIT positivity rates and follow‐up colonoscopy completion among those with a positive FIT for all FIT‐screened enrollees in Health Plan Oregon (because FIT results were obtained from clinic records), and for the subset of enrollees whose FITs were mailed and tracked as returned by the vendor (857 of 1557 completed FIT claims; 55%) in Health Plan Washington. (Health Plan Washington FIT results were not obtained from clinic records).
Statistical Analysis
We obtained claims data from each health plan at least 12 months after the introductory letters were mailed (8551 enrollees for Health Plan Washington and 2812 enrollees for Health Plan Oregon) to allow time for claims to be submitted. We computed the FIT completion rates for each program step and, for Health Plan Oregon, we calculated FITs completed by the health center. For each health plan, among enrollees who were mailed an introductory letter, we also assessed associations between FIT completion and demographic and health care use variables using multivariable logistic regression. All analyses were performed using SAS statistical software (version 9.4 for Windows).
Results
Figure 1 outlines the intervention steps undertaken at each health plan. A total of 57.5% and 49.8%, respectively, of Health Plan Washington and Health Plan Oregon enrollees were female. Enrollees predominantly were aged 50 to 64 years, white or Caucasian, enrolled in Medicaid, lived in an urban zip code, and preferred speaking English. The percentage of enrollees with ≥4 primary care clinic visits within the year prior to the introductory letter was 39.1% in Health Plan Washington and 28.7% in Health Plan Oregon.
Figure 1.
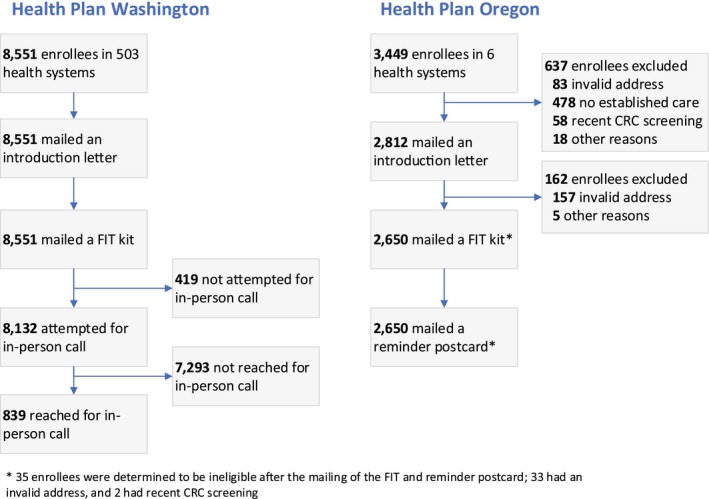
BeneFIT (Pilot Program of Mailed Fecal Immunochemical Tests to Increase Colorectal Cancer Screening Rates) program activities. CRC indicates colorectal cancer; FIT, fecal immunochemical test.
Implementation Outcomes
In Health Plan Washington, a total of 8551 enrollees were identified as being initially eligible with validated addresses (based on US Postal Service records) and all were mailed an introductory letter and FIT kit (Table 1). Live reminder telephone calls were attempted for 8132 Washington enrollees (95.1%); of these, 839 (10.3%) were successfully contacted (ie, a live telephone conversation occurred). Care coordination was attempted for all 125 individuals known to have a positive FIT result and was delivered to 78 (62.4%) within 1 month of the health plan being notified of the FIT result (data not shown).
Table 1.
Mailed FIT Outreach and Reminders Delivered by Health Plans
| Activities | Health Plan Washington: Centralized Model | Health Plan Oregon: Collaborative Model | ||||
|---|---|---|---|---|---|---|
| No. | Percentage (95% CI) Completed FIT | Percentage (95% CI) Completed Any CRC Screeninga | No. | Percentage (95% CI) Completed FITa | Percentage (95% CI) Completed Any CRC Screeninga | |
| Initially eligible | 8551a, b | 18.2 (17.4‐19.0)b | 21.6 (20.8‐22.5)b | 3449 | 14.6 (13.4‐15.8) | 16.8 (15.5‐18.0) |
| Mailed introductory letter | 2812 | 17.4 (16.0‐18.8) | 19.6 (18.1‐21.1) | |||
| Mailed FIT | 2650 | 18.3 (16.8‐19.7) | 20.6 (19.0‐22.2) | |||
| Sent reminder letter | NA | NA | NA | |||
| Attempted reminder telephone call | 8132 | 15.3 (14.5‐16.1) | 18.9 (18.0‐19.7) | NA | NA | NA |
| Answered in personb, c | 839 | 76.2 (73.3‐79.1) | 77.0 (74.0‐79.8) | |||
| Not answered | 7293 | 8.3 (7.7‐9.0) | 12.2 (11.4‐12.9) | |||
| No telephone call needed/madec, d | 419 | NA | NA | |||
Abbreviations: CRC, colorectal cancer; FIT, fecal immunochemical test; NA, not applicable.
Within 6 months after mailing of the introduction letter.
For Health Plan Washington, all initially eligible patients received both the introductory letter and the mailed FIT kit.
In‐person conversations only; no telephone messages were left.
No telephone call was made for 419 enrollees, 307 of whom completed their FIT within 1 month of the introduction letter mailing.
Of the 3449 Health Plan Oregon enrollees who initially were identified as eligible, 637 (18.5%) were excluded by health center staff before introductory letters were mailed. These included 478 enrollees who had not yet established care at that health center, 83 enrollees with an invalid address, 58 enrollees who were determined to be up to date on CRC screening, and 18 enrollees who were excluded for other reasons. The remaining 2812 enrollees (81.5%) were mailed an introductory letter. Of this group, an additional 162 enrollees (5.8%) subsequently were found to have an invalid address (157 enrollees) or to be otherwise ineligible (5 enrollees), and hence were not mailed a FIT kit. This left 2650 enrollees (94.2%) who were mailed a FIT plus reminder postcard.
Effectiveness Outcomes
Health Plan Washington's FIT completion rate was 18.2% (1557 enrollees); the rate of any CRC screening was 21.6% (1847 enrollees). Of the 1557 completed FIT claims, 55% (857 claims) were returned to the vendor and attributable to the mailed FIT program; the remaining 45% (700 claims) were attributable to FITs distributed in the clinics. Among the 8132 enrollees for whom a live telephone call was attempted, FIT completion rates were 15.3% (76.2% in the 839 enrollees who answered in person and 8.3% in the 7293 enrollees who did not answer).
Health Plan Oregon's FIT completion rates were 14.6% (503 of 3449 enrollees) among those initially identified as eligible, 17.4% (488 of 2812 enrollees) among those mailed an introductory letter, and 18.3% (484 of 2650 enrollees) among those mailed a FIT kit plus reminder postcard. Respective rates of completing any CRC screening were 16.8% (579 of 3449 enrollees), 19.6% (551 of 2812 enrollees), and 20.6% (545 of 2650 enrollees). FIT completion rates among those enrollees who were mailed an introductory letter ranged from 10.4% to 25.8% across health centers (data not shown).
FIT positivity rates were 14.6% in Health Plan Washington (in the subset of 857 kits returned to the vendor) and 8.3% in Health Plan Oregon (among all participating enrollees). Among enrollees with positive FIT results, approximately 32.8% in Health Plan Washington and 35.9% in Health Plan Oregon obtained a colonoscopy within 1 year.
Multivariate Analysis
In both health plans, we found higher FIT completion and any CRC screening completion among enrollees with a higher number of primary care visits, and lower completion among dual Medicare‐Medicaid–insured adults (vs those insured by Medicaid only) (Tables 2 and 3). Higher rates for FIT completion and any CRC screening completion were observed for Asian and Pacific Islanders in Health Plan Washington and enrollees shown as being of “other” or “multiple” race in Health Plan Oregon compared with white individuals. Rural enrollees in Health Plan Washington had lower odds of any CRC screening completion compared with urban enrollees.
Table 2.
CRC Screening Completion Rates of Enrollees Who Were Mailed an Introductory Letter In Health Plan Washington By Descriptive Characteristics (N = 8551)
| Characteristics | Health Plan Washington: Centralized Model | ||||
|---|---|---|---|---|---|
| Enrollees No. (%) | FIT Completiona | Any CRC Screening Completiona | |||
| Percentageb | Adjusted OR (95% CI)b | Percentageb | Adjusted OR (95% CI)c | ||
| Overall | 8551 | 18.2 | — | 21.6 | — |
| Sex | |||||
| Male | 3637 (42.5) | 17.3 | 1.0 | 20.7 | 1.0 |
| Female | 4914 (57.5) | 18.8 | 1.06 (0.95‐1.19) | 22.3 | 1.05 (0.95‐1.17) |
| Age, y | |||||
| 50‐64 | 7051 (82.5) | 18.6 | 1.0 | 22.3 | 1.0 |
| 65‐75 | 1500 (17.5) | 16.5 | 0.95 (0.76‐1.19) | 18.7 | 0.86 (0.69‐1.07) |
| Race/ethnicity | |||||
| White | 4797 (56.1) | 17.7 | 1.0 | 21.1 | 1.0 |
| Black/African American | 367 (4.3) | 17.7 | 0.99 (0.75‐1.32) | 22.6 | 1.09 (0.86‐1.39) |
| Asian/Pacific Islander/Native Hawaiian | 552 (6.5) | 27.7 | 1.78 (1.33‐2.77) | 33.3 | 1.87 (1.46‐2.41) |
| American Indian/Alaska Native | 47 (0.5) | 12.8 | 0.68 (0.31‐1.48) | 14.9 | 0.66 (0.32‐1.36) |
| Hispanic | 547 (6.4) | 15.5 | 0.85 (0.65‐1.12) | 18.8 | 0.87 (0.66‐1.15) |
| Missing data | 2241 (26.2) | 17.7 | 0.99 (0.84‐1.18) | 20.6 | 0.97 (0.82‐1.14) |
| Insurance type | |||||
| Medicaid | 6752 (79.0) | 18.8 | 1.0 | 22.4 | 1.0 |
| Medicare‐Special Needs (Medicare‐Medicaid) | 1799 (21.0) | 15.9 | 0.82 (0.67‐0.98) | 18.9 | 0.84 (0.70‐1.00) |
| Residence location | |||||
| Urban | 7452 (87.1) | 18.6 | 1.0 | 22.2 | 1.0 |
| Rural | 1099 (12.9) | 15.8 | 0.82 (0.65‐1.01) | 18.0 | 0.75 (0.61‐0.94) |
| Preferred language | |||||
| English | 7773 (90.9) | 18.1 | 1.0 | 21.5 | 1.0 |
| Non‐English | 754 (8.8) | 20.0 | 1.11 (0.88‐1.40) | 23.3 | 1.09 (0.88‐1.35) |
| Missing data | 24 (0.3) | 12.5 | 0.72 (0.20‐2.57) | 20.8 | 1.09 (0.57‐2.09) |
| Primary care visits within past y | |||||
| 0 | 1625 (19.0) | 10.9 | 1.0 | 12.7 | 1.0 |
| 1‐3 | 3584 (41.9) | 20.0 | 2.01 (1.35‐3.00) | 23.4 | 2.05 (1.37‐3.09) |
| ≥4 | 3342 (39.1) | 19.8 | 2.01 (1.33‐3.03) | 24.0 | 2.14 (1.42‐3.24) |
Abbreviations: CRC, colorectal cancer; FIT, fecal immunochemical test; OR, odds ratio.
Within 6 months of the introduction letter mailing date.
Values shown as row percentages.
ORs were based on logistic regression clustered on health center (n = 504) and adjusted for all other variables in the table.
Table 3.
CRC Screening Completion Rates of Enrollees Mailed an Introductory Letter in Health Plan Oregon By Descriptive Characteristics (N = 2812)
| Characteristicsa | Health Plan Oregon: Collaborative Model | ||||
|---|---|---|---|---|---|
| Enrollees | FIT Completionb | Any CRC Screening Completionb | |||
| Percentagec | Adjusted OR (95% CI)c | Percentagec | Adjusted OR (95% CI)d | ||
| Overall | 2812 | 17.4 | — | 19.6 | — |
| Sexe | |||||
| Male | 1373 (50.2) | 15.7 | 1.0 | 17.7 | 1.0 |
| Female | 1438 (49.8) | 19.0 | 1.09 (0.94‐1.26) | 21.4 | 1.09 (0.89‐1.33) |
| Age, ye | |||||
| 50‐64 | 2490 (89.2) | 17.2 | 1.0 | 19.5 | 1.0 |
| 65‐75 | 321 (10.8) | 18.7 | 1.42 (0.93‐2.19) | 20.6 | 1.35 (0.94‐1.93) |
| Race/ethnicity | |||||
| White | 1947 (69.0) | 17.3 | 1.0 | 19.6 | 1.0 |
| Black/African American | 76 (2.7) | 14.5 | 0.98 (0.38‐2.52) | 17.1 | 1.02 (0.45‐2.31) |
| Asian/Pacific Islander/Native Hawaiian | 127 (3.9) | 18.1 | 1.42 (0.66‐3.06) | 20.5 | 1.40 (0.78‐2.50) |
| American Indian/Alaska Native | 29 (0.1) | 17.2 | 0.99 (0.39‐2.52) | 17.2 | 0.83 (0.32‐2.15) |
| Hispanic | 212 (7.2) | 17.5 | 1.17 (0.93‐1.46) | 18.4 | 1.04 (0.86‐1.26) |
| Other/multiple race | 51 (2.3) | 23.5 | 1.69 (1.04‐2.75) | 25.5 | 1.62 (1.06‐2.48) |
| Missing data | 370 (14.1) | 17.3 | 0.98 (0.69‐1.39) | 19.7 | 1.02 (0.71‐1.47) |
| Insurance typee | |||||
| Medicaid | 2325 (84.0) | 17.5 | 1.0 | 19.8 | 1.0 |
| Medicare‐Special Needs (Medicare‐Medicaid) | 367 (12.1) | 13.4 | 0.56 (0.42‐0.76) | 15.3 | 0.58 (0.41‐0.82) |
| Medicare Advantage | 120 (3.9) | 26.7 | 1.34 (0.93‐1.93) | 29.2 | 1.34 (0.88‐2.04) |
| Preferred language | |||||
| English | 2249 (80.5) | 18.1 | 1.0 | 20.5 | 1.0 |
| Non‐English | 195 (6.4) | 14.4 | 0.74 (0.49‐1.13) | 16.4 | 0.80 (0.55‐1.15) |
| Missing data | 368 (13.1) | 14.4 | 0.71 (0.50‐1.03) | 15.5 | 0.66 (0.46‐0.94) |
| Primary care visits within past y | |||||
| 0 | 994 (40.8) | 7.7 | 1.0 | 8.9 | 1.0 |
| 1‐3 | 918 (30.6) | 20.8 | 3.07 (1.94‐4.84) | 23.4 | 3.09 (1.97‐4.84) |
| ≥4 | 900 (28.7) | 24.4 | 3.77 (2.38‐5.97) | 27.6 | 3.84 (2.41‐6.12) |
Abbreviations: CRC, colorectal cancer; FIT, fecal immunochemical test; OR, odds ratio.
Urban versus rural residence was excluded because of low cell sizes.
Within 6 months of the introduction letter mailing date.
Values shown as row percentages.
ORs were based on logistic regression clustered on health center (n = 6) and adjusted for all other variables in the table.
Value was missing for 1 participant: Medicare‐Special Needs participants were dually enrolled in Medicaid and Medicare.
Discussion
We found similar FIT completion rates across 2 health plan–initiated mailed FIT outreach programs for Medicaid‐insured and Medicare‐insured adults, despite differences in program design and the degree of collaboration with participating health centers. The nonrandomized design of the current study did not allow us to rule out possible confounders that could have influenced the success of these 2 programs, or to compare FIT completion rates among enrollees who did and did not take part in the program.
The 2 health plans in the current study used distinct models for delivering mailed FIT programs, with patient populations that were similar with regard to age, sex, insurance status, and race/ethnicity. The FIT return rates achieved in the current study were similar to those achieved in some clinic‐based studies of mailed FIT outreach,1 suggesting that health plan–based, mailed FIT programs can be as effective as programs initiated by individual clinics or health centers. The current study findings also are approximately consistent with those of a previous investigation of a CRC screening intervention by Medicaid health plans, in which Brenner et al reported a return rate of 21% for a centralized FIT program for Medicaid enrollees that first removed those enrollees who had an invalid address (19%) or self‐reported recent screening (11%).9 The findings of the current study demonstrated completion rates to be particularly high in Health Plan Washington among enrollees who were due for and answered the live reminder telephone call (76.2%); these findings were consistent with previous research indicating that tailored telephone outreach can significantly increase rates of CRC screening.12, 13 Together, these findings suggest that further optimization of a health plan–based mailed FIT program might be achieved by varying the number, types, and reach of the reminders delivered.
Although the additional effort (eg, reviewing enrollee lists) required by health centers in the Health Plan Oregon model did not appear to increase FIT completion rates in comparison with the approach used in Washington, they may have provided some incidental benefits. First, health centers were given an opportunity to update their patient records with claims data and, if desired, outreach to adults who had not yet established care. Furthermore, completed FITs were processed and resulted according to each clinic's standard and FIT results automatically populated the electronic health record and were available immediately for clinical use. Moreover, clinics could easily follow their usual‐care process of providing follow‐up care to patients whose test results were positive.
The centralized model implemented by Health Plan Washington had different potential advantages: the design facilitated the delivery of multiple reminders to enrollees as needed, and nearly 75% of those who received reminder telephone calls returned their kits. However, the vendor achieved a relatively low telephone call reminder completion rate (10.3%) despite making up to 6 call attempts. Moreover, the centralized approach may involve less work for the health plan and health centers.
The data from the current study identified key challenges to program implementation, including patients' lack of engagement with health centers; invalid addresses; and, in Health Plan Washington, low reach of reminder telephone calls. These challenges reflect the realities of outreach to a population that is known to change health plans, move locations, and be hard to find for follow‐up.14 Nevertheless, the current study data from Health Plan Oregon have suggested lower than expected numbers of invalid addresses; only 83 of 3449 addresses (2.4%) initially were determined to be invalid based on US Postal Service records and an additional 157 of 2812 addresses (5.6%) were removed after the introductory letter was mailed. In contrast, Brenner et al reported a 19% rate of invalid addresses among Medicaid enrollees in North Carolina.9 More research is needed to understand and address these and other implementation challenges.
The current study data concerning follow‐up colonoscopy completion rates (33% to 36%) indicated room for improvement in both health plans. Low participation in follow‐up colonoscopy is a recognized limitation of FIT‐based programs, and the rates observed herein were even lower than the 52% to 53% found in previous research involving health centers serving the Medicaid population.15, 16 In Health Plan Washington, this finding may have been attributable to low reach (60.0%) of the care coordinator telephone calls and/or the care coordinators' inability to directly inform patients of their test results. Other factors, such as unestablished care, low understanding of the need for a follow‐up colonoscopy, or other reported obstacles to colonoscopy (eg, bowel preparation, the need to take time away from work, procedure costs) may contribute further.17, 18 In contrast, Brenner et al reported a 66% rate of follow‐up colonoscopy when the health plan care coordinator was able to view enrollees' medical records and directly discuss FIT results with the enrollees.9 These and other innovations to increase follow‐up colonoscopy rates are critical to the success of mailed FIT interventions.
The observation in the current study that FIT positivity rates were 14.6% in Health Plan Washington and 8.3% in Health Plan Oregon is consistent with previous research by our team demonstrating positivity rates of 12% to 23% in health centers using the InSure FIT kit and 7% to 10% in health centers using the OC‐Auto FIT kit (the test most commonly used by health centers in Health Plan Oregon).19 Although data from a recent meta‐analysis demonstrated similar FIT performance characteristics regardless of the number of FIT samples tested,20 patient adherence is reported to be higher with a 1‐sample versus a 2‐sample test.21 Thus, further improvements in FIT completion may be achieved by optimizing the selection of FIT tests.
Among the limitations of the current study was the nonrandomized design and possible nonrepresentativeness of the 6 larger health centers in Health Plan Oregon that participated in the research portion of the program (eg, providing qualitative interviews and results of completed FITs). Moreover, we did not attempt to isolate the effects of various health center activities in Health Plan Oregon (eg, reviewing eligible patient lists, delivering telephone reminders, offering incentives for the return of FIT kits, or using a 1‐sample compared with a 2‐sample FIT). However, when compared with other published data regarding mailed FIT programs, the results of the current observational study provide evidence of the feasibility and effectiveness of programs implemented directly by health plans.
Conclusions
The results of the current observational study demonstrated FIT completion rates of approximately 18% for 2 health plan–initiated, mailed FIT intervention programs for Medicaid and Medicare enrollees. Although many challenges are inherent to implementing such a program at any level, there is early evidence that implementation at the health plan level may be effective and potentially could reach many individuals at risk of developing CRC.
Funding Support
This publication is a product of a Health Promotion and Disease Prevention Research Center grant supported by cooperative agreement U48DP005013 from the Centers for Disease Control and Prevention. The findings and conclusions in this publication do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of Interest Disclosures
Gloria D. Coronado received a grant from the Centers for Disease Control and Prevention for work performed as part of the current study and a grant from Quidel Corporation awarded to Kaiser Permanente Northwest for work performed outside of the current study from September 2017 to June 2018, for which she served as the Principal Investigator to compare the clinical performance of an experimental fecal immunochemical test with that of a fecal immunochemical test approved by the US Food and Drug Administration. Beverly B. Green was supported by a grant from the Centers for Disease Control and Prevention awarded to Kaiser Permanente Washington for work performed as part of the current study. Imara I. West received a grant from the Centers for Disease Control and Prevention for worked performed as part of the current study. Malaika R. Schwartz received a grant from the Centers for Disease Control and Prevention for work performed as part of the current study. Jennifer K. Coury received a grant from the Centers for Disease Control and Prevention awarded to the University of Washington and paid to CareOregon for implementation of a mailed FIT program in a Medicaid plan. William M. Vollmer received a grant from the Centers for Disease Control and Prevention for work performed as part of the current study. Amanda F. Petrik received a grant from the Centers for Disease Control and Prevention for work performed as part of the current study. Laura‐Mae Baldwin received a grant from the Centers for Disease Control and Prevention for work performed as part of the current study. Jean A. Shapiro made no disclosures.
Author Contributions
Gloria D. Coronado: Conceptualization, funding acquisition, and writing–original draft. Beverly B. Green: Conceptualization, funding acquisition, and writing–review and editing. Imara I. West: Data curation, formal analysis, and writing–review and editing. Malaika R. Schwartz: Project administration and writing–review and editing. Jennifer K. Coury: Data curation, project administration, and writing–review and editing. William M. Vollmer: Methodology and writing–review and editing. Jean A. Shapiro: Writing–review and editing. Amanda F. Petrik: Project administration and writing–review and editing. Laura‐Mae Baldwin: Conceptualization, funding acquisition, and writing–review and editing.
We thank the Molina and CareOregon health insurance plans for their leadership and conduct of their mailed fecal immunochemical test programs, as well as for their participation in this research. We also thank Dr. Richard Meenan and Ms. Jennifer Schneider, who contributed to this work, although they are not named as authors.
References
- 1. Dougherty MK, Brenner AT, Crockett SD, et al. Evaluation of interventions intended to increase colorectal cancer screening rates in the United States: a systematic review and meta‐analysis. JAMA Intern Med. 2018;178:1645‐1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Coronado GD, Schneider JL, Petrik A, Rivelli J, Taplin S, Green BB. Implementation successes and challenges in participating in a pragmatic study to improve colon cancer screening: perspectives of health center leaders. Transl Behav Med. 2017;7:557‐566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Medicaid and CHIP Payment and Access Commission . MACStats: Medicaid and CHIP Data Book. Published 2017. Accessed October 11, 2018. https://www.macpac.gov/wp-content/uploads/2015/12/MACStats-Medicaid-CHIP-Data-Book-December-2017.pdf
- 4. de Moor JS, Cohen RA, Shapiro JA, et al. Colorectal cancer screening in the United States: trends from 2008 to 2015 and variation by health insurance coverage. Prev Med. 2018;112:199‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kaiser Family Foundation . Coverage of preventive services for adults in Medicaid. Published 2014. Accessed March 15, 2019. https://www.kff.org/report-section/coverage-of-preventive-services-for-adults-in-medicaid-survey-findings/
- 6. Fitzgerald T, Lea C, Atluri P, Brinkley J, Zervos E. Insurance payer status and race explains much of the variability in colorectal cancer survival. J Cancer Ther. 2014;5:1223‐1233. [Google Scholar]
- 7. Andrew AS, Parker S, Anderson JC, et al. Risk factors for diagnosis of colorectal cancer at a late stage: a population‐based study. J Gen Intern Med. 2018;33:2100‐2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Slater JS, Parks MJ, Nelson CL, Hughes KD. The efficacy of direct mail, patient navigation, and incentives for increasing mammography and colonoscopy in the Medicaid population: a randomized controlled trial. Cancer Epidemiol Biomarkers Prev. 2018;27:1047‐1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brenner AT, Rhode J, Yang JY, et al. Comparative effectiveness of mailed reminders with and without fecal immunochemical tests for Medicaid beneficiaries at a large county health department: a randomized controlled trial. Cancer. 2018;124:3346‐3354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Coury JK, Schneider JL, Green BB, et al. Two Medicaid health plans' models and motivations for improving colorectal cancer screening rates. Transl Behav Med. Published online November 16, 2018. doi: 10.1093/tbm/iby094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Coronado GD, Vollmer WM, Petrik A, et al. Strategies and opportunities to STOP colon cancer in priority populations: pragmatic pilot study design and outcomes. BMC Cancer. 2014;14:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dietrich AJ, Tobin JN, Robinson CM, et al. Telephone outreach to increase colon cancer screening in Medicaid managed care organizations: a randomized controlled trial. Ann Fam Med. 2013;11:335‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Coronado GD, Rivelli JS, Fuoco MJ, et al. Effect of reminding patients to complete fecal immunochemical testing: a comparative effectiveness study of automated and live approaches. J Gen Intern Med. 2018;33:72‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wilensky S. Colorectal Cancer Initiatives in Medicaid Agencies–A National Review. American Cancer Society; 2016. [Google Scholar]
- 15. Liss DT, Brown T, Lee JY, et al. Diagnostic colonoscopy following a positive fecal occult blood test in community health center patients. Cancer Causes Control. 2016;27:881‐887. [DOI] [PubMed] [Google Scholar]
- 16. Coronado GD, Petrik AF, Vollmer WM, et al. Effectiveness of a mailed colorectal cancer screening outreach program in community health clinics: the STOP CRC Cluster Randomized Clinical Trial. JAMA Intern Med. 2018;178:1174‐1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Martin J, Halm EA, Tiro JA, et al. Reasons for lack of diagnostic colonoscopy after positive result on fecal immunochemical test in a safety‐net health system. Am J Med. 2017;130:93.e1‐93.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Issaka RB, Singh MH, Oshima SM, et al. Inadequate utilization of diagnostic colonoscopy following abnormal FIT results in an integrated safety‐net system. Am J Gastroenterol. 2017;112:375‐382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nielson CM, Petrik AF, Jacob L, et al. Positive predictive values of fecal immunochemical tests used in the STOP CRC pragmatic trial. Cancer Med. 2018;7:4781‐4790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Robertson DJ, Lee JK, Boland CR, et al. Recommendations on fecal immunochemical testing to screen for colorectal neoplasia: a consensus statement by the US Multi‐Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2017;85:2‐21.e3. [DOI] [PubMed] [Google Scholar]
- 21. Chubak J, Bogart A, Fuller S, Laing SS, Green BB. Uptake and positive predictive value of fecal occult blood tests: a randomized controlled trial. Prev Med. 2013;57:671‐678. [DOI] [PMC free article] [PubMed] [Google Scholar]


