Randomized control trials in those with impaired glucose tolerance have shown that the onset of Type 2 diabetes can be prevented or delayed through behavioural interventions that promote weight loss, increase physical activity, and improve the quality of nutrition. 1 2
In 2016, the Healthier You: NHS Diabetes Prevention Programme was established to prevent or delay the onset of Type 2 diabetes in adults in England already identified to be at high risk, defined as having non‐diabetic hyperglycaemia [HbA1c 42–47 mmol/mol (6.0–6.4%) or fasting plasma glucose 5.5–6.9 mmol/l]. The Healthier You: NHS Diabetes Prevention Programme delivers behavioural interventions that encourage weight loss for people who are overweight, increased physical activity and a healthier diet through at least 13 face‐to‐face group‐based sessions, over at least 9 months. In July 2018, England became the first country in the world to achieve full national coverage with a Type 2 diabetes prevention programme. As of the end of April 2019, 400 237 people had been referred into the programme.
Our early analyses of referral, uptake and participant characteristics showed that of individuals referred between June 2016 and January 2017 (n = 43 603), 49% attended the initial assessment by April 2017; and that while initial attendance was equitable according to deprivation status and was significantly higher for Asian, Afro‐Caribbean, mixed and other ethnic groups compared with white European ethnic groups, uptake was significantly lower for those of working age. 3
To address inequalities of access according to age, NHS England initiated an uncontrolled pilot of a digital diabetes prevention programme to determine its feasibility, acceptability and impact. While digital options have the potential to offer a flexible alternative, thus widening access and increasing overall uptake, there has been limited evidence of the clinical effectiveness of such approaches and the extent to which they deliver on this potential. 4
Eligibility for the digital service was the same as for the face‐to‐face Healthier You: NHS Diabetes Prevention Programme. Referral pathways were also the same, except for two pilot areas where participants who had already declined the service offer from face‐to‐face providers were identified and offered referral to the digital programme (n = 434).
The digital pilot protocol has already been published 5 and a full process and impact evaluation report will follow in 2020. We aimed to assess programme uptake according to age, comparing that of the digital programme with that of the face‐to‐face programme, in order to inform timely and appropriate evolution of programme approaches to Type 2 diabetes prevention.
Between December 2017 and November 2018, 5337 people with non‐diabetic hyperglycaemia were referred into the digital programme. Of those, 3612 registered and accessed the digital intervention, an uptake of 68%, significantly higher than the 49% conversion of referral to initial assessment observed in the face‐to‐face Healthier You: NHS Diabetes Prevention Programme (z = 25.2, P < 0.001). The mean age (and standard deviation) of digital participants was 58 (12.4) years, significantly lower than the mean age of face‐to‐face participants, 64 (12.4) years (t = 28.7, P < 0.001), with clear differences in the age distribution of participants (Fig. 1). Over two‐thirds (68%) of digital registrations were for participants aged less than 65 years compared with 45% of attendees at initial assessment for the face‐to‐face interventions (z = 24.2, P < 0.001), while 16% of digital registrations were aged between 18–44 years compared with 7% of attendees at initial assessment for the face‐to‐face interventions (z = 16.8, P < 0.001).
Figure 1.
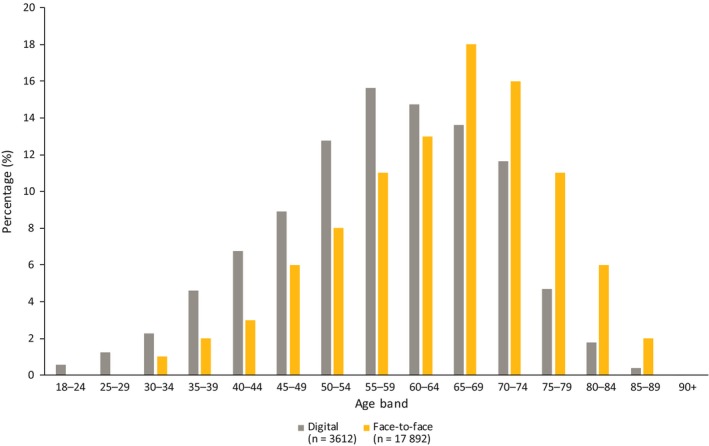
Comparison of digital referrals and registrations between December 2017 and November 2018 with referrals to face‐to‐face service between June 2016 and January 2017 who attended the initial assessment by April 2017.
This is a large‐scale real‐world evaluation of digital services that aims to prevent or delay the onset of Type 2 diabetes implemented in different localities, and the lessons learnt will be of international interest. The emerging findings from this study suggest that a digital diabetes prevention programme has the potential to reach working‐age people who are less likely to engage with group‐based face‐to‐face interventions. A digital diabetes prevention programme could be a useful component of a population‐based approach to addressing Type 2 diabetes prevention.
We await assessment of clinical effectiveness compared with face‐to‐face interventions in terms of weight change, HbA1c change, and impacts upon Type 2 diabetes incidence. However, these initial findings have helped inform a decision to include digital modes of delivery to those individuals who decline or fail to attend the face‐to‐face service within the Healthier You: NHS Diabetes Prevention Programme from summer 2019.
Funding sources
The pilots and evaluation have been funded by NHS England.
Competing interests
EM receives consultancy fees for her work on the evaluation. EM is Managing Director of a not‐for‐profit community interest company, HeLP‐Digital, which exists to disseminate a digital diabetes self‐management programme, HeLP‐Diabetes, across the NHS. LB is an Associate Director at RSM. RSM hold the contract from NHS England to implement and evaluate the Digital Diabetes Prevention Programme. JV is the National Clinical Director for Diabetes and Obesity at NHS England and is the Clinical Lead for the Healthier You: NHS Diabetes Prevention Programme.
Acknowledgements
We thank all service users for participating in this evaluation and the following Clinical Commissioning Groups (CCGs) and their primary care practices for supporting the identification and referral of participants: Bristol, North Somerset, South Gloucestershire CCG, Buckinghamshire CCG, Central West London, Hounslow, Hammersmith and Ealing CCG, Humber Coast and Vale CCG, Lancashire CCG, Luton CCG, North East London CCG Salford CCG, Somerset CCG.
Diabet. Med. 36: 1510–1511(2019)
References
- 1. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne‐Parikka P et al Finnish Diabetes Prevention Study Group. Prevention of Type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343–1350. [DOI] [PubMed] [Google Scholar]
- 2. Diabetes Prevention Program Research Group . Reduction in the incidence of Type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barron E, Clark R, Hewings R, Smith J, Valabhji J. Progress of the Healthier You: NHS Diabetes Prevention Programme: referrals, uptake and participant characteristics. Diabet Med 2017; 35: 513–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Joiner KL, Nam S, Whittemore R. Lifestyle interventions based on the diabetes prevention program delivered via eHealth: a systematic review and meta‐analysis. Prev Med 2017; 100: 194–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Murray E, Daff K, Lavida A, Henley W, Irwin J, Valabhji J. Evaluation of the digital diabetes prevention programme pilot: uncontrolled mixed‐methods study protocol. BMJ Open 2019; 9: e025903. [DOI] [PMC free article] [PubMed] [Google Scholar]


