Abstract
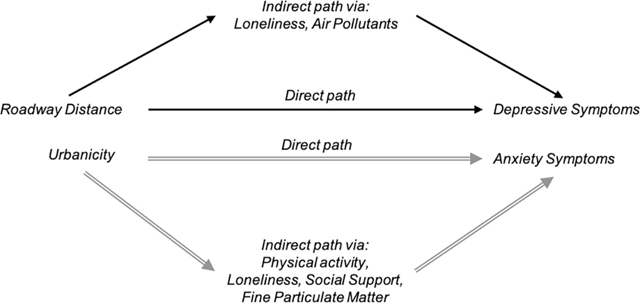
Evidence for the association between built environment and mental ill health, especially in older population where mental ill health is common, remains inconclusive. We examined the association of roadway distance and urbanicity, measured as percentage of urban land use within 1 km from participants’ residence, with mental ill-health in a longitudinal study of community-dwelling older adults in the United States between 2005 and 2006 and 2011–2012. We evaluated perceived stress, depression and anxiety symptoms using the Cohen’s Perceived Stress Scale, the Center for Epidemiological Studies – Depression, and the Hospital Anxiety and Depression Scale – anxiety subscale, respectively. Increment in roadway distance was significantly associated with −0.03 point (95% CI: −0.05, −0.01) change in depressive score, with loneliness and PM2.5 partially mediating the observed associations. Age, gender, race/ethnicity, and physical activity significantly modified the distance-depression association. Anxiety was inversely associated with roadway distance (−0.02; 95% CI: −0.03,0.00), though the associations became insignificant upon adjusting for road traffic or noise. Urbanicity was significantly associated with 0.29 (95% CI: 0.10,0.57) point increase in depressive symptoms in multivariable model; the association was partly mediated by loneliness, physical activity, social support and air pollution. No association was found between roadway distance and perceived stress, and between urbanicity, and anxiety and perceived stress. Built environment was associated with mental ill health, partially through pathways related to air pollution and certain individual characteristics (e.g. loneliness). Our study warrants further examination of the mediation and interaction of the built environment-mental health association.
Keywords: Roadway distance, Urbanicity, Depression, Anxiety, Perceived stress, Older adults
Graphical Abstract
1. Introduction
The concept that neighborhood features may be related to psychological well-being and mental health is not new. As early as 1939, Faris and Dunham found that neighborhood disadvantage was associated with higher rates of depression and substance abuse disorder (Mair et al., 2008); and research since then have showed mental health links with social and economic environment (Clark et al., 2007; Mair et al., 2008). It was only recently that built environment was implicated in the pathogenesis of mental disorders, potentially through its impacts on social connectiveness, access to green space, exposure to noise, traffic or air pollution, and change in individual behaviors (e.g., physical activity). For example, urbanicity, a built environment measure of land use type or diversity, has been shown to influence the ease with which people can stroll, walk, cycle or otherwise be physically active in the neighborhoods, and through this, has been associated with mental health (Miles et al., 2012; Sharma et al., 2006). However, evidence of urbanicity-mental health association remains inconsistent, with some suggesting positive association with schizophrenia (Krabbendam and van Os, 2005), mood and anxiety disorders (Peen et al., 2010) and depression (Saarloos et al., 2011), and others finding no association (Miles et al., 2012). Residential proximity to roadway was associated with phobic anxiety in a cohort of United States (U.S.) nurses (Power et al., 2015); this is contrary to other epidemiological studies (Volk et al., 2011; Wang et al., 2014), but is supported by our recent findings associating fine particulate (PM2.5) with both mood disorders and cognitive function, suggesting a potential pathway through which roadway distance may harm mental health (Pun et al., 2016; Tallon et al., 2017).
Despite the growing research, there remains paucity of evidence on the association of built environment with mental health, especially in older population where mental ill health is common. In this longitudinal study, we examined the association of roadway distance and urbanicity with mental health measures in a cohort of older Americans from the National Social Life, Health and Aging Project (NSHAP), and explored whether these associations are modified or mediated by lifestyle, behavior, health or neighborhood characteristics.
2. Methods
2.1. Study population
NSHAP is a longitudinal, nationally representative study of community-dwelling older individuals (57–85 years), with no known cognitive impairment, living across the U.S. (Shega et al., 2014). Wave 1 recruited 3005 participants between 2005 and 2006, and Wave 2 included 3377 participants in 2011–2012, with 2261 individuals participating in both waves. The survey over-sampled African-Americans, Latinos, men and individuals between 75 and 84 years. The overall weighted response rate was 75.5% and 76.9% for Waves 1 and 2, respectively (Smith et al., 2009). Demographic, social, psychological, and physiological health measures were collected.
2.2. Mental health measures
Depressive and anxiety symptomatology, and self-perceived stress during the previous week were assessed using the 11-item Center for Epidemiological Studies – Depression (CESD-11) Scale, 7-item Hospital Anxiety and Depression Scale — anxiety subscale (HADS-A), and a modified Cohen’s Perceived Stress Scale (PSS-4), respectively (Kohout et al., 1993; Mykletun et al., 2001; Shiovitz-Ezra et al., 2009). Participants were asked to indicate their response to each item by rating the frequency of their feelings in a 4-point Likert scale. The higher the summed scores, more severe depressive or anxiety symptoms, or a higher perceived stress. Detailed description of the questionnaires is documented elsewhere (Pun et al., 2016). Four (<1%), 744 (12%) and 756 (12%) participants did not complete the depression, anxiety or perceived stress assessments, respectively, with missingness not related to the built environment measures but to the mode of questionnaire administration. All missing data was imputed by maximum likelihood estimation (Messer and Natarajan, 2008).
2.3. Built environment measures
The built environment of NSHAP participants was characterized using residential distance from major roadways, accounting for any residential moves between waves. The ESRI StreetMap Pro 2007 road network data in GIS (ArcGIS, version 9.2; ESRI, Redlands, CA) was used to determine the distances from each geocoded residential address to the closest U.S. Census Feature Class Code A1 (primary highway with limited access), A2 (major, non-interstate highway), and A3 (secondary roads) road segments (Yanosky et al., 2014). Distance to the nearest A1–A3 road types was calculated in meters. Urbanicity was calculated as the percentage of low- and high-intensity residential, and industrial/commercial/transportation land use within 1 km of each residence using data from the U.S. Geological Survey 1992 National Land Cover Dataset (Yanosky et al., 2014). Three Wave 2 participants did not live in the continental U.S. and were excluded from the analyses.
2.4. Covariates
Loneliness was assessed using a revised 9-point University of California, Los Angeles (UCLA) Loneliness Scale (Russell et al., 1980). Social support was determined by participants’ frequency of socializing with friends or relatives in the past year, and physical activity by the frequency of rigorous physical activity (e.g., walking, exercise). Physical function was defined as self-rated difficulty in performing daily living activities (e.g., toileting). Chronic disease conditions (i.e., diabetes, hypertension, stroke, heart failure or respiratory illnesses) were measured by asking “Has a medical doctor told you have (had) [condition]?” Temperature and PM2.5 concentrations were calculated from a set of spatio-temporal generalized additive mixed models (Yanosky et al., 2014), whereas NO2 concentrations were measured at the nearest U.S. Environmental Protection Agency ambient monitors within 90 km from the residential address. Three-day moving average exposures were calculated for temperature, while 60-day moving averages were computed for PM2.5 and NO2 exposures, with exposure windows selected based on findings from previous studies (Pun et al., 2016; Welty and Zeger, 2005).
2.5. Statistical analysis
We used linear mixed models to examine the association of built environment with mental health scores, accounting for repeated measurements of participants and households. Base models adjusted for age, gender, race, study year, season and day of week of questionnaire completion, region and whether participants lived within a metropolitan statistical area. Multivariable models further controlled for individual (i.e., education attainment, family income) and census-tract (i.e., median household income level) socioeconomic status (SES). These covariates were selected a priori based on their significance in previous studies of the NSHAP cohort (Pun et al., 2018,2017). We fit additional models to assess potential confounding from individual-specific (i.e., current smoking, physical activity, social support, history of chronic conditions, body mass index and physical function), neighborhood characteristics, air pollution and meteorological factors. Note that in these models, we did not include covariates that were found to be statistically significant mediators.
We assessed mediation of the significant associations from the primary multivariable model by physical activity, loneliness, social support, temperature, PM2.5 and NO2, factors that were shown to be important mediators in prior literature of built environment and mental health (e.g., Maas et al., 2009; Pun et al., 2018; van den Berg et al., 2016). We computed indirect effects as the product of two regression coefficients: (coefficient of exposure with mediator as the dependent variable) × (coefficient of mediator with mental health score as the dependent variable and exposure as another predictor) in multivariable models. Percent of the total effect mediated was calculated, and significance of the mediating effect was assessed using Sobel test (Bauer et al., 2006). Furthermore, we examined effect modification by participants’ individual and neighborhood characteristics using interaction terms.
In sensitivity analyses, we restricted analyses to participants without antidepressant medication, and to Wave 2 participants to evaluate potential confounding by other built environment measures (i.e., traffic, noise) that were only available in Wave 2. We also re-assessed the associations using the categorical built environment measures. All results are expressed as the mean difference in mental health scores per 50 m increase in roadway distance or interquartile-range (IQR) increment of 57.8% in urbanicity, unless otherwise specified. All analyses were performed in SAS 9.4 (Cary, NC).
3. Results
A total of 4118 NSHAP participants, on average 70 years old and predominately white were included in the final analysis. More participants living within 49 m from the nearest roadway were Black, current smokers, less educated or socialized, or had less family income than those living at least 200 m away from the roadway (Table 1). Likewise, more participants living in the most urbanized neighborhood were Black, less physically or socially active, less educated, felt lonely most of the time, or had less family income than those living in the least urbanized neighborhood. Roadway distance moderately and negatively correlates with urbanicity was moderate (r = −0.45, Table S1).
Table 1.
Characteristics of NSHAP study participants by the highest and lowest categories of roadway distance and urbanicity measures, respectively.a
| Characteristic | Proximity to roadway |
Urbanicity |
||||
|---|---|---|---|---|---|---|
| 0–49 m | ≥200 m | p-Value | 1st tertile (least urban) | 3rd tertile (most urban) | p-Value | |
| No. of participants | 1026 | 3724 | 2201 | 2227 | ||
| Age (year, mean ± SD) | 71.0 ± 7.8 | 70.7 ± 8.2 | 70.1 ± 8.0 | 71.1 ± 8.2 | ||
| Male (%) | 47.2 | 48.1 | 0.0198 | 48.8 | 46.2 | 0.0697 |
| Race (%) | ||||||
| White | 69.1 | 73.4 | <0.0001 | 83.0 | 55.3 | <0.0001 |
| Black | 18.7 | 13.8 | 10.5 | 23.3 | ||
| Hispanic non-black | 10.2 | 10.4 | 18.3 | 4.5 | ||
| Other | 2.0 | 2.4 | 3.1 | 2.0 | ||
| BMI (kg/m2, mean ± SD) | 29.5 ± 6.6 | 29.3 ± 6.0 | 29.3 ± 6.0 | 29.3 ± 6.1 | ||
| Current smoking (%) | 15.9 | 13.1 | 0.0417 | 13.8 | 15.0 | 0.2193 |
| Physically active (≥1 times per week %) | 64.2 | 66.9 | 0.1728 | 69.1 | 64.1 | 0.0009 |
| Socioeconomic status | ||||||
| Education attainment (%) | ||||||
| College degree or greater | 22.3 | 24.1 | 0.0015 | 23.9 | 20.5 | <0.0001 |
| High school or equivalent | 52.7 | 55.2 | 58.0 | 54.0 | ||
| Less than high school | 25.0 | 20.7 | 18.0 | 25.5 | ||
| Family income (% ≤$35,000) | 46.1 | 37.8 | <0.0001 | 36.4 | 45.1 | <0.0001 |
| Median household income ($ in thousands, mean ± SD)b | 50.2 ± 24.0 | 57.0 ± 27.3 | 55.5 ± 24.7 | 52.6 ± 24.7 | ||
| Diabetes (%) | 23.1 | 22.5 | 0.8980 | 22.0 | 23.4 | 0.5163 |
| Hypertension (%) | 62.2 | 58.6 | 0.0928 | 57.9 | 61.7 | 0.0286 |
| Stroke (%) | 9.1 | 8.9 | 0.5740 | 9.5 | 9.0 | 0.7426 |
| Diabetes (%) | 8.8 | 6.9 | 0.0435 | 6.7 | 7.8 | 0.2434 |
| Respiratory illness (%) | 17.7 | 15.4 | 0.0982 | 16.6 | 15.2 | 0.2504 |
| Lonely ≥80th percentile (%) | 26.5 | 23.9 | 0.0994 | 22.6 | 26.8 | 0.0043 |
| Social support (socializing ≥1 per month, %) | 44.6 | 48.3 | 0.0027 | 51.4 | 41.7 | <0.0001 |
| Much difficulty get-up-and-go (≥2 score) (%) | 24.5 | 21.2 | 0.0655 | 21.2 | 22.4 | 0.5913 |
| Perceived stress score (mean ± SD) | 2.9 ± 2.4 | 2.6 ± 2.3 | 2.6 ± 2.3 | 2.8 ± 2.3 | ||
| Anxiety score (mean ± SD) | 4.5 ± 3.6 | 4.2 ± 3.3 | 4.2 ±3.3 | 4.3 ±3.4 | ||
| Depressive score (mean ± SD) | 5.7 ± 5.3 | 5.1 ± 4.9 | 4.9 ± 4.7 | 5.7 ± 5.3 | ||
| Resided in MSA (%) | 85.7 | 86.0 | <0.0001 | 74.7 | 98.5 | <0.0001 |
| Temperature annual (C, mean ± SD) | 14.0 ± 4.0 | 14.8 ± 4.5 | 14.4 ± 4.2 | 14.8 ± 4.5 | ||
| PM2.5 annual concentration (μg/m3, mean ± SD) | 9.8 ±3.0 | 9.7 ± 2.9 | 8.6 ± 2.7 | 11.0 ±2.7 | ||
| Urbanicity (mean ± SD) | 48.7 ± 33.9 | 43.0 ± 31.9 | - | - | ||
| Roadway distance (mean ± SD) | - | - | 544.8 ± 394.0 | 222.1 ± 181.4 | ||
| Greenness (mean ± SD) | 0.48 ± 0.18 | 0.53 ± 0.16 | 0.58 ± 0.17 | 0.43 ± 0.14 | ||
Abbreviations: SD refers to standard deviation; BMI refers to body mass index; COPD refers to chronic obstructive pulmonary disease; CESD stands for the Center for Epidemiological Studies – Depression; HADS-A stands for the Hospital Anxiety and Depression Scale – anxiety subscale; NDVI refers to the normalized difference vegetation index; MSA refers to metropolitan statistical area; PM2.5 refers to particulate matter with aerodynamic diameter of 2.5 micro or less.
2261 participants were in both wave 1 and wave 2; 744 participants were in wave 1 only; 1113 were in wave 2 only.
Estimated for census tract of residence using data from the U.S. Census Bureau (2000).
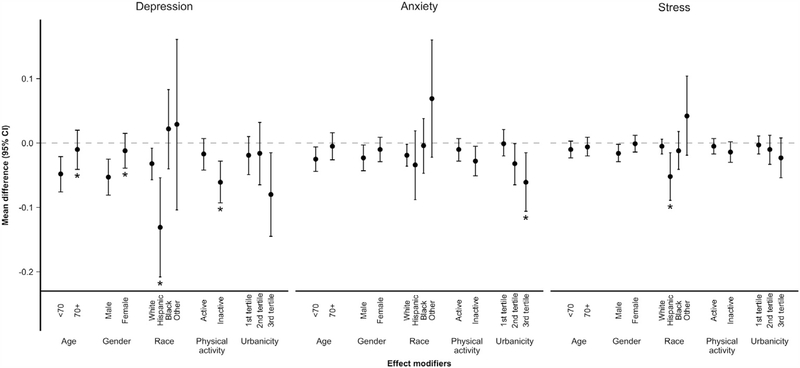
3.1. Roadway distance
An increment in roadway distance was significantly associated with decrease in depressive score (−0.033, 95% CI: −0.055, −0.010) and (−0.030, 95% CI: −0.052, −0.008) in base and multivariable models controlling for SES, respectively (Table 2). Roadway distance was both directly associated with depressive score (−0.020; 95% CI: −0.039, 0.000; Table 3), and indirectly through loneliness (40.7% mediated), in which living further from the roadway was associated with decreased loneliness, and in turn linked to lower depressive score (Sobel p < 0.05). To a lesser extent, roadway distance was also inversely associated with PM2.5 level, and subsequently depressive score (6% mediated). No other significant mediator was found. The inverse distance-depression association was stronger among participants aged <70, men, and those less physically active compared to their counterparts, and in Hispanic non-black as compared to White participants (pinteract < 0.05; Fig. 1). Effect estimates for depressive scores remained unchanged in sensitivity models further adjusting for traffic and noise in Wave 2 models or restricting to participants who did not take antidepressant medication (Table S2), and in additional analyses treating roadway distance as a categorical measure (Table S4).
Table 2.
Mean difference (95% CI) in depression and anxiety symptoms, and self-perceived stress associated with built environment measures.
| Depression | Anxiety | Perceived stress | |
|---|---|---|---|
| Distance to roadway (per 50 m) | |||
| Base modela | −0.033 (−0.055, −0.010)* | −0.017 (−0.032, −0.002)* | −0.009 (−0.019, 0.001) |
| Multivariable modelb | −0.030 (−0.052, −0.008)* | −0.016 (−0.031, −0.001)* | −0.007 (−0.018, 0.003) |
| Urbanicity (per interquartile rangec) | |||
| Base model | 0.370 (0.078, 0.663)* | 0.140 (−0.056, 0.337) | 0.133 (−0.002, 0.267) |
| Multivariable model | 0.288 (0.101, 0.574)* | 0.117 (−0.079, 0.246) | 0.098 (−0.035, 0.232) |
Base models adjusted for age, sex, race/ethnicity, year, season, day of week, MSA and region.
Multivariable Model 1 adjusted for age, sex, race/ethnicity, year, season, day of week, MSA, region, education attainment, family income of the participants, median household income.
Interquartile range of urbanicity was 57.8%.
p < 0.05.
Table 3.
Mediation analysis of the association between built environment and mental health measures in multivariable models.a
| Mediator | Direct effect (path E → O) | Indirect effectb (path E → M → O) | Percent mediatedc |
|---|---|---|---|
| Distance → depression | |||
| Physical activity | −0.030 (−0.052, −0.008)* | −0.001 (−0.004,0.003) | 2.1% |
| Loneliness | −0.020 (−0.039, 0.000)* | −0.012 (−0.020, −0.004)* | 40.7% |
| Social support | −0.029 (−0.051, −0.008)* | −0.001 (−0.004,0.001) | 3.5% |
| PM2.5 | −0.029 (−0.051, −0.006)* | −0.002 (−0.003, 0.000)* | 5.5% |
| NO2d | −0.024 (−0.054, 0.006) | −0.001 (−0.004,0.001) | 5.8% |
| Distance → anxiety | |||
| Physical activity | −0.016 (−0.031, −0.001)* | 0.000 (−0.001,0.001) | 1.3% |
| Loneliness | −0.009 (−0.023,0.005) | −0.007 (−0.011, −0.002)* | 42.2% |
| Social support | −0.016 (−0.031, −0.001)* | 0.000 (−0.002, 0.001) | 3.0% |
| PM2.5 | −0.015 (−0.030, 0.000) | −0.001 (−0.003,0.000)* | 8.7% |
| NO2 | −0.019 (−0.039, 0.001) | −0.002 (−0.004,0.000)* | 9.3% |
| Urbanicity → depression | |||
| Physical activity | 0.228 (−0.054,0.509) | 0.065 (0.021,0.109)* | 22.6% |
| Loneliness | 0.127 (−0.128, 0.382) | 0.193 (0.087, 0.300)* | 67.0% |
| Social support | 0.245 (−0.038, 0.529) | 0.046 (0.012, 0.080)* | 15.9% |
| PM2.5 | 0.203 (−0.094,0.500) | 0.084(0.007, 0.162)* | 29.4% |
| NO2 | 0.133 (−0.238, 0.504) | 0.049 (−0.023,0.122) | 26.9% |
All effects were expressed as the mean difference of the perceived stress per 50 m or interquartile range (57.8%) increment in distance to roadway or urbanicity, respectively.
Indirect effect was calculated as the product of two regression coefficients: (coefficient of exposure with mediator as the dependent variable) × (coefficient of mediator with mental health score as the dependent variable and exposure as another predictor).
Bold text refers to the statistically significant percent of mediation according to Sobel test (pindirect < 0.05).
Mediation analysis treating nitrogen dioxide (NO2) as mediator was restricted to a subset of NSHAP participants that resided within 90 km from a U.S. EPA ambient monitor that measured NO2 concentrations.
p < 0.05.
Fig. 1.
Mean difference (95% CI) in mental ill-health associated with roadway distance among NSHAP participants in multivariable models, stratified by effect modifiers1,2. 1Multivariable models adjusted for age, sex, race/ethnicity, year, season, day of week, MSA, region, education attainment, family income of the participants, and median household income. 2First category of each modifier as reference group; asterisks represent statistically significant effect modification (p interact < 0.05).
Increment in roadway distance was significantly associated with decrease in anxiety scores (−0.017, 95% CI: −0.032, −0.002) and (−0.016,95% CI: −0.031, −0.001) in base and multivariable models, respectively (Table 2). Most sensitivity analyses were consistent with those from the primary analyses, except for adjustment of road traffic or noise after which associations became insignificant (Table S2). As was found for the association with depression, loneliness, PM2.5 and NO2 (but not other examined potential mediators) were found to partially mediate the distance-anxiety association (38%, 8.7%, and 9.3% respectively, Table 3). The inverse distance-anxiety association was stronger in participants living in the most urbanized neighborhoods (Fig. 1), and those without diabetes or hypertension history (Table S5).
Perceived stress was not associated with roadway distance, irrespective of model construct, although we observed larger reductions in perceived stress among Hispanic non-blacks associated with roadway distance compared to Blacks (Fig. 1). Mediation was not evaluated given the null associations between roadway distance and stress across all participants.
3.2. Urbanicity
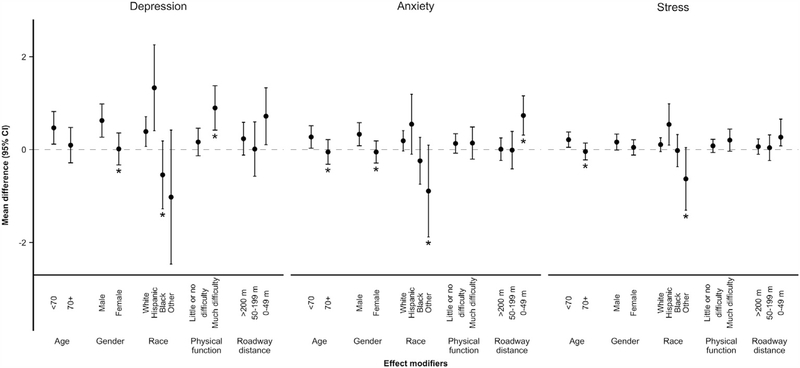
An IQR increase in urbanicity was significantly associated with 0.370 (95% CI: 0.078,0.663) and 0.288 (95% CI: 0.101,0.574) point increase in depressive symptoms in base and multivariable models adjusting for SES, respectively (Table 2). This urbanicity-depression association seemed to be partially mediated by loneliness and PM2.5, accounting for 67.0% and 29.4% of the total effect, respectively, in which living in more urbanized neighborhood was associated with increased loneliness and higher air pollution, and subsequently with increased depressive score (Table 3). The urbanicity-depression association was also significantly mediated by physical activity (22.6%) and social support (15.9%), as increased urbanicity was related to being less physically and socially active, which in turn associated with increased depression. However, the urbanicity-depression association became insignificant in most sensitivity analyses (Tables S3–S4). Nonetheless, men, Hispanic non-black participants, and those had much difficulty in physical function experienced a larger increase in depressive symptoms associated with urbanicity compared to their counterparts (Fig. 2 & Table S5).
Fig. 2.
Mean difference (95% CI) in mental ill-health associated with urbanicity among NSHAP participants in multivariable models, stratified by effect modifiers1,2. 1Multivariable models adjusted for age, sex, race/ethnicity, year, season, day of week, MSA, region, education attainment, family income of the participants, and median household income. 2First category of each modifier as reference group; asterisks represent statistically significant effect modification (p interact < 0.05).
Null associations were found for anxiety symptoms and urbanicity (Table 2). Yet, men, participants aged <70, those with history of diabetes, or lived within 49 m from the roadway had more pronounced positive urbanicity-anxiety association than their counterparts (Fig. 2). Similarly, urbanicity was insignificantly associated with perceived stress, irrespective of model construct. Only younger participants, and those who were physically inactive or had history of diabetes experienced larger increase in stress associated with urbanicity.
4. Discussion
We found that living further from roadway was significantly associated with decreases in depressive and anxiety symptoms among older adults, and mediated partially by loneliness and air pollution. The inverse distance-depression association was the greatest for younger participants, men, Hispanic non-black, and those less physically active, whereas the inverse distance-anxiety association was stronger among individuals without hypertension or diabetes history, lived in the more urbanized neighborhood. No association between roadway distance and perceived stress was found. Furthermore, urbanicity was significantly and positively associated with depressive score. The urbanicity-depression association was partially mediated by physical activity, social support, loneliness, PM2.5 and NO2, and was modified by gender, race/ethnicity, physical function, and season. While no significant urbanicity-anxiety/stress associations across all participants, we observed that urbanicity was associated with greater reductions in anxiety and stress levels among participants with certain individual-specific factors (e.g., younger age, diabetes history).
Wang et al. (2014) found null associations between residential distance to major roadway and depressive symptoms among 732 older adults from the MOBILIZE Boston study, whereas Power et al. (2015) reported associations with increased phobic anxiety only for Nurse Health Study (NHS) participants living within 50–200 m from the roadway, and not those living <50 m from the road, where the impact of traffic air pollution is the greatest. Findings heterogeneity between studies may be attributed to our more ethnically diverse sample of men and women aged 57–85 (mean age of 70) living across the U.S., as compared to the MOBILIZE population that consisted of mostly older (mean age of 78) White women (65%), and the NHS cohort that consisted of only nurses, predominately White. The importance of our study population is supported by our findings showing that the distance-depression/anxiety association was the strongest among younger (<70), Hispanic non-black and male participants, characteristics that were more represented in ours but not other cohorts. Additional possible explanations include difference in geographic area coverage, where a more localized geographic area (e.g., Boston in the MOBILIZE study) may result in lower variation in exposure, and in the examination of phobic anxiety in the NHS study as compared to general anxiety in the current study (Power et al., 2015; Wang et al., 2014).
Importantly, our observation of greater mental health symptoms associated with residence within 50 m of roadway is consistent with previous exposure studies showing elevated traffic-related air pollutant concentrations within 50 m of major roadways, with virtually no elevation in concentrations at further distances (Zhu et al., 2002). It is possible that our findings reflect the mental health impact of long-term exposures to traffic-related air pollutants. Black carbon, ultra-fine particles, and polycyclic aromatic hydrocarbons have been shown to induce oxidative processes, repress enzymatic antioxidants, and up-regulate pro-inflammatory mediators, all of which could result in neuroinflammation, and potentially lead to adverse mental conditions and decreased cognitive function (Power et al., 2011; Suglia et al., 2007). This is supported by our observation that PM2.5 and NO2 partially mediated the distance-depression/anxiety associations. However, while roadway distance has been hypothesized to be a surrogate of traffic noise and through this, to affect depression, stress and annoyance by increasing insomnia or stress hormone levels (Baglioni et al., 2011; Orban et al., 2016), adjustment of traffic or noise did not attenuate the significant distance-depression association in our study.
Our findings showing stronger inverse distance-mental health association among physically inactive older adults suggests that the impacts of roadway distance, potentially through traffic-related air pollution, may be greater in vulnerable individuals. This is consistent with collective evidence indicating that disadvantaged individuals by virtue of their lack of social support and physical health may be more susceptible to environmental hazards and that these characteristics may amplify the adverse health effects through a multiplicative interaction of higher hazard exposure and increased susceptibility (Morello-Frosch et al., 2011; Sacks et al., 2011). We found both direct and indirect inverse association of roadway distance with depression and anxiety symptoms through its ability to reduce the feelings of loneliness, which is contrary to a Dutch cohort where shorter distance to a highway access road was suggestively associated feeling less lonely (van den Berg et al., 2016). The heterogeneous findings may be explained by differences in housing and urban planning between the two countries, in which the Dutch study evaluated accessibility, whereas our measure represents poor access to facilities or parks that help foster local social interaction and community livability, or proxy for traffic-related exposure. Also, the Dutch cohort had a wider age distribution, whereas our cohort was comprised of community dwelling older adults who may be less mobile than the Dutch population. Further work is required to delineate the relative contribution of roadway distance on mental health.
Urbanicity was positively associated with depressive symptoms among older adults, with the association partially mediated by decreased physical activity and social support and increased loneliness and air pollution. This is consistent with findings showing that urbanization may increase mental illness through stressors such as overcrowding, pollution, and reduced social capital and support (Dekker et al., 2008; Peen et al., 2007; Srivastava, 2009), but in contrast with a Miami study that used land-use diversity, a computed index with larger values indicating greater diverse mix of land use categories (e.g., multifamily residential) (Miles et al., 2012). Our observed urbanicity-depression association may be particularly great among sensitive individuals, where Hispanic non-blacks, those with difficulty in physical function or lived <50 m from the roadway had higher depressive scores associated with increased urbanicity. Interestingly, urbanicity-anxiety/stress associations tended to be stronger only in seemingly more advantaged individuals (e.g., male, those without history of stroke), contrary to existing evidence showing that living in an urban neighborhood is a risk factor for mental illnesses.
Our findings have several limitations. Our mental health questionnaires are not clinical diagnostic instruments, but are widely used screening tools for current depressive and anxiety symptom severity in the somatic, psychiatric and general population settings (Bjelland et al., 2002). High PSS has also been shown to correlate with high serum cortisol (Walvekar, 2015). Built environment measures are prone to exposure misclassification error, as roadway distance does not account for traffic volume, prevailing wind speed, or direction or personal behaviors (e.g., time spent indoors), and urbanicity, operationalized by percent of urban land use, may lack specificity that could contribute to the null findings with anxiety and perceived stress. Our findings may not be generalizable to younger populations.
These limitations are substantially outweighed by the many strengths of our study. The application of a nationally representative, longitudinal sample of older, community dwelling Americans allows our findings to be broadly generalizable to older Americans, as compared to previous research that used convenience samples collected using mostly cross-sectional design of younger adults. We also accounted for both inter- and intra-personal variation in the association of the built environment and mental health, and assessed multiple sensitivity regression models. Lastly, we provided a comprehensive picture of association of built environment-mental health associations by exploring how the association was modified or mediated by individual or neighborhood characteristics.
5. Conclusions
Roadway distance was inversely associated with depressive and anxiety symptoms among older Americans, and the association was partially mediated by reducing level of loneliness and higher air pollution. Urbanicity was positively linked to depressive scores, mediated by physical activity, loneliness, social support and air pollutants. Our study findings warrant prospective studies to further examine the mediation and interaction of the impact of built environment on mental health.
Supplementary Material
HIGHLIGHTS.
Roadway distance was inversely linked to depressive and anxiety among older adults.
Loneliness and air pollution mediated the distance-mental health association.
Urbanicity was directly and indirectly linked to depression.
The urbanicity-depression association was evident in certain subpopulations.
Acknowledgement
We acknowledge Dr. Jeffrey Yanosky from the Penn State University for providing the data on proximity to nearest roadway and urbanicity. No disclosures to report.
Funding sources
This work was supported by NIEHS grant 1R01ES022657–01A1, with health and other covariate data obtained through NIH R01-AG021487, R37-AG030481, R01-AG033903, and R01-ES019168.
Footnotes
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2018.12.221.
References
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, Lombardo C, Riemann D, 2011. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 135, 10–19. https://doi.org/10.10167j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Preacher KJ, Gil KM, 2006. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: new procedures and recommendations. Psychol. Methods 11, 142–163. 10.1037/1082-989X.11.2.142. [DOI] [PubMed] [Google Scholar]
- Bjelland I, Bjelland I, Dahl A. a, Dahl A. a, Haug TT, Haug TT, Neckelmann D, Neckelmann D, 2002. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J. Psychosom. Res. 52,69–77. 10.1016/S0022-3999(01)00296-3.. [DOI] [PubMed] [Google Scholar]
- Clark C, Candy B, Stansfeld S. for the M.H.F, 2007. A systematic review on the effect of the built and physical environment on mental health. J. Public Ment. Health 6,14–27. [Google Scholar]
- Dekker J, Peen J, Koelen J, Smit F, Schoevers R, 2008. Psychiatric disorders and urbanization in Germany . BMC Public Health 9,1–9. 10.1186/1471-2458-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J, 1993. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J. Aging Health 5,179–193. [DOI] [PubMed] [Google Scholar]
- Krabbendam L, van Os J, 2005. Schizophrenia and urbanicity: a major environmental influence–conditional on genetic risk. Schizophr. Bull. 31, 795–799. 10.1093/schbul/sbi060. [DOI] [PubMed] [Google Scholar]
- Maas J, van Dillen SME, Verheij RA, Groenewegen PP, 2009. Social contacts as a possible mechanism behind the relation between green space and health. Health Place 15, 586–595. 10.1016/j.healthplace.2008.09.006.. [DOI] [PubMed] [Google Scholar]
- Mair C, Diez Roux AV, Galea S, 2008. Are neighborhood characteristics associated with depressive symptoms? A critical review. J. Epidemiol. Community Health 62, 940–946. 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- Messer K, Natarajan L, 2008. Maximum likelihood, multiple imputation and regression calibration for measurement error adjustment. Stat. Med. 27,6332–6350. 10.1002/sim.3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles R, Coutts C, Mohamadi A, 2012. Neighborhood urban form, social environment, and depression. J. Urban Health 89, 1–18. 10.1007/s11524-011-9621-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, Zuk M, Jerrett M, Shamasunder B, Kyle AD, 2011. Understanding the cumulative impacts of inequalities in environmental health: implications for policy. Health Aff. 30, 879–887. 10.1377/hlthaff.2011.0153. [DOI] [PubMed] [Google Scholar]
- Mykletun A, Stordal E, Dahl AA, 2001. Hospital Anxiety and Depression (HAD) scale: factor structure, item analyses and internal consistency in a large population. Br. J. Psychiatry 179, 540–544. 10.1192/bjp.179.6.540. [DOI] [PubMed] [Google Scholar]
- Orban E, McDonald K, Sutcliffe R, Hoffmann B, Fuks KB, Dragano N, Viehmann A, Erbel R, Jöckel K-H, Pundt N, Moebus S, 2016. Residential road traffic noise and high depressive symptoms after five years of follow-up: results from the Heinz Nixdorf recall study. Environ. Health Perspect. 124, 578–585. 10.1289/ehp.1409400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peen J, Dekker J, Schoevers RA, Beekman AT, ten Have M, de Graaf R, 2007. Is the prevalence of psychiatric disorders associated with urbanization? Soc. Psychiatry Psychiatr. Epidemiol. 42, 984 10.1007/s00127-007-0256-2. [DOI] [PubMed] [Google Scholar]
- Peen J, Schoevers RA, Beekman AT, Dekker J, 2010. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr. Scand. 121, 84–93. 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- Power MC, Weisskopf MG, Alexeeff SE, Coull B, Spiro A, Schwartz J, 2011. Traffic-related air pollution and cognitive function in a cohort of older men. Environ. Health Perspect. 119, 682–687. 10.1289/ehp.1002767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power MC, Kioumourtzoglou M-A, Hart JE, Okereke OI, Laden F, Weisskopf MG, 2015. The relation between past exposure to fine particulate air pollution and prevalent anxiety: observational cohort study. BMJ 350, h1111 10.1136/bmj.h1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pun VC, Manjourides J, Suh H, 2016. Association of ambient air pollution with depressive and anxiety symptoms in older adults: results from the NSHAP study. Environ. Health Perspect. 125, 342–348. 10.1289/EHP494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pun VC, Manjourides J, Suh H, 2017. Association of ambient air pollution with depressive and anxiety symptoms in older adults: results from the NSHAP study. Environ. Health Perspect. 125, 342–348. 10.1289/EHP494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pun VC, Manjourides J, Suh HH, 2018. Association of neighborhood greenness with self-perceived stress, depression and anxiety symptoms in older U.S adults. Environ. Health 17 (39). 10.1186/s12940-018-0381-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D, Peplau LA, Cutrona CE, 1980. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J. Pers. Soc. Psychol. 39, 472–480. [DOI] [PubMed] [Google Scholar]
- Saarloos D, Alfonso H, Giles-Corti B, Middleton N, Almeida OP, 2011. The built environment and depression in later life: the health in men study. Am. J. Geriatr. Psychiatry 19,461–470. 10.1097/JGP.0b013e3181e9b9bf. [DOI] [PubMed] [Google Scholar]
- Sacks JD, Stanek LW, Luben TJ, Johns DO, Buckley BJ, Brown JS, Ross M, 2011. Particulate matter-induced health effects: who is susceptible? Environ. Health Perspect. 119, 446–454. 10.1289/ehp.1002255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A, Madaan V, Petty FD, 2006. Exercise for mental health. Prim. Care Companion J. Clin. Psychiatry 8,106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shega JW, Sunkara PD, Kotwal A, Kern DW, Henning SL, McClintock MK, Schumm P, Waite LJ, Dale W, 2014. Measuring cognition: the Chicago cognitive function measure in the national social life, health and aging project, wave 2. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 69, S166–S176. 10.1093/geronb/gbu106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiovitz-Ezra S, Leitsch S, Graber J, Karraker A, 2009. Quality of life and psychological health indicators in the national social life, health, and aging project. J. Gerontol. B. Psychol. Sci. Soc. Sci. 64 (Suppl. 1), i30–i37. 10.1093/geronb/gbn020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S, Jaszczak A, Graber J, Lundeen K, Leitsch S, Wargo E, O’Muircheartaigh C, 2009. Instrument development, study design implementation, and survey conduct for the national social life, health, and aging project. J. Gerontol. B Psychol. Sci. Soc. Sci. 64 (Suppl. 1), i20–i29. 10.1093/geronb/gbn013.Instrument. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava K, 2009. Urbanization and mental health. Ind. Psychiatry J. 18, 75–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suglia SF, Gryparis A, Wright RO, Schwartz J, Wright RJ, 2007. Association of black carbon with cognition among children in a prospective birth cohort study. Am. J. Epidemiol. 167, 280–286. 10.1093/aje/kwm308. [DOI] [PubMed] [Google Scholar]
- Tallon LA, Manjourides J, Pun VC, Salhi C, Suh H, 2017. Cognitive impacts of ambient air pollution in the National Social Health and Aging Project (NSHAP) cohort. Environ. Int. 104,102–109. 10.1016/j.envint.2017.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census Bureau US, 2000. Census 2000 CD. U.S. Government Printing Office, Washington, DC. [Google Scholar]
- van den Berg P, Kemperman A, de Kleijn B, Borgers A, 2016. Ageing and loneliness: the role of mobility and the built environment. Travel Behav. Soc. 5,48–55. 10.1016/j.tbs.2015.03.001. [DOI] [Google Scholar]
- Volk HE, Hertz-Picciotto I, Delwiche L, Lurmann F, McConnell R, 2011. Residential proximity to freeways and autism in the CHARGE study. Environ. Health Perspect. 119, 873–877. 10.1289/ehp.1002835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walvekar SS, 2015. Study on serum cortisol and perceived stress scale in the police constables. J. Clin. Diagn. Res. 9,10–14. 10.7860/JCDR/2015/12015.5576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Eliot MN, Koutrakis P, Gryparis A, Schwartz JD, Coull B. a, Mittleman M. a, Milberg WP, Lipsitz L. a, Wellenius G. a, 2014. Ambient air pollution and depressive symptoms in older adults: results from the MOBILIZE Boston study. Environ. Health Perspect. 122, 553–558. 10.1289/ehp.1205909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welty LJ, Zeger SL, 2005. Are the acute effects of particulate matter on mortality in the National Morbidity, Mortality, and Air Pollution Study the result of inadequate control for weather and season? A sensitivity analysis using flexible distributed lag models. Am. J. Epidemiol. 162,80–88. 10.1093/aje/kwi157. [DOI] [PubMed] [Google Scholar]
- Yanosky JD, Paciorek CJ, Laden F, Hart JE, Puett RC, Liao D, Suh HH, 2014. Spatiotemporal modeling of particulate air pollution in the conterminous United States using geographic and meteorological predictors. Environ. Health 13 (63). 10.1186/1476-069X-13-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, Hinds WC, Kim S, Shen S, Sioutas C, 2002. Study of ultrafine particles near a major highway with heavy-duty diesel traffic. Atmos. Environ. 36, 4323–4335. 10.1016/S1352-2310(02)00354-0. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.