Abstract
Background:
Articular cartilage health is an important issue following anterior cruciate ligament (ACL) injury and primary ACL reconstruction. Factors present at the time of primary ACL reconstruction may influence the subsequent progression of articular cartilage damage.
Hypothesis:
We hypothesized that larger meniscus resection at primary ACL reconstruction, increased patient age, and increased body mass index (BMI) are associated with increased odds of worsened articular cartilage damage at the time of revision ACL reconstruction.
Study Design:
Prospective cohort study
Methods:
Subjects who had both primary and revision data contained in the Multicenter Orthopaedics Outcomes Network (MOON) and Multicenter ACL Revision Study (MARS) databases were included. Data reviewed included chondral surface status at the time of primary and revision surgery, meniscal status at the time of primary reconstruction, primary reconstruction graft type, time from primary to revision ACL surgery, as well as demographics and Marx activity score at the time of revision. Significant progression of articular cartilage damage was defined in each compartments according to progression on the modified Outerbridge scale (increase of ≥1 grade) or a greater than 25% enlargement in any area of damage. Logistic regression was used to identify predictors of significant chondral surface change in each compartment from primary to revision surgery.
Results:
A total of 134 patients were included with a median age19.5 years at revision surgery. Progression of articular cartilage damage was noted in 34 patients (25.4%) in the lateral compartment, 32 patients (23.9%) in the medial compartment, and 31 patients (23.1%) in the patellofemoral compartment. In the lateral compartment, patients who had greater than 33% of their lateral meniscus excised at primary reconstruction had 16.9 times greater odds of progression of articular cartilage injury than those with an intact lateral meniscus (p < 0.001). In the medial compartment, patients who had less than 33% of their medial meniscus excised at the time of the primary reconstruction had 4.8 times greater odds of progression of articular cartilage injury than those with an intact medial meniscus (p = 0.02). Odds of significant chondral surface change increased by 5% in the lateral compartment and 6% in the medial compartment for each increased year of age (p ≤0.02). In the patellofemoral compartment, the use of allograft was associated with a 15-fold increased odds of progression of articular cartilage damage relative to a patellar tendon autograft (p < 0.001). Each one unit increase in BMI at the time of revision surgery was associated with a 10% increase in the odds of progression of articular cartilage damage (p = 0.046) in the patellofemoral compartment.
Conclusion:
Excision of the medial and lateral meniscus at primary ACL reconstruction increases the odds of articular cartilage damage in the corresponding compartment at the time of revision ACL reconstruction. Increased age is a risk factor for deterioration of articular cartilage in both tibiofemoral compartments, while increased BMI and the use of allograft for primary ACL reconstruction are associated with an increased risk of progression in the patellofemoral compartment.
Keywords: ACL reconstruction, meniscus, articular cartilage, patellofemoral compartment, BMI, allograft
Introduction
The anterior cruciate ligament (ACL) is often injured and frequently reconstructed in young, active patients. While today’s techniques typically result in clinically stable ligament reconstructions that facilitate return to activity, the subsequent development of osteoarthritis following these procedures remains a vexing problem.23 While numerous factors have been associated with increased osteoarthritis risk following ACL tears, the status and treatment of the meniscus at the time of ACL reconstruction has consistently been shown to strongly correlate with subsequent risk of osteoarthritis.11, 17, 25
Patients undergoing revision ACL reconstruction have consistently demonstrated poorer outcomes than those undergoing primary reconstruction and are known to have a higher risk of the development of osteoarthritis.1, 7, 8, 12, 22, 31, 32 These poor results are likely associated with an increased prevalence of additional intra-articular pathology in patients undergoing revision reconstruction compared to those undergoing primary ACL reconstruction.2 The prevalence of additional intra-articular damage has been shown to be higher still among those undergoing repeat revision surgery.5 Brophy et al demonstrated that patients with a history of partial meniscectomy were at increased risk of having significant articular cartilage damage at the time of revision ACL reconstruction compared to those with no history of meniscus surgery.4 Wyatt et al utilized the Kaiser Permanente ACL registry to identify patients who underwent both primary and revision ACL reconstruction. They noted an increase in the prevalence of articular cartilage damage from primary to revision surgery, particularly on the medial tibial plateau and femoral trochlea.33 Previous studies correlating graft type and the risk of subsequent development of osteoarthritis have yielded mixed results, with patellar tendon autografts found to be associated with increased risk in some series,16, 26 but not others.9, 30
Identification of patient, injury, and surgery characteristics that are associated with progression of articular cartilage damage following primary ACL reconstruction is a key step to identifying at-risk patients for potential intervention. No prior work has attempted to identify the factors associated with progression of articular cartilage damage documented arthroscopically. The goal of this study was to identify factors associated with progression of articular cartilage damage from failed primary to revision ACL reconstruction. We hypothesized that larger meniscus resection at primary ACL reconstruction, increased patient age, and increased body mass index (BMI) are associated with increased odds of worsened articular cartilage damage between the time of the patient’s primary and revision surgery.
Methods
The Multicenter Orthopaedics Outcomes Network (MOON) and the Multicenter ACL Revision Study (MARS) databases were queried to identify patients who were enrolled in the MOON database for their primary ACL reconstruction and subsequently enrolled in the MARS database for a revision ACL reconstruction. Patients who underwent a multi-ligament reconstruction or meniscus transplant at primary ACL reconstruction were excluded.
Prospectively collected data on these patients were then extracted from both databases. Data contained in both the MOON and MARS databases were collected in identical fashion from the same set of surgeons. Extracted data included articular cartilage status (modified Outerbridge grade and size of any lesions) at the time of primary and revision reconstruction, meniscus status (no treatment, ≤33% excision, >33% excision, repair), graft type (autograft bone-patellar tendon-bone (BTB), autograft hamstring, allograft) at the time of primary reconstruction, time from primary to revision ACL surgery, as well as patient age, sex, smoking status, body mass index (BMI), Marx activity rating score,20 and situation of injury (sport or non-sport injury) that led to revision reconstruction.
Significant progression of articular cartilage damage was defined for each compartment according to progression on the modified Outerbridge scale24 (Grade 0/1 to Grade 2/3 or Grade 2/3 to Grade 4) or a greater than 25% enlargement in the size of the defect between the primary and revision reconstructions.
Multiple logistic regression modeling was used to evaluate which factors were associated with progression of articular cartilage injury from primary to revision surgery. The lateral, medial, and patellofemoral compartments were modeled separately. Potential variables included meniscus status at primary reconstruction, graft type, time from primary to revision surgery, patient sex, smoking status, body mass index (BMI), mechanism of injury prior to revision reconstruction, age at revision surgery, and Marx activity rating score at revision reconstruction. A forward selection modeling procedure was utilized with variables sequentially added to the model and kept in the model if they were significant predictors of progression of articular cartilage injury. The final model for the lateral compartment included lateral meniscus status at primary reconstruction and patient age at revision surgery. The final model for the medial compartment included medial meniscus status at primary reconstruction and patient age at revision surgery. The final model for the patellofemoral compartment included graft type for the primary ACL reconstruction, patient BMI, and time from primary to revision reconstruction. The presence of interactions between all included predictors was evaluated and no significant interactions were identified. Based on the 4 degrees of freedom required to model these potential predictor variables, the 34 “events” (progression of articular cartilage injury) in the lateral compartment, 32 “events” in the medial compartment, and 31 “events” in the patellofemoral compartment provided sufficient power for this analysis.
Medians and interquartile (IQ) ranges were calculated for time between primary and revision surgery, age at revision, and Marx activity score at revision surgery to evaluate differences between groups with and without progression of articular cartilage injury based on meniscus status at primary reconstruction. STATA version 13.1 (StataCorp LP, College Station, TX) was used for all statistical analyses.
Results
Between 2002 and 2008, 2326 patients who underwent primary ACL reconstruction without posterior cruciate or collateral ligament injuries requiring surgical treatment were enrolled in the MOON prospective cohort. One hundred thirty-four of these patients underwent a subsequent revision ACL reconstruction that was captured in the MARS cohort. Median patient age at time of revision was 19.5 years [IQ range 17–25] and the median time from primary to revision surgery was 462.5 days. Other patient demographics are shown in Table 1. Articular cartilage status at revision and primary surgery are summarized in Table 2. There were 34 patients (25.4%) who demonstrated progression of lateral compartment articular cartilage damage, 32 patients (23.9%) who demonstrated progression of medial compartment articular cartilage damage, and 31 patients (23.1%) who demonstrated progression of patellofemoral articular cartilage damage.
Table 1:
Demographics
| Median | IQ Range | |
|---|---|---|
| Age (years) | 19.5 | 17–25 |
| Body Mass Index (BMI) (kg/m2) | 23.8 | 21.9 – 26.6 |
| Marx Activity Level | 15 | 11 – 16 |
| Time from Primary to Revision Reconstruction (days) | 462.5 | 292–1049 |
| N | Percentage | |
| Sex | ||
| Male | 72 | 53.7% |
| Graft type at primary reconstruction | ||
| Autograft BTB | 37 | 27.6% |
| Medial meniscus status at primary reconstruction | ||
| No treatment | 95 | 70.9% |
| Lateral meniscus status at primary reconstruction | ||
| No treatment | 89 | 66.4% |
| Cartilage procedures at primary reconstruction | ||
| Chondroplasty* | 21 | 15.7% |
| Lateral Femoral Condyle | 4 | |
| Lateral Tibial Plateau | 3 | |
| Medial Femoral Condyle | 10 | |
| Medial Tibial Plateau | 1 | |
| Patella | 13 | |
| Trochlea | 3 | |
| Microfracture | 2 | 1.5% |
| Medial Femoral Condyle | 2 | |
| None | 111 | 82.8% |
| Smoking status at revision | ||
| No | 121 | 90.3% |
| Situation of injury at revision | ||
| Non-sport | 36 | 26.9% |
Note: The total number of patients who underwent chondroplasty is smaller than the sum of the number of chondroplasties performed by compartment as several patients had multiple compartments treated
Table 2:
Summary of articular cartilage Outbridge score for each compartment of the knee at primary and revision ACL reconstruction
| Articular Cartilage Outerbridge Status | ||
|---|---|---|
| Location | Primary Reconstruction n = 134 | Revision Reconstruction n = 134 |
| Lateral Femoral Condyle | Normal 0/1: 116 | Grade 0/1: 100 |
| Lateral Tibial Plateau | Normal 0/1: 126 | Normal 0/1: 118 |
| Medial Femoral Condyle | Normal 0/1: 112 | Normal 0/1: 96 |
| Medial Tibial Plateau | Normal 0/1: 130 | Normal 0/1: 125 |
| Patella | Normal 0/1: 117 | Normal 0/1: 106 |
| Trochlea | Normal 0/1: 115 | Normal 0/1: 94 |
In the lateral compartment, patients who had greater than 33% of their lateral meniscus excised at the time of the primary reconstruction had 16.9 times greater odds of progression of articular cartilage injury than those with an intact lateral meniscus, controlling for age (p < 0.001). Those who had less than 33% of the lateral meniscus excised did not demonstrate increased odds of progression relative to those with a normal meniscus (Table 3). Odds of progression of articular cartilage damage increased by 5% (p = 0.01) for each increased year of age (Table 3).
Table 3:
Risk of significant change in chondral damage by compartment
| Medial Compartment | |||
|---|---|---|---|
| Odds ratio | p | 95% CI | |
| Age | 1.06 | 0.01 | 1.01–1.10 |
| Medial meniscus | |||
| No treatment, n = 95 | REF | REF | REF |
| Lateral compartment | |||
| Odds ratio | p | 95% CI | |
| Age | 1.05 | 0.01 | 1.01–1.10 |
| Lateral meniscus | |||
| No treatment, n = 89 | REF | REF | REF |
| Patellofemoral compartment | |||
| Odds ratio | p | 95% CI | |
| Body Mass Index | 1.11 | 0.046 | 1.00 – 1.22 |
| Time from Primary to Revision (months) | 1.02 | 0.047 | 1.00 – 1.04 |
| Primary Graft Type | |||
| BTB Auto, n = 37 | REF | REF | REF |
| Hamstring Auto, n = 48 | 4.34 | 0.08 | 0.84 – 22.43 |
| Allograft, n = 44 | 15.5 | <0.001 | 3.17 – 75.38 |
| Hybrid, n = 5 | NA | NA | NA |
REF: Reference Group
NA: Not Available due to insufficient numbers
In the medial compartment, patients who had less than 33% of their medial meniscus excised at the time of the primary reconstruction had 4.8 times greater odds of progression of articular cartilage injury than those with an intact medial meniscus, controlling for age (p = 0.02). Those who had greater than 33% of the medial meniscus excised or had a meniscus repair did not demonstrate increased odds of progression relative to those with a normal meniscus (Table 2). Odds of progression of articular cartilage damage increased by 6% (p=0.01) for each increased year of age (Table 3).
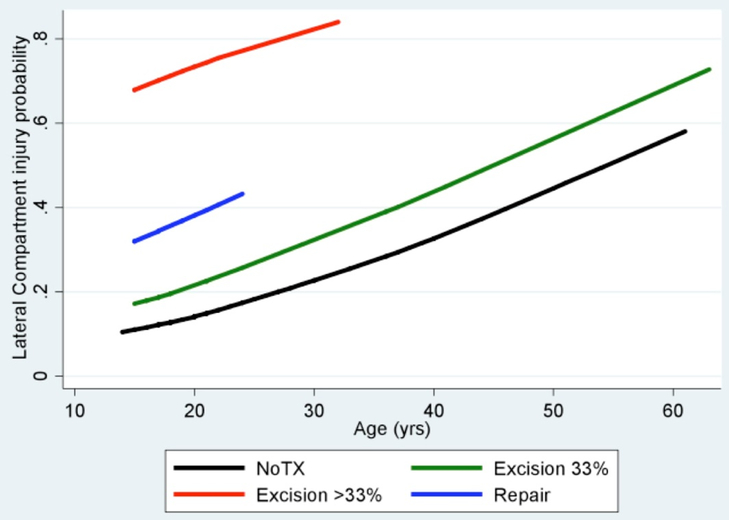
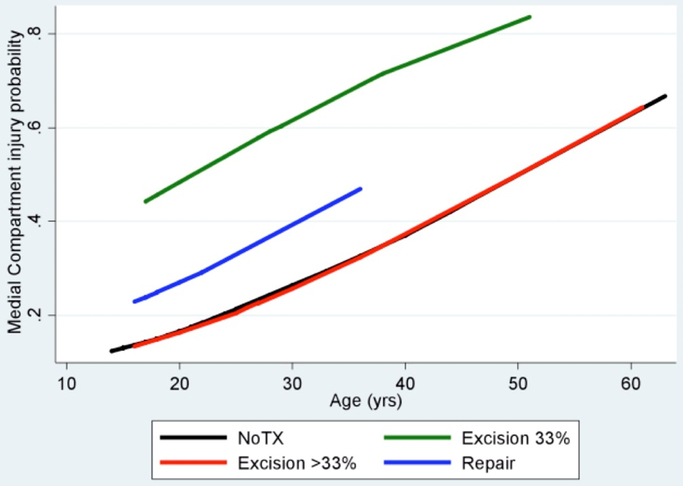
The calculated risk of progression of articular cartilage damage based on meniscus status at primary reconstruction and age at revision surgery in the lateral (Figure 1) and medial (Figure 2) compartments are shown. Graft type, time from primary to revision surgery, patient sex, BMI, smoking status, mechanism of injury, and Marx activity score at revision were not significant predictors of progression of chondral surface change for either tibiofemoral compartment (p > 0.05).
Figure 1:
Calculated probability of progression of lateral compartment chondral surface change from primary to revision ACL reconstruction based on patient age and lateral meniscus status at the time of primary ACL reconstruction.
Figure 2:
Calculated probability of progression of medial compartment chondral surface change from primary to revision ACL reconstruction based on patient age and medial meniscus status at the time of primary ACL reconstruction.
Medians and interquartile ranges of time between primary and revision surgery, age at revision, Marx activity score at revision surgery by meniscus status (for the lateral and medial compartments) and graft type (for the patellofemoral compartment) are shown in Table 4. While numbers are too small for valid statistical comparison, there is a trend toward decreasing Marx activity level with larger amounts of medial meniscus resection. A similar trend is not seen laterally, where activity level remains very high regardless of the degree of lateral meniscus resected.
Table 4:
Median time from primary to revision ACL reconstruction, age, and Marx activity level by meniscal status
| Medial Compartment | |||
|---|---|---|---|
| Time (months) | Age at revision (years) | Marx score at revision | |
| Medial meniscus | Median [Interquartile range] | ||
| No Treatment | 14.7 [9.4–34.4] | 18 [17–22] | 16 [12–16] |
| Excision ≤33% | 13.1 [7.3–23.8] | 27.5 [19–33] | 14.5 [4.5–16] |
| Excision >33% | 32.4 [12.3–47.6] | 25.5 [19.5–33] | 12 [4–14.5] |
| Repair | 14.3 [12.8–25.2] | 18 [17–22] | 16 [9–16] |
| Lateral Compartment | |||
| Time (months) | Age at revision (years) | Marx score at revision | |
| Lateral Meniscus | Median [Interquartile range] | ||
| No Treatment | 14.7 [9.4–32.8] | 20 [17–27] | 13 [10–16] |
| Excision ≤33% | 19.0 [12.6–35.1] | 18 [17–29] | 16 [12–16] |
| Excision >33% | 23.7 [9.4–31.7] | 19 [17–21] | 16 [12–16] |
| Repair | 19.6 [9.1–50.0] | 19 [15–21] | 16 [7–16] |
| Patellofemoral Compartment | |||
| Time (months) | Age at revision (years) | Marx score at revision | |
| Graft Type | Median [Interquartile range] | ||
| BTB Autograft | 14.9 [11.9–32.8] | 19 [17–21] | 16 [12–16] |
| Hamstring Autograft | 12.7 [8.4–41.5] | 18.5 [17–23] | 16 [12–16] |
| Allograft | 18.0 [10.8–34.2] | 24.5 [17.5–36] | 12 [5.5–16] |
| Hybrid | 9.5 [9.1–12.8] | 17 [15–17] | 16 [12–16] |
In the patellofemoral compartment, primary ACL reconstruction with an allograft was associated with a 15-fold increased odds of progression of articular cartilage damage relative to a patellar tendon autograft (OR = 15.5, p < 0.001). The use of a hamstring autograft was not associated with significantly increased odds of progression relative to patellar tendon autograft (OR = 4.3, p = 0.08). Each one unit increase in BMI at the time of revision surgery was associated with a 10% increase in the odds of progression of articular cartilage damage (OR = 1.11, p = 0.046). Each one month increase in time from primary to revision surgery was associated with a 2% increase in the odds of progression of articular cartilage damage (OR = 1.02, p = 0.047). No other potential predictors were associated with increased odds of progression.
Discussion
The most significant findings of this study were that loss of greater than 33% of the lateral meniscus at the time of primary ACL reconstruction resulted in a nearly 17-fold increase in the odds of progression of articular cartilage damage in the lateral compartment, while the use of an allograft for primary reconstruction was associated with a 15-fold increase in the odds of progression of articular cartilage damage in the patellofemoral compartment. The relationship between amount of meniscus resection and risk of progression of articular damage was not reproduced in the medial compartment, where those patients with smaller amount of meniscus loss demonstrated the highest odds of progression of articular cartilage damage. It is important to emphasize that this finding does not imply that resection of the medial meniscus is benign but rather that the relationship between meniscal resection and progression of articular cartilage damage in the medial compartment is not a simple dose response curve. Other factors including knee alignment and activity level may contribute. Further, it is possible that longer-term follow-up for this young cohort will detect further progression of cartilage damage and clarification of the relationship with meniscal resection.
The different findings of this study in the lateral and medial compartments likely reflect differences in anatomy and meniscus function in the two compartments. The extreme increase in odds of progression of cartilage damage following significant lateral meniscal loss may be due to the fact that the key role of the meniscus is dispersing forces in the lateral compartment, which consists of two convex articular cartilage surfaces. Cadaveric work has demonstrated significant increases in contact pressure following partial meniscectomy and more severe changes following complete meniscectomy.10 Repair of the lateral meniscus has been demonstrated to return contact pressure to near, but not quite normal levels, potentially decreasing the risk of subsequent chondral injury.21 The results in this cohort demonstrate a trend toward increased risk of articular cartilage damage progression with lateral meniscus repair compared to no tear, which is consistent with an incomplete restoration of function of the lateral meniscus with repair. Long-term clinical studies have confirmed the association of partial meniscectomy and osteoarthritis and provide evidence that meniscus repair may minimize this risk.17
Cadaveric studies have also demonstrated increased contact pressure in the medial compartment following meniscal resection.10, 13 For this reason, we hypothesized that larger meniscal resection would result in more progression of articular cartilage damage by the time of revision ACL reconstruction; however, the data did not support this model. One possible explanation for this unexpected finding is that the medial meniscus is an important stabilizer of the knee, particularly in the setting of damage to the ACL.14 Those patient with large amount of meniscus loss may experience symptoms in the knee that lead them to limit their activity level and thus their risk of subsequent articular cartilage damage. It is possible that patients with significant meniscal loss have persistent symptoms of instability that preclude their complete return to sports, thus protecting the knee from increased load and articular cartilage damage. While there is not clear evidence in the literature that increased knee laxity or subjective symptoms of instability are more prevalent in the setting of significant medial meniscus loss in ACL-reconstructed knees, several studies have demonstrated an association between meniscus loss and increased laxity in ACL-deficient knees.18, 35 Review of patients in this study support this theory, as those who underwent resection of greater than 33% of the meniscus reported a median Marx activity score of 12, while those with an intact medial meniscus and those with who underwent resection of less than 33% of the meniscus reported median Marx activity scores of 16 (Table 3). No such decreases in Marx activity level were noted for those who underwent resection of greater than 33% of the lateral meniscus (Table 3).
Another possible explanation for the different findings between the medial and lateral compartments is the lack of alignment data. Brophy et al demonstrated that malalignment was associated with medial compartment chondrosis, but not lateral compartment chondrosis, in patients undergoing revision ACL reconstruction.3 The effect of alignment on medial compartment chondral wear could be an important confounder that contributes to this discrepancy between degree of meniscus resection and progression of chondral damage in the medial compartment. More research is warranted to better understand the reasons for this discordance.
The finding that the use of allograft was associated with a significantly increased risk of progression of patellofemoral articular cartilage damage was unexpected. Some previous work has suggested that the use of a BTB autograft is associated with increased risk of osteoarthritis when compared to hamstring autograft - particularly in the patellofemoral joint,16, 26 but other studies, including ours, contradict these findings.9, 30 The difference between BTB and hamstring autograft in the progression of patellofemoral chondrosis was not significant in this cohort. The authors are aware of no previous studies that explicitly demonstrate an increased risk of articular cartilage damage or the development of osteoarthritis with the use of allograft compared to autograft. The known increased failure risk of allograft in many populations may confound any demonstrated association between osteoarthritis and graft choice due to increased failures and subsequent surgery in the allograft group.29
The increased odds of progression of articular cartilage damage in the allograft group in this series that includes only patients with a subsequent graft tear cannot be attributed to an increased failure risk. One could hypothesize as to several potential mechanisms for this association. Allograft may be more likely to stretch,27, 28 potentially leading to increased load on articular cartilage and risk of damage progression. In addition, recent work has highlighted the role of biochemical mediators in the subsequent development of osteoarthritis following ACL injury and reconstruction.15 The use of allograft tissue has been associated with increased risk of poor graft incorporation and the development of “biologic failure” of ACL grafts.34 While the specific mechanism and long-term consequences of such failures are unclear, the potential effect of such failures on cartilage health requires further research.
Strengths of this study include large patient numbers and detailed, prospective data collection. Assessment of the articular cartilage lesions was performed by the same surgeons at primary and revision surgery. These surgeons have previously demonstrated good inter-rater reliability with cartilage assessment using the modified Outerbridge scale19 as well as assessment of meniscal pathology.6 The primary limitation of this study is related to its generalizability. The patients who undergo revision ACL reconstruction are a subset of all patients treated with primary ACL reconstruction. These patients are a very young group undergoing revision ACL reconstruction (mean age under 20) that may not be representative of the average patient undergoing revision surgery. It is also not known whether the factors that lead to articular cartilage progression in a population with a graft tear would also affect articular cartilage in the same way in those who do not tear their ACL grafts. Another limitation is the lack of alignment data, as mentioned previously. Further, the method by which articular cartilage injury progression was defined has limitations. The criteria for progression were chosen arbitrarily as the degree of increase area of cartilage pathology required to be clinically relevant is unknown. All patients who met the criteria for progression were classified in the same way, even though some had progressed more than one Outerbridge grade or had done so over a larger area of the knee than others. The effect of these differences on the study findings is not known. Finally, the study may be subject to selection bias in regards to graft choice for revision surgery. Surgeons likely base graft choice on numerous, uncontrolled factors other than age that may influence the subsequent risk of articular cartilage progression that may be contributing to the demonstrated association between allograft choice and progression of patellofemoral joint articular cartilage damage.
Conclusion
Excision of the medial and lateral meniscus at primary ACL reconstruction increases the odds of articular cartilage damage in the corresponding compartment at the time of revision ACL reconstruction. Increased age is a risk factor for deterioration of articular cartilage in both tibiofemoral compartments, while increased BMI and the use of allograft for primary ACL reconstruction are associated with an increased risk of progression in the patellofemoral compartment.
What is known about the subject:
The status and treatment of the meniscus at the time of ACL reconstruction has consistently been shown to strongly correlate with subsequent risk of osteoarthritis.
What this study adds to existing knowledge:
Loss of greater than 33% of the lateral meniscus at the time of primary ACL reconstruction resulted in a nearly 17-fold increase in the odds of progression of articular cartilage damage in the lateral compartment, while the use of an allograft for primary reconstruction was associated with a 15-fold increase in the odds of progression of articular cartilage damage in the patellofemoral compartment.
References
- 1.Ahn JH, Lee YS, Ha HC. Comparison of revision surgery with primary anterior cruciate ligament reconstruction and outcome of revision surgery between different graft materials. Am J Sports Med. 2008;36(10):1889–1895. [DOI] [PubMed] [Google Scholar]
- 2.Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med. 2011;39(9):1889–1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brophy RH, Haas AK, Huston LJ, Nwosu SK, Wright RW. Association of Meniscal Status, Lower Extremity Alignment, and Body Mass Index With Chondrosis at Revision Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2015;43(7):1616–1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brophy RH, Wright RW, David TS, et al. Association between previous meniscal surgery and the incidence of chondral lesions at revision anterior cruciate ligament reconstruction. Am J Sports Med. 2012;40(4):808–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen JL, Allen CR, Stephens TE, et al. Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: a MARS cohort study. Am J Sports Med. 2013;41(7):1571–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunn WR, Wolf BR, Amendola A, et al. Multirater agreement of arthroscopic meniscal lesions. Am J Sports Med. 2004;32(8):1937–1940. [DOI] [PubMed] [Google Scholar]
- 7.Gifstad T, Drogset JO, Viset A, Grontvedt T, Hortemo GS Inferior results after revision ACL reconstructions: a comparison with primary ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2011–2018. [DOI] [PubMed] [Google Scholar]
- 8.Grassi A, Ardern CL, Marcheggiani Muccioli GM, Neri MP, Marcacci M, Zaffagnini S. Does revision ACL reconstruction measure up to primary surgery? A meta-analysis comparing patient-reported and clinician-reported outcomes, and radiographic results. Br J Sports Med. 2016. [DOI] [PubMed] [Google Scholar]
- 9.Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38(3):448–454. [DOI] [PubMed] [Google Scholar]
- 10.Ihn JC, Kim SJ, Park IH. In vitro study of contact area and pressure distribution in the human knee after partial and total meniscectomy. Int Orthop. 1993;17(4):214–218. [DOI] [PubMed] [Google Scholar]
- 11.Jones MH, Spindler KP, Fleming BC, et al. Meniscus treatment and age associated with narrower radiographic joint space width 2–3 years after ACL reconstruction: data from the MOON onsite cohort. Osteoarthritis Cartilage. 2015;23(4):581–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kievit AJ, Jonkers FJ, Barentsz JH, Blankevoort L. A cross-sectional study comparing the rates of osteoarthritis, laxity, and quality of life in primary and revision anterior cruciate ligament reconstructions. Arthroscopy. 2013;29(5):898–905. [DOI] [PubMed] [Google Scholar]
- 13.Lee SJ, Aadalen KJ, Malaviya P, et al. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006;34(8):1334–1344. [DOI] [PubMed] [Google Scholar]
- 14.Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64(6):883–888. [PubMed] [Google Scholar]
- 15.Li H, Chen C, Chen S. Posttraumatic knee osteoarthritis following anterior cruciate ligament injury: Potential biochemical mediators of degenerative alteration and specific biochemical markers. Biomed Rep. 2015;3(2):147–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Magnussen RA, Carey JL, Spindler KP. Does autograft choice determine intermediate-term outcome of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2011;19(3):462–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009;22(4):347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Magnussen RA, Reinke EK, Huston LJ, Group M, Hewett TE, Spindler KP. Factors Associated With High-Grade Lachman, Pivot Shift, and Anterior Drawer at the Time of Anterior Cruciate Ligament Reconstruction. Arthroscopy. 2016;32(6):1080–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marx RG, Connor J, Lyman S, et al. Multirater agreement of arthroscopic grading of knee articular cartilage. Am J Sports Med. 2005;33(11):1654–1657. [DOI] [PubMed] [Google Scholar]
- 20.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. [DOI] [PubMed] [Google Scholar]
- 21.Ode GE, Van Thiel GS, McArthur SA, et al. Effects of serial sectioning and repair of radial tears in the lateral meniscus. Am J Sports Med. 2012;40(8):1863–1870. [DOI] [PubMed] [Google Scholar]
- 22.Ohly NE, Murray IR, Keating JF. Revision anterior cruciate ligament reconstruction: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2007;89(8):1051–1054. [DOI] [PubMed] [Google Scholar]
- 23.Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38(11):2201–2210. [DOI] [PubMed] [Google Scholar]
- 24.Outerbridge RE. Osteochondritis dissecans of the posterior femoral condyle. Clin Orthop Relat Res. 1983;175:121–129. [PubMed] [Google Scholar]
- 25.Pernin J, Verdonk P, Si Selmi TA, Massin P, Neyret P. Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med. 2010;38(6):1094–1102. [DOI] [PubMed] [Google Scholar]
- 26.Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–574. [DOI] [PubMed] [Google Scholar]
- 27.Poehling GG, Curl WW, Lee CA, et al. Analysis of outcomes of anterior cruciate ligament repair with 5-year follow-up: allograft versus autograft. Arthroscopy. 2005;21(7):774–785. [DOI] [PubMed] [Google Scholar]
- 28.Scheffler SU, Schmidt T, Gangey I, Dustmann M, Unterhauser F, Weiler A. Fresh-frozen free-tendon allografts versus autografts in anterior cruciate ligament reconstruction: delayed remodeling and inferior mechanical function during long-term healing in sheep. Arthroscopy. 2008;24(4):448–458. [DOI] [PubMed] [Google Scholar]
- 29.Wasserstein D, Sheth U, Cabrera A, Spindler KP. A Systematic Review of Failed Anterior Cruciate Ligament Reconstruction With Autograft Compared With Allograft in Young Patients. Sports Health. 2015;7(3):207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Webster KE, Feller JA, Hartnett N, Leigh WB, Richmond AK. Comparison of Patellar Tendon and Hamstring Tendon Anterior Cruciate Ligament Reconstruction: A 15-Year Follow-up of a Randomized Controlled Trial. Am J Sports Med. 2016;44(1):83–90. [DOI] [PubMed] [Google Scholar]
- 31.Weiler A, Schmeling A, Stohr I, Kaab MJ, Wagner M. Primary versus single-stage revision anterior cruciate ligament reconstruction using autologous hamstring tendon grafts: a prospective matched-group analysis. Am J Sports Med. 2007;35(10):1643–1652. [DOI] [PubMed] [Google Scholar]
- 32.Wright R, Spindler K, Huston L, et al. Revision ACL reconstruction outcomes: MOON cohort. J Knee Surg. 2011;24(4):289–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wyatt RW, Inacio MC, Liddle KD, Maletis GB. Prevalence and Incidence of Cartilage Injuries and Meniscus Tears in Patients Who Underwent Both Primary and Revision Anterior Cruciate Ligament Reconstructions. Am J Sports Med. 2014;42(8):1841–1846. [DOI] [PubMed] [Google Scholar]
- 34.Yoo SH, Song EK, Shin YR, Kim SK, Seon JK. Comparison of clinical outcomes and second-look arthroscopic findings after ACL reconstruction using a hamstring autograft or a tibialis allograft. Knee Surg Sports Traumatol Arthrosc. 2015. [DOI] [PubMed] [Google Scholar]
- 35.Zaffagnini S, Signorelli C, Bonanzinga T, et al. Does meniscus removal affect ACL-deficient knee laxity? An in vivo study. Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3599–3604. [DOI] [PubMed] [Google Scholar]