Supplemental Digital Content is available in the text.
Keywords: botulinum toxin type A, neuroscience, pain, quality of life, spasticity, wrist
Background and Purpose—
The aim of this trial was to determine the effect of additional upper limb rehabilitation following botulinum toxin-A for upper limb activity in chronic stroke.
Methods—
We conducted a multicenter phase III randomized trial with concealed allocation, blinded measurement, and intention-to-treat analysis. One hundred forty stroke survivors who were scheduled to receive botulinum toxin-A in any muscle(s) that cross the wrist because of moderate to severe spasticity after a stroke >3 months ago, who had completed formal rehabilitation and had no significant cognitive impairment. Experimental group received botulinum toxin-A plus evidence-based movement training while the control group received botulinum toxin-A plus a handout of exercises. Primary outcomes were goal attainment (Goal Attainment Scaling) and upper limb activity (Box and Block Test) at 3 months (end of intervention). Secondary outcomes were spasticity, range of motion, strength, pain, burden of care, and health-related quality of life.
Results—
In terms of goal attainment, the experimental group scored the same (mean difference, 2 T-score [95% CI, −2 to 7]) as the control group on the Goal Attainment Scale. In terms of upper limb activity, by 3 months the experimental group moved blocks at the same speed (mean difference, 0.00 blocks/s [95% CI, −0.02 to 0.01]) as the control group on the Box and Block Test. There were no differences between groups on any secondary outcome except strength, in favor of the experimental group (mean difference, 1.4 kg [95% CI, 0.2–2.7]).
Conclusions—
Findings suggest that additional intensive upper limb rehabilitation following botulinum toxin-A in chronic stroke survivors with a disabled upper limb is not effective.
Registration—
URL: https://www.clinicaltrials.gov. Unique identifier: ACTRN12615000616572.
Stroke remains a leading cause of major disability internationally and represents a large economic burden on the health care system.1 A meta-analysis has shown that botulinum toxin-A injections reduce spasticity compared with placebo,2 but that this reduction in spasticity does not carry over to an improvement in the ability to perform everyday activities.3,4 Clinical guidelines internationally recommend that management of spasticity include the use of botulinum toxin-A in conjunction with ongoing rehabilitation.5,6 However, this recommendation is based on expert opinion rather than scientific evidence, since there are no sufficiently powered randomized trials which compare the effect of botulinum toxin-A to those of botulinum toxin-A plus comprehensive rehabilitation.4,5 Our Phase II trial investigating the feasibility of additional rehabilitation to botulinum toxin-A demonstrated that rehabilitation can be provided to stroke survivors receiving botulinum toxin-A.7 This pilot study clearly showed that future trials should be performed separately in the upper and lower limb, due to difficulties in finding measures of activity that encompass both limbs.
Difficulty in moving the arm is a common, ongoing problem for around two-thirds of people poststroke.8 After formal rehabilitation ceases, people with persistent spasticity due to their stroke still attend clinics where they may receive botulinum toxin-A injections in the upper limb, particularly into muscles of the forearm and hand.9,10 Thereafter, postinjection intervention varies widely due to a lack of evidence, and in Australia, around one third of clinics only provide handouts or advice to encourage motor training9 in the absence of supervised therapy. Therefore, we designed an intensive upper limb rehabilitation program based on evidence-based guidelines for stroke5,6 that was to be provided postinjection. The 3-month program, known as InTENSE (Intensive Therapy Efficacy After Neurological Spasticity Treatment), includes 2 weeks of serial casting aimed at decreasing any contracture11 that is then followed by 10 weeks of movement training, aimed at decreasing weakness12 and improving movement.13,14 The program was designed to be patient-driven; it is mostly performed at home supported by phone calls, home visits, and occasional attendance at the clinic, and its feasibility has been tested in a Phase II trial.7
The aim of this Phase III randomized trial was to determine both the clinical effect and the cost-benefit of additional intensive upper limb rehabilitation following botulinum toxin-A. The specific research question was:
In stroke survivors attending a spasticity clinic who are scheduled to receive botulinum toxin-A, is additional 3 months of evidence-based movement training more effective than botulinum toxin-A plus usual care in terms of goal attainment and upper limb activity?
Methods
The data that support the findings of this study are available from the corresponding author on reasonable request. The protocol was published,15 approved by the relevant Human Research Ethics Committees and was registered.
Design
The InTENSE trial was a national, multicenter, Phase III randomized trial with concealed allocation, blinded measurement, and intention-to-treat analysis. Stroke survivors were recruited from 7 spasticity clinics across 3 states in Australia. The list of clinics is available on the trial registry. Participants were randomly allocated to receive botulinum toxin-A plus evidence-based movement training or botulinum toxin-A plus usual care. Randomization was computer-generated, independent, and concealed. For each clinic, allocation occurred in random permuted blocks so that after every block (of 4–8 participants), the experimental and control group contained equal numbers. Randomization occurred after injection of botulinum toxin-A. The schedule was stored off-site, and group allocation was revealed online. Outcomes were measured at baseline, 3 months (end of intervention), and 12 months (beyond the intervention). Measurements were collected at the clinic by researchers blind to group allocation. It was not possible to blind participants or therapists to group allocation. Data analyses were conducted by researchers blind to group allocation.
Patients, Therapists, and Clinics
Patients were included if they were adults over 3 months poststroke; were scheduled to receive a botulinum toxin-A injection (in accordance with the Pharmaceutical Benefits Scheme) to a muscle(s) that crosses the wrist; and were not currently receiving upper limb rehabilitation. They were excluded if they had botulinum toxin-A injections and casting in the past 6 months; had contraindications to botulinum toxin-A injections; had other nonstroke related upper limb conditions (eg, fracture, frozen shoulder, and arthritis); had impaired cognition (≥5 errors on the Short Portable Mental Status Questionnaire16); or were unable to attend clinic ≥1/wk. Information such as age, sex, education level, living situation, time since stroke, side of hemiplegic, cognition, sensation, neglect were collected to describe the sample.
Therapists delivering the intervention were included if they were experienced physical or occupational therapists with ≥3 years of experience in stroke rehabilitation.
Spasticity clinics were included if they had a stroke throughput of ≥20/y.
Intervention
Participants in both groups underwent a standard injection program according to Australian practice recommendations.17 Structured goal setting with participants and their carers was completed within the spasticity clinic and identified areas of concern specific to upper limb activity. Rehabilitation physicians selected the muscle(s) for injection before inclusion in the trial depending on these goals and the distribution of the spasticity. Participants received an injection to a muscle(s) crossing the wrist (such as Flexor Digitorum Profundus, Flexor Digitorum Superficialis, Extensor Digitorum, Extensor Digiti Minimi, Flexor Pollicus Longus, Flexor Carpi Radialis, Flexor Carpi Ulnaris, Palmaris Longus, Extensor Carpi Radialis Longus, Extensor Carpi Radialis Brevis, and Extensor Carpi Ulnaris). Botulinum toxin-A were supplied to participants through the Pharmaceutical Benefits Scheme,18 and the maximum dose of at any 1-time point was 600 units (maximum volume per site =0.5–1.0 mL). The trial used one neurotoxin, Botox (100 unit vial), which has approval for upper limb spasticity after stroke. Muscles injected and units per muscle were recorded.
Participants in the experimental group received the InTENSE program immediately after the botulinum toxin-A injection. The program commenced with up to 3 serial casts applied to place the wrist in maximum extension for 2 weeks. This was then followed by 10 weeks of movement training aimed at decreasing weakness (electrical stimulation and progressive resistance exercises)14 and improving active movement.14,19 There were 4 levels of movement training (level 0–3) to allow training to be individualized for each participant’s ability. Participants were encouraged to practice for 60 minutes per day, 7 days a week during the 10 weeks (ie, ≈70 hours in total). Participants were supported by a mix of clinic-based sessions, home visits, and phone calls. Clinic-based sessions were conducted by a physical or occupational therapist, who received training. In addition, participants received an individualized manual outlining their movement training and were required to record the number of minutes of practice daily in a training log. The intervention package is described in detail and according to the template for intervention description and replication (TIDieR) checklist (Table I in the online-only Data Supplement). Adherence to the experimental intervention was monitored by reviewing the training logs and by auditing 1 to 2 sessions per clinic.
Participants in the control group received a handout plus one follow-up telephone call to encourage independent practice. The handout was nonindividualized and contained 7 stretches and 8 arm and hand exercises. They were also required to record the number of minutes of practice daily in a training log. Contamination from the experimental intervention was determined by examining the training logs at the beginning and end of the study.
Participant acceptability was determined by response to the closed question “If you ever have further treatment for spasticity, would you opt to receive the same treatment/s.”
Outcome Measures
The primary outcomes were goal attainment measured using the Goal Attainment Scale20,21 and reported as a T-score, and upper limb activity measured using the Box and Block Test22 and reported as blocks/s.
Secondary outcomes were spasticity, wrist extension range of motion, grip strength, pain, burden of care, and quality of life. Spasticity was measured using the Tardieu Scale and reported as a score 0 to 4, where 0 is no spasticity.23 Passive range of wrist extension was measured using torque-controlled goniometry and reported in degrees.24 Grip strength was measured as a maximum voluntary contraction using a Jamar dynamometer and reported as kilogram.25 Pain was measured using a visual analog scale and reported in centimeter from 0 to 10, where 0 is no pain. Burden of care was measured using the Carer Burden Scale and reported as a score 0 to 16, where 0 is no burden.26 Health-related quality of life was measured using the EuroQol-5D.27 The domain of self-care is reported as a value between 1 and 3 where 1 is no problems, and overall health as a value between 0 and 100, where 0 is poor health.
Statistical Analyses
Sample size was calculated to detect a between-group difference of 7 points on the Goal Attainment Scale T-score and 0.12 blocks/s on the Box and Block test with 80% power at a 2-tailed significance level of 0.05. The calculation was based on the mean scores and standard deviations of the sample studied in our pilot trial,7 and the accepted clinically important differences of the Goal Attainment Scale (ie, one level improvement on one goal)27 and Box and Block test (ie, 6 blocks).28 On the basis of 10% attrition by 12 months, we planned to recruit a total of 136 participants, 68 per group.
An intention-to-treat analysis was conducted. Outcomes were analyzed using ANCOVA, controlling for baseline values, and presented as mean between-group differences (95% CI).
Results
Flow of Participants Through the Trial
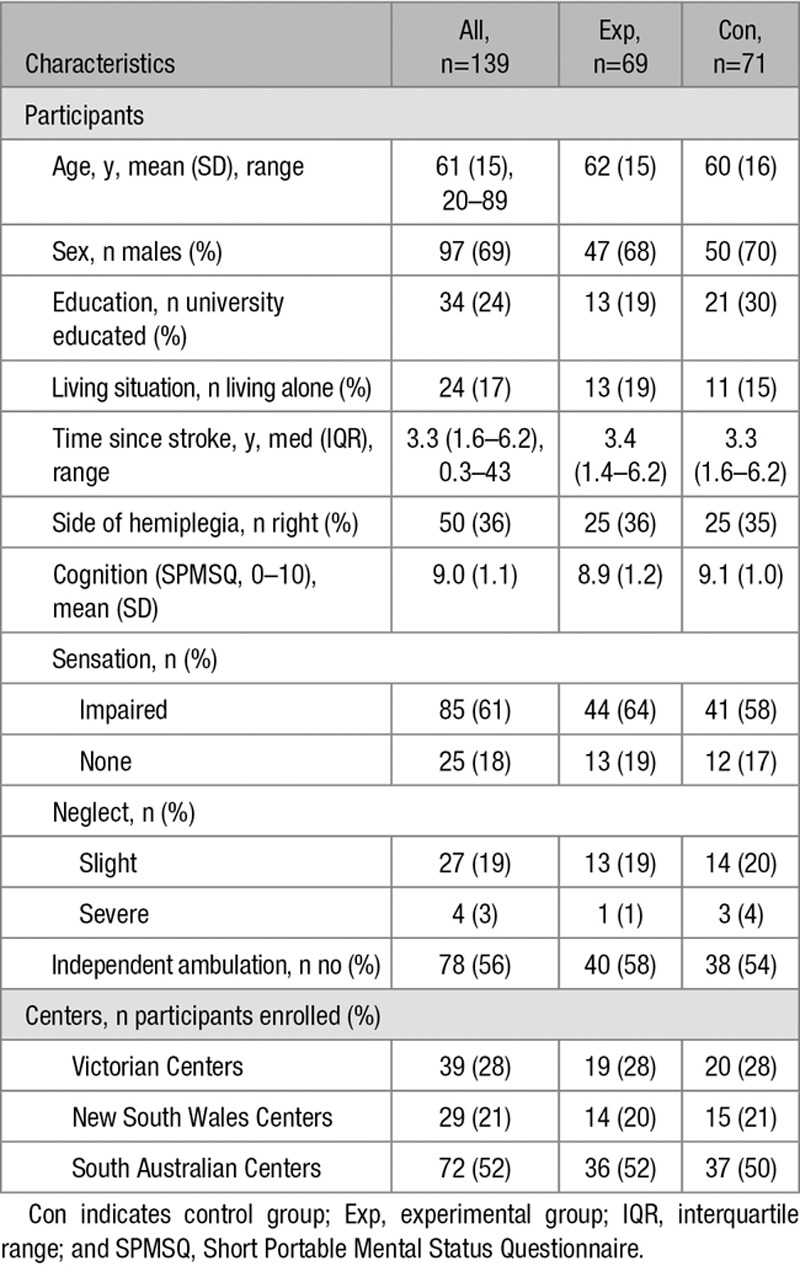
One hundred forty people with stroke were recruited to the study. Participants in both the experimental and control groups were similar in terms of their age, sex, level of education, previous living arrangements as well as chronicity, side of hemiplegia, cognition, sensation, and neglect (Table 1).
Table 1.
Characteristics of Participants and Centers
The flow of participants through the trial is shown in Figure. By Month 3, 2 participants (1%) were lost to follow-up—both from the experimental group. Therefore, 99% of the primary outcomes were collected. In addition, there was some missing data so that 99% of secondary data was collected.
Figure.
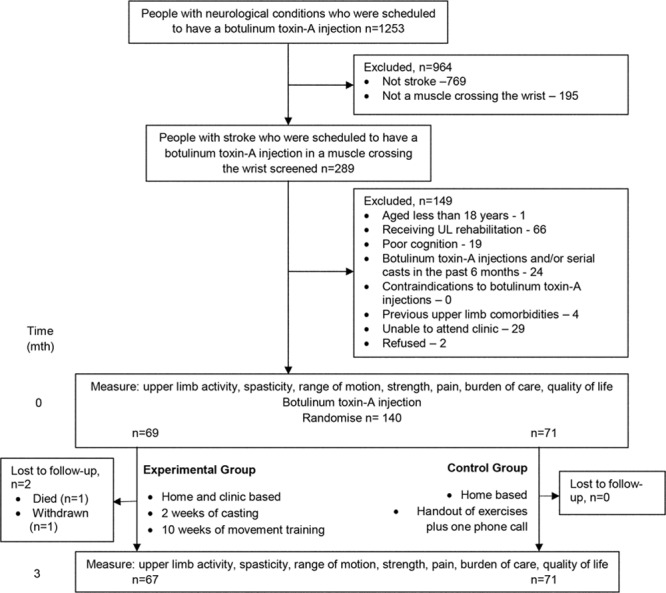
Design of and flow of participants through the study.
Sixteen therapists (4 physiotherapists and 12 occupational therapists) delivered the experimental intervention to a mean of 4.2 (SD 3.4) participants each. On average, they had 13 (SD 10) years of clinical experience in stroke rehabilitation, and 5 (30%) had postgraduate qualifications.
Participants were recruited from 7 spasticity clinics that treated mixed neurological conditions with an average throughput of 26 (SD 12) strokes per clinic per year.
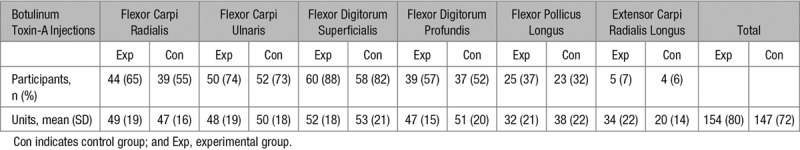
Compliance With Trial Method
Both groups received botulinum toxin-A injections and the muscles injected and the units per muscle for both groups are outlined in Table 2. The number of muscles injected was similar between groups, with the most common muscles being Flexor Digitorum Superficialis and Flexor Carpi Ulnaris. Similarly, the amount botulinum toxin-A used was similar between groups, averaging about 150 units in total. Both groups kept a log to record the content and daily number of minutes of practice. At the beginning (week 3), the experimental group did 52 (SD 21) min/d of practice and ended (week 12) with 37 (SD 28) min/d. At beginning (week 3), the control group did 28 (SD 25) min/d of practice and ended (week 12) at 20 (SD 22) min/d. The control group did less practice at the end than at the beginning suggesting that there was no contamination from the experimental intervention.
Table 2.
Summary of Botulinum Toxin-A Injections
In terms of the experimental intervention, the experimental group received 3.0 (SD 0.3, range 2–4) casts over 2 weeks. At the beginning of movement training (week 3), they started at level 0.7 (SD 0.8) and ended (week 12) at level 0.9 (SD 1.0), suggesting little progression from the level 0 electrical stimulation program across the course of the study. The data is skewed because most participants started (60%) and ended (55%) at level 0. Adherence to the experimental intervention was monitored by auditing 2 sessions per clinic, and the only deviations from protocol that were found involved data collection and storage.
Participant acceptability was determined by response to the closed question “If you ever have further treatment for spasticity, would you opt to receive the same treatment/s”. Eighty percent of the experimental group said yes, compared with 70% of control group.
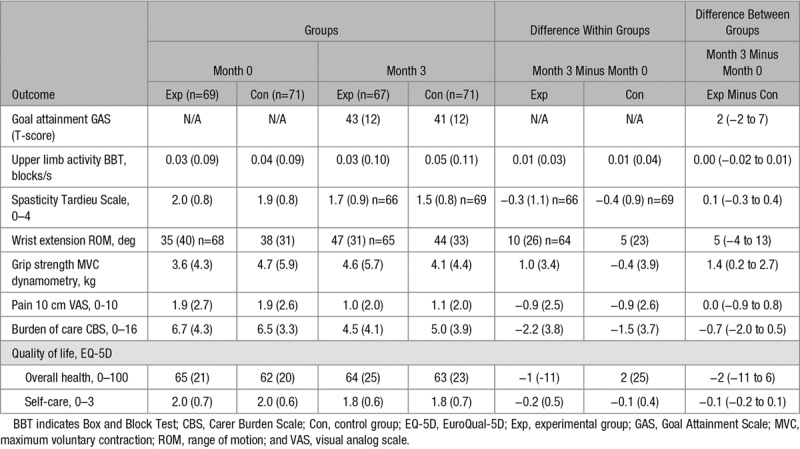
Effect of Intervention Between Groups
Group (SD) data for the 2 measurement occasions, within-group differences and between-group differences are presented in Table 3 for all outcome measures. In terms of goal attainment, the experimental group scored the same (MD, 2 T-score [95% CI, −2 to 7]) as the control group on the Goal Attainment Scale. In terms of upper limb activity, by 3 months the experimental group moved blocks at the same speed (MD blocks/s [95% CI, −0.02 to 0.01]) as the control group on the Box and Block Test. In terms of the secondary outcomes, the experimental group was 1.4 kg (95% CI, 0.2–2.7) stronger in grip strength than the control group. There was no difference between groups in any other measure.
Table 3.
Mean (SD) of Groups, Mean (SD) Difference Within Groups, and Mean (95% CI) Difference Between Groups for All Outcomes
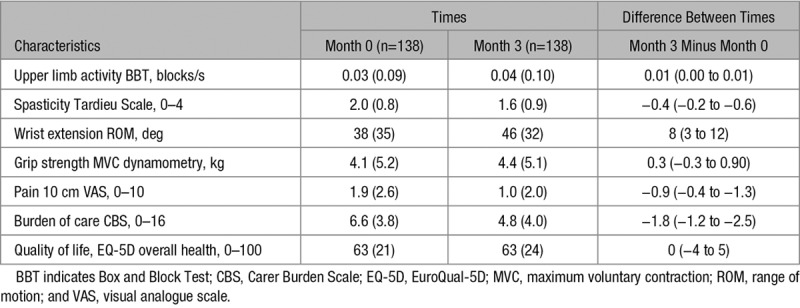
Post Hoc Analysis of Effect of Intervention on Combined Group
When the experimental and control groups were combined into one group (Table 4), there was a statistically significant improvement in upper limb activity (MD, 0.01 blocks/s [95% CI, 0.00–0.01]), spasticity (MD, −0.4 out of 4 [95% CI, −0.2 to −0.6]), contracture (MD, 8 deg [95% CI, 3–12]), pain (MD, −0.9 out of 10 [95% CI, −0.4 to −1.3), and burden of care (MD, −1.8 out of 16 [95% CI, −1.2 to −2.5]).
Table 4.
Mean (SD) of Times and Mean (95% CI) Difference Between Times for All Participants
Discussion
This randomized trial found that, in chronic stroke survivors attending a spasticity clinic who received botulinum toxin-A, additional 3 months of evidence-based movement training was no more effective than botulinum toxin-A plus a handout of exercises in terms of goal attainment and upper limb activity. There was no difference between groups in any other measure, except strength, where evidence-based movement training was effective in terms of grip strength. When the experimental and control groups were combined, overall, there were small improvements in spasticity, contracture, pain, and burden of care (such as cleaning the palm, cutting the fingernails, dressing the arm, and cleaning under the armpit).
The participants in this randomized trial were chronic stroke survivors attending a spasticity clinic who were scheduled to receive botulinum toxin-A to a muscle crossing the wrist. They were representative of stroke survivors receiving intervention for spasticity in terms of chronicity and severity.29 The majority (60%) of stroke survivors attending a spasticity clinic had a muscle crossing the wrist injected, and half of these were enrolled in our trial. However, the participants were very disabled in terms of upper limb activity. On average, they could move 2 blocks in 60 s compared with normal age-matched performance of 70.22 Furthermore, over 3 quarters (78%) of them could not move any blocks, and over a quarter (29%) had no grip strength at all. Since a systematic review has concluded that overall, more severe impairment and activity limitations in the upper limb early after stroke are significantly associated with poor upper limb outcomes,30 it is quite likely that many of our participants did not have an intact corticospinal tract, indicating limited potential for meaningful recovery.31 Perhaps, therefore, it is not surprising that there was little response to the motor training.
Clinical guidelines internationally recommend that management of spasticity include ongoing rehabilitation after botulinum toxin-A.5,6,17 Since undertaking this randomized trial, there has one systematic review published that examines the effect of adjunct therapy following botulinum toxin-A.3 However, there is no meta-analysis performed in this review, and none of the randomized trials included in the review were published after our trial was begun. Therefore, the status quo remains that the recommendation included in most guidelines is based on expert opinion rather than scientific evidence, since there are no sufficiently powered randomized trials which compare the effect of botulinum toxin-A to those of botulinum toxin-A plus comprehensive rehabilitation. Our findings show that this expert opinion is fallible, and raises the question of whether consensus recommendations should be included in stroke guidelines.
This trial has both strengths and weaknesses. Its main strength was that it was fully powered, and participants were representative of those attending spasticity clinics around Australia and internationally29 in terms of time poststroke, muscles injected, and types of goals set. While this study’s main weakness was that the participants, while representative, were some 3 years after their stroke and very disabled, which means that they may not have been able to make improvements in upper limb activity. Another strength was the high adherence to the practice regime, suggesting that the findings are not due to lack of practice. While self-reports of practice have been found to be variable,32 analysis of a sub-group of our sample showed a high degree of accuracy.33 The experimental group was required to undertake 60 minutes of practice per day. They began the trial practicing 87% of the required amount and ended practicing 62% despite the fact that there was very little visible improvement. This suggests that the protocol of clinic-based sessions (20%), supported by home visits, phone calls and individualized manual outlining the movement training and a training log to record the number of minutes of practice daily is highly effective at getting people to practice, at least within a trial.
The findings of this randomized trial suggest that it is not worthwhile to spend resources on providing anything more than a nonindividualized handout plus a phone call to encourage practice after botulinum toxin-A. However, translation of this into practice will require explanation for stroke survivors, who may hold a belief that their upper limb function will improve if they are given more therapy. Interestingly, when the participants of both groups were considered together, the findings raise the question of whether there is enough benefit from the application of botulinum toxin-A itself. In this group of stroke survivors who were representative of those who attend spasticity clinics in Australia, while there was a half-point reduction in spasticity, there was no clinically important improvement in upper limb activity, and little change in range of motion, strength, pain, or burden of care, and no change in quality of life. The findings also raise the question of the timing of botulinum toxin-A. To avoid confounders, we only accepted stroke survivors once they were finished with formal rehabilitation. However, it may be more beneficial if botulinum toxin-A was given earlier.34
In conclusion, this randomized trial found that, in stroke survivors attending a spasticity clinic who received botulinum toxin-A to a muscle crossing the wrist, additional 3 months of evidence-based movement training was no more effective than botulinum toxin-A plus a handout of exercises, in terms of goal attainment and upper limb activity. This suggests that, in chronic, severely disabled stroke survivors who are not already receiving upper limb movement therapy, it is not worthwhile spending resources on commencing intensive upper limb rehabilitation after botulinum toxin-A. On the positive side, we have identified a group who will not benefit from extra intervention, therefore stroke survivors with greater activity, or who are earlier in the trajectory, or with higher baseline pain may benefit more from evidence-based movement training. In addition, we have shown that the structure of training in this trial and the expectation for self-management resulted in a high amount of independent practice of motor activity.
Acknowledgments
Drs Lannin and Crotty conceived the study; Drs Lannin, Ada, and Ratcliffe designed the analysis; Drs Lannin, Ada, English, Ratcliffe, and Crotty designed the study and procured funding; Dr Crotty, S. Faux, M. Palit, S. Gonzalez, and J. Olver were site principal investigators and oversaw site recruitment and site data collection; Dr Cameron oversaw data safety and monitoring; Drs Lannin and Ada performed the analysis and drafted the article; and all authors have read and approved the final article.
Sources of Funding
The study was supported by a project grant from the National Health and Medical Research Council, Australia (NHMRC; GNT1079542). Drs Lannin and English are supported by the National Heart Foundation of Australia (NAL: GN102055; CE: GN101177). Sponsors were not involved in the design, execution, analysis, and interpretation or reporting of the results.
Disclosures
J. Olver and S. Gonzalez declare that they have received honoraria from Allergan; J. Olver, M. Palit, and S. Gonzalez declare that they have received honoraria from Ipsen; and S. Gonzalez declares he has also received honoraria from Merz. The other authors report no conflicts.
Supplementary Material
Appendix
InTENSE Trial Group: Natasha A. Lannin, Julie Ratcliffe, Louise Ada, Coralie English, Maria Crotty, Ian D Cameron, Steven G. Faux, Mithu Palit, John Olver, Malcolm Bowman, Senen Gonzalez, Rachel Milte, Angela Vratsistas-Curto, Annabel McNamara, Christine Shiner, Elizabeth Lynch, Emma Schneider, Louise Beaumont, Maggie Killington, Megan Coulter, Doungkamol Sindhusake, Brian Anthonisz, Hong Mei Khor, Justin Tan, Kwong Teo, Lily Ng, Lydia Huang, Maria Paul, Neil Simon, Nidhi Gupta, Rebecca Martens, Sam Bolitho, Shea Morrison, Sue Hooper, Yan Chow, Yuriko Watanabe, Adrian Cowling, Clara Flu, Debbie Edwards, Emily Toma, Genevieve Hendrey, Jacinta Sheehan, Josh Butler, Judith Hocking, Lauren Rutzou, Megan White, Michael Snigg, Rhiannon Hughes, Sarah Sweeney, Sophie Flint, Tam Levy, Val Bramah, Cameron Lathlean, Carrie McCallum, Elaine Chui, Frances Allan, Heather Webber, Jenna Cameron, Jo Campbell, Julie Lawson, Kalavani Zenouith, Karen Borschmann, Katelyn Moloney, Laura Jolliffe, Lisa Cameron, Owen Howlett, Rebecca Nicks, and Sophie O’Keefe.
Footnotes
A list of all InTENSE Trial Group participants is given in the Appendix.
Presented in part at the Annual Scientific Meeting of the Stroke Society of Australasia, Canberra, Australia, September 10–13, 2019.
The online-only Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/STROKEAHA.119.027602.
References
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2019 update: a Report From the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Cardoso E, Rodrigues B, Lucena R, Oliveira IR, Pedreira G, Melo A. Botulinum toxin type A for the treatment of the upper limb spasticity after stroke: a meta-analysis. Arq Neuropsiquiatr. 2005;63:30–33. doi: 10.1590/s0004-282x2005000100006. doi: 10.1590/s0004-282x2005000100006. [DOI] [PubMed] [Google Scholar]
- 3.Mills PB, Finlayson H, Sudol M, O’Connor R. Systematic review of adjunct therapies to improve outcomes following botulinum toxin injection for treatment of limb spasticity. Clin Rehabil. 2016;30:537–548. doi: 10.1177/0269215515593783. doi: 10.1177/0269215515593783. [DOI] [PubMed] [Google Scholar]
- 4.Kinnear BZ, Lannin NA, Cusick A, Harvey LA, Rawicki B. Rehabilitation therapies after botulinum toxin-A injection to manage limb spasticity: a systematic review. Phys Ther. 2014;94:1569–1581. doi: 10.2522/ptj.20130408. doi: 10.2522/ptj.20130408. [DOI] [PubMed] [Google Scholar]
- 5.Sheean G, Lannin NA, Turner-Stokes L, Rawicki B, Snow BJ Cerebral Palsy Institute. Botulinum toxin assessment, intervention and after-care for upper limb hypertonicity in adults: international consensus statement. Eur J Neurol. 2010;17(suppl 2):74–93. doi: 10.1111/j.1468-1331.2010.03129.x. doi: 10.1111/j.1468-1331.2010.03129.x. [DOI] [PubMed] [Google Scholar]
- 6.Stroke Foundation. Clinical guidelines for stroke management. Available at: https://informme.org.au/en/Guidelines/Clinical-Guidelines-for-Stroke-Management. Accessed September 5, 2019.
- 7.Lannin NA, Ada L, Levy T, English C, Ratcliffe J, Sindhusake D, et al. Intensive therapy after botulinum toxin in adults with spasticity after stroke versus botulinum toxin alone or therapy alone: a pilot, feasibility randomized trial. Pilot Feasibility Stud. 2018;4:82. doi: 10.1186/s40814-018-0276-6. doi: 10.1186/s40814-018-0276-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kwakkel G, Kollen B. Predicting improvement in the upper paretic limb after stroke: a longitudinal prospective study. Restor Neurol Neurosci. 2007;25:453–460. [PubMed] [Google Scholar]
- 9.Cusick A, Lannin N, Kinnear BZ. Upper limb spasticity management for patients who have received botulinum toxin A injection: Australian therapy practice. Aust Occup Ther J. 2015;62:27–40. doi: 10.1111/1440-1630.12142. doi: 10.1111/1440-1630.12142. [DOI] [PubMed] [Google Scholar]
- 10.Bakheit AM, Zakine B, Maisonobe P, Aymard C, Fhedoroff K, Hefter H, et al. The profile of patients and current practice of treatment of upper limb muscle spasticity with botulinum toxin type A: an international survey. Int J Rehabil Res. 2010;33:199–204. doi: 10.1097/MRR.0b013e328332f5e0. doi: 10.1097/MRR.0b013e328332f5e0. [DOI] [PubMed] [Google Scholar]
- 11.Scott H, Lannin NA, English C, Ada L, Levy T, Hart R, et al. Addition of botulinum toxin type A to casting may improve wrist extension in people with chronic stroke and spasticity: a pilot double-blind randomized trial. Edorium J Disabil Rehabil. 2017;3:30–35. [Google Scholar]
- 12.Ada L, Dorsch S, Canning CG. Strengthening interventions increase strength and improve activity after stroke: a systematic review. Aust J Physiother. 2006;52:241–248. doi: 10.1016/s0004-9514(06)70003-4. doi: 10.1016/s0004-9514(06)70003-4. [DOI] [PubMed] [Google Scholar]
- 13.Shaw L, Rodgers H, Price C, van Wijck F, Shackley P, Steen N, et al. BoTULS Investigators. BoTULS: a multicentre randomised controlled trial to evaluate the clinical effectiveness and cost-effectiveness of treating upper limb spasticity due to stroke with botulinum toxin type A. Health Technol Assess. 2010;14:1,iii–113, iii. doi: 10.3310/hta14260. doi: 10.3310/hta14260. [DOI] [PubMed] [Google Scholar]
- 14.Harris JE, Eng JJ, Miller WC, Dawson AS. A self-administered Graded Repetitive Arm Supplementary Program (GRASP) improves arm function during inpatient stroke rehabilitation: a multi-site randomized controlled trial. Stroke. 2009;40:2123–2128. doi: 10.1161/STROKEAHA.108.544585. doi: 10.1161/STROKEAHA.108.544585. [DOI] [PubMed] [Google Scholar]
- 15.Lannin NA, Ada L, English C, Ratcliffe J, Crotty M. Effect of adding upper limb rehabilitation to botulinum toxin-A on upper limb activity after stroke: protocol for the InTENSE trial. Int J Stroke. 2018;13:648–653. doi: 10.1177/1747493018765228. doi: 10.1177/1747493018765228. [DOI] [PubMed] [Google Scholar]
- 16.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 17.Australasian Faculty of Rehabilitation Medicine. Position Statement on the Therapeutic Use of Botulinum Toxin in Rehabilitation Medicine for Spasticity and Dystonia. Sydney, Australia: Australasian Faculty of Rehabilitation Medicine; 2013. [Google Scholar]
- 18.Pharmaceutical Benefits Scheme (PBS) Section 100 – Highly Specialised Drugs Program. Available at: http://www.pbs.gov.au/info/browse/section-100/s100-highly-specialised-drugs. Accessed September 5, 2019.
- 19.Howlett OA, Lannin NA, Ada L, McKinstry C. Functional electrical stimulation improves activity after stroke: a systematic review with meta-analysis. Arch Phys Med Rehabil. 2015;96:934–943. doi: 10.1016/j.apmr.2015.01.013. doi: 10.1016/j.apmr.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 20.Kiresuk TJ, Smith A, Cardillo JE. Goal Attainment Scaling: Applications, Theory, and Measurement. London, UK: Taylor & Francis; 2014. [Google Scholar]
- 21.Turner-Stokes L, Baguley IJ, De Graaff S, Katrak P, Davies L, McCrory P, et al. Goal attainment scaling in the evaluation of treatment of upper limb spasticity with botulinum toxin: a secondary analysis from a double-blind placebo-controlled randomized clinical trial. J Rehabil Med. 2010;42:81–89. doi: 10.2340/16501977-0474. doi: 10.2340/16501977-0474. [DOI] [PubMed] [Google Scholar]
- 22.Mathiowetz V, Volland G, Kashman N, Weber K. Adult norms for the box and block test of manual dexterity. Am J Occup Ther. 1985;39:386–391. doi: 10.5014/ajot.39.6.386. doi: 10.5014/ajot.39.6.386. [DOI] [PubMed] [Google Scholar]
- 23.Patrick E, Ada L. The Tardieu Scale differentiates contracture from spasticity whereas the Ashworth Scale is confounded by it. Clin Rehabil. 2006;20:173–182. doi: 10.1191/0269215506cr922oa. doi: 10.1191/0269215506cr922oa. [DOI] [PubMed] [Google Scholar]
- 24.Ada L, Herbert R. Measurement of joint range of motion. Aust J Physiother. 1988;34:260–262. [Google Scholar]
- 25.Boissy P, Bourbonnais D, Carlotti MM, Gravel D, Arsenault BA. Maximal grip force in chronic stroke subjects and its relationship to global upper extremity function. Clin Rehabil. 1999;13:354–362. doi: 10.1191/026921599676433080. doi: 10.1191/026921599676433080. [DOI] [PubMed] [Google Scholar]
- 26.Bhakta BB. Management of spasticity in stroke. Br Med Bull. 2000;56:476–485. doi: 10.1258/0007142001903111. doi: 10.1258/0007142001903111. [DOI] [PubMed] [Google Scholar]
- 27.Eftekhar P, Mochizuki G, Dutta T, Richardson D, Brooks D. Goal attainment scaling in individuals with upper limb spasticity post stroke. Occup Ther Int. 2016;23:379–389. doi: 10.1002/oti.1440. doi: 10.1002/oti.1440. [DOI] [PubMed] [Google Scholar]
- 28.Connell LA, Tyson SF. Clinical reality of measuring upper-limb ability in neurologic conditions: a systematic review. Arch Phys Med Rehabil. 2012;93:221–228. doi: 10.1016/j.apmr.2011.09.015. doi: 10.1016/j.apmr.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 29.Turner-Stokes L, Fheodoroff K, Jacinto J, Maisonobe P, Zakine B. Upper limb international spasticity study: rationale and protocol for a large international, multicentre prospective cohort study investigating management and goal attainment following treatment with botulinum toxin-A in real-life clinical practice. BMJ Open. 2013;3:e002230. doi: 10.1136/bmjopen-2012-002230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coupar F, Pollock A, Rowe P, Weir C, Langhorne P. Predictors of upper limb recovery after stroke: a systematic review and meta-analysis. Clin Rehabil. 2012;26:291–313. doi: 10.1177/0269215511420305. doi: 10.1177/0269215511420305. [DOI] [PubMed] [Google Scholar]
- 31.Stinear CM, Byblow WD, Ackerley SJ, Smith MC, Borges VM, Barber PA. PREP2: a biomarker-based algorithm for predicting upper limb function after stroke. Ann Clin Transl Neurol. 2017;4:811–820. doi: 10.1002/acn3.488. doi: 10.1002/acn3.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi: 10.1186/1479-5868-5-56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Levy T, Killington M, Lannin N, Crotty M. Viability of using a computer tablet to monitor an upper limb home exercise program in stroke. Physiother Theory Pract. 2019:1–11. doi: 10.1080/09593985.2019.1625092. doi: 10.1080/09593985.2019.1625092. [DOI] [PubMed] [Google Scholar]
- 34.Rosales RL, Efendy F, Teleg ES, Delos Santos MM, Rosales MC, Ostrea M, et al. Botulinum toxin as early intervention for spasticity after stroke or non-progressive brain lesion: a meta-analysis. J Neurol Sci. 2016;371:6–14. doi: 10.1016/j.jns.2016.10.005. doi: 10.1016/j.jns.2016.10.005. [DOI] [PubMed] [Google Scholar]


