Abstract
Forearm fractures are very common orthopaedic injuries in children. Most of these fractures are forgiving due to the unique and excellent remodelling capacity of the juvenile skeleton. However, significant evidence stating the limits of acceptable angulations and taking functional outcome into consideration is scarce. The aim of this study is, therefore, to get a first impression of the remodelling capacity in nonreduced paediatric forearm fractures based on radiological and functional outcome. Children aged 0–14 years with a traumatic angular deformation of the radius or both the radius and ulna, treated conservatively without reduction, were included in this prospective cohort study. Radiographs were taken and functional outcome was assessed at five fixed follow-up appointments throughout a period of one year. Outcome measurements comprised radiographic angular alignment, grip strength and wrist mobility. A total of 26 children (aged 3–13 years) with a traumatic angulation of the forearm were included. Mean dorsal angulation at the time of presentation amounted to 12° (5–18) and diminished after one year to a mean angulation of 4° (0–13). Grip strength, pronation and supination were significantly diminished compared to the unaffected hand up to 6 months after injury. After one year, no significant differences in function between the affected and the unaffected arm were found. Nonreduced angulated paediatric forearm fractures have the potential to remodel in time and have good radiographic and functional outcome one year after trauma, where pronation and grip strength take the longest to recover.
Keywords: angulation, conservative treatment, functional outcome, grip strength, paediatric forearm fractures, remodelling
Introduction
Fractures of the forearm are very common in children and account for more than 30% of all paediatric fractures [1–3]. Angularly deformed forearm fractures are traditionally treated by closed reduction followed by cast immobilisation. Surgical stabilisation is increasingly used as a treatment option, probably due to a relatively high failure rate in the sometimes unpredictable outcome of conservative treatment [4–6]. Redisplacement is the most common complication, especially in primary dislocated forearm fractures (21–40%) [7,8]. Redisplacement or secondary worsening of angulation can be prevented by surgical intervention using percutaneous pinning, intramedullary nailing or plate fixation, which gives maximum stability and the benefit of regaining proper alignment. Fortunately, not all fractures are unstable and require surgical stabilisation since juvenile bone has the unique potency to remodel [9,10]. There is little evidence supporting guidelines on angular acceptance [11]. The uncertainty of predicting fracture stability and the remodelling potential in forearm fractures hinders making a considered decision between conservative and surgical treatment [5,8,12]. Also, there is no convincing literature proving that surgical intervention is superior to conservative treatment in terms of functional outcome [5,8,13].
The limits of acceptable angular deformations are currently based on scarce retrospective studies, case reports and expert opinions [14–16]. Crawford et al. demonstrated that even completely overriding distal radial fractures have the potential to remodel in one year without reduction [17]. On duration of remodelling, both Friberg et al. 1979 and Jeroense et al. found remodelling speed to be faster in larger angulations [15]. This suggests that deformities can remodel in time and result in a normal functional outcome without experiencing the psychological distress of undergoing a surgical procedure, not to mention exposure to anaesthetic and operative risks. Operative risks should not be underestimated, as earlier studies found a complication rate of 14.6% in patients treated with intramedullary nailing [6]. Although research on fracture remodelling is of great importance in clinical decision-making, to our knowledge no prospective studies have been conducted investigating fracture reangulation in time in conservatively treated paediatric forearm fractures as related to function.
The objective of this prospective study is therefore to first get an initial impression of fracture remodelling and functional outcome in nonreduced paediatric forearm fractures, and second to establish which factors influence remodelling and to determine whether functional outcome is correlated with degree of fracture angulation.
Methods
Study design and participants
This prospective single-centre cohort study was conducted at Isala Clinics in Zwolle, the Netherlands. Children and their parents were verbally informed about the study and also received detailed written information. Informed consent was obtained from the parents and from all children aged ≥12 years only if the child was willing to participate. This study is approved by the local Medical Ethical Committee (CCMO NL12576.075.06). Boys (age <14 years) and girls (age <12 years) with a traumatic angular deformity of the radius, confirmed on postero-anterior and lateral radiographs, were included. Fracture types included comprised isolated radius fractures (plastic deformation or complete fracture) and both-bone forearm fractures.
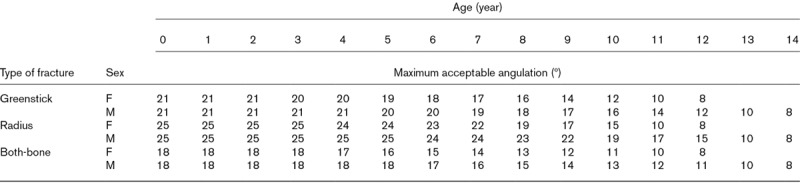
Exclusion criteria were fully ossified physes of the forearm, manipulated fractures, fracture dislocation, apposition and open fractures. Also excluded were polytrauma patients and patients with a bone disease or pathologic fracture. Maximum acceptable angulations according to age were defined according to the Isala Graphs minus one SD, shown in Table 1 [14]. These graphs are based on the outcome of a meta-analysis of existing literature, combined with the opinions of 18 international experts.
Table 1.
Maximum acceptable angulations according to age
Procedures
All fractures were treated with cast immobilisation for 4–6 weeks. On the day of presentation at the hospital (T0), general patient data were collected, including age, gender and hand preference. Patients and their parents were requested to return to the hospital for five follow-up appointments. These sessions were scheduled at 1 week (T1), 4 weeks (T2), 6 weeks (T3), 6 months (T4) and 12 months (T5) postinjury. An optional appointment (T6) was offered when remodelling was delayed.
Data collection
To determine angular alignment, postero-anterior and lateral radiographs were taken at all follow-up sessions. Degree of angulation was defined as the angle between the central longitudinal intramedullary axis of the proximal and the angulated distal fragment as previously described by Hansen et al. (1976) [18] Measurements were taken by two independent observers who were not involved in the treatment (J.J.W.P. and B.B.). The largest angulation at T0 (on the postero-anterior or lateral radiograph) was further observed during follow-up. Additionally, grip strength and passive range of motion of the wrist were tested for both hands at each follow-up appointment, with the exception of T0. Tests were not performed at T0 due to the cast immobilisation. Grip strength measurements were taken using a Jamar hydraulic hand dynamometer (Sammons Preston Rolyan, Chicago). Grip strength was tested twice on both sides and the mean score of the two attempts for each side was used in the analyses. Passive range of motion was measured using a goniometer, and included flexion and extension of the elbow, pronation and supination of the forearm, and palmar and dorsal flexion and ulnar and radial deviation of the wrist.
Statistical analyses
All statistical analyses were conducted using SPSS (version 24.0, SPSS Inc., Chicago). Descriptive statistics were used to describe the main characteristics of the research population and functional outcome parameters. The mean angular deformity as determined by both observers was used in the analyses, as interrater reliability appeared to be excellent (intraclass correlation coefficient 0.98). The Wilcoxon signed-rank test was used to compare grip strength and range of motion of the affected and unaffected hands. A multilevel design was applied, which implies that the follow-up appointments were nested under patients. A multiple regression analysis was performed with fracture angulation as dependent variable. The following factors were tested for association with the above-mentioned variable: time post-injury, dominant arm fractured, type of fracture (plastic deformation or complete fracture) and involvement of the radius or both the radius and ulna. An unconditional growth model will be presented with fracture angulation as dependent variable and time and function tests as independent variables. Results were accepted as significant if P < 0.05.
Results
Patient characteristics
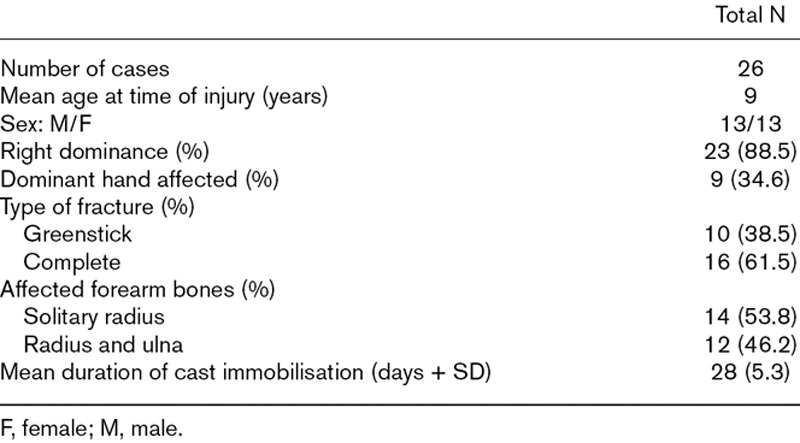
A total of 27 children were enrolled in this study. One child did not show up at the follow-up appointments and was therefore excluded. The final study population comprised 26 children (13 boys), ranging from ages 3.3 to 12.6. Mean age at the time of injury was 9 years (boys: 9.1; girls: 8.9). Of all children, 88.5% were right-hand dominant and 17 fractures (65.4%) affected the nondominant side. In 38.5% the fracture concerned a plastic deformation; 61.5% had a complete fracture (both cortices). This was equally distributed between both sexes. Most boys (61.5%) sustained a both-bone fracture, whereas most girls (69.2%) sustained a solitary radius fracture. All fractures were distally located except in two cases with a midshaft both-bone fracture. All fractures were conservatively treated with cast immobilisation. Mean immobilisation time was 28 days (SD 5.3). The main characteristics of the study population are shown in Table 2.
Table 2.
Characteristics of the study population
Radiographic outcome
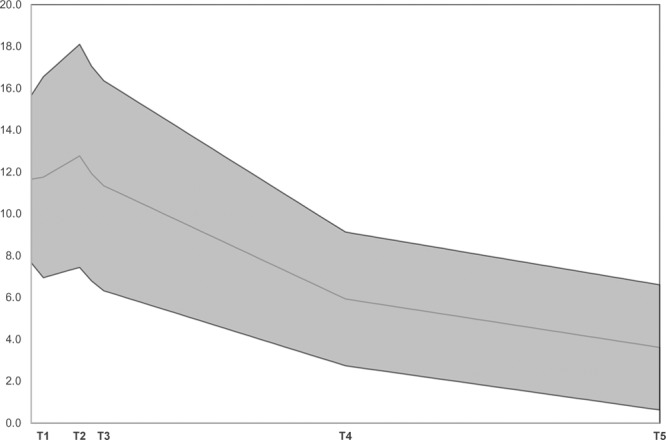
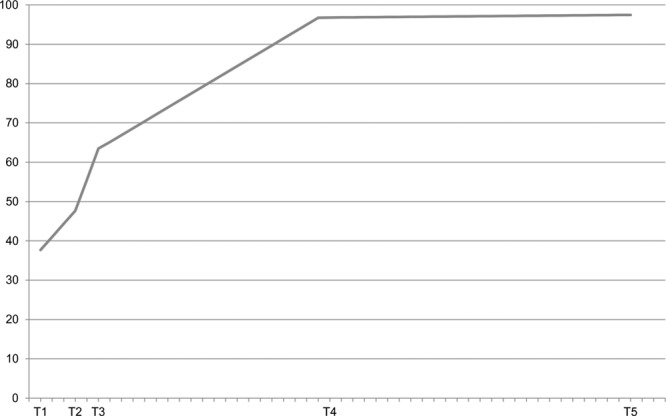
An overview of radiographic outcome is shown in Table 3. All maximum angulations occurred in the sagittal plane. Dorsal angulation occurred in 65.4% of cases. Mean angulation was 11.7° (5.0–18.0) at the day of presentation, 11.8° (4.0–22.5) after 1 week and 12.8° (4.0–22.0) after 4 weeks. Six months after sustaining the fracture, the mean angulation diminished to 6.3° (1.0–10.5) and after 1 year to 3.6° (0.0–13.0), with fracture angulation amounting to less than 5° in 75% of cases. The distribution of fracture angulation is shown in Fig. 1. One outlier remained as a residual angulation of 13° one year postinjury. This concerned a 12-year-old boy with a midshaft both-bone fracture. Because of the remaining angulation, a control radiograph was taken 2.9 years after fracture sustainment. Angulation remained at 11°. Mean angulation and distribution for each follow-up moment is plotted in Fig. 2.
Table 3.
Outcome of fracture angulation
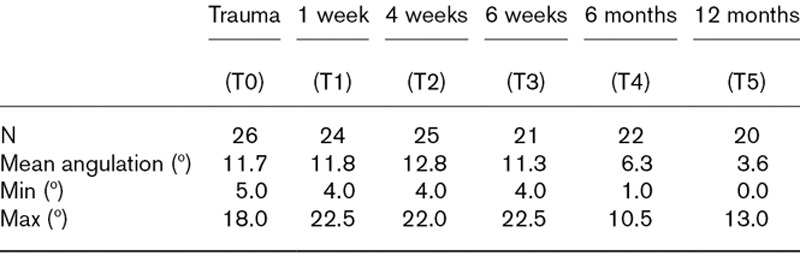
Fig. 1.
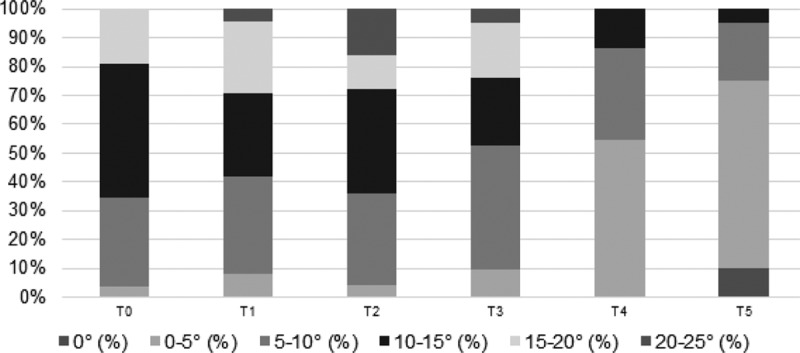
Fracture angulation distribution in % for each follow-up appointment.
Fig. 2.
Mean dorsal angulation (°) and distribution (SD) plotted in time. The line represents the mean dorsal angulation.
Functional outcome
Grip strength
Grip strength is significantly diminished in the affected hand compared to the unaffected hand up to 6 months postinjury (T4). The results show that grip strength is strongly diminished at T1, T2 and T3, and less diminished but still significant at T4. After one year follow-up, grip strength measurements showed no significant difference between the affected and unaffected arm. When describing grip strength of the affected side compared to the unaffected side (%), results show a mean grip strength of 97% at both T4 and T5 (T4: SD 17.6, T5: SD 14.1). An overview of recovery of grip strength is shown in Table 4 and Fig. 3.
Table 4.
Grip strength of affected hand vs. unaffected hand
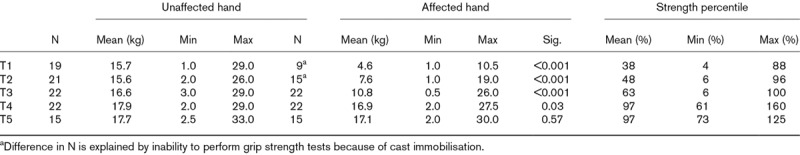
Fig. 3.
Mean grip strength of the affected arm presented as percentage of the unaffected arm.
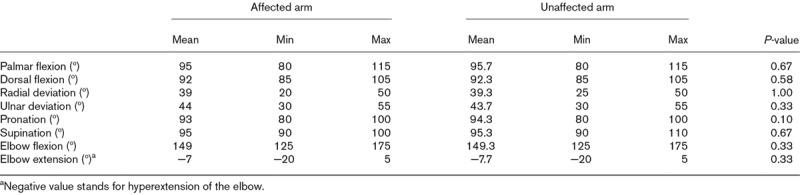
Range of motion
At T2 the affected hand scored significantly lower in all mobility tests, except for extension of the elbow. At T3 the affected hand scored significantly lower in all mobility tests, except for radial deviation. Six months postinjury (T4), only pronation (P ≤ 0.01) and supination (P = 0.03) were significantly diminished in the affected arm.
Range of motion after one year follow-up (T5) showed no statistically significant differences in elbow and wrist motion of the affected arm compared to the unaffected arm (see Table 5). Maximum loss of range of motion at T5 was found to be 10° in radial deviation and pronation.
Table 5.
Range of motion after 1-year follow-up
Factors affecting remodelling
A multiple regression analysis with fracture angulation as dependent variable shows that fracture angulation significantly diminishes in time (adjusted coefficient = −0.03, P ≤ 0.01). Greenstick fractures show significantly faster remodelling than full-thickness fractures (adjusted coefficient = −3.04, P = 0.0145). An affected dominant or non-dominant hand, as well as suffering from a solitary radius fracture or both-bone fracture, is not of significant influence on fracture angulation.
Fracture angulation and function
Using unconditional growth model analyses, grip strength was found to be significantly influenced by fracture angulation (coefficient = −1.52, P = 0.0223). No association was found between fracture angulation and any range of motion tests.
Discussion
The current study shows a first impression of the bone remodelling capacity in nonreduced paediatric forearm fractures, thereby evaluating functional outcome in time. Factors that influence fracture angulation were also determined. The rationale was the lack of clear guidance from the literature for definite acceptable angular deformations and functional restoration in time.
After one year, the mean fracture angulation of 12° measured at initial presentation was reduced to a mean residual angulation of 4°. At this point in time, no significant differences between the affected and the nonaffected hand were found for either grip strength or range of motion. This suggests that a residual angulation of 4° is of no functional concern. Conservative treatment without reduction could therefore be a good treatment option in angulated forearm fractures.
There is a worldwide tendency toward a more aggressive approach in the treatment of the described angular deformities, even without thoroughly weighing noninvasive treatment modalities. Using the Isala Graphs as a safe inclusion, we attempted to obtain more insight into functional outcome in nonreduced angulated fractures. Functional outcome is often overlooked while in daily practice fracture consolidation often equals the end of treatment.
Literature on fracture remodelling in paediatric forearm fractures is scarce, even more so in relation to functional outcome [19]. Crawford et al. performed a retrospective case series amongst 54 children with conservatively treated overriding distal radius fractures [17]. Angulation improved from 4.0 to 2.2° at final follow-up (one-year after fracture) with no functional limitations. Functional outcome during follow up and final scores were, however, not specified and could therefore not be compared to the recent study. Also, their study population consisted of completely displaced fractures and were excluded in our study. In a retrospectively studied population of 33 children with malunited distal radius fractures, Jeroense et al. found a mean residual angulation of 8° after a mean follow-up of 9 months, compared to 4° residual angulation after 12 months in our study population. However, mean angulation at moment of presentation was larger in their population (23°) than in ours (12°) [15]. The study of Van der Sluijs et al. (2016) merged data of two studies (including Jeroense et al. 2015), and included 63 children with a mean angulation at initial trauma of 25°, which remodelled to a mean residual angulation of 6.7° after a mean of 22 months follow-up [16]. Neither of these studies took functional outcome into consideration though.
As mentioned in the Results section, one case maintained a residual angulation of 11°. Stagnation of remodelling in this case could be partially explained by fracture location and age. More proximally located fractures of the radius and ulna are known to have a high probability of residual angulation and pronation loss [20]. Johari et al. described how midshaft forearm fractures in children older than age 10 have a less favourable prognosis in terms of remodelling [19]. Despite the residual angulation, grip strength and range of motion were found to be near-normal, with all scores being equal to the unaffected side except for pronation and grip strength. These scores were both 90% of the unaffected hand. The minimum loss of function despite the residual malalignment of 11° could be explained by the extent of malalignment. Colaris et al. (2014) found a significant loss of pronation (<50°) more than 6 months post-trauma in 31.9% of cases with an angular malunion of 11–15° [20]. Earlier cadaveric studies with artificially created deformities of the forearm bones revealed that angular malalignment of 10° or less will not limit forearm rotation anatomically, while loss of pronation and supination can be expected when residual angles of 20° or more are measured [21,22].
As expected, the radiographs show a reduction of angulation over time. Interestingly, in some cases, angulation seems to increase in the first period before a decrease sets in. This phenomenon is not previously described in studies on nonreduced forearm fractures. However, Colaris et al. described an angulation increase in forearm fractures treated by reduction, in the period between reduction and cast removal [7]. In his study, as in ours, remodelling was seen in the period between cast removal and final examination. Previous studies have shown that fractures with any bayonet apposition are prone to lose reduction, which could probably explain the primary worsening of angulation [23,24].
It would be reasonable to assume that after correction of angular deformity in time, recovery of function would follow. This study found an excellent functional outcome after one year. No significant differences in elbow or wrist range of motion were observed between the affected and the unaffected arm. Pronation and supination took the longest to recover since the scores on these parameters where both still significantly diminished up to 6 months after fracture. This observation is in line with previous literature, where limitations in pronation and supination were most frequently seen in overall mobility of the wrist after sustaining a forearm fracture [25,26].
The potency of angular correction in juvenile bone depends on redirection of the epiphyseal growth plate and remodelling at the fracture site [27,28]. An interesting thought would be that remodelling is being promoted by function. Factors supporting this can be derived from for example, Wolff’s law; malalignment in plane of movement is advantageous and rotational deformities in a fracture do not realign. Redistribution of growth in the physis still remains hard to prove [27,29].
To our knowledge, this study is the first to prospectively investigate fracture remodelling in paediatric nonreduced angulated forearm fractures for functional outcome at fixed follow-up moments. Since assessment took place several times during one year, this study provides good insight into the progression of remodelling as well as recovery of function over time.
The most important limitation of this study is the relatively small study population. This makes the data less reliable to adequately differentiate between subgroups (e.g. hand dominance, sex and fracture type). Second, the range of fracture angulation at the moment of presentation was large and relatively moderate because of the inclusion criteria. More subjects are needed to adequately observe the difference in fracture remodelling, based on severity of angulation at the time of presentation. Lastly, we had to deal with missing data. Not all participants came to all the follow-up appointments. For future studies, the recommendation would be to schedule less follow-up appointments at stricter times to improve attendance.
Conclusion
This study shows that nonreduced angulated paediatric forearm fractures have the potential to remodel in time, and show good radiographic and functional outcome with respect to grip strength and range of motion after one year. Concerning functional outcome, pronation and grip strength take the longest to recover, with grip strength being strongly associated with fracture alignment.
Acknowledgements
The help of R.E. Steward, Methodologist at the University Medical Center Groningen, is greatly appreciated with conducting the analyses.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rennie L, Court-Brown CM, Mok JY, Beattie TF. The epidemiology of fractures in children. Injury. 2007; 38:913–922 [DOI] [PubMed] [Google Scholar]
- 2.Clark EM. The epidemiology of fractures in otherwise healthy children. Curr Osteoporos Rep. 2014; 12:272–278 [DOI] [PubMed] [Google Scholar]
- 3.Mäyränpää MK, Mäkitie O, Kallio PE. Decreasing incidence and changing pattern of childhood fractures: a population-based study. J Bone Miner Res. 2010; 25:2752–2759 [DOI] [PubMed] [Google Scholar]
- 4.Kosuge D, Barry M. Changing trends in the management of children’s fractures. Bone Joint J. 2015; 97-B:442–448 [DOI] [PubMed] [Google Scholar]
- 5.Abraham A, Kumar S, Chaudhry S, Ibrahim T. Surgical interventions for diaphyseal fractures of the radius and ulna in children. Cochrane Database Syst Rev. 2011; 9:CD007907. [DOI] [PubMed] [Google Scholar]
- 6.Flynn JM, Jones KJ, Garner MR, Goebel J. Eleven years experience in the operative management of pediatric forearm fractures. J Pediatr Orthop. 2010; 30:313–319 [DOI] [PubMed] [Google Scholar]
- 7.Colaris JW, Allema JH, Biter LU, de Vries MR, van de Ven CP, Bloem RM, et al. Re-displacement of stable distal both-bone forearm fractures in children: a randomised controlled multicentre trial. Injury. 2013; 44:498–503 [DOI] [PubMed] [Google Scholar]
- 8.Miller BS, Taylor B, Widmann RF, Bae DS, Snyder BD, Waters PM. Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: a prospective, randomized study. J Pediatr Orthop. 2005; 25:490–494 [DOI] [PubMed] [Google Scholar]
- 9.Pretell Mazzini J, Rodriguez Martin J. Paediatric forearm and distal radius fractures: risk factors and re-displacement–role of casting indices. Int Orthop. 2010; 34:407–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodriguez-Merchan EC. Pediatric fractures of the forearm. Clin Orthop Relat Res. 2005; 432:65–72 [PubMed] [Google Scholar]
- 11.Vopat ML, Kane PM, Christino MA, Truntzer J, McClure P, Katarincic J, Vopat BG. Treatment of diaphyseal forearm fractures in children. Orthop Rev (Pavia). 2014; 6:5325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Madhuri V, Dutt V, Gahukamble AD, Tharyan P. Conservative interventions for treating diaphyseal fractures of the forearm bones in children. Cochrane Database Syst Rev. 2013; 4:CD008775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eismann EA, Little KJ, Kunkel ST, Cornwall R. Clinical research fails to support more aggressive management of pediatric upper extremity fractures. J Bone Joint Surg Am. 2013; 95:1345–1350 [DOI] [PubMed] [Google Scholar]
- 14.Ploegmakers JJ, Verheyen CC. Acceptance of angulation in the non-operative treatment of paediatric forearm fractures. J Pediatr Orthop B. 2006; 15:428–432 [DOI] [PubMed] [Google Scholar]
- 15.Jeroense KT, America T, Witbreuk MM, van der Sluijs JA. Malunion of distal radius fractures in children. Acta Orthop. 2015; 86:233–237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Sluijs JA, Bron JL. Malunion of the distal radius in children: accurate prediction of the expected remodeling. J Child Orthop. 2016; 10:235–240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crawford SN, Lee LS, Izuka BH. Closed treatment of overriding distal radial fractures without reduction in children. J Bone Joint Surg Am. 2012; 94:246–252 [DOI] [PubMed] [Google Scholar]
- 18.Hansen BA, Greiff J, Bergmann F. Fractures of the tibia in children. Acta Orthop Scand. 1976; 47:448–453 [DOI] [PubMed] [Google Scholar]
- 19.Johari AN, Sinha M. Remodeling of forearm fractures in children. J Pediatr Orthop B. 1999; 8:84–87 [PubMed] [Google Scholar]
- 20.Price CT, Scott DS, Kurzner ME, Flynn JC. Malunited forearm fractures in children. J Pediatr Orthop. 1990; 10:705–712 [DOI] [PubMed] [Google Scholar]
- 21.Matthews LS, Kaufer H, Garver DF, Sonstegard DA. The effect on supination-pronation of angular malalignment of fractures of both bones of the forearm. J Bone Joint Surg Am. 1982; 64:14–17 [PubMed] [Google Scholar]
- 22.Tarr RR, Garfinkel AI, Sarmiento A. The effects of angular and rotational deformities of both bones of the forearm. An in vitro study. J Bone Joint Surg Am. 1984; 66:65–70 [PubMed] [Google Scholar]
- 23.Alemdaroğlu KB, Iltar S, Cimen O, Uysal M, Alagöz E, Atlihan D. Risk factors in redisplacement of distal radial fractures in children. J Bone Joint Surg Am. 2008; 90:1224–1230 [DOI] [PubMed] [Google Scholar]
- 24.Asadollahi S, Ooi KS, Hau RC. Distal radial fractures in children: risk factors for redisplacement following closed reduction. J Pediatr Orthop. 2015; 35:224–228 [DOI] [PubMed] [Google Scholar]
- 25.Colaris J, Reijman M, Allema JH, de Vries M, Biter U, Bloem R, et al. Angular malalignment as cause of limitation of forearm rotation: an analysis of prospectively collected data of both-bone forearm fractures in children. Injury. 2014; 45:955–959 [DOI] [PubMed] [Google Scholar]
- 26.Sinikumpu JJ, Lautamo A, Pokka T, Serlo W. Complications and radiographic outcome of children’s both-bone diaphyseal forearm fractures after invasive and non-invasive treatment. Injury. 2013; 44:431–436 [DOI] [PubMed] [Google Scholar]
- 27.Ryöppy S, Karaharju EO. Alteration of epiphyseal growth by an experimentally produced angular deformity. Acta Orthop Scand. 1974; 45:490–498 [DOI] [PubMed] [Google Scholar]
- 28.Karaharju EO, Ryöppy SA, Mäkinen RJ. Remodelling by asymmetrical epiphysial growth. An experimental study in dogs. J Bone Joint Surg Br. 1976; 58:122–126 [DOI] [PubMed] [Google Scholar]
- 29.Pauwels F. A clinical observation as example and proof of functional adaptation of bone through longitudinal growth. Z Orthop Ihre Grenzgeb. 1975; 113:1–5 [PubMed] [Google Scholar]


