Purpose:
To investigate effect of metabolic syndrome on blood pressure during cataract surgery with topical anesthesia.
Design:
A single-centered, retrospective case series.
Methods:
Consecutive patients who were hospitalized and underwent phacoemulsification and insertion of intraocular lens with topical anesthesia in October 2016 were included. Perioperative blood pressure and pulse pressure were compared between patients with metabolic syndrome (metabolic group) and sex- and age-matched patients without metabolic syndrome (nonmetabolic group) at six time points: on admission, in the morning of the operation, 2 hours before the operation, at the point of entering the operation room, during the operation, and after the operation. Perioperative use of etizolam and nicardipine was compared between the two groups.
Results:
Thirty patients in the metabolic group and 30 in the nonmetabolic group were included. There was no difference in changes compared with the values on admission in systolic pressure and pulse pressure at any examination point between the two groups. There was no difference in changes in diastolic pressure between the two groups, except for at 2 hours before the operation (1.4 ± 9.6 mm Hg in the metabolic group vs –6.2 ± 8.5 mm Hg in the nonmetabolic group; P = 0.044). The number of patients who were administered etizolam was 5/30 (16.7%) in the metabolic group and 2/30 (6.7%) in the nonmetabolic group, showing no significant difference. No patients were administered intravenous nicardipine in either group.
Conclusions:
Well-controlled metabolic syndrome did not affect the changes in perioperative blood pressure during cataract surgery with topical anesthesia.
Keywords: blood pressure, cataract surgery, metabolic syndrome, pulse pressure
Metabolic syndrome is defined as a condition of central obesity accompanied by hypertension, hyperglycemia, and dyslipidemia and may lead to systemic diseases such as diabetic mellitus, myocardial infarction, and cerebral infarction.1 In the field of ophthalmology, it has been reported that metabolic syndrome is related to retinopathy,2 cataract,3 and glaucoma.4 In particular, a large studies showed a positive correlation between cataract and metabolic syndrome.5,6
Many patients with cataract requiring surgical interventions are aged with underlying age-related diseases such as hypertension.7 Perioperative hypertension is known to be a risk factor of vascular accidents such as suprachoroidal hemorrhage, even after the recent improvements in surgical machines and techniques.8 Perioperative control of blood pressure is required to prevent both ophthalmologic suprachoroidal hemorrhage and systemic cardiovascular accidents.
Hypertension is usually controlled during the preoperative examination by physicians and is perhaps treated preoperatively with oral and or intravenous injection of hypotensive drug. Although anesthesiologists properly control blood pressure during general anesthesia, ophthalmologists are responsible for the control during topical anesthesia. The standards of controlling blood pressure might differ among surgeons or hospitals during cataract surgery. Furthermore, we sometimes experience cases that require urgent perioperative intervention for blood pressure control, even if they are well controlled with medication preoperatively. It was reported that blood pressure was inclined to elevate in patients with high blood pressure perioperatively even though it was well controlled preoperatively.9
However, to our knowledge, no previous reports have examined the relationship between metabolic syndrome and blood pressure during cataract surgery. Therefore, we investigated changes in blood pressure during cataract surgery in patients with metabolic syndrome. We hypothesized that the perioperative blood pressure of patients with metabolic syndrome would be elevated during cataract surgery with topical anesthesia.
METHODS
This was a retrospective observational study. It was approved by the institutional review board of Miyata Eye Hospital and adhered to the tenets of the Declaration of Helsinki. We included consecutive patients with metabolic syndrome, who were hospitalized and underwent phacoemulsification and insertion of intraocular lens with topical anesthesia at Miyata Eye Hospital in October 2016. Sex- and age-matched patients without metabolic syndrome who underwent the same surgery during the same period served as controls. We excluded patients without sufficient information present in medical records.
Metabolic syndrome was diagnosed based on the diagnostic standards used in Japan.10 They require the presence of abdominal obesity (abdominal circumference greater than or equal to 85 cm for men and 90 cm for women) and at least two of three other factors: hypertension (greater than or equal to 130/85 mm Hg), hyperglycemia (fasting blood sugar greater than or equal to 110 mg/dL), and lipid abnormality (greater than or equal to 150 mg/dL triglycerides and/or lower than 40 mg/dL HDL cholesterol). Patients with metabolic syndrome were included in the “metabolic group” and those without metabolic syndrome were included in the “nonmetabolic group.” We reviewed medical and operative records retrospectively to examine perioperative blood pressure and pulse pressure. Pulse pressure was calculated from the difference between systolic pressure and diastolic pressure. Patients were hospitalized the day before the surgery. Blood pressure was recorded six times using an indirect method: on admission, in the morning of the operation, 2 hours before the operation, at the point of entering the operation room, during the operation (at the insertion of intraocular lens), and after the operation. Furthermore, we examined the frequency of perioperative systemic adverse events, such as thoracic aortic dissection or abdominal aortic dissection, and ophthalmologic adverse events, such as suprachoroidal hemorrhages, and examined the perioperative use of etizolam and nicardipine.
Both patients who had and had not been treated by family physicians were examined before surgery by a single physician. Patients who had been prescribed medication for hypertension and those who had not been prescribed but their systolic/diastolic blood pressure was greater than or equal to 130/85 mm Hg were considered to have hypertension. Patient blood pressure was properly controlled by the physician with antihypertensive drugs such as calcium blockers, depending on patient status before the surgery. When elevated blood pressure was noticed on the day of the surgery, oral etizolam 0.5 mg and/or intravenous nicardipine were prescribed by a single physician. Cataract surgery was performed with topical anesthesia of 4% xylocaine instillation. Corneal or sclerocorneal incision was performed. Subconjunctival injection of 4% xylocaine 0.5 mL was added in cases of sclerocorneal incision. After phacoemulsification and aspiration, an intraocular lens was fixed in the capsule. Finally, subconjunctival injection of orgadrone 0.3 mL, instillation of 1.5% levofloxacin, and application of ofloxacin ointment were performed. After the vital signs were checked, the patient was moved to the ward.
The χ2 test was used to compare sex differences and the rate of hypertension, diabetes, and lipid abnormality between the two groups. The Mann-Whitney U test was used to compare ages between the two groups. The Kruskal-Wallis test with the Scheffé test for multiple comparisons was used to compare blood pressure and pulse pressure at each examination point. Fisher exact test was used to compare the usage of etizolam and nicardipine and the rate of patients with high systolic pressure. Data were presented as mean ± standard deviation. P values lower than 0.05 were considered statistically significant.
RESULTS
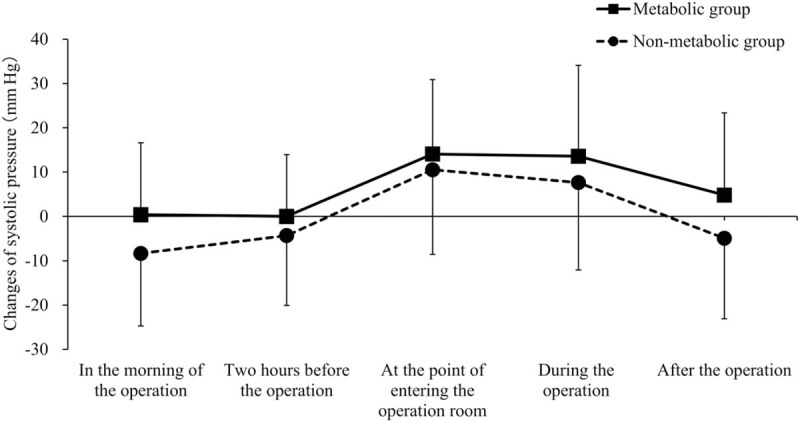
Thirty patients with metabolic syndrome and 30 patients without metabolic syndrome were enrolled. The characteristics of the patients are shown in Table 1. There was no significant difference in systolic pressure, diastolic pressure, and pulse pressure between the two groups.
TABLE 1.
Characteristics of the Metabolic Group and the Nonmetabolic Group
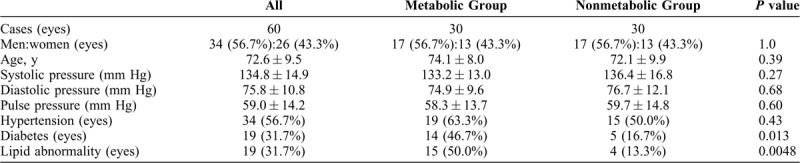
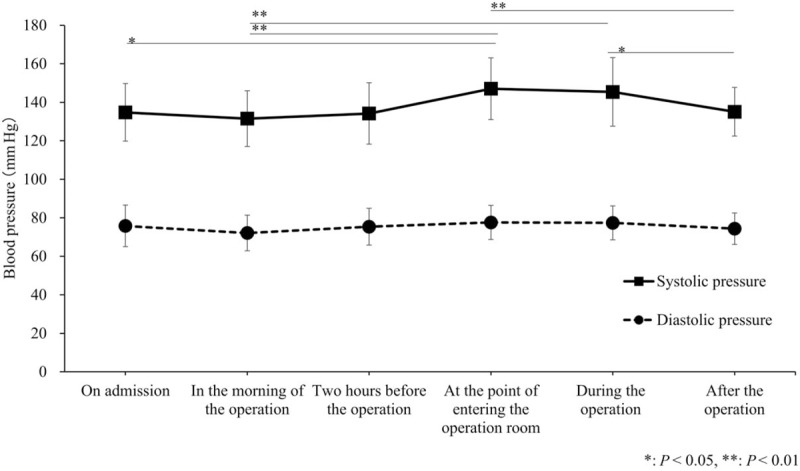
The mean perioperative systolic pressure and diastolic pressure of the patients are shown in Figure 1. On admission, systolic pressure was 134.8 ± 14.9 mm Hg and did not change until 2 hours before the operation but increased significantly to 147.1 ± 16.0 mm Hg at the point of entering the operation room (P = 0.001). It decreased significantly to 135.1 ± 12.6 mm Hg after the operation compared with that during the operation (P = 0.047). In contrast, diastolic pressure was 75.8 ± 10.8 mm Hg on admission and did not change significantly during the observation. The mean pulse pressure of the patients is shown in Figure 2; it was 59.0 ± 14.2 mm Hg on admission and increased significantly to 69.5 ± 14.6 mm Hg at the point of entering the operation room (P = 0.0018). It was 60.5 ± 12.6 mm Hg after the operation, but the change compared with the pulse pressure at the point of entering the operation room was not significant.
FIGURE 1.
Changes in the perioperative systolic pressure and diastolic pressure of all patients. The systolic pressure at the point of entering the operation room was significantly higher than that on admission (P = 0.011), in the morning of the operation (P < 0.001), and after the operation (P = 0.0068). The systolic pressure during the operation was significantly elevated compared with that in the morning of the operation (P = 0.0011) and after the operation (P = 0.047). There was no significant difference in diastolic pressure at any observation point. Data were presented as mean ± standard deviation.
FIGURE 2.
Changes in the perioperative pulse pressure of all patients. The pulse pressure at the point of entering the operation room was significantly higher than that on admission (P = 0.018) and in the morning of the operation (P = 0.03). Data were presented as mean ± standard deviation.
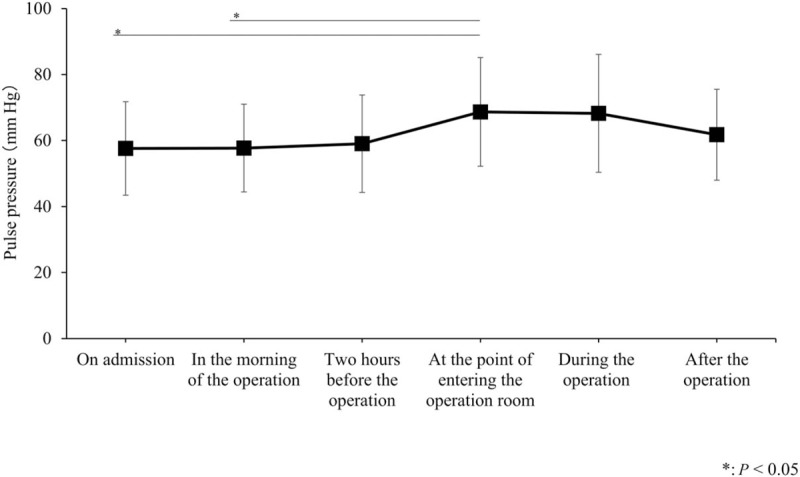
The comparison of changes in systolic pressure compared with the values on admission is shown in Figure 3. At all examination points, there was no difference between the two groups. The comparison of changes in diastolic pressure compared with the values on admission is shown in Figure 4. The change 2 hours before the operation was 1.4 ± 9.6 mm Hg in the metabolic group and −6.2 ± 8.5 mm Hg in the nonmetabolic group, and the difference was significant (P = 0.044). At the other examination points, there was no difference between the two groups. The comparison of changes in pulse pressure compared with the values on admission is shown in Figure 5. At all examination points, there was no difference between the two groups.
FIGURE 3.
Comparison of changes in the perioperative systolic pressure of all patients in the metabolic group and the nonmetabolic group. The values showed the changes in systolic pressure of each observation point compared with the values on admission. There was no difference between the two groups at any examination point. Data were presented as mean ± standard deviation.
FIGURE 4.
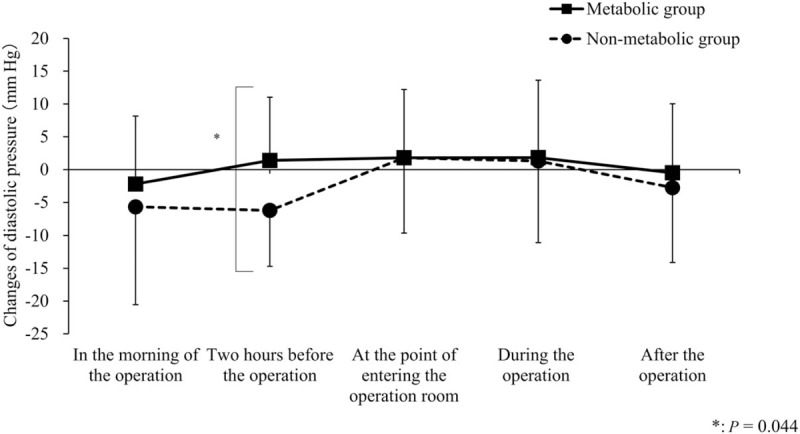
Comparison of changes in the perioperative diastolic pressure of all patients in the metabolic group and the nonmetabolic group. The values showed the changes in systolic pressure of each observation point compared with the values on admission. There was a significant difference in the diastolic pressure 2 hours before the operation between the metabolic group and the nonmetabolic group (P = 0.044). There was no difference between the two groups at the other examination points. Data were presented as mean ± standard deviation.
FIGURE 5.
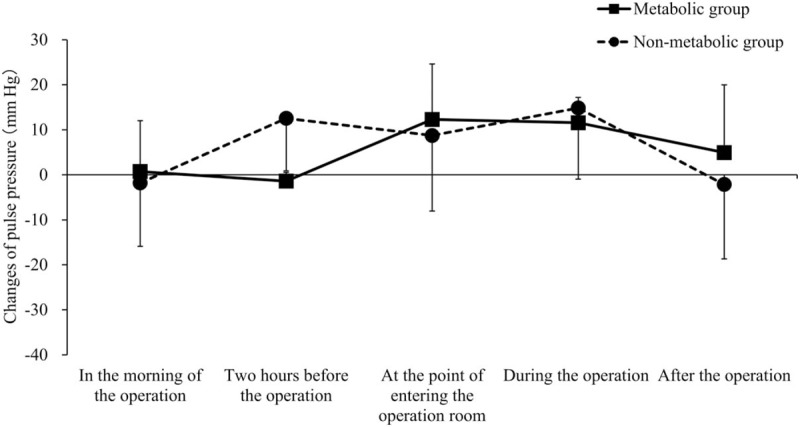
Comparison of changes in the perioperative pulse pressure of all patients in the metabolic group and the nonmetabolic group. There was no difference between the two groups at any examination point. Data were presented as mean ± standard deviation.
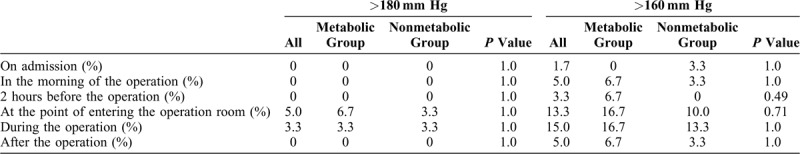
The rate of patients who had systolic pressure higher than 180 mm Hg and 160 mm Hg is shown in Table 2. There was no difference between the two groups. 7 patients were administered etizolam (11.7%), including 5 patients (16.7%) in the metabolic group and 2 patients (6.7%) in the nonmetabolic group. No patients were administered intravenous nicardipine in either group. There was no difference between the groups regarding the use of etizolam and nicardipine. No patients had systemic or ophthalmologic adverse events.
TABLE 2.
Rate of Patients Who Had Systolic Pressure Higher Than 180 mm Hg and 160 mm Hg
DISCUSSION
This report showed that there was no difference in perioperative systolic pressure between the metabolic group and nonmetabolic group under surgery with topical anesthesia, but that diastolic pressure was significantly higher in the metabolic group only at 2 hours before the operation. Because metabolic syndrome comprises central obesity, hypertension, hyperglycemia, and lipid abnormality, patients would also have insulin resistance and arteriosclerosis.11 Therefore, we anticipated that the blood pressure of the metabolic group would be elevated compared with that of the nonmetabolic group, but the results were contrary to this expectation. The first reason for this is that the nonmetabolic group possibly included patients with hypertension who did not satisfy the criteria of metabolic syndrome. Second, etizolam and/or nicardipine were administered after entering the operation room to the patients whose blood pressure was elevated, and this might have affected the results. Although there was no statistically significant difference in the administration of etizolam and nicardipine between the two groups, the preventive intervention could have altered the results. Third, regarding the background of the patients, the rate of patients with diabetes and lipid abnormality was significantly higher in the metabolic group and it could have had a confounding effect. Preoperative medical testing was reported not to increase the safety of cataract surgery,12 but our results showed that perioperative blood pressure changed equally regardless of whether the patients had metabolic syndrome. Therefore, we should properly control blood pressure in all patients, regardless of the presence of metabolic syndrome.
Metabolic syndrome was reported to be present in <10% to 84% of the population and it differed largely depending on the region.13 Although there are several diagnostic criteria of metabolic syndrome, we used the Japanese criteria, which are similar to those set by the International Diabetes Federation.10,11,14 The Japanese diagnostic standards of metabolic syndrome require the presence of abdominal obesity and at least two of three other factors: hypertension, hyperglycemia, and lipid abnormality.10 Cataract reportedly has a relationship with hypertension, hyperglycemia, and hyperlipidemia.5,15,16 A high body mass index was related to cortical cataract.17 Especially, the type of cataract that is affected by hypertension is posterior subcapsular cataract, which leads to visual impairment.16 As the population of patients with metabolic syndrome is large, there is a high probability that patients requiring cataract surgery would also have metabolic syndrome. Due to the progress of surgical machines and sophisticated surgical procedures, the surgical time is short these days. However, many patients with cataract with complications require careful perioperative management.
Pulse pressure increases with aging because systolic pressure increases, whereas diastolic pressure tends not to increase. Pulse pressure reflects arterial stiffness and ventricular ejection.18 Elevated pulse pressure is a risk factor of myocardial infarction and heart failure.19 In the current investigation, we evaluated changes in pulse pressure during topical anesthesia. As a result, pulse pressure significantly increased from the beginning of surgery in all patients. However, changes in pulse pressure in the metabolic group were comparable to those in the nonmetabolic group. A former study showed that increase of arterial stiffness was found in patients with metabolic syndrome and that the pulse pressure of such patients was higher than that of those without.18 Cataract surgery is considered systemically safe if there is sufficient preoperative control of hyperglycemia and hypertension. In topical anesthesia, both systolic and diastolic pressure, including pulse pressure, should be considered when controlling blood pressure.
In this study, perioperative systolic and diastolic pressures were significantly elevated in all patients, although preoperative blood pressure was properly controlled. However, no systemic adverse event was observed. It was reported that during cataract surgery, systolic and diastolic pressures started to elevate when patients preoperatively entered the anesthesia room.9 Additionally, it was reported that entrance to the operation room resulted in elevation of patient blood pressure.20 This former study also reported that not only pain during surgery but also anxiety and stress affected blood pressure, and listening to music in the operation room was useful for suppressing elevation of blood pressure.20 To control blood pressure during cataract surgery, it is important to manage patient anxiety and to decrease pain using proper anesthesia and surgical techniques.
This study had several limitations. The current investigation included only patients requiring cataract surgery who were admitted to measure blood pressure a sufficient number of times in a stable environment. To exclude selection bias, it is necessary to include all patients requiring cataract surgery, including patients undergoing outpatient surgery. Furthermore, this study examined only blood pressure and did not measure heart rate at all examination points. It is possible that there are patients who have tachycardia without hypertension during surgery. Perioperative general evaluation is needed in the next investigation. This study was retrospective, and the number of patients was limited. Further prospective study with a sufficient sample is required.
CONCLUSIONS
In conclusion, metabolic syndrome that was well controlled by the physician did not affect changes in perioperative blood pressure during cataract surgery with topical anesthesia. Because perioperative blood pressure changes equally regardless of whether the patients have metabolic syndrome, proper preoperative control of blood pressure is useful to avoid complications.
Footnotes
Financial Disclosures: No author has a financial or proprietary interest in any material or method mentioned.
REFERENCES
- 1.O’Neill S, O’Driscoll L. Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obes Rev 2015; 16:1–12. [DOI] [PubMed] [Google Scholar]
- 2.Liu L, Yue S, Wu J, et al. Prevalence and risk factors of retinopathy in patients with or without metabolic syndrome: a population-based study in Shenyang. BMJ Open 2015; 5:e008855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park S, Lee EH. Association between metabolic syndrome and age-related cataract. Int J Ophthalmol 2015; 8:804–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Newman-Casey PA, Talwar N, Nan B, et al. The relationship between components of metabolic syndrome and open-angle glaucoma. Ophthalmology 2011; 118:1318–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sabanayagam C, Wang JJ, Mitchell P, et al. Metabolic syndrome components and age-related cataract: the Singapore Malay eye study. Invest Ophthalmol Vis Sci 2011; 52:2397–2404. [DOI] [PubMed] [Google Scholar]
- 6.Lindblad BE, Hakansson N, Philipson B, et al. Metabolic syndrome components in relation to risk of cataract extraction: a prospective cohort study of women. Ophthalmology 2008; 115:1687–1692. [DOI] [PubMed] [Google Scholar]
- 7.Koolwijk J, Fick M, Selles C, et al. Outpatient cataract surgery: incident and procedural risk analysis do not support current clinical ophthalmology guidelines. Ophthalmology 2015; 122:281–287. [DOI] [PubMed] [Google Scholar]
- 8.Ling R, Kamalarajah S, Cole M, et al. Suprachoroidal haemorrhage complicating cataract surgery in the UK: a case control study of risk factors. Br J Ophthalmol 2004; 88:474–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lira RP, Nascimento MA, Arieta CE, et al. Incidence of preoperative high blood pressure in cataract surgery among hypertensive and normotensive patients. Indian J Ophthalmol 2010; 58:493–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Definition and the diagnostic standard for metabolic syndrome: Committee to Evaluate Diagnostic Standards for Metabolic Syndrome [in Japanese]. Nihon Naika Gakkai Zasshi 2005; 94:794–809. [PubMed] [Google Scholar]
- 11.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement: Executive Summary. Crit Pathw Cardiol 2005; 4:198–203. [DOI] [PubMed] [Google Scholar]
- 12.Schein OD, Katz J, Bass EB, et al. The value of routine preoperative medical testing before cataract surgery. Study of Medical Testing for Cataract Surgery. N Engl J Med 2000; 342:168–175. [DOI] [PubMed] [Google Scholar]
- 13.Kaur J. A comprehensive review on metabolic syndrome. Cardiol Res Pract 2014; 2014:943162. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Yamagishi K, Iso H. The criteria for metabolic syndrome and the national health screening and education system in Japan. Epidemiol Health 2017; 39:e2017003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richter GM, Torres M, Choudhury F, et al. Risk factors for cortical, nuclear, posterior subcapsular, and mixed lens opacities: the Los Angeles Latino Eye Study. Ophthalmology 2012; 119:547–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu X, Lyu D, Dong X, et al. Hypertension and risk of cataract: a meta-analysis. PLoS One 2014; 9:e114012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ghaem Maralani H, Tai BC, Wong TY, et al. Metabolic syndrome and risk of age-related cataract over time: an analysis of interval-censored data using a random-effects model. Invest Ophthalmol Vis Sci 2013; 54:641–646. [DOI] [PubMed] [Google Scholar]
- 18.Safar ME, Thomas F, Blacher J, et al. Metabolic syndrome and age-related progression of aortic stiffness. J Am Coll Cardiol 2006; 47:72–75. [DOI] [PubMed] [Google Scholar]
- 19.Chae CU, Pfeffer MA, Glynn RJ, et al. Increased pulse pressure and risk of heart failure in the elderly. JAMA 1999; 281:634–639. [DOI] [PubMed] [Google Scholar]
- 20.Merakou K, Varouxi G, Barbouni A, et al. Blood pressure and heart rate alterations through music in patients undergoing cataract surgery in Greece. Ophthalmol Eye Dis 2015; 7:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]


