Abstract
Background.
The risk of wound healing complications (WHCs) and the early use of mammalian target of rapamycin inhibitors after kidney transplantation (KT) have not been fully addressed.
Methods.
The NEVERWOUND study is a 3-month, multicenter, randomized, open-label study designed to evaluate whether a delayed (ie, 28 ± 4 d posttransplant) immunosuppression regimen based on everolimus (EVR) reduces the risk of WHC versus EVR started immediately after KT. Secondary endpoints were treatment failure (biopsy-proven acute rejection, graft loss, or death), delayed graft function, patient and graft survival rates, and renal function.
Results.
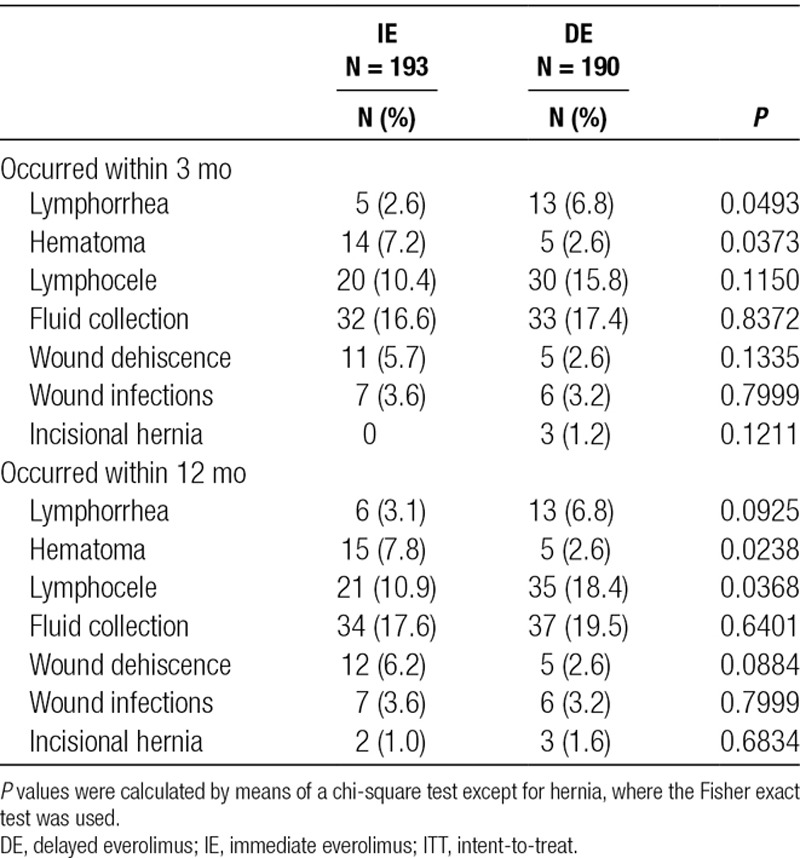
Overall, 394 KT recipients were randomized to receive immediate (N = 197) or delayed (N = 197) EVR after KT. At 3 months, WHC-free rates in the immediate EVR versus delayed EVR arm, considering the worst- and best-case scenario approach, were 0.68 (95% confidence interval [CI], 0.62-0.75) versus 0.62 (95% CI, 0.55-0.68) (log-rank P = 0.56) and 0.70 (95% CI, 0.64-0.77) versus 0.72 (95% CI, 0.65-0.78) (log-rank P = 0.77), respectively. The 3- and 12-month treatment failure rates, delayed graft function and renal function, and patient and graft survival were not different between the arms.
Conclusions.
The early introduction of EVR after KT did not increase the risk of WHC, showing good efficacy and safety profile.
INTRODUCTION
In kidney transplantation (KT), the introduction of new immunosuppressive agents may offer the opportunity to reduce adverse events (AEs) and personalize the therapy, while maintaining a good feasibility and efficacy. The introduction of mycophenolic acid (MPA) and mammalian target of rapamycin inhibitors (mTORis) led, in selected patients, to the reduction or elimination of calcineurin inhibitors (CNIs) in early post-KT.1-5 Everolimus (EVR) (Certican; Novartis Pharma AG, Basel, Switzerland) is a mTORi immunosuppressant drug with antiproliferative properties that reduces growth factor–stimulated lymphocyte proliferation.6,7 In the experimental model and KT human trials, EVR showed good safety and efficacy with an acceptable tolerability,8-11 while reducing vascular smooth muscle cells proliferation6 and neointimal growth12-15 and leading to a reduction in graft arteriosclerosis.16
Several studies suggested that Sirolimus, an mTORi drug, was associated with an increased rate of wound healing complications (WHCs) after solid organ transplantation,17-23 an effect potentially related to the inhibition of the activation and proliferation of fibroblast cells. On the contrary, even if the evidence is still scarce, EVR did not show inferiority versus other immunosuppression (IS)24,25 and only the drug exposure seems to be related with WHC, especially in severely obese recipients.26,27
In the CALLISTO study,28 a 12-month randomized multicenter trial, KT patients at risk of delayed graft function (DGF) were randomized to receive EVR either immediately after KT or in a delayed setting. Composite endpoints were DGF, biopsy-proven acute rejection (BPAR), death, and WHC. The authors eventually specify that the immediate introduction of EVR was not associated with any disadvantage in terms of graft recovery or wound healing.
Considering the small population (ie, 139 randomized patients) of the CALLISTO study and the sample size estimation (calculated for the composite endpoint)—as well as the lack of any randomized trial on mTORi fitted for WHC only—the present study was designed with the aim of evaluating whether the delayed administration of EVR (ie, 28 ± 4 d posttransplant) reduces the risk of WHC in de novo KT recipients.
MATERIALS AND METHODS
Study Design
The NEVERWOUND study was a 3-month, multicenter, randomized, prospective, open-label study with an observational follow-up of 12 months, conducted in 22 Italian kidney transplant centers from November 2011 to December 2015 with the goal of evaluating whether a delayed (ie, 28 ± 4 d posttransplant) EVR-based IS regimen reduces the risk of WHC versus EVR started immediately after KT.
During the screening (day −2 to day 0), patients were assessed for eligibility for the study. At day 0, all patients underwent KT and started the induction treatment as per clinical practice. In all cases, the transplantation consisted in the standard pelvic operation, with heterotopic extraperitoneal placement of the graft and ureteroneocystostomy according to Lich et al29 and Gregoir.30 At baseline (day 1 to day 2), transplanted patients eligible for the study were randomized (ratio, 1:1) to 1 of the 2 following treatment arms: immediate EVR (IE) or delayed EVR (DE) (Figure 1) via a Web-based system and stratified by age at transplant (≤60 or >60) and pretransplant diabetes mellitus status.31
FIGURE 1.
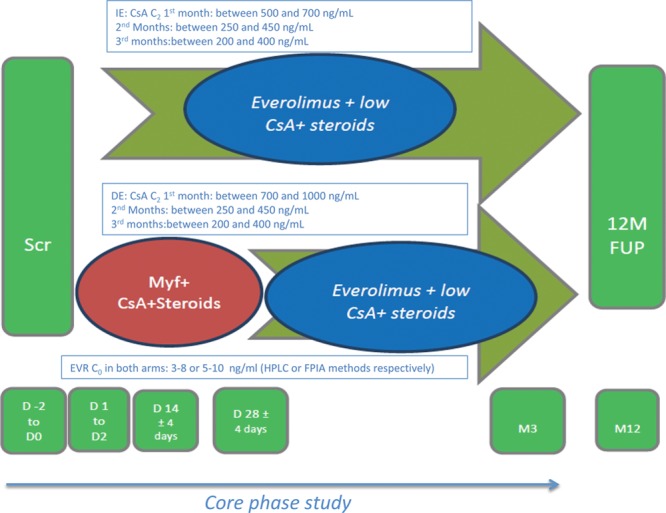
Study design. C0, immunosuppression blood levels, before morning dose; C2, immunosuppression blood levels, 2 h after morning dose; CsA, cyclosporine A; D, day; DE, delayed everolimus; EVR, everolimus; FPIA, fluorescence polarization immunoassay; FUP, follow-up; HPLC, high-performance liquid chromatography; IE, immediate everolimus; M, month; Myf, myfortic; scr, screening.
Upon completion of the 3-month treatment period (CORE phase study), patients entered a 9-month observational follow-up period, where they were treated as per local clinical practice. During the follow-up visit performed 12 months (−1/+6 mo) after KT, information was collected on patient and graft survival, renal function, acute rejection, malignancies, wound assessment, new-onset diabetes mellitus, serum creatinine, and blood levels of EVR and cyclosporine A (CsA).
The study complied with the ICH Harmonized Tripartite Guidelines for Good Clinical Practice and the Declaration of Helsinki and its amendments. A written informed consent was obtained from all patients, and each center’s ethical committee approved the study.
Treatment Regimens
In the IE, EVR was started within 48 hours after graft reperfusion, at the starting dose of 0.75 mg BID, adjusted to target EVR trough level at 0 hour (immunosuppression blood levels, before morning dose [C0]) to reach a range of 3–8 ng/mL (using the high-performance liquid chromatography method) or 5–10 ng/mL (using the fluorescence polarization immunoassay method); CsA (Neoral; Novartis Pharma AG, Basel, Switzerland) was administered BID per os within 48 hours of graft reperfusion, at a starting dose of 4 mg/kg/d. The dose was then adjusted to reach and maintain CsA immunosuppression blood levels 2 h after morning dose (C2) between 500 and 700 ng/mL. When the EVR target level was reached, CsA was tapered up to reach C2 levels between 250 and 450 ng/mL during month 2 and between 200 and 400 ng/mL up to month 3.
In the DE, MPA (Myfortic; Novartis Pharma AG, Basel, Switzerland) was administered within 48 hours after graft reperfusion, at the dose of 720 mg BID. At 28 ± 4 days after KT, MPA was discontinued and EVR was started at 0.75 mg BID to reach and maintain C0 3–8 ng/mL (high-performance liquid chromatography method) or 5–10 ng/mL (fluorescence polarization immunoassay method). CsA was administered BID per os within 48 hours of graft reperfusion, at a starting dose of 6–8 mg/kg/d. The dose was adjusted to reach C2 levels of 700–1000 ng/mL until day 28 ± 4. The dose was then tapered up to reach the same IE arm C2 levels.
Intravenous prednisone (or equivalent) was administered perioperatively, and oral corticosteroids were started the day after, at 20 mg/d, and then tapered according to the center’s clinical practice. Induction therapy was administered, as per local clinical practice (namely IL2 receptor antibodies [Ab-IL2-R] or antithymocyte globuline [ATG]).
Inclusion criteria for the study were as follows: all adult (>18 y) male or female patients who had received first or second single KT from deceased donor or living related were eligible for the study.
Patients were excluded in the following cases: recipients of multiple organ transplants, including 2 kidneys; women of childbearing potential, unless they were using 2 birth control methods; pregnant or nursing (lactating) women; recipients with historical or current peak panel reactive antibodies >50% or unacceptable human leukocyte antigen(s), platelets <75000/mm3, absolute neutrophil count <1500/mm3, leukocytes <2500/mm3, or hemoglobin <7 g/dL; symptoms of significant somatic or mental illness; history of malignancies within the past 5 years; human immunodeficiency virus (HIV) positivity; evidence of severe liver disease; severe active infections; evidence of drug or alcohol abuse; or body mass index (BMI) >30 kg/m2.
Primary Endpoint
The primary objective of the study was to evaluate—during the treatment period (90 ± 4 postoperative days)—whether the delayed administration of EVR in de novo KT recipients reduced the risk of WHC versus the immediate administration.
WHCs were defined as fluid collection, including hematoma and lymphocele (defined as serum >5 cm fluid collections evaluated by ultrasound [assessed at 14 ± 4, 28 ± 4, 90 ± 4, and 360 ± 30 postoperative days]), requiring or not intervention; prolonged lymphatic drainage (ie, lymphorrea) >150 mL/24 h at 7 postoperative days; wound dehiscence, wound infection, and incisional hernia (evaluated after 3 and 12 mo).
Secondary Endpoints and AEs
The secondary objectives were as follows: treatment failure rate (composite endpoint: BPAR [graded according to Banff 97 criteria], graft loss, death); death-censored graft survival rate; graft survival rate; patient survival rate; incidence and duration (days) of DGF (arbitrarily defined as the need of dialysis in the first week after transplant); renal function, through estimated glomerular filtration rate (estimated glomerular filtration rate–modification of diet in renal diseases formula); proteinuria (>1000 mg/24 h or >1.0 protein/creatinine in a spot urine sample); safety; and tolerability (incidence of AEs, serious AEs, infections).
Sample Size
A 2-group continuity-corrected chi-square test with a 0.05 2-sided significance level had a 90% power to detect the difference between a group IE percentage of 0.65 and DE percentage of 0.80 (odds ratio, 2.15) when the sample size in each arm was 198. Three hundred ninety-six patients were therefore enrolled.
Study Population
The following populations were defined in the study:
Intent-to-treat population consisting in all the randomized patients who were treated.
Safety population consisting in all the randomized patients who were treated and had ≥1 safety assessment.
Statistical Analysis
Continuous data are summarized by mean, SD, median, first and third quartile, and minimum and maximum. Categorical data are presented by absolute and relative frequencies (n and %) or contingency tables and, where relevant, with their 95% confidence interval (CI) limits.
The presence/absence of ≥1 WHC was analyzed also by means of a logistic regression model, considering as covariates the type of induction (basiliximab vs ATG), capacity of the center (>10 vs ≤10 patients), diabetes mellitus (yes vs no), age at transplantation, and BMI (<25 vs ≥25 kg/m2).
The primary analysis was performed on the safety population.
The time to event was analyzed by means of a Cox model, considering the same covariate used in the logistic regression model. The hazard ratio (HR) with a 95% CI was presented. Kaplan-Meier curves of time were also calculated. Changes in renal function were analyzed by the ANCOVA model, considering the same covariate used in the logistic regression model.
For the comparison of proportion, the chi-square test or the Fisher exact test was used, while the Wilcoxon test was used for continuous nonnormally distributed data.
All the analysis were produced using 9.4 SAS for Windows.
In order to manage the missing data, patients who discontinued the study before reaching the endpoint, those who discontinued EVR for any reason, and those with missing information about WHC were considered failures, according to the worst-case scenario approach, and successes, according to the best-case scenario approach (Sensitivity Analysis).
RESULTS
Study Population
Three hundred ninety-nine patients were screened; of these, 394 were randomized (IE = 197; DE = 197), and 383 (98.2%) received ≥1 dose of the study drug and were included in both the intent-to-treat and the safety populations. Two patients were treated differently than the assigned treatment arm; 336 patients out of 383 (87.7%) completed the 3-month study (IE = 181; DE = 155); of these, 310 (80.9%) (IE = 161 [81.7%]; DE = 149 [75.6%]) completed the CORE study on treatment. In particular, 12 patients in the IE arm discontinued the study due to graft loss (n = 4); consent withdrawn (n = 3); death (n = 2); administrative reasons (n = 2); and lost to follow-up (n = 1). In the DE arm, 35 patients discontinued due to protocol violation (total n = 28; due to a nonswitch to EVR for unknown reason n = 25; clinical reasons n = 2; error n = 1); death (n = 3); consent withdrawn (n = 2); graft loss (n = 1); or administrative reasons (n = 1). In the IE arm, 32 patients (16.2%) discontinued EVR at 3 months, mainly due to AEs (n = 24, 12.4%), while in the DE arm, only 12 patients (7.4%) required EVR discontinuation. Three hundred seven patients had their 12-month follow-up visit (IE = 159 [82.4%]; DE = 148 [77.9%]) (Figure 2).
FIGURE 2.
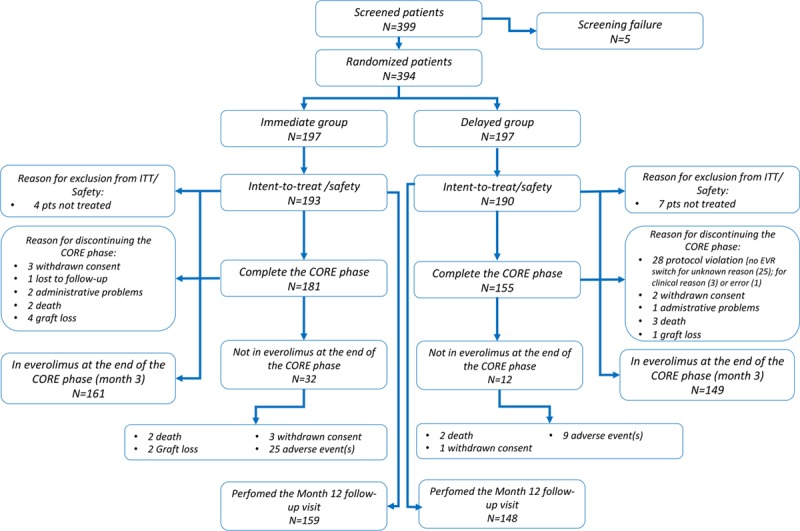
Patient disposition. EVR, everolimus; ITT, intent-to-treat; pts, patients.
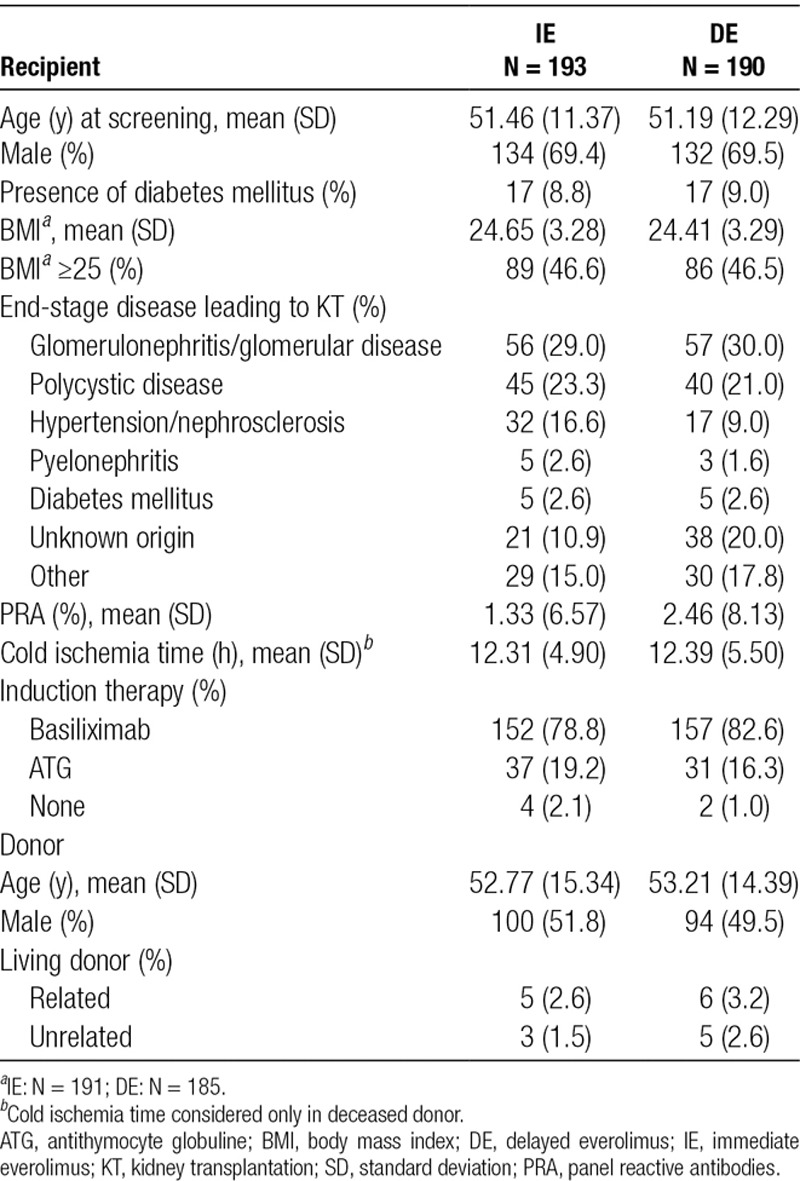
Demographics on recipients’ and donors’ baseline characteristics of the 2 treatment arms are detailed in Table 1.
TABLE 1.
Demographics and baseline recipient and donor characteristics (safety population)
In the DE arm, the switch to EVR was successful in 161 (84.7%) (median time to switch, 29 d [range, 24–62 d]).
At the end of CORE study, the majority of patients in the IE arms were compliant with the C0–EVR protocol (namely 76.2%, 80.4%, and 79.4% after 14 ± 4 and 28 ± 4 days and 3 mo, respectively), while 10% showed blood levels <3–8 ng/mL and 10% above such levels. In the DE arm, 91.8% of patients had levels within range, while in 8.2% of them, levels were below 3–8 ng/mL.
Primary Endpoint: WHCs
Considering the worst-case scenario, the 3-month rate of patients without WHC in the IE and DE arms was 0.68 (95% CI, 0.62-0.75) versus 0.62 (95% CI, 0.55-0.68) (log-rank test: P = 0.56) (Figure 3). This accounted for a 16% increase in the relative risk for WHC occurrence in the DE arm (HR, 1.16; 95% CI, 0.81-1.64; P = 0.42). The results were confirmed considering the best-case scenario (Figure 4); drop out patients seem to have a different impact on the results, according to the above scenarios, especially in the DE arm, where 12.6% did not switch to EVR and therefore dropped out of the study (Table 2).
FIGURE 3.
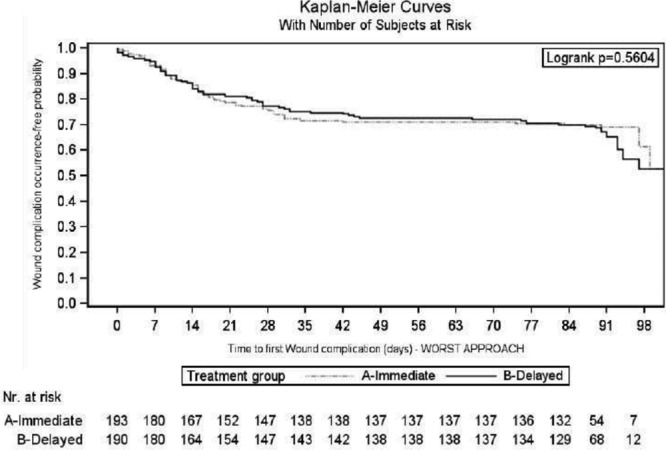
Kaplan-Meier curve of time to first wound healing complication during the first 3 mo after transplantation: worst-case scenario approach (intent-to-treat population). Nr. at Risk, number at risk.
FIGURE 4.
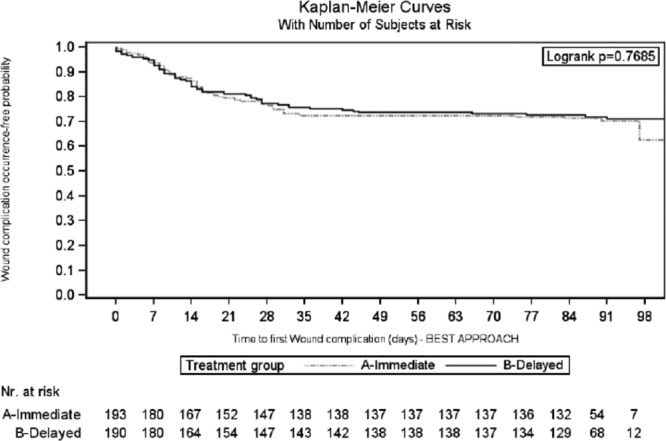
Kaplan-Meier curve of time to first wound healing complication during the first 3 mo after transplantation: best-case scenario approach (intent-to-treat population).
TABLE 2.
WHC at 3 and 12 mo: ITT population
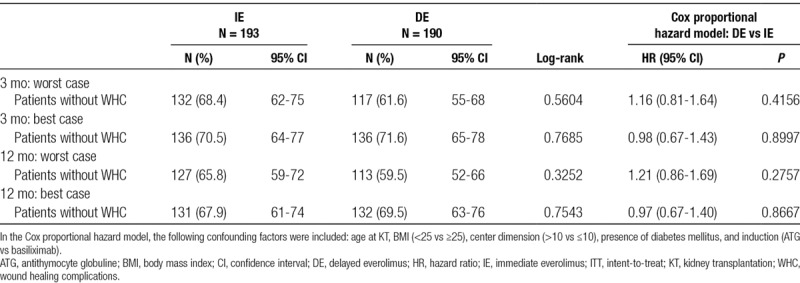
The most frequent complications were as follows: fluid collection (IE = 32 [16.6%] vs DE = 33 [17.4%]; P = 0.84) and lymphocele (IE = 20 [10.4%] vs DE = 30 [15.8%]; P = 012). A lower percentage of patients experienced lymphorrhea (IE = 5 [2.59%] vs DE = 13 [6.84%]; P = 0.05) and hematoma (IE = 14 [7.25%] vs DE = 5 [2.63%]; P = 0.04) (Table 3).
TABLE 3.
Wound healing complication details at 3 and 12 mo: ITT population
Similar results were observed over the entire follow-up period (12 mo), considering the worst- (Figure 5) and best-case (Figure 6) scenario (Table 2).
FIGURE 5.
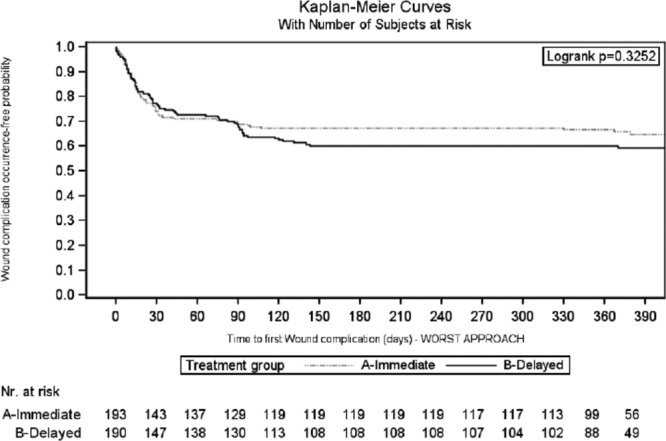
Kaplan-Meier curve of time to first wound healing complication during the 12 mo after transplantation: worst-case scenario approach (intent-to-treat population).
FIGURE 6.
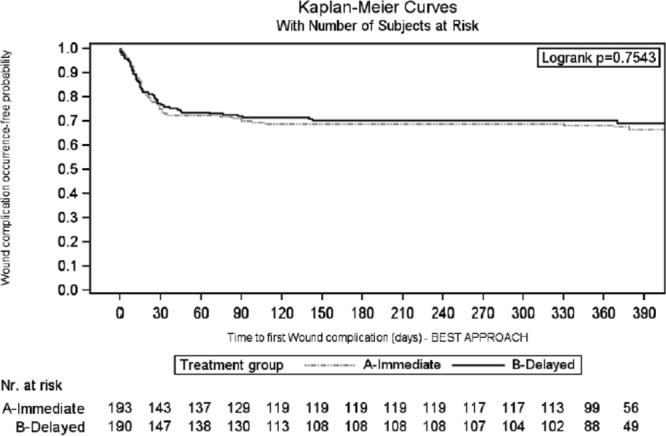
Kaplan-Meier curve of time to first wound healing complication during the 12 mo after transplantation: best-case scenario approach (intent-to-treat population).
After 12 months, the DE arm showed a greater incidence of lymphocele versus the IE arm (IE = 21 [10.88%] vs DE = 35 [18.42%]; P = 0.04); conversely, the occurrence of hematoma was greater in the IE arm (IE = 15 [7.77%] vs DE = 5 [2.63%]; P = 0.02) (Table 3).
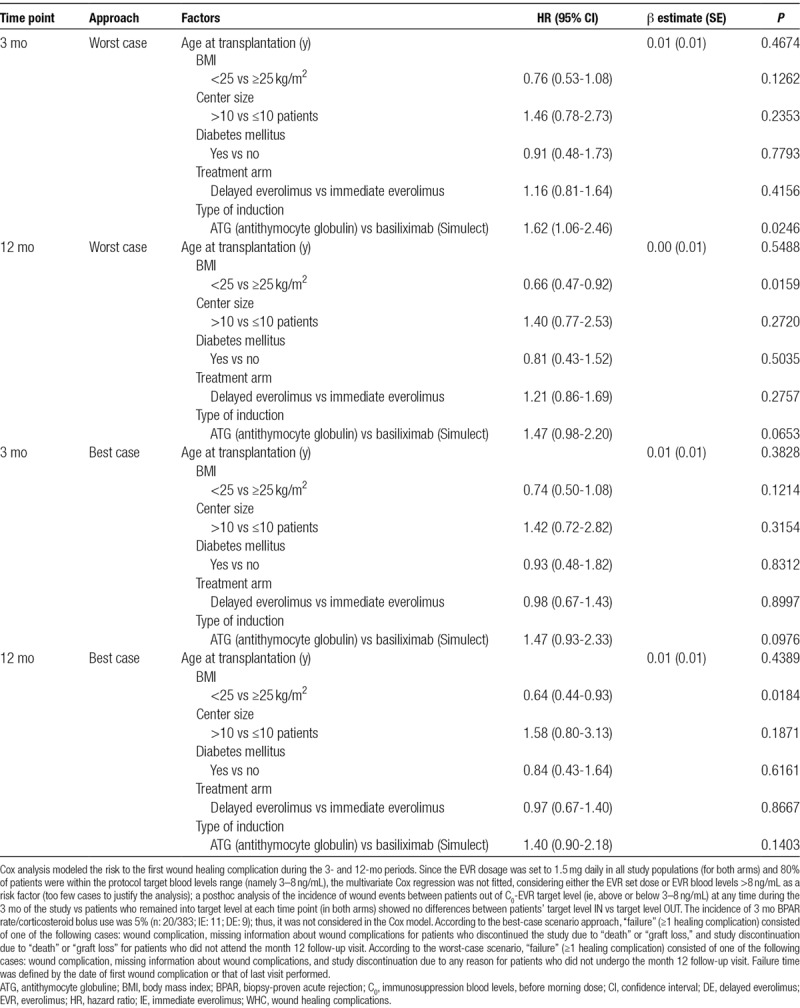
Considering the CORE phase and worst-case scenario, the multivariate Cox model identified ATG as a risk factor for the occurrence of WHC (HR, 1.62; 95% CI, 1.06-2.46; P = 0.02); however, these findings were not confirmed in the best-case scenario approach (HR, 1.47; 95% CI, 0.93-2.33; P = 0.10). BMI <25 kg/m2 was identified as a predictor of WHC-free status at 12 months, both in the worst (HR, 0.66; 95% CI, 0.47-0.92; P = 0.02) and best-case scenario (HR, 0.64; 95% CI, 0.44-0.93; P = 0.02) (Table 4).
TABLE 4.
Cox multivariate analysis on the main risk factors influencing the WHC
Secondary Efficacy Endpoints
At 3 months, considering the worst-case scenario, the composite efficacy treatment failure (ie, death/graft loss/BPAR) was 22 in the IE arm (11.4%) versus 40 (21.0%) in the DE arm (log-rank: P = 0.06; HR, 1.54; 95% CI, 0.90-2.64; P = 0.11). Fitting the best-case scenario approach, the treatment failure rate was lower in both arms (IE = 16 [8.3%] vs DE = 13 [6.8%]; log-rank: P = 0.57; HR, 0.63; 95% CI, 0.29-1.39; P = 0.25). The graft loss in IE was due to acute rejection (n = 3); primary nonfunction (n = 1); or graft artery thrombosis (n = 1), while in DE, it was due to renal vein thrombosis. The difference between the best- and the worst-case scenario approach was due to a difference between the arms in the dropout rate, since in the DE arm, 12% (24/190) of patients did not switch to EVR. Similar results were observed considering the 12-month follow-up period (Table 5).
TABLE 5.
Secondary efficacy endpoint at 3 and 12 mo: ITT population
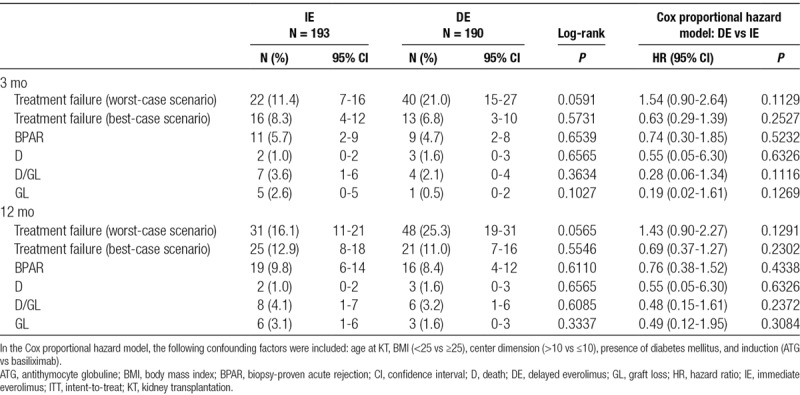
The 1-year patient and graft survival rates, in the IE and DE arms, were 99.0% versus 98.4% (log-rank: 0.6565) and 96.9% versus 98.4% (log-rank: 0.3337), respectively (Figures 7 and 8). Five patients died during the CORE study (IE = 2; DE = 3), due to acute myocardial infarction (IE = 1; DE = 1); cardiovascular accident (IE = 1; DE = 1); and cerebral hemorrhage (DE = 1). None of the deaths were considered by the investigators to be EVR related.
FIGURE 7.
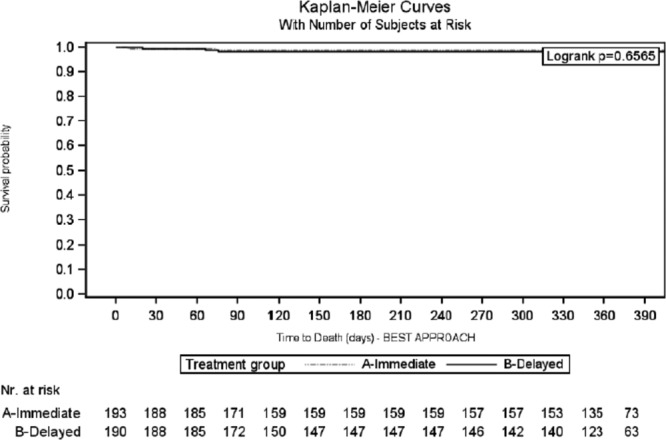
Patient survival analysis during the first 12 mo after transplantation: Kaplan-Meier curve (intent-to-treat population).
FIGURE 8.
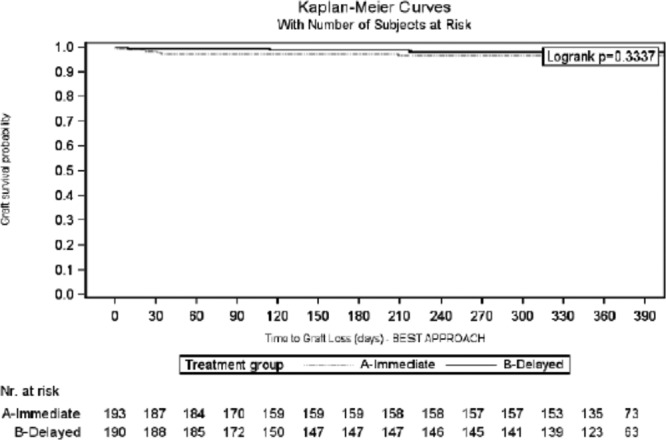
Graft survival analysis during the first 12 mo after transplantation: Kaplan-Meier curve (intent-to-treat population).
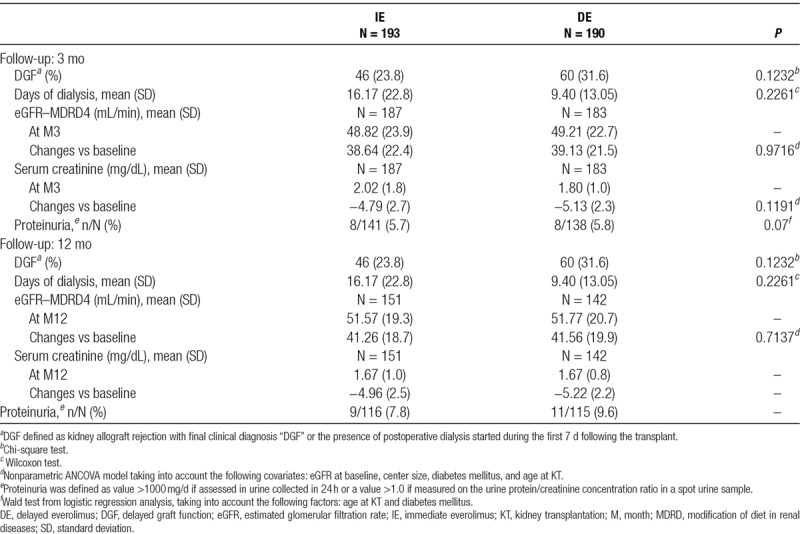
Considering the entire study period, no difference was observed either in BPAR (IE = 19 [9.84%] vs DE = 16 [8.42%]; P = 0.61) or in DGF (IE = 46 [23.8%] vs DE = 60 [31.6%]; P = 0.12) (Table 5).
No differences in renal function and proteinuria were observed at months 3 and 12 (Table 6).
TABLE 6.
Graft function
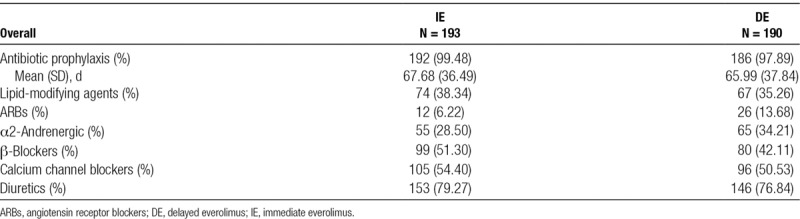
Relevant concomitant medications are listed in Table 7.
TABLE 7.
Concomitant medications
Adverse Events
There were no differences between the arms with regard to patients who experienced ≥1 AE/serious AE/infection or in the number of patients who discontinued treatment due to AE/infection (Table 8). Specifically, 171 patients (88.6%) in the IE arm versus 174 (91.6%) in the DE arm experienced ≥1 AE (P = 0.42); of these AEs, 71 (36.8%) in the IE arm and 53 (27.9%) in the DE arm were considered EVR related (P = 0.06). The shorter exposure to EVR in the DE arm and the fact that 12% of patients did not switch to EVR may have contributed to this result. Patients who showed ≥1 serious AE/infection in the IE versus DE arm were 73 (37.8%) and 61 (32.1%), respectively (P = 0.29). Patients who permanently or temporarily discontinued EVR due to AEs/infections in the IE versus DE arm were 29 (15.0%) versus 21 (11.1%) (P = 0.32) and 18 (9.3%) versus 23 (12.1%) (P = 0.47), respectively.
TABLE 8.
Adverse events

Thirty-three patients experienced ≥1 cytomegalovirus infection (IE = 14 [7.2%] and DE = 19 [10%]; P = 0.33). Of them, only 6 recipients (14%) received cytomegalovirus prophylaxis (P = 0.19). Eleven patients experienced new onset of diabetes mellitus (IE = 5 [3.1%] vs DE = 6 [4.1%]; P = 0.76) (Table 8).
Considering the overall cohort, 1 patient (in the DE arm) experienced a new occurrence of renal cancer.
DISCUSSION
The immediate introduction of EVR after KT does not increase the risk of WHC. In fact, in our population, the DE use was not associated with a decreasing risk of WHC versus those who received IE. Both the worst- and best-case scenario of this analysis—which were fitted to avoid any bias due to missing information—clearly showed that no difference in terms of WHC was identified between the arms. The immediate use of EVR in the study period resulted in a WHC-free rate between 68% and 70% (considering the worst- and best-case approach) versus 62% and 72% in those who received a delayed dose; the most common complications in IE were fluid collection (17%), lymphocele (10%), and wound dehiscence (6%), which were not different at 3 months from the DE arm. Interestingly, at 12 months, the DE arm showed a higher incidence of lymphocele, while hematoma seemed to be more frequent in the IE arm. The risk of WHC increased by >60% in case of use of ATG induction, confirming what already stated by Pourmand et al32 in 2012, suggesting that Ab-IL2-R (namely Basiliximab) should be an induction of choice in mTORi-based IS (also in the delayed introduction protocol). The risk also increases in obese recipients (BMI, >30 kg/m2)27; in fact, in our series, BMI <25 kg/m2 proved to have a protective role on WHC; therefore, we suggest to avoid a combination therapy of ATG and mTORi, especially in overweight recipients to decrease the “synergistic effects” on WHC.
Even if no robust data had previous showed the clear role of mTORi on WHC in the KT setting, these results seem to be consistent with the preliminary issues and previously mentioned CALLISTO study, in which no difference was observed in the incidence or severity of WHC in KT recipients receiving either micophenolate mofetil (MMF) or EVR as de novo immunosuppressive drug.28
These findings, on the contrary, differ from the studies on sirolimus-based IS, since sirolimus seems to lead to WHC following KT17,19-22; the intriguing question thus arises as to why a difference may potentially exist between each other. Pharmacokinetic variations (higher bioavailability and shorter half-life of EVR)33-35 or the loading doses and high exposure level of sirolimus immediately after KT may partly contribute to explaining the difference between the drugs. The high sirolimus exposure (namely C0, 8–30 ng/mL) in the first clinical experiences and association with MPA in CNI-free protocol immediately after transplantation can explain the unfavorable effect on wound healing.26
In 2013, Cooper et al36 showed that the higher blood level of EVR (namely >8 ng/mL) was also associated with an increasing risk (HR, 1.69; 95% CI, 1.20-2.38; P = 0.002) of WHC and the initial dose of 1.5 mg seems to be more protective than 3 mg with regard to WHC. Even if the present study has not explored the role of EVR blood levels on the incidence of WHC (only 10% of patients in the IE arm were above 3–8 ng/mL), we are strongly convinced that a dose adjustment aimed at maintaining a level between 3 and 8 ng/mL is fundamental to decrease or avoid the WHC.
The role of EVR on wound healing was also investigated in heart transplantation by the so-called EVERHEART study. Similar in study design to the present trial, the study showed no superiority in terms of WHC in the DE arm; however, similarly to CALLISTO, the study was not powered for WHC only, but for composite end-points (ie, wound healing delays, pericardial and pleural effusion, and renal insufficiency). Therefore, it was not fit to investigate the final role of EVR in wound healing.33
In the study period, treatment failure does not significantly differ between the arms, but—when considering the entire follow-up period (12 mo) and worst-case scenario—the immediate introduction of EVR seems to be superior, mostly in the graft loss and death rates; this results, however, should not be considered consistent, since they were not confirmed in the best-case scenario, so they cannot be considered conclusive. The 12-month BPAR rate in the IE arm was about 10%, therefore over 10% less than in the CALLISTO study; this first of all confirms the high efficacy of the IE regimen, and also indicates that a high CNI-exposure immediately after KT can be safely avoided. This can also be confirmed by the rate of DGF; as a matter of fact, the IE and DE arms showed the same DGF rates (23% vs 30%); these results are completely in accordance with the CALLISTO study (25%) and larger Symphony study,19 which reported DGF rates ranging between 32% and 36% in CNI-treated recipients. From the current study and CALLISTO series, we can assert—albeit in disagreement with other single experiences17,18,34,35—that the immediate use of mTORi does not influence the initial poor function in KT, a finding that was also confirmed by a similar renal function assessed between the treatment arms throughout the follow-up.
Finally, permanent or temporary discontinuations of EVR were much less than in the CALLISTO study; indeed, in our series, the IE arm permanently discontinued therapy in only 15% of the cases and temporarily in 9%, while in the DE arm, discontinuation occurred in about 12% of the cases. Controversially, the CALLISTO series reported a 25% discontinuation rate; this could be explained—as stated by the authors themselves—by the higher EVR trough levels reached in the DE arm in order, we argue, to avoid an allograft rejection after a decrease in the dose of CNI and the discontinuation of MPA.
The main drawback of the present study is that about 20% of patients in the IE arm and 25% in the DE arm did not complete the CORE-phase study, resulting in a slightly decrease in the previous sample size powered for the aim of the study. In addition, patients were followed up to 3 months, and some WHCs (ie, lymphocele and incisional hernia) need more time to be evaluated conclusively. This limitations were managed adding a follow-up at 12 months even if, during this observational period, patients were treated—as per clinical practice—in 22 different centers, and therefore, they were monitored less strictly than during the first 3 months. Furthermore, the article is not generalizable to all KT patients since it lack the presence of severe obese recipients that could sustain WHC.
Although the enrollment of a small proportion of living KT donors could seem to be a limitation of the study, we think that it is representative of the real setting of KT in Italy37 without affecting the study end-points, since only 5% of the study cohort received a kidney from living donors.
In conclusion, treating patients with DE-based IS after KT does not decrease the risk of WHC after KT; hence, de novo EVR does not expose KT recipients to a higher risk of WHC and also maintains a good efficacy and safety profile. Further studies are needed to confirm the clear role of ATG on WHC, since in the current trial a risk factor was considered only when a worst-case scenario analysis was fitted.
ACKNOWLEDGMENTS
The authors would like to thank Marta Bartezaghi and Roberto Orsenigo, at Novartis Farma Italia, for their statistical and editorial assistance.
Footnotes
Clinical Trial Notation: www.clinicaltrial.gov; NCT01410448.
T.M.M. is the author of the article. M.C. involved in substantial contributions to the work conception. P.T., A.S., S.S., and E.M. involved in data acquisition. L.E. involved in critical revision of the article for important intellectual content. G.S., F.P., G.B.P., and G.C. involved in participation in research. G.T. involved in revision and final approval.
The authors declare no conflicts of interest.
This work was supported by Novartis Farma Italia.
REFERENCES
- 1.Pascual J. Everolimus in clinical practice--renal transplantation. Nephrol Dial Transplant 200621Suppl 3iii18–iii23 [DOI] [PubMed] [Google Scholar]
- 2.Nashan B. Induction therapy and mTOR inhibition: minimizing calcineurin inhibitor exposure in de novo renal transplant patients. Clin Transplant 201327Suppl 2516–29 [DOI] [PubMed] [Google Scholar]
- 3.Budde K, Zeier M, Witzke O, et al. ; HERAKLES Study Group Everolimus with cyclosporine withdrawal or low-exposure cyclosporine in kidney transplantation from month 3: a multicentre, randomized trial. Nephrol Dial Transplant 2017321060–1070 [DOI] [PubMed] [Google Scholar]
- 4.Carmellini M, Collini A, Ruggieri G, et al. Excellent long-term results in de novo renal transplant recipients treated with proliferation signal inhibitors and reduced calcineurin inhibitors exposure. Transplant Proc 2008401858–1861 [DOI] [PubMed] [Google Scholar]
- 5.Ponticelli C, Scolari MP. Calcineurin inhibitors in renal transplantation still needed but in reduced doses: a review. Transplant Proc 2010422205–2208 [DOI] [PubMed] [Google Scholar]
- 6.Schuler W, Sedrani R, Cottens S, et al. SDZ RAD, a new rapamycin derivative: pharmacological properties in vitro and in vivo. Transplantation 19976436–42 [DOI] [PubMed] [Google Scholar]
- 7.Dunn C, Croom KF. Everolimus: a review of its use in renal and cardiac transplantation. Drugs 200666547–570 [DOI] [PubMed] [Google Scholar]
- 8.Vitko S, Tedesco H, Eris J, et al. Everolimus with optimized cyclosporine dosing in renal transplant recipients: 6-month safety and efficacy results of two randomized studies. Am J Transplant 20044626–635 [DOI] [PubMed] [Google Scholar]
- 9.Tedesco-Silva H, Jr, Vitko S, Pascual J, et al. ; 2306 and 2307 Study Groups 12-month safety and efficacy of everolimus with reduced exposure cyclosporine in de novo renal transplant recipients. Transpl Int 20072027–36 [DOI] [PubMed] [Google Scholar]
- 10.Chan L, Greenstein S, Hardy MA, et al. ; CRADUS09 Study Group Multicenter, randomized study of the use of everolimus with tacrolimus after renal transplantation demonstrates its effectiveness. Transplantation 200885821–826 [DOI] [PubMed] [Google Scholar]
- 11.Nashan B, Curtis J, Ponticelli C, et al. ; 156 Study Group Everolimus and reduced-exposure cyclosporine in de novo renal-transplant recipients: a three-year phase II, randomized, multicenter, open-label study. Transplantation 2004781332–1340 [DOI] [PubMed] [Google Scholar]
- 12.Schuurman HJ, Pally C, Weckbecker G, et al. SDZ RAD inhibits cold ischemia-induced vascular remodeling. Transplant Proc 1999311024–1025 [DOI] [PubMed] [Google Scholar]
- 13.Farb A, John M, Acampado E, et al. Oral everolimus inhibits in-stent neointimal growth. Circulation 20021062379–2384 [DOI] [PubMed] [Google Scholar]
- 14.Nishimura T, Faul JL, Berry GJ, et al. 40-O-(2-hydroxyethyl)-rapamycin attenuates pulmonary arterial hypertension and neointimal formation in rats. Am J Respir Crit Care Med 2001163498–502 [DOI] [PubMed] [Google Scholar]
- 15.Waksman R, Pakala R, Baffour R, et al. Optimal dosing and duration of oral everolimus to inhibit in-stent neointimal growth in rabbit iliac arteries. Cardiovasc Revasc Med 20067179–184 [DOI] [PubMed] [Google Scholar]
- 16.Cole OJ, Shehata M, Rigg KM. Effect of SDZ RAD on transplant arteriosclerosis in the rat aortic model. Transplant Proc 1998302200–2203 [DOI] [PubMed] [Google Scholar]
- 17.Troppmann C, Pierce JL, Gandhi MM, et al. Higher surgical wound complication rates with sirolimus immunosuppression after kidney transplantation: a matched-pair pilot study. Transplantation 200376426–429 [DOI] [PubMed] [Google Scholar]
- 18.Goel M, Flechner SM, Zhou L, et al. The influence of various maintenance immunosuppressive drugs on lymphocele formation and treatment after kidney transplantation. J Urol 20041711788–1792 [DOI] [PubMed] [Google Scholar]
- 19.Ekberg H, Tedesco-Silva H, Demirbas A, et al. ; ELITE-Symphony Study Reduced exposure to calcineurin inhibitors in renal transplantation. N Engl J Med 20073572562–2575 [DOI] [PubMed] [Google Scholar]
- 20.Langer RM, Kahan BD. Incidence, therapy, and consequences of lymphocele after sirolimus-cyclosporine-prednisone immunosuppression in renal transplant recipients. Transplantation 200274804–808 [DOI] [PubMed] [Google Scholar]
- 21.Valente JF, Hricik D, Weigel K, et al. Comparison of sirolimus vs. mycophenolate mofetil on surgical complications and wound healing in adult kidney transplantation. Am J Transplant 200331128–1134 [DOI] [PubMed] [Google Scholar]
- 22.Dean PG, Lund WJ, Larson TS, et al. Wound-healing complications after kidney transplantation: a prospective, randomized comparison of sirolimus and tacrolimus. Transplantation 2004771555–1561 [DOI] [PubMed] [Google Scholar]
- 23.Kuppahally S, Al-Khaldi A, Weisshaar D, et al. Wound healing complications with de novo sirolimus versus mycophenolate mofetil-based regimen in cardiac transplant recipients. Am J Transplant 200665 Pt 1986–992 [DOI] [PubMed] [Google Scholar]
- 24.Zuckermann A, Manito N, Epailly E, et al. Multidisciplinary insights on clinical guidance for the use of proliferation signal inhibitors in heart transplantation. J Heart Lung Transplant 200827141–149 [DOI] [PubMed] [Google Scholar]
- 25.Fine NM, Kushwaha SS. Recent advances in mammalian target of rapamycin inhibitor use in heart and lung transplantation. Transplantation 20161002558–2568 [DOI] [PubMed] [Google Scholar]
- 26.Nashan B, Citterio F. Wound healing complications and the use of mammalian target of rapamycin inhibitors in kidney transplantation: a critical review of the literature. Transplantation 201294547–561 [DOI] [PubMed] [Google Scholar]
- 27.Tiong HY, Flechner SM, Zhou L, et al. A systematic approach to minimizing wound problems for de novo sirolimus-treated kidney transplant recipients. Transplantation 200987296–302 [DOI] [PubMed] [Google Scholar]
- 28.Dantal J, Berthoux F, Moal MC, et al. ; RAD A2420 Study Group Efficacy and safety of de novo or early everolimus with low cyclosporine in deceased-donor kidney transplant recipients at specified risk of delayed graft function: 12-month results of a randomized, multicenter trial. Transpl Int 2010231084–1093 [DOI] [PubMed] [Google Scholar]
- 29.Lich R, Jr, Howerton LW, Davis LA. Childhood urosepsis. J Ky Med Assoc 1961591177–1179 [PubMed] [Google Scholar]
- 30.Gregoir W. Congenital vesico-ureteral reflux. Acta Urol Belg 196230286–300 [PubMed] [Google Scholar]
- 31.Rodriguez BL, Abbott RD, Fujimoto W, et al. ; American Diabetes Association; World Health Organization The American Diabetes Association and World Health Organization classifications for diabetes: their impact on diabetes prevalence and total and cardiovascular disease mortality in elderly Japanese-American men. Diabetes Care 200225951–955 [DOI] [PubMed] [Google Scholar]
- 32.Pourmand GR, Dehghani S, Saraji A, et al. Relationship between post-kidney transplantation antithymocyte globulin therapy and wound healing complications. Int J Organ Transplant Med 2012379–84 [PMC free article] [PubMed] [Google Scholar]
- 33.Potena L, Pellegrini C, Grigioni F, et al. ; EVERHEART Investigators Optimizing the safety profile of everolimus by delayed initiation in de novo heart transplant recipients: results of the prospective randomized study EVERHEART. Transplantation 2018102493–501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barsoum RS, Morsey AA, Iskander IR, et al. The Cairo kidney center protocol for rapamycin-based sequential immunosuppression in kidney transplant recipients: 2-year outcomes. Exp Clin Transplant 20075649–657 [PubMed] [Google Scholar]
- 35.Boratynska M, Banasik M, Patrzalek D, et al. Impact of sirolimus treatment in kidney allograft recipients with prolonged cold ischemia times: 5-year outcomes. Exp Clin Transplant 2008659–66 [PubMed] [Google Scholar]
- 36.Cooper M, Wiseman AC, Zibari G, et al. Wound events in kidney transplant patients receiving de novo everolimus: a pooled analysis of three randomized controlled trials. Clin Transplant 201327E625–E635 [DOI] [PubMed] [Google Scholar]
- 37.National Transplant Center. Transplants. Available at http://www.trapianti.salute.gov.it. Accessed April 2019.


