Look for this and other related articles in Instructional Course Lectures, Volume 58, which will be published by the American Academy of Orthopaedic Surgeons in February 2009:
“Prevention of Symptomatic Pulmonary Embolism in Patients Undergoing Total Hip and Total Knee Arthroplasty: Clinical Guidelines of the American Academy of Orthopaedic Surgeons,” by Paul F. Lachiewicz, MD
Femoroacetabular impingement is a relatively recently described condition in which an abnormally shaped proximal part of the femur causes interference between the femoral head-neck junction and the acetabular rim1,2. Although this can occur in normal hips with an increased range of movement, the condition is usually due to abnormal morphology of the hip. Two mechanisms have been described1.
Cam-type impingement is caused by insufficient concavity of the femoral head-neck junction anterolaterally. This has been referred to as a pistol grip deformity3 or a head tilt deformity4. As a consequence, this region of the femoral head has an increased radius of curvature that is too large for the tightly congruent acetabulum. The repeated movement of the deformed femoral head in and out of the acetabulum produces shearing of the labrum and the adjacent acetabular cartilage. This can cause the labrum and articular cartilage to delaminate from the subchondral bone5,6. This damage is consistently seen at the anterosuperior aspect of the acetabular rim. The deformity may be secondary to Legg-Calvé-Perthes disease7 or slipped capital femoral epiphysis8,9; however, the large majority of patients do not have a history of childhood hip problems10.
Pincer-type impingement is caused by overcoverage of the femoral head by the acetabulum. This leads to contact of the labrum against the femoral neck during physiological hip motion11,12. The labrum eventually fails, but damage to the articular cartilage is initially limited to the acetabular rim2. Heterotopic bone growth can occur at the base of the labrum in response to the repeated microtrauma. Pincer-type impingement may be associated with hip dysplasia13 or may be created by overcorrection after periacetabular osteotomy14, but more commonly it is due to a retroverted acetabulum producing impingement anteriorly or coxa profunda producing global impingement. These two classic forms of impingement (cam and pincer) were shown by Beck et al.2 to coexist in a large percentage of cases: 47% (twenty-seven) of fifty-seven hips with cam impingement in their series had an associated acetabular deformity and 63% (thirty-four) of fifty-four hips with pincer impingement had an abnormally shaped femoral head. However, to what degree each coexisting deformity contributes to the intra-articular cartilage damage has yet to be clearly defined.
Diagnosis
Patients typically present with groin pain, usually of insidious onset and sometimes exacerbated by activity. The pain may be felt as the patient starts to walk after rising from a sitting position or it may be a dull groin ache while the patient has the hip in a flexed position. The latter can cause difficulty with sitting at a desk for a prolonged period or with traveling a long distance by automobile or airplane1,2,15. Patients with cam-type impingement most often have the onset of symptoms during their thirties, although the symptoms may occur earlier. Men are more commonly affected and, although the deformity is often bilateral, patients usually have symptoms on only one side. Pincer-type impingement is more common in females and often presents as groin pain after activity in patients in their forties16.
The results of the physical examination may be normal, but most patients have a slightly antalgic gait. Typically, the patient has <20° of internal rotation with the hip in 90° of flexion and a positive impingement sign, which is groin pain with internal rotation combined with adduction of the lower limb with the hip in 90° of flexion17 (Fig. 1). Wyss et al.18 found a strong correlation between a lack of internal rotation of the flexed hip and a lack of space between the acetabular rim and the femoral head-neck junction on magnetic resonance imaging. The abdomen and lower back should be examined to exclude referred pain, and an injection of bupivacaine into the hip joint may help to establish that the pain is from the joint.
Fig. 1.
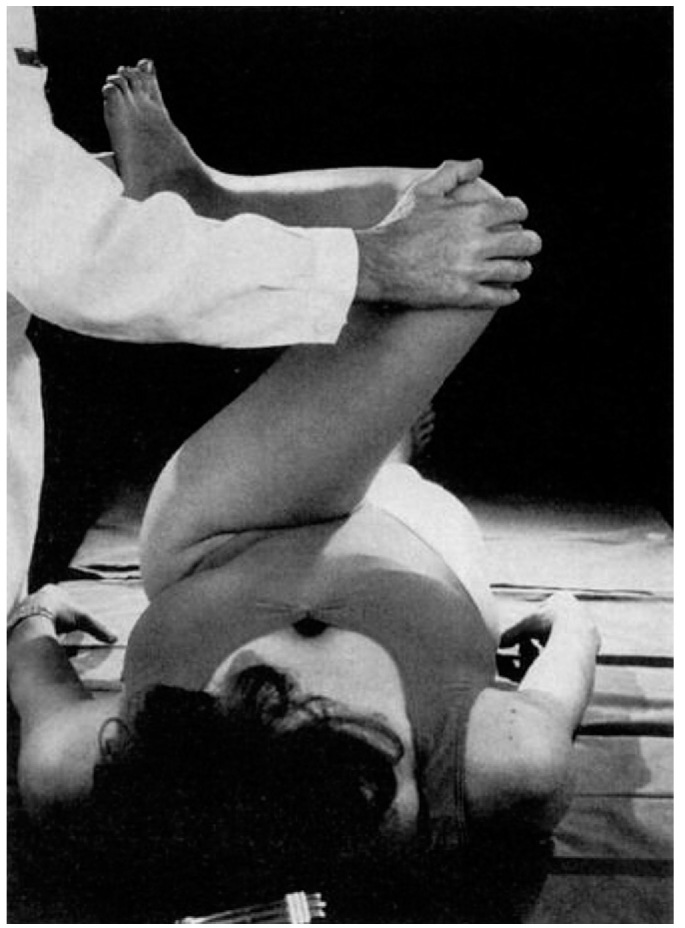
Impingement sign of the hip elicited by forced flexion, adduction, and internal rotation. (Reproduced, with permission and copyright © of the British Editorial Society of Bone and Joint Surgery, from: Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423-9.)
Investigations
Cam-type impingement is characterized by asphericity of the femoral head. As the abnormality is typically in the anterolateral portion of the head-neck junction, it may not be seen on an anteroposterior pelvic radiograph or a simple lateral radiograph of the hip19,20. A cross-table lateral view (with the hip in 10° of internal rotation) or a Dunn view (described below) is required (Fig. 2)21. The authors of most studies have used an α angle (the angle between the axis of the neck and the point where the bone of the head-neck junction crosses outside the radius of curvature of the head) of >50.5° to diagnose the abnormality20,22,23. In addition, a head-neck offset ratio21 of ≤0.15 on the cross-table lateral radiograph has been reported to have a sensitivity and specificity of 68% and 82%, respectively, for the diagnosis of cam impingement19,21. The offset ratio is measured by dividing the anterior offset by the femoral head diameter. The anterior offset is the distance between two parallel lines, one adjacent to the anterior aspect of the neck and the other touching the most anterior part of the femoral head and both parallel to the femoral neck axis. In a comparison of four different lateral radiographic views used to detect femoral head asphericity, Meyer et al.20 found that the modified Dunn view (an anteroposterior radiograph of the hip in neutral rotation, 20° of abduction, and 45° of flexion) was the most sensitive and the cross-table lateral view (with the hip in 10° of internal rotation) and the standard Dunn view (an anteroposterior radiograph of the hip in neutral rotation, 20° of abduction, and 90° of flexion) were quite satisfactory.
Fig. 2.
The impinging lesion can be underestimated on the basis of a standard lateral radiograph (left image). The Dunn radiograph (right image) is more accurate for the assessment of the abnormality.
The anteroposterior pelvic radiograph is the most valuable study for confirming retroversion or coxa profunda in a patient suspected of having pincer-type impingement2,11. Pelvic positioning must be considered when interpreting the radiographic signs associated with pincer impingement. With the coccyx and symphysis pubis aligned, the pelvis should be in neutral flexion-extension, which means that the distance between the top of the pubic symphysis and the sacrococcygeal junction should be 32 mm for men and 47 mm for women24. The retroverted acetabulum is recognized on the basis of one of three findings: the anterior wall of the acetabulum crossing the posterior wall (the so-called crossover sign11), the center of the femoral head lying lateral to the posterior wall (the so-called posterior wall sign12), or the ischial spine projecting into the pelvic cavity on the anteroposterior pelvic radiograph (the so-called ischial sign25) (Fig. 3). Coxa profunda is recognized on the anteroposterior pelvic radiograph when the medial wall of the acetabulum lies on or medial to the ilioischial line; protrusio, which represents the more severe form of coxa profunda, is diagnosed when the femoral head crosses the ilioischial line2.
Fig. 3.
Anteroposterior pelvic radiograph of a twenty-four-year-old woman with evidence of acetabular retroversion. The crossover sign can be seen on both sides, where the anterior wall of the acetabulum crosses the posterior wall, and the ischial sign is present on both sides, as the ischial spine is visible.
Magnetic resonance imaging with gadolinium arthrography and computed tomography are useful as additional investigations to confirm the impingement deformity as well as to identify associated pathological changes and to facilitate surgical planning23,26. Computed tomography scans provide three-dimensional surface renderings of the impingement deformity and aid in determining the area of resection to correct femoral head asphericity23. Magnetic resonance imaging with gadolinium arthrography can demonstrate abnormalities of the acetabular rim such as labral tears27, paralabral cysts, and cartilage delamination6. One of us (M.L.) and colleagues28 demonstrated that magnetic resonance imaging is useful for distinguishing dysplasia from impingement. When there is impingement, the labrum may be normal in size or small, in contrast to the hypertrophied labrum associated with a dysplastic acetabulum28. Fibrocystic changes at the femoral head-neck junction (also known as Pitt's pit), which are often visible on plain radiographs but are more easily seen on computed tomography or magnetic resonance imaging scans, have been reported to be 91% specific and to have a positive predictive value of 71% for the diagnosis of femoroacetabular impingement26. When the plain radiographic examination is inconclusive, both magnetic resonance imaging and computed tomography scans provide radial images of the anatomy of the femoral head-neck junction that are more sensitive in detecting abnormal α angles as well as acetabular version19.
Management
Although we are not aware of any longitudinal studies on the issue, there is evidence that femoroacetabular impingement is a leading cause of so-called primary osteoarthritis of the hip1,2,16. Therefore, early intervention is aimed not only at providing pain relief and improving function but also at delaying and/or preventing subsequent osteoarthritis. Although we are not aware of any long-term follow-up studies demonstrating that the onset of osteoarthritis can be prevented and/or delayed with surgery, Beck et al.5 reported no progression of joint space narrowing in nineteen hips at 4.7 years after surgical treatment of femoroacetabular impingement. However, it is becoming more apparent that one of the greatest challenges in treating femoroacetabular impingement is dealing with the associated damage to the acetabular labral chondral complex, which can range from fraying or irritation of the labral tip to large delaminated flaps of cartilage and/or chondral defects of the acetabulum2,29,30. In addition, the treatment of delamination of acetabular cartilage is still evolving: localized débridement may be sufficient for small acetabular cartilage flaps, whereas larger lesions may require rim trimming in order to restore a stable cartilage edge30. In addition, one must consider the underlying morphological abnormality causing the impingement (cam or pincer, or both); the presence or absence of deformity of the proximal part of the femur; and the physiological age of the patient, especially one with early arthritic changes (1 to 2 mm of joint space narrowing), in whom a joint replacement may offer a more predictable outcome. In contrast to patients with advanced hip arthritis, joint-preserving surgical interventions may be inappropriate for a patient with relatively mild symptoms and/or of advanced age whereas, for young patients, joint preservation to delay and/or prevent arthritis may make even an open approach and femoral head dislocation appropriate. To summarize, the following clinical factors should most strongly influence how one treats a patient with femoroacetabular impingement: (1) the physiological age of the patient; (2) joint space narrowing of 1 to 2 mm; (3) the extent of damage to the acetabular labral chondral complex; (4) in patients with pincer-type impingement, the severity of acetabular retroversion with or without the presence of cam-type impingement; and (5) in those with cam-type impingement, the absence or presence of proximal femoral deformity (for example, a high-riding greater trochanter) and the extent of head asphericity.
The best time for surgery is unknown. Symptoms are usually not as severe as those in patients requiring a joint replacement, and delaying surgery may lead to irreversible cartilage damage. Nevertheless, a course of nonoperative management, consisting of activity modification, anti-inflammatory medication, and range-of-motion exercises, is advisable in most cases. It is not clear if patients benefit substantially from such a regimen, however31.
There are three categories of surgical techniques for the treatment of femoroacetabular impingement: (1) a fully open surgical procedure in which the femoral head is dislocated, providing full access for the correction of cam impingement as well as trimming of the acetabular rim as needed; (2) an arthroscopic technique, wherein the correction is done either arthroscopically only or combined with an arthrotomy (but the femoral head is not dislocated); and (3) a periacetabular osteotomy performed for certain forms of pincer-type impingement. Most patients with femoroacetabular impingement have a mixed type of impingement, and as yet there is no clear information about how to establish the predominant impingement type or if treatment of the cam or pincer-type deformity in isolation is sufficient.
Open Hip Surgery with Dislocation of the Femoral Head
The indications for this approach include (1) cam-type impingement with or without proximal femoral deformity, (2) pincer-type impingement associated with cam-type deformity, and (3) cam-type impingement with 1 mm of joint space narrowing as this approach would allow possible conversion to arthroplasty.
Dislocation of the femoral head allows complete access to both the femoral head-neck junction and the acetabular rim32. The recommended technique for surgical dislocation was developed by Ganz et al.33 for the treatment of intra-articular hip pathology. With this technique, the femoral head vascularity is protected and osteonecrosis is avoided. In brief, the patient is placed in the lateral decubitus position, and the incision is centered over the greater trochanter and angulated slightly posteriorly. After the iliotibial band is released, the posterior border of the gluteus medius and minimus is marked. A trochanteric slide osteotomy is performed with a small sleeve of the gluteus medius left attached and with the vastus lateralis left attached to the trochanteric fragment. The osteotomy must be extracapsular and lateral to the piriformis fossa to avoid damage to the blood supply34. The trochanteric slide osteotomy is mobilized anteriorly, and the femoral head is dislocated anteriorly. This allows a complete view of the femoral head.
Both Beck et al.5 and Murphy et al.32 reported that, in their early experience with the treatment of femoroacetabular impingement with use of the surgical dislocation technique of Ganz et al.33, the result was good to excellent in >65% of cases. In a subsequent study, Espinosa et al.35 reported significantly better outcomes (a 94% rate of good to excellent results) when the labrum had been preserved as compared with when it had been resected (p = 0.01) (Figs. 4-A and 4-B). After following the principles of labral preservation through partial débridement or refixation, Peters and Erickson29 and one of us (P.E.B.) and colleagues30 reported good to excellent clinical scores in >80% of cases, which was an improvement compared with the results in the initial series reported by Beck et al. and Murphy et al. On the basis of these results, surgical dislocation appears to be a safe and effective technique for joint preservation that does not lead to osteonecrosis8. However, this technique has risks. Ganz et al.33 reported two cases of sciatic neurapraxia, three trochanteric nonunions, and eleven cases of clinically relevant heterotopic ossification in a series of 213 hips. In addition, one of us (P.E.B.) and colleagues30 reported ten reoperations directly related to the approach (e.g., screw removal or trochanteric nonunion).
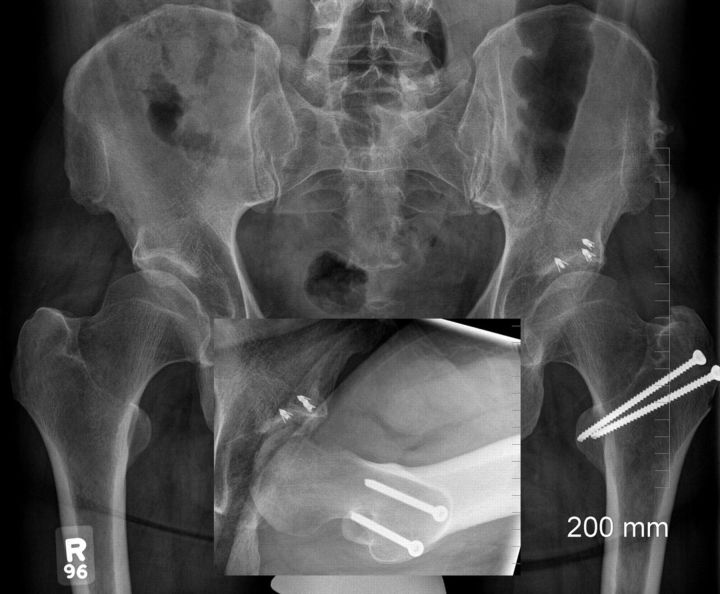
Fig. 4-A A fifty-one-year-old man presented with bilateral hip and groin pain, which was worse on the left. The left hip had caused him discomfort for about twenty years, affecting his activities of daily living and limiting the distance that he was able to walk. The asphericity of the femoral heads and the short acetabular roofs are seen on the anteroposterior radiograph. The diminished anterior concavity of the femoral head is seen on the Dunn radiograph (inset). Fig. 4-B The patient underwent surgical dislocation with osteochondroplasty of the femoral head-neck junction. Labral refixation was performed after the rim was trimmed in order to remove exposed subchondral bone and perform microfracture of the damaged articular surface. The restored head-neck offset is seen on the Dunn radiograph (inset).
Fig. 4-A.
Fig. 4-B.
Periacetabular Osteotomy
The indication for periacetabular osteotomy is acetabular retroversion with an associated posterior wall sign.
A retroverted acetabulum is caused by external rotation of the entire acetabulum36. This produces overcoverage of the anterior aspect of the femoral head and less-than-normal coverage of the posterior part of the femoral head. This altered relationship between the anterior and posterior aspects of the hip leads to the posterior wall sign. This abnormality can be corrected with a periacetabular osteotomy (Figs. 5-A and 5-B), which can also be used to correct a retroverted acetabulum associated with a dysplastic hip37. The cartilage in the anterosuperior aspect of the acetabulum must be intact for a periacetabular osteotomy to be recommended; if it is not intact, acetabular reorientation will place poor cartilage in the main weight-bearing area. Siebenrock et al.12 reported the results of periacetabular osteotomy in the treatment of femoroacetabular impingement secondary to a retroverted acetabulum in twenty-nine hips in twenty-two patients. In conjunction with the periacetabular osteotomy, an anterior hip arthrotomy was performed in twenty-six hips in order to reshape the femoral head-neck junction. The result was good or excellent for twenty-six hips, and the average Merle d'Aubigné score improved from 14.0 points preoperatively to 16.9 postoperatively. Three patients required a reoperation, one because of loss of correction, one because of posteroinferior impingement, and one because of recurrent signs of anterior impingement (due to insufficient correction and lack of a head-neck offset). Pincer impingement due to relative prominence of the anterior wall (the crossover sign) with an absent posterior wall sign (i.e., with the lateral aspect of the posterior wall lateral to the center of the femoral head) is best addressed with localized trimming of the rim, whereas coxa profunda requires global rim trimming; both procedures are best done with open surgery by means of surgical dislocation.
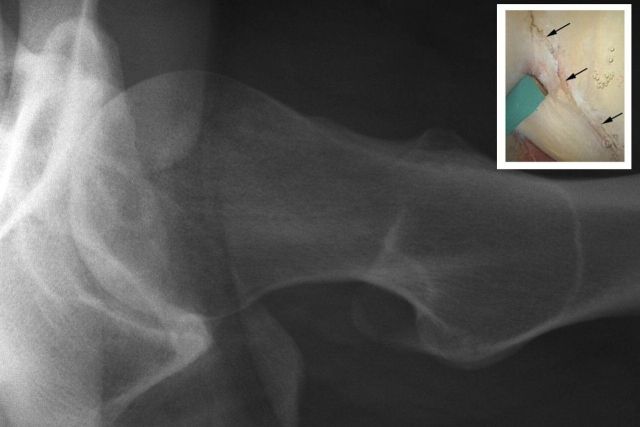
Fig. 5-A An eighteen-year-old male professional ice hockey player complained of persistent pain in the right hip. Retroversion of the acetabulum with deficiency of the posterior acetabular wall (the lateral edge of the posterior wall lying medial to the femoral head center) is seen on the anteroposterior radiograph. Diminished anterior concavity of the femoral neck is seen on the cross-table lateral radiograph (inset). Fig. 5-B One year after a periacetabular osteotomy, the anteroposterior radiograph showed that the crossover sign has been corrected. The anterior concavity of the femoral neck has been restored (inset).
Fig. 5-A.
Fig. 5-B.
Hip Arthroscopy Combined with a Mini-Anterior (Hueter) Hip Arthrotomy
Hip arthroscopy can be combined with a mini open anterior (Hueter) arthrotomy as described by Frederic Laude (personal communication, 1999). The arthroscopy is performed first to inspect the joint as well as to treat labral and chondral pathology. Then the anterior hip arthrotomy is performed to correct a cam deformity, which is most commonly located on the anterior aspect of the femoral head-neck junction. In addition, it is possible to detach the labrum anteriorly in order to trim the acetabular rim. The direct anterior approach involves a dissection within the fascial sheath of the tensor fasciae latae to minimize the risk of damage to the lateral femoral cutaneous nerve. The fascia over the rectus femoris is then released, the rectus femoris is retracted medially, and a T-shaped capsulotomy is performed. Clohisy and McClure37 argued that performance of the anterior hip arthrotomy allows a better exposure of the femoral head-neck junction than is possible with arthroscopy alone and that there is less potential for osseous debris to become trapped in the joint. Furthermore, the risk of an inadequate osseous correction is minimized. However, Ganz et al.33 argued that the open technique with femoral head dislocation offers better inspection of the acetabulum than is possible with an anterior Smith-Petersen approach unless the tensor fasciae latae and gluteus medius are extensively detached from the pelvic brim. Clearly, the mini-anterior approach is not suitable for circumferential lesions of the femoral head or acetabulum (Fig. 6). However, it may be appropriate for most patients in whom preoperative investigation has demonstrated that the lesion is localized mainly anteriorly. Patients should be warned that there is a risk of injury to the lateral femoral cutaneous nerve with this approach. In addition, because the incision is not parallel to the tension lines of the skin, a hypertrophic scar may develop in some patients.
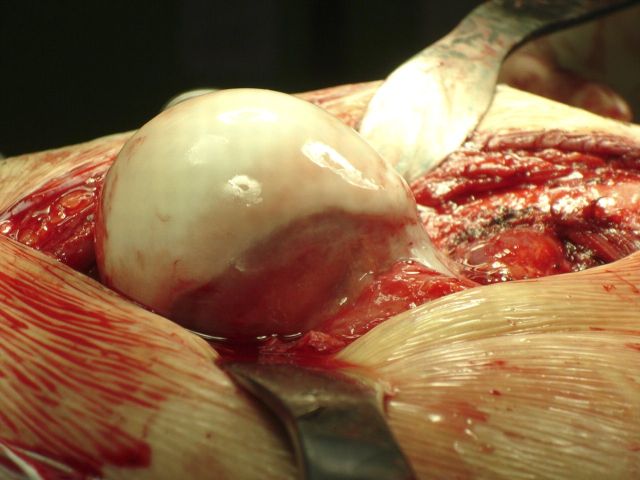
Fig. 6.
The extent of the deformity of a cam-type impingement is seen on this intraoperative photograph of a dislocated femoral head.
Hip Arthroscopy
The indications for hip arthroscopy include (1) cam-type impingement without proximal femoral deformity and (2) isolated acetabular retroversion with or without cam-type deformity.
Arthroscopy is clearly an attractive alternative for patients because it involves smaller incisions, a shorter recovery time, and a lower morbidity rate. Today, the technique of arthroscopy of the hip can be divided into two approaches: one into the central compartment and one into the peripheral compartment. The central compartment includes the labrum and all parts medial to it. The peripheral compartment comprises everything lateral to the labrum within the capsule and includes the head-neck junction. Arthroscopy of the central compartment is typically performed with traction. The labrum can be inspected for tears that can be débrided or, in some cases, treated with refixation. Delaminated articular cartilage can be excised, and exposed acetabular subchondral bone can undergo microfracture. With the traction released, the peripheral compartment can be entered through an anterolateral portal. A partial capsulectomy is then performed to facilitate instrument placement for reshaping of the femoral head-neck junction (Figs. 7-A and 7-B). In more advanced cases of osteoarthritis, peripheral osteophytes can be removed. Incomplete visualization may lead to undertreatment, can lead to errors with defining the extent of rim trimming that is required, or can lead to excessive removal of bone at the femoral head-neck junction and subsequent fracture38. Neurovascular injury is rare but possible; it can be related either to the portals (the superior gluteal nerve can be damaged with creation of the anterolateral portal, and the lateral femoral cutaneous and femoral nerves can be damaged with creation of the anterior portal) or to the traction, which can especially affect the sciatic and pudendal nerves.
Fig. 7-A.
A cross-table lateral radiograph demonstrating an insufficient anterior head-neck concavity. The inset demonstrates the associated damage to the acetabular labral chondral complex (arrows).
Fig. 7-B.
The concavity of the femoral head-neck junction has been restored by means of hip arthroscopy as seen on the postoperative radiograph. The resected head-neck area can be seen on the arthroscopic photograph (inset).
As with any new surgical technique, there is a risk of suboptimal results when arthroscopy is used for the treatment of femoroacetabular impingement39. With increasing clinical experience and training, arthroscopic treatment of femoroacetabular impingement will continue to expand. In a recent paper, Ilizaliturri et al.40 reported on nineteen cases of pure cam impingement treated arthroscopically. Sixteen patients had significant improvement in their WOMAC scores (p = 0.001), two had progression of arthritis, and one was advised to undergo total hip replacement. There were no major complications associated with this procedure. Other surgeons have reported on larger series, but the duration of follow-up was short and no validated scoring was provided38. More importantly, because the indications for and techniques of arthroscopic treatment of pincer-type impingement are still evolving41, great caution should be exercised when one is considering trimming the acetabular rim, which is technically demanding and can create a dysplastic acetabulum if there is overcorrection.
Hip Arthroplasty
The presence of substantial cartilage damage at the time of surgery for the treatment of impingement has been associated with a poor outcome, with patients having a joint replacement in the short-term follow-up period5,40,42. However, it is often unclear whether joint preservation is still indicated or if arthroplasty is preferable in order to provide a more predictable outcome. One of the factors that has discouraged surgeons from proceeding with a total hip replacement is the large leap between joint preservation and resection of the femoral head-neck area to address patients' symptoms. Hip resurfacing represents an attractive alternative bone-preserving option for a young patient with an arthritic hip43. When hip resurfacing is performed in a patient with osteoarthritis due to femoroacetabular impingement, care must be taken to restore the femoral head-neck offset or impingement can still occur19. In addition, restoration of the femoral head-neck offset allows optimization of the sizes of the femoral and acetabular components, since the femoral head diameter drives the acetabular size44. It is recommended that anterior osteophytes be removed from the head-neck junction before the guide pin is placed44. One of us (P.E.B.) performed resurfacing arthroplasty in six patients, with a mean age of 42.4 years (range, thirty-four to forty-eight years), who had initially undergone surgery to treat impingement. All six patients had consented to both procedures because preoperative radiographs had demonstrated joint space narrowing (Fig. 8-A). All patients underwent hybrid metal-on-metal hip resurfacing (Conserve Plus, Wright Medical Technology, Arlington, Tennessee), and one patient also underwent a trochanteric advancement. All had substantial pain relief and improvement in function (Fig. 8-B). Although there were no complications, two of the six patients required removal of screws because of persistent bursitis.
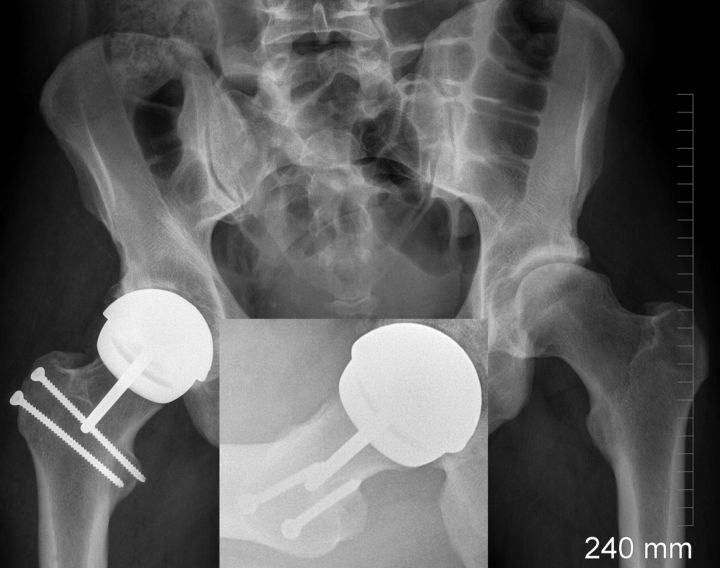
Fig. 8-A.
A thirty-seven-year-old man with pain in the right hip had cam-type impingement and joint space narrowing. The inset Dunn radiograph demonstrates an insufficient head-neck concavity, and the inset intraoperative photograph shows gross cartilage loss from the femoral head.
Fig. 8-B.
Radiograph made following metal-on-metal hip resurfacing done through a surgical dislocation approach. The inset shows optimization of the femoral head-neck concavity.
Overview
Femoroacetabular impingement is a cause of hip pain in young adults, and there is evidence that it is a major cause of osteoarthritis. Treatment of femoroacetabular impingement has been reported to relieve symptoms and perhaps retard the progression of osteoarthritis. The optimal treatment strategies are determined by carefully correlating the patient's history and the findings of physical examination with detailed imaging studies. Surgery should be tailored to treat the individual patient's abnormal hip morphology and should address the major underlying impinging deformities. Future treatments may include cartilage grafting and computer-assisted surgery, further expanding the role of less invasive surgical techniques such as hip arthroscopy. Finally, hip resurfacing is an additional tool for the treatment of young adults with hip pain and early-stage osteoarthritis.
Footnotes
Printed with permission of the American Academy of Orthopaedic Surgeons. This article, as well as other lectures presented at the Academy's Annual Meeting, will be available in February 2009 in Instructional Course Lectures, Volume 58. The complete volume can be ordered online at www.aaos.org, or by calling 800-626-6726 (8 a.m.-5 p.m., Central time).
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from Washington University Institute of Clinical and Translational Sciences (ICTS), the National Center for Research Resources (Award Number UL1RR024992), and the Curing Hip Disease Fund. One or more of the authors, or a member of his or her immediate family, received, in any one year, payments or other benefits in excess of $10,000 or a commitment or agreement to provide such benefits from a commercial entity (Wright Medical Technology). No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated.
An Instructional Course Lecture, American Academy of Orthopaedic Surgeons
References
- 1.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-20. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012-8. [DOI] [PubMed] [Google Scholar]
- 3.Stulberg SD, Cordell LD, Harris WH, Ramsey PL, MacEwen GD. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: The hip. Proceedings of the Third Open Scientific Meeting of the Hip Society. St. Louis: C.V. Mosby; 1975. p 212-28. [Google Scholar]
- 4.Murray RO. The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38:810-24. [DOI] [PubMed] [Google Scholar]
- 5.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67-73. [PubMed] [Google Scholar]
- 6.Beaulé PE, Zaragoza E, Copelan N. Magnetic resonance imaging with gadolinium arthrography to assess acetabular cartilage delamination. A report of four cases. J Bone Joint Surg Am. 2004;86:2294-8. [DOI] [PubMed] [Google Scholar]
- 7.Snow SW, Keret D, Scarangella S, Bowen JR. Anterior impingement of the femoral head: a late phenomenon of Legg-Calve-Perthes' disease. J Pediatr Orthop. 1993;13:286-9. [DOI] [PubMed] [Google Scholar]
- 8.Leunig M, Casillas MM, Hamlet M, Hersche O, Nötzli H, Slongo T, Ganz R. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Othop Scand. 2000;71:370-5. [DOI] [PubMed] [Google Scholar]
- 9.Rab GT. The geometry of slipped capital femoral epiphysis: implications for movement, impingement, and corrective osteotomy. J Pediatr Orthop. 1999;19:419-24. [DOI] [PubMed] [Google Scholar]
- 10.Siebenrock KA, Wahab KH, Werlen S, Kalhor M, Leunig M, Ganz R. Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop Relat Res. 2004;418:54-60. [DOI] [PubMed] [Google Scholar]
- 11.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281-8. [DOI] [PubMed] [Google Scholar]
- 12.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278-86. [DOI] [PubMed] [Google Scholar]
- 13.Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245-53. [DOI] [PubMed] [Google Scholar]
- 14.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93-9. [PubMed] [Google Scholar]
- 15.Beaulé PE, Zaragoza EJ. Femoroacetabular impingement: diagnosis and treatment. In: Beaulé PE, editor. Young adult with hip pain monograph. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2007. p 63-74. [Google Scholar]
- 16.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423-9. [DOI] [PubMed] [Google Scholar]
- 18.Wyss TF, Clark JM, Weishaupt D, Notzli HP. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res. 2007;460:152-8. [DOI] [PubMed] [Google Scholar]
- 19.Beaulé PE, Harvey N, Zaragoza E, Le Duff MJ, Dorey FJ. The femoral head/neck offset and hip resurfacing. J Bone Joint Surg Br. 2007;89:9-15. [DOI] [PubMed] [Google Scholar]
- 20.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/asphericity. Clin Orthop Relat Res. 2006;445:181-5. [DOI] [PubMed] [Google Scholar]
- 21.Eijer H, Leunig M, Mahomed N, Ganz R. Cross-table lateral radiographs for screening of anterior femoral head-neck offset in patients with femoroacetabular impingement. Hip Int. 2001;11:37-41. [Google Scholar]
- 22.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556-60. [DOI] [PubMed] [Google Scholar]
- 23.Beaulé PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ. Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res. 2005;23:1286-92. [DOI] [PubMed] [Google Scholar]
- 24.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241-8. [DOI] [PubMed] [Google Scholar]
- 25.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kassarjian A, Yoon LS, Belzile E, Connolly SA, Millis MB, Palmer WE. Triad of MR arthrographic findings in patients with cam-type femoroacetabular impingement. Radiology. 2005;236:588-92. [DOI] [PubMed] [Google Scholar]
- 27.Leunig M, Werlen S, Ungersbock A, Ito K, Ganz R. Evaluation of the acetabular labrum by MR arthrography. J Bone Joint Surg Br. 1997;79:230-4. Erratum in: J Bone Joint Surg Br. 1997;79:693. [DOI] [PubMed] [Google Scholar]
- 28.Leunig M, Podeszwa D, Beck M, Werlen S, Ganz R. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;418:74-80. [DOI] [PubMed] [Google Scholar]
- 29.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and débridement in young adults. J Bone Joint Surg Am. 2006;88:1735-41. [DOI] [PubMed] [Google Scholar]
- 30.Beaulé PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773-9. [DOI] [PubMed] [Google Scholar]
- 31.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61-6. [PubMed] [Google Scholar]
- 32.Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:78-81. [DOI] [PubMed] [Google Scholar]
- 33.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip: a new technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119-24. [DOI] [PubMed] [Google Scholar]
- 34.Gautier E, Ganz K, Krugel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82:679-83. [DOI] [PubMed] [Google Scholar]
- 35.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925-35. [DOI] [PubMed] [Google Scholar]
- 36.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25:758-65. [DOI] [PubMed] [Google Scholar]
- 37.Clohisy JC, McClure JT. Treatment of anterior femoroacetabular impingement with combined hip arthroscopy and limited anterior decompression. Iowa Orthop J. 2005;25:164-71. [PMC free article] [PubMed] [Google Scholar]
- 38.Sampson TG. Arthroscopic treatment of femoroacetabular impingement: a proposed technique with clinical experience. Instr Course Lect. 2006;55:337-46. [PubMed] [Google Scholar]
- 39.Beaulé PE, Clohisy JC, Schoenecker PE, Kim YJ, Millis M, Trousdale RT. Hip arthroscopy: an emerging gold standard. Arthroscopy. 2007;23:682. [DOI] [PubMed] [Google Scholar]
- 40.Ilizaliturri VM Jr, Orozco-Rodriguez L, Acosta-Rodríguez E, Camacho-Galindo J. Arthroscopic treatment of cam-type femoroacetabular impingement: preliminary report at 2 years minimum follow-up. J Arthroplasty. 2008;23:226-34. [DOI] [PubMed] [Google Scholar]
- 41.Philippon MJ. New frontiers in hip arthroscopy: the role of arthroscopic hip labral repair and capsulorrhaphy in the treatment of hip disorders. Instr Course Lect. 2006;55:309-16. [PubMed] [Google Scholar]
- 42.Peters CL, Erickson J. The etiology and treatment of hip pain in the young adult. J Bone Joint Surg Am. 2006;88 Suppl 4:20-6. [DOI] [PubMed] [Google Scholar]
- 43.Beaulé P. A soft tissue-sparing approach to surface arthroplasty of the hip. Oper Tech Orthop. 2004;14:75-84. [Google Scholar]
- 44.Beaulé PE, Poitras P. Femoral component sizing and positioning in hip resurfacing arthroplasty. Instr Course Lect. 2007;56:163-9. [PubMed] [Google Scholar]