To the Editor: Survival rates for very pre-term infants have risen drastically in recent years owing to successful assisted-ventilation techniques; the latest prenatal and postnatal treatments; and modern, well-equipped, and well-staffed neonatal intensive care units.[1,2] Cranial ultrasound (cUS) is the primary imaging technique for evaluating brain injury in very pre-term infants. Very pre-term infants have several unique features related to their ongoing maturation, and associated findings on cUS should be considered for accurate and early diagnosis.[3,4] The purpose of this study was to summarize the cUS characteristics of the brains of very premature infants of different gestational ages (GAs) ≤ 29 weeks to provide an understanding of the diagnosis of abnormal brain conditions.
The ethical approval from the Institutional Ethics Examining Committee of Human Research (No. sk2019-14) was obtained before patient recruitment. All participants signed an informed written consent and a full explanation was given regarding the coblation annulaplasty and its schematic procedures, and benefits and potential complications. A total of 137 very pre-term infants born at a GAs ≤29 weeks were observed. The infants had a median GA of 27+2 weeks and a minimum age of 22+5 weeks. Their average birth weight was 1002 ± 21 g, and weights ranged from 500 to 1650 g.
The youngest case was a female infant born at a GA of 22+5 weeks and weighing 850 g. The infant's cerebral longitudinal fissure and lateral fissure showed a single linear echo and a wide gap, and her brain surface was smooth with few sulci. Her periventricular echodensities (PVE) were grade II. At 3 weeks after birth, the cingulate sulcus began to appear with a short linear echo in the sagittal section. The cerebral longitudinal fissure exhibited few folds, and the lateral fissure showed short branches. The cerebral sulci significantly increased at 8 weeks after birth. Numerous sulci appeared to the side of the longitudinal fissure and on the surface of the parenchyma. The cingulate sulcus lengthened and became distinct, and gaps in the lateral fissure narrowed and branched. At 11 weeks after birth, the PVE turned to normal, the cerebral sulci developed with many branches, and the hippocampal gyrus had a well-defined boundary.
In infants born at GA of 23 to 24 weeks, the cerebral longitudinal fissure, lateral fissure, hippocampal gyrus, and calcarine sulcus showed single linear echoes with few folds or branches. The lateral fissure had wide gaps. The cerebral parenchyma was smooth without small sulci. In infants born at a GA of 26 weeks, the cingulate sulcus began to take shape and showed short dashed or single linear echoes without obvious branches. At similar GAs, infants with heavier birth weights exhibited clearer cingulate sulci and better-developed brains compared with those born with lower weights. In infants born at GAs of 27 to 28 weeks, the lateral fissure exhibited wide gaps with short branches. Deep inside the cerebral parenchyma, a few shallow sulci appeared perpendicular to the cerebral longitudinal fissure. No obvious cerebral sulcus structures were present in the shallow layer of the cerebral parenchyma. The cingulate gyrus was well developed with few branches in the sulcus. In infants born at a GA of 28 weeks, the parieto-occipital sulcus exhibited short linear echoes in the shallow layer of the parenchyma. In infants born at a GA of 29 weeks, the cingulate sulcus exhibited multiple curved branches that extended into the cerebral parenchyma. The boundary of the cingulate gyrus was essentially formed, and gaps between the lateral fissures narrowed and branched. Numerous cerebral sulci with short line-like echoes appeared next to the longitudinal fissure and the shallow layer of the cerebral parenchyma. The brain development of infants born at a GA of 29 weeks was more mature than that of pre-term infants born at a GA <28 weeks.
The cUS images of the coronal and axial sections of the cerebellum were obtained by scanning the mastoid fontanelle. The coronal section of the cerebellum at the mastoid fontanelle showed the pontine, parts of the cerebellar vermis, the cerebellar hemispheres (including the cortex and medulla), and the cerebellar cistern. The axial section of the cerebellum showed the cerebellar vermis, cerebellar hemisphere, and fourth ventricle. Within the cerebellar hemispheres, the boundary between the cortex and medulla was clear, and numerous shallow sulci were visible in the cortex. Furthermore, the cerebellar vermis was well developed with clear surface textures and plentiful folds and showed caterpillar-like changes in full time infants [Figure 1].
Figure 1.
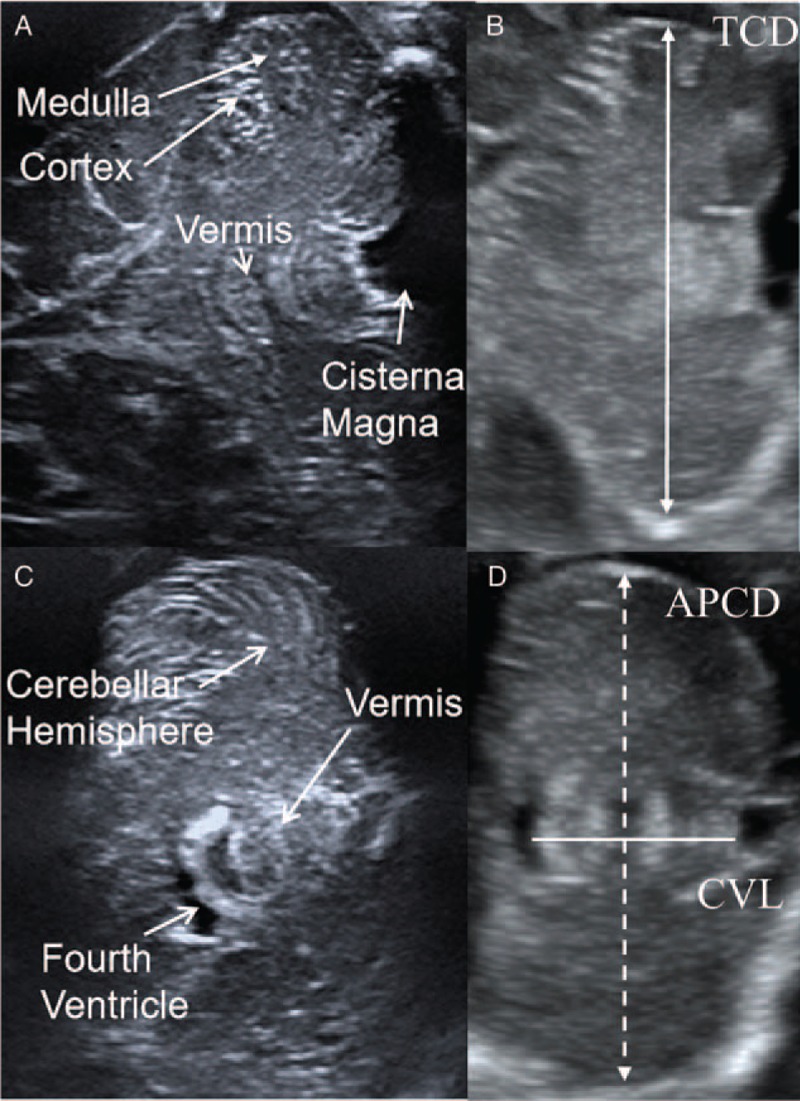
Methods of cerebellar measurement. Coronal sections (A, B) and axial sections (C, D) of the cerebellum were obtained via the mastoid window (mastoid fontanel). The distance between cerebellar hemispheres on the coronary was defined as the transverse cerebellar diameter (TCD), the distance between cerebellar hemispheres on the axial section was defined as anteroposterior cerebellar diameter (APCD), and the length of the cerebellar vermis (CVL) was measured on the axial section.
In infants born at GA of 25 to 28 weeks, the cerebral parenchyma in the cerebellar hemisphere was smooth. However, the boundary between the cortex and medulla was unclear. Few sulci were present in the cortex, and the vermis had a visible but loose texture.
In infants born at a GA of 29 weeks, the cerebellar hemisphere exhibited short, line-like shallow sulci, and the vermis was longer than that in infants born before a GA of 28 weeks.
The transverse cerebellar diameter (TCD), anteroposterior cerebellar diameter (APCD), and length of the cerebellar vermis (CVL) of the infants were measured[5] [Figure 1], and the cerebellar measurements of 38 infants born at different GAs were averaged. The cerebellar measurements of very pre-term infants born at GAs of 25 to 29 weeks, particularly APCD and TCD, gradually increased over time. Analysis of variance revealed that changes in TCD, APCD, and CVL length between the different GA groups were statistically significant (F = 45.57, P < 0.001; F = 33.51, P < 0.001; and F = 11.12, P < 0.001, respectively).
Pearson correlation analyses showed that ACD was significantly correlated with body weight and GA (r = 0.71, P < 0.001; r = 0.86, P < 0.001, respectively), APCD was significantly correlated with body weight and GA (r = 0.66, P < 0.001; r = 0.75, P < 0.001, respectively), and CVL was significantly correlated with body weight and GA (r = 0.71, P < 0.001; r = 0.75, P < 0.001, respectively).
In conclusion, cerebral and cerebellar structures develop in very pre-term infants (GA ≤29 weeks), and cerebellar measurements changed as the GA increased. The brain development of infants born at a GA of 29 weeks was significantly more mature than that of pre-term infants born at a GA <28 weeks. This difference indicates an age watershed between the two groups of infants.
Funding
The study was supported by a grant from the Hunan Provincial Science and Technology Department (No. 2017SK50701).
Conflicts of interest
None.
Footnotes
How to cite this article: Zhang XH, Wu SH, Chen WJ, Zhou MJ, Qiu SJ. Brain structure development of very pre-term infants on serial cranial ultrasound. Chin Med J 2020;133:372–373. doi: 10.1097/CM9.0000000000000607
References
- 1.Pekcevik Y, Ozer EA, Guleryuz H. Cranial sonography in extremely preterm infants. J Clin Ultrasound 2014; 42:283–290. doi: 10.1016/B978-0-444-64029-1.00008-4. [DOI] [PubMed] [Google Scholar]
- 2.Hamrick SE, Miller SP, Leonard C, Glidden DV, Goldstein R, Ramaswamy V, et al. Trends in severe brain injury and neurodevelopmental outcome in premature newborn infants: the role of cystic periventricular leukomalacia. J Pediatr 2004; 145:593–599. doi: 10.1016/j.jpeds.2004.05.042. [DOI] [PubMed] [Google Scholar]
- 3.Steggerda SJ, Bruïne FT, Smitswintjens VE, Verbon P, Walther FJ, van Wezel-Meijler G. Posterior fossa abnormalities in high-risk term infants: comparison of ultrasound and MRI. Eur Radiol 2015; 25:2575–2583. doi: 10.1007/s00330-015-3665-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang XH, Qiu SJ, Chen WJ, Gao XR, Li Y, Cao J, et al. Predictive value of cranial ultrasound for neurodevelopmental outcomes of very preterm infants with brain injury. Chin Med J 2018; 131:920–926. doi: 10.4103/0366-6999.229895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brossard-Racine M, Du Plessis AJ, Limperopoulos C. Developmental cerebellar cognitive affective syndrome in ex-preterm survivors following cerebellar injury. Cerebellum 2015; 14:151–164. doi: 10.1007/s12311-014-0597-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


