Background and Aims
Gastric outlet obstruction (GOO) can result from benign and malignant causes.1 Surgical gastroenterostomy has been the treatment of choice for patients with benign and malignant GOO with a good functional status.2 Placement of luminal self-expandable metal stents is currently accepted as the endoscopic treatment of choice for malignant GOO because of its effectiveness and minimally invasive nature.3 The main limitation of luminal stents is the high incidence of recurrent GOO resulting from tumor/tissue ingrowth/overgrowth.4 More recently, EUS-guided gastroenterostomy (EUS-GE) has emerged as an alternative to both luminal stent placement and surgical gastroenterostomy.5, 6, 7 The advantages of EUS-GE include its less-invasive nature compared with surgery, its efficacy, and the low incidence of recurrent GOO in cancer patients in addition to maintaining nutrition.8 We present 5 techniques of EUS-GE using a lumen-apposing metal stent (LAMS) (Video 1, available online at www.VideoGIE.org).
Endoscopic methods
Patient preparation
Written informed consent is obtained, explaining clearly that EUS-GE is a novel technique and an off-label use of a U.S. Food and Drug Administration—approved stent. A CT scan helps determine the proximity of the small bowel to the stomach and to look for ascites, a contraindication to EUS-GE. Antibiotics are not routinely administered.
Technique 1. Antegrade EUS-GE: the traditional/downstream method
Step 1: An endoscopy is performed to place a guidewire in the proximal jejunum past the obstruction. The endoscope is withdrawn, leaving the guidewire in the jejunum.
Step 2: Under fluoroscopic control, a large dilating balloon is advanced over this wire to the jejunum.
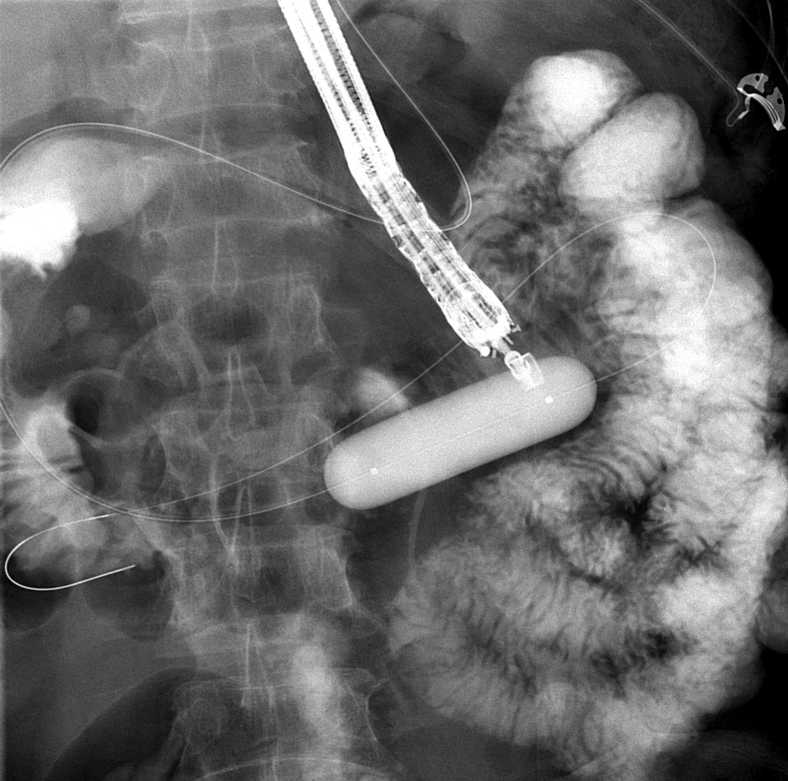
Step 3: EUS-guided 19-gauge needle puncture of the balloon is performed from the stomach (Fig. 1).
Figure 1.
Fluoroscopic view of large dilating balloon inflated in the third portion of the duodenum, to target with a 19-gauge needle through a therapeutic linear echoendoscope.
Step 4: A new guidewire is passed downstream into the jejunum through this 19-gauge needle.
Step 5: Over this guidewire, the LAMS is deployed, creating a gastroenterostomy.
Technique 2. Antegrade EUS-GE: the rendezvous method
Steps 1 to 3 are the same as in Technique 1.
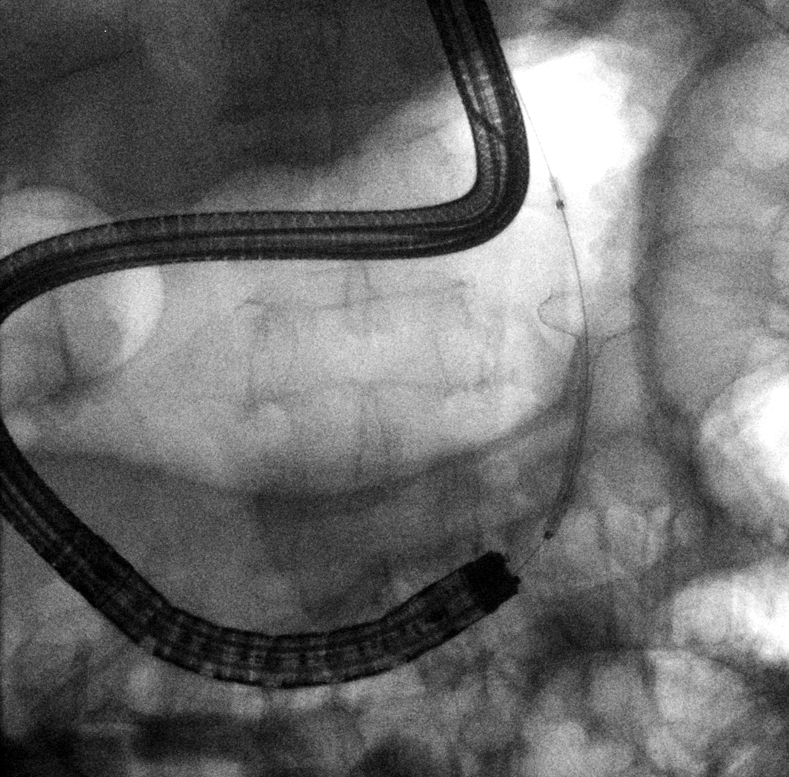
Step 4: Instead of passing a guidewire downstream into the jejunum, the puncturing guidewire is trapped in the dilating balloon that was punctured, or an ERCP extraction balloon and basket, and pulled back through the duodenal obstruction, out of the mouth, securing it (Fig. 2).
Figure 2.
Fluoroscopic view of guidewire having been secured through the scope and out of the mouth through the duodenal obstruction (previously treated with 2 duodenal stents).
Step 5: The LAMS is then deployed over this guidewire under traction.
Technique 3. Retrograde EUS-GE: enterogastrostomy
Steps 1 to 4 are the same as in Technique 2, with the guidewire secured across the stricture and out of the mouth.
Step 5: A therapeutic endoscope is now advanced over the guidewire, traversing the obstruction to the point of duodenal/jejunal insertion of the guidewire.
Step 6: The LAMS is deployed from the jejunum (gastric flange opens first) (Fig. 3).
Figure 3.
Fluoroscopic view of gastric flange being deployed first and seen well because of the large gastric gas shadow by the “jejunogastrostomy technique.”
Advantage: This reduces the chances of the first flange (in this case, gastric) misdeploying because the stomach is less likely to be pushed away, and the gastric gas shadow fluoroscopically allows for easier deployment.
Disadvantage: Traversing the obstruction may increase the risk of perforation and has to be within reach of a therapeutic endoscope.
Technique 4. EUS balloon-occluded GE bypass (EPASS)
Step 1: A double-balloon enteroscope (DBE) is used to place a guidewire in the proximal jejunum.
Step 2: The DBE is withdrawn, leaving the overtube in place.
Step 3: A novel balloon-occlusion catheter is passed over the guidewire, and 2 balloons (20 cm apart) are inflated to fix a segment of duodenum and jejunum, which is filled with contrast material and methylene blue.
Step 4: An EUS-guided puncture of this portion of the small bowel is performed between these 2 balloons.
Step 5: The LAMS is deployed.
Advantage: Fixing the jejunum between the 2 balloons may prevent its migration while the LAMS is deployed.
Limitations of Technique 4: This technique would fail if the proximal jejunum and duodenum aren't in close proximity to the gastric wall, and, furthermore, this novel catheter is not commercially available.
Technique 5. Antegrade EUS-GE: the direct method
Step 1: The duodenum and jejunum are filled with contrast material and methylene blue (Fig. 4).
Figure 4.
Echoendoscopic view of duodenum and jejunum distended with contrast material and methylene blue and seen well before direct puncture.
Step 2: EUS-guided needle puncture of the jejunum without need for a dilating balloon is performed.
Step 3: Methylene blue is aspirated, confirming the needle is in the jejunum (helps avoid unintentionally puncturing the transverse colon).
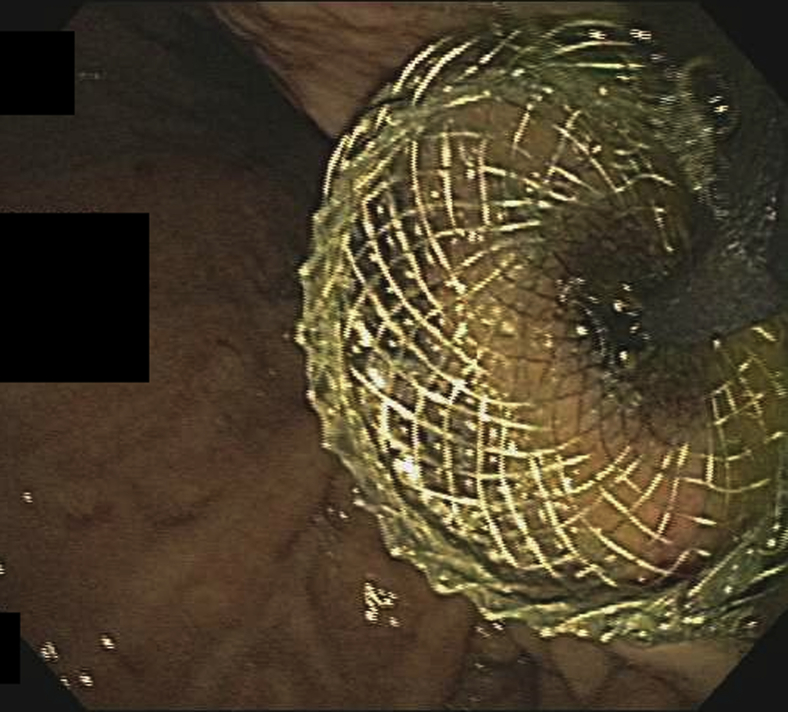
Step 4: The LAMS is deployed without a guidewire (Fig. 5).
Figure 5.
Final view after lumen-apposing metal stent is deployed, creating the gastroenterostomy with the direct technique.
Advantage: There are significantly fewer steps and avoidance of a guidewire; may reduce the chances of pushing away the duodenum/jejunum during LAMS deployment.
Postprocedure care: Patients may be observed overnight. An upper-GI series can help confirm stent patency, lack of migration, or leak before oral intake is given, but it is not needed when the patient is clinically well. A liquid diet is started the same or the next day and advanced to a low-residue diet as tolerated. Stents are left in place indefinitely. Removal would likely result in stricturing of this small (15 mm), albeit adequate, anastomosis.
Clinical implications and conclusions
Multiple techniques are now available for the successful performance of EUS-GE. A randomized control trial comparing this with luminal self-expandable metal stents and even a surgical gastroenterostomy is warranted. The superiority of one method of performing EUS-GE over another has not been demonstrated, and studying this as well would be useful.
Acknowledgement
Supported by a Robert W. Summers grant from the American Society for Gastrointestinal Endoscopy.
Disclosure
Dr Irani is a consultant for Boston Scientific and Gore Medical. Dr Itoi, Dr Baron, and Dr Khashab are consultants for Boston Scientific.
Supplementary data
EUS-guided gastroenterostomy: techniques from East to West.
References
- 1.Chen Y.I., Itoi T., Baron T.H. EUS-guided gastroenterostomy is comparable to enteral stenting with fewer re-interventions in malignant gastric outlet obstruction. Surg Endosc. 2016;31:2946–2952. doi: 10.1007/s00464-016-5311-1. [DOI] [PubMed] [Google Scholar]
- 2.Irani S., Kozarek R.A. Gastrointestinal dilation and stent placement. In: Podolsky D.K., Camillera M., Fitz J.G., editors. Yamada’s textbook of gastroenterology. Sixth ed. John Wiley & Sons Ltd; West Sussex, UK: 2016. [Google Scholar]
- 3.Holt A.P., Patel M., Ahmed M.M. Palliation of patients with malignant gastroduodenal obstruction with self-expanding metallic stents: the treatment of choice? Gastrointest Endosc. 2004;60:1010–1017. doi: 10.1016/s0016-5107(04)02276-x. [DOI] [PubMed] [Google Scholar]
- 4.Oh S.Y., Edwards A., Mandelson M. Survival and clinical outcome after endoscopic duodenal stent placement for malignant gastric outlet obstruction: comparison of pancreatic cancer and nonpancreatic cancer. Gastrointest Endosc. 2015;82:460–468. doi: 10.1016/j.gie.2015.01.026. [DOI] [PubMed] [Google Scholar]
- 5.Adler D.G., Baron T.H. Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol. 2002;97:72–78. doi: 10.1111/j.1572-0241.2002.05423.x. [DOI] [PubMed] [Google Scholar]
- 6.Itoi T., Itokawa F., Uraoka T. Novel EUS-guided gastrojejunostomy technique using a new double-balloon enteric tube and lumen-apposing metal stent (with videos) Gastrointest Endosc. 2013;78:934–939. doi: 10.1016/j.gie.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 7.Khashab M.A., Kumbhari V., Grimm I.S. EUS-guided gastroenterostomy: the first U.S. clinical experience (with video) Gastrointest Endosc. 2015;82:932–938. doi: 10.1016/j.gie.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 8.Itoi T., Ishii K., Tanaka R. Current status and perspective of endoscopic ultrasonography-guided gastrojejunostomy: endoscopic ultrasonography-guided double balloon-occluded gastrojejunostomy (with videos) J Hepatobiliary Pancreat Sci. 2015;22:3–11. doi: 10.1002/jhbp.148. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
EUS-guided gastroenterostomy: techniques from East to West.