56 Dean Street (56DS), a sexual health clinic in London, UK, opened in its present location in 2009. In 2015, new HIV diagnoses at 56DS peaked and began to fall; in that year the service diagnosed ∼25% new HIV diagnoses in men-who-have-sex-with-men (MSM) in England [1]. In this commentary we analyze new HIV diagnoses made at 56DS from 2016 to 2018.
56DS offers HIV testing irrespective of attenders’ sexually transmitted infection (STI) symptomology either a third-generation test if there is no risk within the six-week window period, otherwise a fourth-generation HIV test. Patients with positive HIV serology are recalled for confirmatory testing. 56DS provides a postal home HIV sampling service: ‘Dean Street at Home’ before January 2018 and subsequently via Sexual Health London (SHL) [2]. Patients who test positive elsewhere such as postal tests, private clinics, GP or non-UK services may also attend for confirmatory testing.
In 2014, 56DS opened Dean Street Express (DSE), an asymptomatic STI screening service with results within 6 h [3]. Initially a walk-in service, in January 2016, DSE introduced booked appointments for asymptomatic screening while preserving walk-in appointments for higher risk individuals who were identified at previous attendance and enrolled onto ‘Dean Street PRIME’, a web-based package of information about HIV risk reduction [1,3,4]. DSE was expanded further in April 2018 to provide walk-in appointments for treatment of asymptomatic STIs and contacts.
Since 2015, HIV pre-exposure prophylaxis (PrEP) monitoring at 56DS has continued to increase, initially through online pharmacies and subsequently PrEP Shop, an in-clinic pharmacy, and the PrEP IMPACT trial [5], [6], [7].
We performed a retrospective case-note review of those newly diagnosed HIV-positive at 56DS between 1st January 2016 to 31st December 2018 noting demographic data and baseline test results. The number of HIV tests performed was obtained from clinical coding of attendances. We measured differences between groups using Mann-Whitney U test (e.g. age, CD4 count), chi-squared test (e.g. gender, place of birth) and Z-test (proportions e.g. MSM). As a service evaluation, ethics submission was not required.
Of 737 new HIV diagnoses at 56DS, 114 (15%) had the initial HIV test performed elsewhere: 43%, postal testing; 38% UK service; 11% non-UK service; 7% outreach testing.
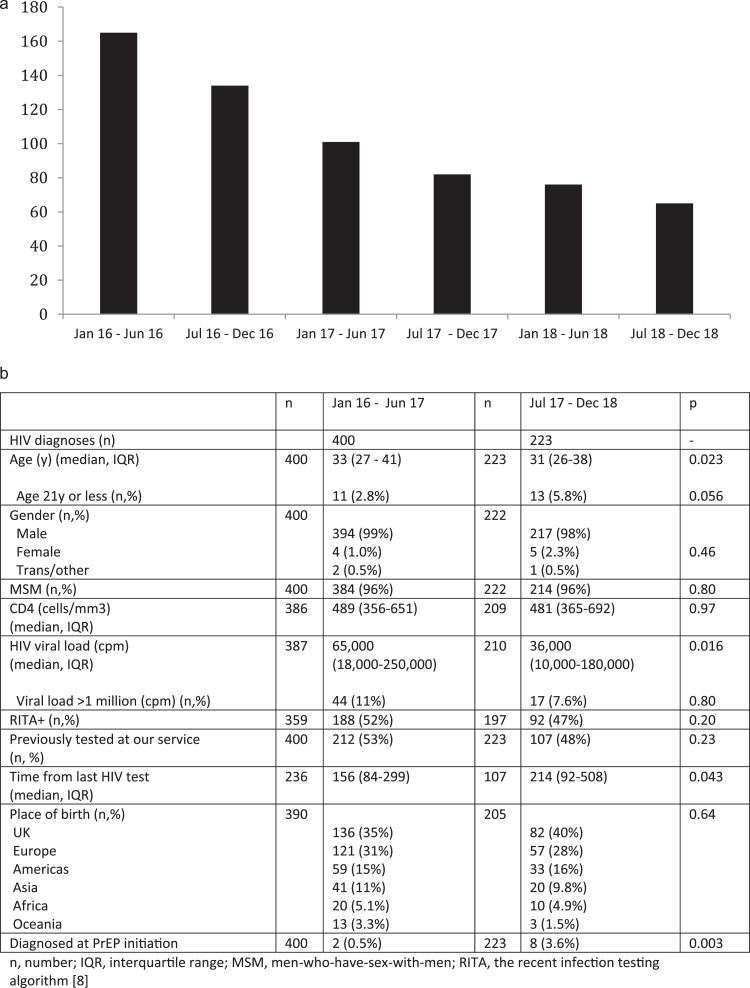
Excluding these 114, the 623 new HIV diagnoses fell at 56DS every year over the three-year period studied: 2016 (299), 2017 (183) and 2018 (141) (Fig. 1(a)).
Fig. 1.
(a) New HIV diagnoses at 56 Dean Street, London, UK excluding those for whom the initial HIV test was performed elsewhere shown for each six-month period from January 2016 to December 2018. (b) Baseline characteristics of 623 newly diagnosed with HIV at 56 Dean Street, London, UK between January 2016–June 2017 and July 2017–December 2018.
Fig. 1(b) shows the baseline characteristics of 623 newly diagnosed individuals for January 2016–June 2017 compared with July 2017-December 2018. Median age at diagnosis was significantly lower more recently (31 years vs 33 years). The proportion of new diagnoses in those aged 21 years or under increased from 2.8% to 5.8%, although this was not significantly different. The proportion of those diagnosed at PrEP baseline increased seven-fold to 3.6%.
The number of HIV tests performed at 56DS for each half-year period from 2016 to 2018 decreased by 23% (39,986 to 30,877). However the number performed in MSM overall only decreased by 3% (21,397 to 20,734) compared with those in MSM aged 21 years and under which fell by 19% (1033 to 835).
Most importantly, the number of HIV infections diagnosed at 56DS continues to fall suggesting the ongoing success of our combination prevention model. Most striking is the doubling in the proportion of new HIV in MSM aged 21 or under, especially as HIV tests performed in this group has also decreased. Although the actual numbers are small and not statistically significant, we wonder if HIV incidence may be increasing in this group and whether this is occurring elsewhere. If true, it is crucial that we improve access to HIV testing in younger MSM. In order to address this, we have engaged younger MSM in focus groups, and created social media content including ‘Plan zero’, ‘Generation zero’ and ‘The Grass is always Grindr’ [8], [9], [10].
It is possible that changes seen with time in the characteristics of those newly diagnosed with HIV may be because DSE moved from walk-in to booked appointments leading to a decrease in the frequency of HIV testing (increasing time between HIV tests) and consequent fewer acute HIV infections (lower baseline viral load, lower RITA positivity).
Moving away from walk-in appointments may also explain the fall in HIV testing in younger MSM.
HIV testing at 56DS is adapting to users’ needs as demonstrated in two ways. Firstly, increasing PrEP use has led to the provision of walk-in monitoring at DSE, and consequently a recent increase in new HIV diagnoses made at PrEP baseline testing. Secondly, the provenance of new diagnoses has shifted with an expansion in new diagnoses made elsewhere, most notably from postal testing. The picture of the service has developed into a ‘hub-and-spoke’ model where newly diagnosed individuals previously unknown to our service are directed to 56DS for confirmatory testing.
Declaration of competing interest
None.
References
- 1.Nwokolo N., Hill A., McOwan A., Pozniak A. Rapidly declining HIV infection in MSM in central London. Lancet HIV. 2017;4(11):e482–e483. doi: 10.1016/S2352-3018(17)30181-9. [DOI] [PubMed] [Google Scholar]
- 2.Sexual health London webpage. https://www.shl.uk/. (accessed November 2019).
- 3.Whitlock G., Gibbons D., Longford N., Harvey M.J. Rapid testing and treatment for sexually transmitted infections improve patient care and yield public health benefits. Int J STD Aids. 2018;29(5):474–482. doi: 10.1177/0956462417736431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nwokolo N., Whitlock G. McOwan not just prep: other reasons for London's HIV decline. Lancet HIV. 2017;4:e153. doi: 10.1016/S2352-3018(17)30044-9. [DOI] [PubMed] [Google Scholar]
- 5.PrEP shop webpage. http://dean.st/prepshop/. (accessed November 2019)
- 6.Girometti N., McCormack S., Devitt E., Gedela K. Evolution of a pre-exposure prophylaxis (PrEP) service in a community-located sexual health clinic: concise report of the prepxpress. Sex Health. 2018;25(6):598–600. doi: 10.1071/SH18055. [DOI] [PubMed] [Google Scholar]
- 7.Whitlock G. Pre-exposure prophylaxis: the english experience. Rev Enf Emerg. 2017;16(2):3–4.. https://webarchive.nationalarchives.gov.uk/20140714095636/http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317139917891 Public Health England RITA website. (accessed November 2019) [Google Scholar]
- 8.Plan zero webpage. https://dean.st/zero/. (accessed November 2019)
- 9.Generation zero youtube animation. https://www.youtube.com/watch?v=gEXcNKtL bIM. (accessed November 2019)
- 10.The grass is always grindr youtube channel. https://www.youtube.com/playlist?list=PLsi7TLi2MKjb96JdzwmOgYhekWj754fpq. (accessed November 2019)