Abstract
Internet-based cognitive behavior therapy (ICBT) has proved effective in reducing mild to moderate depressive symptoms. However, only a few studies have been conducted in a regular healthcare setting which limits the generalizability of the results. The influence of psychiatric comorbidity on outcome is not well understood. In the current study, patients with mild to moderate depressive symptoms in primary and psychiatric care were interviewed using the SCID-I and SCID-II to assess psychiatric diagnoses. Those included were randomly allocated to ICBT (n = 48) or to an active control condition (n = 47). Both groups received therapist support. At post-treatment, ICBT had reduced depressive symptoms on the BDI-II more than the active control intervention (p = .021). However, the difference between groups was no longer significant at the 6-, 12- or 24-month follow-ups. The within-group effect size after ICBT (BDI-II) was large (d = 1.4). A comorbid anxiety disorder didn't moderate the outcome, while the presence of a personality disorder predicted significantly less improvement in depressive symptoms. ICBT had a large effect on depressive symptoms in a sample from regular healthcare. It is possible to obtain a large effect from ICBT despite comorbid anxiety, however, including patients with a comorbid personality disorder in the current form of ICBT seems questionable.
Keywords: Depression, Internet, Comorbidity, Personality disorders, Primary healthcare, Psychiatric care
Highlights
-
•
ICBT had a large effect on depressive symptoms in a sample from primary and psychiatric care.
-
•
A comorbid anxiety disorder did not moderate the outcome significantly.
-
•
A comorbid personality disorder predicted less improvement in depressive symptoms.
1. Introduction
It has been found that cognitive behavioral therapy (CBT) is transferable to Internet format, especially when guided by a therapist (Andersson, 2016) who provides support, encouragement, and occasionally direct therapeutic activities (Johansson and Andersson, 2012). Meta-analyses show that guided Internet-based CBT (ICBT) is an effective treatment for depression (Karyotaki et al., 2018; Richards and Richardson, 2012). ICBT with guidance seems to be equally effective as face-to-face therapy (Andersson et al., 2016), and offering ICBT as a complement to standard care expands the availability of effective psychological treatment, as it enables therapists to increase their case load.
There are clear indications that guided internet-based psychological treatments are more effective than unguided treatments (Richards and Richardson, 2012), although there are exceptions (Titov et al., 2014). The guidance is typically supportive in nature, including encouragement and reinforcement (Holländare et al., 2016; Paxling et al., 2013; Sanchez-Ortiz et al., 2011) but how different aspects of guidance influence outcome is still not fully understood.
Most studies on internet-based psychological treatment have investigated CBT-based interventions, (Ruwaard et al., 2009; Andersson et al., 2005; Hedman et al., 2014; Ruwaard et al., 2012; Williams and Andrews, 2013; Hedman et al., 2012; Dear et al., 2018; Titov et al., 2016; Johansson et al., 2019; Mathiasen et al., 2018) although one study compared internet-based psychodynamic treatment for depression with an active control condition with positive results (Johansson et al., 2013). One study compared guided ICBT with individualized e-mail therapy (Vernmark et al., 2010), and moderate to large effect sizes were found in both groups. Internet-based psychological treatment programs can thus vary in content and presentation, yet still be effective.
Much research on ICBT has been conducted in university settings with nationwide recruitment (Andersson et al., 2013a) or via the media, and several efficacy studies have found that guided ICBT for depression is effective (Andersson et al., 2005; Johansson and Andersson, 2012; Vernmark et al., 2010; Ruwaard et al., 2009; Carlbring et al., 2013; Warmerdam et al., 2008; Perini et al., 2009; Robinson et al., 2010; Hollandare et al., 2013; Carlbring et al., 2005; Andersson et al., 2006; Berger et al., 2011a; Berger et al., 2011b; Botella et al., 2010; Titov et al., 2011; Heinrich et al., 2016; Ivarsson et al., 2014; Zetterberg et al., 2019) with a favorable outcome at the 3.5 year follow-up in one study (Andersson et al., 2013b). Less research has been conducted in representative clinical settings and few studies have had an active control condition. However, some studies on ICBT in health care settings have been carried out (Ruwaard et al., 2012; Watts et al., 2012; Williams and Andrews, 2013; Kessler et al., 2009; Hedman et al., 2014; Titov et al., 2015; Kivi et al., 2014; Johansson et al., 2019; Mathiasen et al., 2018; Hadjistavropoulos et al., 2016; Nordgreen et al., 2018) In a large effectiveness study by Hedman et al. (2014) 1203 patients were treated with ICBT for depression in routine psychiatric care in Stockholm, Sweden. The effect on depressive symptoms was large with a within-group effect size (d) of 1.27. Some studies have used active control conditions, often resulting in smaller between group effects (Kampmann et al., 2016).
Comorbidity is common among depressed persons, and one meta-analysis (Friborg et al., 2014) estimated that as many as 45% of the patients with major depressive disorder (MDD) have a comorbid personality disorder (PD). There is a widespread perception within clinical psychiatry that PD has an adverse effect on the outcome of many treatments, and PD has been found to increase the risk of drop out (Schindler et al., 2013) and fewer patients with a PD responded to CBT compared to those without a PD in one study (Fournier et al., 2008). Meta-analyses have shown that PD is a risk factor for poor outcome in treatment for depression (Newton-Howes et al., 2006; Newton-Howes et al., 2014). However, there are exceptions, i.e. RCTs showing that the effect of CBT on patients with depression and PDs is comparable to that for patients without a PD (Joyce et al., 2007; Lis and Myhr, 2016; van Bronswijk et al., 2018).
It has also been found that at least 50% of depressed persons fulfill the diagnostic criteria for a comorbid anxiety disorder (Kessler et al., 2007). One study demonstrated that a high anxiety level increased the risk of relapse after CBT for depression (Forand and Derubeis, 2013) and that focusing on anxiety during sessions reduced the effect on depressive symptoms (Gibbons and DeRubeis, 2008). However, there are also studies indicating that a comorbid anxiety disorder does not affect the outcome of CBT for depression (Smits et al., 2009), and in a study by Kashdan and Roberts (2011), comorbid social anxiety actually increased the effect of CBT for depression.
The aim of this study was to compare the effect of ICBT with the effect of an active control condition in a clinical sample with a depressive disorder recruited from primary and psychiatric care. An additional aim was to investigate the impact of comorbidity.
We hypothesized that, in comparison to the active control condition, ICBT would lead to reduced depressive symptoms and that improvements would be sustained over time. The second hypothesis was that patients suffering from a comorbid anxiety disorder or a personality disorder would improve less.
2. Material and methods
2.1. Design
A randomized controlled trial (RCT) with repeated measurements was conducted to compare the effects of ICBT with those of an active control group in terms of changes in depressive symptoms and remission rates.
2.2. Participants
Participants were recruited in primary care and psychiatric care in two similarly sized neighboring County Councils in Sweden, Örebro and Värmland, each with around 280,000 inhabitants. Recruitment started in 2007 and ended in 2012. Patients received information about the study from posters in waiting rooms as well as being briefed by primary and psychiatric care staff. Both referrals from a health professional and self-referrals were accepted. To qualify, the participant should have mild to moderate depressive symptoms (15–30 on the MADRS-S (Svanborg and Asberg, 1994)), be at least 18 years old, have internet access and be fluent in Swedish. Reasons for exclusion were ongoing CBT, starting or adjusting antidepressant medication during the past month, being suicidal, suffering from bipolar disorder, psychosis, and/or seasonal affective disorder. A demographic description of the participants is presented in Table 1.
Table 1.
Demographic description of the participants in the ICBT and active control group.
| ICBT (n = 48) |
Control (n = 47) | Total (n = 95) |
|
|---|---|---|---|
| Female; number (%) | 38 (79.2) | 34 (72.3) | 72 (75.8) |
| Mean age (SD) | 42.9 (11.26) | 47.7 (12.74) | 45.30 (12.20) |
| Age range | 20–68 | 23–68 | 20–68 |
| Patients with earlier depressive episode(s); number (%) | 28 (58.3) | 27 (57.4) | 55 (57.9) |
| Patients with ADM at recruitment; number (%) | 20 (41.7) | 22 (46.8) | 42 (44.2) |
Note: ADM = antidepressant medication.
2.3. Procedure
Patients who expressed an interest in the study received a letter containing a formal invitation to participate, a written consent form, and a postage prepaid envelope.
Patients who scored 15–30 on the MADRS-S (Svanborg and Asberg, 1994) were called for a SCID-I (First et al., 1998) and a SCID-II (First et al., 1994) interview to assess psychopathology on the DSM-IV (American Psychiatric Association, 2000) Axis I and comorbid PDs (results are shown in Table 2). The face-to-face interview was conducted by a licensed psychologist and lasted for about two hours. The psychologists were unaware of the study hypotheses and not informed about group allocation to ensure an independent diagnostic process before and after treatment.
Table 2.
Diagnoses of the participants as reported in the SCID interviews at pre-treatment.
| ICBT (n = 48) |
Control (n = 47) |
Total (n = 95) |
|
|---|---|---|---|
| Depressive disorders | |||
| Major depressive disorder | 33 (68.8%) | 35 (74.5%) | 68 (71.6%) |
| Dysthymic disorder | 6 (12.5%) | 3 (6.4) | 9 (9.5%) |
| Depressive disorder NOS | 2 (4.2%) | 2 (4.2%) | 4 (4.2%) |
| MDD in partial remission | 8 (16.7%) | 7 (14.9%) | 15 (15.8%) |
| Any depressive disorder | 48 (100%) | 47 (100%) | 95 (100%) |
| Anxiety disorders | |||
| GAD | 4 (8.3%) | 3 (6.4%) | 7 (7.4%) |
| Panic disorder with or without agoraphobia | 7 (14.6%) | 7 (14.9%) | 14 (14.7%) |
| Specific phobia | 3 (6.3%) | 5 (10.6%) | 8 (8.4%) |
| Social phobia | 4 (8.3%) | 1 (2.1%) | 5 (5.3%) |
| OCD | 3 (6.3%) | 2 (4.3%) | 5 (5.3%) |
| PTSD | 1 (2.1%) | 2 (4.3%) | 3 (3.2%) |
| Anxiety disorder NOS | 4 (8.3%) | 5 (10.6%) | 9 (9.5%) |
| Any anxiety disorder | 21 (43.8%) | 24 (51.1%) | 45 (47.4%) |
| Personality disorders | |||
| Borderline | 1 (2.1%) | 2 (4.3%) | 3 (3.2%) |
| Obsessive-compulsive | 1 (2.1%) | 1 (2.1%) | 2 (2.1%) |
| Antisocial | 2 (4.2%) | 0 (0.0%) | 2 (2.1%) |
| Depressive | 2 (4.2%) | 2 (4.3%) | 4 (4.2%) |
| Avoidant | 0 (0.0%) | 3 (6.4%) | 3 (3.2%) |
| Passive-aggressive | 0 (0.0%) | 1 (2.1%) | 1 (1.1%) |
| Personality disorder NOS | 1 (2.1%) | 1 (2.1%) | 2 (2.1%) |
| Any personality disorder | 7 (14.6%) | 7 (14.9%) | 14 (14.7%) |
| Other disorders | |||
| Maladaptive stress reaction | 3 (6.3%) | 2 (4.3%) | 5 (5.3%) |
| Eating disorder | 1 (2.1%) | 0 (0.0%) | 1 (1.1%) |
| Substance-related disorder | 0 (0.0%) | 3 (6.4%) | 3 (3.2%) |
| Any other disorder | 4 (8.3%) | 5 (10.6%) | 9 (9.5%) |
Note: NOS = not otherwise specified; MDD = Major depressive disorder; GAD = Generalized anxiety disorder; OCD = Obsessive compulsive disorder; PTSD = Post traumatic stress disorder. A patient could have more than one diagnosis.
The participants were randomized to either ICBT or active control. The randomization sequence had differing block sizes, unknown to the researchers, which was prepared in advance by a statistician. A numbered opaque envelope was opened for each participant after the decision of inclusion was made. The patients were recommended to complete approximately one module per week, and hence the treatment in eight weeks. At the start, the participants had access to one module and subsequently to the other modules in sequence when the treating psychologist considered that all homework had been completed satisfactorily. Each module contained questions to answer and return to the psychologist via the online platform.
To identify deterioration or suicidal tendencies, patients were asked to complete weekly self-ratings with the MADRS-S. In cases where a participant rated 4 or higher on MADRS-S item 9 (zest for life) the treating psychologist contacted the participant for an assessment of current suicidal ideation and possible referral to further care.
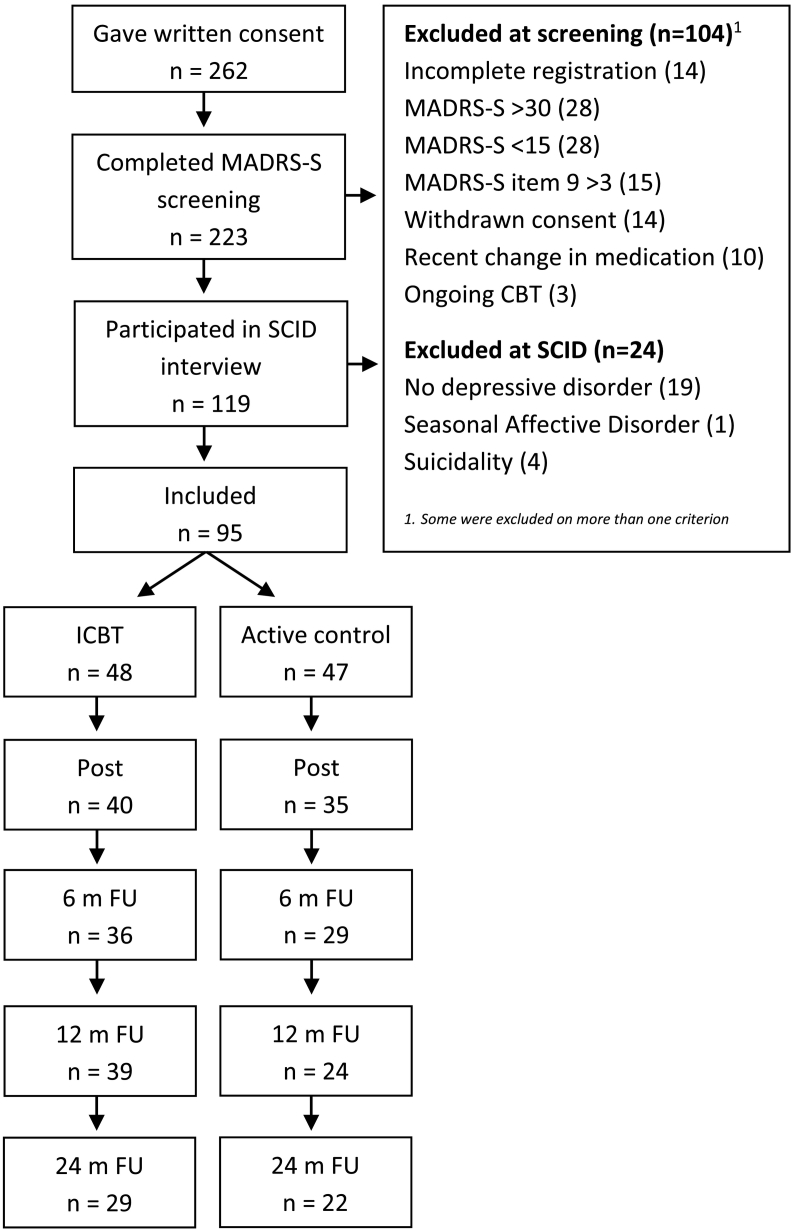
After treatment, all patients were called for a second SCID-I face-to-face interview. They were also asked to fill out self-ratings (MADRS-S and BDI-II) on the website at post-treatment and after 6, 12 and 24 months. A flow chart of patient participation is presented in Fig. 1.
Fig. 1.
Participant flowchart (remaining participants are based on MADRS-S ratings).
The protocol was approved by the Regional Ethics Committee in Uppsala, Sweden (No. 2006:038). No trial registration was made.
2.4. Treatment content
A secure web-based platform was constructed for the study where participants logged in with unique user names and passwords and completed their self-ratings on the MADRS-S and BDI-II. The participants gained access to their treatment material, ICBT, or active control (in accordance with their random allocation) on the platform. There was also a messaging service (similar to email), by which the participants in both groups had most of their contact with the psychologist. The participants could send messages to the psychologist without restrictions and typically did so once a week. Messages were normally responded to within one working day. At the end of each module there were mandatory questions that all participants answered in a message to their psychologist. The psychologist gave feedback on completed homework, answered questions and gave access to the next module in their replies. Feedback on homework in the ICBT-group were typically written to help the participant to understand and to use the strategies in behavioral activation and cognitive restructuring. In the control group however, the messages from the psychologist were restricted to support and did not contain any suggestions about altering behavior or challenging negative thoughts.
The two treatment materials compared in the study differed in content but were both divided into modules with questions at the end. The guided self-help program was a modified version of the material used in previous RCTs (Andersson et al., 2005; Vernmark et al., 2010). It consisted of eight text modules including exercises and comprised 39,000 words (114 pages) in total. The material started with an introduction to CBT followed by a module about depression from a CBT-perspective with a behavioral focus (Martell et al., 2001). There were two modules on behavioral activation and one on cognitive restructuring (Beck, 1979). There was one basic module on sleep and relaxation (Morin, 1996) and one optional module on more advanced strategies for improved sleep. The final module was designed to help patients in defining long-term goals (Wilson and Murrell, 2004) and relapse prevention (Gortner et al., 1998).
The material read by the active control group consisted of information about depression. It was divided into 9 modules without CBT elements and comprised 23,000 words (49 pages). The material covered information about the diagnosis of depression, epidemiology, gender differences, comorbidity and short descriptions of different psychological and pharmacological treatments.
2.5. Outcome measures
The self-reported Montgomery-Åsberg Depression Rating Scale (MADRS-S) (Svanborg and Asberg, 1994) was used to measure depressive symptoms and suicidal thoughts. MADRS-S is a self-administered version of Montgomery-Åsberg Depression Rating Scale (MADRS) (Montgomery and Asberg, 1979) and has been reported to have a high or moderate correlation with MADRS (Svanborg and Asberg, 1994; Svanborg and Asberg, 2001; Fantino and Moore, 2009).
MADRS-S is a 9-item measure where the patient is asked to answer questions by scoring them from 0 to 6. There are four type-statements for each item (representing scores 0, 2, 4 and 6) to make the scoring easier. A higher score indicates more severe depression. The maximum score for MADRS-S is 54 and the cutoff points are; 0–12 minimal, 13–19 mild, 20–34 moderate and > 34 severe(Montgomery and Asberg, 1979).
MADRS-S has been tested for reliability and validity, for instance by Fantino and Moore (2009) who analyzed data from a large group of patients diagnosed with major depressive disorder. In that study, the construct validity was found to be satisfactory and Cronbach's alpha was reported at 0.84. It has been shown that MADRS-S is sensitive to change in depressive symptoms during treatment (Montgomery and Asberg, 1979; Fantino and Moore, 2009).
In addition to MADRS-S, the Beck Depression Inventory – Second edition (BDI-II) (Beck et al., 2005) was used to measure degree of depressive symptoms. BDI-II is self-administered and it comprises 21 items. Each item yields a score of 0–3 which gives a maximum score of 63. Every item consists of a group of statements concerning a specific symptom that is common in depressions. The patient chooses which statement that best describes how he or she felt the last two weeks. BDI-II cutoff scores are; 0–13 minimal, 14–19 mild, 20–28 moderate and 29–63 severe (Beck et al., 2005).
BDI-II is a revised version of BDI, created in 1996 to meet the criteria of depression from Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition (American Psychiatric Association, 2000; Beck et al., 1996). The reliability and validity of BDI-II have been tested with good results in several studies, showing satisfactory internal consistency and test-retest reliability, and was found to differentiate well between grades of depression with sufficient sensitivity to change (Beck et al., 2005; Garcia-Batista et al., 2018; Kuhner et al., 2007; Osman et al., 2004; Storch et al., 2004). A comparative study of MADRS-S and BDI-II applied within primary care was published by (Wikberg et al., 2015), where the two instruments were found to correlate well, both with sufficient reliability measures. Both the MADRS-S and BDI-II have been validated for online use (Hollandare et al., 2010).
For the interviews, the SCID I (Structured Clinical Interview for DSM-IV-Axis I) (First et al., 1998) and SCID II (Structured Clinical Interview for DSM-IV-Axis II) (First et al., 1994) were used to obtain a good diagnostic picture of the participants.
2.6. Analyses
A group (ICBT versus control) × time (pre-, post-treatment, 6-, 12-, and 24-month follow-ups) randomized design based on the intent-to-treat model was used. Linear mixed models (Brown and Prescott, 1999) with full information maximum likelihood estimation were employed to handle missing data because repeated observations for the same individual are correlated which violates the assumption of independence (Gueorguieva and Krystal, 2004; Brown and Prescott, 1999). Full information maximum likelihood estimation has the advantage of providing accurate estimates with missing data under fairly unrestrictive missing data assumptions (Hesser, 2015) and is a recommended method for handling missing data (Schafer and Graham, 2002). Estimated parameters were obtained using a mixed-model approach employing an unstructured covariance structure. The alpha level was set at 0.05. Within and between-group effect sizes (Cohen's d) (Cohen, 1988) were first calculated using the estimated means from the mixed model analysis and are shown in Table 3. We also calculated effect sizes based on observed data (using the pooled standard deviations) for the ICBT and control group (Table 4), as well as between ICBT-patients with or without a PD (Table 5).
Table 3.
Estimated means (standard deviations) for BDI-II and MADRS-S from pre-treatment to the 24-month assessment, effect sizes within and between groups.
| Group | Pre [M (SD)] |
Post [M (SD)] |
WG d | BG d | 6-m [M (SD)] |
WG d | BG d | 12-m [M (SD)] |
WG d | BG d | 24-m [M (SD)] |
WG d | BG d | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BDI-II | ICBT | 29.5 (7.6) | 18.5 (11.8) | 1.11 | 0.23 | 14.7 (10.4) | 1.62 | 0.18 | 15.3 (11.8) | 1.43 | 0.08 | 13.5 (7.5) | 2.11 | 0.00 |
| CONT | 27.0 (7.5) | 21.2 (11.7) | 0.59 | 16.6 (11.0) | 1.10 | 16.3 (13.7) | 0.97 | 13.5 (15.4) | 1.11 | |||||
| MADRS-S | ICBT | 23.2 (4.2) | 14.5 (8.3) | 1.32 | 0.23 | 12.3 (7.6) | 1.78 | 0.27 | 12.9 (9.7) | 1.38 | 0.13 | 11.9 (10.6) | 1.40 | 0.03 |
| CONT | 22.9 (4.1) | 16.5 (8.9) | 0.92 | 14.4 (8.2) | 1.31 | 14.3 (11.7) | 0.98 | 11.6 (12.0) | 1.26 | |||||
| Q9 MADRS-S | ICBT | 2.1 (1.0) | 1.4 (1.1) | 0.67 | 0.09 | 1.1 (1.1) | 0.95 | 0.09 | 1.2 (1.3) | 0.78 | 0.07 | 1.0 (1.7) | 0.81 | 0.06 |
| CONT | 2.2 (1.0) | 1.5 (1.2) | 0.63 | 1.2 (1.2) | 0.91 | 1.3 (1.6) | 0.67 | 1.1 (1.4) | 0.92 |
Note. BDI-II = Beck Depression Inventory – Second Edition, BG = between-group, ICBT = internet-based cognitive behavior therapy, CONT = control group, d = Cohen's d, M = mean, MADRS-S = Montgomery-Åsberg Depression Rating Scale – self-rated version, SD = standard deviation, WG = within-group. All the within-group effect sizes were calculated based on the pre-treatment scores.
Table 4.
Within and between-group effect size (Cohens' d), based on observed data, at post-treatment and the 6-, 12- and 24-month follow-ups.
| Within-group effect size |
Between-group effect size |
||
|---|---|---|---|
| ICBT | Active control | ICBT vs. Active control | |
| MADRS-S | |||
| Post-treatment | 1.57 | 1.00 | 0.31 |
| 6-month follow-up | 2.02 | 1.37 | 0.30 |
| 12-month follow-up | 1.42 | 1.25 | 0.15 |
| 24-month follow-up | 1.80 | 1.55 | 0.01 |
| BDI-II | |||
| Post-treatment | 1.40 | 0.65 | 0.22 |
| 6-month follow-up | 1.78 | 1.11 | 0.20 |
| 12-month follow-up | 1.48 | 0.93 | 0.13 |
| 24-month follow-up | 1.75 | 1.20 | 0.06 |
Table 5.
Mean difference between participants with and without a personality disorder (PD) on the MADRS-S and BDI-II as well as between-group (no PD vs. PD) effect size (Cohens' d), based on observed data, at post-treatment and the 6-, 12- and 24-month follow-ups for the ICBT group.
| Mean difference no PD vs. PD | Between-group effect size | |
|---|---|---|
| MADRS-S | ||
| Pre-treatment | 0.07 | 0.02 |
| Post-treatment | 6.74 | 0.97 |
| 6-month follow-up | 1.77 | 0.28 |
| 12-month follow-up | 10.76 | 1.25 |
| 24-month follow-up | 5.14 | 0.62 |
| BDI-II | ||
| Pre-treatment | −0.80 | −0.11 |
| Post-treatment | 8.06 | 0.90 |
| 6-month follow-up | 1.56 | 0.18 |
| 12-month follow-up | 9.43 | 0.94 |
| 24-month follow-up | 5.93 | 0.54 |
For remission rates, clinically significant change was determined for BDI-II by using a combination of a lower limit cut-off score (two standard deviations from the pretest mean) and a minimum improvement score calculated by means of the Reliable Change Index (RCI) for each individual. The formulas provided by Jacobson and Truax (1991) were employed. The RCI was calculated using a test-retest reliability of 0.80 for both the MADRS-S (Svanborg and Asberg, 1994) and the BDI-II (Beck et al., 1996). The RCI cut-off was 1.96 (p < .05). For the MADRS-S the change is considered reliable and clinically significant if the score is below 15 points and has decreased by at least 5 points, and for the BDI-II when the score is below 13 points and has decreased at least 10 points. Cut-offs using these formulas have been applied in previous ICBT research (Berger et al., 2011b). In the RCI-analyses, missing data was replaced with the last known value. The second way of determining clinical significance was whether the participants were diagnosed with a depressive disorder in the SCID interview after treatment. No assumptions were made about diagnostic status for participants who we were unable to interview at post treatment. Chi 2 tests were used to analyse the difference in proportions with diagnose between the groups.
Multiple regression analyses were performed to assess whether comorbidity predicted the improvement in depressive symptoms. The outcome variables were standardized change scores on the MADRS-S and the BDI-II between pre and post-treatment, calculated with the formula Z2 − (Z1 ∗ R1 2) (Steketee and Chambless, 1992). The independent variables, i.e. the presence (or non-presence) of an anxiety disorder or a personality disorder, were inserted simultaneously into the model.
3. Results
3.1. Adherence
In the ICBT group, the mean number of modules completed was 5.9 (SD = 2.2) (range 1–8) out of a maximum of 8 (73.8%). In the control condition, an average of 6.8 (SD = 3.1) (range 1–9) modules were completed out of a maximum of 9 (75.6%).
3.2. Clinical significance
There was no significant difference between the proportions of patients with the diagnosis of major depression at pre-treatment in the two groups (χ2 = 0.38, df = 1, p = .537) nor any difference between the proportions of those fulfilling the criteria for any depressive disorder at pre-treatment in the two groups (χ2 = 0.56, df = 1, p = .81) (see Table 2). In the ICBT group, the number diagnosed with MDD dropped from 33/48 (68.8%) participants at pre-treatment to 9/38 (23.7%) after treatment. In the control group, the number diagnosed with MDD decreased from 35/47 (74.5%) to 19/36 (52.7%). After treatment, significantly fewer participants in the ICBT group fulfilled the criteria for MDD compared to the control group (χ2 = 6.653, df = 1, p = .01). The proportions fulfilling the criteria for any depressive disorder at post-treatment in the two groups did not differ significantly (χ2 = 1.9, df = 1, p = .168).
From pre- to post-treatment, 56% (n = 27) of the participants in the ICBT group exhibited reliable change (Jacobson and Truax, 1991) on the BDI-II compared to 36% (n = 17) in the control group. Although the difference was not significant, a trend favoring ICBT could be observed (χ2 = 3.646, df = 1, p = .056). At the 6-month follow-up, 60% (n = 29) in the ICBT group and 38% (n = 18) in the control group demonstrated reliable change. At this stage the difference between the two groups had decreased (χ2 = 2.109, df = 1, p = .146). Similar results were found at the 12-month follow-up; 58% (n = 28) in the ICBT group and 30% (n = 14) in the control group exhibited reliable change (χ2 = 1.212, df = 1, p = .271).
3.3. Changes over time on the BDI-II: ICBT versus active control
The estimated means and statistics for the two groups across time for the BDI-II are presented in Table 3. Mixed-effect models showed a non-significant group effect (F = 0.01, df = 94.33, p = .991), a significant time effect (F = 63.28, df = 78.06, p < .001), and a significant group × time effect on the BDI-II (F = 5.52, df = 78.06, p = .021) from pre to post-treatment in favor of the ICBT group.
Further analyses were carried out to examine changes from pre-treatment to 6-, 12- and 24-month follow-ups. Mixed-effect models showed a non-significant group effect (F = 0.08, df = 87.72, p = .782), a significant time effect (F = 64.09, df = 75.86, p < .001), and a non-significant group × time effect on the BDI-II (F = 3.01, df = 75.86, p = .055) from pre-treatment to the 6-month follow-up. Mixed effect models also demonstrated a non-significant group effect (F = 0.19, df = 81.27, p = .661), a significant time effect (F = 42.68, df = 70.61, p < .001), and a non-significant group × time effect on the BDI-II (F = 2.44, df = 70.61, p = .071) from pre-treatment to the 12-month follow-up. There was a non-significant group effect (F = 0.47, df = 73.61, p = .496), a significant time effect (F = 90.91, df = 55.82, p < .001), and a non-significant group × time effect on the BDI-II (F = 0.68, df = 55.82, p = .414) from pre-treatment to the 24-month follow-up.
Finally, analyses were carried out to examine changes from post-treatment to the 6-, 12- and 24-month follow-ups. Mixed-effect models showed a non-significant group effect (F = 0.88, df = 74.96, p = .351; F = 0.36, df = 74.96, p = .553; F = 0.94, df = 68.82, p = .760), a significant time effect (F = 10.17, df = 70.61, p = .002; F = 7.48, df = 67.46 p = .008; F = 15.13, df = 54.75, p < .001), and a non-significant group × time effect on the BDI-II (F = 0.18, df = 70.61, p = .670; F = 0.92, df = 67.46, p = .341; F = 1.51, df = 54.75, p = .225) from post-treatment to the 6-, 12- and 24-month follow-up respectively.
3.4. Changes over time on the MADRS-S: ICBT versus active control
The estimated MADRS-S means and statistics for the two groups over time are presented in Table 3. Mixed-effect models showed a non-significant group effect (F = 0.55, df = 85.56, p = .460), a significant effect of time (F = 83.11, df = 75.41, p < .001), and a non-significant group × time effect on the MADRS-S (F = 1.99, df = 75.41, p = .163) from pre- to post-treatment.
Further analyses were carried out to examine changes from pre-treatment to the 6-, 12- and 24-month follow-ups. Mixed-effect models showed a non-significant group effect (F = 0.99, df = 76.61, p = .323), a significant time effect (F = 74.86, df = 70.63, p < .001), and a non-significant group × time effect on the MADRS-S (F = 1.16, df = 70.63, p = .318) from pre-treatment to the 6-month follow-up. There was a non-significant group effect (F = 1.17, df = 71.28, p = .282), a significant effect of time (F = 53.09, df = 65.53, p < .001), and a non-significant group × time effect on the MADRS-S (F = 1.09, df = 65.53, p = .358) from pre-treatment to the 12-month follow-up. Likewise, there was a non-significant group effect (F = 0.06, df = 60.65, p = .804), a significant time effect (F = 89.46, df = 54.04, p < .001), and a non-significant group × time effect on the MADRS-S (F = 0.01, df = 54.04, p = .974) from pre-treatment to the 24-month follow-up.
Finally, analyses were carried out to examine changes from post-treatment to the 6-, 12- and 24-month follow-ups. There was a non-significant group effect (F = 2.03, df = 74.41, p = .159; F = 1.06, df = 74.91, p = .306; F = 0.24, df = 68.08, p = .627), a significant time effect (F = 4.67, df = 70.99, p = .034; F = 4.05, df = 65.53, p = .048; F = 10.62, df = 55.02, p = .002), and a non-significant group × time effect on the MADRS-S (F = 0.15, df = 70.99, p = .699; F = 0.56, df = 65.53, p = .457; F = 2.23, df = 55.02, p = .141) from post-treatment to the 6-, 12- and 24-month follow-ups.
3.5. Changes over time on suicidal thoughts (MADRS-S item 9): ICBT versus active control
The estimated MADRS-S item 9 (zest for life) means and statistics for the two groups across time are presented in Table 3. Mixed-effect models revealed a non-significant group effect (F = 0.13, df = 91.23, p = .724), a significant effect of time (F = 41.40, df = 80.24, p < .001), and a non-significant group × time effect on item 9 (F = 0.01, df = 80.24, p = .999) from pre- to post-treatment.
There was a non-significant group effect (F = 0.05, df = 85.25, p = .832), a significant time effect (F = 36.50, df = 74.02, p < .001), and a non-significant group × time effect on item 9 (F = 0.07, df = 74.02, p = .935) from pre-treatment to the 6-month follow-up. Likewise, there was a non-significant group effect (F = 0.21, df = 89.72, p = .649), a significant time effect (F = 26.20, df = 69.81, p < .001), and a non-significant group × time effect on item 9 (F = 0.09, df = 69.81, p = .968) from pre-treatment to the 12-month follow-up. There was also a non-significant group effect (F = 0.01, df = 75.92, p = .932), a significant time effect (F = 46.07, df = 57.22, p < .001), and a non-significant group × time effect on item 9 (F = 0.09, df = 57.22, p = .767) from pre-treatment to the 24-month follow-up.
Finally, analyses were carried out to examine changes from post-treatment to the 6-, 12- and 24-month follow-ups. There was a non-significant group effect (F = 0.05, df = 75.60, p = .832; F = 0.28, df = 77.82, p = .597; F = 0.01, df = 68.91, p = .990), a mixed effect of time (F = 3.98, df = 72.02, p = .050; F = 2.06, df = 68.81, p = .156; F = 5.85, df = 53.35, p = .019), and a non-significant group × time effect on item 9 (F = 0.22, df = 72.02, p = .638; F = 0.01, df = 68.81, p = .934; F = 0.86, df = 53.35, p = .358) from post-treatment to the 6-, 12- and 24-month follow-ups.
3.6. Effects of comorbidity
The presence of a personality disorder (PD) was found to significantly predict a lower level of improvement in depressive symptoms between pre- and post-treatment when measured by the MADRS-S (β = −0.342, t(39) = −2.213, p = .033), and when measured by the BDI-II (β = −0.321, t(39) = −2.151, p = .038). The presence of an anxiety disorder did not significantly predict the level of improvement in depressive symptoms when measured by MADRS-S (β = −0.051, t(39) = −0.327, p = .746), or when measured by the BDI-II (β = −0.299, t(39) = −2.009, p = .052) although a trend was observed.
3.7. Effect sizes based on observed data
The effect sizes (Cohen's d) calculated using observed data for both MADRS-S and BDI-II were large within both the ICBT group and the control group at post-treatment and small between groups (Table 4). The between-groups effect sizes (Cohen's d) calculated using observed data to compare participants with and without PDs in the ICBT group were large at post-treatment (Table 5).
4. Discussion
The aim of this study was to compare ICBT to an active control condition in a clinical sample of patients with a depressive disorder recruited from primary and psychiatric care. Significantly more ICBT patients had entered remission after treatment compared to the active control patients. Internet-based CBT reduced depressive symptoms (measured by BDI-II) significantly more than an active control condition between pre- and post-treatment in a clinical sample. During follow-up, the difference in symptom levels between the groups decreased and disappeared after two years, however, the improvements were sustained during two years. The effect size of ICBT in this study can be considered large. The effect of ICBT on depressive symptoms was not significantly moderated by the presence of a comorbid anxiety disorder, but was clearly reduced in cases with a personality disorder.
We are not aware of any previous study that has investigated the effect of comorbid personality pathology on ICBT for depression. In the present study, we found that on average, patients without PD had almost a one standard deviation larger improvement at post-treatment than those with PD. This is in line with previous research on psychotherapy face-to-face (Newton-Howes et al., 2006; Newton-Howes et al., 2014), however, we are not aware of any previous studies showing that patients with PD may also benefit far less from internet based CBT for depression. This result needs to be replicated, preferably with a larger sample that enables examination of possible differences in effect from specific PDs. If this result is replicated it raises the question if ICBT can be adapted to become an effective treatment for depression when comorbidity with a PD is present. Including elements from dialectic behavior therapy (DBT) (Linehan, 1993) could be one way of adapting the treatment for the needs of some patients with a PD since it has been shown to be an effective face-to-face psychotherapy for patients with borderline personality disorder (Linehan et al., 2006; Cristea et al., 2017) and has also shown an effect on depressive symptoms in cases with comorbidity (Lynch et al., 2007).
The within-group effect size of ICBT in this study was (d) = 1.4, which should be compared to (d) = 1.23 in the efficacy study by Andersson et al. (2005), as the treatment content is almost identical. However, the sample in the study by Andersson et al. (2005) was recruited through the media and the study was conducted in a university setting. This provides further evidence that ICBT can yield a similar effect in a health care setting as in previous efficacy studies. The effect in the present study was similar to the effects in previous effectiveness studies, e.g. (d) = 1.27 (Hedman et al., 2014), (d) = 1.0 (calculated with observed means) (Titov et al., 2015), and (d) = 1.09 (Kivi et al., 2014).
The effect of the active control treatment was surprisingly large in view of the fact that the modules did not contain any suggestions for altering behavior or questioning dysfunctional thoughts. One possible explanation is that therapist support seems to be responsible for a large proportion of the effect in meta-analyses. The therapists were instructed to only offer support to the control patients and not provide any guidance resembling CBT techniques to ensure that no CBT elements would seep into the control treatment. However, recent results reveal that therapist guidance in ICBT is also mainly supportive (Holländare et al., 2016) so perhaps the effect of supportive guidance explains why the control patients also improved over time. Another possibility is that merely reading the information material increased activity levels, which could have reduced depressive symptoms.
The effect of ICBT in this study was not significantly reduced by the presence of an anxiety disorder, which is in line with a recent meta-analysis by Karyotaki et al. (2018) which found no difference in outcome after ICBT for depression between patients with and without comorbid anxiety. However, our result showing that the presence of a PD did reduce the effect of ICBT raises questions about the effect of other possible comorbidities, e.g., neuropsychiatric disorders or substance abuse, on the outcome of internet bases CBT. More knowledge about the effect of comorbidities on ICBT outcome could help guide clinical decisions and the development of adapted treatments for subgroups.
The drop-out rate was higher in the control condition compared to the ICBT. Since CBT is a well-known form of therapy and the information condition is not an established intervention, a speculation is that some of those randomized to information dropped out due to disappointment with their allocation. Another speculation is that they might have found the modules or the therapist guidance ineffective or unappealing. The randomized design and long term follow-up are strengths of this study. The inclusion of more than one depressive disorder might increase external validity because the case mix was derived from a recruitment process within a regular clinical health care setting. The aim of the recruitment process was that each participant should be eligible for health care before being asked to participate, making the sample representative of those who normally seek help for depression. Additional strengths are the thorough diagnostic process using face-to-face SCID-I interviews before and after treatment, which were conducted by clinical psychologists who were not aware of the patients' allocation. Another strength is the use of outcome measures that have been validated for online use (Hollandare et al., 2010). The limited sample size did not allow for analyses of the impact on outcome from different personality disorders, and also makes the estimate of the size of differences in outcome between patients with and without PD imprecise (Kapur and Munafo, 2019). Another limitation was missing data during the follow up which limits statistical power. We did not assess PD after the intervention which limits our knowledge of diagnostic status post treatment.
5. Conclusions
In Conclusion, although ICBT reduced depressive symptoms more than an active control condition directly after treatment, the two interventions seemed to have a similar effect over time. Depressed patients within primary and psychiatric care, with or without a comorbid anxiety disorder, can benefit from ICBT. Patients with a PD seem to benefit less from ICBT for depression, however this needs to be investigated further.
Funding
Financial support for the study was provided by two Swedish research funds: Region Örebro County Research Committee [OLL-57/06], and the Regional Research Council [RFR-73351]. No funding body took part in designing the study, collecting or analysing the data, interpreting the results or writing the manuscript.
Declaration of competing interest
The authors have declared that no conflict of interest exists.
Contributor Information
Anna-Lena Flygare, Email: anna-lena.flygare@liv.se.
Ingemar Engström, Email: ingemar.engstrom@regionorebrolan.se.
Mikael Hasselgren, Email: mikael.hasselgren@oru.se.
Markus Jansson-Fröjmark, Email: markus.jansson-frojmark@ki.se.
Rikard Frejgrim, Email: rikard.frejgrim@clarahalsan.se.
Gerhard Andersson, Email: geran@ibv.liu.se.
Fredrik Holländare, Email: fredrik.hollandare@regionorebrolan.se.
References
- American Psychiatric Association . 4th ed. American Psychiatric Press; Washington DC: 2000. Diagnostic and Statistical Manual of Mental Disorders. Text Revision. [Google Scholar]
- Andersson G. Internet-delivered psychological treatments. Annu. Rev. Clin. Psychol. 2016;12:157–179. doi: 10.1146/annurev-clinpsy-021815-093006. [DOI] [PubMed] [Google Scholar]
- Andersson G., Bergstrom J., Hollandare F., Carlbring P., Kaldo V., Ekselius L. Internet-based self-help for depression: randomised controlled trial. Br. J. Psychiatry. 2005;187:456–461. doi: 10.1192/bjp.187.5.456. [DOI] [PubMed] [Google Scholar]
- Andersson G., Carlbring P., Holmstrom A., Sparthan E., Furmark T., Nilsson-Ihrfelt E., Buhrman M., Ekselius L. Internet-based self-help with therapist feedback and in vivo group exposure for social phobia: a randomized controlled trial. J. Consult. Clin. Psychol. 2006;74:677–686. doi: 10.1037/0022-006X.74.4.677. [DOI] [PubMed] [Google Scholar]
- Andersson G., Carlbring P., Ljótsson B., Hedman E. Guided internet-based CBT for common mental disorders. J. Contemp. Psychother. 2013;43:223–233. [Google Scholar]
- Andersson G., Hesser H., Hummerdal D., Bergman-Nordgren L., Carlbring P. A 3.5-year follow-up of internet-delivered cognitive behavior therapy for major depression. J. Ment. Health. 2013;22:155–164. doi: 10.3109/09638237.2011.608747. (Epub 2011 Sep 29) [DOI] [PubMed] [Google Scholar]
- Andersson G., Topooco N., Havik O., Nordgreen T. Internet-supported versus face-to-face cognitive behavior therapy for depression. Expert. Rev. Neurother. 2016;16:55–60. doi: 10.1586/14737175.2015.1125783. (Epub 2015 Dec 15) [DOI] [PubMed] [Google Scholar]
- Beck A.T. Guilford Press; 1979. Cognitive Therapy of Depression. [Google Scholar]
- Beck A.T., Steer R.A., Brown G.K. Psychological Corporation; San Antonio, TX: 1996. Manual for the Beck Depression Inventory-II. [Google Scholar]
- Beck A.T., Steer R.A., Brown G.K. Psykologiförlaget; Sandviken: 2005. BDI-II, Beck Depression Inventory - Second Edition. Manual - Svensk Version. [Google Scholar]
- Berger T., Caspar F., Richardson R., Kneubuhler B., Sutter D., Andersson G. Internet-based treatment of social phobia: a randomized controlled trial comparing unguided with two types of guided self-help. Behav. Res. Ther. 2011;49:158–169. doi: 10.1016/j.brat.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Berger T., Hammerli K., Gubser N., Andersson G., Caspar F. Internet-based treatment of depression: a randomized controlled trial comparing guided with unguided self-help. Cogn. Behav. Ther. 2011;40:251–266. doi: 10.1080/16506073.2011.616531. [DOI] [PubMed] [Google Scholar]
- Botella C., Gallego M.J., Garcia-Palacios A., Guillen V., Banos R.M., Quero S., Alcaniz M. An internet-based self-help treatment for fear of public speaking: a controlled trial. Cyberpsychol. Behav. Soc. Netw. 2010;13:407–421. doi: 10.1089/cyber.2009.0224. [DOI] [PubMed] [Google Scholar]
- Brown H., Prescott R. John Wiley & Sons; Chichester: 1999. Applied Mixed Models in Medicine. [Google Scholar]
- Carlbring P., Nilsson-Ihrfelt E., Waara J., Kollenstam C., Buhrman M., Kaldo V., Soderberg M., Ekselius L., Andersson G. Treatment of panic disorder: live therapy vs. self-help via the internet. Behav. Res. Ther. 2005;43:1321–1333. doi: 10.1016/j.brat.2004.10.002. [DOI] [PubMed] [Google Scholar]
- Carlbring P., Hägglund M., Luthström A., Dahlin M., Kadowaki Å., Vernmark K., Andersson G. Internet-based behavioral activation and acceptance-based treatment for depression: a randomized controlled trial. J. Affect. Disord. 2013;148(2–3):331–337. doi: 10.1016/j.jad.2012.12.020. [DOI] [PubMed] [Google Scholar]
- Cohen J. Lawrence Erlbaum Associates; 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Cristea I.A., Gentili C., Cotet C.D., Palomba D., Barbui C., Cuijpers P. Efficacy of psychotherapies for borderline personality disorder: a systematic review and meta-analysis. JAMA Psychiat. 2017;74:319–328. doi: 10.1001/jamapsychiatry.2016.4287. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Fogliati V.J., Fogliati R., Johnson B., Boyle O., Karin E., Gandy M., Kayrouz R., Staples L.G., Titov N. Treating anxiety and depression in young adults: a randomised controlled trial comparing clinician-guided versus self-guided internet-delivered cognitive behavioural therapy. Aust. N. Z. J. Psychiatry. 2018;52:668–679. doi: 10.1177/0004867417738055. [DOI] [PubMed] [Google Scholar]
- Fantino B., Moore N. The self-reported Montgomery-Asberg Depression Rating Scale is a useful evaluative tool in major depressive disorder. BMC Psychiatry. 2009;9:26. doi: 10.1186/1471-244X-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M., Spitzer R., Gibbon M., Williams J., Benjamin L. Biometric Research Department; New York: 1994. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID II) [Google Scholar]
- First M.B., Gibbon M., Spitzer R.L., Williams J.B.W. Pilgrim Press; Danderyd: 1998. Structured Clinical Interview for DSM-IV Disorders (SCID-I) (Swedish Version) [Google Scholar]
- Forand N.R., Derubeis R.J. Pretreatment anxiety predicts patterns of change in cognitive behavioral therapy and medications for depression. J. Consult. Clin. Psychol. 2013;81:774–782. doi: 10.1037/a0032985. (Epub 2013 May 6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier J.C., Derubeis R.J., Shelton R.C., Gallop R., Amsterdam J.D., Hollon S.D. Antidepressant medications v. cognitive therapy in people with depression with or without personality disorder. Br. J. Psychiatry. 2008;192:124–129. doi: 10.1192/bjp.bp.107.037234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friborg O., Martinsen E.W., Martinussen M., Kaiser S., Overgård K.T., Rosenvinge J.H. Comorbidity of personality disorders in mood disorders: a meta-analytic review of 122 studies from 1988 to 2010. J. Affect. Disord. 2014;152–154:1–11. doi: 10.1016/j.jad.2013.08.023. [DOI] [PubMed] [Google Scholar]
- Garcia-Batista Z.E., Guerra-Pena K., Cano-Vindel A., Herrera-Martinez S.X., Medrano L.A. Validity and reliability of the Beck Depression Inventory (BDI-II) in general and hospital population of Dominican Republic. PLoS One. 2018;13 doi: 10.1371/journal.pone.0199750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons C.J., Derubeis R.J. Anxiety symptom focus in sessions of cognitive therapy for depression. Behav. Ther. 2008;39:117–125. doi: 10.1016/j.beth.2007.05.006. (Epub 2007 Oct 31) [DOI] [PubMed] [Google Scholar]
- Gortner E.T., Gollan J.K., Dobson K.S., Jacobson N.S. Cognitive-behavioral treatment for depression: relapse prevention. J. Consult. Clin. Psychol. 1998;66:377–384. doi: 10.1037//0022-006x.66.2.377. [DOI] [PubMed] [Google Scholar]
- Gueorguieva R., Krystal J.H. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch. Gen. Psychiatry. 2004;61:310–317. doi: 10.1001/archpsyc.61.3.310. [DOI] [PubMed] [Google Scholar]
- Hadjistavropoulos H.D., Nugent M.M., Alberts N.M., Staples L., Dear B.F., Titov N. Transdiagnostic internet-delivered cognitive behaviour therapy in Canada: an open trial comparing results of a specialized online clinic and nonspecialized community clinics. J. Anxiety Disord. 2016;42:19–29. doi: 10.1016/j.janxdis.2016.05.006. [DOI] [PubMed] [Google Scholar]
- Hedman E., Ljotsson B., Lindefors N. Cognitive behavior therapy via the internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev. Pharmacoecon. Outcomes Res. 2012;12:745–764. doi: 10.1586/erp.12.67. [DOI] [PubMed] [Google Scholar]
- Hedman, E., Ljotsson, B., Kaldo, V., Hesser, H., EL Alaoui, S., Kraepelien, M., Andersson, E., Ruck, C., Svanborg, C., Andersson, G. & Lindefors, N. 2014. Effectiveness of internet-based cognitive behaviour therapy for depression in routine psychiatric care. J. Affect. Disord., 155:49–58., 10.1016/j.jad.2013.10.023. (Epub 2013 Oct 26). [DOI] [PubMed]
- Heinrich S., Rozental A., Carlbring P., Andersson G., Cotter K., Weise C. Treating tinnitus distress via the internet: a mixed methods approach of what makes patients seek help and stay motivated during internet-based cognitive behavior therapy. Internet Interv. 2016;4:120–130. doi: 10.1016/j.invent.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesser H. Modeling individual differences in randomized experiments using growth models: recommendations for design, statistical analysis and reporting of results of internet interventions. Internet Interv. 2015;2:110–120. [Google Scholar]
- Hollandare F., Andersson G., Engstrom I. A comparison of psychometric properties between internet and paper versions of two depression instruments (BDI-II and MADRS-S) administered to clinic patients. J. Med. Internet Res. 2010;12:e49. doi: 10.2196/jmir.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollandare F., Anthony S.A., Randestad M., Tillfors M., Carlbring P., Andersson G., Engstrom I. Two-year outcome of internet-based relapse prevention for partially remitted depression. Behav. Res. Ther. 2013;51:719–722. doi: 10.1016/j.brat.2013.08.002. (Epub 2013 Aug 16) [DOI] [PubMed] [Google Scholar]
- Holländare F., Gustafsson S., Berglind M., Grape F., Carlbring P., Andersson G., Hadjistavropoulos H., Tillfors M. Therapist behaviours in internet-based cognitive behaviour therapy (ICBT) for depressive symptoms. Internet Interv. 2016;3:1–7. doi: 10.1016/j.invent.2015.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivarsson D., Blom M., Hesser H., Carlbring P., Enderby P., Nordberg R., Andersson G. Guided internet-delivered cognitive behaviour therapy for post-traumatic stress disorder: a randomized controlled trial. Internet Interv. 2014;1:33–40. [Google Scholar]
- Jacobson N.S., Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Johansson R., Andersson G. Internet-based psychological treatments for depression. Expert. Rev. Neurother. 2012;12:861–870. doi: 10.1586/ern.12.63. [DOI] [PubMed] [Google Scholar]
- Johansson R., Bjorklund M., Hornborg C., Karlsson S., Hesser H., Ljotsson B., Rousseau A., Frederick R.J., Andersson G. Affect-focused psychodynamic psychotherapy for depression and anxiety through the internet: a randomized controlled trial. PeerJ. 2013;1:e102. doi: 10.7717/peerj.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson O., Bjarehed J., Andersson G., Carlbring P., Lundh L.G. Effectiveness of guided internet-delivered cognitive behavior therapy for depression in routine psychiatry: a randomized controlled trial. Internet Interv. 2019;17:100247. doi: 10.1016/j.invent.2019.100247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce P.R., Mckenzie J.M., Carter J.D., Rae A.M., Luty S.E., Frampton C.M., Mulder R.T. Temperament, character and personality disorders as predictors of response to interpersonal psychotherapy and cognitive-behavioural therapy for depression. Br. J. Psychiatry. 2007;190:503–508. doi: 10.1192/bjp.bp.106.024737. [DOI] [PubMed] [Google Scholar]
- Kampmann I.L., Emmelkamp P.M., Morina N. Meta-analysis of technology-assisted interventions for social anxiety disorder. J. Anxiety Disord. 2016;42:71–84. doi: 10.1016/j.janxdis.2016.06.007. [DOI] [PubMed] [Google Scholar]
- Kapur S., Munafo M. Small sample sizes and a false economy for psychiatric clinical trials. JAMA Psychiatry. 2019;76:676–677. doi: 10.1001/jamapsychiatry.2019.0095. [DOI] [PubMed] [Google Scholar]
- Karyotaki E., Ebert D.D., Donkin L., Riper H., Twisk J., Burger S., Rozental A., Lange A., Williams A.D., Zarski A.C., Geraedts A., Van Straten A., Kleiboer A., Meyer B., Unlu Ince B.B., Buntrock C., Lehr D., Snoek F.J., Andrews G., Andersson G., Choi I., Ruwaard J., Klein J.P., Newby J.M., Schroder J., Laferton J.A.C., Van Bastelaar K., Imamura K., Vernmark K., Boss L., Sheeber L.B., Kivi M., Berking M., Titov N., Carlbring P., Johansson R., Kenter R., Perini S., Moritz S., Nobis S., Berger T., Kaldo V., Forsell Y., Lindefors N., Kraepelien M., Bjorkelund C., Kawakami N., Cuijpers P. Do guided internet-based interventions result in clinically relevant changes for patients with depression? An individual participant data meta-analysis. Clin. Psychol. Rev. 2018;63:80–92. doi: 10.1016/j.cpr.2018.06.007. [DOI] [PubMed] [Google Scholar]
- Kashdan T.B., Roberts J.E. Comorbid social anxiety disorder in clients with depressive disorders: predicting changes in depressive symptoms, therapeutic relationships, and focus of attention in group treatment. Behav. Res. Ther. 2011;49:875–884. doi: 10.1016/j.brat.2011.10.002. (Epub 2011 Oct 12) [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Merikangas K.R., Wang P.S. Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annu. Rev. Clin. Psychol. 2007;3:137–158. doi: 10.1146/annurev.clinpsy.3.022806.091444. [DOI] [PubMed] [Google Scholar]
- Kessler D., Lewis G., Kaur S., Wiles N., King M., Weich S., Sharp D.J., Araya R., Hollinghurst S., Peters T.J. Therapist-delivered internet psychotherapy for depression in primary care: a randomised controlled trial. Lancet. 2009;374:628–634. doi: 10.1016/S0140-6736(09)61257-5. [DOI] [PubMed] [Google Scholar]
- Kivi M., Eriksson M.C., Hange D., Petersson E.L., Vernmark K., Johansson B., Bjorkelund C. Internet-based therapy for mild to moderate depression in Swedish primary care: short term results from the PRIM-NET randomized controlled trial. Cogn. Behav. Ther. 2014;43:289–298. doi: 10.1080/16506073.2014.921834. (Epub 2014 Jun 9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhner C., Burger C., Keller F., Hautzinger M. Reliability and validity of the Revised Beck Depression Inventory (BDI-II). Results from German samples. Nervenarzt. 2007;78:651–656. doi: 10.1007/s00115-006-2098-7. [DOI] [PubMed] [Google Scholar]
- Linehan M. The Guilford Press; New York: 1993. Cognitive-behavioral Treatment of Borderline Personality Disorder. [Google Scholar]
- Linehan M.M., Comtois K.A., Murray A.M., Brown M.Z., Gallop R.J., Heard H.L., Korslund K.E., Tutek D.A., Reynolds S.K., Lindenboim N. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch. Gen. Psychiatry. 2006;63:757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Lis E., Myhr G. The effect of borderline personality pathology on outcome of cognitive behavior therapy. J. Psychiatr. Pract. 2016;22:270–282. doi: 10.1097/PRA.0000000000000167. [DOI] [PubMed] [Google Scholar]
- Lynch T.R., Cheavens J.S., Cukrowicz K.C., Thorp S.R., Bronner L., Beyer J. Treatment of older adults with co-morbid personality disorder and depression: a dialectical behavior therapy approach. Int. J. Geriatr. Psychiatry. 2007;22:131–143. doi: 10.1002/gps.1703. [DOI] [PubMed] [Google Scholar]
- Martell C.R., Addis M.E., Jacobson N.S. W W Norton & Company Incorporated; 2001. Depression in Context: Strategies for Guided Action. [Google Scholar]
- Mathiasen K., Riper H., Andersen T.E., Roessler K.K. Guided internet-based cognitive behavioral therapy for adult depression and anxiety in routine secondary care: observational study. J. Med. Internet Res. 2018;20 doi: 10.2196/10927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery S.A., Asberg M. A new depression scale designed to be sensitive to change. Br. J. Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Morin C.M. Broadway Books; 1996. Relief from Insomnia: Getting the Sleep of Your Dreams. [Google Scholar]
- Newton-Howes G., Tyrer P., Johnson T. Personality disorder and the outcome of depression: meta-analysis of published studies. Br. J. Psychiatry. 2006;188:13–20. doi: 10.1192/bjp.188.1.13. [DOI] [PubMed] [Google Scholar]
- Newton-Howes G., Tyrer P., Johnson T., Mulder R., Kool S., Dekker J., Schoevers R. Influence of personality on the outcome of treatment in depression: systematic review and meta-analysis. J. Personal. Disord. 2014;28:577–593. doi: 10.1521/pedi_2013_27_070. [DOI] [PubMed] [Google Scholar]
- Nordgreen T., Gjestad R., Andersson G., Carlbring P., Havik O.E. The effectiveness of guided internet-based cognitive behavioral therapy for social anxiety disorder in a routine care setting. Internet Interv. 2018;13:24–29. doi: 10.1016/j.invent.2018.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A., Kopper B.A., Barrios F., Gutierrez P.M., Bagge C.L. Reliability and validity of the Beck depression inventory—II with adolescent psychiatric inpatients. Psychol. Assess. 2004;16:120–132. doi: 10.1037/1040-3590.16.2.120. [DOI] [PubMed] [Google Scholar]
- Paxling B., Lundgren S., Norman A., Almlov J., Carlbring P., Cuijpers P., Andersson G. Therapist behaviours in internet-delivered cognitive behaviour therapy: analyses of e-mail correspondence in the treatment of generalized anxiety disorder. Behav. Cogn. Psychother. 2013;41:280–289. doi: 10.1017/S1352465812000240. (Epub 2012 May 1) [DOI] [PubMed] [Google Scholar]
- Perini S., Titov N., Andrews G. Clinician-assisted internet-based treatment is effective for depression: randomized controlled trial. Aust. N. Z. J. Psychiatry. 2009;43:571–578. doi: 10.1080/00048670902873722. [DOI] [PubMed] [Google Scholar]
- Richards D., Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin. Psychol. Rev. 2012;32:329–342. doi: 10.1016/j.cpr.2012.02.004. (Epub 2012 Feb 28) [DOI] [PubMed] [Google Scholar]
- Robinson E., Titov N., Andrews G., Mcintyre K., Schwencke G., Solley K. Internet treatment for generalized anxiety disorder: a randomized controlled trial comparing clinician vs. technician assistance. PLoS ONE [Electronic Resource] 2010;5 doi: 10.1371/journal.pone.0010942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruwaard J., Schrieken B., Schrijver M., Broeksteeg J., Dekker J., Vermeulen H., Lange A. Standardized web-based cognitive behavioural therapy of mild to moderate depression: a randomized controlled trial with a long-term follow-up. Cogn. Behav. Ther. 2009;38:206–221. doi: 10.1080/16506070802408086. [DOI] [PubMed] [Google Scholar]
- Ruwaard J., Lange A., Schrieken B., Dolan C.V., Emmelkamp P. The effectiveness of online cognitive behavioral treatment in routine clinical practice. PLoS ONE [Electronic Resource] 2012;7 doi: 10.1371/journal.pone.0040089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Ortiz V.C., Munro C., Startup H., Treasure J., Schmidt U. The role of email guidance in internet-based cognitive-behavioural self-care treatment for bulimia nervosa. Eur. Eat. Disord. Rev. 2011;19:342–348. doi: 10.1002/erv.1074. (Epub 2011 Mar 10) [DOI] [PubMed] [Google Scholar]
- Schafer J.L., Graham J.W. Missing data: our view of the state of the art. Psychol. Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schindler A., Hiller W., Witthoft M. What predicts outcome, response, and drop-out in CBT of depressive adults? A naturalistic study. Behav. Cogn. Psychother. 2013;41:365–370. doi: 10.1017/S1352465812001063. (Epub 2012 Dec 5) [DOI] [PubMed] [Google Scholar]
- Smits J.A., Minhajuddin A., Jarrett R.B. Cognitive therapy for depressed adults with comorbid social phobia. J. Affect. Disord. 2009;114:271–278. doi: 10.1016/j.jad.2008.08.008. (Epub 2008 Sep 18) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steketee G., Chambless D. Methodological issues in prediction of treatment outcome. Clin. Psychol. Rev. 1992;12:387–400. [Google Scholar]
- Storch E.A., Roberti J.W., Roth D.A. Factor structure, concurrent validity, and internal consistency of the Beck Depression Inventory-Second Edition in a sample of college students. Depress. Anxiety. 2004;19:187–189. doi: 10.1002/da.20002. [DOI] [PubMed] [Google Scholar]
- Svanborg P., Asberg M. A new self-rating scale for depression and anxiety states based on the Comprehensive Psychopathological Rating Scale. Acta Psychiatr. Scand. 1994;89:21–28. doi: 10.1111/j.1600-0447.1994.tb01480.x. [DOI] [PubMed] [Google Scholar]
- Svanborg P., Asberg M. A comparison between the Beck Depression Inventory (BDI) and the self-rating version of the Montgomery Asberg Depression Rating Scale (MADRS) J. Affect. Disord. 2001;64:203–216. doi: 10.1016/s0165-0327(00)00242-1. [DOI] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Schwencke G., Andrews G., Johnston L., Craske M.G., Mcevoy P. Transdiagnostic internet treatment for anxiety and depression: a randomised controlled trial. Behav. Res. Ther. 2011;49:441–452. doi: 10.1016/j.brat.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Johnston L., Mcevoy P.M., Wootton B., Terides M.D., Gandy M., Fogliati V., Kayrouz R., Rapee R.M. Improving adherence and clinical outcomes in self-guided internet treatment for anxiety and depression: a 12-month follow-up of a randomised controlled trial. PLoS One. 2014;9 doi: 10.1371/journal.pone.0089591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Staples L.G., Bennett-Levy J., Klein B., Rapee R.M., Shann C., Richards D., Andersson G., Ritterband L., Purtell C., Bezuidenhout G., Johnston L., Nielssen O.B. MindSpot clinic: an accessible, efficient, and effective online treatment service for anxiety and depression. Psychiatr. Serv. 2015;66:1043–1050. doi: 10.1176/appi.ps.201400477. (Epub 2015 Jul 1) [DOI] [PubMed] [Google Scholar]
- Titov N., Fogliati V.J., Staples L.G., Gandy M., Johnston L., Wootton B., Nielssen O., Dear B.F. Treating anxiety and depression in older adults: randomised controlled trial comparing guided v. self-guided internet-delivered cognitive-behavioural therapy. BJPsych Open. 2016;2:50–58. doi: 10.1192/bjpo.bp.115.002139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bronswijk S.C., Lemmens L., Viechtbauer W., Huibers M.J.H., Arntz A., Peeters F. The impact of personality disorder pathology on the effectiveness of cognitive therapy and interpersonal psychotherapy for major depressive disorder. J. Affect. Disord. 2018;225:530–538. doi: 10.1016/j.jad.2017.08.043. [DOI] [PubMed] [Google Scholar]
- Vernmark K., Lenndin J., Bjarehed J., Carlsson M., Karlsson J., Oberg J., Carlbring P., Eriksson T., Andersson G. Internet administered guided self-help versus individualized e-mail therapy: a randomized trial of two versions of CBT for major depression. Behav. Res. Ther. 2010;48:368–376. doi: 10.1016/j.brat.2010.01.005. [DOI] [PubMed] [Google Scholar]
- Warmerdam L., Van Straten A., Twisk J., Riper H., Cuijpers P. Internet-based treatment for adults with depressive symptoms: randomized controlled trial. J. Med. Internet Res. 2008;10 doi: 10.2196/jmir.1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts S., Newby J.M., Mewton L., Andrews G. A clinical audit of changes in suicide ideas with internet treatment for depression. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-001558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wikberg C., Nejati S., Larsson M.E., Petersson E.L., Westman J., Ariai N., Kivi M., Eriksson M., Eggertsen R., Hange D., Baigi A., Bjorkelund C. Comparison between the Montgomery-Asberg depression rating scale-self and the Beck depression inventory II in primary care. Prim Care Companion CNS Disord. 2015;17 doi: 10.4088/PCC.14m01758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams A.D., Andrews G. The effectiveness of Internet Cognitive Behavioural Therapy (iCBT) for depression in primary care: a quality assurance study. PLoS ONE [Electronic Resource] 2013;8:e57447. doi: 10.1371/journal.pone.0057447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson K.G., Murrell A.R. Guilford; New York: 2004. Values Work in Acceptance and Commitment Therapy. Mindfulness and acceptance: Expanding the cognitive–behavioral tradition; pp. 120–151. [Google Scholar]
- Zetterberg M., Carlbring P., Andersson G., Berg M., Shafran R., Rozental A. Internet-based cognitive behavioral therapy of perfectionism: comparing regular therapist support and support upon request. Internet Interv. 2019;17:100237. doi: 10.1016/j.invent.2019.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]