Abstract
Brachiocephalic vein aneurysm is an extremely rare clinical entity, with a limited number of case reports in the literature. We report the case of a 74-year-old woman with a left brachiocephalic vein aneurysm (3 × 3 × 6.5 cm) that was discovered fortuitously by contrast-enhanced chest computed tomography. Surgical intervention was performed simultaneously during tricuspid valve surgery with coronary artery bypass grafting. This paper discusses the details of our case, the surgical treatment of brachiocephalic vein aneurysms, and the different treatment options.
Keywords: Brachiocephalic vein aneurysm, Thoracic venous aneurysm, Mediastinal mass
Brachiocephalic vein aneurysm is an extremely rare clinical entity. Many patients are diagnosed with this incidentally when they undergo routine chest radiography or computed tomography (CT) examinations performed for other reasons.1,2 This report describes the case of a 74-year-old woman with a left brachiocephalic vein (LBCV) aneurysm (3 × 3 × 6.5 cm) that was discovered fortuitously by contrast-enhanced chest CT. The patient gave informed consent to publish her medical data.
Case report
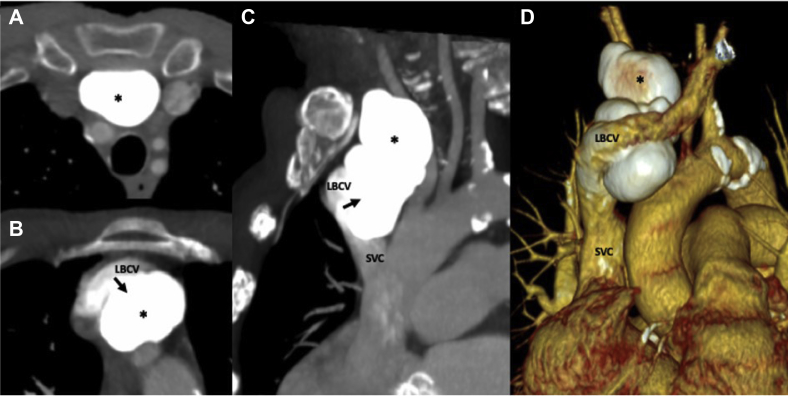
A 74-year-old woman was admitted to the Department of Cardiology for the treatment of cardiac decompensation, manifested with severe bilateral pleural effusions and leg edema. Her medical history included percutaneous closure of an atrial septal defect along with central venous catheterization done 10 years ago and atrial fibrillation treated by rivaroxaban. Transthoracic echocardiography revealed severe isolated tricuspid valve regurgitation secondary to annular dilation with normal left ventricular function and dilated right ventricle yet with normal function. After the administration of diuretics, pleural effusion was not optimized as hypoventilation persisted mostly on the right side. To exclude an underlying lung mass, contrast-enhanced chest CT was performed, and a contrast material-filled mass in the anterior mediastinum communicating with the left LBCV was discovered (Fig 1). This mass was never seen before on other radiologic images. Contrast-enhanced CT of the neck, chest, abdomen, and pelvis revealed no other venous malformation. Because of her tricuspid valve regurgitation along with deteriorating signs of right-sided heart failure, we decided for tricuspid valve repair and resection of the LBCV aneurysm in a single surgical intervention. During the preoperative assessment, two-vessel coronary artery disease was diagnosed with a 90% to 99% stenosis of the middle left anterior descending artery and a 50% stenosis of the left coronary artery.
Fig 1.
A-D, Contrast-enhanced computed tomography (CT) shows a mass filled with contrast material (asterisk) in the anterior mediastinum localized in the thymus lodge and communicating (arrow) with the left brachiocephalic vein (LBCV). SVC, Superior vena cava.
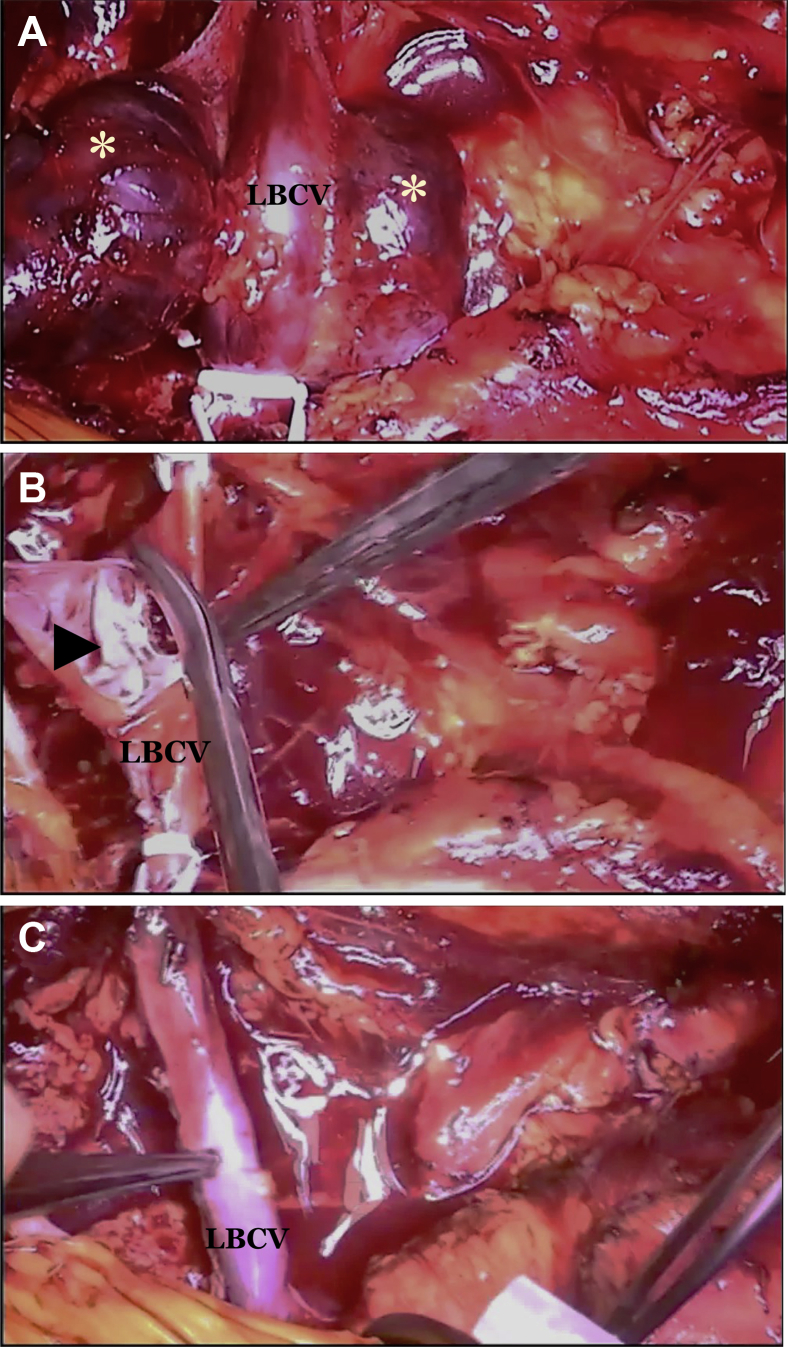
Surgery was performed with femorofemoral cannulation and cardiopulmonary bypass support before a midline sternotomy, which was performed by an oscillating saw. On exploration of the patient's anterior mediastinum, a multilobulated saccular venous aneurysm communicating with the LBCV was found. To dissect the LBCV, proximal and distal controls of the LBCV were made, and the aneurysmal sac was opened and resected. The residual communicating holes were closed with 5-0 polypropylene running suture (Fig 2). Tricuspid valve repair was performed by a rigid ring annuloplasty supported by a central clover stitch. We also resected the percutaneous closure device of the atrial septal defect to repair an atrial septal aneurysm that was discovered during surgery. The operation was completed by external left atrial appendage closure and left internal thoracic artery to left anterior descending coronary artery bypass. After uneventful recovery, the patient was discharged on postoperative day 12 to the rehabilitation department.
Fig 2.
Operative view. A, Vascular control of the left brachiocephalic vein (LBCV) with multilobulated venous aneurysm (asterisk). B, Opening and resection of the aneurysmal sac (arrowhead). C, Final result after running suture of the communicating holes.
Discussion
Isolated LBCV aneurysm is an extremely rare clinical disease. In the literature, fewer than 20 cases are reported.1 Asymptomatic patients with LBVC are incidentally diagnosed during routine chest radiography or chest CT, when a widened mediastinum is observed.2,3 This was the exact scenario with our patient. In some cases, this anomaly can be symptomatic from complications including pulmonary embolus,4 rupture,5 and venous obstruction.6 Other less frequent symptoms are chronic cough, likely to be related to the bronchial irritation and atelectasis caused by the LBCV aneurysm,7 and hoarseness due to left recurrent laryngeal nerve paralysis secondary to compression.8
Venous aneurysms are classified into four groups: congenital, acquired, pseudoaneurysm, and aneurysm secondary to arteriovenous fistula.9 The intraoperative and histopathologic findings of our patient confirmed the pathologic process to be an aneurysm.
The exact cause of mediastinal venous aneurysms is unknown. They can be secondary to congenital malformation or be acquired after trauma, inflammation, degenerative change in the vessel wall, or arteriovenous fistulas. Congenital absence of the longitudinal muscle coat of the adventitia was described in one case.4 Salam et al also recently reported a mycotic aneurysm.10 In our case, the aneurysm might have been secondary to central venous catheterization performed 10 years ago during percutaneous atrial septal defect closure.
The diagnosis of the LBCV aneurysm can be confirmed by contrast-enhanced CT. There were several cases misdiagnosed as thymoma and referred to a surgeon for thymectomy, despite detailed preoperative imaging studies.11,12 When doubt exists about an anterior mediastinal mass, the correct diagnosis can be achieved noninvasively with dynamic contrast-enhanced three-dimensional magnetic resonance angiography or more invasively by venography.13, 14, 15 The initial radiographic diagnosis of our case was a thymus-related contrast-enhancing mass. After careful reanalysis of the images and specific reconstructions showing the link between the brachiocephalic vein and the mass with our radiology and thoracic surgery departments, a diagnosis of LBCV aneurysm was concluded.
Because of the rarity of this condition, there is no consensus on the management of brachiocephalic venous aneurysms. Numerous authors had suggested that asymptomatic nonenlarging venous aneurysms without thrombus may be safely managed conservatively.2,15, 16, 17, 18, 19, 20 For isolated brachiocephalic venous aneurysm, some authors recommended using cardiopulmonary bypass to increase intraoperative security with safe and successful resection6; other reports confirmed an off-pump successful strategy with gentle dissection of the aneurysm and rapid control of the superior vena cava.21 Because of the recent advances in endovascular techniques, minimally invasive, effective percutaneous techniques were described. Some cases in the literature with a specific type of aneurysm called pseudoaneurysm underwent endovascular treatment by uncovered endovascular flexible self-expanding stent placement with trans-stent coil embolization or thrombin injection.22,23 A surgical treatment was chosen for our patient because she mainly needed open heart surgery for symptomatic severe tricuspid regurgitation with coronary artery disease. Without other surgical indication, we would have opted for a less invasive treatment using an endovascular approach.
Conclusions
The superior mediastinal vein aneurysms are rare clinical entities. It is important to keep this rare disease in mind because it may mimic other diseases of the superior mediastinum, such as thymomas. Because of limited case reports and therefore limited unanimity on how to best manage a patient with LBVC, sharing our surgical expertise contributes to better understanding and ease of surgical planning for patients with LBCV aneurysm. Based on modern radiology and endovascular techniques that are less invasive than surgery, we recommend multidisciplinary discussions in an attempt to choose the best management for each patient. However, surgical intervention remains the treatment of choice when chest surgery is required by cases with other surgical indications in the chest.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Lohrenz C., Rückner D., Wintzer O., Gross-Fengels W., Meierling S. Large left innominate vein aneurysm presenting as an anterior mediastinal tumour in a young female. Vasa. 2018;47:515–517. doi: 10.1024/0301-1526/a000733. [DOI] [PubMed] [Google Scholar]
- 2.Burkill G.J., Burn P.R., Padley S.P. Aneurysm of the left brachiocephalic vein: an unusual cause of mediastinal widening. Br J Radiol. 1997;70:837–839. doi: 10.1259/bjr.70.836.9486050. [DOI] [PubMed] [Google Scholar]
- 3.Schellhammer F., Wobker G., Turowski B. Asymptomatic aneurysm of the subclavian vein. Acta Radiol. 2005;46:366–367. doi: 10.1080/02841850510021175. [DOI] [PubMed] [Google Scholar]
- 4.Ream C.R., Giardina A. Congenital superior vena cava aneurysm with complications caused by infectious mononucleosis. Chest. 1972;62:755–757. doi: 10.1378/chest.62.6.755. [DOI] [PubMed] [Google Scholar]
- 5.Taira A., Akita H. Ruptured venous aneurysm of the persistent left superior vena cava. Angiology. 1981;32:656–659. doi: 10.1177/000331978103200912. [DOI] [PubMed] [Google Scholar]
- 6.Pasic M., Schöpke W., Vogt P., von Segesser L., Schneider J., Turina M. Aneurysm of the superior mediastinal veins. J Vasc Surg. 1995;21:505–509. doi: 10.1016/s0741-5214(95)70294-6. [DOI] [PubMed] [Google Scholar]
- 7.Hosein R.B., Butler K., Miller P., Jones T., Brawn W.J., Barron D.J. Innominate venous aneurysm presenting as a rapidly expanding mediastinal mass. Ann Thorac Surg. 2007;84:640–642. doi: 10.1016/j.athoracsur.2007.03.044. [DOI] [PubMed] [Google Scholar]
- 8.Hosaka A., Kato M., Kato I., Isshiki S., Okubo N. Brachiocephalic venous aneurysm with unusual clinical observations. J Vasc Surg. 2011;54(Suppl):77S–79S. doi: 10.1016/j.jvs.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 9.Abbott O.A., Leigh T.F. Aneurysmal dilatations of the superior vena caval system. Ann Surg. 1964;159:858–872. doi: 10.1097/00000658-196406000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salam A., Khan I., Sonawalla A., Fatimi S. Rare mycotic aneurysms of internal jugular vein and innominate vein secondary to untreated parapharyngeal abscess: a case report. Ann Med Surg (Lond) 2017;19:62–64. doi: 10.1016/j.amsu.2017.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang W., Jiang G.N. A rare case of left innominate vein aneurysm mimicking thymoma. Interact Cardiovasc Thorac Surg. 2017;25:669–670. doi: 10.1093/icvts/ivw420. [DOI] [PubMed] [Google Scholar]
- 12.Buehler M.A., 2nd, Ebrahim F.S., Popa T.O. Left innominate vein aneurysm: diagnostic imaging and pitfalls. Int J Angiol. 2013;22:127–130. doi: 10.1055/s-0033-1336606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guney B., Demirpolat G., Savas R., Alper H. An unusual cause of mediastinal widening: bilateral innominate vein aneurysms. Acta Radiol. 2004;45:266–268. doi: 10.1080/02841850410004256. [DOI] [PubMed] [Google Scholar]
- 14.Gozdziuk K., Czekajska-Chehab E., Wrona A., Tomaszewski A., Drop A. Saccular aneurysm of the superior vena cava detected by computed tomography and successfully treated with surgery. Ann Thorac Surg. 2004;78:e94–e95. doi: 10.1016/j.athoracsur.2004.03.103. [DOI] [PubMed] [Google Scholar]
- 15.Tsuji A., Katada Y., Tanimoto M., Fujita I. Congenital giant aneurysm of the left innominate vein: is surgical treatment required? Pediatr Cardiol. 2004;25:421–423. doi: 10.1007/s00246-003-0499-y. [DOI] [PubMed] [Google Scholar]
- 16.Calligaro K.D., Ahmad S., Dandora R., Dougherty M.J., Savarese R.P., Doerr K.J. Venous aneurysms: surgical indications and review of the literature. Surgery. 1995;117:1–6. doi: 10.1016/s0039-6060(05)80222-3. [DOI] [PubMed] [Google Scholar]
- 17.Mikroulis D., Vretzakis G., Eleftheriadis S., Lazarides M. Long-term antiplatelet treatment for innominate vein aneurysm. Vasa. 2010;39:262–264. doi: 10.1024/0301-1526/a000039. [DOI] [PubMed] [Google Scholar]
- 18.Bansal K., Deshmukh H., Popat B., Rathod K. Isolated left brachiocephalic vein aneurysm presenting as a symptomatic mediastinal mass. J Med Imaging Radiat Oncol. 2010;54:462–464. doi: 10.1111/j.1754-9485.2010.02197.x. [DOI] [PubMed] [Google Scholar]
- 19.Dua S.G., Kulkarni A.V., Purandare N.C., Kulkarni S. Isolated left innominate vein aneurysm: a rare cause of mediastinal widening. J Postgrad Med. 2011;57:40–41. doi: 10.4103/0022-3859.74286. [DOI] [PubMed] [Google Scholar]
- 20.Varma P.K., Dharan B.S., Ramachandran P., Neelakandhan K.S. Superior vena caval aneurysm. Interact Cardiovasc Thorac Surg. 2003;2:331–333. doi: 10.1016/S1569-9293(03)00076-8. [DOI] [PubMed] [Google Scholar]
- 21.Galvaing G., Gaudin M., Medous M.T., Filaire M. Left brachiocephalic venous aneurysm: a rare clinical finding. Ann Vasc Surg. 2018;48:253.e5–253.e6. doi: 10.1016/j.avsg.2017.10.027. [DOI] [PubMed] [Google Scholar]
- 22.Choi S.J., Do Y.W., Oh T.H., Lee H., Cheon H., Lim J.K. Central venous catheterization-induced right brachiocephalic vein pseudoaneurysm: successfully treated with stent-assisted coiling. J Vasc Access. 2018;19:319–323. doi: 10.1177/1129729817746581. [DOI] [PubMed] [Google Scholar]
- 23.Elsaadany A.M., Alaeddin F.H., Alsuhaibani H.A. A rare case of iatrogenic pseudoaneurysm of the left brachiocephalic vein after central venous catheterization treated with thrombin injection. Cardiovasc Intervent Radiol. 2014;37:1083–1086. doi: 10.1007/s00270-013-0729-5. [DOI] [PubMed] [Google Scholar]