Summary
Alcohol-related liver disease (ALD) represents a major public health problem worldwide. According to the World Health Organization, the highest levels of per capita alcohol consumption are observed in countries of the European Region. Alcohol consumption is also alarmingly increasing in developing countries. ALD is one of the main contributors to the burden of alcohol-attributable deaths and disability. In the United States, severe forms of ALD such alcoholic hepatitis have increased in the last decade and in the United Kingdom, three-quarters of liver-related mortality results from alcohol consumption. Besides genetic factors, there is strong evidence that the amount of alcohol consumed plays a major role in the development of advanced ALD. Establishing effective public health policies is therefore mandatory to reduce the burden of ALD. Since the 90s, major public health institutions and governments have developed a variety of policies in order to reduce the harm caused by excessive drinking. These policies encompass multiple factors, from pricing and taxation to advertising regulation. Measures focused on taxation and price regulation have been shown to be the most effective at reducing alcohol-related mortality. However, there are few studies focused on the effect of public policies on ALD. This review article summarises the factors influencing ALD burden and the role of different public health policies.
Keywords: Metabolic liver disease, Public Health, Epidemiology, Youth-focused policies, Alcoholic drinks market
Key points
Alcohol-related liver disease (ALD) is a major public health problem worldwide and the main cause of cirrhosis globally.
The main factor influencing the burden of advanced ALD (i.e. cirrhosis), at the population level, is the percentage of the population who drink heavily.
Major public health institutions have been working to develop an array of public health policies aimed at reducing excessive and harmful alcohol use and thereby its detrimental effects on health.
Taxation and price regulation are the most effective measures to reduce alcohol-related mortality, although the effect varies across different countries.
The interaction between pricing policies, other policy types and local factors are critical for reducing alcohol intake and the resulting ALD.
Alt-text: Unlabelled Box
Excessive alcohol consumption as a cause of preventable disability and disease worldwide
Alcohol represents a major health problem at a global scale. There are 2 main organisations that provide comprehensive data on alcohol consumption and the burden of disease: the World Health Organization (WHO)[1], [2], [3] and the Institute for Health and Metrics Evaluation (that leads the Global Burden of Disease Study [GBD]). These organisations use different methodology to assess the burden of alcohol-related liver disease (ALD). Throughout the manuscript we mainly use data from the WHO, nevertheless on certain occasions we highlight data generated by the GBD.4,5
Excessive alcohol use is a leading risk factor for preventable disability and death. Globally, 7.7% of deaths in men are attributable to alcohol and alcohol abuse is the main cause of death among men aged 25–45 years old.3 A total of 3.3 million deaths annually are associated with alcohol use.1,2 In the United Kingdom, standardised mortality rates for liver disease have increased 4-fold since 1970. Three-quarters of those deaths are the result of excess alcohol consumption.6 Besides mortality, alcohol is also a major cause of morbidity and disability. For the population aged 15-49 years, alcohol accounts for 10% of disability-adjusted live years (DALYs) in men. ALD is one of the most well-known detrimental consequences of alcohol abuse and is the main cause of DALYs in European adults.7 In fact, ALD is the main cause of cirrhosis globally and is responsible for 60% of cirrhosis in Europe and North America.8 In the US, the total number of deaths attributable to alcoholic cirrhosis increased 79% from 1990 to 2016.9 Moreover, the economic burden of alcohol-related hospitalisation exceeds all the other causes of liver disease combined.10 Despite this huge health and economic burden, ALD has received scarce attention compared to other types of liver disease.11
Although the amount of alcohol intake influences its deleterious consequences, a precise threshold that is associated with increased morbidity and mortality is unclear. A recent study has shown that even low doses of alcohol intake, historically considered as protective, increase all-cause mortality.4 Alcohol consumption varies widely across the world and is deeply affected by many local factors at a population level, such as culture, religion12,13 and even climate.14 Individual factors also have a deep impact on alcohol consumption, including the co-existence of a mental illness,15,16 history of post-traumatic stress disorder, socioeconomic status17 and genetic factors.18,19 All these factors influence the development and burden of alcohol use disorder (AUD). Identifying factors that influence harmful alcohol consumption at the individual and population level is the first step for designing effective public health policies.20
Factors influencing the burden of alcohol-related liver disease
The main factor influencing the burden of advanced ALD (i.e. cirrhosis) at the population level is the percentage of the population who drink heavily.8 On a global scale, during a period of 27 years (1990 to 2017), annual adult per capita consumption increased by 0.6 litres and is forecast to reach an alarming 7.6 litres by 2030.5
While in some European countries the consumption of alcohol has decreased (i.e. Italy), there has been an alarming increase of heavy drinking in developing countries and in some Western countries. In the US, in the last 15 years, there has been an 11.2% increase in alcohol use, a 30% increase in high-risk drinking and a 59% increase in AUD.21 This tendency is more marked among women, older adults, racial/ethnic minorities and individuals with lower educational level and family income. Another pattern that seems to be increasing, particularly among middle-age and older adults, is binge drinking.22,23 This tendency was recently confirmed on a global level, with reports of an increase of 1.5% from 1990 to 2017 that it is forecast to peak at 23% in 2030.5 Heavy daily alcohol intake at the population level predicts the influence of alcohol on cirrhosis burden worldwide.8 This data has been confirmed by other studies, showing that excessive alcohol use is the strongest risk factor associated with ALD (odds ratio = 6.17).24
Besides the amount of alcohol, the early onset of this unhealthy behaviour can also influence the development of ALD. In fact, a recent study found that alcohol consumption in young men is associated with an increased risk of severe liver disease later in life.25 Importantly, the risk was found to be dose-dependent, with no clear threshold effect. This data implies that educational and regulatory measures aimed at decreasing the burden of ALD should target the young population. It is likely that the early onset of AUD leads to a longer duration of excessive alcohol intake and consequently to severe ALD. Another factor that predisposes individuals to ALD is gender. A recent study found that females that develop ALD had significantly lower alcohol consumption than men, despite a similar duration in years of alcohol intake, supporting the hypothesis that women have increased susceptibility to ALD.26 In conclusion, there is strong evidence that the number and percentage of heavy drinkers play a major role in both the development and the severity of ALD. Public policies should therefore focus on preventing excessive alcohol drinking.
The role of the pattern of alcohol intake on the development of alcohol-related cirrhosis is uncertain. Recent epidemiological studies suggest that binge drinking is particularly deleterious in obese people, who could be predisposed to developing severe forms of liver disease.27 These factors are important in the design of effective policies to reduce the burden of alcohol abuse and its deleterious effects on the liver. Other factors known to have an impact on alcohol intake at the population and individual level include: religious beliefs,28,29 socioeconomic inequality,17 genetic factors,18,30,31 climate factors,14 concomitant addictions and mental diseases including post-traumatic stress disorder.32,33 These factors should be taken into account to better measure the risk of ALD in a given country and to design more effective therapies by targeting at-risk populations. The fact that the development of alcohol policies can influence alcohol consumption at the population level should encourage policy makers to play a more active role in countries with a high prevalence of ALD.34
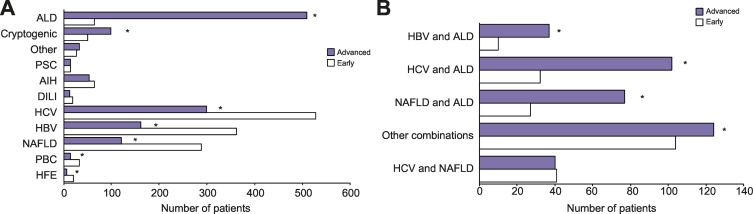
One of the challenges of reducing the burden of severe ALD is the lack of early detection of silent liver disease among heavy drinkers. A recent global study, including countries from 5 continents, showed that ALD is the liver disease in which by far the most patients are seen at advanced stages35 (Fig. 1). Therefore, campaigns for early detection of liver fibrosis using non-invasive tests among at-risk populations (i.e. heavy drinkers and patients diagnosed with AUD) are urgently needed at a global level. It is important to manage these patients with a multidisciplinary team including alcohol addiction specialists. Brief motivational interventions should be used in all patients with ALD and active drinking. The main goal of these interventions is to educate the patient about the impact of alcohol and to stimulate their desire to discontinue alcohol intake. Although these interventions alone are not sufficient to impact alcohol dependence in heavy drinkers, they might reinforce medication compliance. Pharmacological treatment can be useful to prevent relapse in patients with AUD. However, few studies have assessed the efficacy and safety of anticraving drugs in patients with ALD. In particular, naltrexone and acamprosate, both FDA-approved drugs for AUD, have not specifically been tested in patients with ALD. Moreover, other commonly used drugs such as disulfiram can cause severe hepatotoxicity and are contraindicated in patients with advanced ALD. Baclofen, a GABA receptor agonist, is the only anticraving drug tested in a controlled trial in patients with severe ALD, wherein it was shown to be a useful and safe option for preventing relapse.36
Fig. 1.
Lack of early detection of alcohol-related liver disease worldwide. Consecutive patients with a single (A) and double aetiology (B) of liver disease seen in Gatroenterology/Liver centres from 19 patients in the 5 continents were included. Percentage of patients seen at advanced vs early stages of liver disease are shown depending on the etiology of the liver disease. *p ≪0.05. (Adapted from Shah et al. with permission)
AIH, autoimmune hepatitis; ALD, alcohol-related liver disease; DILI, drug-induced liver injury; HBV, hepatitis B virus; HCV, hepatitis C virus; HFE, hemochromatosis; NAFLD, non-alcoholic fatty liver disease; PBC, primary biliary cholangitis; PSC, primary sclerosing cholangitis.
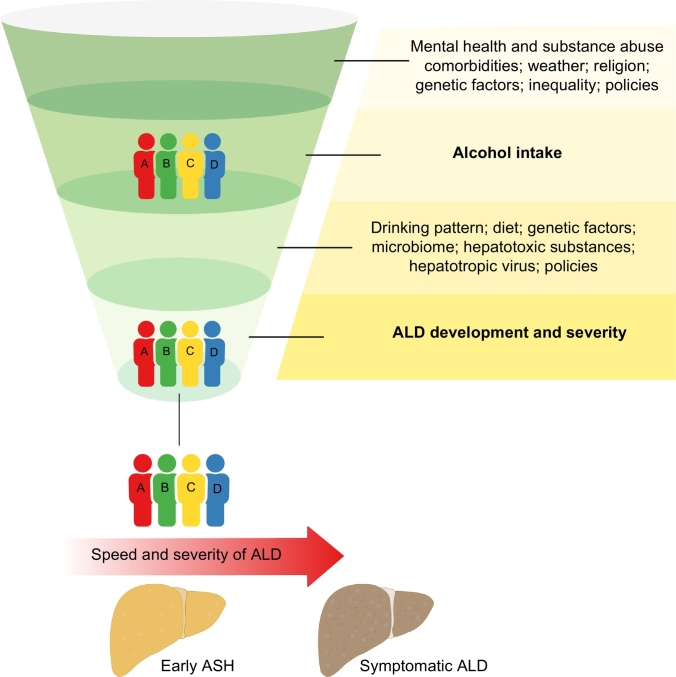
Factors that influence the development of severe forms of ALD among heavy drinkers are now well known. The role of the pattern of drinking (e.g. binge drinking) is uncertain,37 while genetic factors such as PNPLA3 variations influence the progression to cirrhosis.18 Importantly, many patients that drink alcohol have other factors that synergise to cause advanced liver disease. Such factors include prevalent conditions such as viral hepatitis38,39 and obesity40 (Fig. 2). Alcohol consumption is also associated with accelerated fibrosis progression in patients with other types of liver diseases.41 Therefore, campaigns aimed at reducing alcohol consumption should be particularly directed to patients with other synergistic factors such as viral hepatitis or metabolic syndrome.
Fig. 2.
Factors known to influence excessive alcohol intake and alcohol-related liver disease.
The combined effect of different factors (e.g. social, environmental and genetic) influence the amount of alcohol intake at the population and individual levels. Susceptibility to develop ALD is in turn influenced by genetic and environmental factors.
ALD, alcohol-related liver disease.
Type of public policies to reduce alcohol intake according to the World Health Organization
Since the 90s, the WHO and other major public health institutions have been working to develop an array of public health policies aimed at reducing excessive and harmful alcohol use. In 1996, the WHO launched the Global Alcohol Database, the world's largest single source of information on alcohol that resulted in the release of the first Global Status Report on Alcohol.42 The latest version of this comprehensive report, which includes data from every single country, was released in 2018.1 The WHO categorises the existing policies into 8 categories (Box 1). In this review, we focus on policies whose efficacy has been assessed by scientific studies (i.e. pricing policies, restriction to alcohol access policies, drinking age and youth-focused polices and advertising and promotion policies).
Box 1. Classification of alcohol policies according to the Global Status Report on Alcohol and Health 2018 from the World Health Organization.
National plan to fight harmful consequences of alcohol (n = 3)
Written national policy (adopted/revised)
National action plan
Definition of an alcoholic beverage
National license and production and selling control (n = 5)
National control of production any monopoly
National control of sale any monopoly
National control of production any licensing
National control of sale any licensing
Total ban
Taxes control, pricing policies (n = 3)
Excise tax on beer
Excise tax on wine
Excise tax on spirits
Drinking age and youth focus polices (n = 6)
National legal minimum age for off-premise sales of alcoholic beverages beer
National legal minimum age for off-premise sales of alcoholic beverages wine
National legal minimum age for off-premise sales of alcoholic beverages spirits
National legal minimum age for on premise sales of alcoholic beverages beer
National legal minimum age for on premise sales of alcoholic beverages wine
National legal minimum age for on premise sales of alcoholic beverages spirits
Restrictions to alcohol access (n = 7)
Restrictions for on-/off-premise sales of alcoholic beverages: hours
Restrictions for on-/off-premise sales of alcoholic beverages: days
Restrictions for on-/off-premise sales of alcoholic beverages: places
Restrictions for on-/off-premise sales of alcoholic beverages: density
Restrictions for on-/off-premise sales of alcoholic beverages: specific events
Restrictions for on-/off-premise sales of alcoholic beverages: intoxicated persons
Restrictions for on-/off-premise sales of alcoholic beverages: petrol stations
Driving-related alcohol policies (n = 5)
National maximum legal blood alcohol concentration when driving a vehicle general
National maximum legal blood alcohol concentration when driving a vehicle young
National maximum legal blood alcohol concentration when driving a vehicle professional
Sobriety check-points
Random breath testing
Control over advertising and promotion (n = 9)
Legally binding regulations on alcohol advertising
Legally binding regulations on product placement
Legally binding regulations on alcohol sponsorship
Legally binding regulations on sales promotion
Legally required health warning labels on alcohol advertisements
Legally required health warning labels on containers
Alcohol content displayed on containers
Number of standard alcoholic drinks displayed on containers
Any duty paid, excise or tax stamps or labels
Government monitoring systems (n = 4)
National government support for community action
National monitoring system(s)
Monitoring health consequences
Monitoring of social consequences
Alt-text: Box 1
Public health policies: Impact on the burden of alcohol-related liver disease
There are a limited number of well-designed studies assessing the efficacy of public health policies on the burden of ALD. Most studies show an impact of alcohol policies on alcohol-attributable outcomes, mediated by the decrease of alcohol consumption.34 In this section, we review studies assessing the impact of different policies on alcohol consumption and related ALD. The development of ALD requires excessive alcohol intake, so it is conceivable that policies that reduce the rate of hazardous drinking will positively influence the burden of ALD.
Pricing policies
Increasing alcoholic beverage taxes and minimum unit pricing (MUP) are the major pricing policies. Both have proven to have an impact on ALD burden. In the US, the adjusted tax rates have declined over the last decades, in parallel with increased alcohol consumption.43,44 Studies performed across the last decades in different countries showed similar results.45 Thus, a decrease in taxation leads to a dramatic increase in liver cirrhosis mortality,[45], [46], [47] while tax increases reduce cirrhosis mortality rates in the long-term.48,49
The effects of tax increases are not homogenous across all segments of the population and similar pricing policies have a different impact depending of the country.50 Tax increases have a major impact on the middle-aged population (men aged 55–59 and women aged 50–54) and those of low socioeconomic status.46 It is important to highlight that among the adolescent population, the effect of tax increases on ALD, especially beer taxes, has been questioned, as several studies have found an association between tax cuts and a reduction in suicide rates but not with ALD.[51], [52], [53], [54] Nevertheless, other studies did not support this finding55 or found only a marginal association.47 The scarce years of alcohol exposure among the teenage population might be a possible explanation for the lack of association between tax policies and ALD in this segment of the population. Importantly, an association between consumption in late adolescence and an increased risk of severe liver disease later in life has recently been described.25 Further studies should explore whether other measures in combination with tax increases are effective in reducing alcohol consumption and therefore ALD among young people.
The other major pricing policy is MUP. In different societies such as England, Scotland and Ireland, patients with alcohol-related cirrhosis consume mainly cheap alcohol.[56], [57], [58] Different studies and model-based reports, mainly within the UK population, have shown a clear impact of increasing the MUP on ALD reduction.59 A recent report from the Welsh government compared the effects of tax cuts and MUP across different populations.59 They concluded that both MUP and tax cuts will reduce alcohol-attributable mortality and hospital admissions, especially among the most deprived and harmful drinkers. Other studies yield similar results, showing that the major impact of MUP is on heavy drinkers.57,58,60 These modelling studies suggest that alcohol-attributable health inequalities would fall by a greater amount under MUP than tax changes.59 MUP has already been implemented in several countries including Russia, Canada, Kyrgyzstan, Republic of Moldova, Ukraine, Belarus and more recently in the Northern Territory of Australia and in Scotland. One of the first countries to implement MUP was Canada, where they showed that a 1% increase in MUP decreased all causes of alcohol-attributable hospitalisations (1.64% for acute admissions and by 2.24% for chronic admissions).49 Interestingly, another Canadian study observed an immediate impact of price changes on acute alcohol-attributable admissions, while a reduction in chronic alcohol-attributable admissions, including those for liver cirrhosis, was observed after 2 years.61 A recent systematic review summarised the results of 26 studies on alcohol consumption and alcohol-related harm. Remarkably, most of the studies focused on alcohol consumption and not on alcohol-related morbidity and mortality. Nevertheless, they concluded that MUP is likely to reduce alcohol consumption, alcohol-related morbidity and mortality.62 It is important to highlight that none of these studies have investigated specific causes of alcohol-attributable mortality including ALD.
Drinking age and youth-focused policies
The WHO defines adolescents as individuals between 10-19 years old and young people as individuals between 10–24 years old. According to the last global status report on alcohol and health, more than a quarter (27%) of all 15–19-year-olds are current drinkers; this percentage is higher among adolescents from the European region (44%). Moreover, school surveys indicate that in many countries alcohol use starts early in life, before the age of 15 years. The prevalence of heavy episodic drinking increases from ages 15–19 to 20–24, and peaks in all WHO regions in the 20–24 age group.1 Besides promoting violence and accidents, alcohol consumption early in life has been shown to predict the development of cirrhosis in adults, so reducing early consumption could theoretically decrease the prevalence of cirrhosis.25
That heavy drinking early in life causes liver injury is now well known. Alcohol intoxication increases aspartate aminotransferase (AST), alanine aminotransferase (ALT) and AST/ALT ratio among children and adolescents, reflecting hepatocyte damage.63 Some studies suggest there has been a steady increase in the prevalence of ALD in adolescents and young adults in the last decades, of 2% (1988–1994), 4% (1999–2004) and 5% (2007-2012) (15 to 39 years old).64 Another study focusing on alcohol-attributable admissions showed higher rates of acute admissions in adolescents/young adults and middle-aged groups. Chronic conditions wholly attributable to alcohol were concentrated in middle-aged groups (particularly males).65 These data suggest that the problem of early drinking has not improved over the last decades and that urgent public health policies are needed. Unfortunately, educational campaigns have not proven to be effective and, in some cases, they result in negative results.66
Multiple studies have evaluated the impact of minimum age laws on alcohol intake, alcohol drinking patterns and cause of mortality (e.g. road accidents and suicides).[67], [68], [69] All those studies showed a decrease in drinking-related problems when lowering the legal drinking age. Control over alcohol advertising and promotion may play a major role on young people’s drinking behaviour. A recent review showed that the exposure to marketing through digital media influenced drinking behaviour.70 There are multiple concerns that alcohol industry marketing strategies are biased and provide misleading messages to adolescents.71
The impact of youth-focused policies on the prevalence of ALD is unknown and deserves investigation. One study evaluated the impact of drinking age laws on all-cause mortality.72 In this study, they did not find a short-term effect of drinking age laws on gastrointestinal mortality cases. To our knowledge, no studies have evaluated the impact of alcohol policies exclusively on ALD among adolescents. Finally, it is interesting to highlight that there is an epidemic of childhood obesity in the Western world that is leading to the appearance of non-alcoholic fatty liver disease (NAFLD) within this population. Because of the known synergic effects of alcohol drinking and obesity on the development of advanced liver disease,73 health policies should be particularly directed towards promoting healthy lifestyles among children and avoiding the occurrence of multiple causes of liver disease.
Restrictions to alcohol access
Another group of polices are focused on restricting physical access to alcohol, usually by legislating on the hours and days of sale and the density of alcohol outlets. The vast majorities of studies that evaluate the effects of restriction policies are focused on alcohol consumption and alcohol-related harm, including violent crimes and accidents due to driving under the influence of alcohol.[74], [75], [76], [77] There are few studies assessing the role of such measures on the burden of ALD.
Some studies have evaluated the impact of lifting versus reinforcing restriction policies on alcohol-attributable mortality rates, including mortality related to liver cancer and alcohol-related cirrhosis. A 10% increase in private liquor stores was associated with a 2.4%, 2.7% and 3% increase in acute, chronic and total alcohol-attributable mortality rates, respectively, in Canada.78 Two studies from the early 90s performed in Australia showed that a 16% increase in the number of hotels, taverns and store licences/100,000 habitants led to an increase of liver cirrhosis mortality by 24% in males and by 29% in females.79 In a similar manner, a 10% relative increase in the total outlet rate was also associated with a significant increase in liver cirrhosis mortality in both males (22%) and females (18%).80 A more recent study analysed the impact of neighbourhood alcohol outlets on premature mortality among Canadian adults, adjusted by deprivation and crime. When comparing the highest quintiles of alcohol outlet density to the lowest quintiles, the adjusted relative risk of premature mortality was 1.36 for males and 1.11 for females.81 These studies suggest that favouring alcohol availability could negatively impact ALD burden.
It is important to highlight that assessing the role of restricting policies is challenging and has important limitations. These limitations include differences between outlet categories, lack of global studies, difficulties extrapolating the results between different countries or between different areas of the same country, interactions between different restricting policies, and most importantly, the lack of analysis focused on longer-term harms, such as ALD,82 and the complexity of study designs.83 For these reasons, there is a current project in the UK that aims to investigate the association between alcohol outlet density and hospital admissions for alcohol-related conditions in a small area.84
There are additional factors that make restricting policies challenging, including “drinking off premises”. Drinking off premises is not a new phenomenon and several explanations have been proposed for the rising trend, including attempts to avoid paying for high-priced drinks within premises. This phenomenon has been associated with increased binge drinking.85 It is particularly prevalent in underage populations in countries such as Spain86 and in males between 25 and 44 years old in African countries such as Nigeria.28 The health effects of drinking off premises on ALD have not been assessed. Some authors have pointed out that it is extremely important to consider the consequences that policies focused upon reducing drinking in licensed premises may have on displacing drinking to pre-drinking environments and possibly resulting in greater harms.85
Control over alcohol advertising and promotion
Regulating advertising and promotion of alcohol beverages is a very controversial topic. According to different sources, the total alcoholic drinks market was worth $979 billion in 2007,87 and it is expected to reach $1,629 billion by 2024.88 Interestingly, some years ago, some of the most important distilled spirits and beer marketers came together and founded the International Center for Alcohol Policies (ICAP). This centre has been influencing public health policies in some countries and has focused on advertising the possible positive effects of alcohol. The alcohol industry has sponsored alcohol research through different mechanisms, by making donations to grant-making organisations, providing direct funding to academic researchers through public relations organisations and offering ongoing support for research centres.89 A recent meta-analysis assessing the role of the alcohol industry in science concluded that there are serious concerns in at least 3 areas: on evidence-informed policy making, on the processes of undertaking research and on the content of the scientific evidence base itself.90 One of the most striking examples is a $100 million, 9-nation clinical trial, which was mostly funded by major producers to evaluate the health benefits of a single dose of alcohol given daily to individuals at risk of coronary heart disease. This study was terminated early by government agencies in the US.91 The question of whether the scientific community should or should not partner with the alcohol industry is still under debate.92,93
Most of the existing studies are focused on alcohol intake, especially within underage populations. The role of regulating alcohol advertising on ALD burden is not well known. A study from 1991 showed a trend between banning alcohol advertising and a decrease in cirrhosis mortality rate.94 Thus, countries that banned all alcohol advertising had a decreased liver cirrhosis mortality rate. Only 2 out of 7 countries that banned only spirits presented a decrease in liver cirrhosis mortality and only 1 out of 6 countries with no bans at all showed a decrease in mortality. These encouraging results should be replicated on a larger scale. It has been proposed that more aggressive negative advertising on product labels, similar to tobacco, might have a deeper impact on alcohol consumption and alcohol-related harms.95 The latest EASL guidelines on ALD recommend a ban on alcohol advertising and marketing.96 This measure is especially important among young people, since they have been shown to be particularly susceptible.97
A hot topic is the need to regulate alcohol advertising on the internet and social media. Online marketing has become the largest marketing platform in most countries, overtaking television and radio. The word “alcohol” yields 1,320 million results in the search engine Google. The most used social media platforms include Facebook, Youtube, Twitter, Instagram and Snapchat, all founded between 2004 and 2012. These platforms have 2 characteristics that make age-based controls and content regulation very challenging, a) each platform has a different age accessibility policy and b) all these platforms contain both marketer-generated brand content and self-generated content. Although the alcohol industry has its own self-regulation codes, a recent study detected that alcohol brands have alarmingly inadequate age-gates to social media accounts.98 The type and role of different advertising regulations on social media and the internet are not well defined. The first studies investigating the influence of all media advertising on alcohol consumption (including television, radio billboards, internet and social media) did not find robust evidence for or against the implementation of alcohol advertising restrictions.99 Further studies focused on social media and young populations found that alcohol-related social media engagement was correlated with both greater self-reported drinking and alcohol-related problems.100 This is of extreme importance as young populations are more exposed to alcohol advertising content on social media than adults.101 The positive use of social media represents an opportunity to target young people. In fact, a recent study showed that young adults exposed to certain types of alcohol-warning advertising reduce alcohol consumption.102,103 Finally, the internet and social medial have been used to engage young people or target populations, like pregnant women, who otherwise would not seek specialised care for their alcohol problems.104 Further studies should evaluate the efficacy of both regulatory and educational campaigns on social media.
Interactions between different policies
The combined effect of different types of policy measures on the prevalence of heavy alcohol drinking and ALD burden is not well known. There are no well-designed studies assessing the synergistic impact of alcohol policies on ALD. One of the main explanations for this is the variety of different types and number of policies within different countries, and even within different parts of the same country. One option to overcome this issue is the use of scales (i.e. the Alcohol Policy Scale [APS] that contains the efficacy and degree of implementation of different policies). Another factor that limits the accuracy of studies assessing the impact of alcohol policies is that unmarketed/homemade alcohol comsumption is not well recorded. In a recent study, higher APS scores were associated with lower alcohol-related mortality rates among females. Interestingly, they also found a higher impact of the APS on mortality rates among American Indian/Alaskan Native populations.105
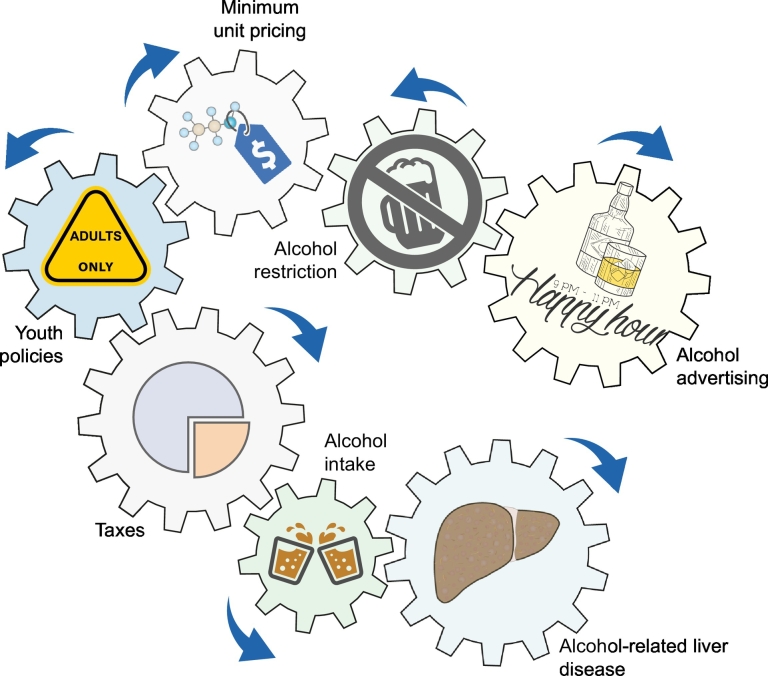
Finally, there are interactions between different policies and local social factors that may lead to the inactivation of the effect of a specific policy.78 For example, increasing the MUP of alcohol is associated with immediate and delayed decreases in alcohol-attributable mortality, while the increased density of private liquor stores is associated with increased alcohol-attributable mortality.78,106 Another clear example was provided by a study suggesting that the most effective measure in countries with high alcohol-related mortality is the combination of different policies, including alcohol market centralisation, reduction of the number of producers and increases in alcohol taxes and prices.107 The potential interaction between different alcohol policies is illustrated in Fig. 3.
Fig. 3.
Interactions between different policies, alcohol intake and alcoholic liver disease.
Graphic representation of the combined effect and interactions between different types of public health policies. The represented polices will impact on alcohol consumption and subsequently can reduce the burden of ALD.
ALD, alcohol-related liver disease. The images are licensed by Creative Commons.
Conclusions
ALD is the main cause of liver-related mortality worldwide. Most patients are seen at advanced stages, so early detection programmes using non-invasive tests are encouraged. Besides treating individual patients, effective public health measures are needed to reduce the burden of ALD. Taxation and price regulation have been shown to be the most effective policies to reduce alcohol-related mortality. The effect of these policies varies across different countries, and the interaction between policies is critical in reducing heavy alcohol intake at the population level. Systematic reviews on the impact of different policies on alcohol consumption and the burden of ALD in this particular field, as well as independent and multidisciplinary studies conducted by epidemiologists and hepatologists, are urgently needed to influence policy makers. Local regulations based on the analysis of the main patterns of alcohol intake and type of alcohol preferred, as well as socioeconomic and cultural factors, are recommended. Understanding other factors that influence alcohol intake is critical to the development of effective policies. The ultimate goal is to design a package of policies that target the specific characteristics of each country or region in order to have the highest impact on both alcohol intake and ALD burden.
Abbreviations
AIH, autoimmune hepatitis; ALD, alcohol-related liver disease; ALT, alanine aminotransferase; APS, alcohol policy scale; AST, aspartate aminotransferase; AUD, alcohol use disorder; DALYs, disability-adjusted live years; DILI, drug-induced liver injury; HFE, hemochromatosis; MUP, minimum unit pricing; NAFLD, non-alcoholic fatty liver disease; PBC, primary biliary cholangitis; PSC, primary sclerosing cholangitis.
Financial support
This study was funded by grants from the National Institute of Alcohol Abuse and Alcoholism (U01AA021908 and U01AA020821).
Conflict of interest
Ramon Bataller received speaking fees from Echosens™. No disclosures from any other co-author.
Please refer to the accompanying ICMJE disclosure forms for further details.
Authors’ contributions
MBP; SR; MVC and RB has contributed to the bibliographic, data search as well as the writing of the paper.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jhepr.2019.07.009.
Supplementary data
Supplementary material
References
- 1.Global status report on alcohol and health 2018. World Health Organitzatione; 2018. [Google Scholar]
- 2.World Health Organisation . 2008. Noncommunicable disease fact sheet. [Google Scholar]
- 3.World Health Organisation Management of substance abuse. 2012. https://www.who.int/substance_abuse/facts/alcohol/en/
- 4.Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016Lancet. 2018;392:1015–1035. doi: 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manthey J, Shield KD, Rylett M, Hasan OSM, Probst C, Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet (London, England) 2019;393:2493–2502. doi: 10.1016/S0140-6736(18)32744-2. [DOI] [PubMed] [Google Scholar]
- 6.Williams R, Aspinall R, Bellis M, Camps-Walsh G, Cramp M, Dhawan A. Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatitis. Lancet (London, England) 2014;384:1953–1997. doi: 10.1016/S0140-6736(14)61838-9. [DOI] [PubMed] [Google Scholar]
- 7.Cortez-Pinto H, Gouveia M, dos Santos Pinheiro L, Costa J, Borges M, Vaz Carneiro A. The burden of disease and the cost of illness attributable to alcohol drinking--results of a national study. Alcohol Clin Exp Res. 2010;34:1442–1449. doi: 10.1111/j.1530-0277.2010.01229.x. [DOI] [PubMed] [Google Scholar]
- 8.Stein E, Cruz-Lemini M, Altamirano J, Ndugga N, Couper D, Abraldes JG. Heavy daily alcohol intake at the population level predicts the weight of alcohol in cirrhosis burden worldwide. J Hepatol. 2016;65:998–1005. doi: 10.1016/j.jhep.2016.06.018. [DOI] [PubMed] [Google Scholar]
- 9.Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E. The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors Among US States. JAMA. 2018;319:1444–1472. doi: 10.1001/jama.2018.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barritt ASt, Jiang Y, Schmidt M, Hayashi PH, Bataller R. Charges for Alcoholic Cirrhosis Exceed All Other Etiologies of Cirrhosis Combined: A National and State Inpatient Survey Analysis. Dig Dis Sci. 2019;64:1460–1469. doi: 10.1007/s10620-019-5471-7. [DOI] [PubMed] [Google Scholar]
- 11.Ndugga N, Lightbourne TG, Javaherian K, Cabezas J, Verma N, Barritt ASt. Disparities between research attention and burden in liver diseases: implications on uneven advances in pharmacological therapies in Europe and the USA. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-013620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heim D, Hunter SC, Ross AJ, Bakshi N, Davies JB, Flatley KJ. Alcohol consumption, perceptions of community responses and attitudes to service provision: results from a survey of Indian, Chinese and Pakistani young people in Greater Glasgow, Scotland, UK. Alcohol and alcoholism (Oxford, Oxfordshire) 2004;39:220–226. doi: 10.1093/alcalc/agh042. [DOI] [PubMed] [Google Scholar]
- 13.Assanangkornchai S, Conigrave KM, Saunders JB. Religious beliefs and practice, and alcohol use in Thai men. Alcohol and alcoholism (Oxford, Oxfordshire) 2002;37:193–197. doi: 10.1093/alcalc/37.2.193. [DOI] [PubMed] [Google Scholar]
- 14.Ventura-Cots M, Watts AE, Cruz-Lemini M, Shah ND, Ndugga N, McCann P. Colder weather and fewer sunlight hours increase alcohol consumption and alcoholic cirrhosis worldwide. Hepatology. 2018;69:1916–1930. doi: 10.1002/hep.30315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ostergaard MLD, Nordentoft M, Hjorthoj C. Associations between substance use disorders and suicide or suicide attempts in people with mental illness: a Danish nation-wide, prospective, register-based study of patients diagnosed with schizophrenia, bipolar disorder, unipolar depression or personality disorder. Addiction. 2017;112:1250–1259. doi: 10.1111/add.13788. [DOI] [PubMed] [Google Scholar]
- 16.Phillips MR, Zhang J, Shi Q, Song Z, Ding Z, Pang S. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey. Lancet (London, England) 2009;373:2041–2053. doi: 10.1016/S0140-6736(09)60660-7. [DOI] [PubMed] [Google Scholar]
- 17.Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob Health. 2017;5:e277-e89. doi: 10.1016/S2214-109X(17)30058-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anstee QM, Daly AK, Day CP. Genetics of Alcoholic Liver Disease. Semin Liver Dis. 2015;35:361–374. doi: 10.1055/s-0035-1567832. [DOI] [PubMed] [Google Scholar]
- 19.Chester JA, Weera MM. Genetic correlation between alcohol preference and conditioned fear: Exploring a functional relationship. Alcohol (Fayetteville, NY) 2017;58:127–137. doi: 10.1016/j.alcohol.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hydes T, Gilmore W, Sheron N, Gilmore I. Treating alcohol-related liver disease from a public health perspective. J Hepatol. 2019;70:223–236. doi: 10.1016/j.jhep.2018.10.036. [DOI] [PubMed] [Google Scholar]
- 21.Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001-2002 to 2012-2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiat. 2017;74:911–923. doi: 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grucza RA, Sher KJ, Kerr WC, Krauss MJ, Lui CK, McDowell YE. Trends in Adult Alcohol Use and Binge Drinking in the Early 21(st) Century United States: A Meta-Analysis of Six National Survey Series. Alcohol Clin Exp Res. 2018;42:1939–1950. doi: 10.1111/acer.13859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kerr WC, Greenfield TK, Ye Y, Bond J, Rehm J. Are the 1976-1985 birth cohorts heavier drinkers? Age-period-cohort analyses of the National Alcohol Surveys 1979-2010. Addiction. 2013;108:1038–1048. doi: 10.1111/j.1360-0443.2012.04055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang C, Lv XW, Xu T, Ni MM, Xia JL, Cai SP. Alcohol use in Hefei in relation to alcoholic liver disease: A multivariate logistic regression analysis. Alcohol (Fayetteville, NY) 2017;71:1–4. doi: 10.1016/j.alcohol.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 25.Hagstrom H, Hemmingsson T, Discacciati A, Andreasson A. Alcohol consumption in late adolescence is associated with an increased risk of severe liver disease later in life. J Hepatol. 2018;68:505–510. doi: 10.1016/j.jhep.2017.11.019. [DOI] [PubMed] [Google Scholar]
- 26.Nielsen JK, Olafsson S, Bergmann OM, Runarsdottir V, Hansdottir I, Sigurdardottir R. Lifetime drinking history in patients with alcoholic liver disease and patients with alcohol use disorder without liver disease. Scand J Gastroenterol. 2017;52:762–767. doi: 10.1080/00365521.2017.1295466. [DOI] [PubMed] [Google Scholar]
- 27.Ventura-Cots M, Watts AE, Bataller R. Binge drinking as a risk factor for advanced alcoholic liver disease. Liver Int. 2017;37:1281–1283. doi: 10.1111/liv.13482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lasebikan VO, Ayinde O, Odunleye M, Adeyefa B, Adepoju S, Fakunle S. Prevalence of alcohol consumption and alcohol use disorders among outdoor drinkers in public open places in Nigeria. BMC Public Health. 2018;18:400. doi: 10.1186/s12889-018-5344-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Witkiewitz K, McCallion E, Kirouac M. Religious Affiliation and Spiritual Practices: An Examination of the Role of Spirituality in Alcohol Use and Alcohol Use Disorder. Alcohol Res. 2016;38:55–58. [PMC free article] [PubMed] [Google Scholar]
- 30.Anstee QM, Daly AK, Day CP. Genetics of alcoholic and nonalcoholic fatty liver disease. Semin Liver Dis. 2011;31:128–146. doi: 10.1055/s-0031-1276643. [DOI] [PubMed] [Google Scholar]
- 31.Stickel F, Moreno C, Hampe J, Morgan MY. The genetics of alcohol dependence and alcohol-related liver disease. J Hepatol. 2017;66:195–211. doi: 10.1016/j.jhep.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 32.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 33.Anthenelli RM. National Institute on Alcohol abuse and Alcoholism; 2011. Alcohol and Health: Focus on Comorbid Mental Health Disorders. [PMC free article] [PubMed] [Google Scholar]
- 34.Pimpin L, Cortez-Pinto H, Negro F, Corbould E, Lazarus JV, Webber L. Burden of liver disease in Europe: Epidemiology and analysis of risk factors to identify prevention policies. J Hepatol. 2018;69:718–735. doi: 10.1016/j.jhep.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 35.Shah ND, Ventura-Cots M, Abraldes JG, Alboraie M, Alfadhli A, Argemi J. Alcohol-related Liver Disease is Rarely Detected at Early Stages Compared With Liver Diseases of Other Etiologies Worldwide. Clin Gastroenterol Hepatol. 2019;17:2320–2329.e12. doi: 10.1016/j.cgh.2019.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Addolorato G, Leggio L, Ferrulli A, Cardone S, Vonghia L, Mirijello A. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet (London, England) 2007;370:1915–1922. doi: 10.1016/S0140-6736(07)61814-5. [DOI] [PubMed] [Google Scholar]
- 37.Aberg F, Helenius-Hietala J, Puukka P, Jula A. Binge drinking and the risk of liver events: A population-based cohort study. Liver Int. 2017;37:1373–1381. doi: 10.1111/liv.13408. [DOI] [PubMed] [Google Scholar]
- 38.Bedogni G, Miglioli L, Masutti F, Ferri S, Castiglione A, Lenzi M. Natural course of chronic HCV and HBV infection and role of alcohol in the general population: the Dionysos Study. Am J Gastroenterol. 2008;103:2248–2253. doi: 10.1111/j.1572-0241.2008.01948.x. [DOI] [PubMed] [Google Scholar]
- 39.Lin CW, Lin CC, Mo LR, Chang CY, Perng DS, Hsu CC. Heavy alcohol consumption increases the incidence of hepatocellular carcinoma in hepatitis B virus-related cirrhosis. J Hepatol. 2013;58:730–735. doi: 10.1016/j.jhep.2012.11.045. [DOI] [PubMed] [Google Scholar]
- 40.Naveau S, Giraud V, Borotto E, Aubert A, Capron F, Chaput JC. Excess weight risk factor for alcoholic liver disease. Hepatology (Baltimore, Md) 1997;25:108–111. doi: 10.1002/hep.510250120. [DOI] [PubMed] [Google Scholar]
- 41.Hagstrom H. Alcohol Consumption in Concomitant Liver Disease: How Much is Too Much? Curr Hepat Rep. 2017;16:152–157. doi: 10.1007/s11901-017-0343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Global Status Report On Alcohol. 1999. https://www.who.int/substance_abuse/publications/en/GlobalAlcohol_overview.pdf
- 43.Xu X, Chaloupka FJ. The effects of prices on alcohol use and its consequences. Alcohol Res Health. 2011;34:236–245. [PMC free article] [PubMed] [Google Scholar]
- 44.Naimi TS, Blanchette JG, Xuan Z, Chaloupka FJ. Erosion of State Alcohol Excise Taxes in the United States. J Stud Alcohol Drugs. 2018;79:43–48. doi: 10.15288/jsad.2018.79.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Makela P, Osterberg E. Weakening of one more alcohol control pillar: a review of the effects of the alcohol tax cuts in Finland in 2004. Addiction. 2009;104:554–563. doi: 10.1111/j.1360-0443.2009.02517.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Herttua K, Makela P, Martikainen P. Changes in alcohol-related mortality and its socioeconomic differences after a large reduction in alcohol prices: a natural experiment based on register data. Am J Epidemiol. 2008;168:1110–1118. doi: 10.1093/aje/kwn216. [discussion 26-31] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wagenaar AC, Tobler AL, Komro KA. Effects of alcohol tax and price policies on morbidity and mortality: a systematic review. Am J Public Health. 2010;100:2270–2278. doi: 10.2105/AJPH.2009.186007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grossman M. The economic analysis of addictive behavior. In: Hilton ME, Bloss G, editors. Economics and the Prevention of Alcohol-Related Problems. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1993. pp. 91–123. National Institute on Alcohol Abuse and Alcoholism Research Monograph No. 25, NIH Pub. No. 93–513. [Google Scholar]
- 49.Zhao J, Stockwell T. The impacts of minimum alcohol pricing on alcohol attributable morbidity in regions of British Colombia, Canada with low, medium and high mean family income. Addiction. 2017;112:1942–1951. doi: 10.1111/add.13902. [DOI] [PubMed] [Google Scholar]
- 50.Nelson JP, AD McNall. Alcohol prices, taxes, and alcohol-related harms: A critical review of natural experiments in alcohol policy for nine countries. Health Policy (Amsterdam, Netherlands) 2016;120:264–272. doi: 10.1016/j.healthpol.2016.01.018. [DOI] [PubMed] [Google Scholar]
- 51.Yamasaki A, Chinami M, Suzuki M, Kaneko Y, Fujita D, Shirakawa T. Tobacco and alcohol tax relationships with suicide in Switzerland. Psychol Rep. 2005;97:213–216. doi: 10.2466/pr0.97.1.213-216. [DOI] [PubMed] [Google Scholar]
- 52.Sloan FA, Reilly BA, Schenzler C. Effects of prices, civil and criminal sanctions, and law enforcement on alcohol-related mortality. J Stud Alcohol. 1994;55:454–465. doi: 10.15288/jsa.1994.55.454. [DOI] [PubMed] [Google Scholar]
- 53.Chatterji P, Dave D, Kaestner R, Markowitz S. Alcohol abuse and suicide attempts among youth. Econ Hum Biol. 2004;2:159–180. doi: 10.1016/j.ehb.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 54.Markowitz S, Chatterji P, Kaestner R. Estimating the impact of alcohol policies on youth suicides. J Ment Health Policy Econ. 2003;6:37–46. [PubMed] [Google Scholar]
- 55.Birckmayer J, Hemenway D. Minimum-age drinking laws and youth suicide, 1970-1990. Am J Public Health. 1999;89:1365–1368. doi: 10.2105/ajph.89.9.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sheron N, Chilcott F, Matthews L, Challoner B, Thomas M. Impact of minimum price per unit of alcohol on patients with liver disease in the UK. Clin Med (Lond) 2014;14:396–403. doi: 10.7861/clinmedicine.14-4-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gill J, Black H, Rush R, O'May F, Chick J. Heavy Drinkers and the Potential Impact of Minimum Unit Pricing-No Single or Simple Effect? Alcohol Alcohol (Oxford, Oxfordshire) 2017;52:722–729. doi: 10.1093/alcalc/agx060. [DOI] [PubMed] [Google Scholar]
- 58.Cousins G, Mongan D, Barry J, Smyth B, Rackard M, Long J. Potential Impact of Minimum Unit Pricing for Alcohol in Ireland: Evidence from the National Alcohol Diary Survey. Alcohol Alcohol (Oxford, Oxfordshire) 2016;51:734–740. doi: 10.1093/alcalc/agw051. [DOI] [PubMed] [Google Scholar]
- 59.Angus CHJ, Brennan A, Meier P. Welsh Government; 2018. Model-based appraisal of the comparative impact of minimun unit pricing and taxation policies in Wales: Final report. [Google Scholar]
- 60.Sharma A, Vandenberg B, Hollingsworth B. Minimum pricing of alcohol versus volumetric taxation: which policy will reduce heavy consumption without adversely affecting light and moderate consumers? PLoS One. 2014;9 doi: 10.1371/journal.pone.0080936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stockwell T, Zhao J, Martin G, Macdonald S, Vallance K, Treno A. Minimum alcohol prices and outlet densities in British Columbia, Canada: estimated impacts on alcohol-attributable hospital admissions. Am J Public Health. 2013;103:2014–2020. doi: 10.2105/AJPH.2013.301289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Boniface S, Scannell JW, Marlow S. Evidence for the effectiveness of minimum pricing of alcohol: a systematic review and assessment using the Bradford Hill criteria for causality. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-013497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Binder C, Knibbe K, Kreissl A, Repa A, Thanhaeuser M, Greber-Platzer S. Does acute alcohol intoxication cause transaminase elevations in children and adolescents? Alcohol (Fayetteville, NY) 2016;51:57–62. doi: 10.1016/j.alcohol.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 64.Doycheva I, Watt KD, Rifai G, Abou Mrad R, Lopez R, Zein NN. Increasing Burden of Chronic Liver Disease Among Adolescents and Young Adults in the USA: A Silent Epidemic. Dig Dis Sci. 2017;62:1373–1380. doi: 10.1007/s10620-017-4492-3. [DOI] [PubMed] [Google Scholar]
- 65.Green MA, Strong M, Conway L, Maheswaran R. Trends in alcohol-related admissions to hospital by age, sex and socioeconomic deprivation in England, 2002/03 to 2013/14. BMC Public Health. 2017;17:412. doi: 10.1186/s12889-017-4265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Moss AC, Albery IP, Dyer KR, Frings D, Humphreys K, Inkelaar T. The effects of responsible drinking messages on attentional allocation and drinking behaviour. Addict Behav. 2015;44:94–101. doi: 10.1016/j.addbeh.2014.11.035. [DOI] [PubMed] [Google Scholar]
- 67.Wagenaar AC, Toomey TL. Effects of minimum drinking age laws: review and analyses of the literature from 1960 to 2000. J Stud Alcohol Suppl. 2002:206–225. doi: 10.15288/jsas.2002.s14.206. [DOI] [PubMed] [Google Scholar]
- 68.Kypri K, Voas RB, Langley JD, Stephenson SC, Begg DJ, Tippetts AS. Minimum purchasing age for alcohol and traffic crash injuries among 15- to 19-year-olds in New Zealand. Am J Public Health. 2006;96:126–131. doi: 10.2105/AJPH.2005.073122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gruenewald PJ, Treno AJ, Ponicki WR, Huckle T, Yeh LC, Casswell S. Impacts of New Zealand's lowered minimum purchase age on context-specific drinking and related risks. Addiction. 2015;110:1757–1766. doi: 10.1111/add.13034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lobstein T, Landon J, Thornton N, Jernigan D. The commercial use of digital media to market alcohol products: a narrative review. Addiction. 2017;112:21–27. doi: 10.1111/add.13493. [DOI] [PubMed] [Google Scholar]
- 71.Noel JK, Babor TF. Does industry self-regulation protect young people from exposure to alcohol marketing? A review of compliance and complaint studies. Addiction. 2017;112:51–56. doi: 10.1111/add.13432. [DOI] [PubMed] [Google Scholar]
- 72.Callaghan RC, Sanches M, Gatley JM, Stockwell T. Impacts of drinking-age laws on mortality in Canada, 1980-2009. Drug Alcohol Depend. 2014;138:137–145. doi: 10.1016/j.drugalcdep.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 73.Raynard B, Balian A, Fallik D, Capron F, Bedossa P, Chaput JC. Risk factors of fibrosis in alcohol-induced liver disease. Hepatology (Baltimore, Md) 2002;35:635–638. doi: 10.1053/jhep.2002.31782. [DOI] [PubMed] [Google Scholar]
- 74.Wilkinson C, Livingston M, Room R. Impacts of changes to trading hours of liquor licences on alcohol-related harm: a systematic review 2005-2015. Public Health Research & Practice. 2016;26 doi: 10.17061/phrp2641644. [DOI] [PubMed] [Google Scholar]
- 75.Popova S, Giesbrecht N, Bekmuradov D, Patra J. Hours and days of sale and density of alcohol outlets: impacts on alcohol consumption and damage: a systematic review. Alcohol Alcohol (Oxford, Oxfordshire) 2009;44:500–516. doi: 10.1093/alcalc/agp054. [DOI] [PubMed] [Google Scholar]
- 76.Middleton JC, Hahn RA, Kuzara JL, Elder R, Brewer R, Chattopadhyay S. Effectiveness of policies maintaining or restricting days of alcohol sales on excessive alcohol consumption and related harms. Am J Prev Med. 2010;39:575–589. doi: 10.1016/j.amepre.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sherk A, Stockwell T, Chikritzhs T, Andreasson S, Angus C, Gripenberg J. Alcohol Consumption and the Physical Availability of Take-Away Alcohol: Systematic Reviews and Meta-Analyses of the Days and Hours of Sale and Outlet Density. J Stud Alcohol Drugs. 2018;79:58–67. [PubMed] [Google Scholar]
- 78.Zhao J, Stockwell T, Martin G, Macdonald S, Vallance K, Treno A. The relationship between minimum alcohol prices, outlet densities and alcohol-attributable deaths in British Columbia, 2002-09. Addiction. 2013;108:1059–1069. doi: 10.1111/add.12139. [DOI] [PubMed] [Google Scholar]
- 79.Smith DI. Effect on liver cirrhosis and traffic accident mortality of changing the number and type of alcohol outlets in western Australia. Alcohol Clin Exp Res. 1989;13:190–195. doi: 10.1111/j.1530-0277.1989.tb00309.x. [DOI] [PubMed] [Google Scholar]
- 80.Smith DI. Relationship between the number and type of alcohol outlets and mortality due to liver cirrhosis and traffic accidents. Drug Alcohol Rev. 1992;11:145–151. doi: 10.1080/09595239200185621. [DOI] [PubMed] [Google Scholar]
- 81.Matheson FI, Creatore MI, Gozdyra P, Park AL, Ray JG. A population-based study of premature mortality in relation to neighbourhood density of alcohol sales and cheque cashing outlets in Toronto, Canada. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2014-006032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Holmes J, Guo Y, Maheswaran R, Nicholls J, Meier PS, Brennan A. The impact of spatial and temporal availability of alcohol on its consumption and related harms: a critical review in the context of UK licensing policies. Drug Alcohol Rev. 2014;33:515–525. doi: 10.1111/dar.12191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gmel G, Holmes J, Studer J. Are alcohol outlet densities strongly associated with alcohol-related outcomes? A critical review of recent evidence. Drug Alcohol Rev. 2016;35:40–54. doi: 10.1111/dar.12304. [DOI] [PubMed] [Google Scholar]
- 84.Maheswaran R, Holmes J, Green M, Strong M, Pearson T, Meier P. Investigation of the Association Between Alcohol Outlet Density and Alcohol-Related Hospital Admission Rates in England: Study Protocol. JMIR research protocols. 2016;5:e243. doi: 10.2196/resprot.6300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wells S, Graham K, Purcell J. Policy implications of the widespread practice of 'pre-drinking' or 'pre-gaming' before going to public drinking establishments: are current prevention strategies backfiring? Addiction. 2009;104:4–9. doi: 10.1111/j.1360-0443.2008.02393.x. [DOI] [PubMed] [Google Scholar]
- 86.Romo-Aviles N, Marcos-Marcos J, Marquina-Marquez A, Gil-Garcia E. Intensive alcohol consumption by adolescents in Southern Spain: The importance of friendship. Int J Drug Policy. 2016;31:138–146. doi: 10.1016/j.drugpo.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 87.Jernigan DH. Global alcohol producers, science, and policy: the case of the International Center for Alcohol Policies. Am J Public Health. 2012;102:80–89. doi: 10.2105/AJPH.2011.300269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Research ZM . 2018. Alcoholic Beverages Market By Type (Wine, Beer, and Spirit), By Packaging (Tin, Glass Bottles, and Plastic Bottles), By Sales Channel (Hotels/Bars/Restaurants and Online Retailers, Specialty Stores, and Convenience Stores): Global Industry Perspective, Comprehensive Analysis and Forecast, 2017 – 2024. [Google Scholar]
- 89.Babor TF, Robaina K. Public health, academic medicine, and the alcohol industry's corporate social responsibility activities. Am J Public Health. 2013;103:206–214. doi: 10.2105/AJPH.2012.300847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.McCambridge J, Mialon M. Alcohol industry involvement in science: A systematic review of the perspectives of the alcohol research community. Drug Alcohol Rev. 2018;37:565–579. doi: 10.1111/dar.12826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.McCambridge J, Kypri K, Sheldon TA, Madden M, Babor TF. Advancing public health policy making through research on the political strategies of alcohol industry actors. J Public Health (Oxf) 2019 doi: 10.1093/pubmed/fdz031. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Petticrew M, McKee M, Marteau TM. Partnerships with the alcohol industry at the expense of public health. Lancet (London, England) 2018;392:992–993. doi: 10.1016/S0140-6736(18)32320-1. [DOI] [PubMed] [Google Scholar]
- 93.Newton JN, Cosford P. Partnerships with the alcohol industry: opportunities and risks. Lancet (London, England) 2018;392:1401–1402. doi: 10.1016/S0140-6736(18)32333-X. [DOI] [PubMed] [Google Scholar]
- 94.Saffer H. Alcohol advertising bans and alcohol abuse: an international perspective. J Health Econ. 1991;10:65–79. doi: 10.1016/0167-6296(91)90017-h. [DOI] [PubMed] [Google Scholar]
- 95.Wilkinson C, Room R. Warnings on alcohol containers and advertisements: international experience and evidence on effects. Drug Alcohol Rev. 2009;28:426–435. doi: 10.1111/j.1465-3362.2009.00055.x. [DOI] [PubMed] [Google Scholar]
- 96.EASL Recommendations on Treatment of Hepatitis C 2018J Hepatol. 2018;69:461–511. doi: 10.1016/j.jhep.2018.03.026. [DOI] [PubMed] [Google Scholar]
- 97.Anderson P, de Bruijn A, Angus K, Gordon R, Hastings G. Impact of alcohol advertising and media exposure on adolescent alcohol use: a systematic review of longitudinal studies. Alcohol Alcohol (Oxford, Oxfordshire) 2009;44:229–243. doi: 10.1093/alcalc/agn115. [DOI] [PubMed] [Google Scholar]
- 98.Lindeman M, Katainen A, Svensson J, Kauppila E, Hellman M. Compliance with regulations and codes of conduct at social media accounts of Swedish alcohol brands. Drug Alcohol Rev. 2019;38:386–390. doi: 10.1111/dar.12928. [DOI] [PubMed] [Google Scholar]
- 99.Siegfried N, Pienaar DC, Ataguba JE, Volmink J, Kredo T, Jere M. Restricting or banning alcohol advertising to reduce alcohol consumption in adults and adolescents. Cochrane Database Syst Rev. 2014;(11) doi: 10.1002/14651858.CD010704.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Curtis BL, Lookatch SJ, Ramo DE, McKay JR, Feinn RS, Kranzler HR. Meta-Analysis of the Association of Alcohol-Related Social Media Use with Alcohol Consumption and Alcohol-Related Problems in Adolescents and Young Adults. Alcohol Clin Exp Res. 2018;42:978–986. doi: 10.1111/acer.13642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jernigan DH, Padon A, Ross C, Borzekowski D. Self-Reported Youth and Adult Exposure to Alcohol Marketing in Traditional and Digital Media: Results of a Pilot Survey. Alcohol Clin Exp Res. 2017;41:618–625. doi: 10.1111/acer.13331. [DOI] [PubMed] [Google Scholar]
- 102.Stautz K, Frings D, Albery IP, Moss AC, Marteau TM. Impact of alcohol-promoting and alcohol-warning advertisements on alcohol consumption, affect, and implicit cognition in heavy-drinking young adults: A laboratory-based randomized controlled trial. Br J Health Psychol. 2017;22:128–150. doi: 10.1111/bjhp.12221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Stautz K, Marteau TM. Viewing alcohol warning advertising reduces urges to drink in young adults: an online experiment. BMC Public Health. 2016;16:530. doi: 10.1186/s12889-016-3192-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.MacDonnell K, Cowen E, Cunningham DJ, Ritterband L, Ingersoll K. Online recruitment of a non-help-seeking sample for an internet intervention: Lessons learned in an alcohol-exposed pregnancy risk reduction study. Internet Interv. 2019;17 doi: 10.1016/j.invent.2019.100240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hadland SE, Xuan Z, Blanchette JG, Heeren TC, Swahn MH, Naimi TS. Alcohol Policies and Alcoholic Cirrhosis Mortality in the United States. Prev Chronic Dis. 2015;12 doi: 10.5888/pcd12.150200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Treno AJ, Ponicki WR, Stockwell T, Macdonald S, Gruenewald PJ, Zhao J. Alcohol outlet densities and alcohol price: the British Columbia experiment in the partial privatization of alcohol sales off-premise. Alcohol Clin Exp Res. 2013;37:854–859. doi: 10.1111/acer.12065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Khaltourina D, Korotayev A. Effects of Specific Alcohol Control Policy Measures on Alcohol-Related Mortality in Russia from 1998 to 2013. Alcohol Alcohol (Oxford, Oxfordshire) 2015;50:588–601. doi: 10.1093/alcalc/agv042. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material