Abstract
Objectives: To explore the effects of membership in a fitness program for older adults on social isolation, loneliness, and health. Method: Using survey responses from SilverSneakers members and matched nonmembers, regression path analysis was used to examine the influence of SilverSneakers membership on physical activity, social isolation, loneliness, and health, and the interrelationships among these concepts. Results: SilverSneakers membership directly increased physical activity and self-rated health, directly decreased social isolation, and indirectly decreased loneliness. Decreased social isolation and loneliness were associated with better self-rated health: social isolation and loneliness had independent direct effects on health, while social isolation also had an indirect effect on health mediated through loneliness. Discussion: Members of SilverSneakers experienced better health through increased physical activity, reduced social isolation, and reduced loneliness. Future research should explore independent effects of social isolation and loneliness on health and the mechanisms by which membership reduces social isolation and loneliness.
Keywords: social isolation, loneliness, physical activity, older adults, group membership
Introduction
Social isolation has been shown to have a significant impact on health and well-being. Older adults—defined as those aged 65 and older—are particularly susceptible to becoming isolated, with an estimated 17% of older Americans reporting being isolated (Ortiz, 2011). Social isolation has been found to be associated with older age, living alone, depressed mood, poor memory, worse functional ability, and poorer self-rated health (Iliffe et al., 2007). Retirement, reduced mobility, and the deaths of friends and family all may play a role in reducing the size of one’s social network (Cornwell, Laumann, & Schumm, 2008).
The detrimental effects of social isolation are related not only to mental health and emotional well-being but also to physical health and functioning. Social isolation has been shown to have a significant effect on the incidence of dementia (Fratiglioni, Wang, Ericsson, Maytan, & Winblad, 2000) and morbidity, particularly the incidence of coronary heart disease and stroke (Valtorta, Kanaan, Gilbody, Ronzi, & Hanratty, 2016). In fact, social isolation’s effect on mortality may be comparable in magnitude to risk factors such as smoking, obesity, and air pollution (Holt-Lunstad, 2017; Pentell et al., 2013). Among social determinants of health, including food security, access to a primary care physician, and educational attainment, social isolation has been shown to have the greatest observed effect on health and well-being (Cordier et al., 2018). As a function of Medicare spending, health care costs of isolated individuals are estimated to be on average US$1,608 per year more than those who are not isolated (Shaw et al., 2017).
The issue of social isolation among older adults has attained national agenda status. The impetus to address the problem is highlighted by publicity in media outlets (Khullar, 2016) and by AARP’s founding of Connect2Affect (PRNewswire, 2016). With the increasing focus on social isolation as a population health issue, an urgency grows to clarify uncertainty around how isolation among older adults can be effectively addressed. One underexplored area of inquiry is the extent to which different kinds of group membership produce impacts on social isolation.
Background and Objectives
Delineating Social Isolation and Loneliness
Defined precisely, social isolation is an “objective and quantifiable reflection of reduced social network size and paucity of social contact” (Steptoe, Shankar, Demakakos, & Wardle, 2013). Social isolation is often conflated conceptually and empirically with loneliness. Loneliness is a distinct construct defined as a subjective state “reflecting the individual’s experienced dissatisfaction with the frequency and closeness of their social contacts or the discrepancy between the relationships they have and the relationships they would like to have.” Although these concepts are closely related (Golden et al., 2009; Shiovitz-Ezra & Leitsch, 2010), one state can be observed without the presence of the other (Golden et al., 2009; Singh & Misra, 2009), and different forms of social engagement could have an effect on one state but not the other (Hall-Lande, Eisenberg, Christenson, & Neumark-Sztainer, 2007). Loneliness, experienced by as many as 43% of older adults in the Health and Retirement Study (Perissinotto, Cenzer, & Covinsky, 2012), is an independent risk factor for health outcomes like depression and premature death (Luo, Hawkley, Waite, & Cacioppo, 2012; Warner, Roberts, Jeanblanc, & Adams, 2017).
Currently there is no consensus on a “gold standard” measure to capture objective social isolation in individuals. This study uses the Berkman social disengagement index (Bassuk, Glass, & Berkman, 1999), which captures the conceptual definition of social isolation in terms of network size and social contact. The concept of loneliness is defined and measured as a distinct construct representing people’s perceived levels of integration with their social environments. The UCLA (University of California, Los Angeles) Loneliness Scale was used to measure loneliness in this study (Hughes, Waite, Hawkley, & Cacioppo, 2004).
Efficacy of Interventions for Isolated Individuals
One would expect any sort of program that brings individuals into contact with others to have a positive effect on objective social isolation. But the effectiveness of a social organization in encouraging bonding between individuals is not guaranteed. In Bowling Alone, Putnam (2007) identified the propensities of modern individuals both to avoid communal activity and to act in solitude even when participating in activities that ought to be communal. He describes a scene at the Holiday Bowling Lanes in New London, Connecticut, in which bowlers focus their attention toward a mounted television between turns instead of engaging in conversation with each other. “Even when they are bowling together,” Putnam writes, “They are watching alone.”
A social support program should be evaluated before assuming its efficacy in affecting social isolation. Findlay (2003) found a lack of evidence as to whether interventions such as support groups or formal outreach to isolated individuals were truly effective in reducing social isolation. A later review of quantitative studies by Cattan, White, Bond, and Learmouth (2005) that evaluated the effectiveness of social programs for reducing isolation observed just one third of them to be effective. Successful programs were primarily “group interventions with an educational or social support input for specific groups of older people.” Another review discovered that interventions that explicitly targeted socially isolated or lonely individuals were less effective than those that did not (Dickens, Richards, Greaves, & Campbell, 2011). There is no clear consensus in the existing research as to what characteristics of a program or intervention effectively influence social isolation.
Membership in a Large-Scale Fitness Program as a Plausible Intervention
Given the prevalence and negative impacts of social isolation, and the limited proven approaches to address the issue, particularly at scale, there is a need to identify large-scale programs that reduce isolation. Even if a program is not expressly designed to reduce isolation, it may nonetheless foster social engagement. One such program may be SilverSneakers, an exercise program available to older adults as part of many Medicare Advantage and Medigap plans that provides gym memberships and offers specialized group exercise classes at no additional cost.
Designed to improve health and functioning for older adults, SilverSneakers has been shown to improve participants’ physical and mental health. For example, over a period of 3 years, SilverSneakers participants showed significantly better physical and mental health and lower impairment than a random sample of other Medicare Advantage members, including participants’ ability to perform activities of daily living (ADLs; Hamar, Coberley, Pope, & Rula, 2013). Other longitudinal studies have demonstrated that the program decreases risk of hospitalization and health care costs (Nguyen, Maciejewski, et al., 2008), and reduces risk of depression (Nguyen, Ackermann, et al., 2008).
SilverSneakers may also positively affect quality of life and health by serving as a form of social engagement. The social environment of the gym and the participatory nature of SilverSneakers group exercise classes should theoretically have a beneficial effect on participants’ objective social isolation and subjective loneliness. In support of this hypothesis, McAuley et al. (2000) found that a 6-month exposure to a socially supportive exercise program led to increased life satisfaction and reduced feelings of loneliness. Although previous studies have demonstrated beneficial health outcomes associated with SilverSneakers participation and that SilverSneakers members have fewer social limitations as a result of improved health (Hamar et al., 2013), no study has evaluated the program’s direct impact on social isolation and how this direct effect may in turn contribute to health outcomes above and beyond the benefits of physical activity.
The Proposed Model
The central aim of this study is to identify whether SilverSneakers membership functions as a mechanism to improve health through reduced social isolation and increased physical activity, while examining the complex pathways through which these concepts are related. To examine the multifarious relationships among the constructs in the study, this study uses a path model analysis. Path analysis is a form of multiple regression where both direct and mediated effects can be estimated simultaneously to test a hypothesized relationship model among a set of variables. The method can be used to determine direction and magnitude of both direct and indirect quantitative relationships. Path model analysis has been utilized in other studies examining well-being, health, and social connection (e.g., Kraut et al., 1998; Lampinen, Heikkinen, Kauppinen, & Heikkinen, 2006).
The proposed path model hypothesizes that SilverSneakers membership will decrease social isolation and increase physical activity directly, controlling for a vector of six covariates. In addition, we hypothesize that SilverSneakers will reduce social isolation through its effect on physical activity level. As a secondary consideration, we expect that SilverSneakers will have an indirect effect on loneliness, mediated through reduced social isolation. Finally, we hypothesize that SilverSneakers will have a positive impact on participants’ health via increased physical activity and reduced social isolation.
Research Design and Method
Study Design
We used a cross-sectional, quasi-experimental study design to examine the impact of the SilverSneakers program on outcomes including health, physical activity, social isolation, and loneliness by comparing SilverSneakers participants with matched nonparticipants. Data were collected via an online survey. The study was reviewed and approved by MIT’s Committee on the Use of Humans as Experimental Subjects (COUHES) (IRB Approval Number: 1706989173A001).
Sample
Respondent selection
The study sample was drawn from a population of members under a large Medicare Advantage insurance provider who were all eligible for the SilverSneakers program as a plan benefit and who had available e-mail addresses. Program members were defined as those people who had been enrolled in the SilverSneakers program for at least 6 months and who had used their membership to take a fitness class or go to a gym at least 1 time in the 30 days prior to drawing the sample. A membership period of at least 6 months was set to ensure that people had been enrolled in the program long enough to experience improved outcomes. Nonmembers were those currently eligible for but who had never been enrolled in the SilverSneakers program. Nonmembers had to be at least 65 years and 7 months of age, to match the age range of members in the participant sample who became eligible at age 65 plus the required length of program enrollment. To explore whether membership in SilverSneakers could have an impact on health over a relatively short period of time and to reduce variance, people who had been enrolled in the program for longer than 3 years were eliminated from the sampling frame. More information on the SilverSneakers program can be found at www.silversneakers.com.
To make the SilverSneakers member and nonmember samples as comparable as possible, the sample was stratified by age in 5-year increments (65 years 7 months to 69, 70-74, 75-79, 80-84, 85-89, and 90 and older) and by gender. A 2:1 ratio of nonmembers to members was also drawn from the sample frame to ensure that sample matching would yield at least an equivalent number of members and nonmembers without substantive loss to the participant sample (Lewallen & Courtright, 1998).
Survey Administration
Participants received an e-mail invitation with a unique link to an online survey on the Qualtrics platform. The survey was fielded between August 9 and September 22, 2017. The sample was released in waves until the target sample size was met. A total of 163,216 e-mail invitations were sent, with an overall response rate of 2.1% (American Association for Public Opinion Research, 2016). The response rate was impacted by the presence of inactive e-mail addresses on the contact list from the insurer. Participants who completed the questionnaire were eligible to enter their e-mail addresses into a compensation lottery for Amazon.com gift cards.
Matching
We used coarsening exact matching (CEM) to reduce confounding bias or imbalance from key demographic variables that might differ between the member and nonmember groups (CEM; Iacus, King, & Porro, 2017). The sample was matched on four variables: gender, age stratum (in 5-year segments used in stratification), education (less than high school diploma, high school graduate or General Educational Development [GED], some college or associates’ degree, college graduate, and completed graduate degree), and household income (less than US$25,000; US$25,000-US$49,999; US$50,000-US$74,999; US$75,000-US$99,999; US$100,000-US$149,999; or US$150,000 or more). Software to calculate the data weights is available free online (Iacus et al., 2017).
Table 1 displays both the prematch and postmatch characteristics of SilverSneakers members and nonmembers. The multivariate imbalance measure (L1, range 0-1 with values closer to 0 indicating less imbalance) before matching was 0.195, and the univariate imbalance for each of the matched variables ranged from 0.006 to 0.035, indicating that our CEM procedure greatly reduced imbalance. The matching process pruned only two SilverSneakers members and 30 nonmembers. After weighting using CEM-generated weights, with the exception of the lowest two income categories that were subsequently controlled for in statistical modeling, there were no statistically significant differences between the member and nonmember groups following the CEM match procedure.
Table 1.
Pre- and Postmatched Sample Characteristics of SilverSneakers Member and Nonmember Control Groups.
| Sample characteristics | Prematch |
CEM-matcheda | ||||
|---|---|---|---|---|---|---|
| Member | Nonmember | Total | Member | Nonmember | Total | |
| Female | 47.7* | 51.1* | 47.7 | 49.2 | ||
| Total N | 1,195 | 2,294 | 3,489 | 1,193 | 2,264 | 3,457 |
| Age group | ||||||
| 65-69 | 30.6 | 31.8 | 30.6 | 28.2 | ||
| 70-74 | 25.1* | 31.5* | 25.1 | 27.6 | ||
| 75-79 | 30.9* | 22.5* | 31.0 | 31.0 | ||
| 80-85 | 11.1 | 10.5 | 11.0 | 11.1 | ||
| 85-89 | 2.3* | 3.8* | 2.3 | 2.2 | ||
| Total N | 1,197 | 2,298 | 3,495 | 1,195 | 2,268 | 3,463 |
| Household income | ||||||
| <US$25,000 | 10.7* | 17.3* | 10.7* | 14.6* | ||
| US$25,000-US$49,999 | 34.2 | 34.0 | 34.2* | 30.3* | ||
| US$50,000-US$74,999 | 26.1* | 21.7* | 26.1 | 26.1 | ||
| US$75,000-US$99,999 | 14.8 | 12.9 | 14.8 | 14.8 | ||
| US$100,000-US$149,999 | 10.2 | 8.7 | 10.2 | 10.2 | ||
| >US$150,000 | 4.1* | 5.5* | 4.0 | 4.1 | ||
| Total N | 1,089 | 2,115 | 3,204 | 1,088 | 2,067 | 3,155 |
| Education | ||||||
| Some high school | 1.0* | 2.2* | 1.0 | 1.6 | ||
| High school graduate | 14.8* | 17.4* | 14.8 | 14.2 | ||
| Some college (associates) | 31.0 | 32.0 | 30.9 | 30.9 | ||
| College graduate | 27.1 | 25.0 | 27.1 | 27.1 | ||
| Graduate degree | 26.1* | 23.4* | 26.2 | 26.1 | ||
| Total N | 1,195 | 2,291 | 3,486 | 1,193 | 2,264 | 3,457 |
Note. Table entries are percentages based on Total N counts. Total N varies by variable based on patterns of missing data and cases that were unable to be matched. CEM = coarsened exact matching.
Percentages in matched groups are weighted values, calculated based on weights generated through CEM on gender, age category, education, and income.
Percentages are statistically significant (p < .05) between members and nonmembers.
Measures
Physical activity
People’s levels of physical activity were captured by items asking, “About how many times during the past week did you participate in the following activities?” Participants were asked about vigorous activity (“activities that cause large increases in breathing, heart rate, or leg fatigue, or that cause you to perspire—for example, running, aerobics, uphill hiking”), moderate (“activities that cause a small to moderate increase in breathing or heart rate. You should be able to talk but not sing—for example, brisk walk, water aerobics”), low-intensity (“activities that do not cause changes in your breathing patterns and do not cause you to perspire. You should be able to carry on a conversation while performing—for example, light walking, stretching, leisurely swimming”), and strength training (“exercises designed to strengthen your muscles—for example, weight lifting, power yoga, heavy gardening”). Each item contained five response categories (0 times, 1-2 times, 3-4 times, 5-6 times, and 7 times per week).
To create the physical activity variable used in the analysis, responses around vigorous and moderate activities were combined, with moderate activities being weighted half as much as vigorous activities. This scaling is consistent with the Centers for Disease Control and Prevention’s (CDC) valuations of intensities of aerobic physical activity for older adults and can be found on the CDC’s website (see https://www.cdc.gov/physicalactivity/basics/older_adults/index.htm).
Social isolation
Social isolation was measured with the Berkman social disengagement scale (Bassuk et al., 1999; Ertel, Glymour, & Berkman, 2008). Bassuk et al. define social engagement as “the maintenance of many social connections and a high level of participation in social activities.” Six different constructs are used to create the measure: marital status (spouse or no spouse), monthly visual and annual nonvisual contact with friends and relatives, attendance at religious services, group memberships, and participation in social activities. The items were combined to create a scale following Bassuk et al. The Berkman social disengagement scale is used in this analysis because it includes only objective elements of social isolation, unlike other widely used social isolation measures such as the Duke Social Support Index (DSSI; Koenig et al., 1993) and the Lubben Social Network Scale (LSNS-R; Lubben & Gironda, 2004), which assess people’s feelings of loneliness as well as isolation.
Loneliness
The three-item version of the widely used UCLA Loneliness Scale was used to measure loneliness (Hughes et al., 2004; Russell, 1996).
Health
Health was captured using the standard measure of self-rated general health from the SF-12: “In general, would you say your health is . . .” with response options of “excellent,” “very good,” “good,” “fair,” and “poor.” The item was rescaled from 0 to 1, with higher scores representing better health (Benyamini, 2011).
Covariates
Control measures were added to the analysis to account for the effects of other individual characteristics that might have a bearing on one or more of the variables in the model. These included gender (dichotomous indicator representing whether the respondent was female), vision (a dichotomous indicator representing if the respondent had glaucoma, macular degeneration, cataracts, blindness in one or both eyes, or any other uncorrected vision impairment), hearing (a dichotomous indicator representing whether the respondent had deafness in one or both ears or any other hearing limitations), and mobility issues (whether the individual had any conditions that substantially limited one or more basic physical activities, represented as a dichotomous indicator). Because racial and ethnic diversity in the sample were low, a single dummy variable for White ethnicity was included as a control variable. Finally, a count of six health conditions was included as a control in the analysis, as previous literature showed these conditions correlate with participants’ levels of physical activity and overall health, which could potentially impact social contact and feelings of loneliness. The six conditions were heart attack, diabetes, stroke or transient ischemic attack (TIA), fibromyalgia, Parkinson’s disease, and postspinal surgery (Herring, Puetz, O’Connor, & Dishman, 2012; Morrato, Hill, Wyatt, Ghushchyan, & Sullivan, 2007).
Analysis
Data from the survey were downloaded and cleaned using IBM SPSS version 24. Analysis of the data was done in SPSS (frequencies and CEM data weighting) and in Mplus version 8 (correlations, path analysis). After CEM was applied and missing cases were removed from the analysis using full information maximum likelihood (FIML), 3,143 cases remained in the final study group. (For more information on how missing data are modeled using the FIML method, see Enders, 2001.) Based on differences between the study groups on two income categories that remained statistically significant following application of matching weights (household incomes of less than US$25,000 and between US$25,000 and US$49,999), the initial path model was adjusted to include these two dichotomous income variables as covariates on each of the endogenous variables. The path model analysis used maximum likelihood estimation with robust standard errors, which allows for nonnormality in the data.
Results
Means of key exogenous and endogenous variables as well as covariates are reported in Table 2. Among study participants, just over one third were active SilverSneakers members, while approximately two thirds were eligible for SilverSneakers but had never participated in the program. Pearson’s correlations among all key exogenous and endogenous variables are displayed in Table 3. All correlations were statistically significant and weak to moderate in strength, with absolute values ranging from about 0.05 to about 0.36.
Table 2.
Sample Statistics for Variables Included in Path Model.
| Variables | M | Variance | Minimum | Maximum | Skew | N |
|---|---|---|---|---|---|---|
| SilverSneakers membership | 0.347 | 0.226 | 0 | 1 | 0.644 | 3,143 |
| Physical activity | 0.517 | 0.135 | 0 | 1.5 | 0.443 | 3,126 |
| Social isolation | 2.147 | 0.701 | 1 | 4 | 0.202 | 3,143 |
| Loneliness | 0.443 | 0.467 | 0 | 3 | 1.605 | 3,136 |
| Health | 0.681 | 0.050 | 0 | 1 | −0.594 | 3,143 |
| Chronic conditions | 0.416 | 0.451 | 0 | 4 | 1.588 | 3,143 |
| Vision | 0.258 | 0.192 | 0 | 1 | 1.105 | 3,143 |
| Hearing | 0.335 | 0.223 | 0 | 1 | 0.698 | 3,143 |
| White | 0.896 | 0.093 | 0 | 1 | −2.603 | 3,143 |
| Mobility issues | 0.253 | 0.189 | 0 | 1 | 1.137 | 3,143 |
| Gender | 0.471 | 0.249 | 0 | 1 | 0.115 | 3,143 |
| Income <US$25,000 | 0.131 | 0.114 | 0 | 1 | 2.183 | 3,143 |
| Income US$25,000-US$50,000 | 0.314 | 0.215 | 0 | 1 | 0.804 | 3,143 |
| Valid N for full model (FIML) = 3,143 | ||||||
Note. FIML = full information maximum likelihood.
Table 3.
Pearson’s Correlations for Variables Included in Path Model.
| SilverSneakers membership | Physical activity | Social isolation | Loneliness | Health | |
|---|---|---|---|---|---|
| SilverSneakers membershipa | 1.00 | ||||
| Physical activity | .165 | 1.00 | |||
| Social isolation | −.083 | −.107 | 1.00 | ||
| Loneliness | −.053 | −.154 | .295 | 1.00 | |
| Health | .158 | .360 | −.170 | −.267 | 1.00 |
Note. All correlations are significant at p < .05, N = 3,143.
SilverSneakers membership is a binary variable modeled here as continuous.
Model Optimization
Examination of correlations and results from the initial hypothesized path model led to several modifications. Hearing was removed as a covariate from both health and social isolation because it did not show a statistically significant relationship with those variables. In addition, vision was removed as a covariate from social isolation because it was not statistically significant. The race variable was removed as a covariate from physical activity and loneliness because it was not statistically significant in predicting those variables. Finally, the chronic condition variable was removed as a covariate from social isolation and loneliness because its relationships with those variables were not statistically significant. Although all paths in the hypothesized model were significant, two additional pathways were added to explain more of the variance in health, based on correlation coefficients in Table 3 and modification indices. The first was a direct path from SilverSneakers to health to capture the impact of membership on health that could not be explained by increases in physical activity or decreases in social isolation. The second was a path added from loneliness to health to capture the distinct impact loneliness has on health.
Final Path Model Results
The final path model is displayed in Figure 1, and the overall model fit statistics are shown in Table 4. The fit statistics for the final path model suggest a good-fitting model. For a model to be considered a good fit for the data, the comparative fit index (CFI) and Tucker–Lewis index (TLI) should be greater than or equal to 0.95, and the root mean square error approximation (RMSEA) should be below 0.07 (Hooper, Coughlan, & Mullen, 2008; Hu & Bentler, 1999). Table 5 reports the R2 values of the four endogenous variables. Although the R2 values are generally low, they are all significant (p < .01). The path coefficients for the covariates included in the model were all statistically significant with p < .05. Several alternative path model specifications were examined, and all had worse fit indices compared with the final path model presented in Figure 1.
Figure 1.
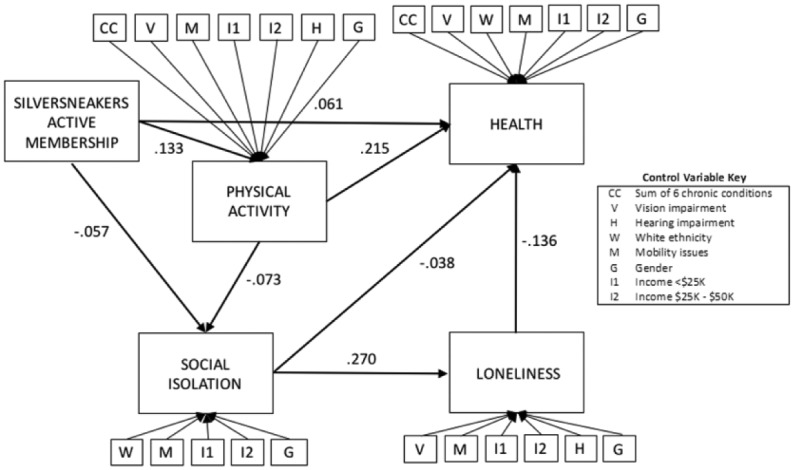
Final path model of SilverSneakers membership on physical activity, social isolation, loneliness, and health.
Note. Path coefficients are standardized values; all path coefficients are statistically significant at p < .05, N = 3,143.
Table 4.
Fit Statistics of Final Path Model.
| CFI | .994 |
| TLI | .973 |
| RMSEA | .021 |
| Probability RMSEA ⩽ .05 | 1.00 |
Note. CFI = comparative fit index; TLI = Tucker–Lewis index; RMSEA = root mean square error approximation.
Table 5.
R2 of endogenous variables.
| Physical activity | .127 |
| Social isolation | .069 |
| Loneliness | .132 |
| Health | .350 |
Note. All R2 are significant at p < .01.
The direct, indirect, and total effects of the path variables on the endogenous variables are provided in Table 6. In the final path model, SilverSneakers membership influenced health status through one direct and several indirect paths. The direct path from SilverSneakers to health accounted for more than 60% (0.061) of the total effect. The indirect impacts of SilverSneakers membership on health (36% or .034) were produced via increased physical activity, reduced social isolation, and reduced loneliness.
Table 6.
Direct, Indirect, and Total Effects of SilverSneakers Membership, Physical Activity, Social Isolation, and Loneliness.
| As predictors | ||||||||
|---|---|---|---|---|---|---|---|---|
| SilverSneakers membership |
Physical activity |
Social isolation |
Loneliness | |||||
| Unstandardized | Standardized | Unstandardized | Standardized | Unstandardized | Standardized | Unstandardized | Standardized | |
| Physical activity | ||||||||
| Direct | .103 | .133 | ||||||
| Indirect | — | — | ||||||
| Total | .103 | .133 | ||||||
| Social isolation | ||||||||
| Direct | −.101 | −.057 | −.167 | −.073 | ||||
| Indirect | −.017 | −.010 | — | — | ||||
| Total | −.118 | −.067 | −.167 | −.073 | ||||
| Loneliness | ||||||||
| Direct | — | — | — | — | .220 | .270 | ||
| Indirect | −.026 | −.018 | −.037 | −.020 | — | — | ||
| Total | −.026 | −.018 | −.037 | −.020 | .220 | .270 | ||
| Health | ||||||||
| Direct | .028 | .061 | .130 | .215 | −.010 | −.038 | −.044 | −.136 |
| Indirect | .016 | .034 | .003 | .006 | −.010 | −.037 | — | — |
| Total | .044 | .094 | .134 | .220 | −.020 | −.075 | −.044 | −.136 |
Note. All direct, indirect, and total effects are statistically significant at p < .05 level.
SilverSneakers membership was associated with increased physical activity and had both a direct and indirect effect on social isolation; that is, SilverSneakers membership was associated with lower isolation. Approximately 85% (–0.057) of the effect of SilverSneakers membership on social isolation was through the direct path, while 15% (–0.010) of the impact was mediated through increased physical activity. SilverSneakers membership was also associated with less loneliness as mediated through both increased physical activity and decreased social isolation. Although there is a direct effect of social isolation on health (–0.038), just under half (49%) of the total effect of social isolation on health was mediated by loneliness (–0.037).
Discussion and Implications
Since 1900, life expectancy has increased for Americans by 29 years (Coughlin, 2017), yet living longer does not necessarily mean living better. Staying socially engaged and physically active is key for maintaining health and quality of life in older age (Hajek et al., 2017; Rejeski & Mihalko, 2001). Although any form of physical activity can be beneficial to the health of older adults, Kanamori et al. (2016) found that exercising with others has significant health benefits regardless of the total frequency of exercise. The social component of group exercise activities may be one mechanism through which these health benefits are realized. Consistent with Kanamori’s findings, the results of this analysis suggest that SilverSneakers membership is associated with improved health not only due to increased physical activity but also due to reduced social isolation and in turn reduced loneliness.
The path analysis merges existing literature with theoretical knowledge of the SilverSneakers program to test hypotheses about how key variables were related empirically. This method offered a means to evaluate the complex ways in which social isolation, loneliness, physical activity, and ultimately health are related to one another directly and indirectly. As a result, we explored multiple channels through which SilverSneakers membership has a positive effect on health.
SilverSneakers members were significantly less likely to be socially isolated than nonmembers. The greatest impacts on social isolation were directly from SilverSneakers membership, although social isolation was also affected by SilverSneakers membership indirectly through increased physical activity. An explanation for this direct effect could be that members use SilverSneakers as a channel to make social connections that are maintained beyond the gym. In addition, participation in the SilverSneakers program may cause members to feel more confident and empowered, thereby increasing their sociability. Previous studies on group membership found that the pride and reputation of a particular group were positively associated with an individual’s self-esteem (Smith & Tyler, 1997). Because SilverSneakers may be considered a nationally recognized and well-known program among older adults, being an active member may increase levels of self-esteem, thereby increasing levels of sociability.
The model also reveals that SilverSneakers members are less likely to experience feelings of loneliness. The reduction in feelings of loneliness was associated directly with improved overall health, independent of the effect of social isolation on overall health. This finding supports the claim that social isolation and loneliness, although related, are distinct concepts that should be modeled separately (Shaw et al., 2017). In addition, this result corroborates findings from previous literature around the relationships between social isolation, loneliness, and health, by showing that both objective social isolation and subjective feelings of loneliness have discrete negative effects on an individual’s health (Holt-Lunstad, Smith, Baker, Harris, & Stephenson, 2015; Shankar, McMunn, Banks, & Steptoe, 2011).
Consistent with Hamar et al. (2013), this study found that SilverSneakers members had significantly better self-rated health than nonmembers. The direct effect of SilverSneakers membership on health was greater, however, than any other indirect pathway from SilverSneakers to health (via social isolation, physical activity, or loneliness), although all paths were significant. One explanation for the magnitude of this direct effect is that a criterion for being included in the member sample was recent participation in SilverSneakers, which may have caused the SilverSneakers sample to be healthier than the nonmember sample. The direct effect of membership on health appears, however, even after controlling for physical activity in the path model, and has an effect size almost double that of all indirect paths from SilverSneakers to health. The size of the direct effect on health after controlling for the indirect effects of membership on health via other variables (including physical activity) suggests that membership may confer other health benefits that are not explicitly captured in our model. Future research may explore other impacts of the SilverSneakers program that may affect health over and above its effects on physical activity and social isolation. For example, individuals who consistently participate in the SilverSneakers program may have higher levels of self-efficacy, confidence, and purposefulness, which may positively affect their health (Grembowski et al., 1993; Kim, Kawachi, Chen, & Kubzansky, 2017).
This is the first study to demonstrate that a program available to millions of older adults has the potential to decrease social isolation, and through this mechanism improve health through social support and decreased loneliness. Membership in a program that encourages social interaction through participation in fitness activities may reduce isolation, which can benefit health above and beyond the direct benefits of fitness. Effective interventions to address social isolation can be built around a compelling activity beyond mere social support. Given the accruing evidence of the impact of social isolation on population health, it is important to continue to refine social isolation conceptually, empirically, and as an issue, such that it can be better understood and addressed from public health and societal perspectives (Brummett et al., 2001). A more focused inquiry is also needed to better understand why SilverSneakers membership in itself has a positive impact on social isolation—in other words, to identify what features of a fitness program provide material social benefits to its participants. Future research might examine whether group membership in SilverSneakers facilitates social capital development. In addition, given that some SilverSneakers members may never have had a fitness membership before joining, future inquiry may evaluate later-life exercise adoption vis-à-vis social engagement.
Limitations
Due to the cross-sectional design of the study, it cannot be concluded that the intervention was the direct cause of the measured outcomes; the methodology only tests the direction and magnitude of relationships. The generalizability of the findings is limited because our sample was from a single Medicare Advantage insurer. There may also be selection bias effects due to the administration of the survey via e-mail and self-selection on the part of individuals in the sample. Although attempting to control for selection bias through the use of matching, the low survey response rate may also reduce generalizability. Future work should assess the causal impact of SilverSneakers on social isolation, loneliness, and health over time and should expand the study sample to improve generalizability.
Conclusion
This study offers initial evidence that a nationally available fitness program for older adults has a significant impact in reducing social isolation, which accrues to better health above and beyond physical activity levels alone. SilverSneakers members are less lonely as a result of having more social connections, and this reduced loneliness provides additional health benefits for participants in the program. Although more research is needed to flesh out the program aspects or mechanisms that lead to better health via lessened social isolation and loneliness, these findings are consistent with previously shown impacts of SilverSneakers on health through physical activity. The results of this study also reveal previously unexplored pathways by which the SilverSneakers program improves health through its effects on social isolation and loneliness.
Footnotes
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Drs. Rula and Kell are employees of Tivity Health, Inc., the provider of SilverSneakers, and own stock in the company. Dr. Coughlin is a member of the AARP Board of Directors.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Brady, D’Ambrosio, Felts, and Coughlin were supported by unrestricted grants from AARP and Tivity Health, Inc. to the MIT AgeLab.
ORCID iD: Samantha Brady  https://orcid.org/0000-0002-0461-7281
https://orcid.org/0000-0002-0461-7281
References
- American Association for Public Opinion Research. (2016). Response rate calculator V4.0. Retrieved from https://www.aapor.org/Education-Resources/For-Researchers.aspx
- Bassuk S. S., Glass T. A., Berkman L. F. (1999). Social disengagement and incident cognitive decline in community-dwelling elderly persons. Annals of Internal Medicine, 131, 165-173. doi: 10.7326/0003-4819-131-3-199908030-00002 [DOI] [PubMed] [Google Scholar]
- Benyamini Y. (2011). Why does self-rated health predict mortality? An update on current knowledge and a research agenda for psychologists. Psychology & Health, 26, 1407-1413. doi: 10.1080/08870446.2011.621703 [DOI] [PubMed] [Google Scholar]
- Brummett B. H., Barefoot J. C., Siegler I. C., Clapp-Channing N. E., Lytle B. L., Bosworth H. B., . . . Mark D. B. (2001). Characteristics of socially isolated patients with coronary artery disease who are at elevated risk for mortality. Psychosomatic Medicine, 63, 267-272. doi: 10.1097/00006842-200103000-00010 [DOI] [PubMed] [Google Scholar]
- Cattan M., White M., Bond J., Learmouth A. (2005). Preventing social isolation and loneliness among older people: A systematic review of health promotion interventions. Ageing & Society, 25, 41-67. doi: 10.1017/s0144686x04002594 [DOI] [PubMed] [Google Scholar]
- Cordier T., Song Y., Cambon J., Haugh G. S., Steffen M., Hardy P., . . . Renda A. (2018). A bold goal: More healthy days through improved community health. Population Health Management, 21, 202-208. doi: 10.1089/pop.2017.0142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B., Laumann E. O., Schumm L. P. (2008). The social connectedness of older adults: A national profile. American Sociological Review, 73, 185-203. doi: 10.1177/000312240807300201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughlin J. F. (2017). The longevity economy: Unlocking the world’s fastest-growing, most misunderstood market. New York, NY: PublicAffairs. [Google Scholar]
- Dickens A. P., Richards S. H., Greaves C. J., Campbell J. L. (2011). Interventions targeting social isolation in older people: A systematic review. BMC Public Health, 11(1), Article 647. doi: 10.1186/1471-2458-11-647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders C. K. (2001). The performance of the full information maximum likelihood estimator in multiple regression models with missing data. Educational and Psychological Measurement, 61, 713-740. doi: 10.1177/0013164401615001 [DOI] [Google Scholar]
- Ertel K. A., Glymour M. M., Berkman L. F. (2008). Effects of social integration on preserving memory function in a nationally representative US elderly population. American Journal of Public Health, 98, 1215-1220. doi: 10.2105/ajph.2007.113654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findlay R. A. (2003). Interventions to reduce social isolation amongst older people: Where is the evidence? Ageing & Society, 23, 647-658. doi: 10.1017/s0144686x03001296 [DOI] [Google Scholar]
- Fratiglioni L., Wang H., Ericsson K., Maytan M., Winblad B. (2000). Influence of social network on occurrence of dementia: A community-based longitudinal study. The Lancet, 355, 1315-1319. doi: 10.1016/s0140-6736(00)02113-9 [DOI] [PubMed] [Google Scholar]
- Golden J., Conroy R. M., Bruce I., Denihan A., Greene E., Kirby M., Lawlor B. A. (2009). Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. International Journal of Geriatric Psychiatry, 24, 694-700. doi: 10.1002/gps.2181 [DOI] [PubMed] [Google Scholar]
- Grembowski D., Patrick D., Diehr P., Durham M., Beresford S., Kay E., Hecht J. (1993). Self-efficacy and health behavior among older adults. Journal of Health and Social Behavior, 34, 89-104. doi: 10.2307/2137237 [DOI] [PubMed] [Google Scholar]
- Hajek A., Brettschneider C., Mallon T., Ernst A., Mamone S., Wiese B., . . . König H. (2017). The impact of social engagement on health-related quality of life and depressive symptoms in old age—Evidence from a multicenter prospective cohort study in Germany. Health and Quality of Life Outcomes, 15(1). doi: 10.1186/s12955-017-0715-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall-Lande J. A., Eisenberg M. E., Christenson S. L., Neumark-Sztainer D. (2007). Social isolation, psychological health, and protective factors in adolescence. Adolescence, 42, 265-286. [PubMed] [Google Scholar]
- Hamar B., Coberley C. R., Pope J. E., Rula E. Y. (2013). Impact of a senior fitness program on measures of physical and emotional health and functioning. Population Health Management, 16, 364-372. doi: 10.1089/pop.2012.0111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herring M. P., Puetz T., O’Connor P., Dishman R. (2012). Effect of exercise training on depressive symptoms among patients with a chronic illness: A systematic review and meta-analysis of randomized controlled trials. Archives of Internal Medicine, 172, 101-111. doi: 10.1001/archinternmed.2011.696 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J. (2017). The potential public health relevance of social isolation and loneliness: Prevalence, epidemiology, and risk factors. Public Policy & Aging Report, 27, 127-130. doi: 10.1093/ppar/prx030 [DOI] [Google Scholar]
- Holt-Lunstad J., Smith T. B., Baker M., Harris T., Stephenson D. (2015). Loneliness and social isolation as risk factors for mortality. Perspectives on Psychological Science, 10, 227-237. doi: 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Hooper D., Coughlan J., Mullen M. (2008). Structural equation modelling: Guidelines for determining model fit. Electronic Journal of Business Research Methods, 6, 53-60. [Google Scholar]
- Hu L., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1-55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hughes M. E., Waite L. J., Hawkley L. C., Cacioppo J. T. (2004). A short scale for measuring loneliness in large surveys. Research on Aging, 26, 655-672. doi: 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacus S., King G., Porro G. (2017). CEM: Coarsened exact matching software. Available from https://gking.harvard.edu/cem
- Iliffe S., Kharicha K., Harari D., Swift C., Gillmann G., Stuck A. E. (2007). Health risk appraisal in older people 2: The implications for clinicians and commissioners of social isolation risk in older people. British Journal of General Practice, 57, 277-282. [PMC free article] [PubMed] [Google Scholar]
- Kanamori S., Takamiya T., Inoue S., Kai Y., Kawachi I., Kondo K. (2016). Exercising alone versus with others and associations with subjective health status in older Japanese: The JAGES Cohort Study. Scientific Reports, 6(1). doi: 10.1038/srep39151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khullar D. (2016, December 22). How social isolation is killing us. The New York Times. Retrieved from https://www.nytimes.com/2016/12/22/upshot/how-social-isolation-is-killing-us.html?_r=0
- Kim E. S., Kawachi I., Chen Y., Kubzansky L. D. (2017). Association between purpose in life and objective measures of physical function in older adults. JAMA Psychiatry, 74, 1039-1045. doi: 10.1001/jamapsychiatry.2017.2145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig G., Westlund R., George L., Hughes D., Blazer D., Hybels C. (1993). Abbreviating the Duke Social Support Index for use in chronically ill older adults. Psychosomatics, 34, 61-69. doi: 10.1016/S0033-3182(93)71928-3 [DOI] [PubMed] [Google Scholar]
- Kraut R., Patterson M., Lundmark V., Kiesler S., Mukophadhyay T., Scherlis W. (1998). Internet paradox: A social technology that reduces social involvement and psychological well-being? American Psychologist, 53, 1017-1031. doi: 10.1037//0003-066x.53.9.1017 [DOI] [PubMed] [Google Scholar]
- Lampinen P., Heikkinen R., Kauppinen M., Heikkinen E. (2006). Activity as a predictor of mental well-being among older adults. Aging & Mental Health, 10, 454-466. doi: 10.1080/13607860600640962 [DOI] [PubMed] [Google Scholar]
- Lewallen S., Courtright P. (1998). Epidemiology in practice: Case-control studies. Community Eye Health Journal, 11(28), 57-58. [PMC free article] [PubMed] [Google Scholar]
- Lubben J., Gironda M. (2004). Measuring social networks and assessing their benefits. Social networks and social exclusion: Sociological and policy perspectives, 20-34. [Google Scholar]
- Luo Y., Hawkley L. C., Waite L. J., Cacioppo J. T. (2012). Loneliness, health, and mortality in old age: A national longitudinal study. Social Science & Medicine, 74, 907-914. doi: 10.1016/j.socscimed.2011.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley E., Blissmer B., Marquez D. X., Jerome G. J., Kramer A. F., Katula J. (2000). Social relations, physical activity, and well-being in older adults. Preventive Medicine, 31, 608-617. doi: 10.1006/pmed.2000.0740 [DOI] [PubMed] [Google Scholar]
- Morrato E. H., Hill J. O., Wyatt H. R., Ghushchyan V., Sullivan P. W. (2007). Physical activity in U.S. adults with diabetes and at risk for developing diabetes, 2003. Diabetes Care, 30, 203-209. doi: 10.2337/dc06-1128 [DOI] [PubMed] [Google Scholar]
- Nguyen H. Q., Ackermann R. T., Maciejewski M., Berke E., Patrick M., Williams B., LoGerfo J. P. (2008). Managed-Medicare health club benefit and reduced health care costs among older adults. Preventing Chronic Disease, 5(1), A14. [PMC free article] [PubMed] [Google Scholar]
- Nguyen H. Q., Maciejewski M. L., Gao S., Lin E., Williams B., Logerfo J. P. (2008). Health care use and costs associated with use of a health club membership benefit in older adults with diabetes. Diabetes Care, 31, 1562-1567. doi: 10.2337/dc08-0624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz H. (2011). Crossing new frontiers: Benefits access among isolated seniors (National Center for Benefits Outreach and Enrollment). National Council on Aging; Retrieved from https://www.ncoa.org/wp-content/uploads/crossing-new-frontiers.pdf [Google Scholar]
- Pentell M., Rehkopf D., Jutte D., Syme S. L., Balmes J., Adler N. (2013). Social isolation: A predictor of mortality comparable to traditional clinical risk factors. American Journal of Public Health, 103, 2056-2062. doi: 10.2105/ajph.2013.301261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perissinotto C. M., Cenzer I. S., Covinsky K. E. (2012). Loneliness in older persons. Archives of Internal Medicine, 172, 1078-1084. doi: 10.1001/archinternmed.2012.1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- PRNewswire. (2016, December 6). AARP foundation draws attention to social isolation with the launch of Connect2Affect. AARP Press Room; Retrieved from https://press.aarp.org/2016-12-07-AARP-Foundation-Draws-Attention-to-Social-Isolation-with-the-Launch-of-Connect2Affect [Google Scholar]
- Putnam R. D. (2007). Bowling alone: The collapse and revival of American community. New York, NY: Simon & Schuster. [Google Scholar]
- Rejeski W. J., Mihalko S. L. (2001). Physical activity and quality of life in older adults. The Journals of Gerontology Series A: Biological Sciences & Medical Sciences, 56(Suppl.), 23-35. doi: 10.1093/gerona/56.suppl_2.23 [DOI] [PubMed] [Google Scholar]
- Russell D. W. (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66, 20-40. doi: 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Shankar A., McMunn A., Banks J., Steptoe A. (2011). Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychology, 30, 377-385. [DOI] [PubMed] [Google Scholar]
- Shaw J. G., Farid M., Noel-Miller C., Joseph N., Houser A., Asch S. M., . . . Flowers L. (2017). Social isolation and Medicare spending: Among older adults, objective isolation increases expenditures while loneliness does not. Journal of Aging and Health, 29, 1119-1143. doi: 10.1177/0898264317703559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiovitz-Ezra S., Leitsch S. A. (2010). The role of social relationships in predicting loneliness: The national social life, health, and aging project. Social Work Research, 34, 157-167. doi: 10.1093/swr/34.3.157 [DOI] [Google Scholar]
- Singh A., Misra N. (2009). Loneliness, depression and sociability in old age. Industrial Psychiatry Journal, 18, 51-55. doi: 10.4103/0972-6748.57861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith H. J., Tyler T. R. (1997). Choosing the right pond: The impact of group membership on self-esteem and group-oriented behavior. Journal of Experimental Social Psychology, 33, 146-170. doi: 10.1006/jesp.1996.1318 [DOI] [Google Scholar]
- Steptoe A., Shankar A., Demakakos P., Wardle J. (2013). Social isolation, loneliness, and all-cause mortality in older men and women. Proceedings of the National Academy of Sciences, 110, 5797-5801. doi: 10.1073/pnas.1219686110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valtorta N. K., Kanaan M., Gilbody S., Ronzi S., Hanratty B. (2016). Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. Heart, 102, 1009-1016. doi: 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner C. B., Roberts A. R., Jeanblanc A. B., Adams K. B. (2017). Coping resources, loneliness, and depressive symptoms of older women with chronic illness. Journal of Applied Gerontology. doi: 10.1177/0733464816687218 [DOI] [PubMed] [Google Scholar]


