Abstract
Background
Gestational diabetes mellitus (GDM) - a transitory form of diabetes induced by pregnancy - has potentially important short and long-term health consequences for both the mother and her baby. There is no globally agreed definition of GDM, but definition changes have increased the incidence in some countries in recent years, with some research suggesting minimal clinical improvement in outcomes. The aim of this qualitative systematic review was to identify the psychosocial experiences a diagnosis of GDM has on women during pregnancy and the postpartum period.
Methods
We searched CINAHL, EMBASE, MEDLINE and PsycINFO databases for studies that provided qualitative data on the psychosocial experiences of a diagnosis of GDM on women across any stage of pregnancy and/or the postpartum period. We appraised the methodological quality of the included studies using the Critical Appraisal Skills Programme Checklist for Qualitative Studies and used thematic analysis to synthesis the data.
Results
Of 840 studies identified, 41 studies of diverse populations met the selection criteria. The synthesis revealed eight key themes: initial psychological impact; communicating the diagnosis; knowledge of GDM; risk perception; management of GDM; burden of GDM; social support; and gaining control. The identified benefits of a GDM diagnosis were largely behavioural and included an opportunity to make healthy eating changes. The identified harms were emotional, financial and cultural. Women commented about the added responsibility (eating regimens, appointments), financial constraints (expensive food, medical bills) and conflicts with their cultural practices (alternative eating, lack of information about traditional food). Some women reported living in fear of risking the health of their baby and conducted extreme behaviours such as purging and starving themselves.
Conclusion
A diagnosis of GDM has wide reaching consequences that are common to a diverse group of women. Threshold cut-offs for blood glucose levels have been determined using the risk of physiological harms to mother and baby. It may also be advantageous to consider the harms and benefits from a psychosocial and a physiological perspective. This may avoid unnecessary burden to an already vulnerable population.
Keywords: Gestational diabetes mellitus, Systematic review, Qualitative, Diagnostic impacts
Background
Gestational diabetes mellitus (GDM) is diagnosed by elevated blood glucose in pregnancy though the definition has changed repeatedly since its first description in the 1960’s [1, 2]. The most frequently reported perinatal consequence of GDM is macrosomia (usually defined as a neonate weighing over 4 kg) which can increase the risk of caesarean section and shoulder dystocia. For the mother, there are also potential longer-term consequences including an increased risk of type 2 diabetes post-pregnancy and/or in later life [3]. The investigators of a large international Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study aimed to identify a cut-point in the continuum to decide the blood glucose level (BGL) thresholds that should be used to define GDM [4]. However, a definitive cut-point was not identified and using the HAPO data the International Association of the Diabetes and Pregnancy Study Groups (IADSPG) consensus panel recommended a BGL threshold associated with the risk of adverse infant outcomes (such as risk of macrosomia, excess infant adiposity and neonatal hyperinsulinemia) [5]. This change was controversial, and there is currently a lack of an agreed standard for diagnosing high blood glucose in pregnancy.
Pregnancy can be a vulnerable period when a woman is adapting and responding to changes in body perceptions, such as loss of strength or fitness, which can result in reduced self-esteem and depression [6]. Many women report depression and anxiety during pregnancy which often includes worry for the baby’s wellbeing [7, 8]. A diagnosis of a health condition such as GDM could have a detrimental effect on a pregnant woman’s quality of life due to fears that the illness may affect her and/or her baby [9]. This has potential to convert pregnancy, a natural process, into one associated with risks, ill-health and increased surveillance [10]. Understanding a women’s response to the GDM diagnosis and its psychological impact has emerged as an important issue [11]. Some studies report women describing the initial response as one of ‘shock’ [12, 13], ‘sadness’ and ‘guilt’ [13]. A women’s acceptance of risk and fear of complications is likely to influence the acceptability of various interventions. Therefore, it is imperative to amalgamate the findings of these studies to synthesise the array of potential psychosocial consequences of a diagnosis of GDM.
In many countries the prevalence of GDM is rising [14–16]. Some of this is due to the increasing age at which women are becoming pregnant, an increase in obesity amongst women, more testing during pregnancy, and better recording during pregnancy. However, much of the rise has occurred since 2013 when some countries adopted the new IADPSG criteria and testing regimen for gestational diabetes. This resulted in the anomalous position that two women in two countries with exactly the same glucose levels may or may not be diagnosed with GDM depending on the country’s definition. Caution had been previously raised that the new IADPSG definition would increase prevalence of women diagnosed with GDM by two-to-three-fold [17].
Despite a significant increase in prevalence of GDM after the introduction of the new IADPSG criteria [15, 16], some pre-post studies suggest negligible clinical improvement in the adverse outcomes measured [17, 18]. Findings from a qualitative study of 19 women of different cultural backgrounds investigating women’s experiences of a GDM diagnosis reported that the diagnostic criteria itself was viewed as ‘confusing’ by some women and treatment for their ‘borderline’ condition unnecessary [19].
Although multiple studies have considered the impact of a diagnosis of GDM, a systematic review to synthesise the evidence around the emotional impact of a diagnosis at different stages, i.e. time of diagnosis, after diagnosis, at the delivery of the baby, and post-delivery, is lacking. The findings could inform healthcare clinicians of women’s attitudes and the consequences of a diagnosis and illuminate potential opportunities to provide support and advise. Therefore, in this systematic review, we aim to synthesise the evidence of the psychosocial experiences a diagnosis of GDM has on women during pregnancy and the postpartum period.
Methods
We followed the Enhancing Transparency in Reporting the Synthesis of Qualitative Research Guidelines (ENTREQ; Additional file 1: Table S1) [20]. We included primary studies published in peer-review journals that:
included pregnant women with a current diagnosis or women with a history of GDM;
provided qualitative data on the psychosocial experiences of a diagnosis of GDM on women across any stage of pregnancy and/or the postpartum period; and
where participants have provided an account of their experience or perspective of living with GDM
No restrictions were placed on country, written language, or year of publication.
Studies were excluded, if:
the primary aim was to identify barriers and/or facilitators to service as these focused on the management of GDM rather than the GDM diagnosis; or
participants were women diagnosed with diabetes before pregnancy
Abstracts, letters, editorials and commentaries were also excluded.
Search methods for identification of studies
The search strategy (MEDLINE version provided in the Additional file 1) was developed using a combination of Medical Subject Headings terms centred around three key areas: i) gestational diabetes mellitus ii) diagnostic testing for gestational diabetes mellitus and iii) patient experiences. The Systematic Review Accelerator software was used to translate the search strategy for each of the different databases and to remove duplicated articles [21]. We searched CINAHL, EMBASE, MEDLINE and PsycINFO databases from inception to April 2018. Forward and backward citation searching of included studies was conducted.
Selection process
A single reviewer (LC) screened the titles and abstracts of retrieved references using Endnote Version X7.7.1. Potentially eligible full-texts were independently reviewed by LC and RS with conflicts resolved via discussion. Two full-text studies published in Portuguese were first translated using Google Translate and then validated by a researcher with both spoken and written Portuguese language skills located within our research network.
Data extraction
All data labelled as results or findings including themes, categories, theories were extracted and imported into NVivo Version 12 by LC. Study characteristics were extracted by LC which included study location, reported research aims, study design, methodology and the analytical approach. Information about the diagnostic criteria used to determine GDM in women was also extracted.
Data synthesis and analysis
To synthesise the findings, we used a thematic synthesis described by Thomas and Harden [22]. Thematic synthesis has the potential for conclusions to be drawn based on common aspects across otherwise heterogeneous studies and produce findings that directly inform health practitioners [22, 23]. Coding was inductive, with codes derived from the data. First, extracted text relevant to patient experiences and perspectives was coded line by line. A subset of studies (n = 5) were coded independently by LC and RS to develop a coding framework. Disagreements were resolved by discussion. LC and RS coded a further subset (n = 4) and established an inter-rater reliability of Kappa = 0.87. Following this, LC applied the coding framework to the remaining studies. New codes were iteratively developed as new concepts arose.
Second, relationships between the codes were identified by LC to form the basis of descriptive themes across the studies. Similar codes were grouped to generate themes and less frequently used codes were classified into sub-themes. In the final stage, analytical themes were developed to ‘go beyond’ the primary studies to amalgamate and interpret the findings. The relevant quotes to support each theme were tabulated.
Quality assessment
As recommended by the Cochrane Qualitative Research Methods Group, we assessed the quality of the included studies using the Critical Appraisal Skills Programme Qualitative Checklist (CASP). This tool uses a systematic approach to appraise three key areas: study validity, an evaluation of methodological quality, and an assessment of external validity [24]. Critical appraisal was conducted by one reviewer (LC) for all studies, with second reviewer appraisal (RS) for a sub-set of included papers. The findings from the two reviewers were compared and any contrasting items were discussed and re-reviewed.
Results
The search identified 840 studies. After deduplication and screening of titles and abstracts 88 full-text articles were assessed (Fig. 1). Seven further articles were identified through citation searching. Data were extracted from 41 studies meeting eligibility criteria and were included in the review [11–13, 19, 25–61].
Fig. 1.
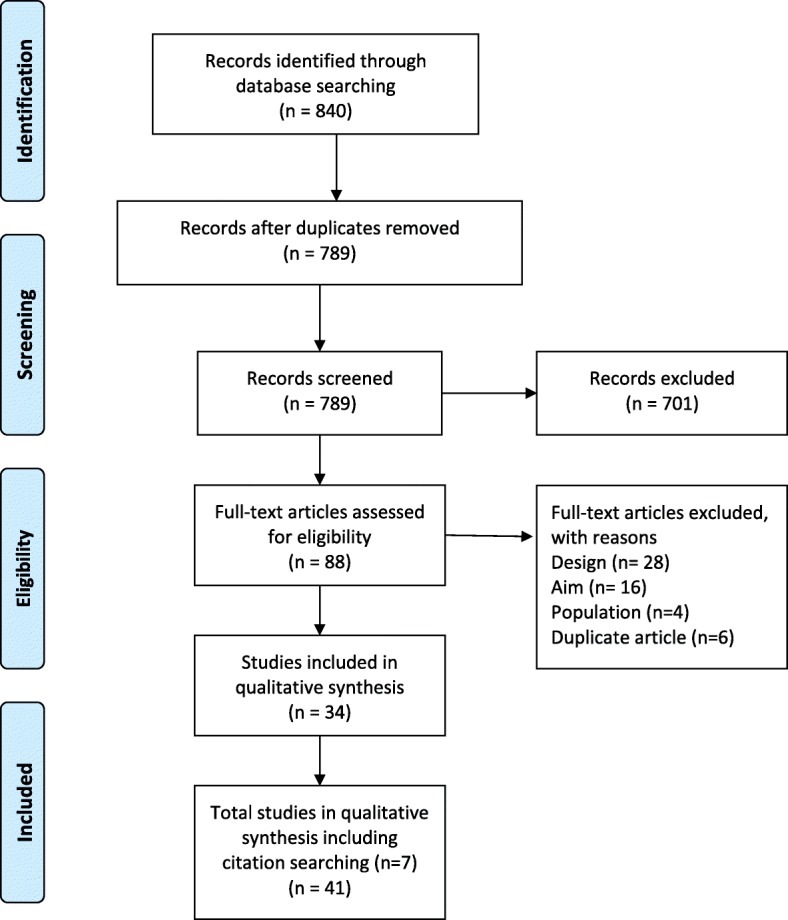
Prima flow diagram
Study characteristics
The studies reflected a variety of sampling methods and data collection methods. For example, interviews were conducted in 34 studies [10, 12, 13, 25, 27, 28, 30–32, 34–36, 38–50, 52–58, 60, 61], focus group methods were used in three [19, 32, 37], and interviews and focus groups were used in two studies [29, 51]. Two studies used a mixed method approach [26, 59]. The sample sizes ranged from 6 to 57 women. Eighteen studies were conducted in Europe, 10 in Australia, 9 in North America, and 2 studies each in Asia and South America. Table 1 details the characteristics of the included studies.
Table 1.
Characteristics of included studies
| Author/Date/country | Aim of study | Method of data collection/point of data collection | Conceptual basis underlying the study (e.g. thematic analysis, grounded theory) | Participants/Recruitment/N/Population description |
|---|---|---|---|---|
| Studies collecting data during pregnancy | ||||
| Carolan/2013 [29] Australia | To understand the experiences of women self-managing GDM | Phone interview, face-to-face interview and focus group | Thematic analysis |
Pregnant women with a diagnosis of GDM/purposive sample/ N = 15 Caucasian, Asian, South Asian, Indian and Arabic |
| Carolan-Olah et al./2017 [12] Australia | To explore the experiences of a group of Hispanic women of Mexican origin who had been diagnosed with GDM | Semi-structured interviews | Thematic analysis |
Pregnant Hispanic women with a diagnosis of GDM/convenience sample/ N = 18 Hispanic women of Mexican origin |
| Doran/ 2008 [30] Australia | To explore lifestyle changes during pregnancy and post-partum with women who had experienced a pregnancy complicated by GDM | Interviews | Thematic analysis |
Pregnant women with GDM and women who has accessed centres for GDM management within the past 18 months/purposive sample/ N = 38 Pacific Islanders |
| Hjelm et al./2005 [41] Sweden | The aim of the present study was to compare beliefs about health and illness in women with GDM born in Swedish and in the Middle East | Semi-structured interviews | Thematic analysis |
Pregnant women with GDM Interviews conducted at weeks 34–38/consecutive sample/ N = 27 (Sweden = 13) Swedish/Middle Eastern |
| Persson et al./2010 [13] Sweden | To describe pregnant women’s experiences of acquiring and living with GDM during pregnancy | Semi-structured interviews | Grounded theory |
Pregnant women with GDM/convenience sample N = 10 Swedish |
| Kaptein et al./2015 [45] Canada | To gain insight into the reactions and experiences of women from multiple ethnic background diagnosed with GDM | Semi-structured telephone interviews | Thematic analysis |
Pregnant women with a diagnosis of GDM/consecutive sample/ N = 19 Non-Caucasian (79%) |
| Trutnovsky et al./2012 [59] Austria | To explore concerns, treatment motivation, mood state, QoL, and treatment satisfaction of women treated for GDM. | Semi-structured interviews and survey | Thematic analysis |
Pregnant women with GDM/convenience sample/ N = 45 Caucasian |
| Wah et al./2018 [60] Australia | To explore the understanding and self-management experiences of GDM among Chinese migrants | Semi-structured face-to-face interviews | Thematic analysis |
Pregnant migrants of China ethnicity residing in Australia with a diagnosis of GDM/convenience sample/ N = 18 Chinese |
| Salomon et Soares/2004 [55] Portugal | To understand how gestational diabetes patients experience the impact of this diagnosis during pregnancy and of significance they attribute to the disease | Semi-structured interviews | Content analysis |
Pregnant women with a diagnosis of GDM/unclear N = 9 Not reported |
| Hui et al./2014 [44] Canada | To explore the stress and anxiety experienced during dietary management for women with GDM |
Food choice map semi structured interview Interviews conducted at 26–28 weeks gestation |
Not specifically reported, described as thematic Themes |
Pregnant women with diagnosis of GDM/purposive sample/ N = 30 Caucasian, Asian, African, and Aboriginal |
| Hjelm et al. 2012 [42] Sweden | Explore beliefs about health and illness in women with gestational diabetes living in Sweden and born in Sweden or Africa |
Semi-structured interviews Interviews conducted at weeks 34–38 |
Categories with description extract |
Pregnant women with a diagnosis of GDM/consecutive sample/ N = 23 (N = 13, Sweden) Swedish/African |
| Hjelm et al. 2008 [43] Sweden | To explore beliefs about health, illness and health care in women with gestational diabetes mellitus (GDM) managed in two different organisations based on diabetology or obstetrics |
Semi-structured interviews Interviews conducted at gestational weeks 34–38 |
Thematic analysis |
Women with a diagnosis of GDM/consecutive sample/ N = 23 Swedish/African |
| Hirst et al. 2012 [37] Vietnam | To determine attitudes and health behaviours of pregnant women with GDM in Vietnam | Focus groups | Thematic analysis |
Women with a diagnosis of GDM/purposive sample (Women sampled at gestational ages 28–38 weeks) N = 34 Vietnamese |
| Han et al. 2015 [36] Australia | To explore women’s experiences after being diagnosed with borderline GDM | Semi-structured interviews |
Content analysis Categories |
Women with a diagnosis of borderline GDM Borderline GDM as a positive 50 g OGCT (1 h venous plasma glucose ≥7.8 mmol/L) followed by abnormal oral75g OGTT (fasting venous plasma glucose < 5.5 mmol/L and a 2 h glucose < 7.8 mmol/L) Eligible if they were participants in the IDEAL study/purposive sample/ N = 22 Caucasian and Asian |
| Ge, Wikby et al. 2016 [35] Sweden | To explore beliefs about illness and health and self-care behaviour among urban Chinese women | Semi-structured interviews |
Content analysis Categories |
Pregnant women with diagnosis of GDM, 34-38th gestational weeks/purposive sample/ N = 17 Chinese |
| Ge, Albin et al. 2016 [34] Sweden | To explore beliefs about health and illness and health-related behaviours among Chinese women with GDM in a Chinese sociocultural context. | Semi-structured interviews |
Content analysis Categories |
Pregnant women with a diagnosis of GDM, 34-38th gestational weeks/purposive sample/ N = 15 Chinese |
| Bandyopadhyay et al. 2011 [28] Australia | To explore the experiences and understanding of South Asian women after a diagnosis of GDM | Face-to-face interviews |
Not specifically reported, described as thematic analysis Themes |
South Asian women diagnosed with GDM/convenience sample/ N = 17 South Asian |
| Araujo et al./2013 [26] Brazil | To understand the significance of the experiences of women with gestational diabetes mellitus |
Open interviews and participant drawings 4 women in 1st trimester, 3 in 2nd trimester & 3 in 3rd trimester |
Not specifically reported, described as thematic analysis |
Women with GDM diagnosis/convenience sample/ N = 12 South American |
| Evan et Brien 2005 [12] Canada | To gain an in-depth understanding of GDM as experienced by pregnant women |
Interviews Interviews conducted prior to delivery and 6–8 weeks postpartum |
Thematic analysis |
Women with GDM diagnosis/purposive sample/ N = 12 Caucasian |
| Studies collecting data within the 1st 12 months post-natal | ||||
| Bandyopadhyay et al./2015 [27] Australia | To capture in-depth exploration of the experiences and perspectives on postpartum glucose tolerance test screening of South Asian women diagnosed with GDM |
Interviews Interviews were conducted antenatally after diagnosis, after birth, 9 weeks to 52 weeks |
Thematic analysis |
South Asian women with diagnosis of GDM/convenience sample/ N = 40 South Asian |
| Draffin et al./2016 [19] United Kingdom | To explore the concerns, needs and knowledge of women diagnosed with GDM | Focus groups | Thematic analysis |
Pregnant women with a diagnosis of GDM or a history of GDM within past 12 months/convenience sample/ N = 19 White, Black African, Pakistani Latin American, Bangladeshi, Indian |
| Doran et Davis 2010 [31] Tongan | To explore GDM in Tonga, with women who experienced GDM and health professionals who worked in the GDM/diabetes area | Semi-structured face to face interviews |
Not specifically reported, described as thematic analysis Themes |
Women who had experienced GDM in the previous 12 months /unclear/ N = 11 Pacific Islanders |
| Figueroa Gray et al./2017 [33] USA | To foreground women’s experience with insulin and oral hypoglycemic agents. | Focus group | Thematic analysis |
Women with GDM history and completed at least one prescription for insulin or oral hypoglycaemic medication during pregnancy within past 3 years/purposive sample/ N = 16 Caucasian, African American, Asian, Hispanic or Latina |
| Hjelm et al. 2009 [40] Sweden | To explore beliefs about health and illness 3 month postpartum in women born in Sweden and the Middle East, and to study whether they perceive gestational diabetes mellitus as a prediabetic condition | Interviews |
Headings and descriptions Divided into Middle-Eastern born and Swedish born women |
Women 3 months postpartum who had previously had GDM /consecutive sample/ N = 27 Swedish and Middle Eastern |
| Hjelm et al./2012 [42] Sweden | To explore the development over time of belief about health, illness and health care in migrant women with gestational diabetes born in the Middle East and living in Sweden |
Semi-structured interviews Interviews conducted at weeks 34–38, three and 14 months after delivery |
Content analysis |
Middle Eastern women with a diagnosis of GDM/consecutive sample/ N = 14 Swedish and Middle Eastern |
| Hjelm et al. 2018 [39] Sweden | To explore the development over time, during and after pregnancy, of beliefs about health, illness and healthcare in migrant women with GDM born in Africa living in Sweden |
Semi-structured Interviews conducted in gestational weeks 34–38 and 3 and 14 months after delivery |
Framework analysis using the Health Belief Model |
Women with a diagnosis of GDM/convenience sample/ N = 9 African |
| Kilgour et al./2015 [46] Australia | To explore and assess women’s communication experiences of postnatal GDM follow-up |
Interviews Interviews at 12–16 weeks after birth |
Thematic analysis |
Women with GDM diagnosis/“theoretical sample”/ N = 13 Caucasian, Asian and Indian |
| Lawson et Rajaram/1994 [47] USA | To explore the meaning women attach to GDM |
Semi-structured interviews Interviews once prenatally and again at 6 weeks |
Thematic analysis |
Women with diagnosis of GDM/purposive sample/ N = 17 Caucasian, Black and Asian-American |
| Neufeld/2011 [49] Canada | To describe how aboriginal women in an urban setting perceive dietary treatment recommendations associated with GDM | Interviews | Thematic analysis |
Aboriginal women with GDM or a previous diagnosis of GDM within past 5 years/convenience sample/ N = 29 Aboriginal |
| Svensson et al./2018 [56] Denmark | To examine how Danish women with a history of GDM experience the transition from a GDM-affected pregnancy to the postpartum period |
Interviews Interviews within 3–5 months after delivery |
Content analysis Themes |
Women diagnosed with GDM/convenience sample/ N = 6 Caucasian |
| Tang et al./2015 [57] USA | To gain insight of Hispanic and African-American women’s views on prevention of T2DM after GDM. | Semi-structured interviews | Thematic analysis |
Women with a history of GDM (within 12 months of delivery at the time of initial contact)/purposive sample/ N = 23 African-American |
| Whitty-Rogers et al./2016 [61] Canada | To explore Mi’kmaq women’s experiences with GDM. | Conversational interviews |
Hermeneutic phenomenology Themes |
Mi’kmaq women with history of GDM/purposive and snowballing sample/ N = 9 Aboriginal |
| Studies collecting data at follow up screening for Type II diabetes | ||||
| Abraham et Wilk/2014 [25] USA | To explore the lived experiences of women in rural communities with GDM and potentially gain insight into the low reported return rates for PPG testing | Semi-structured interviews |
Phenomenological approach Themes |
Women with a history of GDM in the last 2 to 5 years/purposive and snowballing sample/ N = 10 Caucasian |
| Eades et al./2018 [32] UK | To explore experiences, knowledge and perceptions of women with GDM to inform the design of interventions to prevent or delay Type 2 diabetes | Semi-structured interviews | Theoretical framework – Self-Regulation Themes |
Women with history of GDM diagnosis, within 1-year post delivery/convenience sample/ N = 16 Caucasian, Asian, Black and African |
| Nielsen et al./2015 [50] Denmark | To improve our understanding of how women with gestational diabetes experience the treatment and care offered by a regional health service. To understand how the women’s experiences influenced their subsequent participation in follow-up screening. | Semi-structured interviews | Thematic analysis |
Women with a previous diagnosis of GDM within 1–2 years after birth/convenience sample/ N = 7 Caucasian and Asian |
| Parsons et al./2018 [51] UK | To describe the experiences of women from a demographically diverse population of their GDM and GDM care, to help inform healthcare delivery for women both during and after pregnancy | Interviews and focus groups | Framework analysisThemes |
Women with a previous diagnosis of GDM (within past 5 years)/purposive sample/ N = 50 Black, Caucasian, and Asian |
| Razee et al./2010 [54] Australia | To explore the beliefs, attitudes, social support, environmental influences and other factors related to diabetes risk behaviours among Arabic, Cantonese/Mandarin, and English speaking women with recent GDM | Semi-structured interviews | Not specifically reported, described as thematic analysis |
Women who had completed a GDM pregnancy in the previous 6–36 months/purposive sample/ N = 57 Middle Eastern, Chinese and White Australian |
| Rafii et al./2017 [53] Iran | To understand Iranian women’s experiences in diabetes screening after childbirth |
Semi-structured interviews Interviews at 6–21 months postpartum |
Grounded theory methodology Themes and sub-themes |
Women with previous GDM diagnosis /purposive sample/ N = 22 Asian |
| Tierney et al./2015 [58] Ireland | To assess the lifestyle behaviours undertaken by a group of women both during and after their GDM pregnancy | Semi-structured interview | Thematic analysis |
Women with a history of GDM in the previous 3.6–6.6 years/convenience sample/ N = 13 Not reported |
| Pennington et al./2017 [52] Australia | To explore the views of GPs and women who have had GDM | Semi-structured interviews | Content analysis |
Women with a history of GDM/purposive sample/ Timeframe not reported N = 16 Not reported |
| Lie et al./2013 [48] United Kingdom | To explore factors influencing post-natal health behaviours following the experience of gestational diabetes | Semi-structured interviews | Framework analysis |
Women with a history of GDM within the last 2 years/purposive sample/ N = 37 Caucasian and non- Caucasian |
Quality appraisal
Most studies were assessed as high quality (Additional file 1: Table S2). Study aims were stated in all but one study [47]. As the purpose of all included studies was to explore or gain knowledge, opinions or attitudes about GDM, the qualitative methods employed in all the studies were appropriate. Different study designs were used and in some cases the lack of reporting details made judgments of the appropriateness of study methods difficult. Data were collected in a way that addressed the research issue, however, a few authors did not discuss or report details such as saturation of data [31, 47, 56, 59]. The relationship between researcher and participants was considered in only two studies [51, 61]. Appropriateness of data analysis was assessed as “unclear” when there was a lack of details about how themes were derived.
Thematic analyses
Eight themes were generated from the data synthesis: 1. initial psychological impact; 2. communicating the diagnosis; 3. knowledge of GDM; 4. risk perception; 5. management of GDM; 6. burden of GDM; 7. social support; and 8. gaining control. The relevant quotes to support each theme are presented in Table 2.
Table 2.
Data to support identified themes
| No | Theme | Supporting data |
|---|---|---|
| 1 | Initial psychological impact |
‘I was very surprised and very upset to be diagnosed. I felt a little bit of a failure.’ [31] ‘You actually feel guilty, right? Because this baby hasn’t asked for this; and what if the baby comes out and has some kind of disease? Then it’s my fault.’ [58] ‘GDM was a hidden blessing for me... GDM can go away after you have the baby but diabetes is not so easily fixable …I am much more aware of [the] need to prevent it.’ [32] ‘It’s also good with my diabetes diet I ended up weighing pretty much the same at the end of the pregnancy as I did at the beginning.’ [31] |
| 2 | Communicating the diagnosis |
‘Like they don’t have time to sit there and talk to you about what to do about it [GDM], but they are always in a hurry [………] so I just don’t bring it up and they don’t bring it up; so you just get checked out and leave.’ [26] ‘They sent me off to the dietician and I came out depressed....I went “nuh - if I eat what you’re telling me”... and she was telling me I had to eat carbs with every meal. I knew it wouldn’t control my BSL [blood sugar level]...hadn’t they read the latest research about a high protein diet being more beneficial that a high carb diet? [32]. ‘scared that if the sugar was too high they would take the baby out [33]. ‘Nobody told me anything about type 2 diabetes...they were so focused on the immediate pregnancy problems; within a medical model...OK, if we don’t get it under control, we will just put you on insulin... just a drug solution.’ [32] ‘They [hospital dieticians] don’t have much information on for example some Chinese dishes, so I would go on the Internet and check if they’d raise my blood sugar. .. but even on the Internet, it’s hard to find information like that.’ [62] |
| 3 | Knowledge of GDM |
‘I thought it was the end of the world because I didn’t fully understand it’ [27]. ‘At first I thought: it must be because I ate a lot sweet, overweight ... but then I was talking to the girl, she said it must be family, right??’ [57] ‘My husband, he always knew me like this ... is ... healthy, without any illness. [...] Because he is kind of ignorant in these matters, you know. He thinks that diabetes ... that I’m dying! ... And my boy too, is half pensive, cautious, thinking I’m going to die.’ [57] ‘I did not know that rice can have that much sugar. That’s one thing really, really surprised me. I’m thinking that sugar normally comes from cakes and chocolate.’ [31] I’ve eaten something and I’ve thought my reading’s not going to be good after this and it’s been fine. So it was mainly getting my head around it’s not just the sugars. Like Special K for example. That was on my list of things that I could have and then the lady (educator) said, ‘What did you have for breakfast? And I said I had Special K. She said, ‘it obviously doesn’t work for you. So you either have to up your insulin, if you want to just keep eating Special K, or just stop eating it.’ [31] ‘You’d think, okay, well this will be good; this will be fine for me to eat. Then I will check my sugars 2 h later and it would not. I would be why? That’s not okay. It was disappointing, and it was definitely stressful, like it was just really not fun.’ [46] If the mother breastfeeds her baby the ‘diabetes factor’ may transmit to the baby and it’s no good. It may make the baby have the same disease afterwards’ [39] ‘I’m concerned about that (transmission of diabetes to the infant) of course’ [39] |
| 4 | Risk perception |
‘coming back as borderline gestational diabetes wasn’t such an issue as having full-blown diabetes...and I don’t worry about it.’ [38] ‘I’m afraid this diet won’t provide enough nutrients for the baby, but the doctor told me to do that’ [38] ‘since, after giving birth and everything’s back to normal so I’ve sort of been making up for lost time a little bit with all the chocolate I couldn’t have.’ [52] ‘It’s actually quite odd that during birth, they monitored everything closely, and as soon as I had delivered they served me a piece of white bread.’ [52] |
| 5 | Managing GDM |
‘It is frustrating still when you watch your carbs, you portion it and your reading is still high, almost every day.’ [46] ‘I’ve been doing everything right. My sugar is so unstable. The highest reading was 202 with my insulin. I have eaten the right foods, exercised, and tested my glucose levels four times a day. I had some high ones of 151. When my insulin dosages are increased, I am more depressed. I feel worthless.’ [49] ‘I really wanted to control it through my diet and exercise. I was strongly motivated to do all I could so I didn’t have to introduce another needle.... But when I went on insulin I relaxed.’ [32] ‘..my baby might die if I’m not on [a] diet.’ [39] ‘Well, you are deviant from others. It’s like a functional handicap in that aspect’ [15]. ‘I’m a full-time working mom, so I had to carry a little refrigerator with me with the insulin to work every day and on weekends to the restaurant and have to hide in the bathroom. It made me feel like I’m totally an illegal person.’ [35] |
| 6 | Burden of GDM |
‘The whole pressure with the whole everything, it really did affect me and I think it’s probably one of the worst times I’ve had in my life actually.’ [53] ‘I would have crashes where I’d be driving on the freeway, and I’m at a crazy low number, and I have to try to find some candy or something in my car. So it was very frustrating.’ [35] ‘because it is really ugly to have, in fact I wanted to have another baby and since I got this I do not want to anymore.’ [14] |
| 7 | Social support |
‘Well, I wouldn’t have done it without my partner like because he was like, “Up, eat now, insulin,” you know, and I would be, “Yeah, I’m going to get up in 20 min and I’m going to do this,” and he was like, “Now, eat, your insulin,” you know.’ [21] ‘he’s now cooking more for me and he’s healthier because he doesn’t, because if he’s going to eat junk food that’s just going to make me jealous. So he’s kind of trying to eat healthy as well for me.’ [31] ‘My mother-in-law phoned relatives and told the villagers that my baby was not healthy because I had GDM...’ [37] |
| 8 | Gaining control |
‘You have an active role and you can take charge of what’s going on rather than just roll along.’ [12] ‘I believe in not giving in to diabetes. I will take care of myself and control the diabetes.’ [49] ‘I looked at herbal remedies because that’s something that [laughing], you know, you think is quite safe [21] |
Initial psychological impact
When initially diagnosed with GDM, most women reported reactions such as self-blame, failure, fear, sadness, concern and confusion. Women often focused on the uncertainty of diagnostic prognosis and some considered it to be a life-altering experience. Some women felt lost and unsure what to do next. Often women felt an overwhelming sense of vulnerability and guilt. In some cases, the diagnosis was received positively and was viewed as an opportunity for lifestyle improvements. For example, some women viewed the diagnosis as a ‘wake up’ call and were grateful for the chance to intervene and potentially prevent adverse outcomes for their babies and themselves. Some women viewed gaining less weight than expected during their pregnancy as a benefit of having a GDM diagnosis.
Communicating the diagnosis
Communication with healthcare professionals (HCPs) and their families was a common theme throughout the findings of the included studies. Generally, the level and quality of communication with HCPs was mixed – with some women reporting positive and informative encounters, while others described brief encounters with overly technical language and unsupportive consultations. The main issues were limited time available to spend with the HCP, lack of continuity of care and lack of understanding about the role of the HCP at follow-up. In some instances, women felt that GDM was not a topic that HCPs were keen to discuss -‘the nurses, they never talked to me about my gestational diabetes’. [23] The level and quality of information provided was often conflicting, confusing or insufficient. Areas of contention were appropriate foods and the dietary changes that should be made.
Some women formed a dependency on HCPs to know what to do and on the electronic reminders for follow-up appointments and monitoring. Often women reported having no choice in treatment resulting in them feeling threatened and frustrated. Often women were automatically booked in for a caesarean section without consultation or lived in fear of this occurring. One woman referred to GDM as being over medicalised. Receiving limited information also prompted women to independently seek information about the impact and management of GDM from other sources such as the internet. However, some women found the internet limited for specific information or confusing.
Knowledge of GDM
Women had varying levels of understanding of GDM which impacted on their initial reaction to the diagnosis. Those who were able to explain the cause of GDM were able to process and accept the diagnosis more readily than those who had little understanding of GDM, or were confused as to how GDM occurred. Lack of knowledge also extended to and impacted on relatives. Some women stated that they would have preferred to be more prepared to receive the diagnosis by having early knowledge about the testing for diabetes. Women reported being on a steep learning curve, especially the onerous approach of dietary trial and error whereby women learnt what foods would increase their blood glucose level (BGL) and what food to avoid. Women also reported challenges in adopting new habits to manage their GDM, including understanding food labels and nutritional values of food. Often this required a trial and error approach. There was also a lack of understanding about the impact of GDM on their baby with some women believing it would be transmitted to their baby via breastmilk.
Risk perception
Women’s perception of risk were reported before the diagnosis of GDM, after they were diagnosed in pregnancy, and after the delivery. Some women attempted to understand their level of risk in context of family history. Some were very surprised by the diagnosis, especially if they were asymptomatic; and some women found it difficult to come to terms with the diagnosis. There was uncertainty about the severity of the condition. Some women considered the condition to be mild, downplaying the disease and believing that too much ‘fuss’ was being made about GDM and other women doubted the diagnosis and its seriousness. Women often discussed: the adverse effects that GDM would have on her baby; frustration that the focus was on risks to the baby and less so them; their worry about the consequences for the future; and questioned the impact of insulin on the baby. Women worried that their diet was too restrictive for their growing baby and would not provide the nutrients that the baby required. Some women held the view that GDM was a temporary condition and would disappear once the baby was born, and many women reverted to old eating habits after the baby’s birth. Often women referred to the birth as a ‘moment of truth’ or as an endpoint to their GDM. This was also reflected in the level of care that the women received after the birth of their baby.
Managing GDM
Dietary management-related stress was commonly reported amongst interviewed women and was experienced by both insulin and non-insulin users. Stress and frustrations often occurred as a consequence of an unexpected abnormal blood glucose reading following strict adherence to dietary advice. Maintaining stable BGL was an ongoing struggle and in some cases the burden proved too much, with a few women ceasing employment. Insulin users described the process as a ‘roller coaster’ as well as the emotional and physical discomfort of injecting, while non-insulin users often became obsessed with a well-controlled diet, with some women viewing this as a way to avoid the use of insulin. Conversely, some women felt relieved when they were transitioned onto insulin, as it reduced the need for dietary restriction.
Making lifestyle changes was considered stringent and restrictive by the majority of women, and for some required ‘major restructuring’ to their diet and daily routines to incorporate exercise. Some women reported extreme behaviours, including falsifying blood glucose readings, self-starvation and hiding their condition, including from family members. Often the impact of non-adherence to lifestyle changes resulted in guilt and belief that the baby would know they have cheated. Other pregnancy related ailments and the need to care for other children interfered with the ability to make the required changes. Women who had a specific culture-related diet discussed the impact and difficulty of applying or tailoring the dietary recommendations to their diet.
The key motivator to making required lifestyle changes, despite the associated hardships, was to minimise the risks to their unborn baby. Women prioritised the health of the baby over their own health and were willing to do anything to ensure that the health of their baby was not compromised. Over time, management of the GDM became a part of their normal routine for many women. However, some women expressed a desire to have a ‘normal’ pregnancy similar to their friends, discussing that a diagnosis of GDM made them feel as though their pregnancy was atypical, leading to defining their pregnancy as ‘abnormal’ or as an ‘illness’. For one woman, it made her feel like an ‘illegal’ person.
Burden of GDM
Women reported that a diagnosis of GDM came with extra responsibility, which added pressure whilst trying to juggle life commitments such as work, childcare, and daily living responsibilities. Monitoring and treating GDM placed burden on women’s daily routines and most woman agreed that taking BGL measurements was time consuming and disruptive. There was a constant need to prudently plan meals and co-ordinate the attendance at additional hospital appointments, all of which were considered time intensive, especially with travel and wait times. Women expressed that GDM consumed a lot of their thinking time e.g., ‘I think about diabetes everyday’ and felt that they had to acknowledge GDM all the time and became ‘super-conscious’. In some instances, women reported a GDM diagnosis took away some of the ‘joy of pregnancy’. One woman described her pregnancy as a ‘misfortune’. Women mentioned the financial burden of buying healthier food – ‘it would take lots of money just because it is so expensive to eat healthy’. [25] Women also considered the physical burden of GDM such as fatigue and the side effects of treatment such as insulin. There was a longer-term impact on family planning, where in some cases women decided not to have another child because they were fearful of enduring a similar restrictive and stressful pregnancy due to GDM.
Social support
Social support, including family and HCP support, was an important aspect for women during their experience of a GDM diagnosis. Changes in lifestyle often had an overflow effect, with other family members adopting healthier lifestyles. Women not in their country of birth, and without family, often reported feeling isolated and lonely. Disappointment and isolation were also expressed by some women when they perceived a lack of healthcare system support. This often occurred postnatally when the expectations of postpartum care were high, however, in reality, support was absent. In some cases, women were stigmatised by their families and in a few cases received undesirable feedback that they were not doing enough to protect their unborn child.
Gaining control
Control was a frequently used word when women described living with and managing a GDM diagnosis. Initially women reported a lack of control especially over their emotions, however, over time women transitioned from feeling like a victim of diabetes, to being active agents in controlling their GDM. The terms ‘balance’ and ‘adjustment’ were used to describe how some women tried to offset the strict compliance and active self-management with reducing their risk to their unborn baby and their own future risk of developing diabetes after pregnancy. Some women reported feeling empowered as their pregnancies progressed, especially when they gained more knowledge about GDM and what action they could take to accept and make sense of the diagnosis. Taking control included realising the changes that were required to their lifestyle, self-initiated care, and self-education. Often investigating alternative options, such as natural remedies outside those recommended by HCPs, provided women with some autonomy in managing their condition and some believed that it was a safer option to medication.
Discussion
Summary of main findings
This synthesis of the qualitative evidence of women’s experiences of being diagnosed with GDM highlighted the psychosocial consequences a diagnosis of GDM can have on women. The purported benefits of a GDM diagnosis identified from our review, were largely behavioural and included an opportunity to improve health, prevent excessive weight gain, control weight during pregnancy, and prompts to make healthy eating changes. However, the purported harms included the added responsibility (eating regimens, appointments), financial constraints (expensive food, medical bills), and conflicts with their cultural practices (alternative eating, lack of information about traditional food). The psychosocial consequences were wide reaching and often resulted in significant social isolation with women only sharing their diagnosis with partners. Furthermore, there were a few reports of over-medicalisation due to a GDM diagnosis, with the perception that HCPs were often authoritarian, focusing on physiological aspects, with little attempt to involve women in decision making. This is noteworthy considering a non-GDM pregnancy has already come under scrutiny as being over-medicalised with increasing levels of unnecessary intervention [62].
Women from studies included in our review frequently reported inconsistent information provision. Limited GDM information provision has been identified in another systematic review regarding healthcare seeking for GDM during the postpartum period [63]. In contrast, findings from another study which aimed to evaluate satisfaction with obtaining a diagnosis of GDM concluded that the majority of women were satisfied with their experience of being diagnosed [64]. Further, women in the latter study associated poor GDM control with perinatal complications and an increased risk of type 2 diabetes following pregnancy [64].
Another key finding from this review was low awareness of the potential risks of GDM, particularly in the long-term. Low health literacy levels could be one factor to explain knowledge deficits and understanding of GDM, especially given the sociodemographic diverse population included in this review. One study found that low literacy among disadvantaged women had a significant impact on their understanding of GDM information [65]. Other research found that women who live in an English-speaking country but primarily speak a non-English language, have lower rates of dietary awareness compared with their English speaking counterparts, and this may affect compliance to dietary interventions [66]. Therefore, it is important that new educational interventions are developed to target those with lower health literacy as well as cultural factors when diagnosing and managing multi-ethnic populations with GDM [66].
Interestingly, women with a borderline diagnosis of GDM did not seem as concerned as other women and in some cases were dismissive of the diagnosis and the potential consequences. Similarly, in a study which specifically included women with a borderline diagnosis of GDM, the majority of women reported that they were not worried by the diagnosis [67]. For some women, the potential transitory nature of GDM was emphasised and some reported that it didn’t seem like a real illness. The diagnostic criteria for GDM has previously been compared with the established criteria used to classify a condition as a disease. This comparison revealed disparity which Goer, in 1996, used to suggest that GDM did not pose a serious health risk, was neither easily nor accurately diagnosed, was not treated effectively and that treatment outweighed the risks of the condition [68]. Therefore, the levels of heightened psychological distress as reported by the women in our review, may actually be unnecessary and others have gone as far as saying that GDM is an example of ‘obstetric iatrogenesis’ [69].
The findings of this review did underline a few unmet service needs with recurring themes around the lack of individualised care and its continuity, lack of choice regarding important aspects of care such as birthing options, and the scarcity of comprehensive follow-up. There was a sense of abandonment amongst women after delivery in that they had experienced intensive intervention and then nothing. This could be viewed as a missed opportunity to capitalise on the motivation to make changes during pregnancy. Researchers have previously highlighted that adherence to postpartum screening and continued lifestyle modifications to prevent future diabetes seems to dissipate after birth, possibly because the driver to protect their unborn child is no longer there [70].
The studies included in our review had participants of varying cultures sampled from countries with different GDM definitions. However, there appeared no difference in the qualitative outcomes between studies/countries. In our review, the experiences of women diagnosed with GDM suggest psychosocial harms appear to outweigh the qualitative benefits. Quantitative studies [14, 15] that report prevalence increases in GDM after the IADSPG [71] definition changed, also report minimal improvements to maternal and infant physical outcomes.
This synthesis of women’s experiences of a GDM diagnosis could be used to inform the content of communication materials both before and after a GDM diagnosis. For example, an awareness of GDM testing and basic information including cultural adaptations to dietary guidelines and addressing misconceptions around breastfeeding. There is also an opportunity for HCPs to use teachable moments with women who have been identified at risk of developing type 2 diabetes post-pregnancy and offer supportive, effective advice about lifestyle changes. This is particularly relevant considering a previous review highlighted a significant time is spent in sedentary behaviour during pregnancy [72]. A study which examined HCPs views of healthcare provision to women with GDM showed that HCPs themselves perceived that there was a shortfall in GDM education [73]. There are also signals for service improvement and potential for service redesign, such as increasing community-delivered care for women diagnosed with GDM. This would assist in alleviating the burden on women to attend hospital appointments and potentially offer flexible appointment times. Follow-up appointments post-pregnancy could be made with consideration of other appointments such as maternal and child health milestones and breastfeeding weaning classes, and could also focused on healthy eating for both mother and baby.
Strengths and limitations
This systematic review included studies with women of different demographic characteristics and multicultural samples. The themes identified were represented in the majority of studies which increased the internal validity. The relatively high participation rate in the included studies, and that most studies were conducted during pregnancy or shortly after delivery, contributes to the external validity of our study. Although some participants were interviewed antenatally and some postnatally, this distribution over different gestational stages assists the generalisability of the study findings.
The comparison of coding between authors, discussion of the results and reaching consensus was a robust approach to improve the credibility of the results. Overall, the quality of most studies was good, however, a third of the studies used convenience methods to recruit participants which could contribute to sampling bias and limit the external validity of our findings. Only two studies adequately described the facilitator’s prior experience and the relationship between the participants and the facilitator/researcher. Unfortunately, this review did not capture the perception of HCPs which might be used to explain some of the behaviours and attitudes of the women, particularly in relation to communication of the diagnosis and information provision. Finally, although the data were collected from diverse populations, the majority of the countries in which research were conducted in were high-income countries, which could be considered to have more established and evidence-based healthcare systems than low-income countries.
Further research
A previous study has suggested the need for more research on the benefits and harms of alternative treatment choices for women with GDM [33]. The findings from this review suggest a need for more investigation around the psychosocial benefits and harms of a diagnosis of GDM. Given some women viewed treatment of ‘borderline GDM’ as unimportant, a new model of care based on stratification or individual level of risk for pregnancy and birth complications could be further explored. This may reduce the need for all women to be labelled as having GDM and negate unnecessary anxiety and burden for those at the lower ‘borderline’ threshold. This would then potentially offer tailored treatment options, improve shared-decision making, and improve women’s knowledge about how a diagnosis of GDM might affect them.
Conclusion
Consequences of a GDM diagnosis are multidimensional and highly contextual. Despite the psychosocial challenges frequently experienced, many women (driven by the innate response to safeguard their unborn baby) were able to gradually adapt to the required lifestyle changes and monitoring regimens. Perhaps a question is whether some of them should have to. There is opportunity to improve lifestyle and to assist the prevention of diabetes after pregnancy, however, this needs to be managed alongside the potential harms of a GDM diagnosis such as the negative psychological impact and social isolation. In the context of rising prevalence [14–17], potential minimal clinical [14–16] improvements, and the wide range of psychosocial experiences identified in this study, the findings of this review highlight the need for HCPs to consider the implications that a GDM diagnosis may have on women. It is essential that women diagnosed with GDM receive consistent evidence-based information and ongoing psychological and social support.
Supplementary information
Additional file 1: Table S1. Enhancing Transparency in Reporting the Synthesis of Qualitative Research Guidelines Checklist. Table S2. Assessment of quality of included studies using the CASP tool.
Acknowledgements
Not applicable.
Abbreviations
- BGL
Blood glucose level
- CASP
Critical Appraisal Skills Programme Checklist (Qualitative)
- ENTREQ
Enhancing Transparency in Reporting the Synthesis of Qualitative Research
- GDM
Gestational diabetes mellitus
- HAPO
Hyperglycemia and Adverse Pregnancy Outcomes
- HCP
Health care professional
- IADSPG
International Association of the Diabetes and Pregnancy Study Groups
Authors’ contributions
PG, LC and RT conceived the project design, LC conducted the search, extracted, analysed and interpreted the data assisted by RS. RT assisted in data interpretation. All authors contributed to the drafting of the manuscript and approve the final version.
Funding
LC is supported by a National Health and Medical Research Council Partnership Centre for Health System Sustainability grant (#9100002). RS and RT are supported by a National Health and Medical Research Council Program grant (#1106452) and PG is supported by a NHMRC Research Fellowship (#1080042). The funders had no role in design, data collection, analysis, interpretation or writing of the manuscript.
Availability of data and materials
The datasets generated during the current systematic review are available from the lead author upon request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12884-020-2745-1.
References
- 1.O'Sullivan JB, Mahan CM. Criteria for the oral glucose tolerance test in pregnancy. Diabetes. 1964;13:278–285. [PubMed] [Google Scholar]
- 2.Mishra S, Rao CR, Shetty A. Trends in the diagnosis of gestational diabetes mellitus. Scientifica (Cairo) 2016;2016:5489015. doi: 10.1155/2016/5489015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes. Syst Rev. 2002;25(10):1862–1868. doi: 10.2337/diacare.25.10.1862. [DOI] [PubMed] [Google Scholar]
- 4.HAPO Study Cooperative Research Group Hyperglycaemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002. doi: 10.1056/NEJMoa0707943. [DOI] [PubMed] [Google Scholar]
- 5.McIntyre HD, Gibbons KS, Lowe J, Oats JJN. Development of a risk engine relating maternal glycemia and body mass index to pregnancy outcomes. Diabetes Res Clin Pract. 2018;139:331–338. doi: 10.1016/j.diabres.2018.02.036. [DOI] [PubMed] [Google Scholar]
- 6.Kamysheva E, Skouteris H, Wertheim EH, et al. Examination of a multi-factorial model of body-related experiences during pregnancy: The relationships among physical symptoms, sleep quality, depression, self-esteem, and negative body attitudes. Body Image. 2008;5(2):152–163. doi: 10.1016/j.bodyim.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Carolan-Olah M, Barry M. Antenatal stress: an Irish case study. Midwifery. 2014;30(3):310–316. doi: 10.1016/j.midw.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Ferreira CR, Orsini MC, Vieira CR, et al. Prevalence of anxiety symptoms and depression in the third gestational trimester. Arch Gynecol Obstet. 2015;291(5):999–1003. doi: 10.1007/s00404-014-3508-x. [DOI] [PubMed] [Google Scholar]
- 9.Dalfra MG, Nicolucci A, Bisson T, et al. Quality of life in pregnancy and post-partum: a study in diabetic patients. Qual Life Res. 2012;21(2):291–298. doi: 10.1007/s11136-011-9940-5. [DOI] [PubMed] [Google Scholar]
- 10.Evans MK, O’Brien B. Gestational diabetes: the meaning of an at-risk pregnancy. Qual Health Res. 2005;15(1):66–81. doi: 10.1177/1049732304270825. [DOI] [PubMed] [Google Scholar]
- 11.Devsam BU, Bogossian FE, Peacock AS. An interpretive review of women's experiences of gestational diabetes mellitus: proposing a framework to enhance midwifery assessment. Women Birth. 2013;26(2):E69–E76. doi: 10.1016/j.wombi.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 12.Carolan-Olah M, Duarte-Gardea M, Lechuga J, et al. The experience of gestational diabetes mellitus (GDM) among Hispanic women in a U.S. border region. Sex Reprod Healthc. 2017;12:16–23. doi: 10.1016/j.srhc.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Persson M, Winkvist A, Mogren I. ‘From stun to gradual balance’—women’s experiences of living with gestational diabetes mellitus. Scand J Caring Sci. 2010;24(3):454–462. doi: 10.1111/j.1471-6712.2009.00735.x. [DOI] [PubMed] [Google Scholar]
- 14.Cade TJ, Polyakov A, Brennecke SP. Implications of the introduction of new criteria for the diagnosis of gestational diabetes: a health outcome and cost of care analysis. BMJ Open. 2019;9(1):e023293–e023e93. doi: 10.1136/bmjopen-2018-023293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sexton H, Heal C, Banks J, et al. Impact of new diagnostic criteria for gestational diabetes. J Obstet Gynaecol Res. 2018;44(3):425–431. doi: 10.1111/jog.13544. [DOI] [PubMed] [Google Scholar]
- 16.Erjavec K, Poljičanin T, Matijević R. Impact of the implementation of new WHO diagnostic criteria for gestational diabetes mellitus on prevalence and perinatal outcomes: a population-based study. J Pregnancy. 2016;2016:2670912. doi: 10.1155/2016/2670912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feldman RK, Tieu RS, Yasumura L. Gestational diabetes screening the international association of the diabetes and pregnancy study groups compared with carpenter-coustan screening. Obstet Gynecol. 2016;127(1):10–17. doi: 10.1097/aog.0000000000001132. [DOI] [PubMed] [Google Scholar]
- 18.Pocobelli G, Yu O, Fuller S, et al. One-step approach to identifying gestational diabetes mellitus: association with perinatal outcomes. Obstet Gynecol. 2018;132(4):859–867. doi: 10.1097/aog.0000000000002780. [DOI] [PubMed] [Google Scholar]
- 19.Draffin CR, Alderdice FA, McCance DR, et al. Exploring the needs, concerns and knowledge of women diagnosed with gestational diabetes: a qualitative study. Midwifery. 2016;40:141–147. doi: 10.1016/j.midw.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 20.Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181. doi: 10.1186/1471-2288-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rathbone J, Carter M, Hoffmann T, et al. Better duplicate detection for systematic reviewers: evaluation of systematic review assistant-deduplication module. Syst Rev. 2015;4:6. doi: 10.1186/2046-4053-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lucas PJ, Baird J, Arai L, et al. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med Res Methodol. 2007;7(1):4. doi: 10.1186/1471-2288-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Group CCQM . Chapter 4: critical appraisal of qualitative research. In: Noyes J, Booth A, Hannes K, Harden A, Harris J, Lewin S, Lockwood C, editors. Supplementary guidance for inclusion of qualitative research in cochrane systematic reviews of interventions. Version 1. 2011. [Google Scholar]
- 25.Abraham K, Wilk N. Living with gestational diabetes in a rural community. MCN Am J Matern Child Nurs. 2014;39(4):239–245. doi: 10.1097/NMC.0000000000000047. [DOI] [PubMed] [Google Scholar]
- 26.Araujo MF, Pessoa SM, Damasceno MM, et al. Gestational diabetes from the perspective of hospitalized pregnant women. Rev Bras Enferm. 2013;66(2):222–227. doi: 10.1590/S0034-71672013000200011. [DOI] [PubMed] [Google Scholar]
- 27.Bandyopadhyay M, Small R, Davey MA. Attendance for postpartum glucose tolerance testing following gestational diabetes among south Asian women in Australia: a qualitative study. Int J Gynecol Obstet. 2015;131:E149. [Google Scholar]
- 28.Bandyopadhyay M, Small R, Davey MA, et al. Lived experience of gestational diabetes mellitus among immigrant South Asian women in Australia. Aust N Z J Obstet Gynaecol. 2011;51(4):360–364. doi: 10.1111/j.1479-828X.2011.01322.x. [DOI] [PubMed] [Google Scholar]
- 29.Carolan M. Women’s experiences of gestational diabetes self-management: a qualitative study. Midwifery. 2013;29(6):637–645. doi: 10.1016/j.midw.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 30.Doran F. Gestational diabetes mellitus: perspectives on lifestyle changes during pregnancy and post-partum, physical activity and the prevention of future type 2 diabetes. Aust J Prim Health. 2008;14(3):85–92. doi: 10.1071/PY08040. [DOI] [Google Scholar]
- 31.Doran F, Davis K. Gestational diabetes mellitus in Tonga: insights from healthcare professionals and women who experienced gestational diabetes mellitus. N Z Med J. 2010;123(1326):59–67. [PubMed] [Google Scholar]
- 32.Eades CE, France EF, Evans JMM. Postnatal experiences, knowledge and perceptions of women with gestational diabetes. Diabet Med. 2018;35(4):519–529. doi: 10.1111/dme.13580. [DOI] [PubMed] [Google Scholar]
- 33.Figueroa Gray M, Hsu C, Kiel L, et al. “It's a very big burden on me”: Women’s experiences using insulin for gestational diabetes. Matern Child Health J. 2017;21(8):1678–1685. doi: 10.1007/s10995-017-2261-8. [DOI] [PubMed] [Google Scholar]
- 34.Ge L, Albin B, Hadziabdic E, et al. Beliefs about health and illness and health-related behavior among urban women with gestational diabetes mellitus in the south east of China. J Transcult Nurs. 2016;27(6):593–602. doi: 10.1177/1043659615594677. [DOI] [PubMed] [Google Scholar]
- 35.Ge L, Wikby K, Rask M. ‘Is gestational diabetes a severe illness?’ Exploring beliefs and self-care behaviour among women with gestational diabetes living in a rural area of the south east of China. Aust J Rural Health. 2016;24(6):378–384. doi: 10.1111/ajr.12292. [DOI] [PubMed] [Google Scholar]
- 36.Han S, Middleton PF, Bubner TK, et al. Women’s views on their diagnosis and management for borderline gestational diabetes mellitus. J Diabetes Res. 2015;2015:209215. doi: 10.1155/2015/209215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hirst JE, Tran TS, Do MAT, et al. Women with gestational diabetes in Vietnam: a qualitative study to determine attitudes and health behaviours. BMC Pregnancy Childbirth. 2012;12:81. doi: 10.1186/1471-2393-12-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hjelm K, Bard K, Apelqvist J. Gestational diabetes: prospective interview-study of the developing beliefs about health, illness and health care in migrant women. J Clin Nurs. 2012;21(21–22):3244–3256. doi: 10.1111/j.1365-2702.2012.04069.x. [DOI] [PubMed] [Google Scholar]
- 39.Hjelm K, Bard K, Apelqvist J. A qualitative study of developing beliefs about health, illness and healthcare in migrant African women with gestational diabetes living in Sweden. BMC Womens Health. 2018;18(1):34. doi: 10.1186/s12905-018-0518-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hjelm K, Bard K, Berntorp K, et al. Beliefs about health and illness postpartum in women born in Sweden and the Middle East. Midwifery. 2009;25(5):564–575. doi: 10.1016/j.midw.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 41.Hjelm K, Bard K, Nyberg P, et al. Swedish and middle-eastern-born women’s beliefs about gestational diabetes. Midwifery. 2005;21(1):44–60. doi: 10.1016/j.midw.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 42.Hjelm K, Berntorp K, Apelqvist J. Beliefs about health and illness in Swedish and African-born women with gestational diabetes living in Sweden. J Clin Nurs. 2012;21(9–10):1374–1386. doi: 10.1111/j.1365-2702.2011.03834.x. [DOI] [PubMed] [Google Scholar]
- 43.Hjelm K, Berntorp K, Frid A, et al. Beliefs about health and illness in women managed for gestational diabetes in two organisations. Midwifery. 2008;24(2):168–182. doi: 10.1016/j.midw.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 44.Hui AL, Sevenhuysen G, Harvey D, et al. Stress and anxiety in women with gestational diabetes during dietary management. Diabetes Educ. 2014;40(5):668–677. doi: 10.1177/0145721714535991. [DOI] [PubMed] [Google Scholar]
- 45.Kaptein S, Evans M, McTavish S, et al. The subjective impact of a diagnosis of gestational diabetes among ethnically diverse pregnant women: a qualitative study. Can. 2015;39(2):117–122. doi: 10.1016/j.jcjd.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 46.Kilgour C, Bogossian FE, Callaway L, et al. Postnatal gestational diabetes mellitus follow-up: Australian women’s experiences. Women Birth. 2015;28(4):285–292. doi: 10.1016/j.wombi.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 47.Lawson EJ, Rajaram S. A transformed pregnacy – the psychological consequences of gestational diabetes. Sociol Health Illn. 1994;16(4):536–562. doi: 10.1111/1467-9566.ep11347644. [DOI] [Google Scholar]
- 48.Lie MLS, Hayes L, Lewis-Barned NJ, et al. Preventing type 2 diabetes after gestational diabetes: women’s experiences and implications for diabetes prevention interventions. Diabet Med. 2013;30(8):986–993. doi: 10.1111/dme.12206. [DOI] [PubMed] [Google Scholar]
- 49.Neufeld HT. Food perceptions and concerns of aboriginal women coping with gestational diabetes in Winnipeg, Manitoba. J Nutr Educ Behav. 2011;43(6):482–491. doi: 10.1016/j.jneb.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 50.Nielsen JH, Olesen CR, Kristiansen TM, et al. Reasons for women’s non-participation in follow-up screening after gestational diabetes. Women Birth. 2015;28(4):e157–e163. doi: 10.1016/j.wombi.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 51.Parsons J, Sparrow K, Ismail K, et al. Experiences of gestational diabetes and gestational diabetes care: a focus group and interview study. BMC Pregnancy Childbirth. 2018;18:25. doi: 10.1186/s12884-018-1657-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pennington AVR, O’Reilly SL, Young D, et al. Improving follow-up care for women with a history of gestational diabetes: perspectives of GPs and patients. Aust J Prim Health. 2017;23(1):66–74. doi: 10.1071/PY15177. [DOI] [PubMed] [Google Scholar]
- 53.Rafii F, Vasegh Rahimparvar SF, Keramat A, et al. Procrastination as a key factor in postpartum screening for diabetes: A qualitative study of Iranian women with recent gestational diabetes. Iran Red Crescent Med J. 2017;19(5). 10.5812/ircmj.44833.
- 54.Razee H, van der Ploeg HP, Blignault I, et al. Beliefs, barriers, social support, and environmental influences related to diabetes risk behaviours among women with a history of gestational diabetes. Health Promot J Austr. 2010;21(2):130–137. doi: 10.1071/HE10130. [DOI] [PubMed] [Google Scholar]
- 55.Salomon IMM, Soares SM. Understanding the impact of gestational diabetes diagnosis. Revista Mineira de Enfermagem. 2004;8(3):349–357. [Google Scholar]
- 56.Svensson L, Nielsen KK, Maindal HT. What is the postpartum experience of Danish women following gestational diabetes? A qualitative exploration. Scand J Caring Sci. 2018;32(2):756–764. doi: 10.1111/scs.12506. [DOI] [PubMed] [Google Scholar]
- 57.Tang JW, Foster KE, Pumarino J, et al. Perspectives on prevention of type 2 diabetes after gestational diabetes: a qualitative study of Hispanic, African-American and White women. Matern Child Health J. 2015;19(7):1526–1534. doi: 10.1007/s10995-014-1657-y. [DOI] [PubMed] [Google Scholar]
- 58.Tierney M, O'Dea A, Danyliv A, et al. Factors influencing lifestyle behaviours during and after a gestational diabetes mellitus pregnancy. Health Psychol Behav Med. 2015;3(1):204–216. doi: 10.1080/21642850.2015.1073111. [DOI] [Google Scholar]
- 59.Trutnovsky G, Panzitt T, Magnet E, et al. Gestational diabetes: women's concerns, mood state, quality of life and treatment satisfaction. J Matern Fetal Neonatal Med. 2012;25(11):2464–2466. doi: 10.3109/14767058.2012.683900. [DOI] [PubMed] [Google Scholar]
- 60.Wah Yat Yin Eric, McGill Margaret, Wong Jencia, Ross Glynis P., Harding Anna-Jane, Krass Ines. Self-management of gestational diabetes among Chinese migrants: A qualitative study. Women and Birth. 2019;32(1):e17–e23. doi: 10.1016/j.wombi.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 61.Whitty-Rogers J, Caine V, Cameron B. Aboriginal women’s experiences with gestational diabetes mellitus: a participatory study with mi'kmaq women in Canada. ANS Adv Nurs Sci. 2016;39(2):181–198. doi: 10.1097/ANS.0000000000000115. [DOI] [PubMed] [Google Scholar]
- 62.Johanson R, Newburn M, Macfarlane A. Has the medicalisation of childbirth gone too far? BMJ. 2002;324(7342):892–895. doi: 10.1136/bmj.324.7342.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Van Ryswyk E, Middleton P, Shute E, et al. Women's views and knowledge regarding healthcare seeking for gestational diabetes in the postpartum period: a systematic review of qualitative/survey studies. Diabetes Res Clin Pract. 2015;110(2):109–122. doi: 10.1016/j.diabres.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 64.Goldstein RF, Gibson-Helm ME, Boyle JA, et al. Satisfaction with diagnosis process for gestational diabetes mellitus and risk perception among Australian women. Int J Gynaecol Obstet. 2015;129(1):46–49. doi: 10.1016/j.ijgo.2014.10.033. [DOI] [PubMed] [Google Scholar]
- 65.Carolan M. Diabetes nurse educators’ experiences of providing care for women, with gestational diabetes mellitus, from disadvantaged backgrounds. J Clin Nurs. 2014;23(9–10):1374–1384. doi: 10.1111/jocn.12421. [DOI] [PubMed] [Google Scholar]
- 66.Yuen L, Wong VW. Gestational diabetes mellitus: challenges for different ethnic groups. World J Diabetes. 2015;6(8):1024–1032. doi: 10.4239/wjd.v6.i8.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Carolan M, Steele C, Margetts H. Knowledge of gestational diabetes among a multi-ethnic cohort in Australia. Midwifery. 2010;26(6):579–588. doi: 10.1016/j.midw.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 68.Goer H. Gestational diabetes: the emperor has no clothes. The Birth Gazette Summertown: Second Foundation. 1996. pp. 32–35. [PubMed] [Google Scholar]
- 69.Han S, Bubner T, Middleton PF, et al. A qualitative study of women's views on diagnosis and management for borderline gestational diabetes. J Paediatr Child Health. 2013;49:128. doi: 10.1111/jpc.12133. [DOI] [Google Scholar]
- 70.Nielsen KK, Kapur A, Damm P, et al. From screening to postpartum follow-up - the determinants and barriers for gestational diabetes mellitus (GDM) services, a systematic review. BMC Pregnancy Childbirth. 2014;14:41. doi: 10.1186/1471-2393-14-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.International Association of Diabetes and Pregnancy Study Groups Consensus Panel International Association of Diabetes and Pregnancy Study Groups Recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–682. doi: 10.2337/dc09-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fazzi C, Saunders DH, Linton K, et al. Sedentary behaviours during pregnancy: a systematic review. Int J Behav Nutr Phys Act. 2017;14:32. doi: 10.1186/s12966-017-0485-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Van Ryswyk E, Middleton P, Hague W, et al. Clinician views and knowledge regarding healthcare provision in the postpartum period for women with recent gestational diabetes: A systematic review of qualitative/survey studies. Diabetes Res Clin Pract. 2014;106(3):401–411. doi: 10.1016/j.diabres.2014.09.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Enhancing Transparency in Reporting the Synthesis of Qualitative Research Guidelines Checklist. Table S2. Assessment of quality of included studies using the CASP tool.
Data Availability Statement
The datasets generated during the current systematic review are available from the lead author upon request.


