Abstract
Background
Colon cancer is common worldwide and is the leading cause of cancer-related death. Multiple levels of omics data are available due to the development of sequencing technologies. In this study, we proposed an integrative prognostic model for colon cancer based on the integration of clinical and multi-omics data.
Methods
In total, 344 patients were included in this study. Clinical, gene expression, DNA methylation and miRNA expression data were retrieved from The Cancer Genome Atlas (TCGA). To accommodate the high dimensionality of omics data, unsupervised clustering was used as dimension reduction method. The bias-corrected Harrell’s concordance index was used to verify which clustering result provided the best prognostic performance. Finally, we proposed a prognostic prediction model based on the integration of clinical data and multi-omics data. Uno’s concordance index with cross-validation was used to compare the discriminative performance of the prognostic model constructed with different covariates.
Results
Combinations of clinical and multi-omics data can improve prognostic performance, as shown by the increase of the bias-corrected Harrell’s concordance of the prognostic model from 0.7424 (clinical features only) to 0.7604 (clinical features and three types of omics features). Additionally, 2-year, 3-year and 5-year Uno’s concordance statistics increased from 0.7329, 0.7043, and 0.7002 (clinical features only) to 0.7639, 0.7474 and 0.7597 (clinical features and three types of omics features), respectively.
Conclusion
In conclusion, this study successfully combined clinical and multi-omics data for better prediction of colon cancer prognosis.
Keywords: Colon cancer, Prognostic prediction, Integrative analysis, Multi-omics study, The Cancer genome atlas (TCGA)
Background
Colon cancer, which is a subset of colorectal cancer (CRC), is common worldwide and is the leading cause of cancer-related death. Although incidence and mortality rates have declined in recent years due to changes in risk factors and recent improvements in screening tests and treatments, there are large differences in 5-year colon cancer survival rates across countries and regions [1, 2].
Because of the development of sequencing technology, precision medicine has become a popular field in cancer research. Omics data have been widely used for cancer classification based on identified gene signatures, gene pathways, and protein-protein interaction networks, among others [3–5]. Such classifications can help oncologists provide more accurate treatment regimens for individuals. Gene expression data are among the most widely analyzed types of omics data and can be used for such endeavors as biomarker identification, patient classification, and prognostic prediction [4, 6–8]. In addition, one published classification organized CRC into four consensus molecular subtypes using gene expression data, and this classification represents the best description of CRC heterogeneity at the gene expression level and shows the potential of merging additional scale data in the future [9].
The American Joint Committee on Cancer (AJCC) tumor, node and metastasis (TNM) staging system is an important tool used for clinical colon cancer prognostic predictions. However, no molecular factors or omics features were included in the TNM system for colon cancer in the recently published 8th version [10]. In contrast, the 8th AJCC TNM staging system for breast cancer already includes biomarkers, which is very different from the 7th AJCC TNM staging system [11]. The National Comprehensive Cancer Network (NCCN) Guidelines for Patients includes RAS mutations, BRAF V600E mutations, mismatch repair (MMR) and microsatellite instability (MSI) as recommended molecular testing in colon cancer patients [12].
As cancer research has entered the fields of precision medicine and personalized medicine, non-molecular features have become insufficient, whereas the inclusion of molecular features is becoming an increasingly popular research direction. Scientists have been attempting to integrate multiscale omics data to gain deeper insight into cancer mechanisms as the human body is a complex system. The Cancer Genome Atlas (TCGA) conducted a series of comprehensive integrative molecular analyses with multiscale data types to identify the genomic alterations in several cancer types; five genome-wide platforms were used to identify somatic alterations in colorectal carcinoma [13]. Kim D. et al. conducted a series of studies with TCGA datasets to identify interactions among multi-omics data and associate these interactions with cancer clinical outcomes [14–16]. Pan-cancer studies were also performed with integrative analyses [17, 18]. These studies suggest that multiscale or multiplatform genomic studies outperform single-scale studies in cancer research.
The performance of cancer prognostic analyses may benefit from the integration of clinical features and molecular features [19]. Previous studies have identified several candidate biomarkers, and some biomarkers, such as HER2 status and ER status in breast cancer patients, have been verified and used in clinical decision making, suggesting that the integration of clinical features and single-scale molecular features can improve the performance of cancer prognosis [11, 20]. Another study combined clinical, genomic and treatment domains to predict GBM survival outcomes, though the genomic domain only used 33 specific gene signatures [21]. Exarchos and colleagues combined clinical, imaging tissue and gene expression data from circulating blood cells to model the progression of oral cancer [22]. Recently, a workflow named SwissMTB was reported that could link molecular profiling to treatment decisions [23]. Combining clinical data with single-scale omics data has shown a considerable effect on cancer prognosis, but it remains unclear whether the integration of clinical data and multiscale omics data can help improve cancer prognosis performance.
To improve the prediction performance of colon cancer prognosis, an integrative prognostic analysis of colon cancer was proposed in this study based on clinical, gene expression, DNA methylation and miRNA expression data from TCGA.
Methods
Data preparation
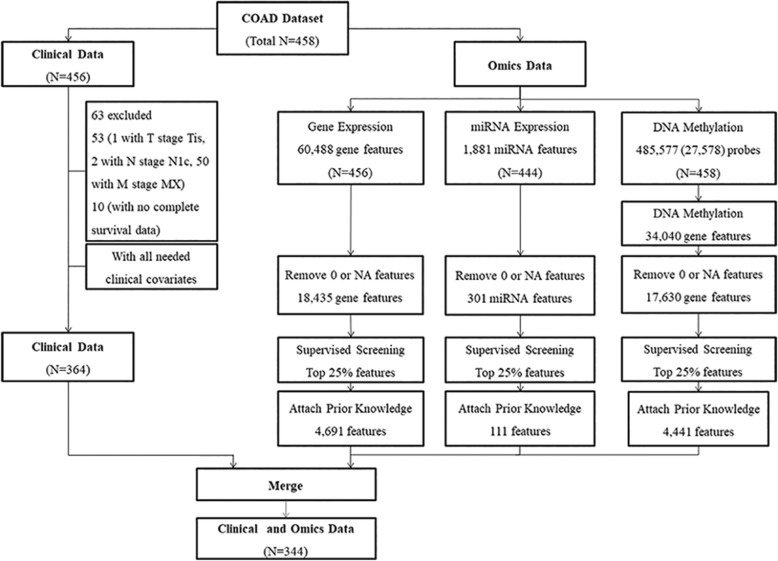
Normalized and preprocessed clinical data and omics data (gene expression, DNA methylation and miRNA expression data) of primary tumors included in the TCGA-COAD (colon adenocarcinoma) project were downloaded from the new TCGA data portal (https://portal.gdc.cancer.gov/repository) with the provided data-transfer tool. Then, the downloaded raw data files were reprocessed following the flowchart shown in Fig. 1. This procedure aimed to merge the individual files of each patient into one matrix of samples and features by data type.
Fig. 1.
Flowchart of data processing for the TCGA-COAD dataset
Clinical data preparation
The tumor invasion depth, lymph node status, metastatic status (T, N and M stages) and age at initial diagnosis were chosen as clinical features, as previous studies have shown that these four features have significant effects on CRC prognosis [24]. Patients with Tis tumor invasion depth (1 patient), N1c lymph node status (2 patients), and Mx metastatic status (metastatic status that could not be assessed) were removed from the study. Patients without any of these four features or survival information were also removed. Survival information, including survival time and death status, was also obtained from the clinical data. Overall survival was used for the following analyses in this study to reflect the overall survival information of the patients.
Omics data preparation
Prior Knowledge
Prior knowledge was based on the pathways and microRNAs involved in CRC according to the Kyoto Encyclopedia of Genes and Genomes (KEGG, http://www.genome.jp/kegg/) database and other omics features that showed potential relationships with colon cancer prognosis in previous articles [25–27]. A collection of prior knowledge lists of the three types of omics data was built, including 114 features of gene expression, 56 features of DNA methylation and 56 features of microRNA expression. The details of the prior knowledge lists are provided in Additional file 1.
Gene Expression
For gene expression data, fragments per kilobase of transcript per million mapped reads (FPKM) normalized data were chosen for further analysis, and the original Ensembl IDs were converted to gene symbols with the biomaRt R package. Then, each feature with more than 5% NA or 0 values was removed. Features with the top 25% of coefficients of the variable along with features in the prior knowledge list of gene expression were selected. Ultimately, 4691 features were selected for further analysis.
MicroRNA Expression
For miRNA expression data, reads per million mapped reads (RPM) normalized data were chosen for further analysis. Each feature with more than 5% NA or 0 values was removed. Features with the top 25% of coefficients of the variable along with features in the prior knowledge list of microRNA expression were selected. Ultimately, 111 features were selected for further analysis.
DNA Methylation
For DNA methylation data, the beta values were used in the analysis, whereas various probes (485,577 probes for HM450 and 27,578 probes for HM27) were converted into 34,040 gene symbols. The conversion procedure was performed by calculating the average DNA methylation beta value of the CpG sites in a particular region of a gene based on TCGA-assembler 2 [28]. In addition, CpG sites with chromosome X or Y and more than 5% NA beta values were removed as colon cancer is not a gender-specific disease. Each feature with more than 5% NA or 0 values was removed. Features with the top 25% of coefficients of the variable along with features in the prior knowledge list of DNA methylation were selected. Ultimately, 4441 features were selected for further analysis.
Results of the data preparation
Patients with both clinical data and the three types of omics data were chosen for our analysis. Overall, 344 patients had both clinical data and the three types of omics data, resulting in 4691 features in the gene expression profiles, 4441 features in the DNA methylation profiles and 111 features in the miRNA expression profiles. Detailed information regarding the clinical and omics data is shown in Table 1 and Table 2, respectively.
Table 1.
Feature statistics of the clinical data used in the prognostic analysis
| Features | Statistics | |
|---|---|---|
| Cases with Clinical and Omics Data | 344 | |
| Gender: | Male | 182 (52.9%) |
| Female | 162 (47.1%) | |
| Survival Status: | Alive | 273 (79.4%) |
| Dead | 71 (20.6%) | |
| Survival Time: | Mean | 779.8 (days) |
| Median | 575.5 (days) | |
| T Stage: | T1 | 10 (2.91%) |
| T2 | 62 (18.02%) | |
| T3 | 254 (73.84%) | |
| T4a | 12 (3.49%) | |
| T4b | 6 (1.74%) | |
| N Stage: | N0 | 211 (61.3%) |
| N1a | 35 (10.2%) | |
| N1b | 40 (11.6%) | |
| N2a | 32 (9.3%) | |
| N2b | 26 (7.6%) | |
| M Stage: | M0 | 292 (84.9%) |
| M1 | 52 (15.1%) | |
| Age at Initial Diagnosis: | Basic Statistics (years) | Min: 31, Median: 69, Mean: 66, Max: 90 |
| 31–59 | 86 (25.0%) | |
| 59–69 | 85 (24.7%) | |
| 69–77 | 82 (23.8%) | |
| 77–90 | 91 (26.5%) |
Table 2.
Information regarding the omics data used in the prognostic analysis
| Features | Statistics or Description |
|---|---|
| Gene Expression | |
| Platform | Illumina Genome Analyzer RNA Sequencing |
| Reference Genome | GRCh38 |
| Measurement | FPKM normalized value |
| Number of Features | 4691 |
| DNA Methylation | |
| Platform | Illumina Infinium Human Methylation 27 (HM27) and Human Methylation 450 (HM450) |
| Reference Genome | GRCh38 |
| Measurement | Beta value |
| Number of Features | 4441 |
| miRNA Expression | |
| Platform | Illumina Genome Analyzer miRNA Sequencing |
| Reference Annotation | miRBase v21 and UCSC |
| Measurement | RPM |
| Number of Features | 111 |
Pipeline of the prognostic study
The overall pipeline for the construction of the prognosis prediction model is shown in Fig. 2. First, we solved the problem of imbalanced feature numbers and different measurements between the clinical features and multi-omics features by unsupervised clustering and generated new omics features with low dimensions. Then, a prognostic prediction model was constructed using both the clinical features and new omics features. Different combinations of the clinical features and omics features were tested and compared to determine whether the integration of the clinical features, gene expression profiles, DNA methylation profiles and miRNA expression profiles could offer the best prognostic performance.
Fig. 2.
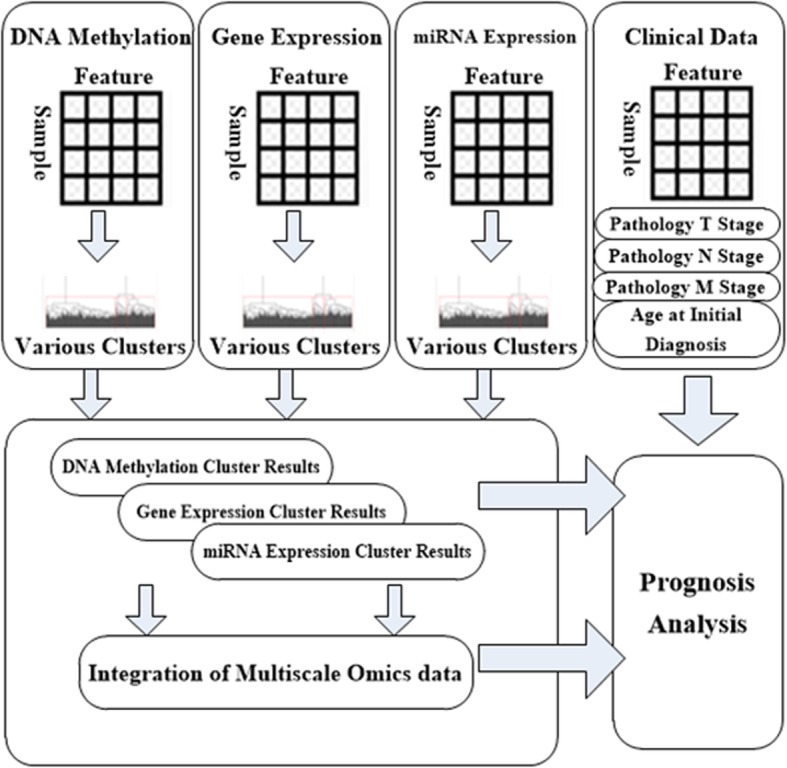
Pipeline of the integration of the clinical data and multi-omics data for the prognostic analysis
Processing of the multi-Omics data
Hierarchical clustering was used for the cluster analysis because this approach is an unsupervised cluster method that is widely used in omics data analyses. The following three parameters were employed in this unsupervised clustering step: the distance method was used as the metric, the linkage method was used as the linkage criteria, and the cluster number was used as the cut-off condition. In addition, each cluster should contain at least 10 patients. Overall, seven distance methods, including Euclidean, Maximum, Manhattan, Canberra, Binary, Minkowski and Correlation; eight linkage methods, including Ward.D, Ward.D2, Single, Complete, Average, Mcquitty, Median and Centroid; and cluster numbers ranging from 2 to 11 were applied to evaluate different combinations of the cluster parameters.
Clustering of the three types of omics data was performed. Different combinations of distance methods, linkage methods and cluster numbers were used, and the combination that provided the best prognostic information was selected by fitting a single-covariate Cox proportional hazards (PH) model. The cluster labels generated by the identified clustering parameters were used as new omics features for the three types of omics data. In addition, we investigated whether the integrated multi-omics data could improve the prognostic prediction performance over that of separate multi-omics data combined with clinical features. Then, we conducted a cluster-of-clusters (C-o-C) approach based on these new omics features to integrate the three types of omics data because this approach has shown excellent performance in previous single-cancer and pan-cancer studies [17, 29, 30]. The newly generated features of the three types of omics data were coded into one binary matrix of patients and cluster labels, and clustering by hierarchical clustering was performed again. The same varieties of combinations of distance methods, linkage methods and cluster numbers were used, and the combination that provided the best prognostic information was selected by fitting a single-covariate Cox PH model. These identified cluster labels were regarded as features of the integrated omics data. The generated omics features in both the separated status and integrated status were used for further analysis. Finally, cluster analyses of the three single types of omics data and one cluster analysis of the integration of the three types of omics data were performed for further analysis.
Integration of clinical data and Omics data for the construction of the prognostic prediction model
A multi-covariate Cox PH model was used for the prognostic analysis, and different combinations of clinical features and omics features were used as covariates in the Cox PH model. The formula of the Cox PH model used in our study was as follows:
where h(t) is the hazard (risk of death) at time t, h0(t) is the baseline hazard (when covariates zn and zm are all zero), βn is the regression coefficient of the clinical features, βm is the regression coefficient of the omics features, zn represents the different clinical features, and zm represents the different omics features. The T, N, and M stages and age at initial diagnosis were used as the clinical features. The omics features consisted of different types of omics data, including three features of the single types of omics data and one feature of three integrated types of omics data. Cox PH models with different combinations of clinical features and omics features were constructed. The prognostic performance of each model was compared to verify that the integration of clinical data and multi-omics data provided the best prognostic performance.
Model evaluation
We focused on the discriminative performance of the prognostic model. Therefore, the concordance index (C-index) was used as the main evaluation metric, with a C-index of 1 indicating perfect discrimination and a C-index 0.5 indicating a random guess. We used Harrell’s C-index during the model construction procedure to select the model with best overall discriminative performance [31]. Then Uno’s C-index, which is free of censoring, and the likelihood ratio test were used to compare the performance of different models [32, 33]. The PH assumption was tested to ensure that the constructed Cox PH model satisfied the assumption and that the covariates had no time-varying coefficients; a p-value greater than 0.05 suggests no time-variation issue [34]. In addition, the likelihood ratio, score and Wald test were applied to investigate the covariate effect in the Cox PH model; a p-value of less than 0.05 indicates that the covariate in the model has a significant effect [35]. These metrics were calculated with the rms (https://cran.r-project.org/web/packages/rms/index.html) and survC1 (https://cran.r-project.org/web/packages/survC1/index.html) R package.
Considering the moderate sample size, we preferred a bootstrapping analysis, which revealed the ability to optimize the estimation of the C-index caused by overfitting, to generate the bias-corrected C-index rather than the original Harrell’s C-index [36–39]. Random resampling with replacement was performed with 500 iterations to generate a distribution of the 500 bias-corrected C-indexes and the mean value was used as the final bias-corrected C-index during model construction. In addition to the original Uno’s C-index, we resorted to 5-fold cross-validation with 500 iterations to obtain more reliable values following a procedure similar to that introduced in Zhao’s work, with 500 Uno’s C-indexes and one average Uno’s C-index for each model [40]. Based on the distribution of C-indexes of different prognostic models, the Wilcoxon signed-rank tests were used to evaluate the significance of the difference in prediction performance between the C-indexes.
Results
Results of Omics data processing
Overall, eight combinations of distance methods, linkage methods and cluster numbers were identified for clustering of different types of omics data while combining with clinical features, including two combinations for gene expression, three combinations for DNA methylation and three combinations for miRNA expression. Cluster parameters of the three types of omics data for prognostic models with different covariates are listed in Table 3. For the C-o-C approach, the Manhattan distance method, Average linkage method and cluster number 3 were used to cluster the newly generated features of the three types of omics data used in the integrated prognostic model with covariates of clinical features and all three types of omics data.
Table 3.
Cluster parameters selected for different types of omics data in prognostic models with different covariates
| Covariates | Gene Expression | DNA Methylation | miRNA Expression | |
|---|---|---|---|---|
| Gene Expression | Distance Method: | Canberra | ||
| Linkage Method: | Ward.D | |||
| Cluster Number: | 6 | |||
| DNA Methylation | Distance Method: | Maximum | ||
| Linkage Method: | Ward.D | |||
| Cluster Number: | 10 | |||
| miRNA Expression | Distance Method: | Maximum | ||
| Linkage Method: | Ward.D2 | |||
| Cluster Number: | 4 | |||
| Clinical and Gene Expression | Distance Method: | Manhattan | ||
| Linkage Method: | Ward.D | |||
| Cluster Number: | 4 | |||
| Clinical and DNA Methylation | Distance Method: | Canberra | ||
| Linkage Method: | Ward.D | |||
| Cluster Number: | 3 | |||
| Clinical and miRNA Expression | Distance Method: | Canberra | ||
| Linkage Method: | Ward.D | |||
| Cluster Number: | 3 | |||
| Clinical and Gene Expression and DNA Methylation | Distance Method: | Manhattan | Correlation | |
| Linkage Method: | Ward.D | Ward.D2 | ||
| Cluster Number: | 4 | 3 | ||
| Clinical and Gene Expression and miRNA Expression | Distance Method: | Manhattan | Manhattan | |
| Linkage Method: | Ward.D | Ward.D | ||
| Cluster Number: | 4 | 4 | ||
| Clinical and DNA Methylation and miRNA Expression | Distance Method: | Maximum | Canberra | |
| Linkage Method: | Ward.D | Ward.D | ||
| Cluster Number: | 10 | 3 | ||
| Clinical and All Three Types of Omics Data | Distance Method: | Manhattan | Maximum | Manhattan |
| Linkage Method: | Ward.D | Ward.D | Ward.D2 | |
| Cluster Number: | 4 | 10 | 4 |
Prognostic performance of the models based on Harrell’s C-index
Overall, we included four clinical covariates, three omics covariates and one integrated omics covariate. The four clinical covariates were used as clinical covariates; alongside the three omics covariates, they formed seven different combinations. The prognostic model we proposed was constructed with clinical, gene expression, DNA methylation and miRNA expression as covariates. In addition, we constructed three models with clinical covariates and two types of omics data, three models with clinical covariates and one type of omics data, four models with clinical covariates or one type of omics data alone, and one model with clinical covariates and C-o-C results.
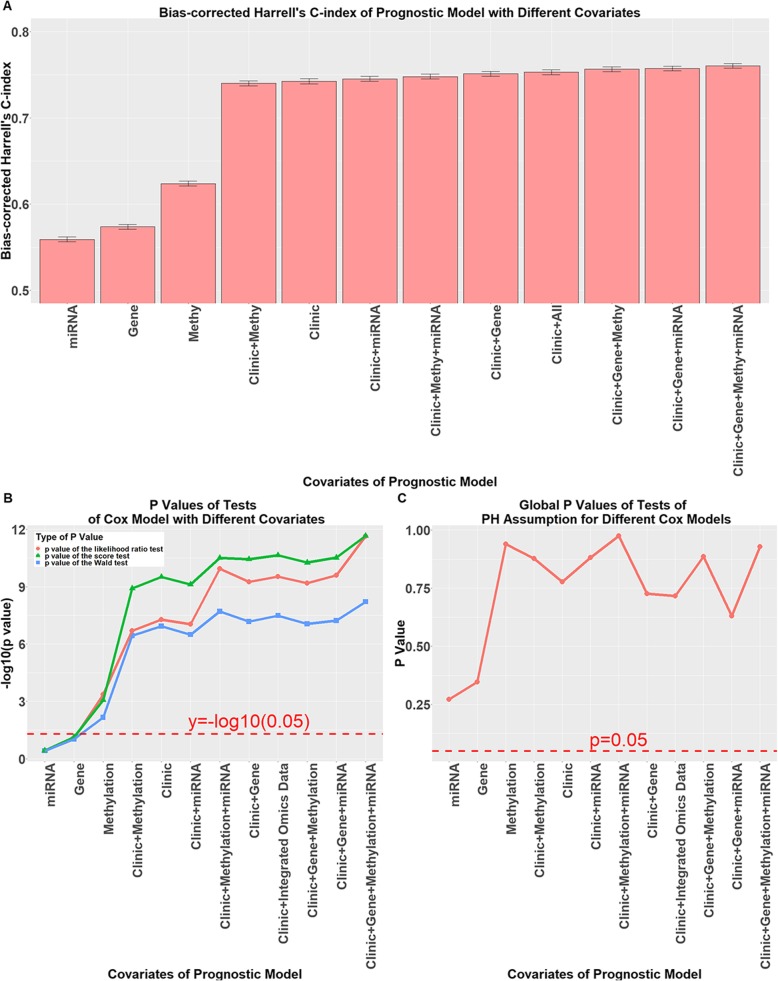
First, all models passed the PH assumptions test, as shown in Fig. 3c. The bias-corrected C-index of the different models is shown in Fig. 3a. These results suggest that the model with only the clinical covariates (0.7424 ± 0.0030) performed better than any model with the omics covariates (range from 0.5591 ± 0.0029 to 0.6238 ± 0.0029). A combination of clinical covariates and all three types of omics data achieved the best performance among all prognostic models (0.7604 ± 0.0028). The regression coefficients of the integrated prognostic model constructed with clinical, gene expression, DNA methylation and miRNA expression features are summarized in Table 4. Detailed origin concordance and bias-corrected concordance statistics for all models are listed in Additional file 2: Table S1.
Fig. 3.
Performance of prognostic models with different covariates. For the labels used in the figure, the symbol “+” indicates that the covariates were used separately in the model. a Bias-corrected Harrell’s C-index of prognostic models with different covariates with 95% CIs summarized from 500 bootstrapping replicates; b -log10(p-values) of the likelihood ratio test, the score test and the Wald test of Cox models with different covariates; the red dotted line indicates –log10(0.05); c Plot of the p-values of the global PH assumption tests
Table 4.
Regression coefficients of our integrated prognostic model
| Covariate | Coefficient ± SE | HR | 95% CI | P |
|---|---|---|---|---|
| T stage | ||||
| T1 | 1 | |||
| T2 | −3.125 ± 1.253 | 0.0439 | 0.00377–0.513 | 0.0127 |
| T3 | −1.186 ± 0.810 | 0.305 | 0.0624–1.493 | 0.143 |
| T4a | −0.298 ± 1.069 | 0.742 | 0.0913–6.033 | 0.780 |
| T4b | 0.530 ± 1.152 | 1.699 | 0.178–16.241 | 0.646 |
| N stage | ||||
| N0 | 1 | |||
| N1a | 0.266 ± 0.504 | 1.305 | 0.486–3.506 | 0.598 |
| N1b | 0.175 ± 0.450 | 1.191 | 0.493–2.877 | 0.697 |
| N2a | 1.355 ± 0.396 | 3.876 | 1.785–8.416 | 0.0006 |
| N2b | 0.985 ± 0.468 | 2.679 | 1.071–6.703 | 0.0352 |
| M stage | ||||
| M0 | 1 | |||
| M1 | 1.644 ± 0.362 | 5.178 | 2.546–10.532 | 5.64 e-6 |
| Age | ||||
| 31–58 | 1 | |||
| 59–70 | 0.654 ± 0.449 | 1.923 | 0.798–4.635 | 0.145 |
| 70–78 | 1.045 ± 0.411 | 2.842 | 1.269–6.363 | 0.0111 |
| 79–90 | 1.244 ± 0.382 | 3.469 | 1.641–7.333 | 0.0011 |
| Gene Expression | ||||
| Cluster1 | 1 | |||
| Cluster2 | 0.970 ± 0.454 | 2.638 | 1.083–6.429 | 0.0328 |
| Cluster3 | 2.404 ± 0.551 | 11.067 | 3.758–32.591 | 1.28 e-5 |
| Cluster4 | 0.597 ± 1.160 | 1.817 | 0.187–17.641 | 0.606 |
| DNA Methylation | ||||
| Cluster1 | 1 | |||
| Cluster2 | −0.138 ± 0.576 | 0.871 | 0.281–2.695 | 0.811 |
| Cluster3 | 0.764 ± 0.577 | 2.146 | 0.693–6.645 | 0.185 |
| Cluster4 | 0.352 ± 0.465 | 1.423 | 0.572–3.539 | 0.449 |
| Cluster5 | −0.132 ± 0.667 | 0.876 | 0.237–3.239 | 0.843 |
| Cluster6 | −0.895 ± 0.604 | 0.409 | 0.125–1.336 | 0.139 |
| Cluster7 | − 0.397 ± 0.673 | 0.672 | 0.180–2.514 | 0.555 |
| Cluster8 | −1.960 ± 1.128 | 0.141 | 0.0155–1.284 | 0.0822 |
| Cluster9 | −1.848 ± 0.809 | 0.157 | 0.0323–0.769 | 0.0223 |
| Cluster10 | −1.015 ± 0.732 | 0.362 | 0.0863–1.521 | 0.165 |
| miRNA Expression | ||||
| Cluster1 | 1 | |||
| Cluster2 | 0.527 ± 0.341 | 1.693 | 0.867–3.305 | 0.123 |
| Cluster3 | 0.276 ± 0.450 | 1.318 | 0.546–3.182 | 0.539 |
| Cluster4 | −0.669 ± 0.503 | 0.512 | 0.191–1.373 | 0.184 |
Origin concordance: 0.8345; bias-corrected concordance: 0.7604
SE standard error, HR hazard ratio, CI confidence interval
The p-values of the likelihood ratio test, the score test and the Wald test are plotted in Fig. 3b; these plots indicate that each combination of covariates had a significant effect on each prognostic model. However, using omics data alone as covariates had a reduced effect.
Prognostic performance of the models based on Uno’s C-index
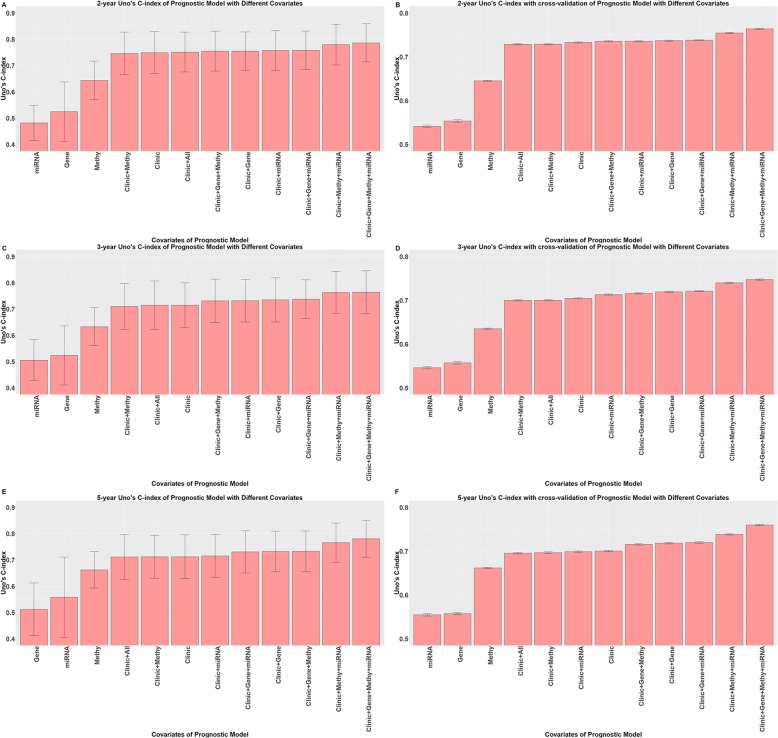
We calculated 3-year and 5-year Uno’s C-index values for all 12 prognostic models. In addition, as the median survival time of the dataset was approximately 26 months, the 2-year Uno’s C-index was also inferenced. The 2 year Uno’s C-indexes without and with cross-validation are shown in Fig. 4a and b, respectively. The 3-year Uno’s C-indexes without and with cross-validation are shown in Fig. 4c and d, respectively. The 5-year Uno’s C-index without and with cross-validation are shown in Fig. 4e and f, respectively. The difference in the 2-year, 3-year and 5-year Uno’s C-indexes with 95% CI are summarized in Table 5, with p values of the likelihood ratio tests between different prognostic models. The results of the Wilcoxon signed-rank test for the differences in the C-indexes of different models further confirmed that our prognostic model showed the best prognostic performance, as summarized in Table 6.
Fig. 4.
The 2-year, 3-year and 5-year Uno’s C-index of different prognostic models. a 2-year Uno’s C-index of prognostic models with different covariates; b 2-year Uno’s C-index with cross-validation of prognostic models with different covariates; c 3-year Uno’s C-index of prognostic models with different covariates; d 3-year Uno’s C-index with cross-validation of prognostic models with different covariates; e 5-year Uno’s C-index of prognostic models with different covariates; f 5-year Uno’s C-index with cross-validation of prognostic models with different covariates
Table 5.
Difference in discriminative performance between our prognostic model and other models
| Comparison | 2-year ∆C ± 95% CI | 3-year ∆C ± 95% CI | 5-year ∆C ± 95% CI | P value of LRT |
|---|---|---|---|---|
| CGMm vs CMm | 0.0067 ± 0.027 | 0.0010 ± 0.040 | 0.0152 ± 0.033 | 0.00147 |
| CGMm vs CGM | 0.0317 ± 0.033 | 0.0328 ± 0.032 | 0.0480 ± 0.047 | 0.000217 |
| CGMm vs CGm | 0.0284 ± 0.035 | 0.0266 ± 0.035 | 0.0497 ± 0.054 | 0.000582 |
| CGMm vs CA | 0.0349 ± 0.040 | 0.0497 ± 0.040 | 0.0694 ± 0.057 | 0.000312 |
| CGMm vs CG | 0.0315 ± 0.037 | 0.0293 ± 0.031 | 0.0485 ± 0.049 | 0.000203 |
| CGMm vs CM | 0.0402 ± 0.041 | 0.0541 ± 0.042 | 0.0687 ± 0.056 | 6.919 e-7 |
| CGMm vs Cm | 0.0291 ± 0.044 | 0.0324 ± 0.045 | 0.0654 ± 0.060 | 1.528 e-6 |
| CGMm vs C | 0.0374 ± 0.040 | 0.0496 ± 0.042 | 0.0683 ± 0.054 | 2.335 e-6 |
| CGMm vs G | 0.262 ± 0.12 | 0.241 ± 0.13 | 0.268 ± 0.12 | 2.178 e-12 |
| CGMm vs M | 0.143 ± 0.076 | 0.131 ± 0.079 | 0.119 ± 0.069 | 3.426 e-10 |
| CGMm vs m | 0.305 ± 0.10 | 0.259 ± 0.11 | 0.223 ± 0.15 | 7.776 e-13 |
| CMm vs CG | 0.0247 ± 0.042 | 0.0284 ± 0.055 | 0.0333 ± 0.056 | 0.0118 |
| CMm vs Cm | 0.0224 ± 0.035 | 0.0314 ± 0.040 | 0.0502 ± 0.054 | 8.658 e-5 |
| CMm vs C | 0.0307 ± 0.040 | 0.0273 ± 0.052 | 0.0531 ± 0.061 | 0.000130 |
| CG vs C | 0.00591 ± 0.030 | 0.0203 ± 0.032 | 0.0198 ± 0.028 | 0.000689 |
| Cm vs C | 0.00825 ± 0.024 | 0.0173 ± 0.036 | 0.00290 ± 0.029 | 0.270 |
∆C difference in C-index, CI confidence interval, LRT likelihood ratio test;
In the Comparisons column, C stands for clinical, G for gene expression, M for DNA methylation and m for miRNA expression. The words on both sides of vs are the covariates in prognostic model
Table 6.
Wilcoxon signed-rank test of difference in C-index distribution between our prognostic model and other models
| Comparison | P value of the 2-year C-index | P value of the 3-year C-index | P value of the 5-year C-index | P value of the bootstrap results |
|---|---|---|---|---|
| CGMm vs CMm | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| CGMm vs CGM | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | 1.091 e-5 |
| CGMm vs CGm | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | 0.000102 |
| CGMm vs CA | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | 5.028 e-12 |
| CGMm vs CG | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| CGMm vs CM | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| CGMm vs Cm | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| CGMm vs C | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| CGMm vs G | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| CGMm vs M | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| CGMm vs m | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| CMm vs CG | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | 0.0209 |
| CMm vs Cm | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | 0.00161 |
| CMm vs C | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | 1.452 e-7 |
| CG vs C | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| Cm vs C | 3.413 e-16 | < 2.2 e-16 | 0.00323 | 7.012 e-13 |
In the Comparison column, C stands for clinical, G for gene expression, M for DNA methylation and m for miRNA expression. The words on both sides of vs are the covariates in the prognostic model
In summary, these results clearly indicate that among all models, our prognostic model showed the best discriminative performance. Both the likelihood ratio test and the Wilcoxon signed-rank test of difference between distributions of C-index of these two models suggest our prognostic model owned better prognostic performance. In addition, paired comparisons of prognostic model with only clinical covariates, the best prognostic model with clinical covariates and one type of omics data and the best prognostic model with clinical covariates and two types of omics data suggested that the more types of omics data that were used, the better the prognostic performance was.
Evaluation of the contribution of each covariate in our prognostic model
We investigated how the performance of our prognostic model changed after one of the covariates was removed. The same evaluation procedures were used to compare the performance of our prognostic model with that of the model with one covariate removed.
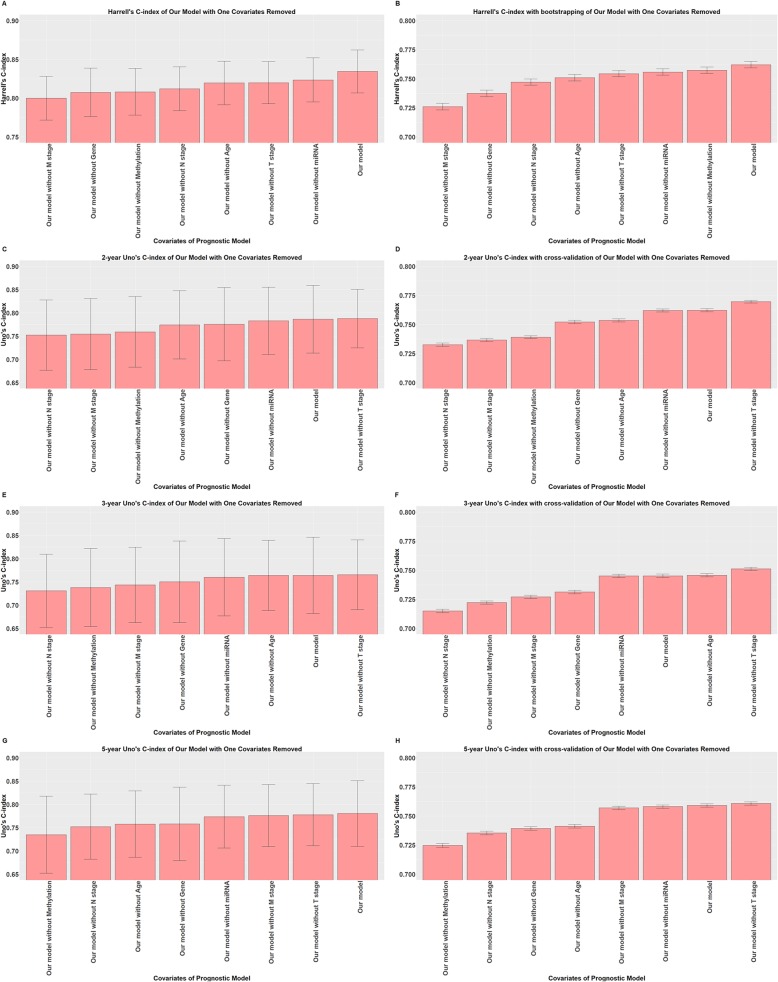
The results of the comparison of the Uno’s C-index without cross-validation and the likelihood ratio test are summarized in Table 7 and shown in Fig. 5c, e and g, and the results of the Harrell’s C-index without bootstrapping are shown in Fig. 5a. The likelihood ratio test suggested that only removing miRNA expression caused no significant difference in the model. In addition, the 2-year, 3-year and 5-year Uno’s C-index without cross-validation all suggested that removing miRNA expression would cause a negligible decrease. However, the 2-year and 3-year Uno’s C-index without cross-validation both suggested that removing T stage would cause a slight improvement, while the 5-year Uno’s C-index without cross-validation suggested that removing miRNA expression would cause a numerically larger decrease than removing T stage.
Table 7.
Difference in performance of our prognostic model and the model with one covariate removed
| Comparison | 2-year ∆C ± 95% CI | 3-year ∆C ± 95% CI | 5-year ∆C ± 95% CI | P value of LRT |
|---|---|---|---|---|
| Without T stage | −0.00141 ± 0.027 | −0.00135 ± 0.024 | 0.00264 ± 0.021 | 0.0126 |
| Without N stage | 0.0341 ± 0.043 | 0.0332 ± 0.041 | 0.0285 ± 0.037 | 0.00863 |
| Without M stage | 0.0320 ± 0.042 | 0.0203 ± 0.038 | 0.00457 ± 0.031 | 7.755 e-6 |
| Without Age | 0.0121 ± 0.029 | 0.000144 ± 0.034 | 0.0227 ± 0.036 | 0.00688 |
| Without Gene | 0.0108 ± 0.025 | 0.0138 ± 0.024 | 0.0225 ± 0.030 | 0.000133 |
| Without Methylation | 0.0273 ± 0.035 | 0.0260 ± 0.037 | 0.0457 ± 0.052 | 0.000609 |
| Without miRNA | 0.00357 ± 0.011 | 0.00380 ± 0.013 | 0.0068 ± 0.018 | 0.103 |
Fig. 5.
C-indexes of our prognostic model with one covariate removed. a Harrell’s C-index of our prognostic model with one covariate removed; b Harrell’s C-index with bootstrapping of our prognostic model with one covariate removed; c 2-year Uno’s C-index of our prognostic model with one covariate removed; d 2-year Uno’s C-index with cross-validation of our prognostic model with one covariate removed; e 3-year Uno’s C-index of our prognostic model with one covariate removed; f 3-year Uno’s C-index with cross-validation of our prognostic model with one covariate removed; g 5-year Uno’s C-index of our prognostic model with one covariate removed; h 5-year Uno’s C-index with cross-validation of our prognostic model with one covariate removed
The results of the comparison of Harrell’s C-index with bootstrapping and Uno’s C-index with cross-validation are summarized in Table 8 and shown in Fig. 5b, d, f and h. The comparison of Harrell’s C-index with bootstrapping suggested that removing any covariates would cause a significant decrease. In contrast, Uno’s C-index suggested that removing miRNA expression would significantly reduce the model’s performance only at the 5-year time point, while removing T stage would significantly increase the model’s performance at all three time points. In addition, removing age would not affect the discriminative performance of our prognostic model at the 3-year time point.
Table 8.
Test of C-index distribution differences between our prognostic model and model with one covariate removed
| Comparison | P value of the 2-year C-index | P value of the 3-year C-index | P value of the 5-year C-index | P value of bootstrap results |
|---|---|---|---|---|
| Without T stage | < 2.2 e-16 | < 2.2 e-16 | 2.384 e-6 | < 2.2 e-16 |
| Without N stage | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| Without M stage | < 2.2 e-16 | < 2.2 e-16 | 4.5 e-5 | < 2.2 e-16 |
| Without Age | < 2.2 e-16 | 0.228 | < 2.2 e-16 | < 2.2 e-16 |
| Without Gene | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 |
| Without Methylation | < 2.2 e-16 | < 2.2 e-16 | < 2.2 e-16 | 9.179 e-9 |
| Without miRNA | 0.102 | 0.431 | 0.00527 | < 2.2 e-16 |
Based on current analysis pipeline and results, removing miRNA expression from our prognostic model may have a minimal effect on short-term prognostic prediction, but would have a significant effect on long-term prognostic prediction. In addition, removal of T stage had a positive prognostic effect on our model.
Considering the overall evaluation, T stage was the least important covariate of the clinical covariates in our prognostic model, while miRNA expression was the least important covariate of the omics covariates in our prognostic model.
Discussion
First, we successfully performed unsupervised clustering to aggregate patients in our dataset into different groups based on different types of omics data profiles. According to the evaluation of the single-covariate Cox PH model shown in Fig. 3a and b, DNA methylation can be used as a prognostic predictor even when used alone, whereas gene expression and miRNA expression performed relatively poorly on this task.
Then, we integrated the clinical data and used different combinations of omics data by fitting a multi-covariate Cox PH model, and the results confirmed that we had successfully integrated the clinical features, gene expression, DNA methylation and miRNA expression to improve the colon cancer prognostic performance. The evaluation metrics used on the models based on different covariates suggested that combining clinical features and all three types of omics data could offer the best prognostic performance. The p-values of the three tests of the prognostic model were improved, especially the score test, which is consistent with the findings from a previous study [20]. In Table 4, Cluster 3 of gene expression showed the highest HR, thus differential expression analysis and pathway enrichment analysis were conducted based on cluster labels of gene expression, with the edgeR (https://bioconductor.org/packages/release/bioc/html/edgeR.html) and the Database for Annotation, Visualization and Integrated Discovery database (DAVID; version 6.8; david.ncifcrf.gov/). In total, 57 differentially expressed genes were identified, as listed in Additional file 3. These included PRSS2, EPHB6 and FABP4, which showed correlation with colorectal cancer prognosis, whereas high expression of these genes was related to poor prognosis [41–43]. These genes were enriched in Reactome pathway EPH-ephrin mediated repulsion of cells, which might be a potential therapeutic target in colon cancer [44, 45].
Our study indicated that combining clinical covariates with omics data could improve prognostic performance, and that the more types of omics data that were used, the better the improvement was. Compared to a previous study conducted by Zhao et al. [40], our study successfully integrated gene expression, miRNA expression, DNA methylation and clinical features rather than using only gene expression and clinical features. In addition, the integration of clinical and multi-omics data may offer researchers more appealing discoveries than would result from exploring clinical or omics data separately.
This study highlights our ongoing work. Colon cancer prognosis may benefit from the integration of clinical and omics features. However, cooperation among biomedical scientists, oncologists and biologists is necessary for implementing the practical application of a personalized prognostic model. A platform that offers integrative analyses of clinical and omics data and management and storage of clinical and omics data is essential. Our current study approach offers a fundamental framework for this type of platform. In addition, our approach can be easily extended to other types of omics data, such as copy number variations or somatic mutations. We aim to build a classifier based on the identified cluster labels of different omics data and develop a web-based tool for practical application in the coming future. Moreover, we aim to identify patients with good versus poor prognoses with integrated clinical and multi-omics features.
However, our current study was limited by the TCGA-COAD datasets and the use of only three types of omics data and four clinical features. Therefore, we hope to collect omics data from patient follow-ups performed at the hospital. Such collection may provide access to more clinical features, including treatment, larger samples and more types of omics data for analysis. Such advancements may validate the extensibility of this integrative analytic approach. The finding that miRNA expression had a negligible prognostic contribution to the short-term prognosis indicated that we might need a better analysis method for miRNA expression. Based on Uno’s C-index, the contribution of T stage to our prognostic model was questionable, though Harrell’s C-index suggested that T stage had a positive contribution to our prognostic model. These inverse results might be due to the limitation of Uno’s C-index, as there were no events for different T stages except for the T3 stage before the 2-year time point, as shown in Additional file 4. Such phenomenon could also be observed for the covariate age in Additional file 5, as rare events occurred between the 2-year and 3-year time points, causing age to have no significant prognostic contribution at 3-year time point based on Uno’s C-index.
The results suggested that the current C-o-C approach may not be suitable for integrating multi-omics data in our current study [17, 29, 30]. This might be caused by the insufficient use of interactions between different omics data sets in the second layer of clustering or the limitations of our dataset. In addition, our C-o-C approach was carried out separately with the clinical features, which might contain several pieces of information overlapping with the clinical features. More complex methods, such as machine learning methods or deep learning methods, may be good replacements for the current C-o-C approach and may make better use of integrated omics data in combination with clinical features, as has been shown in recent studies applying deep learning methods or similarity network fusion to integrate multi-omics data [46–50].
Conclusion
In conclusion, we applied a pilot integrative prognostic analysis of colon cancer based on clinical features, gene expression, DNA methylation and miRNA expression data. This approach successfully increased the predictive performance of an integrated prognostic model of colon cancer patients compared to the performance achieved using clinical features alone, and all types of omics data had significant effects on the prognostic model. Therefore, our study has the potential to help colon cancer oncologists treat patients more accurately.
Supplementary information
Additional file 1. List of prior knowledge. List of gene symbols for gene expression, gene symbols for DNA methylation and miRNA ids for miRNA expression used as prior knowledge.
Additional file 2: Additional table for the detailed concordance of different prognostic models. Table S1. Origin concordance and bias-corrected concordance of the Cox models with different covariates.
Additional file 3. Differentially expressed genes identified based on cluster labels of gene expression. Differentially expressed genes identified based on cluster labels of gene expression.
Additional file 4. KM-curve of the dataset based on the covariate T stage. KM-curve of the dataset based on the covariate T stage.
Additional file 5. KM-curve of the dataset based on the covariate age. KM-curve of the dataset based on the covariate age.
Acknowledgments
This work was supported by the National Natural Science Foundation of China [No. 81771936, No. 81801796 and No. 81672916], Major Scientific Project of Zhejiang Lab [2018DG0ZX01] and the National Key Research and Development Program of China [No. 2017YFC0908200]. In addition, we acknowledge the TCGA Research Network and all staff members involved in the TCGA Project for providing the data.
Abbreviations
- AJCC
American Joint Committee on Cancer
- CI
Confidence Interval
- C-index
Concordance statistic
- COAD
Colon Adenocarcinoma
- C-o-C
Cluster of Clusters
- CRC
Colorectal Cancer
- FPKM
Fragments per Kilobase of Transcript per Million Mapped Reads
- GBM
Glioblastoma Multiforme
- HM27
Illumina Infinium Human Methylation 27
- HM450
Illumina Infinium Human Methylation 450
- HR
Hazard Ratio
- KEGG
Kyoto Encyclopedia of Genes and Genomes
- M
Metastatic Status
- MMR
Mismatch Repair
- MSI
Microsatellite Instability
- N
Lymph Node Status
- NCCN
National Comprehensive Cancer Network
- PH
Proportional Hazards
- RPM
Reads per Million Mapped Reads
- T
Tumor Invasion Depth
- TCGA
The Cancer Genome Atlas
- TNM
Tumor, Node, Metastasis
Authors’ contributions
DT and YT contributed to the conception of the study. DT, TZ, JL and QY performed the data preparation. DT and YT performed the data analyses and wrote the manuscript. JSL and KD provided critical revisions. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81771936 to JSL, No. 81801796 to YT) and Major Scientific Project of Zhejiang Lab (2018DG0ZX01 to JSL), which provide financial support in the design of study, analysis of data and writing the manuscript, the National Natural Science Foundation of China (No. 81672916 to JL) and the National Key Research and Development Program of China (No. 2017YFC0908200 to KD), which provide financial support in analysis and interpretation of data.
Availability of data and materials
The dataset analysed during the current study is available in the TCGA repository, https://portal.gdc.cancer.gov/repository.
Ethics approval and consent to participate
The TCGA dataset used and analysed in this study are unrestricted-access, which are available without any permission request through the TCGA portal (https://portal.gdc.cancer.gov/repository). We definitely followed the National Institutes of Health Genomic Data Sharing Policy as well as the National Cancer Institution Genomic Data Sharing Policy in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12911-020-1043-1.
References
- 1.Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, et al. Colorectal cancer statistics, 2017. CA Cancer J Clin. 2017;67(3):177–193. doi: 10.3322/caac.21395. [DOI] [PubMed] [Google Scholar]
- 2.Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Niksic M, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wuchty S, Zhang A, Walling J, Ahn S, Li AG, Quezado M, et al. Gene pathways and subnetworks distinguish between major glioma subtypes and elucidate potential underlying biology. J Biomed Inform. 2010;43(6):945–952. doi: 10.1016/j.jbi.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen YC, Chang YC, Ke WC, Chiu HW. Cancer adjuvant chemotherapy strategic classification by artificial neural network with gene expression data: an example for non-small cell lung cancer. J Biomed Inform. 2015;56:1–7. doi: 10.1016/j.jbi.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Ruffalo M, Husseinzadeh H, Makishima H, Przychodzen B, Ashkar M, Koyuturk M, et al. Whole-exome sequencing enhances prognostic classification of myeloid malignancies. J Biomed Inform. 2015;58:104–113. doi: 10.1016/j.jbi.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Jin H, Lee HC, Park SS, Jeong YS, Kim SY. Serum cancer biomarker discovery through analysis of gene expression data sets across multiple tumor and normal tissues. J Biomed Inform. 2011;44(6):1076–1085. doi: 10.1016/j.jbi.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Zhao LP, Bolouri H. Object-oriented regression for building predictive models with high dimensional omics data from translational studies. J Biomed Inform. 2016;60:431–445. doi: 10.1016/j.jbi.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joe S, Nam H. Prognostic factor analysis for breast cancer using gene expression profiles. BMC Med Inform Decis Mak. 2016;16:9. doi: 10.1186/s12911-016-0292-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guinney J, Dienstmann R, Wang X, de Reyniès A, Schlicker A, Soneson C, et al. The consensus molecular subtypes of colorectal cancer. Nat Med. 2015;21:1350–1356. doi: 10.1038/nm.3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weiser MR. AJCC 8th edition: colorectal Cancer. Ann Surg Oncol. 2018;25(6):1454–1455. doi: 10.1245/s10434-018-6462-1. [DOI] [PubMed] [Google Scholar]
- 11.Giuliano AE, Edge SB, Hortobagyi GN. Eighth edition of the AJCC Cancer staging manual: breast Cancer. Ann Surg Oncol. 2018;25(7):1783–1785. doi: 10.1245/s10434-018-6486-6. [DOI] [PubMed] [Google Scholar]
- 12.Benson AB, Venook AP, Cederquist L, Chan E, Chen Y-J, Cooper HS, et al. Colon Cancer, version 1.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2017;15(3):370–398. doi: 10.6004/jnccn.2017.0036. [DOI] [PubMed] [Google Scholar]
- 13.Network TCGA. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–337. doi: 10.1038/nature11252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim D, Li RW, Dudek SM, Ritchie MD. ATHENA: identifying interactions between different levels of genomic data associated with cancer clinical outcomes using grammatical evolution neural network. BioData Min. 2013;6(1):285–293. doi: 10.1186/1756-0381-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim D, Shin H, Sohn KA, Verma A, Ritchie MD, Kim JH. Incorporating inter-relationships between different levels of genomic data into cancer clinical outcome prediction. Methods. 2014;67(3):344–353. doi: 10.1016/j.ymeth.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim D, Li R, Dudek SM, Ritchie MD. Predicting censored survival data based on the interactions between meta-dimensional omics data in breast cancer. J Biomed Inform. 2015;56:220–228. doi: 10.1016/j.jbi.2015.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoadley KA, Yau C, Wolf DM, Cherniack AD, Tamborero D, Ng S, et al. Multiplatform analysis of 12 Cancer types reveals molecular classification within and across tissues of origin. Cell. 2014;158(4):929–944. doi: 10.1016/j.cell.2014.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoadley KA, Yau C, Hinoue T, Wolf DM, Lazar AJ, Drill E, et al. Cell-of-Origin Patterns Dominate the Molecular Classification of 10,000 Tumors from 33 Types of Cancer. Cell. 2018;173(2):291–304. doi: 10.1016/j.cell.2018.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phan JH, Quo CF, Cheng C, Wang MD. Multiscale integration of -omic, imaging, and clinical data in biomedical informatics. IEEE Rev Biomed Eng. 2012;5:74–87. doi: 10.1109/RBME.2012.2212427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang SJ, Yee C, Ching T, Yu H, Garmire LX. A novel model to combine clinical and pathway-based Transcriptomic information for the prognosis prediction of breast Cancer. PLoS Comput Biol. 2014;10(9):e1003851. doi: 10.1371/journal.pcbi.1003851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malhotra K, Navathe SB, Chau DH, Hadjipanayis C, Sun JM. Constraint based temporal event sequence mining for Glioblastoma survival prediction. J Biomed Inform. 2016;61:267–275. doi: 10.1016/j.jbi.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 22.Exarchos KP, Goletsis Y, Fotiadis DI. A multiscale and multiparametric approach for modeling the progression of oral cancer. BMC Med Inform Decis Mak. 2012;12(1):136. doi: 10.1186/1472-6947-12-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singer F, Irmisch A, Toussaint NC, Grob L, Singer J, Thurnherr T, et al. SwissMTB: establishing comprehensive molecular cancer diagnostics in Swiss clinics. BMC Med Inform Decis Mak. 2018;18(1):89. doi: 10.1186/s12911-018-0680-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chi SQ, Tian Y, Li J, Tong DY, Kong XX, Poston G, et al. Time-dependent and nonlinear effects of prognostic factors in nonmetastatic colorectal cancer. Cancer Medicine. 2017;6(8):1882–1892. doi: 10.1002/cam4.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Okugawa Y, Grady WM, Goel A. Epigenetic Alterations in Colorectal Cancer: Emerging Biomarkers. Gastroenterology. 2015;149(5):1204–1225. doi: 10.1053/j.gastro.2015.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lao VV, Grady WM. Epigenetics and colorectal Cancer. Nat Rev Gastroenterol Hepatol. 2011;8(12):686–700. doi: 10.1038/nrgastro.2011.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taby R, Issa JP. Cancer epigenetics. CA Cancer J Clin. 2010;60(6):376–392. doi: 10.3322/caac.20085. [DOI] [PubMed] [Google Scholar]
- 28.Wei L, Jin ZL, Yang SJ, Xu YX, Zhu YT, Ji Y. TCGA-assembler 2: software pipeline for retrieval and processing of TCGA/CPTAC data. Bioinformatics. 2018;34(9):1615–1617. doi: 10.1093/bioinformatics/btx812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Network TCGA. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490(7418):61–70. doi: 10.1038/nature11412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu G, Dong CP, Liu L. Integrated multiple "-omics" data reveal subtypes of hepatocellular carcinoma. PLoS One. 2016;11(11):e0165457. doi: 10.1371/journal.pone.0165457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harrell FE, Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA-J Am Med Assoc. 1982;247(18):2543–2546. doi: 10.1001/jama.1982.03320430047030. [DOI] [PubMed] [Google Scholar]
- 32.Uno H, Cai T, Pencina MJ, D'Agostino RB, Wei LJ. On the C-statistics for evaluating overall adequacy of risk prediction procedures with censored survival data. Stat Med. 2011;30(10):1105–1117. doi: 10.1002/sim.4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Riester M, Taylor JM, Feifer A, Koppie T, Rosenberg JE, Downey RJ, et al. Combination of a novel gene expression signature with a clinical Nomogram improves the prediction of survival in high-risk bladder Cancer. Clin Cancer Res. 2012;18(5):1323–1333. doi: 10.1158/1078-0432.CCR-11-2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grambsch PM, Therneau TM. Proportional hazards tests and diagnosis based on weighted residuals. Biometrika. 1994;81(3):515–526. doi: 10.1093/biomet/81.3.515. [DOI] [Google Scholar]
- 35.Devarajan K, Ebrahimi N. Testing for covariate effect in the cox proportional hazards regression model. Commun Stat-Theory Methods. 2009;38(14):2333–2347. doi: 10.1080/03610920802536958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith GCS, Seaman SR, Wood AM, Royston P, White IR. Correcting for optimistic prediction in small data sets. Am J Epidemiol. 2014;180(3):318–324. doi: 10.1093/aje/kwu140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rudloff U, Jacks LM, Goldberg JI, Wynveen CA, Brogi E, Patil S, et al. Nomogram for predicting the risk of local recurrence after breast-conserving surgery for ductal carcinoma in situ. J Clin Oncol. 2010;28(23):3762–3769. doi: 10.1200/JCO.2009.26.8847. [DOI] [PubMed] [Google Scholar]
- 38.Albert JM, Liu DD, Shen Y, Pan IW, Shih Y-CT, Hoffman KE, et al. Nomogram to predict the benefit of radiation for older patients with breast Cancer treated with conservative surgery. J Clin Oncol. 2012;30(23):2837–2843. doi: 10.1200/JCO.2011.41.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rose PG, Java J, Whitney CW, Stehman FB, Lanciano R, Thomas GM, et al. Nomograms predicting progression-free survival, overall survival, and pelvic recurrence in locally advanced cervical Cancer developed from an analysis of identifiable prognostic factors in patients from NRG oncology/gynecologic oncology group randomized trials of Chemoradiotherapy. J Clin Oncol. 2015;33(19):2136–2142. doi: 10.1200/JCO.2014.57.7122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhao Q, Shi X, Xie Y, Huang J, Shia B, Ma S. Combining multidimensional genomic measurements for predicting cancer prognosis: observations from TCGA. Brief Bioinform. 2015;16(2):291–303. doi: 10.1093/bib/bbu003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lukkonen A, Sorsa T, Salo T, Tervahartiala T, Koivunen E, Golub L, et al. Down-regulation of trypsinogen-2 expression by chemically modified tetracyclines: association with reduced cancer cell migration. Int J Cancer. 2000;86(4):577–581. doi: 10.1002/(SICI)1097-0215(20000515)86:4<577::AID-IJC21>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 42.Xu D, Yuan L, Liu X, Li MQ, Zhang FB, Gu XY, et al. EphB6 overexpression and Apc mutation together promote colorectal cancer. Oncotarget. 2016;7(21):31111–21. doi: 10.18632/oncotarget.9080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang YQ, Zhao XT, Deng LL, Li XT, Wang GB, Li YX, et al. High expression of FABP4 and FABP6 in patients with colorectal cancer. World J Surg Oncol. 2019;17(1):13. doi: 10.1186/s12957-019-1559-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lodola A, Giorgio C, Incerti M, Zanotti I, Tognolini M. Targeting Eph/ephrin system in cancer therapy. Eur J Med Chem. 2017;142:152–162. doi: 10.1016/j.ejmech.2017.07.029. [DOI] [PubMed] [Google Scholar]
- 45.DiPrima Michael, Wang Dunrui, Tröster Alix, Maric Dragan, Terrades‐Garcia Nekane, Ha Taekyu, Kwak Hyeongil, Sanchez‐Martin David, Kudlinzki Denis, Schwalbe Harald, Tosato Giovanna. Identification of Eph receptor signaling as a regulator of autophagy and a therapeutic target in colorectal carcinoma. Molecular Oncology. 2019;13(11):2441–2459. doi: 10.1002/1878-0261.12576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liang MX, Li ZZ, Chen T, Zeng JY. Integrative data analysis of multi-platform Cancer data with a multimodal deep learning approach. IEEE-ACM Trans Comput Biol Bioinform. 2015;12(4):928–937. doi: 10.1109/TCBB.2014.2377729. [DOI] [PubMed] [Google Scholar]
- 47.Chaudharyl K, Poirionl OB, Lu LQ, Garmire LX. Deep learning-based multi-Omics integration robustly predicts survival in liver Cancer. Clin Cancer Res. 2018;24(6):1248–1259. doi: 10.1158/1078-0432.CCR-17-0853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Poirion OB, Chaudhary K, Garmire LX. Deep learning data integration for better risk stratification models of bladder cancer. AMIA Joint Summits on Translational Science proceedings AMIA Joint Summits on Translational Science. 2017;2018:197–206. [PMC free article] [PubMed] [Google Scholar]
- 49.Wang B, Mezlini AM, Demir F, Fiume M, Tu Z, Brudno M, et al. Similarity network fusion for aggregating data types on a genomic scale. Nat Meth. 2014;11(3):333–337. doi: 10.1038/nmeth.2810. [DOI] [PubMed] [Google Scholar]
- 50.Zizzo AN, Erdman L, Feldman BM, Goldenberg A. Similarity Network fusion a novel application to making clinical diagnoses. Rheum Dis Clin N Am. 2018;44(2):285–293. doi: 10.1016/j.rdc.2018.01.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. List of prior knowledge. List of gene symbols for gene expression, gene symbols for DNA methylation and miRNA ids for miRNA expression used as prior knowledge.
Additional file 2: Additional table for the detailed concordance of different prognostic models. Table S1. Origin concordance and bias-corrected concordance of the Cox models with different covariates.
Additional file 3. Differentially expressed genes identified based on cluster labels of gene expression. Differentially expressed genes identified based on cluster labels of gene expression.
Additional file 4. KM-curve of the dataset based on the covariate T stage. KM-curve of the dataset based on the covariate T stage.
Additional file 5. KM-curve of the dataset based on the covariate age. KM-curve of the dataset based on the covariate age.
Data Availability Statement
The dataset analysed during the current study is available in the TCGA repository, https://portal.gdc.cancer.gov/repository.