Abstract
De winter pattern on the ECG is associated with occlusion of proximal left anterior descending artery. It is an atypical presentation of acute myocardial infarction due to LAD occlusion. We report a case due to thromboembolic occlusion of LAD after chemical cardioversion. It is imperative for cardiologists and physicians to instantly identify the De Winter pattern on ECG to appropriately triage these patients without delay.
Keywords: Coronary angiography, palpitation, thromboembolic, winter T-wave pattern
INTRODUCTION
De Winter pattern has been described in literature as associated with occlusion of proximal left anterior descending artery (LAD) and acute anterior myocardial infarction.
Initially reported in 2008 by De Winter et al. as upsloping ST-segment depression at the J point with tall, peaked T waves in precordial leads.[1,2] It is recorded in 2% of cases with LAD occlusion.[1]
Patients requiring percutaneous coronary intervention (PCI) to LAD with De Winter pattern on electrocardiogram (ECG) were noted to be younger males with a higher incidence of hypercholesterolemia.[3]
De Winter pattern is highly predictive of acute LAD occlusion with a positive predictive value of 95%–100%.[4] While it may precede ST-segment elevation, it is imperative for cardiologists and physicians to instantly identify the De Winter pattern on ECG to appropriately triage these patients without delay. Some have also proposed to consider De Winter ECG pattern as a STEMI equivalent as it warrants emergent reperfusion therapy with PCI or thrombolysis.[3,5]
To the best of our knowledge, this case is the first presentation of De Winter pattern due to thromboembolic event to coronary artery after chemical cardioversion in a patient found to have rheumatic mitral valve stenosis and left atrial appendage thrombus.
CASE PRESENTATION
A 35-year-old male patient presented to the emergency department (ED) of the primary health center with a complaint of new-onset of palpitations. Initial ECG revealed atrial flutter with the rapid ventricular response (heart rate 160/min) for which he received 5 mg intravenous (IV) verapamil. The ventricular response was controlled. Subsequently, he developed another episode of fast atrial flutter. 300 mg IV amiodarone was given and he reverted to sinus rhythm. However, after he reverted to sinus rhythm, his cardiovascular examination was significant for soft S1, loud S2, and 1/6 diastolic rumble in apex. Transthoracic echocardiography showed ejection fraction of 41%, mild global hypokinesia, severe mitral stenosis.
On the second day of admission, he developed severe retrosternal chest pain with diaphoresis. ECG showed upsloping ST depression with hyperacute symmetrical T wave in leads V3 to V5 at the J point [Figure 1], suggestive of De Winter sign. Subsequently, he underwent urgent coronary angiography, which revealed fresh thrombus in the second diagonal. He underwent balloon angioplasty. He was restored to TIMI III flow [Figures 2 and 3]. Transesophageal echocardiography showed severely dilated left atrium with thrombus in the left atrial appendage [Figure 4]. He was discharged on oral anticoagulation therapy with follow-up in the outpatient valve clinic for mitral valve intervention.
Figure 1.
Electrocardiogram showed sinus rhythm with upsloping ST segment depression by ≥0.7 mV at the V 4–5 leads, and tall and symmetrical T waves, a J point rise of 0.5 mm at lead AVR. All these electrocardiogram changes represent De Winter T wave pattern
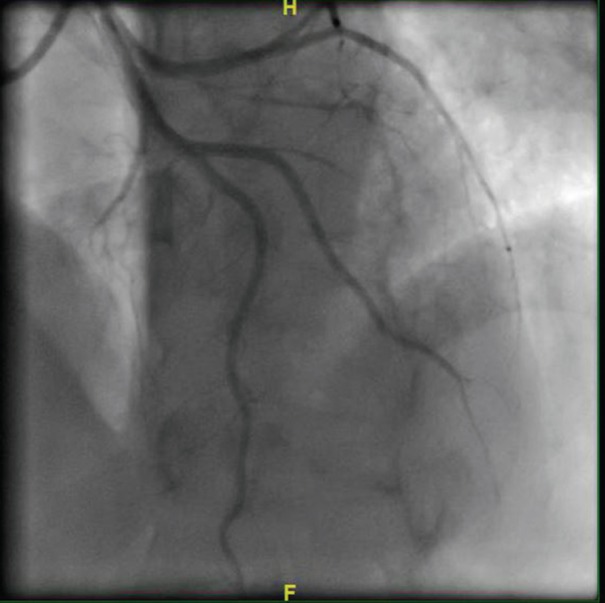
Figure 2.
Thrombotic occlusion of second diagonal branch of left anterior descending artery
Figure 3.
Transesophageal echocardiogram findings of left atrial appendage thrombus in patient with rheumatic mitral valve disease
Figure 4.
Second diagonal branch of left anterior descending artery after coronary intervention with thrombus aspiration. TIMI III flow achieved
DISCUSSION
De Winter ECG pattern in anterior and inferior leads has been previously reported as highly predictive of LAD or right coronary artery occlusion in patients found to have coronary artery disease.[6,7] To the best of our knowledge, this is the first reported case of De Winter pattern involving anterior-lateral leads due to thromboembolic event after chemical cardioversion rather than atherosclerotic coronary artery disease.
While the exact pathophysiologic mechanism of De Winter ECG pattern is unknown, it is stipulated to be associated with endocardial conduction delay due to anatomical variation of Purkinje fibers.[1] Another hypothesis suggests that the absence of ST elevation in De Winter sign may be attributed to ischemia-induced Intracellular adenosine triphosphate (ATP) depletion, which possibly results in a lack of activation of ATP-sensitive potassium channels in the cardiac sarcolemma.[8] Other authors reported De Winter pattern may be attributed to residual flow owing to subtotal occlusion, thrombotic cascade phases, variations in coronary anatomy, collateral recruitment, and recurrent ischemic episodes with preconditioning.[9,10]
The ECG presentation of De Winter pattern may appear similar to hyperacute T-waves as noted in hyperkalemia or early ischemia after total coronary artery occlusion; however, there is usually a complete resolution of hyperacute T-waves within minutes, whereas De Winter pattern may last until primary percutaneous intervention or change into ST-segment elevation.[3]
Previously reported cases illustrated the occurrence of De Winter pattern within 1.5 h of chest pain; however, recent cases reported the prolonged duration of about 5 h before the occurrence of De Winter pattern. Primarily, it was perceived that De Winter pattern persists from initial ECG until reperfusion therapy; however, recent reports illustrated that it may evolve into STEMI or may follow the ECG manifestations of STEMI.[11,12]
In our case, the patient was chemically cardioverted considering the first episode of atrial flutter in initial ECGs and no prior history of palpitations with lack of obvious clinical findings supporting severe mitral stenosis at presentation, but after chemical cardioversion, his cardiovascular clinical exam suggests that he has the valvular disease which was confirmed by transthoracic echocardiography. Transesophageal echocardiography confirmed that there is thrombus in the left atrial appendage. It is most likely that diagonal artery thrombotic occlusion is due to thromboembolisation event from the left atrial appendage.
Patterns of ST-T changes that are not typical or classical for STEMI may conjure a diagnostic dilemma. De Winter ECG pattern may be overlooked due to its relative infrequency, and delayed diagnosis can result in higher mortality due to increased total ischemic duration.[13] Owing to its high positive predictive value for anterior myocardial infarction due to acute LAD occlusion and the need for urgent action, it must be emphasized that cardiologists as well as emergency and internal medicine physicians should be well-trained to rapidly identify this ECG pattern and activate the pathway for emergent reperfusion as they would in a case of acute STEMI.[14,15]
Since 2008, many cases have been reported of De winter sign T-wave in the context of acute anterior myocardial ST-segment elevation myocardial infarction. In 2018, one case report showed the case of De Winter sign in a patient with left main coronary artery occlusion. However, there were no cases of De Winter ECG pattern as a result of the embolic event.
CONCLUSION
De Winter ECG is an atypical presentation of acute myocardial infarction due to LAD occlusion, which some authors propose to be considered as a STEMI equivalent. The timely diagnosis must be emphasized with immediate activation for emergent reperfusion therapy. This case report highlights that this ECG phenomenon is not exclusive to LAD occlusion by atherosclerotic disease but can also be caused by coronary artery thromboembolism.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.de Winter RJ, Verouden NJ, Wellens HJ, Wilde AA Interventional Cardiology Group of the Academic Medical Center. A new ECG sign of proximal LAD occlusion. N Engl J Med. 2008;359:2071–3. doi: 10.1056/NEJMc0804737. [DOI] [PubMed] [Google Scholar]
- 2.Littmann L. The Dressler – De Winter sign of acute proximal LAD occlusion. J Electrocardiol. 2018;51:138–9. doi: 10.1016/j.jelectrocard.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 3.Verouden NJ, Koch KT, Peters RJ, Henriques JP, Baan J, van der Schaaf RJ, et al. Persistent precordial “hyperacute” T-waves signify proximal left anterior descending artery occlusion. Heart. 2009;95:1701–6. doi: 10.1136/hrt.2009.174557. [DOI] [PubMed] [Google Scholar]
- 4.Morris NP, Body R. The De Winter ECG pattern: Morphology and accuracy for diagnosing acute coronary occlusion: Systematic review. Eur J Emerg Med. 2017;24:236–42. doi: 10.1097/MEJ.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 5.Rokos IC, French WJ, Mattu A, Nichol G, Farkouh ME, Reiffel J, et al. Appropriate cardiac cath lab activation: Optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction. Am Heart J. 2010;160:995–1003. doi: 10.1016/j.ahj.2010.08.011. 1003.e1-8. [DOI] [PubMed] [Google Scholar]
- 6.Carrington M, Santos AR, Picarra BC, Pais JA. De Winter pattern: A forgotten pattern of acute LAD artery occlusion. BMJ Case Rep 2018. 2018 doi: 10.1136/bcr-2018-226413. pii: Bcr-2018-226413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karna S, Chourasiya M, Chaudhari T, Bakrenia S, Patel U. De Winter sign in inferior leads: A rare presentation. Heart Views. 2019;20:25–7. doi: 10.4103/HEARTVIEWS.HEARTVIEWS_4_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li RA, Leppo M, Miki T, Seino S, Marbán E. Molecular basis of electrocardiographic ST-segment elevation. Circ Res. 2000;87:837–9. doi: 10.1161/01.res.87.10.837. [DOI] [PubMed] [Google Scholar]
- 9.Sunbul M, Erdogan O, Yesildag O, Mutlu B. De Winter sign in a patient with left main coronary artery occlusion. Postepy Kardiol Interwencyjnej. 2015;11:239–40. doi: 10.5114/pwki.2015.54019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Donato M, Evelson P, Gelpi RJ. Protecting the heart from ischemia/reperfusion injury: An update on remote ischemic preconditioning and postconditioning. Curr Opin Cardiol. 2017;32:784–90. doi: 10.1097/HCO.0000000000000447. [DOI] [PubMed] [Google Scholar]
- 11.Pranata R, Huang I, Damay V. Case Reports in Cardiology. Hindawi: 2018. Should de Winter T-Wave electrocardiography pattern be treated as ST-segment elevation myocardial infarction equivalent with consequent reperfusion? A dilemmatic experience in rural area of Indonesia. Article ID 6868204, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goebel M, Bledsoe J, Orford JL, Mattu A, Brady WJ. A new ST-segment elevation myocardial infarction equivalent pattern? Prominent T wave and J-point depression in the precordial leads associated with ST-segment elevation in lead aVr. Am J Emerg Med. 2014;32:287.e5–8. doi: 10.1016/j.ajem.2013.09.037. [DOI] [PubMed] [Google Scholar]
- 13.Denktas AE, Anderson HV, McCarthy J, Smalling RW. Total ischemic time: The correct focus of attention for optimal ST-segment elevation myocardial infarction care. JACC Cardiovasc Interv. 2011;4:599–604. doi: 10.1016/j.jcin.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Rao MY, Wang YL, Zhang GR, Zhang Y, Liu T, Guo AJ, et al. Thrombolytic therapy to the patients with de Winter electrocardiographic pattern, is it right? QJM. 2018;111:125–7. doi: 10.1093/qjmed/hcx253. [DOI] [PubMed] [Google Scholar]
- 15.Xu W, Xu L, Peng J, Huang S. Thrombolytic therapy in a patient with chest pain with de Winter ECG pattern occurred after ST-segment elevation: A case report. J Electrocardiol. 2019;56:4–6. doi: 10.1016/j.jelectrocard.2019.06.010. [DOI] [PubMed] [Google Scholar]