Abstract
Background
Practice management is an overlooked and undertaught subject in medical education. Many physicians feel that their exposure to billing education during residency training was inadequate. The purpose of this study was to compare resident and staff physicians in terms of their billing knowledge and exposure to billing education during residency training.
Methods
Senior residents and staff physicians completed a scenario-based clinical billing assessment. Posttest surveys were completed to determine exposure to practice management and billing education during training.
Results
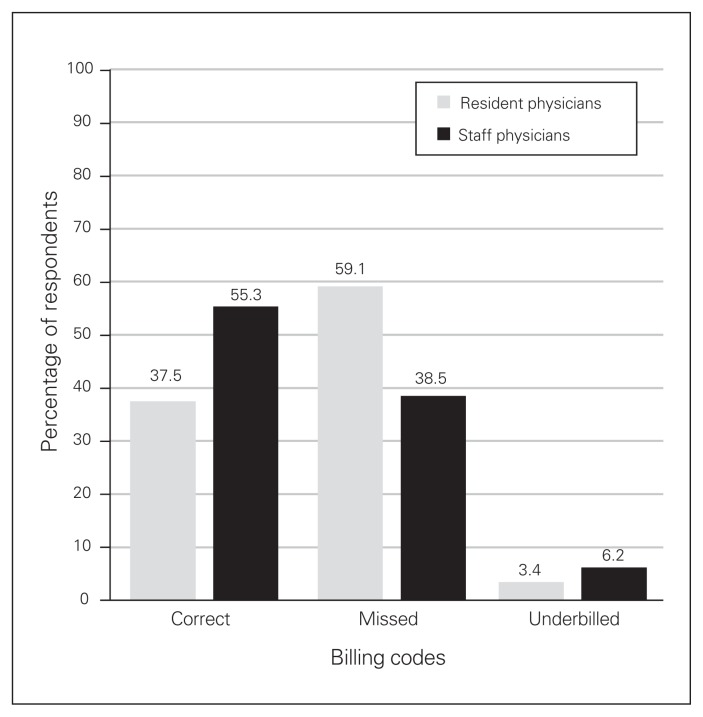
A total of 16 resident physicians and 17 staff physicians completed the billing assessment. Overall, the billing accuracy of respondents was poor. Staff physicians had a greater percentage of correct billing codes (55.3% v. 37.5%, p < 0.001) and underbilled codes (6.2% v. 3.4%, p = 0.009), with fewer missed billing codes (38.5% v. 59.1%, p < 0.001), compared with resident physicians. The percentage value of correct billings was significantly higher for staff physicians (71.5% v. 56.8%, p = 0.01). In the posttest survey, 100.0% of residents and 79.0% of staff physicians desired more billing education during training.
Conclusion
In general, staff physicians billed more accurately than resident physicians, but even experienced staff physicians missed a substantial amount of potential revenue because of billing errors and omissions. The majority of the residents and staff physicians who participated in our study felt that current billing education is both insufficient and ineffective. Incorporating practice management and billing education into residency training is critical to ensure that the next generation of medical trainees possess the financial competence to required to manage a successful medical practice.
Abstract
Contexte
La gestion médicale est un sujet souvent oublié et trop peu enseigné durant les études de médecine. Beaucoup de médecins ont l’impression que la formation sur la facturation offerte durant leur résidence était insuffisante. L’objectif de cette étude était de comparer les connaissances sur la facturation et l’exposition, durant la résidence, à la formation sur ce sujet des résidents et des médecins membres du personnel.
Méthodes
Les résidents seniors et les médecins membres du personnel ont effectué une évaluation de facturation clinique à partir de mises en situation. Ils ont répondu à un sondage après le test pour déterminer leur exposition à la formation sur la gestion médicale et la facturation durant leurs études.
Résultats
Au total, 16 médecins résidents et 17 médecins membres du personnel ont fait l’évaluation de facturation. Dans l’ensemble, l’exactitude de leur facturation était faible. Les médecins membres du personnel avaient un pourcentage plus élevé de codes de facturation corrects (55,3 % contre 37,5 %, p < 0,001) et de codes de facturation insuffisants (6,2 % contre 3,4 %, p = 0,009), et avaient moins de codes manquants (38,5 % contre 59,1 %, p < 0,001), comparativement aux médecins résidents. Le pourcentage de facturations correctes était significativement plus élevé chez les médecins membres du personnel (71,5 % contre 56,8 %, p = 0,01). Dans le sondage post-test, 100,0 % des résidents et 79,0 % des médecins membres du personnel désiraient avoir davantage de formation sur la facturation durant les études.
Conclusion
En général, les médecins membres du personnel ont produit des factures plus exactes que les médecins résidents, mais même des médecins membres du personnel expérimentés ont perdu des revenus potentiels considérables en raison d’erreurs de facturation et d’omissions. La majorité des résidents et des médecins membres du personnel qui ont participé à l’étude avaient l’impression que la formation actuelle sur la facturation était à la fois insuffisante et inefficace. Il est essentiel d’intégrer la formation sur la gestion médicale et la facturation dans la résidence pour garantir que la prochaine génération de futurs médecins possède les compétences financières nécessaires pour gérer un cabinet prospère.
Practice management is a taboo subject in medical education. During medical school and residency education, trainees are provided with the knowledge required to care for patients. However, at the completion of this finite training period, when the majority of physicians in Canada and the United States enter practice as self-employed entrepreneurs, most lack the basic financial competence required to effectively manage this small business.
As part of the transition to competency-based medical education, trainees are supposed to receive a “competency-based, outcomes-oriented education.”1 Educating physicians to effectively run a medical practice has been recognized as a core competency in many competency-based educational curricula.1–3 For example, the CanMEDS 2015 Physician Competency Framework labels the ability to “manage career planning, finances, and health human resources in a practice” as a key competency under the Leader role.4
Unfortunately, the practice-management aspect of competency-based medical education remains overlooked and undertaught. Studies have shown that medical trainees and graduates believe that their exposure to billing and practice management education during training was inadequate, even though they feel that these topics are important for practice preparation.5–12 Even program directors and educators have acknowledged the importance of practice management education, although many feel that this subject is difficult to teach.11,13,14 A variety of teaching methods for practice management have been studied, ranging from lecture series to educational weekend retreats, with varying degrees of success.8,14–21
The purpose of this study was (a) to determine the current level of knowledge of surgical resident physicians on topics relating to billing and physician remuneration, (b) to compare the accuracy of residents’ billing with the accuracy of the billing of staff physicians already in independent practice and (c) to explore resident and staff physician experiences and opinions regarding practice management education during residency training.
Methods
Billing assessment and survey design and development
We developed specialty-specific billing assessments, focused on core billing themes (e.g., admissions/consultations, procedures and add-on premiums) for plastic and reconstructive surgery (PRS) and orthopedic surgery (OS). Each billing assessment consisted of 10 hypothetical case-based scenarios. Although the scenarios for PRS and OS differed in content, core billing themes were equally represented on both assessments. The most appropriate responses for each scenario were determined by a professional billing agent and the senior author (H.v.S.) on the basis of the Ontario Ministry of Health and Long-Term Care (MOHLTC) Schedule of Benefits for Physician Services under the Health Insurance Act (SOB). Billing assessment questions were carefully worded to directly reflect the language in the MOHLTC SOB. A total billable value for each scenario was calculated in Canadian dollars on the basis of SOB remuneration values (Oct. 1, 2013, update). The OS assessment contained 65 billable codes (total of $8062.64) and the PRS assessment contained 63 billable codes (total of $10 911.34). Posttest surveys were developed to assess resident and staff physician experiences and opinions of billing and practice management education during residency training.
Participant recruitment
We recruited 2 groups of participants: resident trainees and staff physicians. Subject pools were limited to PRS and OS for feasibility of study design and because of the authors’ affiliations. Senior resident physicians (i.e., postgraduate year 3 or higher) enrolled in PRS and OS at the University of Toronto were contacted through program administrators via institutional email in January 2014. Staff physicians in active practice in Ontario were contacted via email through their provincial (Ontario Orthopaedic Association) or national (Canadian Society of Plastic Surgeons) association in February 2014. All email messages contained a copy of the specialty-specific billing assessment, an up-to-date copy of the MOHLTC SOB for fee coding and a copy of the posttest survey.
Billing assessment and survey analysis
When completing the billing assessment, participants were instructed to write down all billing codes they felt were applicable for each scenario. Participants were given no indication as to the correct number of billable codes for each scenario. The codes selected by the participants in the billing assessment were compared with the most appropriate responses. For their results to be included in this study, participants had to complete all 10 questions in the billing assessment. However, if participants stated that no codes were applicable to a given scenario, this was considered an acceptable response.
Participant responses were classified as correct (their response matched the most appropriate response), underbilled (they suggested an applicable code but not the most appropriate response), overbilled (they suggested an appropriate modifying code combined with an inappropriate base code, resulting in an inflated modifying code value) or incorrect (their response was not appropriate for the scenario). Appropriate codes that were not included in participant responses were deemed missed. For scenarios that involved billing of multiple procedure codes, the highest code was billed at 100% value and all subsequent codes were billed at 85% value as per SOB guidelines. We calculated the total billing values for each scenario, along with the overall total billing value for the entire assessment.
We performed basic statistical calculations using Microsoft Excel (Microsoft Office 2016). Given the differences in the number and value of billable codes between the OS and PRS billing assessments, all results were converted to percentages to allow for direct comparison. We analyzed billing assessment results using a 2-tailed Student t test with statistical significance defined as p < 0.05. Survey responses were analyzed using descriptive statistics. This study was approved by the Health Sciences Research Ethics Board at the University of Toronto.
Results
A total of 16 resident physicians (11 OS, 5 PRS) and 19 staff physicians (6 OS, 13 PRS) completed the billing assessment. Two PRS staff physicians did not adequately complete the billing assessment and were therefore excluded, leaving a total of 17 staff physicians (6 OS, 11 PRS) for final analysis. Response rates for resident physicians in OS and PRS were 42.3% and 38.5%, respectively. Response rates for staff physicians were not calculable, as all communication occurred through the 2 professional organizations, independent of the investigators.
At the time of the study, 25.0% of resident respondents were in their third year of training, 25.0% were in their fourth year of training and 50.0% were in their fifth year of training. Of note, 2 of the third-year and one of the fourth-year respondents in OS were enrolled in a 4-year training program. Regarding staff physician experience, 10.5% of staff respondents had been in practice 1–2 years, 0.0% in practice 3–5 years, 31.6% in practice 6–10 years, 36.8% in practice 11–20 years and 21.1% in practice over 20 years.
Overall, the accuracy of the billing assessments was poor (Fig. 1). On average, staff physicians had a higher percentage of correct codes (55.3% v. 37.5%, p < 0.001), a higher percentage of underbilled codes (6.2% v. 3.4%, p = 0.009) and fewer missed codes (38.5% v. 59.1%, p < 0.001) compared with resident physicians. Staff physicians also had a lower average number of incorrect billing codes per scenario (1.7 v. 2.0 codes, p = 0.36).
Fig. 1.
Comparison of resident physician and staff physician responses to a 10-question scenario-based billing assessment. Percentages were calculated on the basis of the number of responses (e.g., 5 correct codes out of 10 most-accurate responses = 50% correct).
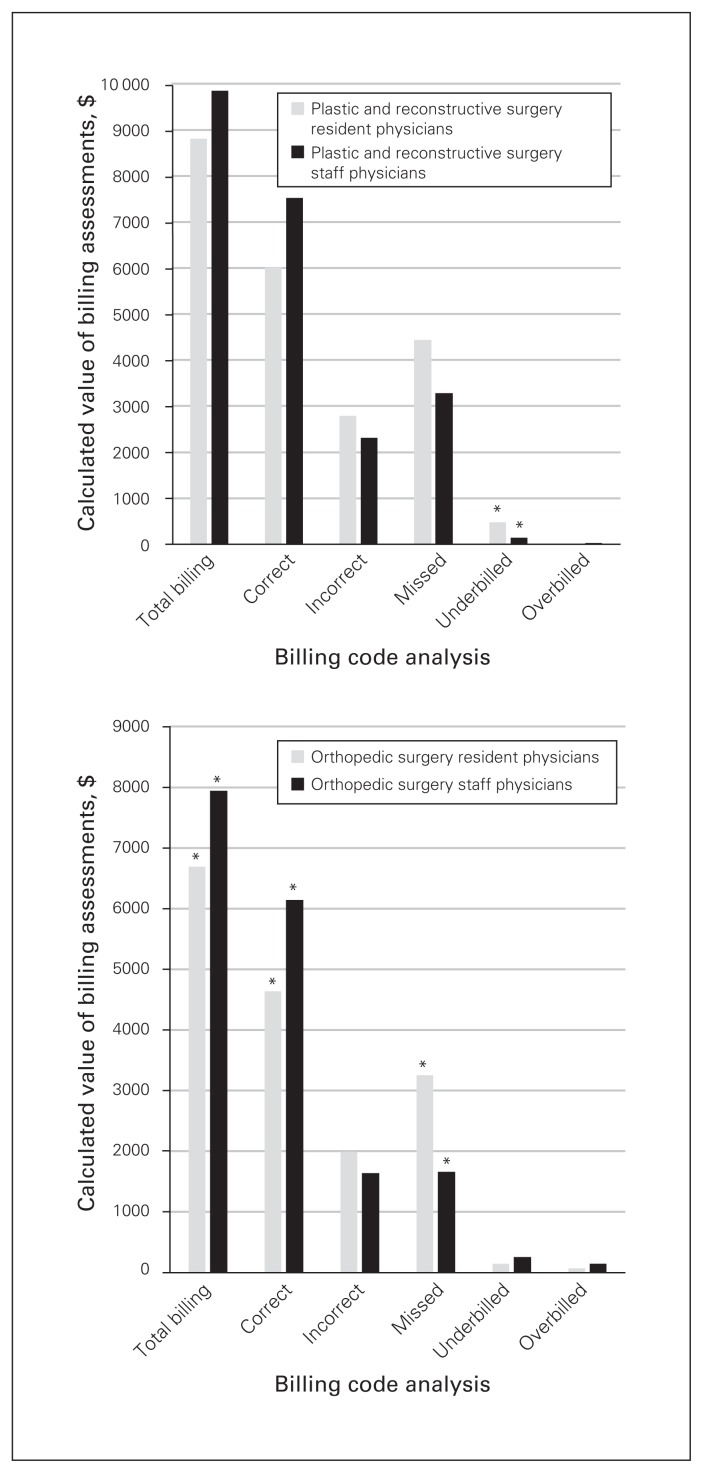
The calculated values of the billing assessments by specialty are depicted in Figure 2. When we calculated the dollar amount that would have been billed with all the codes chosen by the participants as a percentage of the dollar amount that would have been billed with the most appropriate codes, the percentage for staff physicians was higher than for resident physicians, on average (93.1% v. 82.3%, p = 0.09). The percentage of correct billings was significantly higher for staff physicians (71.5% v. 56.8%, p = 0.01), and the percentage of missed billings was significantly lower (26.7% v. 40.4%, p = 0.02). There was no statistically significant difference between staff physicians and resident physicians in regard to the percentage underbilled (1.9% v. 2.6%, p = 0.44), the total amount overbilled ($65.35 v. $45.68, p = 0.49) or the total amount of incorrect billings ($2073.24 v. $2240.08, p = 0.76).
Fig. 2.
Average amount billed for resident physician and staff physician billing assessments. On the basis of the most appropriate responses, total possible billings were $10 931.34 for the plastic and reconstructive surgery assessment and $8062.64 for the orthopedic surgery assessment. *Statistically significant differences (p < 0.05).
A subanalysis was performed for all missed codes from the billing assessments (Table 1). The most commonly missed billing codes for both resident and staff physicians were add-on premium codes (62.4% and 64.8% of all missed billing codes), while procedure codes were the least commonly missed (9.5% and 13.9%). Among the add-on premium codes, travel premium codes were the most commonly missed for both resident and staff physicians (41.8% and 38.9%).
Table 1.
Comparison of missed billing codes for resident and staff physicians on the 10-question billing assessment
| Missed billing assessment code | Percentage of all missed billing codes | |
|---|---|---|
| Resident physicians | Staff physicians | |
| Consult code* | 28.1% | 21.3% |
| Procedure code* | 9.5% | 13.9% |
| Premium code* | 62.4% | 64.8% |
| Admission† | 29.5% | 36.9% |
| After hours† | 14.5% | 11.1% |
| Procedure† | 12.9% | 11.4% |
| Travel† | 41.8% | 38.9% |
| Other† | 1.3% | 1.7% |
Values are calculated on the basis of the total number of missed billing codes for resident physicians (n = 609) and staff physicians (n = 460), respectively.
Values are calculated as the percentage of premium codes within the column.
A total of 15 resident physicians (11 OS, 4 PRS) and 19 staff physicians (6 OS, 13 PRS) completed the posttest survey. When asked about the amount of formal billing teaching they received during residency training, 86.9% of residents and 79.0% of staff physicians reported 0 hours of teaching, 13.1% and 15.8% reported 1–2 hours and 0.0% and 5.3% reported 3–5 hours of teaching. No residents or staff physicians reported more than 5 hours of formal billing teaching during residency training.
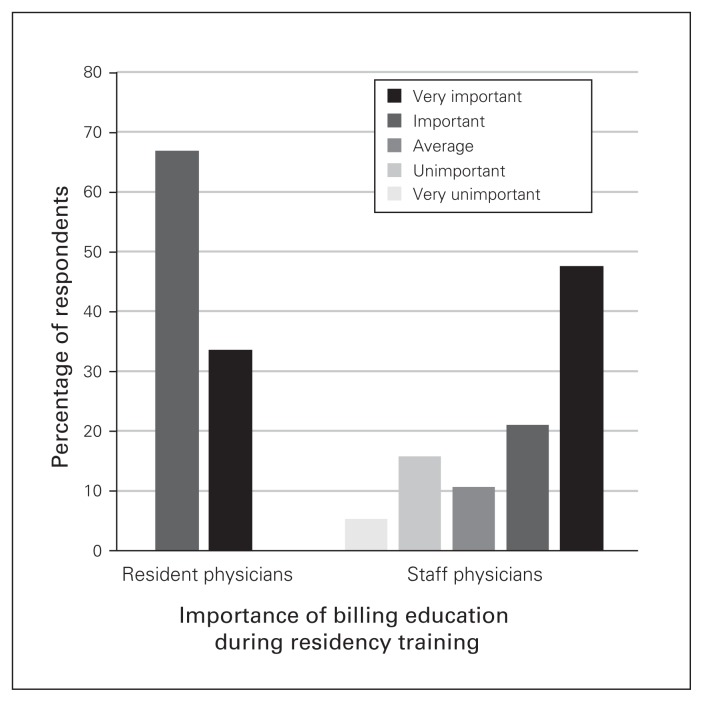
Respondents were asked about the importance of teaching billing during residency training (Fig. 3). All residents (100.0%) stated that they would like to have more formal billing education during residency training. In comparison, 79.0% of staff physicians stated that they would have liked more formal billing teaching during residency, 10.5% stated that they would not have liked more billing teaching and 10.5% were unsure.
Fig. 3.
Resident and staff physician opinions regarding the importance of incorporating billing education into residency training.
When asked to rate the formal billing teaching they received during residency training, 73.3% of residents rated the teaching as poor while the remaining 26.7% responded “not applicable/none.” In comparison, 63.1% of staff physicians rated their billing teaching as poor, 5.3% rated it as fair and 5.3% rated it as excellent, and 26.3% of them responded “not applicable/none.”
Respondents were asked to subjectively rate how knowledgeable they feel when it comes to billing. A total of 93.3% of residents rated themselves at the beginner level and 6.7% rated themselves at the advanced level. In comparison, no staff physicians rated themselves at the beginner level, 26.3% rated themselves at the novice level, 57.9% at the advanced level and 15.8% at the expert level.
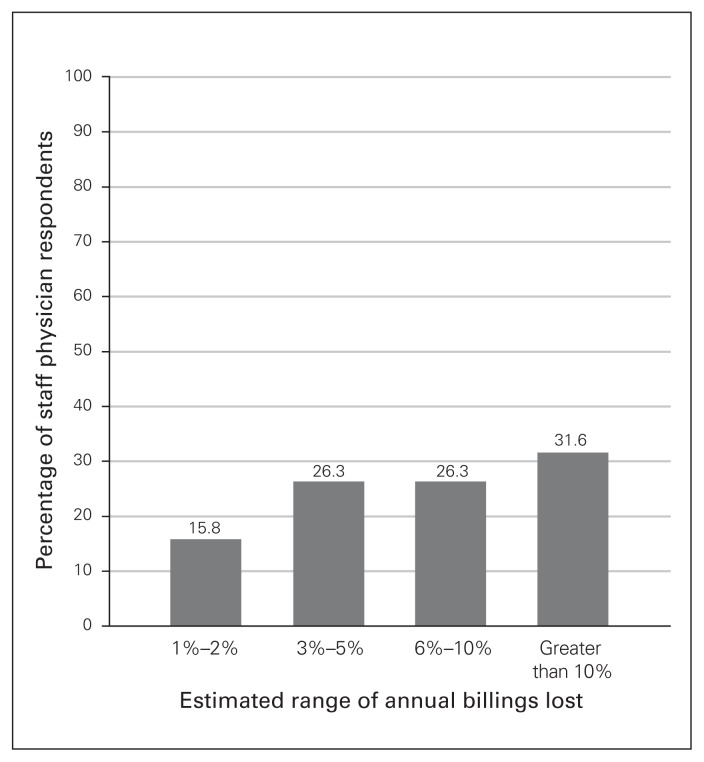
Staff physicians were asked to estimate the percentage of annual billings they missed because they had inadequate knowledge or made billing errors, demonstrating the perceived inadequacy of billing knowledge and the potential loss of revenue for physicians (Fig. 4).
Fig. 4.
Staff physician estimates of the percentage of annual billing revenue lost as a result of missed billing codes and billing error.
Discussion
Although the financial aspects of practice management remain largely undiscussed throughout medical education, the same cannot be said of the mainstream media. Physician remuneration has become a highly politicized topic. In Canada, where governments face constant pressure to lower taxes and reduce health care costs, physician compensation is commonly discussed as the primary target for clawbacks and cuts. Viewed through the lens of the health care industry as a whole, this argument has gained traction in the press. However, on an individual level physicians are not “big business”; they are small-business operators who depend solely on their billings to pay not only their own salary but also the salaries of their employees, and they must also pay for office space, office expenses, malpractice fees, licensing fees, continuing medical education, taxes and other expenses. In the face of this mounting pressure within a single-payer health care system, the burden falls upon individual physicians to optimize billings to ensure the long-term financial stability of their practice.
Unfortunately, the results of this study suggest that significant improvements are still required. Although staff physicians were more accurate than resident trainees in the billing scenarios, even experienced physicians missed on average 38.5% of billing codes and 28.5% of potential billings, a revenue loss that would be catastrophic for any small business. While this finding may be due in part to the nature of the scenario-based assessment, the survey results suggest that the assessment cannot be entirely to blame. Over half of the staff physician respondents in this study self-report believing that they lose over 5% of their annual revenue due to billing errors, with nearly one-third of all respondents believing that they lose over 10% of annual revenue (Fig. 4). Even if these more conservative self-reported estimates are to be believed, projected over the entire course of a physician’s career these billing errors could represent hundreds of thousands of dollars of lost revenue simply because of a lack of billing education. Had these staff physicians been better trained in billing and practice management in the first place, this glaring disparity may have been much less significant.
When it comes to billing education, the survey results demonstrate that both resident and staff physicians consider billing education an important topic that goes largely overlooked. As resident physicians typically do not bill in the Canadian health care system, they receive little to no on-the-job exposure to billing during training. Even though resident physicians desire more billing education and practising physicians believe that this education would be beneficial for transitioning to practice, this core-competency topic remains neglected.
One of the major barriers to implementation of a practice management curriculum is the fact that residency training is a busy and finite period of time during which educational efforts are primarily directed to clinical knowledge. Unfortunately, an equal barrier to practice management education is the taboo nature of the financial aspects of medicine. The only way to overcome this barrier and start the discussion about financial competency is to formally incorporate practice management education into residency training. Ideally, this nonclinical curriculum would be targeted to senior residents and fellows and would be delivered outside of clinical teaching hours. A transition-to-practice evening seminar series for senior residents and fellows, led by senior staff mentors and outside consultants, would target these educational resources to the appropriate audience without diluting clinical education. Furthermore, a seminar series may also be of interest to junior faculty or physicians who are new to the area, potentially serving as a source of revenue generation for residency programs.
We are not suggesting that a practice management curriculum be implemented at the cost of clinical experience; instead, we believe that financial training must become valued and taught such that we may provide the next generation of Canadian physicians with the financial competency required to run a successful medical practice. Until this essential element of professional development becomes a formalized part of residency education, we will not be able to break this cycle of financial incompetence.
Limitations
We acknowledge that there were several limitations inherent in this study. First, the billing assessment comprised hypothetical scenarios presented in a paragraph format, which is not the way that billing occurs in day-to-day practice. It is possible that some respondents missed some of the nuances of the scenarios (e.g., holiday billing) because these were hypothetical scenarios. However, this format allowed for the scenarios to be worded such that there was clearly a most appropriate response based on the wording of the MOHLTC SOB. Overall response rates were low for both residents and staff physicians, resulting in a low overall sample size that may have affected the study findings and generalizability. This low response rate was probably due to the significant time commitment required to complete the billing assessment and survey (> 60 min). Although a shorter billing assessment may have increased the response rate, we felt that the 10-question assessment provided a more accurate depiction of billing knowledge. The responses to the billing assessments were evaluated by a single person to provided consistency for interpretation of the assessments, although this may represent a potential source for bias. In regard to the posttest survey, it is possible that recall bias may have affected participant responses to questions about billing education during training. Nevertheless, the purpose of the posttest survey was to assess participants’ experience with billing education rather than to calculate their true exposure, and we feel this is accurately reflected in the survey results. Finally, when it came to assessment of respondent billing codes, in some situations, judgment was required to distinguish an incorrect code from an acceptable alternative. In these situations, if a specific concept was being tested the criteria were more stringent than in situations of procedural coding. The criteria used to determine correct versus incorrect codes do not necessarily reflect the criteria that the MOHLTC would use to accept or reject billing codes; however, they do accurately reflect the wording contained within the MOHLTC SOB.
Conclusion
To our knowledge, this is the first study that has used a billing assessment to compare the accuracy of billing between resident physicians and staff physicians. The results of the study clearly demonstrate that while staff physicians are more accurate at billing than resident physicians, a knowledge gap exists even among practising physicians. No matter the stage of one’s career, whether one is starting a practice or planning for retirement, financial competence is an integral component of being a complete physician. By formally incorporating practice management education into residency training, we can equip the next generation of medical trainees with the knowledge they require to succeed as small-business owners.
Acknowledgements
The authors thank Dr. Brandon Girardi (Division of Orthopaedic Surgery, University of Toronto) and Ms. Farah Rizvi (Accu-Med Billing Solutions) for assisting in the creation of the billing assessments.
Footnotes
Competing interests: None declared.
Contributors: Both authors designed the study. R. Austin acquired the data, which both authors analyzed. R. Austin wrote the article, which both authors reviewed and approved for publication. Both authors agreed to be accountable for all aspects of the work.
References
- 1.Frank JR. The CanMEDS physician competency framework. Better standards. Better physicians. Better care. Ottawa (ON): Royal College of Physicians and Surgeons of Canada; 2005. [Google Scholar]
- 2.Swing SR. The ACGME outcome project: retrospective and prospective. Med Teach. 2007;29:648–54. doi: 10.1080/01421590701392903. [DOI] [PubMed] [Google Scholar]
- 3.Simpson JG, Furnace J, Crosby J, et al. The Scottish doctor — learning outcomes for the medical undergraduate in Scotland: a foundation for competent and reflective practitioners. Med Teach. 2002;24:136–43. doi: 10.1080/01421590220120713. [DOI] [PubMed] [Google Scholar]
- 4.Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 physician competency framework. Ottawa (ON): Royal College of Physicians and Surgeons of Canada; 2015. [accessed 2018 Jan 27]. Available: www.royalcollege.ca/rcsite/canmeds/canmeds-framework-e. [Google Scholar]
- 5.Dawson B, Carter K, Brewer K, et al. Chart smart: a need for documentation and billing education among emergency medicine residents? West J Emerg Med. 2010;11:116–9. [PMC free article] [PubMed] [Google Scholar]
- 6.Howell J, Chisholm C, Clark A, et al. Emergency medicine resident documentation: results of the 1999 American Board of Emergency Medicine in-training examination survey. Acad Emerg Med. 2000;7:1135–8. doi: 10.1111/j.1553-2712.2000.tb01263.x. [DOI] [PubMed] [Google Scholar]
- 7.Andreae MC, Dunham K, Freed GL. Inadequate training in billing and coding as perceived by recent pediatric graduates. Clin Pediatr (Phila) 2009;48:939–44. doi: 10.1177/0009922809337622. [DOI] [PubMed] [Google Scholar]
- 8.Patel AT, Bohmer RM, Barbour JR, et al. National assessment of business-of-medicine training and its implications for the development of a business-of-medicine curriculum. Laryngoscope. 2005;115:51–5. doi: 10.1097/01.mlg.0000150677.75978.75. [DOI] [PubMed] [Google Scholar]
- 9.Adiga K, Buss M, Beasley BW. Perceived, actual, and desired knowledge regarding Medicare billing and reimbursement. A national needs assessment survey of internal medicine residents. J Gen Intern Med. 2006;21:466–70. doi: 10.1111/j.1525-1497.2006.00428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDonnell PJ, Kirwan TJ, Brinton GS, et al. Perceptions of recent ophthalmology residency graduates regarding preparation for practice. Ophthalmology. 2007;114:387–91. doi: 10.1016/j.ophtha.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 11.Fakhry SM, Robinson L, Hendershot K, et al. Surgical residents’ knowledge of documentation and coding for professional services: an opportunity for a focused educational offering. Am J Surg. 2007;194:263–7. doi: 10.1016/j.amjsurg.2006.11.031. [DOI] [PubMed] [Google Scholar]
- 12.Watanabe Y, Madani A, Bilgic E, et al. Don’t fix it if it isn’t broken: a survey of preparedness for practice among graduates of fellowship council-accredited fellowships. Surg Endosc. 2017;31:2287–98. doi: 10.1007/s00464-016-5231-0. [DOI] [PubMed] [Google Scholar]
- 13.Lusco VC, Martinez SA, Polk HC. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg. 2005;189:11–3. doi: 10.1016/j.amjsurg.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Sprtel SJ, Zlabek JA. Does the use of standardized history and physical forms improve billable income and resident physician awareness of billing codes? South Med J. 2005;98:524–7. doi: 10.1097/01.SMJ.0000149388.95575.72. [DOI] [PubMed] [Google Scholar]
- 15.Lister JR, Friedman WA, Murad GJ, et al. Evaluation of a transition to practice program for neurosurgery residents: creating a safe transition from resident to independent practitioner. J Grad Med Educ. 2010;2:366–72. doi: 10.4300/JGME-D-10-00078.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holak EJ, Kaslow O, Pagel PS. Facilitating the transition to practice: a weekend retreat curriculum for business-of-medicine education of United States anesthesiology residents. J Anesth. 2010;24:807–10. doi: 10.1007/s00540-010-0973-7. [DOI] [PubMed] [Google Scholar]
- 17.Jones K, Lebron RA, Mangram A, et al. Practice management education during surgical residency. Am J Surg. 2008;196:878–81. doi: 10.1016/j.amjsurg.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Levesque AY, Tauber DM, Lee JC, et al. The impact of a standardized consultation form for facial trauma on billing and evaluation and management levels. Ann Plast Surg. 2014;72:196–9. doi: 10.1097/SAP.0b013e31825c0871. [DOI] [PubMed] [Google Scholar]
- 19.Ng M, Lawless ST. What if pediatric residents could bill for their outpatient services? Pediatrics. 2001;108:827–34. doi: 10.1542/peds.108.4.827. [DOI] [PubMed] [Google Scholar]
- 20.Gala RB, Chiang S. The impact of a documentation and coding curriculum in an obstetrics and gynecology continuity clinic. Ochsner J. 2012;12:354–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Ghaderi KF, Schmidt ST, Drolet BC. Coding and billing in surgical education: a systems-based practice education program. J Surg Educ. 2017;74:199–202. doi: 10.1016/j.jsurg.2016.08.011. [DOI] [PubMed] [Google Scholar]