Abstract
Background
Appropriate, timely trauma team activation (TTA) can directly affect outcomes for patients with trauma. A review of quality-performance indicators at our Canadian level 1 trauma centre showed a high level of undertriage, with TTA compliance rates less than 60% for major trauma. A quality-improvement project was undertaken, targeting a sustained goal of at least 90% TTA compliance based on Accreditation Canada guidelines.
Methods
Quality-improvement action followed a well-defined process. Baseline data collection was performed, and, in keeping with the Donabedian approach, we brought together stakeholders to collectively review and understand the reasons behind poor TTA compliance; and root-cause analysis. This was followed by rapid change cycles that focused on structure and processes with ongoing audits to support and sustain change.
Results
Trauma team activation compliance improved from 58.8% to more than 90% over 2 years. Quality indicators showed a statistically significant reduction in the time to computed tomography scanner, time in the acute care region of the emergency department and total time in the emergency department, with improved TTA compliance.
Conclusion
Compliance with TTA protocols improved to more than 90% over a 2-year period, which shows the benefit of having a clearly outlined quality-improvement process. This well-defined quality-improvement method provides a framework for use by other institutions that seek to improve their processes of trauma care, including activation rates.
Abstract
Contexte
Le déploiement rapide et approprié de l’équipe de traumatologie (DÉT) peut avoir une influence directe sur les résultats chez les polytraumatisés. Une revue des indicateurs de qualité/performance dans notre centre de traumatologie canadien de niveau 1 a révélé une lacune importante au plan du triage, et des taux de conformité aux protocoles de DÉT atteignant moins de 60 % pour les traumatismes majeurs. Un projet d’amélioration de la qualité a donc été entrepris avec pour objectif une conformité soutenue d’au moins 90 % aux protocoles de DÉT selon les lignes directrices d’Agrément Canada.
Méthodes
Les mesures d’amélioration de la qualité ont suivi un processus bien défini. Une collecte des données de référence a été effectuée, et conformément au modèle de Donabedian, nous avons réuni les différentes parties intéressées pour revoir et comprendre ensemble les raisons de la piètre conformité aux protocoles de DÉT et procéder à leur analyse en profondeur. On a ensuite appliqué des cycles de changements rapides axés sur la structure et les procédés, accompagnés de vérifications en continu pour les appuyer et les maintenir.
Résultats
La conformité aux protocoles de déploiement de l’équipe de traumatologie s’est améliorée, passant de 58,8 % à plus de 90 % en l’espace de 2 ans. Les indicateurs de qualité ont montré des réductions statistiquement significatives du délai prétomographie, du temps passé dans la section de soins aigus du service des urgences et du temps total passé aux urgences, de même qu’une meilleure conformité aux protocoles de DÉT.
Conclusion
La conformité aux protocoles de DÉT s’est améliorée pour dépasser les 90 % en l’espace de 2 ans, ce qui montre l’efficacité d’un processus d’amélioration de la qualité clairement défini. Cette méthode d’amélioration de la qualité bien définie fournit un cadre que d’autres établissements peuvent appliquer s’ils cherchent à améliorer leurs protocoles de traumatologie, y compris la vitesse de leur déploiement.
Appropriate and timely trauma team activation (TTA) can directly affect outcomes for critically injured patients. The presence of a trauma team led by an experienced trauma physician facilitates resuscitation, diagnosis and definitive treatment of patients with polytrauma.1–4 The presence of a trauma team leader (TTL) also increases adherence to advanced trauma life support protocols.5 Consistent and appropriate TTA has been shown to improve outcomes, reduce length of stay and reduce mortality.2,3,6–9 Decreased time in the emergency department, decreased time to obtain imaging, decreased time to the operating room and fewer missed injuries can also be achieved with appropriate TTA.4,10–12
Trauma team activations should occur according to predetermined, institution-specific criteria. These criteria may reflect the mechanism of injury, physiologic status of the patient, treatment that is required or a combination thereof. Compliance with TTA is a process indicator that reflects the quality of trauma care provided. Accreditation Canada has determined that, in cases in which TTA criteria are met, a TTA should occur at least 90% of the time.13 The American College of Surgeons Committee on Trauma similarly recommends TTA compliance rates of at least 80% for severely injured patients.14 The committee defines over- and undertriage using a simple goal to treat the “right patient, right place, and right time.”14 Undertriage therefore includes events when severely injured patients are inappropriately transported to lower-level trauma centres or do not trigger appropriate level of TTA at that acute care centre. Appropriate triage criteria outlined by the American College of Surgeons Committee on Trauma, based on physiologic parameters such as heart rate and blood pressure, experienced triage personnel and physician triage, have shown low undertriage rates without excessive overtriage.14–16
A review of quality-performance indicators at our centre showed a high level of undertriage, with TTA compliance rates less than 60% for patients with major trauma. Consequently, a quality-improvement project was undertaken, targeting a sustained goal of at least 90% TTA compliance. In the current paper we outline our approach, focused on stakeholder engagement, followed by “Plan–Do–Study–Act” (PDSA) rapid change cycles. The PDSA rapid change cycles were directed toward the cause of TTA noncompliance and were defined within the 3 pillars of Donabedian thinking: structure, process and outcomes. 17–22 This approach provides a framework for use by other institutions that seek to improve their processes of trauma care.
Methods
Quality-improvement action followed a well-defined PDSA process. Baseline data collection and stakeholder analysis were performed from April to August 2015. Multidisciplinary stakeholder engagement (supported by active trauma medical and operational leadership) and root-cause analysis were subsequently completed to define the TTA process, barriers to its success and problem-specific solutions. Plan–Do–Study–Act rapid change cycles were then implemented from August 2015 to September 2016, focusing on structure, process and outcomes, to elicit TTA compliance. Continued auditing and measurement of trauma quality indicators until February 2017 allowed measurement of success and feedback acquisition, and ensured improvement sustainability.
Data collection
Baseline data collection was performed to determine baseline TTA compliance and identify areas for improvement. These audits continued throughout the study period to monitor any improvement. All patients were treated at a Canadian level 1 trauma centre that treats more than 800 major adult traumas (Injury Severity Score [ISS] ≥ 12) per year. The hospital trauma coordinator identified all patients with trauma at our centre and enrolled them using the Alberta Trauma Registry (a prospective database that records data regarding patients with trauma). The patients’ charts were audited, and data were collected on the total number of TTAs, the number of patients who met TTA criteria, the specific criteria that triggered the TTA and missed TTAs. Missed TTAs were identified when patients met TTA criteria but there was no evidence of trauma team care, including but not limited to within physician notes, consultation notes and nursing notes (including specific TTA recording notes).
Additional data were collected from October 2016 to February 2017, following the implementation of change cycles, to assess quality indicators that are directly linked to patient outcomes. Operational process quality indicators collected included the time from patient presentation in the emergency department to computed tomography (CT) scan, time from emergency department presentation to admission and time spent in the acute care area of the emergency department. These quality indicators were collected for all patients with major trauma. We compared results between patients who received TTA care and those who did not using a 1-tailed Welch t test assuming unequal variance.
Stakeholder engagement and root-cause analysis
A formal stakeholder analysis was conducted to identify key groups involved with the TTA process. Root-cause analysis was then performed, with both a survey and a multidisciplinary working group used to assess attitudes toward, knowledge of and barriers to compliance with TTA. The survey was distributed to TTLs, emergency department physicians, surgeons, emergency department clinical managers, emergency department nurse educators, nurses, respiratory therapists and radiography technicians. The TTA working group engaged members from these same disciplines but also included prehospital staff. A process map was subsequently formulated, and a root-cause analysis was conducted with the aid of a fishbone diagram to outline the TTA pathway and identify areas that required improvement.
Rapid change cycles
Root-cause analysis identified structure and process barriers that prevented appropriate TTA. Potential solutions to these issues were implemented via PDSA rapid change cycles (Table 1).
Table 1.
“Plan–Do–Study–Act” rapid change cycles, the months that they were completed and the letter that corresponds to their timing on the run chart
| Rapid change cycle action | Change date | Letter on run chart |
|---|---|---|
| Structure changes | ||
| Mandatory agenda item for discussion at monthly trauma committee meetings | April 2015 | A |
| Process map of the areas in which gaps were identified with the multidisciplinary stakeholders | July 2015 | B |
| Addition of the ability to “stand down” TTA if the patient did not meet criteria | August 2015 | C |
| Change in TTA criteria to be more anatomic and physiologic and therefore have more clarity; objective rather than subjective standards (e.g., mechanism) | August 2015 | D |
| Change in TTA members (more senior residents and staff surgeon involvement) | August 2015 | E |
| Clarification of roles and responsibilities | August 2015 | F |
| Process changes | ||
| Displaying of ongoing audit results via posters in readily visible areas for all stakeholders | August 2015 | G |
| Criteria for TTA outlined on quick-reference cards given to all trauma team members | September 2015 | H |
| Monthly simulations | September 2015 | I |
| Ongoing education on importance and purpose of TTA | September 2015 | J |
| Results presented and discussed at 2 emergency department leadership meetings | October 2015 | K |
| Additional system improvements | ||
| Improved remuneration and TTL engagement | January 2016 | L |
| TTA alphanumeric pagers | September 2016 | M |
PDSA = Plan–Do–Study–Act; TTA = trauma team activation; TTL = trauma team leader.
Structure barriers
Plan–Do–Study–Act cycles that focused on structure barriers included the following:
Altering TTA criteria to focus on anatomic and physiologic variables: with feedback from local clinical emergency department physicians and trauma surgeons as well as national experts at other level 1 Canadian trauma centres, we developed TTA criteria that were objective and based on anatomic and physiologic criteria. The updated criteria were as follows: systolic blood pressure less than 90 mm Hg or heart rate greater than 130 beats/min in the last hour before arrival, respiratory or airway compromise requiring emergent intervention in the emergency department, blood transfusion en route, penetrating trauma to the head, neck, chest or abdomen, or at the discretion of the emergency department doctor or charge nurse.
Changing the composition of the trauma team: trauma team reconfiguration involved adding more senior clinicians and ensuring clarity regarding roles and responsibilities for all trauma team members. The trauma team initially included the TTL or emergency department physician, junior and senior residents in general surgery, an orthopedic surgery resident, a neurosurgery resident and an anesthesiologist. The general surgery staff physician and general surgery chief were added to facilitate trauma resuscitation processes, trauma management and treatment decisions.
Clarifying roles for each member of the trauma team: senior leadership within the trauma team facilitated clarification of roles and responsibilities, and efficiently directed actions of the trauma team.
Standardization of TTA criteria throughout the city and improved TTA notification: the city’s trauma program developed trauma advisory committees involving multiple previously identified stakeholders. Collaboration with the other major trauma centre in the city allowed TTA criteria to be consistent. Trauma team activation was also added as a mandatory agenda item for discussion at monthly trauma committee meetings. A major barrier to TTA was lack of dedicated TTLs, and therefore appropriate funding, recruitment and engagement of TTLs was reexamined. This funding also facilitated access to alphanumeric pagers to improve TTA notification.
Involving prehospital providers with TTA: The Shock Trauma Air Rescue Service and emergency medical services were notified and educated regarding the new TTA criteria. Collaborative leadership support with the Shock Trauma Air Rescue Service allowed early TTA by their prehospital personnel. Shock Trauma Air Rescue Service prehospital providers are aware of the objective physiologic TTA criteria and inform receiving facilities to trigger a TTA. Providers also supply the receiving facility with key clinical information that can be included with TTA using the alphanumeric paging system. It should be noted that a prehospital triage tool existed before project implementation that successfully diverted all patients with major trauma to 1 of 2 major trauma centres within our region.
Ability to “stand down” the trauma team: a quality-assurance form was also implemented that would be filled out by members of the multidisciplinary trauma team if TTA criteria were met but the patient’s illness or injuries did not require management by the full trauma team (i.e., a superficial penetrating injury that did not penetrate the dermis). The form required explanation of the clinical scenario and would allow our hospital to record instances in which the trauma team is activated unnecessarily.
Process barriers
Subsequent PDSA cycles clarified and improved TTA processes. This was facilitated by clear leadership support and sponsorship from the health care organization (Alberta Health Services) and leadership within Alberta Health Services Trauma Services and prehospital care teams. Process improvement involved the following actions:
Communication and dissemination of the updated TTA protocols and team roles: a list of responsibilities for each trauma team member was disseminated and posted in the emergency department as a visual reminder. Discussions with each group further clarified any uncertainty regarding roles within the trauma team. We also performed monthly TTA simulations where the focus was on trauma team dynamics (communication, delegation of tasks, leveling of hierarchy, and education around leadership and crisis resource management principles) and further strengthening roles and responsibilities.
Formal educational sessions about TTA importance for patient outcomes: members of Trauma Services, including the trauma coordinator and medical director, outlined the changes and their rationale at emergency department morning “huddles,” resident physician education half-days, each month at the adult TTL meetings, and during face-to-face discussions with emergency department nursing and medical staff.
Ongoing education regarding new TTA criteria: to ensure uptake of the new TTA criteria, additional educational sessions were held with medical staff, residents and frontline emergency department staff. Criteria for TTA were also outlined on laminated quick-reference cards on lanyards given to all trauma team members (medical and nonmedical).
Ongoing audits of TTA compliance: data were collected and charted on posters that were displayed in a visible, transparent manner for all stakeholders.
Results
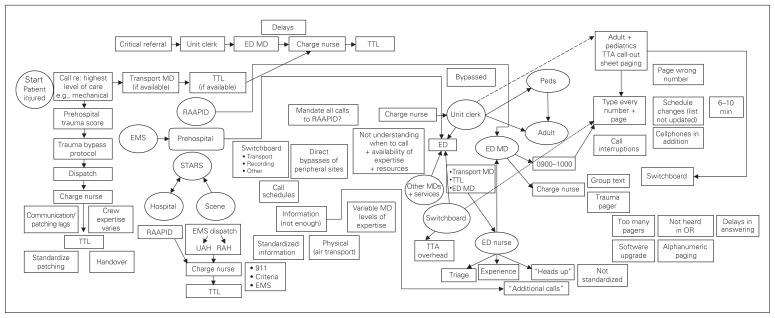
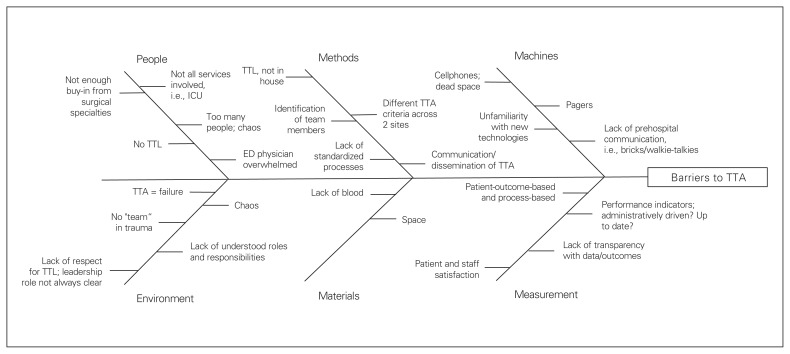
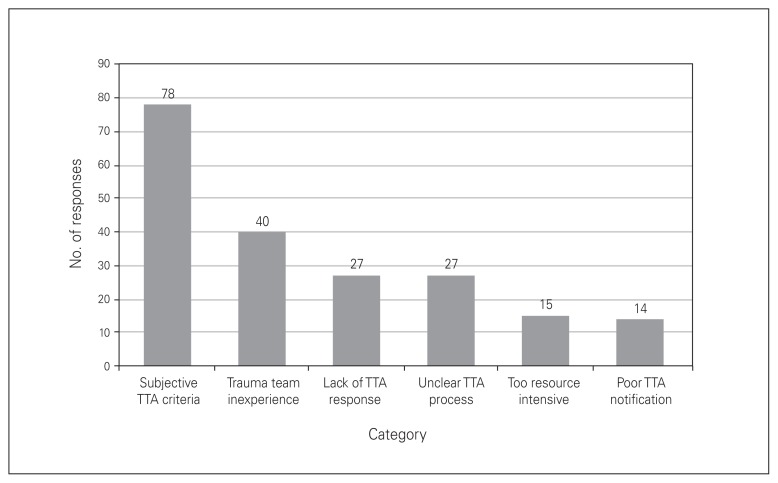
Formal root-cause analysis identified key stakeholders, and, with their engagement, a process map was created that identified major barriers to achieving high rates of TTA compliance (Fig. 1). The fishbone and Pareto diagrams in Fig. 2 and Fig. 3, respectively, helped further clarify the barriers. Poor buy-in from surgical subspecialties, lack of staff surgeon involvement, inconsistent TTL coverage and miscommunication with prehospital providers were outlined as key problems. Other major barriers identified included subjective TTA criteria, uncertain TTA process, lack of clarity regarding the role of the trauma team, inconsistent notification process for the trauma team and reluctance to activate the trauma team owing to its junior composition.
Fig. 1.
Trauma team activation process map used to identify areas of improvement. ED = emergency department; EMS = emergency medical services; MD = medical doctor; OR = operating room; RAAPID = Referral, Access, Advice, Placement, Information & Destination; RAH = Royal Alexandra Hospital; STARS = Shock Trauma Air Rescue Service; TTA = trauma team activation; TTL = trauma team leader; UAH = University of Alberta Hospital.
Fig. 2.
Fishbone diagram showing barriers to successful trauma team activation (TTA). ED = emergency department; ICU = intensive care unit; TTL = trauma team leader.
Fig. 3.
Reasons cited as barriers to compliance with trauma team activation (TTA) protocols identified on root-cause analysis.
Baseline data were collected for 114 patients from April to August 2015. During this period, a TTA occurred for 61 (66%) of the 93 patients who met the current criteria for TTA. Of the 21 missed TTAs, 5 (24%) were due to penetrating trauma, 3 (14%) were due to airway issues and 2 (10%) were due to hemodynamic instability. There were also 11 process issues (52%) that led to a missed TTA, where 1 of the following errors occurred: overhead trauma team call but no paging, not all members of the trauma team were paged, trauma team was paged but no overhead call, and TTA documented but no evidence to support the presence of a trauma team.
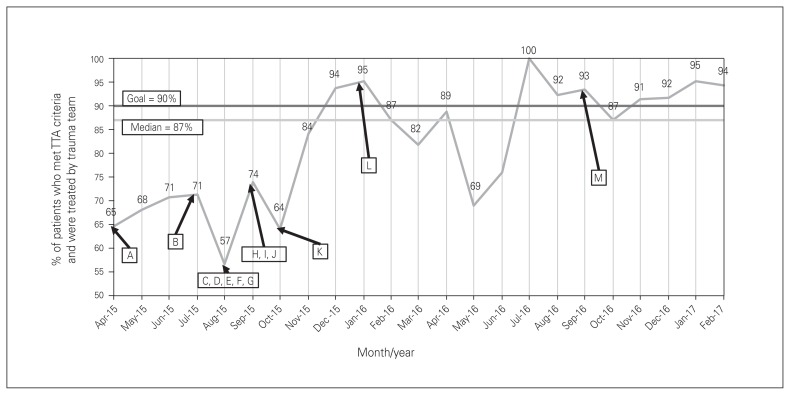
Change cycle implementation in August 2015 was associated with an increase in TTA compliance to 71.4% in the subsequent month (Fig. 4). Compliance averaged 81.2% from September 2015 to June 2016 but was not consistently reaching the 90% goal. During this time, the rate of TTA for penetrating trauma increased. Also, the number of missed TTAs due to process errors decreased, from 2.2 per month between April and August 2015 to 1.9 per month for the subsequent 10 months.
Fig. 4.
Run chart displaying compliance with trauma team activation (TTA) based on the current criteria throughout project, April 2015–February 2017. Letters correspond to steps in Table 1.
In July 2016, the goal of at least 90% compliance with TTA protocols was met and was sustained for the subsequent 7 months. During this period, penetrating trauma was again the most commonly missed TTA criterion (56%). However, the number of missed TTAs due to process errors decreased to 0.125 per month during this time.
Measurement of quality indicators following achievement of at least 90% TTA compliance showed that, for patients treated by the trauma team, the mean time from emergency department presentation to CT scan (assumed to be representative of resuscitation time as patients are taken to the CT scanner only when their condition has been stabilized appropriately) was 78 minutes (Table 2). The mean time that patients spent in the acute care area of the emergency department was 3 hours and 54 minutes, and their total time in the emergency department was 4 hours and 14 minutes. Over this same period, on average, patients who were not treated by the trauma team took 2 hours and 10 minutes to reach the CT scanner, were in the acute care area of the emergency department for 6 hours and 1 minute, and remained in the emergency department for 7 hours and 36 minutes, all statistically significantly longer than for patients who were treated by the trauma team (p < 0.01). Time from emergency department presentation to arrival of the trauma team averaged 6 minutes (n = 51), with prehospital TTA occurring in 32 cases (63%).
Table 2.
Trauma quality indicators measured following the implementation of rapid change cycles, October 2016 to February 2017
| Quality indicator | Mean time, h:min:sec | Difference between TTA v._no TTA, h:min:sec | p value |
|---|---|---|---|
| Time from emergency department presentation to CT scanner | |||
| Received TTA | 1:17:43 (n = 42) | 0:52:32 | < 0.01 |
| No TTA | 2:10:15 (n = 99) | — | |
| Time spent in emergency department acute care area | |||
| Received TTA | 3:53:47 (n = 51) | 2:06:48 | < 0.01 |
| No TTA | 6:00:35 (n = 112) | — | |
| Total time spent in emergency department | |||
| Received TTA | 4:13:34 (n = 51) | 3:22:09 | < 0.01 |
| No TTA | 7:35:43 (n = 127) | — |
CT = computed tomography; TTA = trauma team activation.
Discussion
The success of process-specific PDSA cycles hinges on previous background review of practice standards that are evidence based, stakeholder analysis, staff engagement and structure solutions, which should be the primary actions of a change project. Review of our hospital’s compliance with TTA showed gaps in trauma care, and quality-improvement action was initiated in April 2015 with the goal of activating the trauma team in at least 90% of major traumas within a 6-month time frame. This goal was met by July 2016 and was sustained for the following 7 months.
Trauma undertriage is common, occurring in up to 34% of patients in the United States.23 Our baseline data collection showed that 34.2% of severely injured patients at our hospital were not effectively triaged to TTA. Undertriage occurs because of inadequate triage scoring systems (despite good interrater reliability),24,25 undertriage of older patients,16,23,26 different triage rates based on experience and profession,15,16 neurosurgical injuries27,28 and poor compliance with TTA protocols, as we showed in our hospital.9,28–30 Poor compliance with penetrating trauma criteria throughout our study shows that this injury may also be commonly undertriaged. Penetrating trauma is diverse, and low rates of TTA for penetrating trauma are likely because emergency physicians feel comfortable treating patients with distal extremity or superficial penetrating trauma without the support of a large trauma team if they are in stable condition. Overtriage is similarly detrimental, yet some degree of overtriage may be necessary to capture all the patients requiring trauma team treatment. The American College of Surgeons Committee on Trauma accepts 25%–30% overtriage to achieve the goal of less than 5% undertriage.14
In keeping with the Donabedian approach, we brought together stakeholders to more fully understand the reasons behind poor TTA compliance.21,22,31 The importance of understanding a problem before attempting improvement is crucial when implementing change in a complex, multidisciplinary field such as health care.31–33 Prior studies have shown the importance of understanding an issue before change management, for example, when improving compliance with medication reconciliation34,35 and infection control measures.20 Thorough understanding of the problem should be the basis of quality improvement.18,21,22,36 Creating a collaborative and broad understanding of a problem helps to limit resistance and allows successful change to occur.22,31,32,34,35
Multidisciplinary working groups helped engage staff with participative techniques during the initial stages of the project. Compliance with TTA protocols increased slightly, but not to 90% or more, following these discussions. This was likely in part due to engagement but may have also been due to a Hawthorne effect, as there were fluctuations almost back to baseline over time. Lack of substantial results with initial efforts is likely why these crucial steps may often seem unimportant and may be overlooked. The success of subsequent PDSA cycles and change management efforts is largely attributable to the nonidentifiable understanding, awareness and engagement that occurred as a result of the work done before roll-out; i.e., stakeholder engagement and leadership support.21,22,31 Such engagement and recruiting “champions” are often cited as central to successful implementation of change.17,31,34,37 The initial stages of this project created an environment for staff support, awareness and investment into the future change cycles we introduced.
The project’s change cycles also followed Donabedian principles, with an initial focus on clarifying protocols and creating an effective structure, before process change was introduced and outcomes were reviewed.21,22 This “system first, process second” approach has improved TTA compliance at other centres11,38,39 and has been shown to improve trauma outcome measures.36,39,40 Therefore, initial PDSA cycles targeted structure changes, whereas later cycles involved change management processes through education, awareness and bedside actions, led by project champions. Examples of process-focused changes include steps G–K in Table 1.
Structure-focused solutions generated trust and increased compliance by the providers who were involved with the working groups, as their responses resulted in obvious changes. The rate of compliance with TTA protocols increased from 66.4% at baseline to 82.2% in the subsequent 5 months. The immediate response to structure changes and provider-generated change was largely attributable to the relationships that were formed through working groups. As an example, the working group identified lack of role clarification and trauma team composition as issues that reduced TTA compliance. In the past, one reason cited for not activating the trauma team was to “avoid chaos in the trauma bay.” Similarly, root-cause analysis identified barriers such as a lack of clarity regarding roles and responsibilities, incorrect services involved, poor identification of team members, not enough buy-in from surgical specialties and a lack of TTA leadership. The introduction of senior trauma team members (general surgery chiefs and senior surgeon) during the TTA, role clarification and consistent TTL scheduling (steps C–E in Table 1) directly responded to these barriers and increased TTA compliance by enhancing the trauma team dynamics. Role clarification, team dynamics and trauma leadership are all critical aspects of a successful trauma team.3,5,11,41
Root-cause analysis also identified that different TTA criteria across hospitals, emergency department physicians’ being overwhelmed, lack of prehospital communication, concern about up-to-date performance indicators and a lack of transparency with TTA data were barriers to achieving the target compliance rate. Rapid change cycles including implementation of standardized and objective TTA criteria clarified uncertainty as to when to activate the trauma team and helped facilitate TTA decision-making. Empowerment of prehospital personnel allowed them to preactivate the trauma team before arrival to improve trauma team notification, preparedness of trauma team members and compliance with TTA. The TTA review form helped support root-cause analysis by facilitating feedback regarding TTA criteria and implementation issues. Participative techniques, reflective processes and feedback, as applied through this form, reduce resistance to change and aid sustainability.37,42
Structure changes were supported with ongoing staff engagement and additional process solutions during August 2015–February 2016. These included PDSA cycles regarding education, transparency of audit results and feedback on recent change cycles (steps G–K in Table 1). These actions targeted other barriers by developing a team mentality for trauma, improving communication, providing data feedback, and further clarifying roles and responsibilities. In addition, efforts to activate the trauma team were positively reinforced with more consistent TTA, since fewer process errors were occurring, and helped sustain compliance at our goal of at least 90% after July 2016.
Alongside increased TTA compliance, our review of quality indicators showed that, with improved TTA compliance, quality indicators were similar to results published by other hospitals. For patients treated with TTA care, our time to the CT scanner was 78 minutes, compared to 41–195 minutes for others who have assessed their trauma team indicators.43–45 Our time in the emergency department with TTA was 2 hours 29 minutes, compared to 1.95 hours and 2 hours and 55 minutes from other studies.4,46 In addition, when we compared patients who were treated by the trauma team to those who were not after our intervention, the former had much shorter time to the CT scanner, shorter treatment duration in acute care region of the emergency department and shorter overall time in the emergency department. Trauma team activation also resulted in timely treatment of severely injured patients, with a substantial proportion of TTAs occurring via prehospital activation, which allowed the trauma team to be on hand immediately at presentation.
Future projects are suggested to assess the ISS before and after TTA interventions to better outline any unwanted overtriage that may result from changes as well as to assess the timeliness of treatment by the trauma team following patient arrival in the emergency department. Although our study did show good quality-indicator performance (time to CT scan, time in the acute care region of the emergency department and overall time in the emergency department) and timely patient treatment following achievement of our goal of at least 90% compliance, future studies could benefit from including these measures in their baseline data collection to better define the change associated with quality-improvement cycles. We also suggest assessing 30-day mortality and hospital length of stay to better assess clinical outcomes of patients managed by TTA for others who are planning to apply this quality-improvement process. However, it should be recognized that an assumption of this project was that improved TTA compliance also improves care and quality indicators for trauma and decreases mortality rates and length of stay, as shown by other investigators.2,3,6–9 Assessing the ISS of patients who are treated by the trauma team versus other care groups would ensure that the rapid care they receive is not hinged on their acuity. In addition, researchers wishing to replicate this quality-improvement project could benefit from assessing the timeliness of TTA and extensively defining the demographic characteristics of patients who are not appropriately triaged to TTA. These data would benefit others to further improve the sensitivity and specificity of TTA criteria for diverse patient populations and better define methods of improving the timeliness of TTA. Understanding the patient demographic characteristics associated with undertriage at each centre may also provide important information for improving a centre’s TTA processes.
Limitations
We were limited in our change management process by baseline data collection only for patients with an ISS of 12 or greater, as the Alberta Trauma Registry records data only for these patients, whereas ongoing audits collected data for all such patients but also included those who may have had a lower ISS but met the new TTA criteria. In addition, the secondary measure of overtriage was not monitored during our study implementation. Therefore, a potential risk exists that overtriage increased substantially to capture all patients with major trauma, although it is possible that overtriage was limited by our improved physiologic TTA criteria. Future projects could include assessment of overtriage as a quality indicator. Our study did not assess clinical outcomes before rapid change cycles and therefore cannot comment on any specific associated improvements in clinical outcomes.
Conclusion
The rate of compliance with TTA protocols improved from 58.8% to more than 90% over a 2-year period, which shows the benefit of having a clearly outlined quality-improvement process. Baseline audits, a root-cause analysis to determine barriers, ongoing audits and transparency of data, as well as engagement of stakeholders to garner leadership support, determine organizational priority and carry out solutions were crucial. Changing cultural perception and practice to achieve compliance with an existing protocol requires engagement of stakeholders from the beginning of any change process. This allows for successful PDSA rapid change cycle implementation that focuses first on structure barriers, followed by process and outcomes.
Footnotes
This paper was presented at the Trauma Quality Improvement Program Annual Scientific Meeting and Training, Nov. 16–18, 2018, Anaheim, Calif.
Competing interests: V. Fawcett and S. Widder are members of the CJS editorial board, but they were not involved in the review or acceptance of this manuscript. No other competing interests declared.
Contributors: R. Saybel, V. Fawcett, B. Tsang, P. Mathura and S. Widder designed the study. K. Verhoeff, R. Saybel and S. Widder acquired and analyzed the data, which V. Fawcett and B. Tsang also analyzed. K. Verhoeff and S. Widder wrote the article, which all authors reviewed and approved for publication.
References
- 1.West JG, Cales RH, Gazzaniga AB. Impact of regionalization. The Orange County experience. JAMA Surg. 1983;118:740–4. doi: 10.1001/archsurg.1983.01390060058013. [DOI] [PubMed] [Google Scholar]
- 2.West JG, Trunkey DD, Lim RC. Systems of trauma care. A study of two counties. JAMA Surg. 1979;114:455–60. doi: 10.1001/archsurg.1979.01370280109016. [DOI] [PubMed] [Google Scholar]
- 3.Georgiou A, Lockey DJ. The performance and assessment of hospital trauma teams. Scand J Trauma Resusc Emerg Med. 2010;18:66. doi: 10.1186/1757-7241-18-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang C, Hsiao K, Shih H, et al. The role of trauma team activation by emergency physicians on outcomes in severe trauma patients. JACME. 2014;4:1–5. [Google Scholar]
- 5.Tsang B, McKee J, Engels PT, et al. Compliance to advanced trauma life support protocols in adult trauma patients in the acute setting. World J Emerg Surg. 2013;8:39. doi: 10.1186/1749-7922-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gerardo CJ, Glickman SW, Vaslef SN, et al. The rapid impact on mortality rates of a dedicated care team including trauma and emergency physicians at an academic medical center. J Emerg Med. 2011;40:586–91. doi: 10.1016/j.jemermed.2009.08.056. [DOI] [PubMed] [Google Scholar]
- 7.Petrie D, Lane P, Stewart TC. An evaluation of patient outcomes comparing trauma team activated versus trauma team not activated using TRISS analysis. Trauma and Injury Severity Score. J Trauma. 1996;41:873–5. doi: 10.1097/00005373-199611000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Mullins RJ, Mann NC, Hedges JR, et al. Preferential benefit of implementation of a statewide trauma system in one of two adjacent states. J Trauma. 1998;44:609–16. doi: 10.1097/00005373-199804000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Simons R, Eliopoulos V, Laflamme D, et al. Impact on process of trauma care delivery 1 year after the introduction of a trauma program in a provincial trauma center. J Trauma. 1999;46:811–5. doi: 10.1097/00005373-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Khetarpal S, Steinbrunn BS, McGonigal MD, et al. Trauma faculty and trauma team activation: impact on trauma system function and patient outcome. J Trauma. 1999;47:576–81. doi: 10.1097/00005373-199909000-00028. [DOI] [PubMed] [Google Scholar]
- 11.Driscoll PA, Vincent CA. Organizing an efficient trauma team. Injury. 1992;23:107–10. doi: 10.1016/0020-1383(92)90043-r. [DOI] [PubMed] [Google Scholar]
- 12.Perno JF, Schunk JE, Hansen KW, et al. Significant reduction in delayed diagnosis of injury with implementation of a pediatric trauma service. Pediatr Emerg Care. 2005;21:367–71. doi: 10.1097/01.pec.0000166726.84308.cf. [DOI] [PubMed] [Google Scholar]
- 13.Appendix A: Trauma Distinction indicator summary. Ottawa: Accreditation Canada; 2014. Trauma Distinction information package; pp. 6–9. [Google Scholar]
- 14.Rotondo MF, Cribari C, Smith RS, editors. Resources for optimal care of the injured patient 2014. Chicago: American College of Surgeons; 2014. [Google Scholar]
- 15.Mohan D, Barnato AE, Rosengart MR, et al. Trauma triage in the emergency departments of nontrauma centers: an analysis of individual physician caseload on triage patterns. J Trauma. 2013;74:1541–7. doi: 10.1097/TA.0b013e31828c3f75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rehn M, Eken T, Krüger AJ, et al. Precision of field triage in patients brought to a trauma centre after introducing trauma team activation guidelines. Scand J Trauma Resusc Emerg Med. 2009;17:1. doi: 10.1186/1757-7241-17-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mann D. The missing link: lean leadership. Front Health Serv Manage. 2009;26:15–26. [PubMed] [Google Scholar]
- 18.Block DJ. Healthcare outcome management: strategies for planning and evaluation. Sudbury (MA): Jones and Bartlett Learning; 2006. Quality improvement in health care — Donabedian’s principles of quality improvement; pp. 9–24. [Google Scholar]
- 19.The W Edwards Deming Institute. PDSA cycle. [accessed 2016 June 1]. Available: https://deming.org/explore/p-d-s-a.
- 20.van Tiel FH, Elenbaas TWO, Voskuilen BMAM, et al. Plan–Do–Study–Act cycles as an instrument for improvement of compliance with infection control measures in care of patients after cardiothoracic surgery. J Hosp Infect. 2006;62:64–70. doi: 10.1016/j.jhin.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 21.Donabedian A. The quality monitoring cycle. In: Bashshur R, editor. An introduction to quality assurance in health care. New York: Oxford University Press; 2003. p. XXVII. [Google Scholar]
- 22.Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260:1743–8. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- 23.Xiang H, Wheeler KK, Groner JI, et al. Undertriage of major trauma patients in the US emergency departments. Am J Emerg Med. 2014;32:997–1004. doi: 10.1016/j.ajem.2014.05.038. [DOI] [PubMed] [Google Scholar]
- 24.Smith TD, Snyder A, Hollen PJ, et al. Analyzing the usability of the 5-level Canadian Triage and Acuity Scale by paramedics in the prehospital environment. J Emerg Nurs. 2015;4:489–95. doi: 10.1016/j.jen.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 25.Mirhaghi A, Heydari A, Mazlom R, et al. The reliability of the Canadian Triage and Acuity Scale: meta-analysis. N Am J Med Sci. 2015;7:299–305. doi: 10.4103/1947-2714.161243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gage AM, Traven N, Rivara FP, et al. Compliance with Centers for Disease Control and Prevention field triage guidelines in an established trauma system. J Am Coll Surg. 2012;215:148–54. doi: 10.1016/j.jamcollsurg.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 27.Dehli T, Monsen SA, Fredriksen K, et al. Evaluation of a trauma team activation protocol revision: a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2016;24:105. doi: 10.1186/s13049-016-0295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rainer TH, Cheung NK, Janice HH, et al. Do trauma teams make a difference? Resuscitation. 2007;73:374–81. doi: 10.1016/j.resuscitation.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 29.Deane SA, Gaudry PL, Pearson I, et al. The hospital trauma team: a model for trauma management. J Trauma. 1990;30:806–12. doi: 10.1097/00005373-199007000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Krüger AJ, Hesselberg N, Abrahamsen GT, et al. When should the trauma team be activated? Tidsskr Nor Laegeforen. 2006;126:1335–7. [PubMed] [Google Scholar]
- 31.Duffy G, Moran J, Riley W. Solve the real problem using root cause analysis. Washington: Public Health Foundation; 2012. [Google Scholar]
- 32.Brugha R, Varvasovszky Z. Stakeholder analysis: a review. Health Policy Plan. 2000;15:239–46. doi: 10.1093/heapol/15.3.239. [DOI] [PubMed] [Google Scholar]
- 33.Rossi MCE, Nicolucci A, Arcangeli A, et al. Baseline quality-of-care data from a quality-improvement program implemented by a network of diabetes outpatient clinics. Diabetes Care. 2008;31:2166–8. doi: 10.2337/dc08-0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fernandes O, Shojania KG. Medication reconciliation in the hospital. Healthc Q. 2012;15:42–9. doi: 10.12927/hcq.2012.22842. [DOI] [PubMed] [Google Scholar]
- 35.Etchells E, Matlow A, Coffey M, et al. Implementation of admission medication reconciliation at two academic health sciences centres: challenges and success factors. Healthc Q. 2009;12:102–9. doi: 10.12927/hcq.2009.20719. [DOI] [PubMed] [Google Scholar]
- 36.Moore L, Lavoie A, Bourgeois G, et al. Donabedian’s structure–process–outcome quality of care model: validation in an integrated trauma system. J Trauma Acute Care Surg. 2015;78:1168–75. doi: 10.1097/TA.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 37.Iedema R, Ball C, Daly B, et al. Design and trial of a new ambulance-to-emergency department handover protocol: ‘IMIST-AMBO’. BMJ Qual Saf. 2012;21:627–33. doi: 10.1136/bmjqs-2011-000766. [DOI] [PubMed] [Google Scholar]
- 38.Sakellariou A, McDonald PJ, Lane RH. The trauma team concept and its implementation in a district general hospital. Ann R Coll Surg Engl. 1995;77:45–52. [PMC free article] [PubMed] [Google Scholar]
- 39.Cornwell EE, 3rd, Chang DC, Phillips J, et al. Enhanced trauma program commitment at a level 1 trauma center: effect on the process and outcome of care. Arch Surg. 2003;138:838–43. doi: 10.1001/archsurg.138.8.838. [DOI] [PubMed] [Google Scholar]
- 40.Kunkel S, Rosenqvist U, Westerling R. The structure of quality systems is important to the process and outcome, an empirical study of 386 hospital departments in Sweden. BMC Health Serv Res. 2007;7:104. doi: 10.1186/1472-6963-7-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Deane SA, Gaudry PL, Pearson I, et al. Implementation of a trauma team. Aust N Z J Surg. 1989;59:373–8. doi: 10.1111/j.1445-2197.1989.tb01589.x. [DOI] [PubMed] [Google Scholar]
- 42.Waddell D, Amrik SS. Resistance: a constructive tool for change management. Manage Decis. 1998;36:543–8. [Google Scholar]
- 43.Yoo YMS. The advantages of early trauma team activation in the management of major trauma patients who underwent exploratory laparotomy. Ann Surg Treat Res. 2014;87:319–24. doi: 10.4174/astr.2014.87.6.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shim H, Jang JY, Lee JG, et al. Application of critical pathway in trauma patients. J Trauma Inj. 2012;25:159–65. [Google Scholar]
- 45.Lee DK, Lee KH, Cha KC, et al. Effectiveness of simple trauma team activation criteria on prognosis of severe trauma patients. J Korean Soc Traumatol. 2009;22:71–6. [Google Scholar]
- 46.Kaplan LJ, Santora TA, Blank-Reid, et al. Improved emergency department efficiency with a three-tier trauma triage system. Injury. 1997;28:449–53. doi: 10.1016/s0020-1383(97)00088-0. [DOI] [PubMed] [Google Scholar]