Abstract
Intestinal obstruction caused by pericecal internal herniation are rare and only described in a few cases. This case describes an 80-year-old man presented with acute abdominal pain, nausea and vomiting, with no prior surgical history. Computed tomography was performed and showed a closed loop short bowel obstruction in the right lower quadrant and ascites. Laparoscopy revealed pericecal internal hernia. This is a viscous protrusion through a defect in the peritoneal cavity. Current operative treatment modalities include minimally invasive surgery. Laparoscopic repair of internal herniation is possible and feasible in experienced hands. It must be included in the differential diagnoses of every patient who presents with abdominal pain. When diagnosed act quick and thorough and expeditiously. Treatment preference should be a laparoscopic procedure.
Keywords: intestinal obstruction, pericecal internal herniation
INTRODUCTION
Internal hernias have an overall incidence of <1% [1]. Intestinal obstruction caused by pericecal internal herniation is rare and only described in a few cases [2]. Early recognition can be challenging, especially with no surgical abdominal history. Untreated strangulated internal hernias have an overall mortality exceeding 50% [1,3,4]. Internal hernias are protrusion of viscus through a normal or abnormal aperture. The orifice can be either acquired or congenital, including both normal apertures, such as the foramen of Winslow, and abnormal apertures arising from anomalies of internal rotation and peritoneal attachment [1]. Laparoscopic repair of internal herniation is possible and feasible in experienced hands. We present a case of an 80-year-old man with a strangulated jejunum in a pericecal internal herniation.
CASE REPORT
An 80-year-old man, with a history of peripheral arterial disease, presented with acute abdominal pain, nausea and vomiting. On physical examination, the patient was afebrile with a blood pressure of 141/79 mmHg and pulse rate of 51 beats per minute. Abdominal examination revealed a tender palpable mass in the right lower quadrant. His white blood cell count was 10.0 x 109/l, and the C-reactive protein level was <1 mg/l. Ultrasonography revealed short bowel distension. A complementary computed tomography (CT) was performed and showed a closed loop short bowel obstruction in the right lower quadrant and ascites (Fig. 1).
Figure 1.
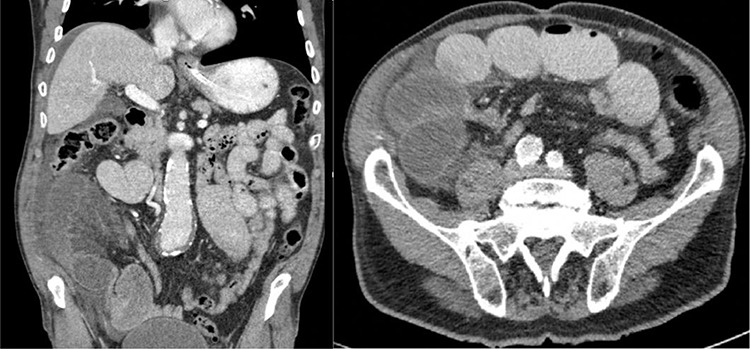
CT: demonstrates closed loop short bowel obstruction with dilated small-bowel loops and ascites
It was decided to perform a diagnostic laparoscopy. Surgery showed a small bowel obstruction. At the same time, there was ischemic intestine visible through the connections of coecum to the abdominal wall (Fig. 2).
Figure 2.
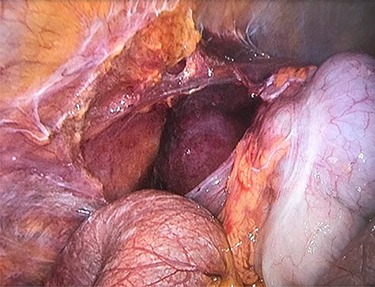
ischemic intestine visible through the incised connections of coecum to the abdominal wall during laparoscopy
There appeared to be an incarcerated pericecal internal herniation of small intestine in the retrocecal fossa. After incising the fascia of Told, we managed to free the ischemic looking small intestine (Fig. 3). A laparoscopic small bowel resection and an isoperistaltic stapled intracorporeal side-to-side anastomosis were performed. The postoperative course was uneventful. After 1 month, the patient was seen at the outpatient clinic and showed complete recovery without any complications.
Figure 3.
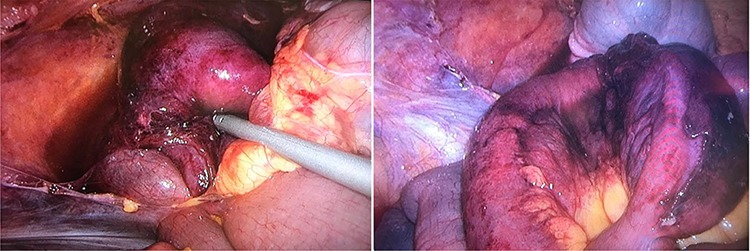
perioperative pictures of the pericecal internal hernia and the necrotic small bowel
DISCUSSION
As mentioned before, internal hernias are a rare phenomenon, especially without a surgical abdominal history. In this case, it is most likely that the hernia orifice is a congenital anatomic structure. An internal hernia is defined as a protrusion of the abdominal viscera into the fossae, recesses or congenital defects within the abdominal or pelvic cavity [5]. The pericecal fossa is located behind the cecum and ascending colon and is limited by the parietocecal fold outward and the mesentericocecal fold inward [6]. The pericecal peritoneum is the end result of ileocecal migration occurring during midgut rotation in the fifth month of gestation. Toward the end of the rotational process, the cecum normally arrives in the right iliac fossa, then fuses and resorbs the peritoneal surface. Four types of peritoneal recesses of various depths resulting from imperfect fusion or resorption occur in the pericecal area superior ileocecal recess, inferior ileocecal recess, retrocecal recess and paracolic sulci all of which may become hernia orifices [5]. In this case, the jejunum was probably incarcerated in a retrocecal recess. Rapid and adequate diagnosis is essential in the treatment of pericecal hernias, but this can be difficult due to its exceptional incidence and vague symptoms. In the past, a laparotomy was often performed for intestinal obstructions. Nowadays, the minimal invasive laparoscopy is feasible for small bowel obstructions in experienced hands. When intracorporeal anastomosis is performed, this will lead to less traction on the mesentery. By performing an intracorporeal anastomosis, the incision for specimen extraction can be smaller and the incision can be performed in the lower part of the abdomen, which has shown to be associated with less pain, less pulmonary morbidity, a lower infection rate and on the long-term lower herniation rate [7].
In conclusion, we should be aware of this rare entity, and it must be included in the differential diagnoses of every patient who presents with abdominal pain. When diagnosed with an intestinal obstruction caused by pericecal internal herniation act quick and thorough treatment preference should be a laparoscopic procedure and when resection is necessary, an intracorporeal anastomosis is feasible in experienced hands.
Conflict of interest statement
None declared.
References
- 1. Martin LC, Merkle EM, Thompson WM. Review of internal hernias: radiographic and clinical findings. Am J Roentgenol 2006;186:703–17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16498098[cited 20 February 2019]. [DOI] [PubMed] [Google Scholar]
- 2. Lee JE, Choi S-Y, Lee MH, Yi BH, Lee HK, Ko BM. Pericecal herniation of sigmoid colon diagnosed by computed tomography: two case reports. Medicine (Baltimore) 2018;97:e11336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Newsom BD, Kukora JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg 1986;152:279–85. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3752377[cited 19 February 2019]. [DOI] [PubMed] [Google Scholar]
- 4. Ghahremani G. Abdominal and pelvic hernias In: Gore RMLM. (ed). Textbook of Gastrointestinal Radiology, 2nd edn. Philadelphia: PA: Saunders, 2000, 1993–2009 [Google Scholar]
- 5. Kabashima A, Ueda N, Yonemura Y, Mashino K, Fujii K, Ikeda T, et al. Laparoscopic surgery for the diagnosis and treatment of a paracecal hernia repair: report of a case. Surg Today 2010;40:373–5. [DOI] [PubMed] [Google Scholar]
- 6. Mathieu D, Luciani A, GERMAD Group . Internal abdominal herniations. AJR Am J Roentgenol 2004;183:397–404. Available from: http://www.ajronline.org/doi/10.2214/ajr.183.2.1830397[cited Feb 3 February 2019]. [DOI] [PubMed] [Google Scholar]
- 7. Oostendorp S, Elfrink A, Borstlap W, Schoonmade L, Sietses C, Meijerink J. et al. Intracorporeal versus extracorporeal anastomosis in right hemicolectomy: a systematic review and meta-analysis. Surg Endosc 2017;31:64–77. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27287905[cited 19 February 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]


