Abstract
Root resorption (RR) refers to noninfectious damage related to the loss of hard and soft dental tissue that results from clastic cell activity. It is observed as a pathologic process that is predominantly asymptomatic in the permanent dentition and physiological during the shedding of primary teeth. Roots are protected by unmineralized organic cementoid and predentine. RR occurs because of the inability of the clastic cells to adhere to unmineralized surfaces. Since the first RR classification was described by Andreasen in the 1970s, several classifications have been proposed with diverse terminology. A narrative literature review was undertaken on the current classification, diagnosis, pathophysiology, and treatment of RR. A bibliographic search resulted in 434 titles and abstracts, and from those, 17 articles were obtained that alluded to 15 RR classifications. A total of 28 articles that met the inclusion criteria were included. Results showed that Andreasen’s classification is the most widely used for classifying RR. In terms of epidemiologic data, studies are scarce, although RR pathophysiology is well described in the literature. Overall clinical guidelines are summarized in a new RR classification diagram. The choice of RR treatment application should be in line with the RR type and the dentist’s experience. However, an earlier and correct diagnosis will significantly improve final outcomes and long-term prognosis, especially with the current evolution of advanced imaging techniques, such as cone-beam computed tomography and bioceramic-based endodontic sealers.
Keywords: Root resorption classification, root resorption clinical aid proposal, RR diagnosis, RR pathophysiology and RR treatment
HIGHLIGHTS.
The present narrative review aims to synthetize information from the 15 RR classifications with a focus on a new RR classification diagram to help the clinician.
A new RR clinical aid proposal is elaborated for use and validation in the clinical area; however, it can also be applied in the education and research fields.
With the current progress of laboratorial and histological techniques, RR classifications have become itemized with several subcategories, and based on this, the present review endorsed for the first time a summary in which it is possible to compare and analyse numerous terms from several RR classifications from 1970 to 2016.
INTRODUCTION
Resorption of hard dental structures was first described in the 16th century, and root resorption (RR) in deciduous teeth is a typical physiologic response. However, in permanent dentition, RR has a pathologic basis, and the aetiology requires two phases: an injury and stimulus (1-3). RR types can be classified into internal (pulp source) and external (periodontal ligament origin). Dentine is lined internally from the pulpal surface by the odontoblastic layer and predentine and externally from the periodontium by the cementoblastic layer and precementum. Both layers form the barrier that prevents resorption and odontoclasts (similar to osteoclasts) from adhering or reabsorbing unmineralized matrix. Because of the inhibitory effects of organic precementum and predentine, even in the presence of inflammation, an intact root is resistant to resorption. However, with an initial stimulus (infection or trauma) at one or more of the four barriers (3), mineralized dentine is vulnerably exposed, and for RR to occur, two events are necessary: (1) loss or alteration of the precementum or predentine protective layer and (2) injury of the unprotected root surface (4).
The RR process may be self-limiting and go undetected clinically; however, once initiated and with the initial injury and stimulus sustained, destruction of hard dental tissue will continue, and tooth tissue loss may occur (5). External RR (ERR) has various causes and is more prevalent than internal RR (IRR), which is relatively rare (6). Several classifications have been proposed, with distinctive terms and categories used to describe RR.
This article reviews the literature concerning RR classifications and introduces for the first time a table summary to compare several taxonomy variations of RR concepts. In addition, it presents a new classification diagram with synthetized RR information to guide the clinician toward a clear diagnosis. The article also proposes a new clinical aid for routine assessment to be used and validated in the clinical field, which highlights the key role of bioceramic-based endodontic sealers.
MATERIALS AND METHODS
For this comprehensive narrative literature review (7), eligibility criteria were (a) complete articles published in the English language, (b) original papers with complete RR classification, (c) clinical studies, and (d) reviews. The exclusion criteria were (a) non-English and unpublished data, (b) conference papers, (c) letters to the editor, and (d) papers regarding RR subcategories. Initially, the aim was to investigate the terms “Tooth Resorption” AND “Root Resorption.” Briefly, the authors used PubMed to identify Medical Subject Heading (MeSH) terms corresponding to each term. However, the use of MeSH terms is not common to all articles, which made this search method unfeasible. Subsequently, widespread Wiley Online Library (WOL), Cochrane Collaboration, Evidence Based Dentistry (EBD), Journal of Evidence-Based Dental Practice (JEBDP), and PubMed automated searches were performed from January 1966 to May 2018 using various combinations of the following key indexing terms: (a) dental root resorptions, (b) root resorptions classification, (c) root resorptions diagnosis, (d) root resorptions pathophysiology, and (e) root resorptions treatment.
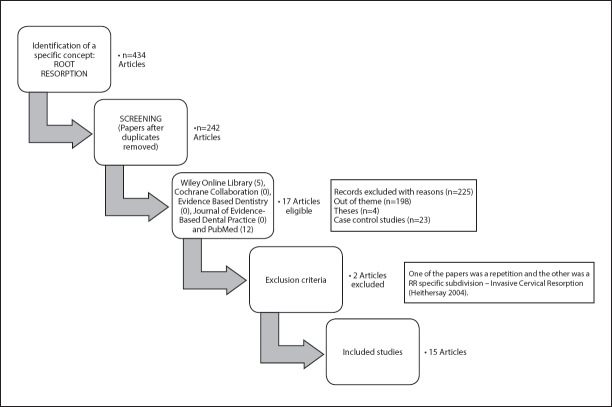
Two reviewers screened all article titles and abstracts retrieved from the electronic search independently and in duplicate. A review was then performed to reject articles that did not meet inclusion criteria. Disagreement between reviewers was solved via debate. Hand searching of reference lists of original and reviewed articles that were found to be relevant was also performed. Full-text copies of all articles were obtained, and each reviewer determined which were eligible based on the inclusion and exclusion criteria. The literature search provided 434 titles and abstracts (Fig. 1).
Figure 1.
Study selection flowchart incorporated in the present narrative review
RESULTS
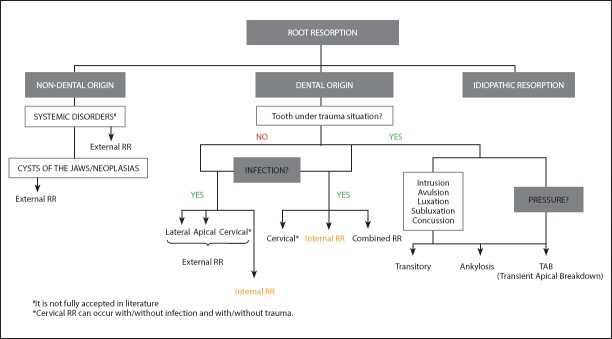
Fifteen studies from the past 50 years were related to RR classification (1-5, 8-17) and are summarized in Table 1. The Heithersay classification of invasive cervical RR (and its four subdivisions) was not included as it relates to only a specific subdivision of RR (10). Amongst all RR classifications, the Andreasen classification is fundamental and the most widespread (1), as all subsequent classifications have cited it, and comparison amongst classifications are always made with the Andreasen classification. Moreover, the authors consider the Kanas classification to be the most complete with full descriptions and categorizations (11). In Figure 2, a new classification diagram based on clinical features and etiological evaluations is suggested to help the clinician classify the RR cases by organizing and summarizing information from entirely previous classifications (Table 2).
TABLE 1.
Chronological RR classifications reviewed from 1970 to 2016
| Author | Year | Based on | Classification divisions |
|---|---|---|---|
| Andreasen J. | 1970 | Localization, type and trauma | I. Internal resorption-Replacement, Inflammatory II. External resorption-Surface, Replacement, Inflammatory |
| Gartner et al. | 1976 | Localization | I. Internal resorption-Coronal, Mid-root II. External resorption-Coronal, Mid-root, Apical |
| Feiglin B. | 1986 | Localization | I. Internal resorption II. External resorption-Physiological, Orthodontic treatment, Trauma, Impacted tooth pressure III. Inflammatory resorption-Cervical, Apical |
| Tronstad L. | 1988 | Localization and type | I. Transient inflammatory resorption II. Progressive inflammatory resorption III. Internal resorption IV. External resorption-Progressive inflammatory, Cervical, Dentoalveolar Ankylosis and Replacement |
| Trope M. | 1998 | Aetiology and trauma origin | I. External resorption Type 1–Attachment Damage Alone (Pressure, Mild and Severe Traumatic Injury) Type 2–Infection Alone (Apical and Marginal Periodontitis) Type 3–Attachment Damage Plus Infection (Periradicular Root Resorption of Pulpar Origin and Subattachment Root Resorption of Sulcular Origin) II. Internal resorption |
| Ne et al. | 1999 | Localization and type | I. Internal resorption–Metaplastic resorption (root canal replacement resorption); Inflammatory II. External resorption-Surface, Inflammatory (External and Cervical RR with or without vital pulp as Invasive Cervical RR), Replacement and Ankylosis III. Combined internal and external resorption IV. Transient Apical Breakdown (TAB) |
| Gunraj et al. | 1999 | Localization and type | I. External resorption associated with traumatic injuries-Surface, Inflammatory and Replacement II. External resorption from pulp necrosis and periradicular pathosis III. External resorption from pressures in the PDL IV. Internal resorption V. Cervical resorption |
| Trope M. | 2002 | Dental trauma | I. External resorption-a) Stimulus of short duration (transient stimulus); b) Stimulus of long time periods (progressive stimulus): pression and pulp space infection (apical and lateral periodontitis); c) Sulcular infection. II. Internal resorption |
| Fuss et al. | 2003 | Aetiology | I. Pulpal infection II. Periodontal infection III. Orthodontic pressure IV. Impacted tooth or tumour pressure V. Ankylotic |
| Lindskog et al. | 2006 | Aetiology | I. Trauma-Surface, Transient Apical Internal Resorption (TAIR), Orthodontic, Pression, Replacement. II. Infection-Internal inflammatory apical and radicular, External inflammatory, Inflammatory communicative (internal-external) III. Hyperplasic invasive-Internal replacement, coronal, cervical and radicular Patel and Pitt-Ford 2007 Localization I. External resorption-Surface, Replacement, Inflammatory, Cervical and TAB II. Internal resorption-Inflammatory |
| Santos et al. | 2011 | Aetiology | I. External resorption-Trauma II. Surface resorption III. Replacement resorption IV. Inflammatory resorption V. Atypical resorption |
| Kanas and Kanas | 2011 | Localization, aetiology and Type | I. Dental Origin 1. Internal resorption-Infective, inflammatory, trauma: a) Radial pulp enlargement resorption; b) Metaplastic (replacement) pulp resorption I. Dental Original - External resorption 2. External resorption-a) Physiological apical resorption: External surface resorption, TAR; b) Infective/Inflammatory resorption: Apical (pulp) inflammatory resorption, Cervical (periodontal) inflammatory resorption; c) Trauma (avulsed/luxated/fractured): TAB, Periapical replacement resorption (PARR) with ankylosis, Infective/inflammatory (apical or cervical); d) Pressure: Orthodontic (TAB, PARR without ankylosis), Impacted teeth, Occlusal forces; e) Idiopathic: Localized apical resorption (PARR without ankylosis), Multiple apical resorption (PARR without ankylosis); Multiple cervical resorption; f) Surgical: Bone grafts of alveolar clefts. Ii. Nondental Origin 1. Internal resorption - Herpes zoster infection. 2. External resorption - Neoplasia/cysts of the jaws; Systemic disorders. |
| Darcey and Qualtrough | 2013 | Aetiology | I. External surface resorption II. External inflammatory resorption III. External cervical resorption IV. External replacement resorption V. Internal resorption - Surface, inflammatory, replacement |
| Sak et al. | 2016 | Aetiology | I. Internal resorption - Inflammatory (types A, B, C, D); Replacement. II. External resorption - Ankylosis and replacement resorption; Apical inflammatory RR; Resorption associated with systemic diseases; Lateral inflammatory resorption; Resorption caused by chronic mechanical injuries; Cervical resorption. |
Figure 2.
A new RR classification diagram based on clinical features and aetiological evaluations
TABLE 2.
Analogous terms of RR reviewed among the 15 RR classifications
| J. ANDREASEN (1970) | GARTNER et al. (1976) | B. FEIGLIN (1986) | L. TRONSTAD (1988) | M. TROPE (19987) | NE et al. (1999) | GUNRAJ et al. (1999) | M. TROPE (2002) | FUSS et al. (2003) | LINDSKOG et al. (2006) | PATEL and PITT- FORD (2007) | SANTOS et al. (2011) | KANAS and KANAS (2011) | DARCEY and QUALTROUGH (2013) | SACK et al. (2016) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surface RR | External RR (ERR) Coronal | Transient Inflammatory Resorption | ERR - Type 1 Attachment Damage Alone: Pressure, mild and severe traumatic injury | Surface RR | Surface RR (trauma) | Transient ERR (stimulus of short duration) | Surface RR | Surface RR | Surface RR | Surface RR | Surface RR | |||
| Transient Apical Breakdown (TAB) | Transient Apical Internal Resorption (TAIR) | TAB | TAB | TAB | ||||||||||
| External Replacement | ERRR and Dentoalveolar | ERRR and Ankylosis | ERRR (trauma) | Ankylosis | ERRR | ERRR | ERRR | Periapical Replacement | ERRR | ERRR and Ankylosis | ||||
| RR (ERRR) | Ankylosis | RR (PARR) with ankylosis | ||||||||||||
| External Inflammatory RR (EIRR) | ERR Midroot | ERR - Type 2 Infection Alone: Alone and Marginal Periodontitis | EIRR | EIRR (trauma) | Lateral periodontitis with RR | Pulpal Infection RR | EIRR | EIRR | EIRR | EIRR | EIRR and Lateral RR EIRR and Lateral RR | |||
| ERR Apical | Apical Inflammatory RR (AIRR) | Periradicular RR of Pulpar Origin | AIRR | ERR from Pulp Necrosis and Periradicular Pathosis | Apical periodontitis with RR | AIRR (pulp origin) | AIRR | |||||||
| Orthodontic forces; pressure and trauma | Progressive Inflammatory Resorption | ERR from the periodontal ligament pressure | ERR (stimulus of long duration – progressive) | Orthodontic pressure | RR induced by Trauma (pressure or orthodontic forces) | External RR (pressure) | ||||||||
| Internal Inflammatory RR (IIRR) | Internal RR (IRR) (Coronal and Mid-root) | IRR | IRR | IRR | IIRR | IIRR | IRR | IRR | IIRR (Apical and Radicular) | IIRR | IIRR | Radial Pulp Enlargement RR | IRR | IIRR (Types A, B, C and D) |
| Internal Replacement RR (IRRR) | Metaplastic Resorption | IRRR | IRRR (Hyperplasic Invasive) | Metaplastic (Replacement) Pulp | IRRR | |||||||||
| Cervical Inflammatory RR | Cervical RR (CRR) | Subattachment RR of Sulcular Origin | CRR | CRR | ERR with Sulcular Infection | Periodontal Infection RR | Hyperplasic Invasive Cervical RR | CRR | Resorption Cervical (periodontal) Inflammatory RR | CRR | CRR | |||
| ERR - Type 3 Attachment damage plus infection | Combined RR (internal- external) | Inflammatory communicative (internal- external) | ||||||||||||
| ERR from impacted tooth | ERR from impacted tooth or tumour | ERR from Neoplasia/ cysts of the jaws |
RR diagnosis
An early diagnosis is the most critical and favourable factor in RR management, because the earlier the treatment is initiated, the less severe the resorption consequences will be. Classical diagnosis was obtained from the combination of a rigorous clinical examination and radiography, as the lack of pathognomonic symptoms increases the difficulty of an accurate diagnosis (12). Although teeth affected by RR are usually asymptomatic, and the diagnosis may result in its incidental discovery upon radiographic examination, sensibility tests might be useful for RR recognition (13, 14) and are mandatory for differential diagnosis. Full extra- and intraoral clinical examination must be implemented as a first step. In particular, cervical teeth discoloration, described earlier as Mummery or pink spot (15), is indicative of RR as it is related to the highly vascularized connective tissue adjacent to the resorbing cells. Moreover, as the pulp becomes necrotic, this colour turns grey (16). All restorations should be verified (leaking margins and recurrent caries), and the percussion should be noted and compared with adjacent teeth (as an example, a metallic sound may suggest an ankylosis). In terms of teeth mobility, it should be noticed that an increase in mobility may indicate attachment loss or pathological fracture due to extensive ERR or IRR, and a complete loss of physiological mobility may also indicate an ankylosed tooth (17).
Intraoral radiographies are the most common approach used for RR diagnosis, and most clinical studies use the radiographies of an irregular root surface outline at different angles to determine which surface is affected (18). Panoramic radiography is a classical technique that has been used to assess RR (19), and the use of an intraoral radiograph combined with a panoramic radiography has been proposed to reduce the evaluation shortcomings in the anterior regions (20).
Currently, as the limitations of routine dental radiography are widely known, a significant number of case reports have demonstrated that cone-beam computed tomography (CBCT) can enhance the diagnosis of resorptive lesions in earlier stages. The detailed visualization afforded by CBCT is also associated an improvement in final outcomes (21, 22). However, the accuracy of CBCT in the detection of surface defects (although higher than conventional imaging modalities) is not perfect (23) and appears to spread with increasing voxel resolution of the volumetric data set (24). CBCT can also be applied accurately in the assessment of the postorthodontic apical RR (19) and can be used to meticulously and rigorously observe lateral maxillary incisors roots by impacted maxillary canines (25). Unlike ERR, with its irregular radiolucency of the intact root canal, IRR has clearly defined borders with no canal delineation visible radiographically in the defect. CBCT has been successfully used to confirm the presence of IRR and differentiate it from ERR (21). CBCT has also been shown to determine the RR complexity with precision, and it can guide the clinician as to the detailed extent of the resorptive lesion (26). However, CBCT must be considered as an adjunct and not a substitute for conventional radiography, as it can be considered only after clinical and conventional radiographic examination (5).
CBCT referrers and interpreters are strongly advised to follow the European Society of Endodontology position statement on the use of CBCT in endodontics (27).
RR treatment
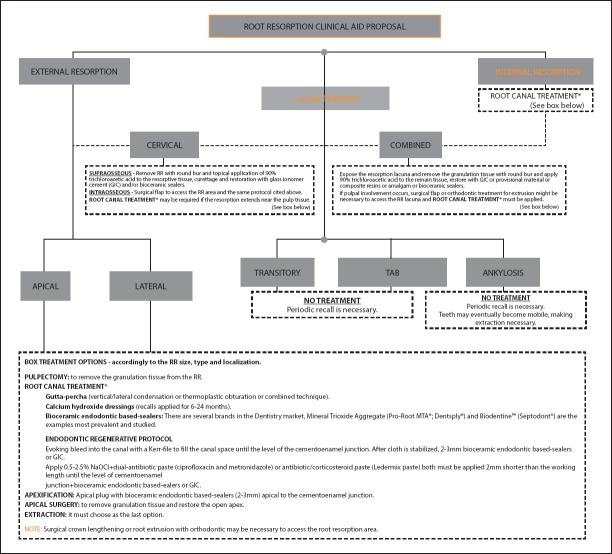
The proper treatment selection must address the combination of identified stimulation factors (13), and clinician experience (36). Subsequent to this theoretical concept, the authors add a clinical aid proposal in which are summarized the RR types and correspondent treatment options, drafted in Figure 3. Bioceramic-based endodontic sealers (calcium-silicate and calcium-phosphate based) present high biocompatibility and bioactivity with cicatrisation properties and new hard tissue formation. These hydraulic bioceramic sealers can be used in humid and wet environments and in direct contact with organic tissue fluids such as blood and water, and they release calcium hydroxide, which interacts with tissue fluids and phosphates, leading to hydroxyapatite formation during the setting process (37). Once the apatite nuclei are formed, they grow spontaneously by consuming the calcium and phosphates from high-pH physiological fluids. Calcium ions released from sealers to host tissue also accelerate apatite formation, because of the ionic activity product of apatite of fluids, and this property is responsible for the tissue-inductive properties of CsbES sealers (38, 39). The initial dressing of calcium hydroxide followed by obturation with bioceramic sealers may be considered an alternative treatment modality for several types of RR (internal, combined, cervical, external, apical, and lateral). However, it is important to mention that in specific RR cases, especially in teeth under trauma but with no signals of infections (transitory, transient apical breakdown, and ankylosis), no treatment is recommended.
Figure 3.
Clinical aid proposal for root resorption assessment
RR pathophysiology
Bone and RR in both physiologic and pathologic instances involves a coordinated interaction among osteoblasts and osteoclasts as well as odontoblasts and odontoclasts that are regulated by the OPG/RANK/RANKL system (28) (Fig. 4). Osteoprotegerin (OPG), a receptor activator of nuclear factor kappa B (RANK) and receptor activator of nuclear factor kappa B ligand (RANKL), is involved as a paracrine regulator of odontoclastogenesis and bone metabolism (29). The RR cellular complex mechanism is analogous to osteoclastic bone resorption, and the origin of clastic cells is related to the viable blood supply, which is one of the reasons for the minor incidence of IRR (3). At RR, the resorbing activity of odontoclasts is related to the expression of the OPG/RANK/RANKL system by periodontal ligament (PDL) cells (30). The interaction between RANK and RANKL is required for odontoclast differentiation, and OPG acts as a soluble receptor antagonist for neutralized-RANKL that prevents it from binding to an activated RANK (31).
Figure 4.
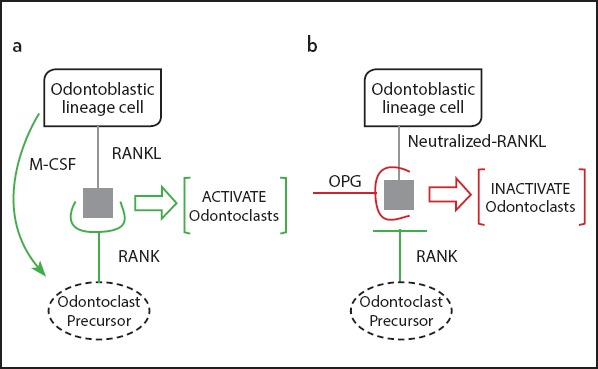
Representative scheme of RANK/RANKL/OPG system in the activation and inactivation of odontoclasts adapted from Tyrovola et al. in 2008
The summarized RR mechanism includes the mediation of three types of local cells (T-cells, odontoblasts, and fibroblasts from PDL). Under a stimulus, with a local increase of cytokines, T-cells are activated and express RANKL, and subsequently, differentiation and activation of pre-odontontoclasts occur. Odontoblasts and fibroblasts, which express RANKL, interact with mononuclear progenitors as well as bioactive neuropeptides such as substance neurokinin A (NKA), neuropeptide (NPY), and calcitonin gene-related peptide (CGRP) (32). Cytokines, interleukin-β (IL-β) and IL-6, prostaglandin E2, tumour necrosis factor α (TNF-α), and hormones induced by the debilitated PDL stimulate the expression of RANKL by fibroblasts and play a part through their vasoactive, chemotactic, and cellular effects. Those events consequently led to the recruitment of active odontoclasts, which promotes the beginning of the RR process (30). The clastic cells adhere to the mineralized surface, leading to the release of hydrogen ions and proteolytic enzymes, crafting a localized and acidic microenvironment, and resulting in mineralized tissue dissolution and loss (32). Although the RANKL expression is not directly affected by OPG synthesis, it has been shown that PDL from nonresorbing deciduous teeth and permanent teeth express OPG but not RANKL (30). In contrast, PDL from resorbing teeth express predominantly RANKL and less OPG (28). In the dental follicle environment, the ratio of OPG to RANKL supports, rather than inhibits, osteoclastogenesis. Also, the role of RANKL with macrophage colony-stimulating factor is to promote supportive bone production. The primary OPG function is as a soluble decoy receptor for RANKL as it lacks its transmembrane and cytoplasmic domains secreted as soluble protein, as well as inhibition of osteoclast differentiation, osteoclast resorptive function, and stimulation of osteoclast apoptosis (33). The presence of OPG in serum is an absolute requirement for bone mass maintenance by making sufficient quantities of RANKL unavailable. Several studies (34, 35) have investigated the use of OPG as an antiresorptive mediator for treating a variety of bone resorptions, but until now, its use for endodontic clinical RR management has not been addressed.
DISCUSSION
The present narrative review aims to compile the 15 RR classifications and compare them to find their similarities and differences and to expose several taxonomy divergences. Amongst all of the classifications, the most complete is the Kanas and Kanas classification (11), although Andreasen’s was the first RR classification resulting from several years of reliable clinical dental traumatology documentation (1). Andreasen’s is also the RR classification most cited in the literature and is widely accepted as the historical reference; subsequently, all of the fourteen following classifications that categorize RR by localization (internal and external) cite Andreasen study. Subsequently, IRR is segmented into replacement and inflammatory, and ERR is divided into surface, replacement, and inflammatory.
RR is considered a single pathological entity and with an early diagnosis, and complemented with CBCT, a better treatment prognosis is expected (19). However, the major difficulty within RR is the proper diagnosis of each entity, as it relies mostly on clinician experience. Even more, the same resorptive lesion area can be classified with different RR terms according to the author who introduces a new RR classification. For this reason, this review intends to correlate similar pathophysiology entities (with distinct designations) as well as help the clinician not only in properly classification but also in treating the RR correctly.
External surface RR (ESRR) results from a minimal pathological stimulus on the root surface PDL and matches to a transient lesion that is repaired with the formation of a cement-like tissue and a new PDL with vital pulp (1). When the pathological stimulus is extensive (≥20%) and there is proximity to the alveolar bone and/or the bone grafts are nearly to the root (40), the bone repair process overlaps the PDL reparation, resulting in root surface fusion, with the adjacent bone initiating an ankylosis (41). A continuous and prolonged substitution of dentaltissue by bone results in an external replacement RR (ERRR) because of the nature of bone modulation. Ne et al. performed a differential diagnosis of ankylosis with ERRR, and found that, as supported by histology, ERRR is associated with inflammation of the connective tissue whereas ankylosis is not (42).
IRR is relatively rare and characterized by an uneven root canal enlargement (1). It initiates from the canal to the mineralized walls and occurs as a result of trauma or caries with micro-organism invasion to the pulp. The resorptive process is active only in areas where the pulp remains vital (11). Internal replacement RR (IRRR) is associated with mineralized tissue deposition within the pulp inside the canal after misplacement of a substantial amount of dentine and is also visible in internal inflammatory RR (IIRR), which was primarily described by Andreasen (1). In recent years, two distinct teams have defined IIRR as internal metaplastic RR, since it allocates the dentine reabsorption and the subsequent deposition of hard tissue (bone or cement) but never dentine (11, 16).
IRR nomenclature has varied slightly over the past years, being characterized by the presence of a vital pulp at least in the root apical region. Even within this, Sak et al. subdivided IRR into two groups (replacement and inflammatory) (3). Consequently, IIRR is allocated to four subtypes (A and D due to crown; B and C proper to the root). In A, there is a tooth crown alteration (mainly described as a pink tooth), wherein the crown limits intact. In type D, the crown presents perforation. In type B, a bubble or oval resorption of the symmetrical gap of the root canal with a clearly regular and well-limited smooth wall is observed. In C, there is a canal wall perforation, and additional thinning of the alveolar bone in the perforation vicinity occurs (3).
In 1976, Gartner et al. expressed the same RR categorization as Andreasen with the root split into three portions (coronal, mid-root, and apical). They described the radiographic criteria of the mesial-buccal-distal (MBD) rule as a predictable method for differentiation among RR entities (8).
A decade later, Feiglin classified RR as internal, external, and inflammatory based on localization, with particular emphasis on avulsion cases (43). Afterward, Tronstad elaborated a review centred on RR localization and type, such as inflammatory RR (transient and progressive), IRR, and ERR (40).
In 1998, Trope described two groups of IRR and ERR based on the aetiology and trauma origin (2) and exclusively dental trauma based in 2002 (4). Trope made a substantial effort to define the precise IRR and ERR aetiology. In 1998, the assessment was related to the presence of the periodontal lesion, infection, or combination of both. In 2002, the aetiology appraisal of ERR was broadened to include stimulus duration (short or extended) and infection in an attempt to determine how root-protective layers have been affected and the source of the inflammatory response (4).
Ne et al. (42) elaborated a classification centred on a triad (site, nature, and root process pattern) with four clinical RR known as IRR, ERR, combined internal and ERR (for the first time this entity is titled), and transient apical breakdown (TAB). TAB indicates a temporary phenomenon detected radiologically in which the root apex apparently reveals resorption as a consequence of certain traumatic injuries. In TAB, the damaged mineralized tissue undergoes a spontaneous reparation process with no perpetual damage to the pulp (42), which was first described by Frances Andreasen in 1986 (44). For other authors, TAB is a transitory process that occurs in the apex area in which there is some evidence of aetiological features (occlusion trauma and orthodontic treatment) followed by mild apical resorption or apical pulp obliteration (14, 16).
Gunraj et al., in the same year and based on the same aspects as Ne et al. (42) (localization and type), developed an alternative RR classification, giving emphasis to ERR (based on trauma, pulp necrosis, and pressures applied to PDL), IRR, and cervical RR (CRR) (41).
Patel and Pitt-Ford attested the existence of several methods to categorize RR, elaborating their classification centred on resorption localization with a main focus on ERR and IRR with an undeniable inflammatory pathophysiology (45).
In 2003, Fuss et al. covered five clinical features of RR based on aetiology: RR from pulpal infection, periodontal infection, orthodontic pressure, impacted tooth or tumour pressure, and ankylotic RR (13). Three years later, centred also on aetiology, Lindskog et al. classified RR into three groups: induced by trauma, infection, and hyperplasic invasive RR (46). Lindskog and collaborators introduced the term transient apical internal resorption to indicate a noninfectious, self-limited IRR subtype caused by a trauma episode (luxation). This clinical scenario was also described by Andreasen (47) and was considered a positive response initiated by the tooth’s own vascular system functions of internal pulp repair, and its pathophysiology has been linked to TAB (an ERR type) (48).
Investigators (49) developed an RR classification composed of five independent groups (external, surface, replacement, inflammatory, and atypical) based on aetiology. Santos research group classified ERR specifically after trauma based on a literature review, and for each category, they indicated a set of clinical, histological, and radiographic characteristics to fulfil. Furthermore, they introduced the atypical RR concept as an ERR subcategory frequently diagnosed in the primary teeth of young asymptomatic patients undergoing follow-up appointments for dental trauma (49).
Kanas and Kanas, unlike previous classifications, distinguished RR from dental and nondental origin due to traumatic, pressure, or idiopathic factors and elaborated the most complete etiologic and morphologic RR classification in permanent teeth based on localization, aetiology, and RR type. From nondental origin, Kanas and Kanas indicated an ERR from systemic disorders and neoplasia/cysts from the jaws and IRR from Herpes zoster infection (a controversial subject minimally discussed in the literature), as this nontypical RR pattern is near the cervical area and involves the pulp, with extension to the PDL, which challenges the differential diagnosis between internal and external. Consequently, Kanas and Kanas included it under the IRR group, because the recommended therapy is endodontic treatment (11).
From dental origin, the nomenclature varies from previous classification systems. The terms external surface resorption (ESR) and transient apical resorption (TAR) designate the natural physiologic root response of permanent teeth, preferring the term physiologic apical resorption. An ERR distinct pattern, periapical replacement RR (PaRRR) is portrayed by the replacement of the resorbing root with normal-appearing trabeculae bone. This process has also been referred as external apical replacement resorption, and for this entity, Kanas and Kanas preferred the term PaRRR (11).
Kanas and Kanas (11) considered a Mummery pink tooth a radial pulp enlargement resorption (internal subtype), and if the resorption becomes larger (progressive), it will eventually perforate the lateral root wall and may appear similar to CRR. However, this clinical dilemma must be solved since IRR appears to be a well-defined radiolucency of the root canal space in contrast to an ill-defined radiolucency of the canal space in CRR. For this, the radiographic MBD rule may be employed, whereby two radiographs are taken (one perpendicular to the root and the other at a mesial angle), and the authors’ conclusion is clear: IRR will not shift no matter how severe an angle at which the radiograph is taken, whereas CRR will shift from its overlaid position over the root canal space and usually extend to the root surface (11).
In 2013, Darcey and Qualtrough reported an RR classification with five independent RR entities, four of which were due to ERR with differential diagnosis among surface, inflammatory, and replacement. In opposition, IRR had similar features inside this category, although cervical exclusively fits in externals (9). The last RR classification, from Sak et al. (3), assembles all resorptions into two categories of IRR and ERR. Internal RR might present inflammatory (types A, B, C, and D) or replacement resorption, and ERR is subdivided into six categories from dental origin and nondental origin (ankylosis and replacement RR, apical inflammatory RR, resorption associated with systemic diseases, lateral inflammatory RR, resorption caused by chronic mechanical injuries, and cervical RR) (3). From the 15 RR classifications intensely analysed, we observed a chronological taxonomy discrepancy in order to quote the RR pathophysiological entities accordingly with the histological diagnostic techniques in progress. For example, ESR first defined by Andreasen does not suffer changes in physiopathology over the time; however, the terminology has undergone variations, such as ERR of type 1, attachment damage alone categorized by Martin Trope (2). Ne et al. confirmed that ESR is a physiological process that affects almost all teeth in diverse degrees (42), as a transient inflammatory resorption, since it can occur both on the external surface of the root (40), and as transient RR (4) and TAR as Kanas and Kanas associated ESR to the term of apical physiological resorption related to the root surface’s response to masticatory system pressure on the teeth (11). Attention should be given to potential confusions for the misperception of ESR with transient apical internal resorption caused by trauma, as cited by Lindskog et al. (12, 43).
ESR is repetitively followed by ankyloses, and some authors, based on these chronological events, include ankylosis as an ERR subcategory designation (4, 10, 16). This is advocated by Ne and co-workers as ankylosis is a direct union between the tooth and bone with no intervening connective tissue (42). Ankylosis follows ESR with extensive necrosis of the PDL (especially in avulsion cases) and bone formation on the denuded root surface area (42). It differs from ERRR, as ankylosis does not have inflamed connective tissue intervention.
Fuss et al. settled ankylotic RR as an entity by itself, associated with an extended root surface injury in which healing mechanisms with cementum are not possible and the bone comes into contact with the root surface with no intermediate attachment, as a result of severe traumatic injuries (intrusive luxation or avulsion with extended dry time). The resorption process might be reversed if less than 20% of the root surface is involved (13). However, if the root surface area is ≥20%, the ankylosed tooth is definitely embedded in the alveolar bone as a result of direct bone attachment to the dentine (2, 10).
In the Andreasen RR classification (1), there is no mention of CRR first categorized in 1975 by Makkes and Velzen as an inflammatory resorption group subtype with an insidious process in which the root pulp may be either vital (odontoblasts inhibiting resorption) or nonvital. Those authors indicated that CRR starts in a small cavity below the gingival margin and spreads from the small cavity to involve a variable volume of dentine, and the gingival tissue might be inflamed (50). Tronstad (40) introduced the CRR inside ERR group, often misdiagnosed as IRR, as a not well-recognized progressive external inflammatory RR type, subsequent to an injury to the cervical attachment apparatus of the root surface (precementum) and below the epithelial attachment or more apical at the root surface where damage to the PDL or cementum has occurred. The damaged root surface area is colonized by hard-tissue–resorbing cells and remains transient (the cementum reparation occurs within 2-3 weeks with no treatment necessary). Longer stimulation periods may provide bacterial products inside cervical dentinal tubules from the gingival sulcus, and the dental surface resorption process reaches the supragingival crown area. Furthermore, the vascularized granulation tissue may be visible through the enamel with a so-called pink spot or pink tooth (40), as former authors have also considered CRR as a subtype of ERR (4, 11, 14, 16).
Gunraj et al. (41) and Darcey and Qualtrough (9) considered CRR an independent entity that might result from orthodontic movement, complication after traumatic injury, internal bleaching, periodontal treatment, or orthognathic or dentoalveolar surgery; in some cases, the aetiology is obscure and is referred to as idiopathic (2, 17). Trope identified CRR as a subattachment RR of sulcular origin, as it mostly occurs below the epithelial attachment (but not exclusively) at the cervical area (2). In 2002, Trope named it sulcular infection RR (4).
CRR has several aetiological factors that may induce this resorption, and in 2004, Geoffrey Heithersay developed a CRR classification (also described as extracanalar invasive RR, subepithelial ERR, hyperplastic dental RR, or sulcular infection RR), cataloguing CRR as an uncommon form of ERR. This classification has been a source of interest and academic debate, with four subtypes distributed in classes according to the lesion extent within the tooth: class 1, small invasive resorptive lesion near the cervical area with shallow penetration into dentine; class 2, well-defined invasive resorptive lesion that penetrates close to the coronal pulp chamber but shows little (or no extension) into the radicular dentine; class 3, deeper invasion of dentine by resorbing tissue, not only involving the coronal dentine but also extending into the coronal third of the root; and class 4, a large invasive resorptive process that has extended beyond the coronal third of the root (10).
External inflammatory RR (EIRR), initially described by Andreasen (1), is the most common external resorption type with several uncertainties throughout all of its classifications. It is classically described as a resorptive lesion occurring after a trauma (or periodontal infection or orthodontic treatment) that initiates an inflammatory response within the PDL and leads to a characterized deep, bowl-shaped resorptive defect that penetrates dentine and root cementum. It can occur over any part of the root, and it is frequently named according to the area where it occurs (42).
Some authors denoted EIRR cases with intact or affected cement and necrotic pulp (5, 13, 46), and as consequence, apical periodontitis is mentioned as an independent entity (9, 15, 17) or included in the same RR category as the original Andreasen classification (1, 2, 4, 10, 11, 14, 16). If the pulp is vital, the canal is free of microorganisms, and thus, ESRR will occur instead of EIRR, unrelated to the cavity depth (51).
In 1986, Feiglin defined apical inflammatory RR (AIRR) as exclusively dependent upon the nonvital pulp presence. which occurs in the apical tooth region. Endodontic therapy is the treatment of choice, but if a thin vestige of root canal is visible, endodontic surgery must be also an option. As described, AIRR may also occur in avulsion cases, when PDL and cementum are removed by the resorption process, exposing dentinal tubules with a direct communication between necrotic pulp tissue and PDL. This results in diffusion of products from the pulp via dentinal tubules that might induce and sustain periodontium inflammation (43).
Kanas and Kanas used the same term, AIRR, whereas cervical inflammatory root resorption has been associated with bacterial extension into the PDL near the cervical one-third of the root. According to these researchers, AIRR is analogous to EIRR, inflammatory RR, periapical inflammation RR, and apical inflammatory RR, which are used to describe this common form of ERR (11).
The new classification diagram attempts to help the clinician establish correlations among the RR concepts to accomplish the most accurate diagnosis. It also provides specific guidelines supporting the best treatment option to be applied. Subsequently, a new clinical aid proposal has been constructed to be used and validated in the clinical area for routine assessment, highlighting the key role of bioceramic-based endodontic sealers that might improve the final prognosis.
CONCLUSION
The main purpose of the present narrative review was to collect and synthetize all information from 15 RR classifications constructed based on multiple causes. In this regard, aetiology is the most common feature used to elaborate a classification. In addition, taxonomy variations were accessed to evaluate whether different terms used by different authors were unique or described similar clinical entities, since ambiguous terms have been used for the same root resorptive lesion, leading to misinterpretation, especially in the clinical field. Furthermore, the most prevalent terms found were ERR, IRR, and CRR. Despite numerous terminologies, with the evolution of diagnosis techniques such as advanced medical imaging procedures and molecular approaches, as well as the current progress of laboratorial and histological techniques, there has been a well-defined progression on more complex RR classifications with several additional RR subtypes. Based on this, the present review endorses a table summary in which it is possible to compare and analyse terms used to classify several RR entities from 1970 to 2016. Furthermore, a new classification diagram with synthetized RR information based on clinical and aetiological features is described that can be easily consulted by the clinician to provide guidance for a clear and rapid diagnosis and subsequent implementation of the proper treatment decision.
Footnotes
Disclosures
Conflict of interest: No conflict of interest was declared by the authors.
Ethics Committee Approval: This paper is a review, not applied.
Peer-review: Externally peer-reviewed.
Financial Disclosure: The authors declared that this study has received no financial support.
Authorship contributions: Concept – J.M.S., P.D.; Design – J.M.S., P.D.; Supervision – J.M.S., P.D.; Materials – Not applied; Data collection &/or processing – P.D., H.A.; Analysis and/or interpretation – H.A., P.D., J.M.S.; Literature search – H.A., P.D., J.M.S.; Writing – H.A., P.D., J.M.S.; Critical review – P.D., J.M.S.
REFERENCES
- 1.Andreasen JO. Luxation of permanent teeth due to trauma A clinical and radiographic follow-up study of 189 injured teeth. Scand J Dent Res. 1970;78(3):273–86. doi: 10.1111/j.1600-0722.1970.tb02074.x. [DOI] [PubMed] [Google Scholar]
- 2.Trope M. Root resorption of dental and traumatic origin:classification based on etiology. Pract Periodontics Aesthet Dent. 1998;10(4):515–22. [PubMed] [Google Scholar]
- 3.Sak M, Radecka M, Karpiński T, Wędrychowicz-Welman A, Szkaradkiewicz A. Tooth root resorption:etiopathogenesis and classification. MicroMedicine. 2016;4(1):21–31. [Google Scholar]
- 4.Trope M. Root Resorption due to dental trauma. Endodontic Topics. 2002;1(1):79–100. [Google Scholar]
- 5.Patel S, Saberi N. The ins and outs of root resorption. Br Dent J. 2018;224(9):691–699. doi: 10.1038/sj.bdj.2018.352. [DOI] [PubMed] [Google Scholar]
- 6.Patel S, Ricucci D, Durak C, Tay F. Internal root resorption:a review. J Endod. 2010;36(7):1107–21. doi: 10.1016/j.joen.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 7.Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals:secrets of the trade. J Chiropr Med. 2006;5(3):101–17. doi: 10.1016/S0899-3467(07)60142-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gartner AH, Mack T, Somerlott RG, Walsh LC. Differential diagnosis of internal and external root resorption. J Endod. 1976;2(11):329–34. doi: 10.1016/S0099-2399(76)80071-4. [DOI] [PubMed] [Google Scholar]
- 9.Darcey J, Qualtrough A. Resorption:part 1 Pathology, classification and aetiology. Br Dent J. 2013;214(9):439–51. doi: 10.1038/sj.bdj.2013.431. [DOI] [PubMed] [Google Scholar]
- 10.Heithersay GS. Invasive cervical resorption. Endodontic Topics. 2004;7(1):73–92. [Google Scholar]
- 11.Kanas RJ, Kanas SJ. Dental root resorption:a review of the literature and a proposed new classification. Compend Contin Educ Dent. 2011;32(3):38–52. [PubMed] [Google Scholar]
- 12.da Silveira HL, Silveira HE, Liedke GS, Lermen CA, Dos Santos RB, de Figueiredo JA. Diagnostic ability of computed tomography to evaluate external root resorption in vitro. Dentomaxillofac Radiol. 2007;36(7):393–6. doi: 10.1259/dmfr/13347073. [DOI] [PubMed] [Google Scholar]
- 13.Fuss Z, Tsesis I, Lin S. Root resorption--diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003;19(4):175–82. doi: 10.1034/j.1600-9657.2003.00192.x. [DOI] [PubMed] [Google Scholar]
- 14.Nance RS, Tyndall D, Levin LG, Trope M. Diagnosis of external root resorption using TACT (tuned-aperture computed tomography) Endod Dent Traumatol. 2000;16(1):24–8. doi: 10.1034/j.1600-9657.2000.016001024.x. [DOI] [PubMed] [Google Scholar]
- 15.Thomas P, Krishna Pillai R, Pushparajan Ramakrishnan B, Palani J. An insight into internal resorption. ISRN Dent 2014. 2014:759326. doi: 10.1155/2014/759326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silveira FF, Nunes E, Soares JA, Ferreira CL, Rotstein I. Double 'pink tooth'associated with extensive internal root resorption after orthodontic treatment:a case report. Dent Traumatol. 2009;25(3):43–7. doi: 10.1111/j.1600-9657.2008.00755.x. [DOI] [PubMed] [Google Scholar]
- 17.Darcey J, Qualtrough A. Resorption:part 2 Diagnosis and management. Br Dent J. 2013;214(10):493–509. doi: 10.1038/sj.bdj.2013.482. [DOI] [PubMed] [Google Scholar]
- 18.Bergmans L, Van Cleynenbreugel J, Verbeken E, Wevers M, Van Meerbeek B, Lambrechts P. Cervical external root resorption in vital teeth. J Clin Periodontol. 2002;29(6):580–5. doi: 10.1034/j.1600-051x.2002.290615.x. [DOI] [PubMed] [Google Scholar]
- 19.Dudic A, Giannopoulou C, Leuzinger M, Kiliaridis S. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2009;135(4):434–7. doi: 10.1016/j.ajodo.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Laux M, Abbott PV, Pajarola G, Nair PN. Apical inflammatory root resorption:a correlative radiographic and histological assessment. Int Endod J. 2000;33(6):483–93. doi: 10.1046/j.1365-2591.2000.00338.x. [DOI] [PubMed] [Google Scholar]
- 21.Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J. 2007;40(10):818–30. doi: 10.1111/j.1365-2591.2007.01299.x. [DOI] [PubMed] [Google Scholar]
- 22.Cohenca N, Simon JH, Mathur A, Malfaz JM. Clinical indications for digital imaging in dento-alveolar trauma. Part 2:root resorption. Dent Traumatol. 2007;23(2):105–13. doi: 10.1111/j.1600-9657.2006.00546.x. [DOI] [PubMed] [Google Scholar]
- 23.Hahn W, Fricke-Zech S, Fricke J, Gruber RM, Dullin C, Zapf A, et al. Detection and size differentiation of simulated tooth root defects using flat-panel volume computerized tomography (fpVCT) Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(2):272–8. doi: 10.1016/j.tripleo.2008.04.030. [DOI] [PubMed] [Google Scholar]
- 24.Ludlow J. Dosimetry of the Kodak 9000 3D Small FOV CBCT and Panoramic Unit. Oral Surg, Oral Med, Oral Pathol, Oral Radiol Endod. 2009;107(4):29. [Google Scholar]
- 25.Liu DG, Zhang WL, Zhang ZY, Wu YT, Ma XC. Localization of impacted maxillary canines and observation of adjacent incisor resorption with cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105(1):91–8. doi: 10.1016/j.tripleo.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 26.Jaju PP, Jaju SP. Clinical utility of dental cone-beam computed tomography:current perspectives. Clin Cosmet Investig Dent. 2014;6:29–43. doi: 10.2147/CCIDE.S41621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.European Society of Endodontology. Patel S, Durack C, Abella F, Roig M, Shemesh H, et al. European Society of Endodontology position statement:the use of CBCT in endodontics. Int Endod J. 2014;47(6):502–4. doi: 10.1111/iej.12267. [DOI] [PubMed] [Google Scholar]
- 28.Tyrovola JB, Spyropoulos MN, Makou M, Perrea D. Root resorption and the OPG/RANKL/RANK system:a mini review. J Oral Sci. 2008;50(4):367–76. doi: 10.2334/josnusd.50.367. [DOI] [PubMed] [Google Scholar]
- 29.Terpos E, Szydlo R, Apperley JF, Hatjiharissi E, Politou M, Meletis J, et al. Soluble receptor activator of nuclear factor kappaB ligand-osteoprotegerin ratio predicts survival in multiple myeloma:proposal for a novel prognostic index. Blood. 2003;102(3):1064–9. doi: 10.1182/blood-2003-02-0380. [DOI] [PubMed] [Google Scholar]
- 30.Kamat M, Puranik R, Vanaki S, Kamat S. An insight into the regulatory mechanisms of cells involved in resorption of dental hard tissues. J Oral Maxillofac Pathol. 2013;17(2):228–33. doi: 10.4103/0973-029X.119736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Theoleyre S, Wittrant Y, Tat SK, Fortun Y, Redini F, Heymann D. The molecular triad OPG/RANK/RANKL:involvement in the orchestration of pathophysiological bone remodeling. Cytokine Growth Factor Rev. 2004;15(6):457–75. doi: 10.1016/j.cytogfr.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 32.Väänänen HK, Zhao H, Mulari M, Halleen JM. The cell biology of osteoclast function. J Cell Sci. 2000;113(Pt 3):377–81. doi: 10.1242/jcs.113.3.377. [DOI] [PubMed] [Google Scholar]
- 33.Khosla S. Minireview:the OPG/RANKL/RANK system. Endocrinology. 2001;142(12):5050–5. doi: 10.1210/endo.142.12.8536. [DOI] [PubMed] [Google Scholar]
- 34.Capparelli C, Morony S, Warmington K, Adamu S, Lacey D, Dunstan CR, et al. Sustained antiresorptive effects after a single treatment with human recombinant osteoprotegerin (OPG):a pharmacodynamic and pharmacokinetic analysis in rats. J Bone Miner Res. 2003;18(5):852–8. doi: 10.1359/jbmr.2003.18.5.852. [DOI] [PubMed] [Google Scholar]
- 35.Li D, Gromov K, Proulx ST, Xie C, Li J, Crane DP, et al. Effects of antiresorptive agents on osteomyelitis:novel insights into the pathogenesis of osteonecrosis of the jaw. Ann N Y Acad Sci. 2010;1192:84–94. doi: 10.1111/j.1749-6632.2009.05210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ahangari Z, Nasser M, Mahdian M, Fedorowicz Z, Marchesan MA. Interventions for the management of external root resorption. Cochrane Database Syst Rev. 2015;11:CD008003. doi: 10.1002/14651858.CD008003.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Richardson I. The calcium silicate hydrates. Cement and Concrete Research. 2008;38(2):137–58. [Google Scholar]
- 38.Trope M, Bunes A, Debelian G. Root filling materials and techniques:bioceramics a new hope? Endod Top. 2015;32(1):86–96. [Google Scholar]
- 39.Dudeja C, Taneja S, Kumari M, Singh N. An in vitro comparison of effect on fracture strength, pH and calcium ion diffusion from various biomimetic materials when used for repair of simulated root resorption defects. J Conserv Dent. 2015;18(4):279–83. doi: 10.4103/0972-0707.159720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tronstad L. Root resorption--etiology, terminology and clinical manifestations. Endod Dent Traumatol. 1988;4(6):241–52. doi: 10.1111/j.1600-9657.1988.tb00642.x. [DOI] [PubMed] [Google Scholar]
- 41.Gunraj MN. Dental root resorption. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(6):647–53. doi: 10.1016/s1079-2104(99)70002-8. [DOI] [PubMed] [Google Scholar]
- 42.Ne RF, Witherspoon DE, Gutmann JL. Tooth resorption. Quintessence Int. 1999;30(1):9–25. [PubMed] [Google Scholar]
- 43.Feiglin B. Root resorption. Aust Dent J. 1986;31(1):12–22. doi: 10.1111/j.1834-7819.1986.tb02978.x. [DOI] [PubMed] [Google Scholar]
- 44.Andreasen FM. Transient apical breakdown and its relation to color and sensibility changes after luxation injuriesto teeth. Endod Dent Traumatol. 1986;2(1):9–19. doi: 10.1111/j.1600-9657.1986.tb00118.x. [DOI] [PubMed] [Google Scholar]
- 45.Patel S, Ford TP. Is the resorption external or internal? Dent Update. 2007;34(4):218–20. doi: 10.12968/denu.2007.34.4.218. 222, 224-6, 229. [DOI] [PubMed] [Google Scholar]
- 46.Lindskog S, Heithersay G, Pierce A Dental resorptions. Scandinavian Yearbook of Dentistry. Blackwell Munksgaard; 2006. pp. 1–22. [Google Scholar]
- 47.Heithersay GS. Management of tooth resorption. Aust Dent J. 2007;52(1 Suppl):S105–21. doi: 10.1111/j.1834-7819.2007.tb00519.x. [DOI] [PubMed] [Google Scholar]
- 48.Andreasen FM. Transient root resorption after dental trauma:the clinician's dilemma. J Esthet Restor Dent. 2003;15(2):80–92. doi: 10.1111/j.1708-8240.2003.tb00322.x. [DOI] [PubMed] [Google Scholar]
- 49.Santos B, Mendonça D, Sousa D, Neto J, Araújo R. Root resorption after dental traumas:classification and clinical, radiographic and histologic aspects. RSBO. 2011;8(4):439–45. [Google Scholar]
- 50.Makkes PC, Thoden van Velzen SK. Cervical external root resorption. J Dent. 1975;3(5):217–22. doi: 10.1016/0300-5712(75)90126-8. [DOI] [PubMed] [Google Scholar]
- 51.Finucane D, Kinirons MJ. External inflammatory and replacement resorption of luxated, and avulsed replanted permanent incisors:a review and case presentation. Dent Traumatol. 2003;19(3):170–4. doi: 10.1034/j.1600-9657.2003.00154.x. [DOI] [PubMed] [Google Scholar]