Abstract
Background
We aimed to investigate the associations of critical care provided in a cardiac surgical intensive care unit (CSICU) staffed by an attending intensivist with improvements in intensive care unit (ICU) quality and reductions in postoperative complications.
Methods
Patients who underwent elective isolated coronary artery bypass grafting (CABG) between January 2007 and December 2012 (the control group) were propensity-matched (1:1) to CABG patients between January 2013 and June 2018 (the intensivist group).
Results
Using propensity score matching, 302 patients were extracted from each group. The proportion of patients with at least 1 postoperative complication was significantly lower in the intensivist group than in the control group (17.2% vs. 28.5%, p=0.001). In the intensivist group, the duration of mechanical ventilation (6.4±13.7 hours vs. 13.7±49.3 hours, p=0.013) and length of ICU stay (28.7±33.9 hours vs. 41.7±90.4 hours, p=0.018) were significantly shorter than in the control group. The proportions of patients with prolonged mechanical ventilation (2.3% vs. 7.6%, p=0.006), delirium (1.3% vs. 6.3%, p=0.003) and acute kidney injury (1.3% vs. 5.3%, p=0.012) were significantly lower in the intensivist group than in the control group.
Conclusion
A transition from an open ICU model with trainee coverage to a closed ICU model with attending intensivist coverage can be expected to yield improvements in CSICU quality and reductions in postoperative complications.
Keywords: Intensivist, Critical care, Intensive care unit staffing, Coronary artery bypass grafting, Postoperative complications
Introduction
Cardiac surgical intensive care units (CSICUs) have commonly been established with an open intensive care unit (ICU) model. In this model, the most responsible physicians are cardiac surgeons who are not always available to immediately manage postoperative patients in the ICU. In the closed model, in contrast, intensivists are responsible for the care of patients and almost always remain in the ICU during working hours to manage patients in a prompt manner. Although several studies have demonstrated that the closed ICU model could improve clinical outcomes relative to the open ICU model [1–5], fewer reports have evaluated the effectiveness of the closed model in CSICUs [6–8]. At Seoul National University Bundang Hospital, in 2013, a transition took place from an open ICU model with trainee coverage to a closed ICU model with attending intensivist coverage. An intensivist who was board-certified in cardiothoracic surgery and critical care remained in the CSICU during daytime hours and promptly made independent decisions on most medical issues, but communicated with cardiac surgeons about critical surgical decisions, such as re-exploration. The hypothesis of our study was that critical care provided by an attending intensivist who was board-certified in cardiothoracic surgery would be associated with improvements in CSICU quality and reductions in postoperative complications.
Methods
Study population and outcomes measured
We retrospectively reviewed the electronic medical records of all patients who were admitted to the CSICU after undergoing coronary artery bypass grafting (CABG) between January 2007 and June 2018 (n=1,521). Although there were several changes of staffing in the Department of Thoracic and Cardiovascular Surgery during that period, we included only patients who underwent surgery performed by 2 cardiac surgeons (surgeons A and B), who worked at our institution throughout the entire study period (n=1,284). These 2 cardiac surgeons already had more than 10 years of surgical experience in 2007. We excluded cases of CABG with any type of concomitant cardiovascular surgery, such as valvular, aortic, and peripheral vascular surgery (n=238). We also excluded urgent or emergent cases of isolated CABG (n=249). The remaining 797 patients who underwent elective isolated CABG were included in the final analysis. These patients were divided into 2 groups according to the presence of an attending intensivist. At our institution in 2013, a transition took place from an open ICU model with trainee coverage to a closed ICU model with attending intensivist coverage. From January 2007 to December 2012, management of CSICU patients undergoing open cardiac surgery was provided by a resident or fellow with back-up from the cardiac surgeon who had operated on each patient (control group, n=369). From January 2013 to June 2018, patients who were admitted to the CSICU after undergoing open cardiac surgery were managed by a single intensivist who was board-certified in cardiothoracic surgery and critical care (intensivist group, n=428). Starting in January 2013, the intensivist provided critical care for CSICU patients during daytime hours (08:00–18:00, Monday to Friday, except for holidays). Overnight coverage (18:00–08:00) was provided by an on-duty resident or fellow with back-up from the intensivist providing home-call consultation. The intensivist remained in the CSICU during the daytime hours and served as the primary decision-maker for all aspects of patient care. The intensivist made independent decisions on most medical issues, but communicated with cardiac surgeons about critical surgical decisions, such as re-exploration. We investigated whether the ICU quality improved and the incidence of common postoperative complications decreased due to the presence of an attending intensivist in the CSICU. The primary outcome was a composite of postoperative complications, including indicators reflecting the quality of ICU care. These included prolonged mechanical ventilation for more than 24 hours, re-intubation within 48 hours after extubation, a prolonged ICU stay for more than 72 hours, ICU re-admission within 48 hours after discharge, re-exploration for postoperative bleeding, cardiac arrest, deep sternal wound infection, ventilator-associated pneumonia (VAP), delirium, stroke, acute kidney injury (AKI), the use of intermittent dialysis or continuous renal replacement therapy (RRT), a prolonged hospital stay for more than 14 days, and 30-day mortality. The secondary outcomes were the duration of mechanical ventilation, the length of ICU and hospital stay, the rate of early extubation within 6 hours, and the percentage of patients with 2 or more complications. This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB approval no., B-1910-568-106).
Statistical analysis
Continuous variables were expressed as mean±standard deviation. Categorical variables were expressed as number (%). Statistical comparisons between the 2 unmatched groups were made via the Student t-test for continuous variables and the chi-square test for categorical variables. To overcome the differences in baseline characteristics between the 2 groups, a propensity score for group assignment was calculated. One-to-one propensity score matching was performed. The following underlying characteristics were used to calculate the propensity score: age, sex, height, body weight, body mass index, European System for Cardiac Operative Risk Evaluation (EuroSCORE) II, EuroSCORE II ≥5, diabetes mellitus, hypertension, dyslipidemia, history of stroke, chronic renal failure, peripheral vascular disease, chronic obstructive pulmonary disease, left ventricular dysfunction (left ventricular ejection fraction <40%), the operating surgeon, off-pump CABG (OPCAB), use of a saphenous vein graft, number of anastomoses, and operating time. The p-value of the Hosmer-Lemeshow test and the c-statistic of the propensity score model, which reflected its calibration and discriminatory power, were 0.56 and 0.69, respectively. Differences in the baseline characteristics between the 2 groups were calculated before and after propensity score matching to evaluate the balance among covariates. Covariates with a standardized mean difference (SMD) less than 0.15 were considered acceptable. The SMDs of all covariates are shown in Table 1. To compare categorical and continuous variables between the 2 matched groups, the McNemar test and the Wilcoxon signed-rank test were used. Associations between the presence of an intensivist and clinical outcomes were presented as odds ratios (ORs) and 95% confidence intervals (CIs). IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis, and p-values <0.05 were considered to indicate statistical significance.
Table 1.
Demographic and clinical characteristics of patients before and after propensity score matching
| Characteristic | All patients | Matched patients | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Control group (n=369) | Intensivist group (n=428) | SMD | p-value | Control group (n=302) | Intensivist group (n=302) | SMD | p-value | |
| Age (yr) | 66.4±9.1 | 66.5±10.5 | 0.016 | 0.809 | 66.6±9.0 | 66.4±10.5 | −0.025 | 0.742 |
|
| ||||||||
| Male | 278 (75.3) | 319 (74.5) | −0.018 | 0.794 | 223 (73.8) | 226 (74.8) | 0.023 | 0.780 |
|
| ||||||||
| Height (cm) | 162.7±7.9 | 162.8±8.6 | 0.019 | 0.780 | 162.6±8.2 | 162.9±8.7 | 0.027 | 0.739 |
|
| ||||||||
| Body weight (kg) | 65.1±10.3 | 64.9±11.3 | −0.017 | 0.802 | 64.9±10.5 | 65.7±11.7 | 0.072 | 0.359 |
|
| ||||||||
| Body mass index (kg/m2) | 24.5±2.9 | 24.3±3.4 | −0.057 | 0.392 | 24.4±2.9 | 24.7±3.3 | 0.083 | 0.265 |
|
| ||||||||
| EuroSCORE II | 1.7±1.3 | 2.0±2.2 | 0.110 | 0.055 | 1.8±1.3 | 1.9±2.2 | 0.064 | 0.338 |
|
| ||||||||
| EuroSCORE II ≥5 | 14 (3.8) | 31 (7.2) | 0.133 | 0.035 | 13 (4.3) | 20 (6.6) | 0.089 | 0.210 |
|
| ||||||||
| Diabetes | 187 (50.7) | 243 (56.8) | 0.123 | 0.085 | 158 (52.3) | 163 (54.0) | 0.033 | 0.683 |
|
| ||||||||
| Hypertension | 279 (75.6) | 312 (72.9) | −0.061 | 0.383 | 226 (74.8) | 227 (75.2) | 0.007 | 0.925 |
|
| ||||||||
| Dyslipidemia | 163 (44.2) | 193 (45.1) | 0.018 | 0.794 | 130 (43.0) | 125 (41.4) | −0.033 | 0.680 |
|
| ||||||||
| History of stroke | 77 (20.9) | 86 (20.1) | −0.019 | 0.787 | 66 (21.9) | 66 (21.9) | 0.000 | 1.000 |
|
| ||||||||
| Chronic renal failure | 41 (11.1) | 60 (14.0) | 0.084 | 0.219 | 34 (11.3) | 41 (13.6) | 0.067 | 0.388 |
|
| ||||||||
| Peripheral vascular disease | 61 (16.5) | 88 (20.6) | 0.100 | 0.146 | 55 (18.2) | 52 (17.2) | −0.025 | 0.749 |
|
| ||||||||
| Chronic obstructive pulmonary disease | 22 (6.0) | 40 (9.3) | 0.116 | 0.075 | 21 (7.0) | 24 (7.9) | 0.034 | 0.642 |
|
| ||||||||
| Left ventricle dysfunction | 47 (12.7) | 66 (15.4) | 0.074 | 0.279 | 42 (13.9) | 49 (16.2) | 0.064 | 0.426 |
|
| ||||||||
| Surgeon A | 243 (65.9) | 183 (42.8) | −0.466 | <0.001 | 177 (58.6) | 168 (55.6) | −0.060 | 0.459 |
|
| ||||||||
| Off pump coronary artery bypass grafting | 273 (74.0) | 350 (81.8) | 0.202 | 0.008 | 238 (78.8) | 238 (78.8) | 0.000 | 1.000 |
|
| ||||||||
| Use of saphenous vein graft | 69 (18.7) | 81 (18.9) | 0.006 | 0.935 | 49 (16.2) | 61 (20.2) | 0.101 | 0.206 |
|
| ||||||||
| No. of anastomoses | 3.5±1.1 | 3.0±1.1 | −0.474 | <0.001 | 3.3±1.1 | 3.2±1.1 | −0.102 | 0.190 |
|
| ||||||||
| Operating time (min) | 269.0±57.8 | 255.5±65.4 | −0.206 | 0.002 | 263.2±56.8 | 261.8±62.1 | −0.021 | 0.781 |
Values are presented as mean±standard deviation or number (%).
EuroSCORE; European System for Cardiac Operative Risk Evaluation; SMD, standardized mean difference.
Results
The propensity score matching analysis extracted 302 patients from each group. Because the SMDs of all covariates after matching were less than 0.15, we considered them to be acceptable. Before propensity score matching, some significant differences were observed in clinical characteristics between the 2 groups. The proportion of high-risk patients with a EuroSCORE II ≥5 in the intensivist group was higher than that in the control group (7.2% versus 3.8%, p=0.035). In the control group, more patients underwent surgery performed by surgeon A than in the intensivist group (65.9% versus 42.8%, p<0.001). The intensivist group showed a higher percentage of OPCAB (81.8% versus 74.0%, p=0.008), fewer anastomoses (3.0±1.1 versus 3.5±1.1, p<0.001), and a shorter operating time (255.5±65.4 minutes versus 269.0±57.8 minutes, p=0.002) than the control group. After propensity score-matching, the demographic and clinical characteristics of the patients were evenly distributed between the 2 matched groups (Table 1).
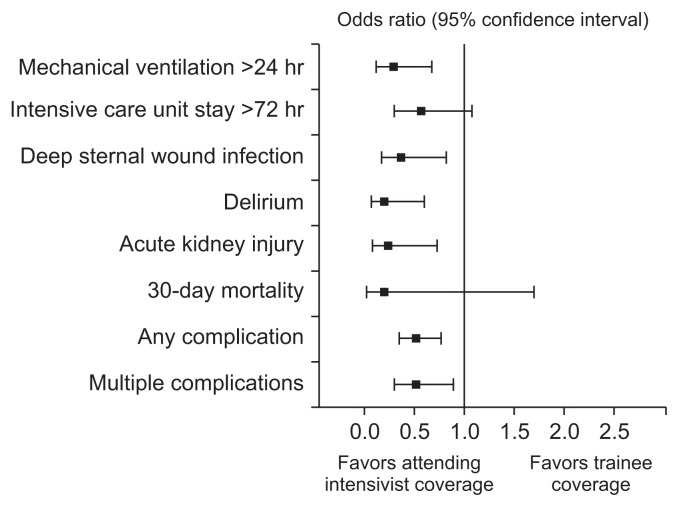
The primary outcome was a composite of postoperative complications. The proportion of patients with at least 1 postoperative complication was significantly lower in the intensivist group than in the control group (17.2% versus 28.5%; OR, 0.52; 95% CI, 0.30–0.77; p=0.001). The percentage of patients who had 2 or more complications was also significantly lower in the intensivist group than in the control group (7.3% versus 13.2%; OR, 0.52; 95% CI, 0.30–0.89; p=0.014). The average duration of mechanical ventilation was significantly shorter in the intensivist group than in the control group (6.4±13.7 hours versus 13.7±49.3 hours, p= 0.013). The proportion of patients who underwent mechanical ventilation for more than 24 hours was significantly lower in the intensivist group than in the control group (2.3% versus7.6%; OR, 0.29; 95% CI, 0.12–0.68, p=0.006). In the intensivist group, significantly more patients were extubated within 6 hours (77.8% versus 58.9%; OR, 2.44; 95% CI, 1.71–3.49; p<0.001), while the percentage of patients requiring re-intubation within 48 hours was significantly lower than in the control group (0% versus 3.0%, p=0.004). The average length of ICU stay was significantly shorter in the intensivist group than in the control group (28.7±33.9 hours versus 41.7±90.4 hours, p=0.018). The proportion of patients who stayed in the ICU for more than 72 hours was higher in the control group than in the intensivist group (8.9% versus 5.3%), but this difference was not statistically significant. Although the rate of ICU re-admission within 48 hours after discharge was slightly lower in the intensivist group (0.7% versus 1.0%), this difference did not show statistical significance. There were no significant differences in the rate of re-exploration for postoperative bleeding and cardiac arrest requiring cardiopulmonary resuscitation (CPR) between the 2 matched groups. Although no patient experienced cardiac arrest due to cardiac tamponade in the intensivist group, this difference was not statistically significant when compared to the control group (0% versus 0.7%). The intensivist group had a significantly lower rate of deep sternal wound infections (3.0% versus 7.6%; OR, 0.37; 95% CI, 0.17–0.82; p=0.011) and delirium (1.3% versus 6.3%; OR, 0.20; 95% CI, 0.07–0.60; p=0.003) than the control group. Although the incidence of VAP was also lower in the intensivist group (0.7% versus 2.0%), this difference did not reach statistical significance. The incidence of stroke was also similar in both groups. Although the rate of AKI was significantly lower in the intensivist group (1.3% versus 5.3%; OR, 0.24; 95% CI, 0.08–0.73; p=0.012), no statistically significant difference was found in the proportion of patients who required RRT, such as intermittent dialysis or continuous RRT. There were no significant differences in the length of hospital stay and the rate of prolonged hospital stay for more than 14 days between the 2 matched groups. The 30-day mortality rate in the intensivist group was lower than that in the control group (0.3% versus 1.7%), but the difference was not statistically significant (Table 2, Fig. 1).
Table 2.
Comparison of clinical outcomes between control group and intensivist group after propensity score matching
| Variable | Control group | Intensivist group | p-value | Odds ratio (95% confidence interval) |
|---|---|---|---|---|
| Mechanical ventilation (hr) | 13.7±49.3 | 6.4±13.7 | 0.013 | |
| Mechanical ventilation >24 hr | 23 (7.6) | 7 (2.3) | 0.006 | 0.29 (0.12–0.68) |
| Extubation within 6 hr | 178 (58.9) | 235 (77.8) | <0.001 | 2.44 (1.71–3.49) |
| Re-intubation within 48 hr after extubation | 9 (3.0) | 0 | 0.004 | NA |
| Length of ICU stay (hr) | 41.7±90.4 | 28.7±33.9 | 0.018 | |
| ICU stay >72 hr | 27 (8.9) | 16 (5.3) | 0.091 | 0.57 (0.30–1.08) |
| ICU re-admission within 48 hr after discharge | 3 (1.0) | 2 (0.7) | 1.000 | 0.66 (0.11–4.01) |
| Re-exploration for postoperative bleeding | 4 (1.3) | 3 (1.0) | 1.000 | 0.75 (0.17–3.37) |
| Cardiac arrest | 4 (1.3) | 2 (0.7) | 0.688 | 0.50 (0.09–2.73) |
| Cardiac arrest due to cardiac tamponade | 2 (0.7) | 0 | 0.500 | NA |
| Deep sternal wound infection | 23 (7.6) | 9 (3.0) | 0.011 | 0.37 (0.17–0.82) |
| Ventilator-associated pneumonia | 6 (2.0) | 2 (0.7) | 0.289 | 0.33 (0.07–1.64) |
| Delirium | 19 (6.3) | 4 (1.3) | 0.003 | 0.20 (0.07–0.60) |
| Stroke | 5 (1.7) | 3 (1.0) | 0.727 | 0.60 (0.14–2.52) |
| Acute kidney injury | 16 (5.3) | 4 (1.3) | 0.012 | 0.24 (0.08–0.73) |
| Intermittent dialysis | 4 (1.3) | 1 (0.3) | 0.375 | 0.25 (0.03–2.23) |
| Continuous renal replacement therapy | 6 (2.0) | 1 (0.3) | 0.125 | 0.16 (0.02–1.37) |
| Length of hospital stay (day) | 10.1±15.1 | 9.5±7.0 | 0.512 | |
| Hospital stay >14 day | 34 (11.3) | 32 (10.6) | 0.896 | 0.93 (0.56–1.56) |
| 30-day mortality | 5 (1.7) | 1 (0.3) | 0.219 | 0.20 (0.02–1.70) |
| Any complication | 86 (28.5) | 52 (17.2) | 0.001 | 0.52 (0.35–0.77) |
| Multiple complications | 40 (13.2) | 22 (7.3) | 0.014 | 0.52 (0.30–0.89) |
Values are presented as mean±standard deviation or number (%).
NA, not applicable; ICU, intensive care unit.
Fig. 1.
Odds ratio plot of clinical outcomes according to trainee coverage versus attending intensivist coverage.
Discussion
The average age of patients undergoing cardiac surgery and the burden of their accompanying diseases have increased over the past 20 years [9]. With the increased preoperative risk of patients undergoing cardiac surgery, more patients experience postoperative complications, leading to prolonged ICU stays and mortality [10]. Great efforts have been made to reduce the complication rates of cardiac surgery and to improve ICU quality, and many ICUs are moving from open systems to closed systems based on the results of previous studies and critical care guidelines. Previous studies comparing the open and closed models showed that the outcomes of the closed ICU model were better than those of the open model [1–5]. The Society of Critical Care Medicine recommended the closed ICU model because it was associated with a shorter length of ICU stay, lower mortality, and improved patient safety [11]. Although the aforementioned studies did not specifically investigate CSICUs, some studies have demonstrated that attending intensivist coverage was associated with a reduction in major postoperative complications in patients who underwent cardiac surgery [6–8]. Although these results are very meaningful, it is also necessary to consider some factors that could potentially confound the association between the presence of an intensivist and improved clinical outcomes. The most important confounding factor may be the considerable heterogeneity of the patient populations analyzed in previous studies. Postoperative outcomes can vary greatly depending on the type of surgery, the urgency of the operation, and who the surgeon was. Although previous studies applied propensity score matching to overcome such heterogeneity, even with positive results, it may be difficult to fully distinguish whether these results were due to the presence of an intensivist because of the possibility of unidentified confounding factors. Therefore, we only included patients who underwent elective isolated CABG to minimize patients’ heterogeneity. The preoperative status of patients electively undergoing isolated CABG is generally expected to be similar. In this study, although the intensivist group contained a larger proportion of high-risk patients with a EuroSCORE II ≥5, we could not find any other significant differences in the preoperative demographic and clinical characteristics between the 2 unmatched groups. Moreover, we only included patients who underwent surgery performed by 2 cardiac surgeons (surgeons A and B), who worked at our institution throughout the entire study period and already had more than 10 years of surgical experience in 2007. Given that the surgical and anesthetic policies for performing CABG remained constant throughout the study period, we expected that there would be no significant difference in the operative details between the 2 unmatched groups. However, we found some significant differences in the percentage of OPCAB procedures, the number of anastomoses, and the operating time. In addition, the proportion of CABG procedures performed by surgeon A decreased over time compared to surgeon B. To overcome these differences, propensity score matching of the included patients was conducted. As a result of these processes, we expected that the differences between the 2 groups—except for the presence of an attending intensivist—would be minimized in this study compared to previous studies.
The primary outcome was a composite of postoperative complications, including indicators reflecting the quality of ICU care. With reference to the indicators identified by the European Society of Intensive Care Medicine for improving safety and quality in the ICU [12], we investigated the rate of re-intubation within 48 hours, the incidence of VAP, and the rate of ICU re-admission within 48 hours after discharge. We examined the rate of the 5 major postoperative complications defined by the Society of Thoracic Surgeons (stroke, AKI, prolonged intubation more than 24 hours, unplanned reoperation, and deep sternal wound infection). In addition, we investigated the rate of prolonged ICU and hospital stays, cardiac arrest, delirium, the use of intermittent dialysis or continuous RRT, and 30-day mortality. We compared the proportions of patients with any of the complications described above between the 2 groups. The percentage of patients with 2 or more complications was also investigated. We also investigated the rate of early extubation within 6 hours, which is used as a quality marker by the Society of Thoracic Surgeons.
Since an attending intensivist started providing critical care in the CSICU, the duration of mechanical ventilation significantly decreased by an average of more than 6 hours, and the frequency of prolonged mechanical ventilation also significantly declined. A possible explanation for this is that patients in the intensivist group were extubated earlier than those in the control group. In fact, we found that the proportion of patients who were extubated within 6 hours was significantly higher in the intensivist group. The criterion of extubation within 6 hours has been considered as an indicator of a successful fast-track ventilator weaning protocol [13]. Another significant finding was that the number of patients who required re-intubation within 48 hours after extubation was significantly lower in the intensivist group, even though the rate of early extubation was higher. This may indicate that the decision to extubate was more appropriate in the intensivist group. As the rate of early extubation increased and the duration of mechanical ventilation was shortened, we expected the incidence of VAP and delirium to decrease because both are associated with a longer mechanical ventilation time [14,15]. Although the incidence of VAP was lower in the intensivist group, as we expected, this difference did not reach statistical significance. However, we noted that the incidence of VAP was similar between the 2 unmatched groups (1.6% versus 1.4%), even though more patients at high risk (EuroSCORE II ≥5) were included in the intensivist group before propensity score matching. This means that significant differences could have been found if high-risk cases such as emergent operations, which are expected to have a high incidence of VAP, were included. The incidence of delirium in the intensivist group was significantly lower, as expected. A prolonged ICU stay, especially longer than 72 hours, in patients undergoing cardiac operations is known to be associated with higher hospital mortality and poorer long-term survival [16]. In this study, the length of ICU stay in the intensivist group was significantly lower than in the control group, by an average of more than 12 hours. Although the number of patients with an ICU stay over 72 hours was also lower, this difference did not reach statistical significance. We found that the incidence of delirium and AKI in the intensivist group was significantly lower than in the control group, as mentioned previously. These findings may be associated with the shorter duration of mechanical ventilation and length of ICU stay as a result of early extubation. These results may also have been due to immediate interventions made by the attending intensivist in response to changes in patients’ condition, which helped to achieve hemodynamic stability [17]. The attending intensivist remained in the CSICU during daytime hours and promptly made independent decisions on most medical issues as the primary decision-maker. These results could be attributed to the rapid correction of electrolyte and metabolic disturbances with appropriate fluid replacement provided by the attending intensivist [18], although further research is needed to support this hypothesis. The incidence of deep sternal wound infections was also significantly reduced, and regular rounding, active use of antibiotics, and immediate action in communication with cardiac surgeons may have contributed to this. No statistically significant difference was found in the rate of cardiac arrest. The main causes of cardiac arrest were arrhythmia and postoperative bleeding. In the control group, 2 patients had cardiac tamponade due to postoperative bleeding and they required CPR before re-exploration. However, there were no cases of cardiac arrest due to cardiac tamponade in the intensivist group. This may have been due to the early diagnosis of postoperative bleeding, before the occurrence of cardiac arrest due to cardiac tamponade. Because the attending intensivist was credentialed as an echocardiography specialist, he regularly performed echocardiographic examinations and communicated with cardiac surgeons about the results of those examinations. The attending intensivist frequently performed echocardiographic examinations of patients who were likely to develop cardiac tamponade due to postoperative bleeding. Based on the results of those examinations and subsequent communication with cardiac surgeons, if deemed necessary, immediate re-exploration was performed. We believe that the decreased number of cases of cardiac arrest due to cardiac tamponade may have been associated with regular echocardiographic examinations by the attending intensivist. These results might also have been due to the attending intensivist’s thorough understanding of cardiac surgery and ability to communicate clearly with the cardiac surgeons, as the attending intensivist was board-certified in cardiothoracic surgery. The length of hospital stay was decreased by an average of 0.6 days (=14 hours), in line with the decrease in the length of ICU stay, but there was no significant difference in the overall length of hospital stay or the proportion of patients with a prolonged hospital stay of more than 14 days. The 30-day mortality rate was lower in the intensivist group, but no statistically significant difference was found between the 2 matched groups, which may have been due to the fact that elective isolated CABG has a much lower mortality rate than other types of cardiac surgery. Although further investigations are needed, a greater improvement in the mortality rate in the intensivist group would be expected if patients undergoing valvular or aortic surgery, which pose a higher risk for mortality, are included. The proportion of patients with any of the abovementioned complications was significantly lower in the intensivist group. The percentage of patients with 2 or more complications was also significantly lower in the intensivist group.
There are several limitations of our study. The first limitation is that only patients who underwent elective isolated CABG were included. Given that the intensivist in this study managed every postoperative patient regardless of the type of surgery, in principle, all types of open cardiac surgery—including aortic and valvular surgery—could have been included. If we did so, the results could have been different, but as mentioned previously, the heterogeneity of the population might have led to difficulties in interpreting the results. In a future study, the same method could be used to determine whether the presence of an attending intensivist had a positive effect on clinical outcomes in patients undergoing aortic or valvular surgery. The second limitation is that there was only 1 intensivist in this study. The presence of a homogeneous group of intensivists in this study would have yielded more meaningful results. However, due to the lack of intensivists, previous studies have assessed the impact of a heterogeneous group of intensivists with various specialties. It would be very interesting if a future study investigated whether intensivists with different specialties have different impacts on clinical outcomes. Finally, even though several studies have proven that the presence of an attending intensivist is associated with improved clinical outcomes, the cost of introducing the closed ICU system should be considered. Therefore, the cost-effectiveness of the closed CSICU model with attending intensivist coverage should be analyzed in future studies.
In conclusion, we found that a transition from an open ICU model with trainee coverage to a closed ICU model with attending intensivist coverage was associated with better clinical outcomes. Our findings indicate that the presence of an attending intensivist who was board-certified in cardiothoracic surgery and critical care was associated with improvements in CSICU quality and reductions in postoperative complications.
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Dimick JB, Pronovost PJ, Heitmiller RF, Lipsett PA. Intensive care unit physician staffing is associated with decreased length of stay, hospital cost, and complications after esophageal resection. Crit Care Med. 2001;29:753–8. doi: 10.1097/00003246-200104000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Treggiari MM, Martin DP, Yanez ND, Caldwell E, Hudson LD, Rubenfeld GD. Effect of intensive care unit organizational model and structure on outcomes in patients with acute lung injury. Am J Respir Crit Care Med. 2007;176:685–90. doi: 10.1164/rccm.200701-165OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pronovost PJ, Jenckes MW, Dorman T, et al. Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. JAMA. 1999;281:1310–7. doi: 10.1001/jama.281.14.1310. [DOI] [PubMed] [Google Scholar]
- 4.Carson SS, Stocking C, Podsadecki T, et al. Effects of organizational change in the medical intensive care unit of a teaching hospital: a comparison of ‘open’ and ‘closed’ formats. JAMA. 1996;276:322–8. doi: 10.1001/jama.1996.03540040066035. [DOI] [PubMed] [Google Scholar]
- 5.Multz AS, Chalfin DB, Samson IM, et al. A “closed” medical intensive care unit (MICU) improves resource utilization when compared with an “open” MICU. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1468–73. doi: 10.1164/ajrccm.157.5.9708039. [DOI] [PubMed] [Google Scholar]
- 6.Kumar K, Zarychanski R, Bell DD, et al. Impact of 24-hour in-house intensivists on a dedicated cardiac surgery intensive care unit. Ann Thorac Surg. 2009;88:1153–61. doi: 10.1016/j.athoracsur.2009.04.070. [DOI] [PubMed] [Google Scholar]
- 7.Benoit MA, Bagshaw SM, Norris CM, et al. Postoperative complications and outcomes associated with a transition to 24/7 intensivist management of cardiac surgery patients. Crit Care Med. 2017;45:993–1000. doi: 10.1097/CCM.0000000000002434. [DOI] [PubMed] [Google Scholar]
- 8.Huard P, Kalavrouziotis D, Lipes J, et al. Does the full-time presence of an intensivist lead to better outcomes in the cardiac surgical intensive care unit? J Thorac Cardiovasc Surg. 2019;(19):30976–6. doi: 10.1016/j.jtcvs.2019.03.124. S0022-5223. [DOI] [PubMed] [Google Scholar]
- 9.Ferguson TB, Jr, Hammill BG, Peterson ED, DeLong ER, Grover FL STS National Database Committee. A decade of change: risk profiles and outcomes for isolated coronary artery bypass grafting procedures, 1990–1999 a report from the STS National Database Committee and the Duke Clinical Research Institute. Society of Thoracic Surgeons. Ann Thorac Surg. 2002;73:480–9. doi: 10.1016/S0003-4975(01)03339-2. [DOI] [PubMed] [Google Scholar]
- 10.Rahmanian PB, Kroner A, Langebartels G, Ozel O, Wippermann J, Wahlers T. Impact of major non-cardiac complications on outcome following cardiac surgery procedures: logistic regression analysis in a very recent patient cohort. Interact Cardiovasc Thorac Surg. 2013;17:319–26. doi: 10.1093/icvts/ivt149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haupt MT, Bekes CE, Brilli RJ, et al. Guidelines on critical care services and personnel: recommendations based on a system of categorization of three levels of care. Crit Care Med. 2003;31:2677–83. doi: 10.1097/01.CCM.0000094227.89800.93. [DOI] [PubMed] [Google Scholar]
- 12.Rhodes A, Moreno RP, Azoulay E, et al. Prospectively defined indicators to improve the safety and quality of care for critically ill patients: a report from the Task Force on Safety and Quality of the European Society of Intensive Care Medicine (ESICM) Intensive Care Med. 2012;38:598–605. doi: 10.1007/s00134-011-2462-3. [DOI] [PubMed] [Google Scholar]
- 13.Probst S, Cech C, Haentschel D, Scholz M, Ender J. A specialized post anaesthetic care unit improves fast-track management in cardiac surgery: a prospective randomized trial. Crit Care. 2014;18:468. doi: 10.1186/s13054-014-0468-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu D, Wu C, Zhang S, Zhong Y. Risk factors of ventilator-associated pneumonia in critically III patients. Front Pharmacol. 2019;10:482. doi: 10.3389/fphar.2019.00482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park SY, Lee HB. Prevention and management of delirium in critically ill adult patients in the intensive care unit: a review based on the 2018 PADIS guidelines. Acute Crit Care. 2019;34:117–25. doi: 10.4266/acc.2019.00451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahesh B, Choong CK, Goldsmith K, Gerrard C, Nashef SA, Vuylsteke A. Prolonged stay in intensive care unit is a powerful predictor of adverse outcomes after cardiac operations. Ann Thorac Surg. 2012;94:109–16. doi: 10.1016/j.athoracsur.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Siepe M, Pfeiffer T, Gieringer A, et al. Increased systemic perfusion pressure during cardiopulmonary bypass is associated with less early postoperative cognitive dysfunction and delirium. Eur J Cardiothorac Surg. 2011;40:200–7. doi: 10.1016/j.ejcts.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 18.Brown CH. Delirium in the cardiac surgical ICU. Curr Opin Anaesthesiol. 2014;27:117–22. doi: 10.1097/ACO.0000000000000061. [DOI] [PMC free article] [PubMed] [Google Scholar]