ABSTRACT
Background: The STEPS programme has been succesfully implemented as a group-based treatment of trauma symptoms after rape for adolescents. The STEPS intervention was translated from Dutch to Danish and offered to adults in addition to adolescents as well as an individual intervention in addition to a group-based intervention at a Danish Centre for Rape Victims through 2011 to 2014. The programme was translated from Dutch to Danish and expanded to adults in addition to adolescents as well as to an individual intervention in addition to a group-based intervention at a Danish Centre for Rape Victims through 2011 to 2014.
Objective: The present study observes development in trauma symptoms and ICD-11 diagnostic status during an adapted version of the intervention programme ‘STEPS’ for survivors of sexual assault.
Methods: A prospective uncontrolled study was conducted, monitoring symptoms of posttraumatic stress and other trauma-related symptomatology before treatment, after treatment and at 6 and 12 months' follow up for 103 referrals receiving individual or group-based STEPS. Tentative diagnoses of posttraumatic stress disorder (PTSD) and complex PTSD were assigned to participants according to the ICD-11 to observe the development in diagnostic status across time, and multilevel modelling was used to assess the development of symptom severity and to assess the moderating effect of age-group and mode of delivery.
Results: A loglinear function representing large and statistically significant decline in symptomatology over time provided the best fit for all measures of trauma-related symptomatology. The decline was not moderated by age-group or mode of intervention. Dropout rates were independent of mode of intervention and age.
Conclusion: The adaption of the STEPS programme to adults and as an individual intervention is feasible and maintains effect sizes comparable to those observed in the original intervention. Further research using randomized controlled trials is needed to ascribe the observed effect to the STEPS programme.
KEYWORDS: Sexual assault, rape, PTSD, CPTSD, ICD-11, treatment, Intervention, STEPS
HIGHLIGHTS: • The STEPS intervention is feasible for adult survivors and individual treatment in addition to adolescents and group-based treatment.• Observed ICD-11 CPTSD-caseness decreases over time in referrals receiving the STEPS intervention.
Antecedentes: El programa STEPS se ha implementado con éxito como un tratamiento grupal de síntomas de trauma después de una violación en adolescentes. La intervención STEPS se tradujo del holandés al danés y se ofreció a adultos además de adolescentes, así como una intervención individual además de una intervención grupal en un Centro danés para víctimas de violación hasta el 2011 y el 2014.
Objetivo: El presente estudio observa el desarrollo de síntomas de trauma y el estado de diagnóstico de la CIE-11 durante una versión adaptada del programa de intervención “PASOS” para los sobrevivientes de agresión sexual.
Métodos: Se realizó un estudio prospectivo no controlado, monitorizando los síntomas de estrés postraumático y otras sintomatologías relacionadas con trauma antes del tratamiento, después del tratamiento y a los 6 y 12 meses de seguimiento para 103 derivaciones. Se asignaron a los participantes los diagnósticos tentativos de trastorno de estrés postraumático (TEPT) y TEPT complejo según la CIE-11 para observar el desarrollo en el estado de diagnóstico a través del tiempo, y se usó un modelado multinivel para evaluar el desarrollo de la severidad de los síntomas y evaluar el efecto moderador del grupo de edad y modo de entrega.
Resultados: Un función lineal logarítmica que representa una disminución grande y estadísticamente significativa de la sintomatología a lo largo del tiempo proporcionó el mejor ajuste para todas las medidas de la sintomatología relacionada con trauma. El efecto no fue moderado por grupo de edad o tipo de intervención. Las tasas de abandono fueron independientes del tipo de intervención y edad.
Conclusión:: La adaptación del programa STEPS para adultos y como una intervención individual es factible y mantiene el tamaño del efecto comparable con aquellos observados en la intervención original. Se necesita más investigación usando estudios controlados aleatorizados para atribuir el efecto observado al programa STEPS.
PALABRAS CLAVE: Abuso sexual, violación, TEPT, TEPT complejo, CIE-11, Tratamiento, Intervención, STEPS
背景: STEPS计划已成功实施为基于小组的针对青少年强奸后创伤症状的治疗方法。 STEPS干预从荷兰语翻译成丹麦语,并在2011年至2014年期间向青少年,成年人以及成人干预的个人干预以及丹麦基于强奸受害者的团体干预提供该计划由荷兰语翻译成丹麦语, 并且在2011年至2014年期间, 在丹麦强奸受害者中心从青少年扩展到成年人受众, 从团体干预扩展到个体干预形式。
目的: 本研究观察针对性攻击幸存者的改版“ STEPS”干预计划期间创伤症状和ICD-11诊断状态的发展。
方法: 进行了一项前瞻性非对照研究, 在治疗前后及六个月, 十二个月后对103例患者进行随访时, 对其创伤后应激症状和其他创伤相关症状进行了监测。根据ICD-11将参与者初步诊断为创伤后应激障碍 (PTSD) 和复杂性PTSD, 以观察不同时间段诊断状态的发展, 并使用多层模型来评估症状严重性的发展以及年龄段和分娩方式的调节作用。
结果: 对数线性函数反映出症状随时间的推移出现大幅且统计显著的下降, 且对于所有创伤相关症状测量都是最佳拟合。此效应并不被年龄段或干预类型调节。辍学率与干预类型和年龄无关。
讨论: 将STEPS程序应用于成人以及作为个体干预是可行的, 且效果保持了与原始干预中观察到的效果大小相当。需要使用随机对照试验进行进一步研究, 以确保观察到的效果可归因于STEPS计划。
关键词: 性侵犯, 强奸, 创伤后应激障碍, 复杂性PTSD, ICD-11, 治疗, 干预措施, STEPS
Every year, it is estimated that 4.7000 women become victims of rape in Denmark (based on the average number reported in yearly surveys conducted from 2008–2015, Pedersen, Kyvsgaard, & Balvig, 2016). However, many sexual assaults never come to light, since many victims do not report the assault or make use of services available for survivors of sexual assault. Therefore, many victims of sexual assault never get professional help after the assault (Balvig & Kyvsgaard, 2009), and this is problematic, since sexual assault can be traumatic and have severe consequences for the survivors. For instance, sexual assault significantly increases the risk of physical and social problems, as well as severe mental health problems, in particular, anxiety, depression, and posttraumatic stress disorder (PTSD; Hansen, Armour, & Elklit, 2012; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). A recent meta-analysis and review indicated that people who had been sexually assaulted reported significantly worse psychopathology than comparisons who were not assaulted. Sexual assault was associated with an increased risk for many forms of psychopathology, and particularly, stronger associations were found for posttraumatic stress (Dworkin, Menon, Bystrynski, & Allen, 2017). Particularly female survivors of sexual assault are at risk of developing PTSD compared to other trauma victims (Foa, 1997), and previous research shows that up to half of the victims go on to develop PTSD after the sexual assault (Elklit & Christiansen, 2010; Rothbaum et al., 1992). Furthermore, a recent review established rape as the trauma-type with the highest risk for subsequent PTSD (Kessler et al., 2017).
With the latest version of the International Classification of Diseases (ICD-11, World Health Organization, 2018), a comprehensive reassessment of stress-related disorders has resulted in a reconceptualization of PTSD symptomatology focusing on the three core symptoms of the response (i.e. intrusion, avoidance and hypervigilance), while introducing a sibling disorder of Complex PTSD (CPTSD) characterized by disturbances in self-organization, affective dysregulation and negative self-concept. In a preliminary study using the ICD-11 criteria for posttraumatic stress, Elklit, Hyland, and Shevlin (2014) found that survivors of sexual assault display the highest rates of PTSD (43.2%) and CPTSD (20.7%) compared to survivors of physical assault (PTSD: 33.6% and CPTSD: 13%) and parents that have suffered a sudden loss of their infant (PTSD: 25.2% and CPTSD: 10.4%). Similarly, a nationally representative study of ICD-11 posttraumatic stress in the German population found that sexual assault was among the trauma types most strongly related to both PTSD and CPTSD (Maercker, Hecker, Augusburger, & Kliem, 2018).
It is highly important to treat posttraumatic symptomatology following a sexual assault because of the associated suffering and significant disruption of important life-areas such as family-life, work-, school-, social- and sexual functioning. Moreover, PTSD appears to be a risk factor for experiencing subsequent sexual victimization (Elwood et al., 2011; Risser, Hetzel-Riggin, Thomsen, & McCanne, 2006), meaning that interventions could serve an additional preventive purpose. Several treatments have been found to effectively reduce PTSD severity in sexual assault victims. The most commonly studied types of psychotherapy are cognitive behavioural therapies (CBT), and a recent meta-analysis on the efficacy of treatments for PTSD found that several types of CBTs were effective (Watts et al., 2013). The most effective tend to be trauma-focused treatments combining elements of exposure and cognitive re-structuring such as cognitive behavioural therapy (Vickerman & Margolin, 2009), eye movement desensitization reprocessing (EMDR; Rothbaum, Astin, & Marsteller, 2005), prolonged exposure (PE, Foa & Rauch, 2004) and trauma-focused CBT (TF-CBT; Avinger & Jones, 2007; Deblinger, Mannarino, Cohen, & Steer, 2006). In particular, the latter has been shown to be especially effective in 8- to 14-year-old children when their parents are included in the treatment (Cohen, Deblinger, Mannarino, & Steer, 2004). The importance of involving parents in the treatment of PTSD following a sexual assault is emphasized by research showing that the debilitating consequences of sexual assault are not limited to the victim. Rather, relatives of the victim are also at risk of traumatization (Elklit, Christensen, & Bak, 2012). This suggests that it might be beneficial to involve the relatives in the treatment of survivors of sexual assault, particularly when the victim is underage.
The STEPS cognitive behaviour group-based intervention was developed in the Netherlands for adolescent survivors of sexual assault who had no prior sexual trauma (Bicanic & Kremers, 2007a, 2007b, 2007c, 2009). STEPS refers to the step-by-step approach in identifying problems after a sexual assault and pursuing new goals. Besides the aim of reducing posttraumatic symptomatology, STEPS also aims at facilitating the survivors’ coping with the fears relating to sexual assault and regaining balance in life. The group-therapy protocol included eight sessions for the victims, with a parallel group for parents which included six sessions focusing on psychoeducation, exposure in sensu, exposure in vivo, cognitive restructuring and relapse prevention.
The short- and long-term symptom trajectories following the STEPS intervention have been evaluated in a prospective observational study among female adolescents aged 13–18 years referred to two Dutch psychotrauma-centres between the years of 2005 and 2009. Sexual assault-related symptomatology including posttraumatic stress symptoms, and behavioural problems, was assessed, and the results showed a large and statistically significant decrease in both posttraumatic stress symptoms and behavioural problems immediately following treatment that was maintained at follow up after 12 months (Bicanic, De Roos, Van Wesel, Sinnema, & Van de Putte, 2014). Results from these studies suggested a positive development across a range of trauma-related symptoms, and although previous research has documented high dropout rates in PTSD treatment (approximately 18%), particularly in sexual assault-related PTSD, the STEPS programme demonstrated extremely low dropout rates of 1.8% (Bicanic et al., 2014; Imel, Laska, Jakupcak, & Simpson, 2013).
There might be several reasons for this. For example, individual differences among patients have been found to influence dropouts (Keefe et al., 2018), and since the STEPS programme was developed for adolescent victims of a single sexual assault, the somewhat strict inclusion criteria may partly explain the low dropout rates as well as the involvement of parents in treatment. However, in many treatment facilities, patients are likely to be characterized by individual differences in age and ability to participate in group-based interventions, etc. The STEPS programme can be delivered in groups and individually (Bicanic et al., 2014) with different benefits and drawbacks. Group-interventions can be beneficial due to sharing among peers and overcoming feelings of stigma and isolation. A supportive atmosphere makes it easier to open up, feel understood and learn from others. However, the group-format also implies less flexibility for when to start, and some victims will have to stay on a waiting list for a long time. In assigning victims to a group-based intervention, age and developmental level of the participants as well as specific challenges related to psychopathology, intelligence, drug-abuse, etc. must be considered.
While the original STEPS programme was developed for use with adolescent girls, nothing in the programme itself excludes the use of it among older survivors of sexual assault. Indeed, the significant results reported in the original work (Bicanic et al., 2014) should encourage further research into the utility of the programme to other formats and age-groups. Thus, in an effort to overcome some of the shortcomings of the group-based approach and the previous limitations on patient age-group, the current study translated and offered the STEPS intervention in a Danish treatment facility for survivors of sexual assault (Centre for Rape Victims, CRV). The intervention was offered to both adolescents and adults and as a group-based intervention and individual therapy dependent on a clinical assessment of optimal treatment-approach. While Bicanic et al. (2014) suggested that the STEPS intervention can indeed also be applied as an individual intervention, research is needed that examines whether the usefulness of the programme can be generalized to a naturalistic setting with participants of varying ages and modes of treatment (individual as well as group-based treatment).
The objective of the current pilot-study, therefore, was to observe the feasibility of delivering the STEPS intervention to Danish survivors of sexual assault, and to observe the short- and long-term symptom trajectories, including PTSD, CPTSD, negative affectivity, somatization and dissociation in a group of Danish adolescent and adult survivors of sexual assault receiving an adapted version of the STEPS programme. We expected to reproduce Bicanic et al. (2014)’s finding of declining symptom scores over time (hypothesis 1), and we hypothesized that the observed trend would be present across both age-groups (hypothesis 2) and both modes of intervention (hypothesis 3).
Furthermore, while a criterion for being offered treatment via the STEPS programme is clinically significant levels of PTSD assessed at visitation, the data for the current study was collected using the DSM-IV-R criteria for PTSD. Meanwhile, a revised version of ICD-11 has been released that will guide the diagnosis of posttraumatic sequelae in Denmark under the diagnoses of PTSD and Complex PTSD (CPTSD). As yet, it appears that no studies have been conducted that investigates the development in posttraumatic stress symptomatology over time as defined per ICD-11 in survivors of sexual assault. Thus, a secondary exploratory goal of the current study was to trace the development in diagnostic status as per ICD-11 across time for the participants enrolled in STEPS-treatment.
1. Methods
Between 2011 and 2014, the STEPS programme was implemented in an intervention study at the CRV in Aarhus, Denmark. The CRV is an interdisciplinary centre, providing medical and psychosocial care and support for survivors of sexual assaults aged 12 and above (Bramsen, Elklit, & Nielsen, 2009).
1.1. Translation and adaptation of the treatment protocol
The original Dutch-language version of the STEPS programme was translated into Danish by a professional translation company, the Avantigroup, and then further edited by members of staff from CRV in Aarhus and the police in Aarhus to ensure correspondence with Danish legislation and procedures. The STEPS protocol consists of two parts: one for the victim and one for the parents. Figure 1 describes the content of the sessions for survivors of sexual assault. The programme consists of five steps: (1) psychoeducation about sexual assault and the common consequences provided by psychologists, police officers and forensic doctors, (2) in sensu exposure to the sexual assault by talking and writing about it, (3) cognitive restructuring of the experience, (4) in vivo exposure by confronting reminders of the trauma, such as situations and objects in real life, and (5) relapse prevention.
Figure 1.
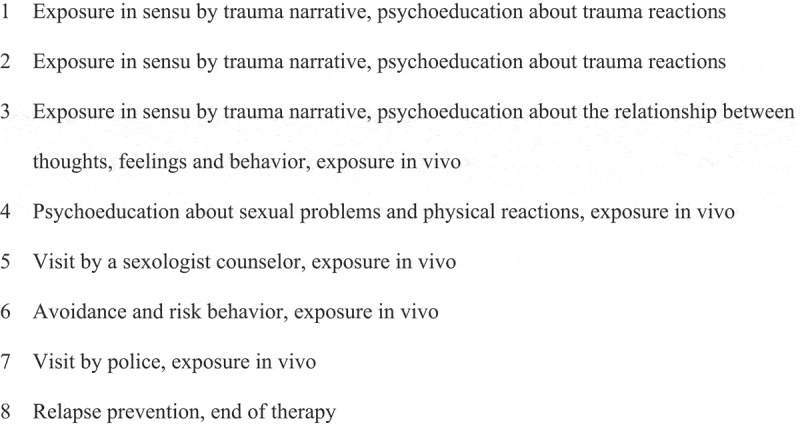
An outline of the STEPS protocol, session-by-session (1–8), victim group.
An intervention-group for parents of adolescent survivors of sexual assault was offered simultaneously with the intervention for survivors. The purpose of the parental programme was to reduce parental stress and assisting parents in how to best support their children by sharing their own feelings and concerns in a considerate way, informing them about general consequences of sexual assault and challenges that the survivors might meet.
The STEPS programme is scheduled as an eight-week intervention commencing after an individual introductory session where personal goals are set and an in vivo hierarchy was established. In the last half of the victims’ programme, the focus is on individual goals and in vivo exposure as home work. All participants receive an exercise book (Bicanic & Kremers, 2007b, 2007c) with general information about trauma reactions and coping as well as instructions for homework to facilitate this.
1.2. Participants
Participants were survivors of sexual assault referred in 2011–2014 to treatment at the Danish CRV for mental health problems related to a sexual assault that took place at least a month before referral. A total of 250 survivors of sexual assault were referred to CRV to participate in STEPS during this period, and 165 referrals were screened for study inclusion. The occurrence of a sexual assault was assessed in an interview by a staff member; 82% had experienced penetration; 8% a rape attempt; 5% had amnesia about what happened; and 6% were ‘other’ (e.g. forced kissing, touch). Figure 2 displays selection criteria and dropout during the study period. The final sample consisted of 36 adolescents (age 13–18) and 60 adults (age 19–37) with a mean age of 21.2 years (SD = 6.53, range: 14–58). The mean time since the assault was 46.2 months, but a standard deviation of 67.7 months suggested that there was a considerable variability in time since the assault (range = 1–479, median = 16, mode = 3 months). A majority of the participants were under education (n = 72, 75%), whereas 9.4% were working (n = 9), 10.4% were unemployed (n = 10) and 5.2% were under rehabilitation or registered as long-term sick (n = 5). A total of 52 referrals were offered an individualized version of the STEPS programme (54.2%), 23 referrals were offered an intervention combining group-based STEPS and individual supportive sessions (24%), and 21 dropped out before being assigned an intervention. Table 1 displays sample descriptive statistics and attrition rates across T1-T4.
Figure 2.
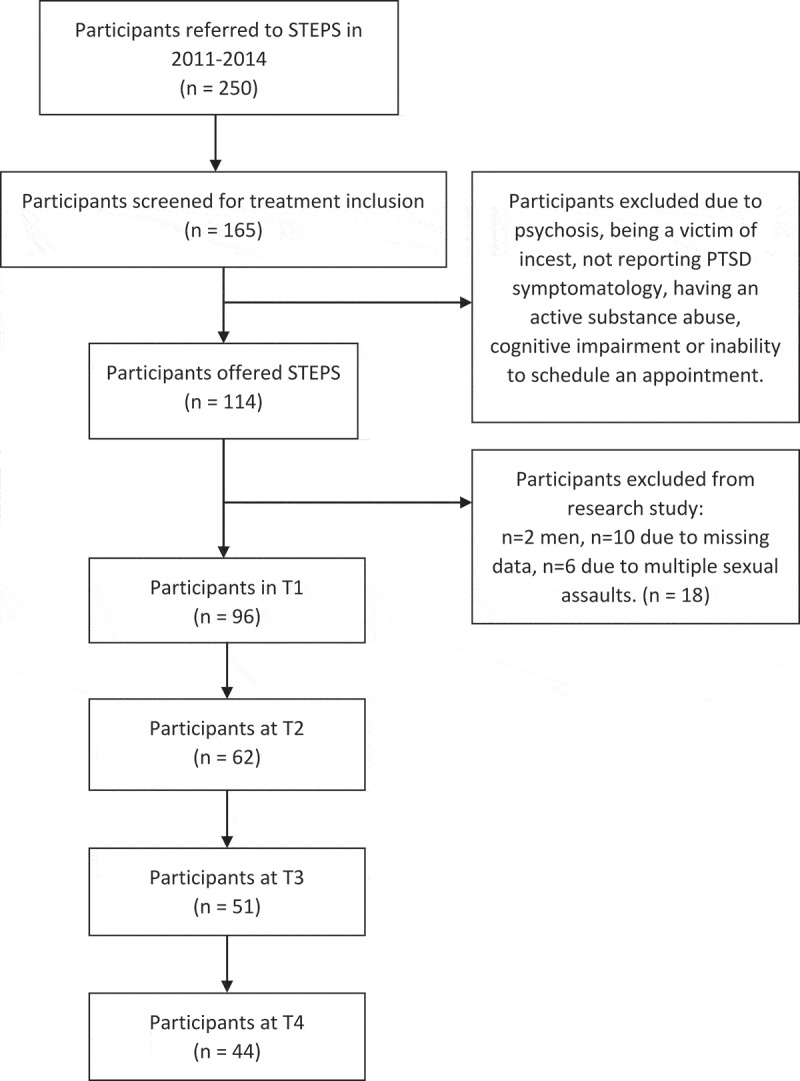
Flowchart of participant recruitment and dropout.
Table 1.
Descriptive statistics and attrition for sample at T1-T4
| T1 |
T2 |
T3 |
T4 |
|||||
|---|---|---|---|---|---|---|---|---|
| N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | |
| HTQ | 96 | 45.7 (7.1) | 62 | 35.4 (8.8) | 51 | 34.3 (9.1) | 44 | 31.7 (8.5) |
| TSC total | 89 | 57.7 (9.3) | 61 | 45.3 (9.6) | 50 | 43.7 (9.9) | 41 | 41.1 (9.4) |
| TSC Negative affectivity | 89 | 22.5 (5.1) | 61 | 17.4 (4.3) | 50 | 16.8 (4.8) | 41 | 16 (4.5) |
| TSC Somatization | 89 | 25.3 (4.6) | 61 | 20 (5) | 50 | 19.4 (4.5) | 41 | 17.9 (4.9) |
| TSC Dissociation | 89 | 9.8 (2.3) | 61 | 7.9 (2) | 50 | 7.5 (2) | 41 | 7.2 (1.8) |
| Attrition-rate | ||||||||
| HTQ | 35.4% | 17.8% | 13.7% | |||||
| TSC | 31.5% | 18% | 18% | |||||
Attrition is calculated with reference to the previous time-point.
1.3. Measures
The participants were asked to complete questionnaires assessing demographic factors and psychological symptoms before treatment (T1), after treatment (T2). Participants went on to be monitored by completing two additional questionnaires at 6- and 12-months' follow up (T3 and T4, respectively). The questionnaires included the following measures:
1.3.1. PTSD severity
Participants completed the Harvard Trauma Questionnaire (HTQ) to assess levels of DSM-IV-R PTSD. The HTQ consists of 31 items that are scored on a 4-point Likert-type scale ranging from 1 (‘not at all’) to 4 (‘all the time’). Summarizing items 1–17 provides an index of PTSD-severity that has been used in the current study. The HTQ has shown cultural sensitivity as well as good internal and external validity (Mollica et al., 1992), and has previously been used in studies of survivors of sexual violence (Armour, Shevlin, Elklit, & Mroczek, 2012; Bicanic et al., 2014). The scale displayed good internal reliability in the current study (Cronbach’s α = 0.84).
1.3.2. Other trauma-related symptoms
Participants completed the Trauma Symptom Checklist (TSC), a 35-item questionnaire assessing the occurrence of other types of trauma symptomatology (Briere & Runtz, 1989; Elklit, 1990). The scale is scored on a 4-point Likert-type scale ranging from 0 to 3 (‘not at all’ to ‘very often’). The TSC was used to operationalize the occurrence of dissociation, somatization, and negative affectivity. It has good psychometric qualities (Krog & Duel, 2003), and displayed good internal reliability in the current study (Cronbach’s α = .87).
1.4. Data analysis
Before analysis, missingness was assessed for HTQ and TSC separately at all timepoints. Testing the pattern of missing data, there was no indication of systematic missingness (MCAR, p > .10), and any missing data was imputed using the EM-algorithm for all cases missing ≤20% of data for each scale. There were no statistically significant deviations from normality in the data.
Independent samples t-test was used to assess significant differences on the HTQ and TSC-scales at T1 between (a) adolescents and adults, (b) referrals receiving individual treatment only and referrals receiving group-based treatment in addition to individual treatment, and (c) dropouts after T1 and participants completing at minimum T1 and T2.
Tentative diagnostic codes reflecting ICD-11 PTSD and CPTSD were computed for all participants using items from the HTQ and TSC following the procedure described in Elklit et al. (2014). Specifically, a score of ≥2 on the TSC and ≥3 on the HTQ comprised symptom-endorsement. Pertaining to the ICD-11 guidelines for PTSD and CPTSD, a minimum of one item per symptom cluster is required to endorse the diagnoses. PTSD consists of three symptom clusters: re-experiencing, avoidance and heightened sense of threat. CPTSD consists of PTSD and endorsement of at least one item in all three additional symptom clusters: Affective dysregulation, negative self-concept and interpersonal problems. HTQ items 2 and 3 were used as indicators for re-experiencing, HTQ items 11 and 15 were used as indicators for avoidance, and HTQ items 6 and 9 were used as indicators for heightened sense of threat. TSC items 14 and 16 were used as indicators for affective dysregulation, TSC items 28 and 29 were used as indicators for negative self-concept, and finally, TSC item 6 and HTQ item 27 were used as indicators for interpersonal problems. All analyses were conducted using SPSS version 25.
The symptom development during and after delivery of the STEPS programme was evaluated using multilevel modelling (MLM). As there was attrition in the sample, MLM is a flexible and advantageous strategy for analysis as maximum likelihood estimation allows for use of all available data to test our hypotheses. Analyses were conducted separately for the total HTQ and TSC score as well as for the subscales measuring negative affectivity, somatization and dissociation on the TSC. All outcomes were treated as continuous and all models were specified with a random intercept. Any between-model comparison was conducted using changes in −2LL and BIC values for the model fit. For changes in the −2LL, a difference of at least 3.84 was required for representing a significantly better fit for models including an extra parameter. For the BIC, a decline of 10 points was required for improved model fit (Raftery, 1995). First, we specified two types of null models to assess the amount of variability expected to reside at each level: A two-level null model where measurement points were nested within individuals, and a three-level null model where individuals were nested in age-groups and modes of intervention. The three-level MLM either did not converge or did not improve the model fit compared to the two-level MLM, meaning that all subsequent analyses were conducted as a two-level MLM.
Second, after inspecting a graphical representation of the data, we proceeded to test two models of time: a linear function and a loglinear function, the latter representing a steeper initial decline in symptomatology between pre- and post-treatment that flattens across subsequent measurement points. These models were specified with a fixed slope and random intercept. Third, we proceeded to test if models including individual variability around the slope would improve the description of the data by testing the best fitting model from step 2 with a random slope and random intercept for all models. Fourth, we proceeded to test hypotheses 2 and 3 by including the age-group and delivery of intervention as time-invariant covariates in separate models for all outcomes and covariates. Effect-sizes are reported using Cohen’s d with d = 0.2; 0.5 and 0.8 constituted a small, medium and large effect, respectively. Cohen’s d was derived from the F test calculated as d = 2 * √(F/df).
2. Results
A total of 26 referrals completed all data points for the individual intervention, and 11 referrals completed all data points for the group-based intervention, leaving a total of 37 completers and 35 dropouts completing only T1. The remaining 24 referrals contributed to either two or three of the data points of the study as per the description in Table 1.
Table 2 displays the results from the independent samples t-test. There was a significant difference between adolescents and adults on time since the sexual assault with adults reporting significantly more time passed since the assault than adolescents, although standard deviations for both groups were of a considerable magnitude. There were no differences in symptom level of participants offered individual STEPS compared to group-based STEPS, but referrals receiving individual therapy were slightly older than referrals receiving the group-intervention. Finally, dropouts and participants differed significantly in PTSD-severity (p = .011) and other trauma-related symptoms (TSC total: p = .009, negative affectivity: p = .017, somatization p = .045) apart from dissociation, with dropouts reporting significantly lower levels across all measures. There was no statistically significant difference in dropout rates between referrals receiving individual treatment and group-treatment (χ2 (1), .52, p = .47), or between adults and adolescents (χ2 (1), .002, p = .96). Finally, while there was variation in age depending on mode of intervention with referrals receiving the individual STEPS being slightly older than referrals receiving the group-intervention, this difference did not reach statistical significance across the age-groups (χ2 (1), 3.27, p = .07).
Table 2.
Descriptive statistics for outcomes at T1 across sample characteristics
| HTQ total |
TSC total |
TSC negative affectivity |
TSC somatization |
TSC dissociation |
N months since assault |
Age |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | ||
| Age-group | 13–18 yr | 45.94 | 8.23 | 59.26 | 9.54 | 24.11 | 5.42* | 25.09 | 3.98 | 10.06 | 2.29 | 17.79 | 17.92 | 16.33 | 1.44 |
| 19–100 yr | 45.51 | 6.43 | 56.67 | 9.06 | 21.44 | 4.62 | 25.51 | 4.91 | 9.70 | 2.39 | 65.46 | 80.54** | 24.78 | 7.84** | |
| Intervention | Individ. | 45.94 | 7.14 | 58.58 | 8.61 | 23.18 | 4.15 | 25.46 | 4.15 | 9.94 | 2.43 | 55.78 | 85.22 | 22.79 | 7.90* |
| Group | 47.36 | 5.41 | 58.89 | 8.78 | 22.89 | 4.92 | 26.16 | 4.8 | 9.84 | 1.89 | 39.05 | 33.51 | 19.05 | 3.43 | |
| Dropout | Dropout | 43.25 | 8.08 | 54.19 | 9.42 | 20.74 | 4.75 | 24.03 | 4.7 | 9.42 | 2.31 | 37 | 47.03 | 21.5 | 7.49 |
| Particip. | 47.07 | 6.15 | 59.55 | 8.72 | 23.43 | 5.05 | 26.05 | 4.35 | 10.07 | 2.35 | 54.58 | 79.03 | 21.63 | 7.5 | |
Independent samples t-test was used to test differences across outcomes for each of the conditions. Significant differences are listed in bold and the significantly larger of the two is flagged using *p ≤ .05, ** p ≤ .01. ‘Particip.’ refers to participants who participated in the treatment and completed at least T1 and T2. ‘Dropout’ refers to participants who dropped out after visitation. 'Individ.' refers to participants receiving the individual intercention.
Table 3 displays the results from the multilevel model and Cohen’s d calculations. The ICC of the two-level models indicated that between 19.7% and 25.8% variance was explained at the individual level. The loglinear model represented the best description of the development across time for all outcomes. Adding a random slope to the models did not improve the model fit for any of the models. Consequently, the final models were estimated as two-level models with fixed slopes and fixed intercepts. There were no statistically significant interaction effects of age-group or mode of intervention. However, there was a main-effect for age-group for negative affectivity, where adults scored significantly lower than adolescents (F (1, 180) = 6.65, p = .011, t (180) = – 2.58, p = .011). There was a statistically significant decline in symptomatology across time for all symptomatology, by far surpassing the cut-off for a large effect. Figure 3 displays the main effect for HTQ as an example of the trajectories over time.
Table 3.
Estimates of main and interaction effect for the final model across outcomes
| Main effect |
Main effect |
|||||
|---|---|---|---|---|---|---|
| Time (log) |
Age-group |
|||||
| Estimate | t(df), p | Cohen’s d | Estimate | t(df), p | Cohen’s d | |
| HTQ | −18.84 | t(179.3) = −5.39, <.001 | 1.97 | NS | ||
| TSC total | −20.6 | t(175.3) = −5.03, <.001 | 2.01 | NS | ||
| TSC Negative aff. (NA) | −7.07 | t(180.1) = −3.28, <.001 | 1.55 | 6,65 | t (180) = −2.58, .011 | |
| TSC Somatization (Som) | −10.31 | t(169.5) = −5.18, <.001 | 1.83 | NS | ||
| TSC Dissociation (Dis) | −3.22 | t(168.3) = −3.36, <.001 | 1.43 | NS | ||
NS: Statistically nonsignificant. As noted in the Results section, the interaction-effect for age-group was statistically nonsignificant across all outcomes: HTQ: F(1,197.6) = .000, p = .993; TSC: F(1,188.3) = 1.388, p = .240; TSC_NA: F(1,192.2) = 2.068, p = .152; TSC_Som: F(1,186.3) = 0.676, p = .412; TSC_Dis: F(1,186.5) = 0.008, p = .928. The main effect for age-group was statistically non-significant, apart from for TSC_NA: HTQ: F(1,171.9) = 0.305, p = .993; TSC: F(1,188.3) = 1.388, p = .240; TSC_NA_ F(1,180) = 6.65, p = .011, t(180) = – 2.58, p = .011; TSC_Som: F(1,163.2) = 0.025, p = .875; TSC_Dis: F(1,170.4) = .649, p = .422. The interaction-effect for mode of intervention was statistically nonsignificant across all outcomes: HTQ: F(1,172.9) = 2.233, p = .137; TSC: F(1,167.6) = 2.315, p = .130; TSC_NA: F(1,170) = 1.991, p = .160; TSC_Som: F(1,164.2) = 3.674, p = .057; TSC_Dis: F(1,165.8) = 0.435, p = .510. The main effect for mode of intervention was statistically non-significant: HTQ: F(1,145.6) = 0.710, p = .401; TSC: F(1,151.4) = 0.363, p = .548; TSC_NA: F(1,161.6) = 0.140, p = .708; TSC_Som: F(1,142.7) = 1.254, p = .265; TSC_Dis: F(1,152.6) = 0.411, p = .522.
Figure 3.
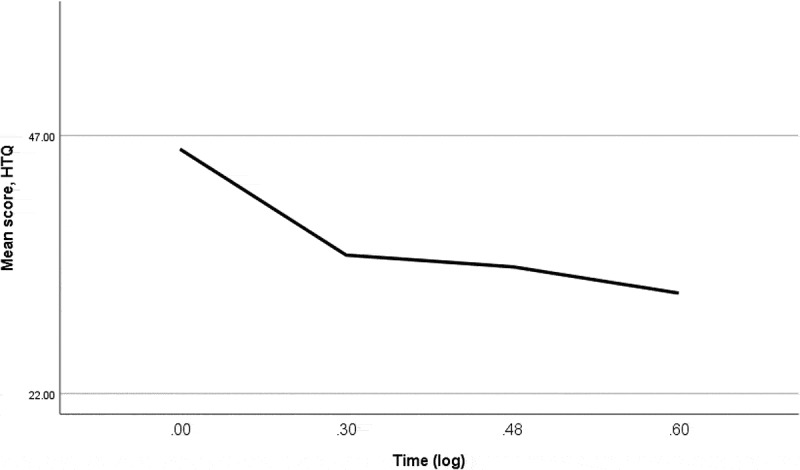
Symptom development in HTQ score for all participants.
Note: Y-axis is scaled to the range of scores at T1: 22–58.
Table 4 displays probable diagnostic status as per ICD-11 for participants across T1-T4.
Table 4.
Probable endorsement of ICD-11 diagnoses
| T1 |
T2 |
T3 |
T4 |
|
|---|---|---|---|---|
| Diagnosis | (n = 82) | (n = 61) | (n = 50) | (n = 41) |
| No diagnosis | 14.6% (n = 12) | 36.1% (n = 22) | 40% (n = 20) | 57.1% (n = 24) |
| PTSD | 12.2% (n = 10) | 29.5% (n = 18) | 26% (n = 13) | 23.8% (n = 10) |
| CPTSD | 73.2% (n = 60) | 34.4% (n = 21) | 34% (n = 17) | 19% (n = 8) |
Diagnostic codes could not be assigned to all participants due to missing data. Percentages reported are valid percentages.
At baseline, most participants fulfilled the criteria for probable CPTSD according to the ICD-11. This proportion was markedly reduced after treatment (T2) and continued to decrease across measurement points. Similarly, the proportion of participants endorsing no diagnosis continued to increase across measurement-points. There was an increase of participants endorsing PTSD from T1 to T2. Out of these, the majority of participants had endorsed a CPTSD diagnosis at T1 (75%, n = 12), and the remainder endorsed a diagnosis of PTSD at T1. Participants dropping out after baseline-assessment reported higher proportions of no diagnosis (21.9%, n = 7), lower proportions of PTSD (6.3%, n = 2) and comparable proportions of CPTSD (71.9%, n = 23) compared to the participating group.
3. Discussion
The purpose of the present study was to observe the short- and long-term symptom development during an adapted version of the STEPS programme offered as individual- and group-based treatment to adolescent and adult referrals to the Danish CRV. The STEPS programme is specifically designed for survivors of sexual assault but includes features similar to other effective programmes, for example, exposure in sensu, exposure in vivo, psychoeducation and cognitive restructuring (Cohen et al., 2004; Deblinger et al., 2006). Differences between the programmes include the multidisciplinary provision of STEPS involving forensic and medical professionals, and the education on sex and sexual problems, including relapse prevention.
When interpreting the findings, two limitations should be noted: All participants in the current study received individual supportive sessions in addition to the STEPS programme whether delivered as an individual or group-based intervention, and there was no control group, meaning that the current study does not provide sufficient basis to construe any decline in symptomatology as an effect of the STEPS programme or any other factors. Notably however, although the age-group and mode of treatment were expanded from the original protocol, referrals presented with comparable level of symptom severity in each group and there was no significant difference in symptom development based on whether they were offered individual treatment or individual and group-based treatment, suggesting that the provision of STEPS to an expanded target-group and in an adapted format is feasible. After the completion of STEPS, the survivors of sexual assault reported a large and statistically significant decrease in the severity of psychological symptoms across all indicators. For all measures of posttraumatic sequelae, the decrease was maintained at 12 months' follow up. Although not directly comparable, the effect sizes found in the current study were similar to the ones previously reported in studies on the efficacy of the original STEPS programme (Bicanic et al., 2014), suggesting that the adapted version of the STEPS programme maintains its properties in an expanded target-group in addition to being feasible. The largest decrease of symptomatology occurred between T1 and T2 for all outcomes. Across outcomes, the largest decrease occurred in posttraumatic symptoms as measured by the HTQ and general trauma-related symptoms as measured by the TSC.
A secondary, exploratory aim of the present study was to observe the development in diagnostic status as per the ICD-11 criteria over time for the participants in the STEPS programme. Compared to previous estimates of diagnostic status in survivors of sexual assault using the same calculation method (43.2% and 20.7% for PTSD and CPTSD, respectively, Elklit et al., 2014), the current sample displayed markedly higher rates of CPTSD (73.2%) and slightly lower rates of PTSD (12.2%) at T1, whereas 14.6% did not qualify for either diagnosis. Recent research suggests that CPTSD might be more common in clinical populations than PTSD (Karatzias et al., 2017), and for that reason, it is notable that at T4 (12-month follow up), the majority of participants did not qualify for a diagnosis, while we observed a large decrease in rates of probable CPTSD and an increase in rates of probable PTSD. A recent meta-analysis of interventions for CPTSD suggests that these can be built upon interventions effective for treating PTSD (Karatzias et al., in press). In light of these findings, the current results might suggest that the STEPS programme could be beneficial in addressing disturbances in self-organization (that together with PTSD comprise CPTSD), as the majority of the PTSD-cases at T2 qualified for probable CPTSD at T1. Alternatively, they could suggest that levels of CPTSD symptomatology fluctuate over time, as any decline in symptomatology cannot be ascribed to the STEPS-intervention due to the design of the present study. There is currently insufficient knowledge on the longitudinal development in diagnostic status on ICD-11 PTSD and CPTSD to speculate on the cause of these changes and future research using controlled designs is needed that investigates the effectiveness of group-based interventions versus individual interventions for CPTSD as well as the effect of interventions across age-groups. Referrals who dropped out after baseline assessment had lower rates of PTSD and comparable rates of CPTSD compared to the referrals who completed treatment but did not differ in the severity of posttraumatic symptomatology as indicated by the total score on the HTQ. Rather, they reported lower levels of depressive symptoms and other trauma-related symptomatology, and dropout-rates were unaffected by the mode of intervention offered, suggesting that the elevated dropout-rates in the current study compared to Bicanic et al. (2014) could be ascribed to other factors than symptom severity. The increase in dropout-rates was notable but should be interpreted with caution due to the small sample size. More research that explores potential explanations for dropout during the STEPS intervention is needed to facilitate that referrals receive the full benefit of the intervention.
The STEPS programme was developed for survivors with sexual assault-related mental health problems who had experienced no prior sexual abuse. This group might not be representative of the sexual assault survivors at large as sexual assaults have shown to be strongly related to childhood sexual abuse and sexual revictimization (Maker, Kemmelmeier, & Peterson, 2001), with approximately one-third of sexual assault survivors having experienced previous sexual assaults. The efficacy of the STEPS programme for survivors of multiple sexual assaults needs to be investigated in future research.
Furthermore, some additional limitations of the current study need to be observed when interpreting the findings. There was no estimate of time passed since the initial assessment (T1) and commencement of treatment, and it is likely that this period of time has varied between participants. While the sample was larger than the sample in Bicanic et al. (2014), there was considerable attrition and future evaluations of the STEPS programme are required using larger sample sizes. There were no follow-up questionnaires for participants who dropped out after T1 which precluded the conduction of an intent-to-treat analysis. Furthermore, the tentative ICD-11 diagnostic status was computed using an unofficial measure, meaning that the actual rates might differ if assessed using the International Trauma Questionnaire (ITQ, Cloitre et al., 2018). Further research is required to explore whether the changes in diagnostic status can be linked to particular elements of the STEPS intervention. Time since trauma was not controlled for, since the only inclusion criterion regarding time was that at least 1 month had passed since the sexual assault. Some of the referrals might, therefore, have received treatment during a time where natural recovery may have occurred. The encouraging findings in the present study, therefore, need additional exploration in future controlled studies. A prospective study in adult survivors of sexual assault showed that 94% reported PTSD symptoms after 1 week, and that the percentage decreased to 65% after 1 month, and then again to 47% after 3 months (Rothbaum et al., 1992). However, sexual assault is among the trauma types with the highest risk of PTSD (Kessler et al., 2017, 1995), and although there might be some victims who will recover naturally given time, the sample in the current study was actively seeking treatment which could mean that they did not experience spontaneous remission of distressing symptoms. However, as the design of the current study does not allow for any attribution of effect, it cannot be ruled out that the decline in symptomatology observed in the current study is due to natural recovery.
Only one group-intervention for relatives was implemented due to low number of referrals registering for treatment, and due to anonymization procedures, we were unable to assess whether providing group-interventions for relatives affected completion rates or symptom-decline for the referrals. Parental stress has in general been shown to predict PTSD in children (Alisic, Jongmans, Van Wesel & Kleber, 2011), which suggests that involving parents in trauma-focused treatments is beneficial. Without education and explanation of PTSD symptoms, especially the ones that could be difficult to observe, such as re-experiencing and avoidance, parents might misperceive behaviour changes in their children as part of normal adolescence. Additionally, the low number of relatives offered enrolment in the parental intervention group might be a potential explanation for the higher dropout-rates seen in the present study compared to Bicanic et al. (2014).
The experience of sexual assault is a traumatic event which can have devastating effects for the survivors as well as the survivors’ relatives. Therefore, it is important to identify effective treatment programmes. The STEPS programme appears to be a feasible option for helping survivors of sexual assault recover from the trauma. To best assess the effectiveness of STEPS, the treatment should be compared to a control group and another exposure-based treatment in a randomized study. Research with appropriate study designs is needed to confirm the results from Bicanic et al. (2014) and the present study regarding the effectiveness of STEPS.
Funding Statement
The European Union’s Horizon 2020 research and innovation programme has generously supported Maria Louison Vang during this work under the Marie Skłodowska-Curie Grant Agreement No. 722523.
Acknowledgements
The authors would like to thank the survivors of sexual assault and the Danishc Center for Rape Victims for contributing to this piece of research.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Alisic, E., Jongmans, M., van Wesel, F., & Kleber, R. (2011). Building child trauma theory from longitudinal studies: A meta-analysis. Clinical Psychology Review, 31, 736–11. [DOI] [PubMed] [Google Scholar]
- Armour, C., Shevlin, M., Elklit, A., & Mroczek, D. (2012). A latent growth mixture modeling approach to PTSD symptoms in rape victims. Traumatology, 18(1), 20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avinger, K. A., & Jones, R. A. (2007). Group treatment of sexually abused adolescent girls: A review of outcome studies. The American Journal of Family Therapy, 35(4), 315–326. [Google Scholar]
- Balvig, F., & Kyvsgaard, B. (2009). Udsathed for vold og andre former for kriminalitet: Offerundersøgelserne 2005-08. Copenhagen, Denmark: Department of Justice. [Google Scholar]
- Bicanic, I., De Roos, C., Van Wesel, F., Sinnema, G., & Van de Putte, E. (2014). Rape-related symptoms in adolescents: Short- and long-term outcome after cognitive behavior group therapy. European Journal of Psychotraumatology, 5(1), 22969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bicanic, I., & Kremers, A. (Eds.). (2007a). STEPS: Cognitive behavior therapy for post traumatic stress disorder due to sexual violence. Manual. Amsterdam: Uitgeverij Boom. [Google Scholar]
- Bicanic, I., & Kremers, A. (Eds.). (2007b). STEPS: Cognitive behavior therapy for post traumatic stress disorder due to sexual violence. Workbook for adolescents. Amsterdam: Uitgeverij Boom. [Google Scholar]
- Bicanic, I., & Kremers, A. (Eds.). (2007c). STEPS: Cognitive behavior therapy for post traumatic stress disorder due to sexual violence. Workbook for parents. Amsterdam: Uitgeverij Boom. [Google Scholar]
- Bicanic, I., & Kremers, A. (2009). Behandelprotocol STEPS. Kind & Adolescent Praktijk, 8(1), 39–39. [Google Scholar]
- Bramsen, R. H., Elklit, A., & Nielsen, L. H. (2009). A Danish model for treating victims of rape and sexual assault: The multidisciplinary public approach. Journal of Aggression, Maltreatment & Trauma, 18(8), 886–905. [Google Scholar]
- Briere, J., & Runtz, M. (1989). The Trauma Symptom Checklist (TSC-33) early data on a new scale. Journal of Interpersonal Violence, 4(2), 151–163. [Google Scholar]
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavia, 138(6), 536–546. [DOI] [PubMed] [Google Scholar]
- Cohen, J. A., Deblinger, E., Mannarino, A. P., & Steer, R. A. (2004). A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry, 43(4), 393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deblinger, E., Mannarino, A. P., Cohen, J. A., & Steer, R. A. (2006). A follow-up study of a multisite, randomized, controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry, 45(12), 1474–1484. [DOI] [PubMed] [Google Scholar]
- Dworkin, E. R., Menon, S. V., Bystrynski, J., & Allen, N. E. (2017). Sexual assault victimization and psychopathology: A review and meta-analysis. Clinical Psychology Review, 56, 65–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elklit, A. (1990). Measurement of stress after a violent attack using the TSC-33 (Trauma Symptom Checklist). Nordic Psychology, 42, 281–289. [Google Scholar]
- Elklit, A., Christensen, D. M., & Bak, R. (2012). Secondary victims of rape. Violence and Victims, 27, 246–262. [DOI] [PubMed] [Google Scholar]
- Elklit, A., & Christiansen, D. M. (2010). ASD and PTSD in rape victims. Journal of Interpersonal Violence, 25, 1470–1488. [DOI] [PubMed] [Google Scholar]
- Elklit, A., Hyland, P., & Shevlin, M. (2014). Evidence of symptom profiles consistent with posttraumatic stress disorder and complex posttraumatic stress disorder in different trauma samples. European Journal of Psychotraumatology, 5(1), 24221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwood, L. S., Smith, D. W., Resnick, H. S., Gudmundsdottir, B., Amstadter, A. B., Hanson, R. F., … Kilpatrick, D. G. (2011). Predictors of rape: Findings from the National Survey of Adolescents. Journal of Traumatic Stress, 24, 166–173. [DOI] [PubMed] [Google Scholar]
- Foa, E. B. (1997). Trauma and women: Couse, predictors, and treatment. Journal of Clinical Psychiatry, 15, 25–28. [PubMed] [Google Scholar]
- Foa, E. B., & Rauch, S. A. (2004). Cognitive changes during prolonged exposure versus prolonged exposure plus cognitive restructuring in female assault survivors with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 72(5), 879. [DOI] [PubMed] [Google Scholar]
- Hansen, M., Armour, C., & Elklit, A. (2012). Assessing a dysphoric arousal model of acute stress disorder symptoms in a clinical sample of rape and bank robbery victims. European Journal of Psychotraumatology, 3, 18201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imel, Z. E., Laska, K. M., Jakupcak, M., & Simpson, T. L. (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81(3), 394–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias, T., Cloitre, M., Maercker, A., Kazlauskas, E., Shevlin, M., Hyland, P., … Brewin, C. R. (2017). PTSD and Complex PTSD: ICD-11 updates on concept and measurement in the UK, USA, Germany and Lithuania. European Journal of Psychotraumatology, 8(sup7), 1418103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias, T., Murphy, D., Cloitre, M., Bisson, J., Roberts, N., Shevlin, M., … Hutton, P. (in press). Psychological interventions for ICD-11 Complex PTSD symptoms: Systematic review and meta-analysis. Psychological Medicine. [DOI] [PubMed] [Google Scholar]
- Keefe, J. R., Wiltsey Stirman, S., Cohen, Z. D., DeRubeis, R. J., Smith, B. N., & Resick, P. A. (2018). In rape trauma PTSD, patient characteristics indicate which trauma-focused treatment they are most likely to complete. Depression & Anxiety, 35(4), 330–338. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., … Florescu, S. (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060. [DOI] [PubMed] [Google Scholar]
- Krog, T., & Duel, M. (2003). Trauma Symptom Checklist. Psykologisk Studie Skriftserie, 6(4), 1–162. [Google Scholar]
- Maercker, A., Hecker, T., Augusburger, M., & Kliem, S. (2018). ICD-11 prevalence rates of posttraumatic stress disorder and complex traumatic stress disorder in a German nationwide sample. The Journal of Nervous and Mental Disease, 206(4), 270–276. [DOI] [PubMed] [Google Scholar]
- Maker, A. H., Kemmelmeier, M., & Peterson, C. (2001). Child sexual abuse, peer sexual abuse, and sexual assault in adulthood: A multi-risk model of revictimization. Journal of Traumatic Stress, 14(2), 351–368. [DOI] [PubMed] [Google Scholar]
- Mollica, R. F., Caspi-Yavin, Y., Bollini, P., Truong, T., Tor, S., & Lavelle, J. (1992). Harvard trauma questionnaire: Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. Journal of Nervous and Mental Disease, 180, 111–116. [PubMed] [Google Scholar]
- Pedersen, A. B., Kyvsgaard, B., & Balvig, F. (2016). Udsathed for vold og andre former for kriminalitet: Offerundersøgelserne 2005–2015. København: Københavns Universitet, Justitsministeriet, Det kriminalpræventive råd, Rigspolitichefen. [Google Scholar]
- Raftery, A. E. (1995). Bayesian model selection in social research. In Raftery A. E. (Ed.), Sociological methodology (pp. 111–164). Oxford: Blackwell. doi: 10.2307/271063 [DOI] [Google Scholar]
- Risser, H. J., Hetzel-Riggin, M. D., Thomsen, C. J., & McCanne, T. R. (2006). PTSD as a mediator of sexual revictimization: The role of reexperiencing, avoidance, and arousal symptoms. Journal of Traumatic Stress, 19(5), 687–698. [DOI] [PubMed] [Google Scholar]
- Rothbaum, B. O., Astin, M. C., & Marsteller, F. (2005). Prolonged exposure versus eye movement desensitization and reprocessing (EMDR) for PTSD rape victims. Journal of Traumatic Stress, 18(6), 607–616. [DOI] [PubMed] [Google Scholar]
- Rothbaum, B. O., Foa, E. B., Riggs, D. S., Murdock, T., & Walsh, W. (1992). A prospective examination of post traumatic stress disorder in rape victims. Journal of Traumatic Stress, 5(3), 455–475. [Google Scholar]
- Vickerman, K. A., & Margolin, G. (2009). Rape treatment outcome research: Empirical findings and state of the literature. Clinical Psychology Review, 29(5), 431–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts, B. V., Schnurr, P. P., Mayo, L., Young-Xu, Y., Weeks, W. B., & Friedman, M. J. (2013). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. Journal of Clinical Psychiatry, 74(6), 541–550. [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2018). International classification of diseases and related mental health problems (11th Revision). Geneva: WHO. [Google Scholar]


