Abstract
Background and purpose — Clinical care pathways for knee osteoarthritis (OA) are not always in line with clinical guidelines. We investigated (1) the patient-perceived quality of OA management, (2) which physiotherapist-delivered treatments patients with knee OA have attempted, and (3) patients’ expected subsequent treatment, at the time of referral to an orthopedic surgeon.
Patients and methods — This cross-sectional study included all patients with scheduled first-time appointments for knee OA at an orthopedic outpatient clinic from April 2017 to February 2018. Postal questionnaires included the 16-item OsteoArthritis Quality Indicator (OA-QI) questionnaire and questions about physiotherapist-delivered treatment for knee OA.
Results — 517 of 627 (82%) eligible patients responded. Responders’ (63% female) mean age was 67 years. The mean pass rate for the 16 independent quality indicators was 32% (8–74%). Sub-grouped into 4 categories, pass rates for independent quality indicators ranged from 16–52% regarding information, 9–50% regarding pain and functional assessment, 8–35% regarding referrals, and 16–74% regarding pharmacological treatment. While half of responders felt informed of physical activity benefits, only one-third had consulted a physiotherapist during the past year. Commonest physiotherapist-delivered treatments were exercise therapy for 22% and participation in the Good Life with osteoArthritis in Denmark (GLA:D) program for12% of responding patients. 65% expected surgery as subsequent treatment.
Interpretation — Patients with knee OA are undertreated in primary care in Denmark; however, our findings may only reflect healthcare settings that are comparably organized. Our results call for better structure and uniform pathways for primary care knee OA treatment before referral to an orthopedic surgeon.
According to national and international clinical guidelines, first-line treatment strategies for knee osteoarthritis (OA) should have been offered prior to referral for knee replacement surgery (Danish Health Authority 2012, American Academy of Orthopaedic Surgeons 2013, Fernandes et al. 2013, National Clinical Guideline Centre 2014, Bannuru et al. 2019).
In Scandinavia, several implementation strategies have been undertaken to optimize the adherence to clinical guideline recommendations for non-operative treatment of OA (Thorstensson et al. 2015, Skou and Roos 2017, Moseng et al. 2019). In Denmark, the focus on patient education and exercise has been strengthened with the physiotherapist-led treatment program Good Life with Osteoarthritis in Denmark (GLA:D) that was launched in 2013. Results from the GLA:D registry are promising and show that patients experience pain relief, and improved physical function and quality of life after attending the program (Skou and Roos 2017). Clarifying what patients expect from their subsequent treatment may help understand what drives patients to seek referral to an orthopedic surgeon. We therefore (1) evaluated the patient-perceived quality of OA management, (2) described which physiotherapist-delivered treatments patients with knee OA have attempted, and (3) described the patients’ expectations of their subsequent treatment, at the point in time when patients are referred to an orthopedic surgeon in Denmark.
Patients and methods
We followed the STROBE guidelines for the reporting of this study. In this cross-sectional study, we consecutively included patients from 1 outpatient orthopedic department at a public hospital in Denmark. The inclusion criterion was patients having been referred for first-time appointments with an orthopedic surgeon for an assessment of knee OA. Patients unable to speak or read Danish and patients who cancelled their consultation were excluded. In the period March 2018 to February 2019, patients were sent a postal invitation and were asked to respond to a self-reported questionnaire and return this in a pre-stamped envelope before the appointment with the orthopedic surgeon.
Questionnaire
The questionnaire included the patient-reported OsteoArthritis Quality Indicator questionnaire (OA-QI). The 17-item OA-QI was developed in 2010 by Østerås et al. (2013, 2015), who found it to have acceptable validity and moderate reliability in patients with knee, hip, or hand OA. The OA-QI includes quality indicators related to patient education and information, assessment of pain and function, referrals, and pharmacologic treatment for OA. For this study, we adjusted the OA-QI to specifically reflect knee OA and removed the item regarding referral to an orthopedic surgeon.
We further asked about the number of physiotherapy consultations for knee OA the patient had attended during the past year. Patients who had consulted a physiotherapist were asked which types of treatments they had received from a predefined list and could add other treatments in free text, if relevant. Patients also responded to a question about their expectations of subsequent treatment following the consultation with the orthopedic surgeon. The following 6 response options were given: surgical intervention, exercise therapy recommendation, weight loss recommendation, pain intervention recommendation, no further treatment recommended, or other, with the opportunity to expand on other expectations in free text.
The patients’ knee pain and functional limitations due to knee problems were measured using the Oxford Knee Score (OKS). The OKS was developed in 1998 as an outcome measure for people having total knee replacement, and its reliability and validity characteristics were later confirmed in non-operatively treated patients with knee OA. The 12 items are each scored from 0 to 4, summed to a total score of 0 (worst) to 48 (best) (Dawson et al. 1998). Additionally, patients reported their average knee pain intensity during the past week on a 0–100 mm VAS scale ranging from no pain to worst pain imaginable. Finally, patient demographics—height, weight, age, education level, employment status, smoking, residential status, comorbidities, and symptom duration—were collected.
The degree of radiographic OA was evaluated for patients with routinely obtained anteroposterior, weight-bearing radiographs available, and classified with the Kellgren and Lawrence (KL) classification system, ranging from grade 0 to 4 OA. For patients who reported problems with both knees, the most severe KL grade was recorded.
Pilot study
To test the feasibility of the questionnaire, we conducted a pre-test of the questionnaire on 6 patients who completed the questionnaire in the waiting room, prior to their consultation with an orthopedic surgeon. The patients were observed while completing the questionnaire, followed by a semi-structured interview to assess the feasibility, comprehensibility, and relevance of the questions. The time to complete the questionnaire ranged from 9 to 20 minutes. We subsequently conducted a pilot study to test the feasibility of the data collection procedure. Of 114 patients who were sent a postal questionnaire, only 52 (46%) responded and 3 items had more than 10% missing responses. Based on the pilot study, we made smaller wording edits to the items with large degrees of missing items.
Statistics
Data are presented as mean (SD) for normally distributed continuous data and median with 25th and 75th quantiles for non-normally distributed data. Categorical data are presented as numbers and percentages. Results from the OA-QI are reported as pass rates for each of the 16 quality indicators separately, and as summary pass rates across all quality indicators for each patient, as described in the original publication. Separate quality indicator pass rates were calculated as the percentage of patients responding “yes” out of the total number responding either “yes” or “no,” combined, taking the relevance of the quality indicator into account. Summary pass rates for each individual patient were calculated as the percentage of indicators with the response “yes” out of the total number of indicators with responses “yes” or “no,” combined (Østerås et al. 2013). Statistical analyses were performed with the statistical package R, version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria).
Ethics, funding, and potential conflicts of interest
The study was approved by the national data protection agency (Journal number AHH-2015-093). Since only questionnaire-based data were used, ethical committee approval was not required. The study was conducted in accordance with the WMA Declaration of Helsinki. The study was funded by the Danish Rheumatism Association and by the Orthopaedic Department at the Copenhagen University Hospital Hvidovre. ER is co-founder of GLA:D. The authors declare no other potential conflicts of interest.
Results
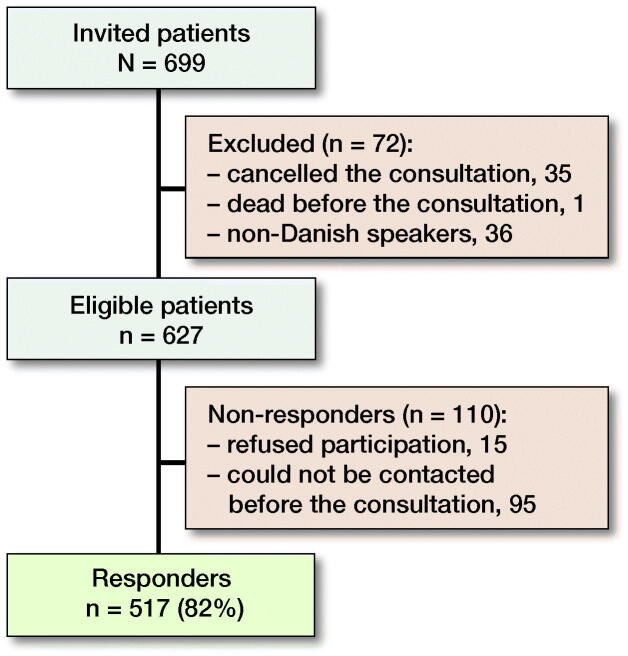
517 of 627 (82%) eligible patients responded (Figure 1). The responders had a mean (SD) age of 67 (11) and 63% were female. In comparison, the non-responders’ mean (SD) age was 63 (12) years and 65% were female (Table 1).
Figure 1.
Flow diagram.
Table 1.
Patient characteristics. Values are frequency (%) unless otherwise specified
| Factor | Responders | Respons |
|---|---|---|
| Age, mean (SD) | 515 | 67 (11) |
| Female | 517 | 324 (63) |
| BMI, mean (SD) | 503 | 30 (5) |
| Education level | 498 | |
| Primary | 129 (26) | |
| Secondary | 141 (28) | |
| Tertiary | 228 (46) | |
| Current smoker | 515 | 74 (14) |
| Occupation | 514 | |
| Working full-time or part-time | 141 (27) | |
| Unemployed | 28 (5) | |
| Sick leave | 23 (4) | |
| Retired | 322 (63) | |
| Living alone | 517 | 208 (40) |
| Comorbidities | 517 | |
| None | 105 (20) | |
| Heart disease | 54 (10) | |
| Hypertension | 231 (45) | |
| Cerebral vascular disease | 18 (3) | |
| Peripheral artery disease | 62 (12) | |
| Lung disease | 55 (11) | |
| Diabetes | 58 (11) | |
| Kidney disease | 13 (3) | |
| Neurologic disease | 9 (2) | |
| Liver disease | 7 (1) | |
| Cancer within 5 years | 35 (7) | |
| Depression | 39 (8) | |
| Spinal arthritis or other spinal condition | 172 (33) | |
| Other arthritides | 92 (18) | |
| Knee OA duration | 512 | |
| 0–6 months | 43 (8) | |
| 6–12 months | 49 (10) | |
| 1–2 years | 73 (14) | |
| 2–5 years | 105 (21) | |
| 5–10 years | 122 (24) | |
| > 10 years | 120 (23) | |
| Knee pain (VAS) median (IQR) | 486 | 7 (5–8) |
| OKS, mean (SD) | 501 | 23 (8) |
| KL grade | 459 | |
| 0 | 1 (0) | |
| 1 | 29 (6) | |
| 2 | 89 (19) | |
| 3 | 171 (37) | |
| 4 | 169 (37) |
The number of missing items varied across the variables, thus the specific numbers of included observations are presented.
Abbreviations: BMI: body mass index, OA: osteoarthritis,
VAS: visual analogue scale, OKS: Oxford Knee Score,
KL grade: Kellgren and Lawrence classification system.
Quality indicators for knee OA treatment
The mean pass rate for the 16 independent quality indicators was 32% (8–74) (Table 2). Sub-grouped into 4 categories, the pass rates were 16–52% related to OA information, 9–50% related to assessment of pain and function, 8–35% related to referrals, and 16–74% related to pharmacological treatment (Table 2). The median (25th to 75th quantile) summary pass rate, i.e., the percentage of fulfilled quality indicators overall per patient, was 29% (18–50). 1% of patients reported “yes” to all the quality indicators that were relevant to them, while 6% had not achieved any of the relevant quality indicators.
Table 2.
Patient self-reported quality indicator pass rates for knee osteoarthritis treatment during the past year at the point of referral to an orthopedic surgeon for an evaluation of surgical appropriateness. Values are frequency (%) unless otherwise specified
| OA-QI (n = 508)a | Yes | No | Missing | Pass rate (95% CI)b | |
|---|---|---|---|---|---|
| Do not remember | |||||
| 1. Information about disease development | 128 (25) | 319 (63) | 50 (10) | 11 (2) | 29 (25–33) |
| 2. Information about treatment modalities | 148 (29) | 320 (63) | 23 (5) | 17 (3) | 32 (28–36) |
| 3. Information about self-management | 72 (14) | 390 (77) | 28 (6) | 18 (4) | 16 (13–19) |
| 4. Information about lifestyle adaptation | 100 (20) | 364 (72) | 23 (5) | 21 (4) | 22 (18–26) |
| 5. Information about physical activity | 247 (49) | 228 (45) | 15 (3) | 18 (4) | 52 (48–56) |
| 6. Referral for physical activity | 167 (33) | 310 (61) | 12 (2) | 19 (4) | 35 (31–39) |
| Not overweight | |||||
| 7. Information about weight reduction | 113 (22) | 247 (49) | 140 (28) | 8 (2) | 31 (27–36) |
| 8. Referral for weight reduction | 29 (6) | 326 (64) | 139 (27) | 14 (3) | 8 (6–11) |
| Do not have this problem | |||||
| 9. Assessment of problems in daily activities | 117 (23) | 319 (63) | 48 (9) | 24 (5) | 27 (23–31) |
| 10. Assessment for walking aid | 72 (14) | 335 (66) | 84 (17) | 17 (3) | 18 (14–22) |
| 11. Assessment for other daily living aids | 33 (6) | 345 (68) | 109 (21) | 21 (4) | 9 (6–12) |
| Do not have pain | |||||
| 12. Assessment of pain | 242 (48) | 241 (47) | 11 (2) | 14 (3) | 50 (46–55) |
| 13. Recommended paracetamol | 349 (69) | 125 (25) | 11 (2) | 23 (5) | 74 (69–77) |
| 14. Offered stronger pain killers | 182 (36) | 276 (54) | 23 (5) | 27 (5) | 40 (35–44) |
| 15. Information about NSAIDS (side) effects | 219 (43) | 232 (46) | 29 (6) | 28 (6) | 49 (44–53) |
| 16. Offered joint injection | 72 (14) | 386 (76) | 25 (5) | 25 (5) | 16 (13–19) |
| 17. Referral to orthopedic surgeon | Not applicable in this study | ||||
Abbreviations: OA-QI: OsteoArthritis Quality Indicator questionnaire.
9 of the 517 responders had not answered any of the questions in the OA-QI.
Pass rates were calculated as the percentage of patients responding “yes” out of the total number responding either “yes” or “no.”
Physiotherapist-delivered treatment
184 of 494 (37%) responders who completed the question regarding the number of physiotherapy consultations during the past year had had at least 1 consultation. Of these, 66 had seen the physiotherapist 1 to 3 times (Table 3).
Table 3.
Number of physiotherapy consultations due to knee osteoarthritis received during the past year prior to consulting with an orthopedic surgeon
| Physiotherapy consultationsa | n (%) |
|---|---|
| None | 309 (63) |
| 1–3 | 66 (13) |
| 4–6 | 31 (6) |
| 7–9 | 30 (6) |
| 10–12 | 21 (4) |
| > 12 | 36 (7) |
23 of 517 did not respond to this question (n = 494).
The 2 most frequently reported physiotherapist-delivered treatments were “any type of exercise therapy” for 22% and participation in the GLA:D program (the combination of patient education and supervised group-based neuromuscular exercise therapy) for 12% of the 513 patients who had completed the question. Furthermore, OA information, stretching, and massage where each reported by 9% of the responding patients (Table 4). Most patients had received several treatments in combination.
Table 4.
Type of physiotherapist-delivered treatments for knee osteoarthritis during the past year
| Percentage ofa |
|||
|---|---|---|---|
| Physiotherapist-delivered treatment | n | total responders (n = 513)b | those consulting a physiotherapist (n = 184) |
| GLA:D participation | 61 | 12 | 33 |
| OA information | 44 | 9 | 24 |
| Any type of exercise | 114 | 22 | 62 |
| Stretching | 45 | 9 | 24 |
| Massage | 47 | 9 | 26 |
| Electrotherapy | 24 | 5 | 13 |
| Acupuncture | 37 | 7 | 20 |
| Insoles | 34 | 7 | 18 |
| Gait assessment | 17 | 3 | 9 |
| Other | 43 | 8 | 23 |
Abbreviations: GLA:D: Good Life with Osteoarthritis in Denmark (the combination of patient education and supervised group-based exercise therapy).
Percentages do not add up to 100% across the treatment types because some patients received several treatments in combination.
4 patients out of the total 517 responders did not answer the question about type of physiotherapist-delivered treatments.
Patients’ expectations of treatment suggested by the orthopedic surgeon
Prior to their consultation with the orthopedic surgeon, the majority (65%) expected to be offered a surgical intervention, followed by expecting to be recommended exercise therapy (30%), pain management (22%), or weight loss intervention (15%) (Table 5).
Table 5.
Patients’ expectations of their subsequent treatment after consulting with the orthopedic surgeon
| Expectationsa | n (%)b |
|---|---|
| Surgery | 324 (65) |
| Exercise | 150 (30) |
| Weight loss | 76 (15) |
| Pain management | 108 (22) |
| No treatment | 22 (4) |
| Other | 101 (20) |
20 of 517 did not respond to this question (n = 497).
Percentages do not add up to 100% because patients may have responded to several expectations.
Discussion
We investigated the quality of care delivered in primary care for patients with knee OA, prior to referral for an orthopedic surgeon. We found that while quality indicators regarding pharmacological pain relief were fulfilled by one-third to two-thirds, most quality indicators relating to patient information, exercise, weight loss, and functional assessment were fulfilled for at most one-third of patients. Of special note is that less than 1 in 3 felt informed about the way the OA disease develops, possible treatment modalities, how to self-manage their disease, and how to change their lifestyle. Furthermore, even though 1 in 2 felt informed about the importance of physical activity and exercise, only 1 in 3 had consulted a physiotherapist during the past year before referral to an orthopedic surgeon.
Our results support prior studies reporting suboptimal quality of knee OA care in Denmark and other countries. In a study of hand, knee, and hip OA in a primary care setting in 1 municipality in Norway, the median summary pass rate was 27%, which is comparable to our finding of 29% (Østerås et al. 2013). Our results further confirm the results from the smaller (n = 49) Danish knee OA cohort in a study comparing the quality of knee OA care across 4 European countries (Østerås et al. 2015). In that study, quality indicators regarding OA information were fulfilled by only 17% to 38% in the Danish cohort, which is comparable to the 16% to 32% from our study. Furthermore, Østerås et al. found that around half the responders had received referrals for supervised exercise (i.e., physiotherapy) in Norway, Portugal, and the UK, while that proportion was only 21% in Denmark. In comparison, in our study, only 35% were referred, even though they were at a later stage of disease. These findings highlight that access to physiotherapists should be facilitated since physiotherapists have a core role in prescribing and supervising exercise therapy for patients with knee OA. A financial barrier may be present for patients in Denmark. Although patients can directly access private physiotherapy clinics they then have to pay the full treatment cost, while those with a referral from a general practitioner are reimbursed approximately 40%.
Skou et al. (2015b) suggested that knee replacement can be postponed, even in those with moderate to severe OA, and also that patients undergoing a structured and optimized non-operative treatment program may be better prepared for a surgical decision. In their clinical trial, comparing an optimized non-operative treatment strategy with an optimized non-operative treatment strategy combined with total knee replacement, only 26% of those in the non-operative group subsequently decided to undergo surgery during the following 12 months. Rheumatologists, orthopedic surgeons, and general practitioners considered that a barrier to referring patients with OA to physiotherapy is that patients receive non-evidence-based passive treatment modalities, instead of exercise therapy (Selten et al. 2017). Correspondingly, only 2 in 3 patients in our study had received exercise as part of their physiotherapy treatment. 10 years ago, Holden et al. (2009) found that physiotherapists in the UK were concerned about the real benefits of exercise for knee OA, and moreover many believed that exercise would potentially be harmful for the osteoarthritic joint. More recent studies have, however, established that patients with severe radiographic OA grades can also achieve pain relief and functional improvement with exercise (Juhl et al. 2014, Skou et al. 2015a), and even large exercise loads do not seem to be harmful for the cartilage in the osteoarthritic knee (Bricca et al. 2018). Even though a more recent report suggests that physiotherapists are convinced by this contemporary knowledge (Spitaels et al. 2016), another study pointed at several healthcare providers doubting the real benefits of exercise (Selten et al. 2017). Furthermore, lack of support, or conflicting information from different healthcare providers, were found to be important barriers for patients to adhere to exercise therapy (Kanavaki et al. 2017). Motivating patients to exercise is challenging if they believe that their joint is worn down, which may partly explain our finding of low adherence to exercise therapy. While providing patient education on OA and self-management strategies is crucial for long-term adherence, only 1 in 4 patients in our study had received information about OA from the physiotherapist. A lack of established self-management and patient education tools amongst physiotherapists (Holden et al. 2009) may explain why few patients experienced OA information as being part of the physiotherapist-delivered treatment. The GLA:D program does incorporate a structured approach and specific tools for patient education (Skou and Roos 2017); however, only 1 in 3 patients from our study who had consulted a physiotherapist had participated in the GLA:D program.
We found that 2 in 3 patients expected to be waitlisted for surgery at their consultation with the orthopedic surgeon. This may reflect that 1/3 of patients see the orthopedic surgeon as the OA expert providing a second opinion instead of a professional carrying out surgery. This proportion might have been higher had the OA education for general practitioners and physiotherapists been improved, and had the non-operative treatment strategy been optimized. This hypothesis is strengthened by our additional finding that 1 in 3 expected to be referred for exercise therapy. A commonly elaborated response to the question regarding expectations of the following consultation was that they hoped to “find out what is wrong with my knee” (data not shown). These statements may indicate that the patients had not received a clinical OA diagnosis in general practice and support the idea that the surgeon is seen as the OA expert.
Differences in healthcare systems across countries may limit the external validity of our findings. The generalizability is, however, strengthened by the high response rate of consecutively invited patients from a large-volume orthopedic department with a large area of uptake that includes both rural and urban settlement. Despite our consecutive approach, there is a risk of selection bias since non-responders were on average 4 years younger than the responders. A possible explanation could be that younger patients with knee problems often did not consider their OA diagnosis definitive, and therefore did not consider it relevant to answer the questionnaire. Further limitations involve a risk of recall bias (Basedow and Esterman 2015). Patients may have forgotten which specific type of physiotherapist-delivered treatment they had received, and the number of physiotherapy consultations. Furthermore, patients may have had previous 1st-time appointments due to their knee OA at other specialist centers than ours, or at our center due to OA in the opposite knee. However, we hypothesize that any previous specialist consultations would have led to an improved pass rate. Finally, there may be a discrepancy between the degrees of fulfilled quality indicators from the patients’ perspective, in comparison with the healthcare professional’s perspective. Quality assessment based on reviewing medical records is commonly used to reflect the professionals’ perspectives (Basedow and Esterman 2015). A shortcoming of this approach, however, is that it may lead to both under- or overestimating the usage of healthcare processes due to inaccurate information in the medical records (Luck et al. 2000).The self-reported OA-QI has demonstrated adequate content and construct validity (Østerås et al. 2013), and is a feasible option to capture patient-perceived quality of care.
In conclusion, patients with knee OA are undertreated in primary care; however, our findings may only reflect healthcare settings that are comparably organized. Only about 1/3 had consulted a physiotherapist during the last year, and only 1/4 were informed about the disease and its management options prior to seeing an orthopedic surgeon. Our results calls for better structure and uniform pathways for knee OA treatment in the primary sector before referral to an orthopedic surgeon. Future studies should investigate whether optimizing the quality of care in the primary health care sector has a positive effect on the outcomes of knee OA treatment across treatment sectors.
Acknowledgements
Conception and design: LHI, ER, AT. Collection and assembly of data: LHI, SS. Analysis: LHI. Interpretation of the data: LHI, ER, KG, SST, AT. Drafting of the manuscript: LHI, AT. Critical revision and final approval of the article: LHI, ER, KG, SST, AT.
The authors would like to thank all the patients for their time and effort in replying to our questionnaire. They further thank Fie Tillie Schlippe, Anne Birgitte Larsen, and Ina Hjortkjaer Stark for contributing to the data collection.
Acta thanks Thea Vliet Vlieland for help with peer review of this study.
References
- American Academy of Orthopaedic Surgeons . Treatment of osteoarthritis of the knee: evidence-based guideline, 2nd ed. Adopted by the American Academy of Orthopaedic Surgeons Board of Directors. Am Acad Orthop Surg; 2013. [DOI] [PubMed] [Google Scholar]
- Bannuru R R, Osani M C, Vaysbrot E E, Arden N K, Bennell K, Bierma-Zeinstra S M A, Kraus V B, Lohmander L S, Abbott J H, Bhandari M, Blanco F J, Espinosa R, Haugen I K, Lin J, Mandl L A, Moilanen E, Nakamura N, Snyder-Mackler L, Trojian T, Underwood M, McAlindon T E. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage 2019. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Basedow M, Esterman A. Assessing appropriateness of osteoarthritis care using quality indicators: a systematic review. J Eval Clin Pract 2015; 21(5): 782–9. [DOI] [PubMed] [Google Scholar]
- Bricca A, Struglics A, Larsson S, Steultjens M, Juhl C B, Roos E M. Impact of exercise therapy on molecular biomarkers related to articular cartilage and inflammation in people at risk of, or with established, knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Arthritis Care Res 2018; 26: S314–S15. [DOI] [PubMed] [Google Scholar]
- Danish Health Authority . Knaeartrose: nationale kliniske retningslinjer og faglige visitationsretningslinjer (Knee osteoarthritis: National clinical guidelines and visitation guidelines) [in Danish]; 2012.
- Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg 1998; 80(1): 63- 9. [DOI] [PubMed] [Google Scholar]
- Fernandes L, Hagen K B, Bijlsma J W J, Andreassen O, Christensen P, Conaghan P G, Doherty M, Geenen R, Hammond A, Kjeken I, Lohmander L S, Lund H, Mallen C D, Nava T, Oliver S, Pavelka K, Pitsillidou I, da Silva J A, de la Torre J, Zanoli G, Vliet Vlieland T P M. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis 2013; 72(7): 1125–35. [DOI] [PubMed] [Google Scholar]
- Holden M A, Nicholls E E, Young J, Hay E M, Foster NE. UK-based physical therapists’ attitudes and beliefs regarding exercise and knee osteoarthritis: Findings from a mixed-methods study. Arthritis Care Res 2009; 61(11): 1511–21. [DOI] [PubMed] [Google Scholar]
- Juhl C, Christensen R, Roos E M, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol 2014; 66(3): 622–36. [DOI] [PubMed] [Google Scholar]
- Kanavaki A M, Rushton A, Efstathiou N, Alrushud A, Klocke R, Abhishek A, Duda J L. Barriers and facilitators of physical activity in knee and hip osteoarthritis: a systematic review of qualitative evidence. BMJ Open 2017; 7:e017042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luck J, Peabody J W, Dresselhaus T R, Lee M, Glassman P. How well does chart abstraction measure quality? A prospective comparison of standardized patients with the medical record. Am J Med 2000; 108(8): 642–9. [DOI] [PubMed] [Google Scholar]
- Moseng T, Dagfinrud H, Østerås N. Implementing international osteoarthritis guidelines in primary care: uptake and fidelity among health professionals and patients. Osteoarthritis Cartilage 2019; 27:1138–47. [DOI] [PubMed] [Google Scholar]
- National Clinical Guideline Centre . Osteoarthritis care and management in adults. Clin Guidel CG177; 2014. [Google Scholar]
- Østerås N, Garratt A, Grotle M, Natvig B, Kjeken I, Kvien T K, Hagen K B. Patient-reported quality of care for osteoarthritis: development and testing of the osteoarthritis quality indicator questionnaire. Arthritis Care Res 2013; 65(7): 1043–51. [DOI] [PubMed] [Google Scholar]
- Østerås N, Jordan K P, Clausen B, Cordeiro C, Dziedzic K, Edwards J, Grønhaug G, Higginbottom A, Lund H, Pacheco G, Pais S, Hagen K B. Self-reported quality care for knee osteoarthritis: comparisons across Denmark, Norway, Portugal and the UK. RMD Open 2015; 1(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selten E M H, Vriezekolk J E, Nijhof M W, Schers H J, Van Der Meulen-Dilling R G, Van Der Laan W H, Geenen R, Van Den Ende C H M. Barriers impeding the use of non-pharmacological, non-surgical care in hip and knee osteoarthritis: the views of general practitioners, physical therapists, and medical specialists. J Clin Rheumatol 2017; 23(8): 405–10. [DOI] [PubMed] [Google Scholar]
- Skou S T, Roos E M. Good Life with osteoArthritis in Denmark (GLA:DTM): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet Disord 2017; 18(1): 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skou S T, Derosche C, Andersen M M, Rathleff M S, Simonsen O. Nonoperative treatment improves pain irrespective of radiographic severity. Acta Orthop 2015a; 86(4): 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skou S T, Roos E M, Laursen M B, Rathleff M S, Arendt-Nielsen L, Simonsen O, Rasmussen S. A randomized, controlled trial of total knee replacement. N Engl J Med 2015b; 373(17): 1597–606. [DOI] [PubMed] [Google Scholar]
- Spitaels D, Hermens R, Van Assche D, Verschueren S, Luyten F, Vankrunkelsven P. Are physiotherapists adhering to quality indicators for the management of knee osteoarthritis? An observational study. Man Ther 2016; 27:112–23. [DOI] [PubMed] [Google Scholar]
- Thorstensson C A, Garellick G, Rystedt H, Dahlberg L E. Better management of patients with osteoarthritis: development and nationwide implementation of an evidence-based supported osteoarthritis self-management programme. Musculoskeletal Care 2015; 13(2): 67–75. [DOI] [PubMed] [Google Scholar]