Abstract
Objective
Women have a greater overall risk of developing posttraumatic stress disorder (PTSD) than men after exposure to trauma. In addition to gender, other sociodemographic factors have been identified as risk factors for PTSD; however, research has typically examined these factors separately. Age has been found to contribute to the development of psychiatric disorders, and both linear and curvilinear relationships have been reported between age and risk of developing PTSD. Recent research has suggested that this relationship may vary depending on gender.
Method
We performed a secondary analysis of data from a prospective study of 287 (164 men, 123 women) motor vehicle accident (MVA) patients (aged 18–81) who completed clinical interviews 6 weeks, 6 months, and/or 1 year after an MVA.
Results
Overall, women developed more severe PTSD symptoms than men; however, gender differences were small in the young (18–24 years) and the old (55 and older) groups. In women, age was not associated with PTSD symptoms at 6-weeks and 6-months; however, age was curvilinearly associated with PTSD severity at 1-year post-MVA such that middle-aged women reported greater symptom severity than younger and older women. Prior trauma exposure and social support mediated this relationship. In men, PTSD severity was not associated with age, but was related to income and social support.
Conclusions
These findings highlight age-based subgroups of women at elevated risk for PTSD following a traumatic injury and suggest that psychosocial intervention with middle-aged women following trauma exposure may help reduce the risk of persistent PTSD symptoms.
Keywords: posttraumatic stress disorder, gender, age, motor vehicle accident
Women have a greater overall risk (11 – 20%) for developing posttraumatic stress disorder (PTSD) than men (4 – 8%) following trauma exposure (Breslau, Peterson, & Schultz, 2008; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Although a number of sociodemographic and trauma-related factors have been identified as risk factors for developing PTSD (e.g., age, marital status, race, income, and type of trauma), these factors have been less consistently associated with PTSD risk than has gender (Acierno, Ruggiero, Kilpatrick, Resnick, & Galea, 2006; Kessler et al., 1995; Roberts, Gilman, Breslau, Breslau, & Koenen, 2011). Research has often examined the predictive value of these risk factors individually; however, it is likely that risk factors interact to predict PTSD. For instance, gender and trauma type interact in the prediction of PTSD; women are at greater risk for PTSD than men following disaster or fire, accident, non-sexual assault, and childhood physical and sexual abuse, but not after adult sexual assault (Kessler et al., 1995; Koenen & Widom, 2009; Tolin & Foa, 2006). Examination of the extent to which gender interacts with other sociodemographic factors to influence risk for PTSD may increase the ability to identify and target treatment approaches for high-risk trauma victims.
Age is associated with a wide range of psychological processes including the development of psychiatric disorders. With respect to PTSD risk, epidemiological studies have shown that the median age of onset of PTSD was 23 years old with an interquartile range of 15 – 39 years (Kessler et al., 2005). However, this is undoubtedly confounded by age-related risk of trauma exposure, as the age associated with highest risk for trauma exposure is 16 – 20 years (Breslau et al., 1998). Studies examining PTSD risk in different age groups following a specific similar traumatic event allow for estimating age-related risk for PTSD without this confound. However, findings of such studies are inconsistent (Acierno et al., 2006; Adams & Boscarino, 2006; Chossegros et al., 2011; Kun, Tong, Liu, Pei, & Luo, 2013; Norris, Kaniasty, Conrad, Inman, & Murphy, 2002). Methodological differences (e.g., timing of assessment, age ranges of participants) as well as other factors that interacted with age might have contributed to the inconsistent findings.
Research has suggested that gender may interact with age in predicting the development of a number of psychiatric disorders (Dekker et al., 2007; Eranti, MacCabe, Bundy, & Murray, 2013; Perlis et al., 2009). However, for PTSD, this has largely been extrapolated from studies examining PTSD prevalence rates in trauma-exposed samples differing by age. Two studies (Creamer & Parslow, 2008; Ditlevsen & Elklit, 2010) that included participants older than age 65 found lower prevalence of PTSD in older versus younger age groups for both genders. Similarly, the smallest gender differences in prevalence and severity of PTSD were found in the older age groups (the age 65 and older group in Creamer & Parslow, 2008; the age 66 – 70, 71 – 75, 76 – 80 groups in Ditlevsen & Elklit, 2001). However, as these studies did not consider time since trauma, it is also possible that older adults had a longer time to recover from the traumatic event (Creamer & Parslow, 2008).
Few studies have examined the interaction between gender and age while controlling for the amount of time elapsed since trauma exposure. A study of adult victims (age 18 – 88) of natural disasters living in the United States, Mexico, and Poland found that, across sites, women were at greater risk of developing PTSD than men; however, there were cultural differences in the way that gender and age interacted (Norris et al., 2002). An age × gender interaction was found only in the Polish sample 1 year after a flood, such that middle-aged women exhibited more PTSD symptoms than younger and older women, while in men, the relationship of age to PTSD was positive and linear. In the U.S. sample, an inverted U-shaped relationship between age and PTSD symptoms was found regardless of gender six months after Hurricane Andrew (Norris et al., 2002). Norris and colleagues (2002) speculated that the greater familial and societal responsibilities imposed on middle-aged adults (i.e., the burden perspective) contributed to the higher symptoms. In the Mexican sample, age was negatively and linearly associated with PTSD symptoms regardless of gender at 6-months post-hurricane. The burden perspective could also explain this finding as young Mexican adults in poor communities tend to take on greater financial responsibilities to support their children and family of origin (Norris et al., 2002). In contrast to the victims of natural disasters in Norris et al’s study, a Danish study of adults (age 18 - 95) exposed to the explosion of a firework factory (Christiansen & Elklit, 2008) did not find associations between age and PTSD severity in either gender 1 year after the explosion. These cultural differences suggest that psychosocial factors associated with age and/or gender might have influenced the development of PTSD symptoms.
A number of other risk and resilience factors have been found to predict PTSD including social support (Brewin, Andrews, & Valentine, 2000; Ozer, Best, Lipsey, & Weiss, 2008), trauma history (Cougle, Resnick, & Kilpatrick, 2009; Delahanty, Raimonde, Spoonster, & Cullado, 2003; Liu et al., 2017), and household income (Breslau et al., 1998; Kun et al., 2013; Naeem et al., 2011). We have previously reported that lower social support (Gabert-Quillen et al., 2012), lower household income (Irish et al., 2011) and greater number of types of prior trauma (Gabert-Quillen et al., 2012) were associated with higher PTSD symptoms following an MVA. Each of these risk factors may also impact the extent to which gender and age interact to predict risk for PTSD.
For instance, women are more likely to seek social support than men as a coping strategy (Tamres, Janicki, & Helgeson, 2002), and associations between perceived social support and the development of PTSD symptoms tend to be stronger in women than men (Andrews, Brewin, & Rose, 2003; Israel-Cohen & Kaplan, 2016). A longitudinal epidemiological study in Australia found that greater perceived social support more strongly predicted better mental health in younger compared to older individuals in both genders (Milner, Krnjacki, & LaMontagne, 2016). The Socioemotional Selectivity Theory posits that, as time left to live becomes shorter, older adults change their priorities from preparing for the future to maintaining their emotional well-being (Charles & Carstensen, 2010). Further, the Socioemotional Selectivity Theory predicts that older adults maintain their emotional well-being by selectively engaging in important relationships rather than peripheral ones.
Although women are at lower overall risk for trauma exposure than men, they are more likely to have been previously exposed to traumas associated with increasing risk for PTSD upon subsequent trauma exposure. For instance, women are more likely to experience rape, sexual assault, intimate partner violence, and childhood physical abuse than men (Benjet et al., 2016; Breslau et al., 1998; Jonas et al., 2014; Kessler et al., 1995; Liu et al., 2017). The Socioemotional Selectivity Theory also predicts that memories of older people are biased toward positive rather than negative information (Charles & Carstensen, 2010). Thus, it is possible that memories of prior traumas may be less salient in older individuals, and this may protect older adults from the typical increased risk associated with prior trauma history.
It is not known whether income and PTSD symptoms are differentially associated in men versus women. In the U.S., women’s median income is approximately 84% that of men’s although unemployment rates are similar between genders (U.S. Department of Labor, 2017a; U.S. Department of Labor, 2017b). In both genders, incomes are highest in age groups between 35 – 64 years old and lowest in young individuals (16 – 24 years old). Income gaps between genders are widest in the age groups with highest incomes (age 35 – 64) and narrower in younger groups. Although income levels are similar between middle-aged and older individuals, considering that middle-aged individuals are often financially supporting their families, older people may have more disposable financial resources which could cover additional financial needs following a traumatic event.
In sum, only a few studies of victims of natural and manmade disasters have examined interaction effects of gender and age on PTSD controlling for time since trauma, and those studies have produced mixed findings. Prior theory and research findings suggest that various psychosocial and other factors contribute to one’s vulnerability to traumatic stress and that the degree to which each factor affects risk for PTSD can vary by age and/or gender. Therefore, the purpose of the present study was to determine whether gender and age interacted to impact the development of PTSD. Further, we examined the extent to which psychosocial factors previously associated with PTSD impacted these interaction effects. To accomplish these goals, we examined the impact of age, gender, and their interaction on PTSD symptoms after an MVA. Given prior findings and the Socioemotional Selectivity Theory suggesting smaller gender differences and resilience in older adults, we hypothesized that women would develop more severe PTSD symptoms than men across age groups except for the oldest age group (age 55 and older). We also examined how gender moderated the relationship between age and PTSD symptoms and whether the abovementioned psychosocial factors mediated the relationship. Given prior findings indicating curvilinear relationships (i.e., the American and Polish samples in Norris et al., 2002) as well as protective factors in old women (e.g., focus on emotional well-being) and young women (e.g., limited trauma history), we hypothesized that in women, age and PTSD symptoms would be curvilinearly associated with PTSD symptoms with higher PTSD symptoms in middle-aged individuals. Further, we hypothesized that these relationships would be mediated by psychosocial factors including income, social support, and trauma history. Considering the relatively overall favorable characteristics of risk and protective factors in men, we hypothesized that age and PTSD symptoms would not be related in men.
Methods
Participants
Participants were 287 (164 men and 123 women) motor vehicle or motorcycle accident victims (aged 18 – 81) admitted to one of two level-1 trauma centers in the Midwestern United States who completed at least one PTSD assessment at 6 weeks, 6 months, and/or 1 year following their accident. Participant characteristics are presented in Table 1.
Table 1.
Participant Characteristics
| Women | Men | ||||
|---|---|---|---|---|---|
|
|
|||||
| Characteristic | M | SD | M | SD | t |
| Age (years) | 39.93 | 15.29 | 37.41 | 15.00 | 0.84 |
| Injury severity score | 7.48 | 6.54 | 7.47 | 6.16 | 0.01 |
| Number of prior trauma types | 3.24 | 1.99 | 3.11 | 1.82 | 0.55 |
| ISEL scores | 41.07 | 5.39 | 40.04 | 6.09 | 1.63 |
| 6-week CAPS total score | 31.90 | 24.79 | 21.77 | 16.93 | 3.85*** |
| 6-month CAPS total scorea | 26.40 | 21.44 | 14.42 | 14.57 | 5.03*** |
| 1-year CAPS total scorea | 23.68 | 23.89 | 14.96 | 13.71 | 2.78** |
|
| |||||
| n | % | N | % | X2 | |
|
| |||||
| Race: White | 114 | 92.7 | 149 | 90.9 | 0.31 |
| Marital status: | 6.33* | ||||
| Single | 41 | 33.6 | 70 | 42.9 | |
| Married/long term live-in | 50 | 41.0 | 70 | 42.9 | |
| Previously married | 31 | 25.4 | 23 | 14.1 | |
| Income | 14.76** | ||||
| $20,000 or less | 62 | 52.5 | 47 | 32.0 | |
| $20,001 - $40,000 | 41 | 34.7 | 60 | 40.8 | |
| $40,001 - $60,000 | 8 | 6.8 | 27 | 18.4 | |
| $60,001 or greater | 7 | 5.9 | 13 | 8.8 | |
Note. N = 287.
p < .050.
p < .010.
p < .001.
Scores were square-root transformed before t-tests were performed. ISEL = Interpersonal Support Evaluation List. CAPS = Clinician Administered PTSD Scale for DSM-IV.
Measures
PTSD Symptoms
The Clinician Administered PTSD Scale for DSM-IV (CAPS: Blake et al., 1995) is a structured interview that assesses current and lifetime PTSD symptom severity and diagnostic status. The frequency and intensity of each of the 17 DSM-IV PTSD symptoms experienced during the past month in relation to the MVA were rated on 5-point scales ranging from 0 [never (frequency); none (intensity)] to 4 (daily or almost daily; extreme). A symptom was considered to be present when the frequency rating was 1 or greater and the intensity rating was 2 or greater (Blake et al., 1995). The sum of frequency and intensity scores of the 17 items was computed to index symptom severity. Internal consistency in this study was high (α = .92 at 6-weeks, .92 at 6-months, and .93 at 1-year post-MVA).
Trauma History
A modified Traumatic Stress Schedule (TSS: Norris, 1990) was used to assess lifetime trauma exposure. Seven of the 10 types of traumatic events in this modified form were from the original TSS (robbery, assault, rape, MVA, death of a loved one, fire, and other natural or manmade disaster); three additional types were added (i.e., witnessing someone seriously injured or killed, non-MVA accident, and an open-ended question for any other types of traumatic events experienced). The total number of different types of trauma reported was computed to index lifetime trauma load.
Injury Severity
The injury severity score (ISS: Baker, O’Neill, Haddon, & Long, 1974) was obtained from participants’ medical records. An ISS is computed by summing the squares of the highest injury severity grade of the three most severely injured areas of the body. It ranges from 0 to 75 with higher scores indicating more severe injury.
Social Support
Perceived availability of social support was measured with the Interpersonal Support Evaluation List (ISEL: Cohen, Mermelstein, Kamarck, & Hoberman, 1985), a 12-item measure of appraisal, tangible, and belonging aspects of social support. Items were scored on a 4-point scale (1 = definitely false to 4 = definitely true), and a total score of the 12 items was computed. Internal consistency in this study was high (α = .88).
Procedures
The following procedures were approved by the institutional review boards of Kent State University, Summa Health System, and Akron General Medical Center. A trauma nurse approached consecutive, eligible patients admitted to a level-1 trauma center following an MVA. The eligibility criteria included age 18 or older, a Glasgow Coma Scale (Teasdale & Jennett, 1974) score of 14 or greater, not being in a coma or unconscious for more than one hour before or during emergency room admission, being able to communicate in English, not being actively treated for any psychiatric disorders, and living within 25 miles of the hospital. The nurse administered the Mini Mental Status Exam (Folstein, Folstein, & McHugh, 1975) to ensure that the patient was capable of giving informed consent (required score ≥ 25). Subsequently, the study was described, and patients who expressed interest in participating were approached by a research staff member who provided further information about the study and obtained written informed consent. Eighty-seven percent of patients meeting inclusion criteria agreed to participate. During the in-hospital assessment, participants provided demographic information including age, gender, race, household income, and marital status.
At 6-weeks, 6-months, and 1-year post-MVA, a clinical psychology graduate student visited participants in their homes and administered the CAPS. The TSS and the ISEL were completed during the 6-week visit. Participants received $25 for completing each assessment.
Data Analysis
Analyses were conducted using SPSS 24 (IBM, Armonk, NY) with an alpha level of .05 (two-tailed). Missing data points of continuous variables (i.e., CAPS scores, injury severity, the number of prior trauma types, income, and social support) were imputed using an expectation-maximization algorithm. Square-root transformations were performed for 6-month and 1-year CAPS total scores to normalize the distributions. Gender differences were tested using t-tests for continuous variables and chi-square tests for categorical variables. Associations of participant characteristics with CAPS scores and age were examined using Pearson correlation coefficients (race: White = 1, non-White = 0). Household income was measured on a 9-point scale (ranging from 0 = ≤ $10,000 to 8 = > $70,001) and treated as a continuous variable. One-way ANOVAs were computed to examine associations between marital status and CAPS scores. To examine whether males and females differed in PTSD severity across different age groups, participants were divided into five age groups (18 – 24, 25 – 34, 35 – 44, 45 – 54, 55 and older) selected to be consistent with prior studies that examined age and PTSD associations, such as the National Comorbidity Survey (Bromet, Sonnega, & Kessler, 1998) and the Australian National Survey of Mental Health (Creamer & Parslow, 2008). An ANCOVA was performed for each age group covarying for household income, the number of prior trauma types, and ISEL scores. Partial η2 was obtained as an index for effect size. Partial η2 s of 0.01, 0.06, and 0.14 are considered “small,” “medium,” and “large” effects, respectively (Richardson, 2011). The moderating effects of gender on the relationship between continuous age (in years) and PTSD severity were examined with separate regression analyses predicting 6-week, 6-month, and 1-year CAPS scores from linear and quadratic age, gender (men = −1, women = 1), and interactions between gender and standardized linear and quadratic age (Age × Gender; Age2 × Gender). Following a significant Age2 × Gender effect, separate hierarchical regression analyses were performed for each gender. Specifically, linear age was entered at step 1 (Model 1), quadratic age at step 2 (Model 2), and income, the number of prior trauma types, and ISEL at step 3 (Model 3).
Results
Preliminary Analyses
Two hundred eighty [120 women, 160 men (7 of the total 287 participants missed the 6-week assessment)], 217 (99 women, 118 men), and 195 (92 women, 103 men) participants completed 6-week, 6-month, and 1-year CAPS assessments, respectively. Participants who dropped out between the 6-week and 6-month assessment were younger (M = 34.49 vs. 39.13 years, t = −2.20, p = .029) and more likely to be single (X2 = 9.52, p = .009) than those who were retained, but they were not different in terms of gender, race, income, injury severity, prior trauma exposure, social support, and 6-week CAPS scores. Participants who dropped out between the 6-month and 1-year assessment were also younger (M = 34.31 vs. 40.15, t = −2.06, p = .041), but they did not differ from those retained on any other variable.
Women were more likely to be previously married and less likely to be single than men (Table 1). Women also reported lower family income than men. Further, women had more severe PTSD symptoms at all assessment points than men Women’s mean CAPS total scores at all assessment points and men’s score at 6-weeks post-MVA were within the mild severity range, and men’s scores, on average, at the last two assessment points fell within the asymptomatic range. Women were more likely to meet diagnostic criteria for PTSD at 6-weeks (19.2% vs. 8.1%, X2 = 7.46, p = .006), 6-months (14.1% vs. 2.5%, p = .002), and 1-year (14.1% vs. 3.9%, p = .020) post-MVA than men. Because of the small percentage of participants who met diagnostic criteria for PTSD, especially in men, continuous CAPS total scores were used in all analyses.
Overall, higher household income was associated with lower CAPS scores in men, but not in women (Table 2). A greater number of prior trauma types was associated with higher CAPS scores at all assessment points in women; however, it was associated only with 6-month CAPS scores in men. Higher levels of social support were associated with lower CAPS scores in both genders at all assessment points. Injury severity, marital status, and race were not associated with CAPS scores in either gender. Given the pattern of associations between participant characteristics and CAPS scores, household income, social support, and the number of prior trauma types were controlled in appropriate analyses.
Table 2.
Correlations (r) Between Participant Characteristics and PTSD Symptoms and Age
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| 6-week CAPS | 6-month CAPS | 1-year CAPS | Age | 6-week CAPS | 6-month CAPS | 1-year CAPS | Age | |
|
|
||||||||
| n → | 120 | 99 | 92 | 123 | 160 | 118 | 103 | 164 |
|
| ||||||||
| Race | .02 | .07 | −.01 | .08 | .03 | −.11 | −.09 | .12 |
| Income | −.01 | −.15 | −.01 | .20* | −.18* | −.24** | −.24* | .49*** |
| Injury severity | −.09 | −.03 | .09 | .04 | −.01 | −.06 | −.06 | −.07 |
| No. of prior trauma types | .20* | .27** | .38*** | .16 | .10 | .22* | .04 | .17* |
| Social support | −.22* | −.26** | −.22* | −.06 | −.24** | −.21* | −.31*** | −.14 |
Note.
p < .050.
p < .010.
p < .001. Six-month and 1-year CAPS scores were square-root transformed. CAPS = Clinician Administered PTSD Scale for DSM-IV, PTSD = posttraumatic stress disorder.
Moderating Effects of Age on the Relationship between Gender and PTSD Symptoms
ANCOVAs comparing CAPS scores between genders in each age group revealed significantly higher 6-week CAPS score in women in all age groups [all ps ≤ .050, medium-to-large effects (η2 = .06 - .21)] except for the oldest group (age 55 and older). Figure 1a shows mean 6-week CAPS scores for men and women in each age group and partial η2. At 6-months post-MVA, women in the 25 – 34, 35 – 44, and 45 – 54 age groups had significantly higher CAPS scores compared with men [all ps ≤ .004, large effects (η2 = .19 - .29)] (Figure 1b); however, no gender differences were found in the youngest and the oldest groups. At 1-year post-MVA, the only significant gender difference in CAPS scores was for the 35 – 44 age group [p = .012, large effect (η2 = .14)] (Figure 1c).
Figure 1.
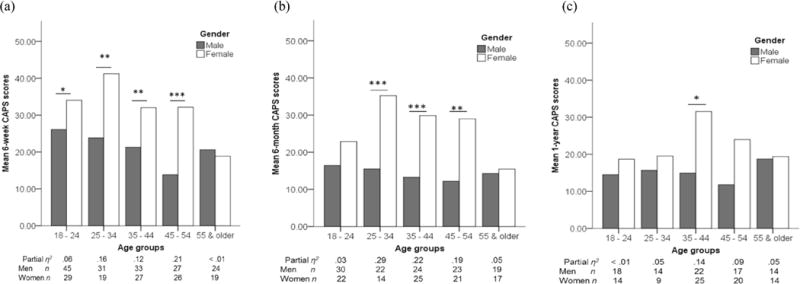
(a) Mean 6-week CAPS scores for men and women in each age group. (b) Mean 6-month CAPS cores for men and women in each age group. (c) Mean 1-year CAPS cores for men and women in each age group. * p < .05 ** p < .01. *** p < .001. CAPS = Clinician Administered PTSD Scale.
Moderating Effects of Gender on the Relationship between Age and PTSD Symptoms
Regression analyses predicting CAPS scores from gender, linear and quadratic age, Age × Gender, and Age2 × Gender were performed separately for each assessment point. Female gender significantly predicted higher CAPS scores at all assessment points (β = 0.25, p < .001 at 6 weeks; β = 0.34, p < .001 at 6 months; β = 0.19, p = .010 at 1 year) while linear or quadratic age did not. Age × Gender (β = 0.79, p = 023) and Age 2 × Gender (β = −0.77, p = 027) interactions significantly predicted 1-year, but not 6-week or 6-month, CAPS scores. To unpack the interaction effects, separate regression analyses were performed for men and women predicting 1-year CAPS scores from linear (Model 1), quadratic age (Model 2), and additional participant characteristics (Model 3). Results (Table 3) of Model 2 showed that quadratic age significantly predicted 1-year CAPS scores in women. Quadratic age did not predict 1-year CAPS scores in men. These results indicate that the association between age and CAPS scores was an inverted-U shape in women, but not in men. Adding income, the number of prior trauma types, and social support to the model (Model 3) resulted in non-significant findings for linear and quadratic age in women. The number of prior trauma types significantly positively predicted 1-year CAPS scores only in women, while income and social support significantly negatively predicted 1-year CAPS only in men. Social support only marginally predicted CAPS scores in women. For women, the differences in the coefficients for linear and quadratic age between Model 2 and Model 3 were tested using Clogg and colleagues’ (1995) method. Both coefficients changed more than three standard errors (Linear age: t = 3.27; Quadratic age: t = −3.46), suggesting that prior trauma exposure and social support mediated the curvilinear relationship.
Table 3.
Gender Specific Hierarchical Regression Analyses Predicting PTSD Severity at 1-Year Post-MVA
| Women (n = 92) | Men (n = 103) | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Predictor | β | Adjusted R2 | ΔR2 | β | Adjusted R2 | ΔR2 |
| Model 1 | −.01 | <.01 | −.01 | <.01 | ||
| Age | 0.04 | −0.21 | ||||
|
| ||||||
| Model 2 | .03 | .05* | −.01 | <.01 | ||
| Age | 1.04*a | −0.48 | ||||
| Age2 | −1.02*a | 0.47 | ||||
|
| ||||||
| Model 3 | .14 | .14** | .10 | .13** | ||
| Age | 0.40 | −0.10 | ||||
| Age2 | −0.44 | 0.22 | ||||
| Income | 0.03 | −0.24* | ||||
| Number of trauma | 0.34** | 0.01 | ||||
| Social support | −0.18+ | −0.27** | ||||
Note.
p < .010.
p < .050.
p = .069.
β can be greater than one when predictors are correlated each other (Deegan, 1978). MVA = motor vehicle accident; PTSD = posttraumatic stress disorder.
Discussion
The present study is the first investigation into interactions between gender and age in the development of PTSD symptoms in adult MVA patients. Results indicated that women aged 25-54 (including the 25 – 34, 35 – 44, and 45 – 54 age groups) developed more severe PTSD symptoms at 6-weeks and 6-months post-MVA compared with similarly aged men after controlling for potentially confounding factors (i.e., household income, social support, and the number of prior trauma types). Women aged 35 – 44 had higher PTSD symptoms than similarly aged men one year after the MVA. In the oldest group, men and women did not differ in PTSD symptom severity at any time point. In the youngest group, men and women did not differ in PTSD symptoms at 6-months and 1-year post-MVA. Further, in women, the association between age and PTSD symptom severity at 1-year post-MVA was curvilinear with elevated PTSD symptoms in the middle-age range. Age and PTSD symptoms were not associated in men. The curvilinear relationship between age and PTSD symptoms in women was partially explained by trauma history and social support.
Our finding that women developed more severe PTSD symptoms than men in all but the oldest and the youngest age groups partially supports our hypothesis that women would develop more severe PTSD symptoms than men in all but the oldest age group. It appears that the smaller gender differences in the oldest age group is mostly due to decreased PTSD symptom severity in women (Figure 1). The aforementioned protective psychosocial factors related to old age, such as placing a high priority on maintaining emotional well-being might have contributed to the older women’s resilience. Alternatively, age-related changes in gonadal hormone levels may also contribute to lower PTSD symptoms in older women. It has been suggested that fluctuations of gonadal hormone levels rather than hormone levels per se increase susceptibility to depressive and anxiety symptoms as they are more likely to develop during periods of significant hormonal fluctuation such as the premenstrual, postpartum, and menopausal transition periods (Lokuge, Frey, Foster, Soares, & Steiner, 2011; Ross & McLean, 2006; Yonkers, O’Brien, & Eriksson, 2008). It is possible that consistently low gonadal hormone levels in postmenopausal women would protect them from the impacts of traumatic stress. However, given the small – medium effect sizes found in the oldest group at 6-months and 1-year post-MVA, these non-significant gender differences could also be due to low statistical power.
A number of possible explanations can account for the smaller gender difference observed in the youngest group (age 18 – 24) at the later assessment points, including less prior trauma exposure in young women and lower income in young men. Women in the youngest group had less prior trauma exposure than all other age groups (the mean number of prior trauma types was 2.25 in the youngest group, and all other groups were >3.23). The lower household income in young men might have increased their risk of developing PTSD symptoms (resulting in nonsignificant gender differences) as income was associated with PTSD symptoms in men.
Women aged 25-54 developed more severe PTSD symptoms compared with age-matched men after controlling for social support, the number of prior trauma types, and household income. The effect sizes for the gender difference were large. As mentioned, the burden perspective (Norris et al., 2002) may offer an explanation for this finding. Norris and colleagues (2002) speculated that the heightened distress levels in middle-aged adults may be accounted for by the greater burden of societal and familial responsibilities put on them compared to younger and older adults who are more likely to be receivers than providers of support. Disruption to their roles as a support provider due to the impact of trauma may also have contributed to heightened distress levels in middle-aged adults (Norris et al., 2002; Thompson, Norris, & Hanacek, 1993). Women, particularly middle-aged women, spend more time than men providing care for their family members including their children and elderly parents (Bianchi & Milkie, 2010; Conway-Giustra, Crowley, & Gorin, 2002). Family caregiving can exert a toll on caregivers’ mental health, and female caregivers are at greater risk for experiencing anxiety and depressive symptoms and stress than male caregivers (Schulz & Sherwood, 2008). The middle-aged women in our sample could be disproportionately burdened by responsibilities, leading to increased PTSD severity.
The finding of the curvilinear relationship between age and PTSD symptoms only in women is consistent with our hypothesis. However, it is not consistent with the prior study of American victims of Hurricane Andrew (Norris et al., 2002) in which a similar pattern was observed regardless of gender. In the present sample, PTSD severity was not associated with age in males, but was associated with income and social support. Income was strongly negatively associated with age, which may suggest that middle-aged men’s better access to financial resources buffered the impact of age-related burdens. Further, middle-aged male MVA victims in the present sample may have had sufficient resources to offset damage to vehicles; while middle-aged men in Norris et al’s American sample likely suffered a wider range of damage and greater cost of hurricane-related damage to their property.
In women, the curvilinear relationship between age and 1-year PTSD symptoms was mediated by prior trauma exposure and social support, which is consistent with our hypothesis that the relationship between age and PTSD symptoms would be mediated by psychosocial factors. Although levels of perceived social support were not associated with age in women, its beneficial effects on PTSD symptoms might be different depending on age. The Socioemotional Selectivity Theory posits that older adults’ emotion-focused goals lead them to form smaller but emotionally close social networks (Charles & Carstensen, 2010). As mentioned above, the previous epidemiological study showed that high levels of social support more strongly predicted better mental health in young adults (Milner et al., 2016). It is possible that middle-aged women in our sample received less beneficial effects of social support compared to younger and older women. The Socioemotional Selectivity Theory also suggests that older adults have a greater tendency to remember and appraise events more positively than younger adults. The less prior trauma exposure in younger adults and reduced negative memories and appraisal of prior trauma experiences in older adults might have further contributed to the inverted-U shape relationship.
The present findings should be interpreted with caution due to some methodological limitations. This study included predominantly White MVA patients who developed mild PTSD symptoms; therefore, the generalizability of the current findings may be limited. However, given that MVAs are associated with gender-based differences in PTSD risk [i.e., women are at higher risk following an MVA (Tolin & Foa, 2006)] and that gender by age interactions have not been examined in MVA victims, MVA patients were a suitable population for this investigation. Further, the small number of older participants limited statistical power. The small-medium size gender differences in the oldest group at later assessment points may have reached statistical significance with sufficient power.
Despite these limitations, the present findings contribute to our current understanding of gender differences in risk for developing PTSD. A limited number of studies have examined interaction effects between age and gender on the development of PTSD following recent trauma exposure. Roles of psychosocial risk factors have normally been examined in relation to either age or gender, but not both. The present findings indicate that middle-aged women are at a greater risk for developing more severe PTSD symptoms after an MVA compared with men and younger and older women. It is well-established that women are at a greater risk for PTSD following an accident; however, to the best of our knowledge, this is the first study to demonstrate that women’s vulnerability following an accident varies depending on their age. Further, we identified psychosocial factors that at least partially explain the elevated risk for PTSD symptoms in middle-aged women, which can inform identification and treatment of at-risk women. Assessing social support and trauma history of middle-aged women immediately after an accident would help identify individuals as higher risk and allow for targeted preventive intervention. Present findings and theories of emotional aging suggest that interventions that promote social support and thoughts and behaviors focusing on enhancing one’s own emotional well-being may mitigate PTSD symptoms in middle-aged women. Further research should be conducted to identify additional age and gender-related psychosocial and biological factors contributing to the greater vulnerability of middle-aged women to inform the development of early intervention strategies for these individuals.
Clinical Impact Statement.
We found that middle-aged women were at higher risk for developing PTSD symptoms after a motor vehicle accident than men and women in other age groups. Our finding will help health care providers to identify women at higher risk for PTSD and provide appropriate early intervention to facilitate their psychological recovery.
Acknowledgments
This study was supported by NIH grant R01MH62042 to Douglas L. Delahanty. The preparation of this manuscript was supported by KL2TR001432-01 and UL1TR001409 from the National Center for Advancing Translational Science and NIH grant K01MH110647.
Footnotes
Potential conflicts of interest disclosure: Ihori Kobayashi receives research funding from Merck & Co.
Contributor Information
Ihori Kobayashi, Department of Psychological Sciences, Kent State University, Kent, Ohio, USA.
Eve M. Sledjeski, Department of Psychological Sciences, Kent State University, Kent, Ohio, USA
Douglas L. Delahanty, Department of Psychological Sciences, Kent State University, Kent, Ohio, USADepartment of Psychology in Psychiatry, Northeastern Ohio Medical University (NEOMED), Rootstown, Ohio, USASumma Health System, Akron, Ohio, USA
References
- Acierno R, Ruggiero KJ, Kilpatrick DG, Resnick HS, Galea S. Risk and protective factors for psychopathology among older versus younger adults after the 2004 Florida hurricanes. The American Journal of Geriatric Psychiatry. 2006;14:1051–1059. doi: 10.1097/01.JGP.0000221327.97904.b0. [DOI] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA. Predictors of PTSD and delayed PTSD after disaster: The impact of exposure and psychosocial resources. The Journal of Nervous and Mental Disease. 2006;194:485–493. doi: 10.1097/01.nmd.0000228503.95503.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews B, Brewin CR, Rose S. Gender, social support, and PTSD in victims of violent crime. Journal of Traumatic Stress. 2003;16:421–427. doi: 10.1023/A:1024478305142. [DOI] [PubMed] [Google Scholar]
- Baker SP, O’Neill B, Haddon WJ, Long WB. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. The Journal of Trauma. 1974;14:187–196. doi: 10.1097/00005373-197403000-00001. [DOI] [PubMed] [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, Koenen KC. The epidemiology of traumatic event exposure worldwide: Results from the world mental health survey consortium. Psychological Medicine. 2016;46:327–343. doi: 10.1017/S0033291715001981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianchi SM, Milkie MA. Work and family research in the first decade of the 21st century. Journal of Marriage and Family. 2010;72:705–725. doi: 10.1111/j.l741-3737.2010.00. [DOI] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: A prospective epidemiological study. Archives of General Psychiatry. 2008;65:431–437. doi: 10.1001/archpsyc.65.4.431. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting & Clinical Psychology. 2000;68:748–766. doi: 10.1037/0022-006X.68.5.748. [DOI] [PubMed] [Google Scholar]
- Bromet E, Sonnega A, Kessler RC. Risk factors for DSM-III-R posttraumatic stress disorder: Findings from the national comorbidity survey. American Journal of Epidemiology. 1998;147:353–361. doi: 10.1093/oxfordjournals.aje.a009457. [DOI] [PubMed] [Google Scholar]
- Charles ST, Carstensen LL. Social and emotional aging. Annual Review of Psychology. 2010;61:383–409. doi: 10.1146/annurev.psych.093008.100448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chossegros L, Hours M, Charnay P, Bernard M, Fort E, Boisson D, Laumon B. Predictive factors of chronic post-traumatic stress disorder 6 months after a road traffic accident. Accident Analysis & Prevention. 2011;43:471–477. doi: 10.1016/j.aap.2010.10.004. [DOI] [PubMed] [Google Scholar]
- Christiansen DM, Elklit A. Risk factors predict post-traumatic stress disorder differently in men and women. Annals of General Psychiatry. 2008;7 doi: 10.1186/1744-859X-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clogg CC, Petkova E, Haritou A. Statistical methods for comparing regression coefficients between models. American Journal of Sociology. 1995;100:1261–1293. doi: 10.1086/230638. [DOI] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Social Support: Theory, Research and Applications. Springer; 1985. Measuring the functional components of social support; pp. 73–94. [Google Scholar]
- Conway-Giustra F, Crowley A, Gorin SH. Crisis in caregiving: A call to action. Health & Social Work. 2002;27:307–311. doi: 10.1093/hsw/27.4.307. [DOI] [PubMed] [Google Scholar]
- Cougle JR, Resnick H, Kilpatrick DG. Does prior exposure to interpersonal violence increase risk of PTSD following subsequent exposure? Behaviour Research and Therapy. 2009;47:1012–1017. doi: 10.1016/j.brat.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer M, Parslow R. Trauma exposure and posttraumatic stress disorder in the elderly: A community prevalence study. The American Journal of Geriatric Psychiatry. 2008;16:853–856. doi: 10.1097/01.JGP.0000310785.36837.85. [DOI] [PubMed] [Google Scholar]
- Deegan J. On the occurrence of standardized regression coefficients greater than one. Educational and Psychological Measurement. 1978;38:873–888. doi: 10.1177/001316447803800404. [DOI] [Google Scholar]
- Dekker MC, Ferdinand RF, Van Lang ND, Bongers IL, Van Der Ende J, Verhulst FC. Developmental trajectories of depressive symptoms from early childhood to late adolescence: Gender differences and adult outcome. Journal of Child Psychology and Psychiatry. 2007;48:657–666. doi: 10.1111/j.1469-7610.2007.01742.x. [DOI] [PubMed] [Google Scholar]
- Delahanty DL, Raimonde AJ, Spoonster E, Cullado M. Injury severity, prior trauma history, urinary cortisol levels and acute PTSD in motor vehicle accident victims. Journal of Anxiety Disorders. 2003;17:149–164. doi: 10.1016/S0887-6185(02)00185-8. [DOI] [PubMed] [Google Scholar]
- Ditlevsen DN, Elklit A. The combined effect of gender and age on post traumatic stress disorder: Do men and women show differences in the lifespan distribution of the disorder. Annals of General Psychiatry. 2010;9 doi: 10.1186/1744-859X-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eranti SV, MacCabe JH, Bundy H, Murray RM. Gender difference in age at onset of schizophrenia: A meta-analysis. Psychological Medicine. 2013;43:155–167. doi: 10.1017/S003329171200089X. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gabert-Quillen C, Irish LA, Sledjeski E, Fallon W, Spoonster E, Delahanty DL. The impact of social support on the relationship between trauma history and posttraumatic stress disorder symptoms in motor vehicle accident victims. International Journal of Stress Management. 2012;19:69–79. doi: 10.1037/a0026488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irish LA, Fischer B, Fallon W, Spoonster E, Sledjeski EM, Delahanty DL. Gender differences in PTSD symptoms: An exploration of peritraumatic mechanisms. Journal of Anxiety Disorders. 2011;25:209–216. doi: 10.1016/j.janxdis.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel-Cohen Y, Kaplan O. Traumatic stress during population-wide exposure to trauma in Israel: Gender as a moderator of the effects of marital status and social support. Stress and Health. 2016;32:636–640. doi: 10.1002/smi.2647. [DOI] [PubMed] [Google Scholar]
- Jonas S, Khalifeh H, Bebbington PE, McManus S, Brugha T, Meltzer H, Howard LM. Gender differences in intimate partner violence and psychiatric disorders in England: Results from the 2007 adult psychiatric morbidity survey. Epidemiology and Psychiatric Sciences. 2014;23:189–199. doi: 10.1017/S2045796013000292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Widom CS. A prospective study of sex differences in the lifetime risk of posttraumatic stress disorder among abused and neglected children grown up. Journal of Traumatic Stress. 2009;22:566–574. doi: 10.1002/jts.20478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kun P, Tong X, Liu Y, Pei X, Luo H. What are the determinants of post-traumatic stress disorder: Age, gender, ethnicity or other? Evidence from 2008 Wenchuan earthquake. Public Health. 2013;127:644–652. doi: 10.1016/j.puhe.2013.04.018. [DOI] [PubMed] [Google Scholar]
- Liu H, Petukhova MV, Sampson NA, Aguilar-Gaxiola S, Alonso J, Andrade LH, Hinkov H. Association of DSM-IV posttraumatic stress disorder with traumatic experience type and history in the world health organization world mental health surveys. JAMA Psychiatry. 2017;74:270–281. doi: 10.1001/jamapsychiatry.2016.3783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lokuge S, Frey BN, Foster JA, Soares CN, Steiner M. Depression in women: Windows of vulnerability and new insights into the link between estrogen and serotonin. The Journal of Clinical Psychiatry. 2011;72:e1563–9. doi: 10.4088/JCP.11com07089. [DOI] [PubMed] [Google Scholar]
- Milner A, Krnjacki L, LaMontagne AD. Age and gender differences in the influence of social support on mental health: A longitudinal fixed-effects analysis using 13 annual waves of the HILDA cohort. Public Health. 2016;140:172–178. doi: 10.1016/j.puhe.2016.06.029. [DOI] [PubMed] [Google Scholar]
- Naeem F, Ayub M, Masood K, Gul H, Khalid M, Farrukh A, Chaudhry HR. Prevalence and psychosocial risk factors of PTSD: 18 months after Kashmir earthquake in Pakistan. Journal of Affective Disorder. 2011;130:268–279. doi: 10.1016/j.jad.2010.10.035. [DOI] [PubMed] [Google Scholar]
- Norris FH, Kaniasty K, Conrad ML, Inman GL, Murphy AD. Placing age differences in cultural context: A comparison of the effects of age on PTSD after disasters in the United States, Mexico, and Poland. Journal of Clinical Geropsychology. 2002;8:153–173. [Google Scholar]
- Norris FH. Screening for traumatic stress: A scale for use in the general population. Journal of Applied Social Psychology. 1990;20:1704–1718. doi: 10.1111/j.1559-1816.1990.tb01505.x. [DOI] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Trauma: Theory, Research, Practice, and Policy. 2008;S(1):3–36. doi: 10.1037/1942-9681.S.1.3. [DOI] [PubMed] [Google Scholar]
- Perlis RH, Dennehy EB, Miklowitz DJ, DelBello MP, Ostacher M, Calabrese JR, Sachs G. Retrospective age at onset of bipolar disorder and outcome during two-year follow-up: Results from the STEP-BD study. Bipolar Disorders. 2009;11:391–400. doi: 10.1111/j.1399-5618.2009.00686.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson JTE. Eta squared and partial eta squared as measures of effect size in educational research. Educational Research Review. 2011;6:135–147. doi: 10.1016/j.edurev.2010.12.001. [DOI] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine. 2011;41:71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: A systematic review. Depression. 2006;6:1285–1298. doi: 10.4088/JCP.v67n0818. [DOI] [PubMed] [Google Scholar]
- Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. Journal of Social Work Education. 2008;44:105–113. doi: 10.1097/01.NAJ.0000336406.45248.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamres LK, Janicki D, Helgeson VS. Sex differences in coping behavior: A meta-analytic review and an examination of relative coping. Personality and Social Psychology Review. 2002;6:2–30. doi: 10.1207/S15327957PSPR0601_1. [DOI] [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Norris FH, Hanacek B. Age differences in the psychological consequences of hurricane Hugo. Psychology and Aging. 1993;8:606. doi: 10.1037/0882-7974.8.4.606. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Labor. Unemployment rates by age, sex, and marital status, seasonally adjusted. 2017a Retrieved from www.bls.gov/web/empsit/cpseea10.htm.
- U.S. Department of Labor. Usual Weekly Earnings of Wage and Salary Workers. U.S. Department of Labor; 2017b. (No. USDL-17-1011). [Google Scholar]
- Yonkers KA, O’Brien PS, Eriksson E. Premenstrual syndrome. Lancet. 2008;371:1200–1210. doi: 10.1016/S0140-6736(08)60527-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


