Abstract
Objective/Background: To examine how demographic and injury characteristics identify satisfaction with life (SWL), and assess the differential effects of a wellness intervention by baseline SWL groups.
Design: Baseline and longitudinal analysis of a randomized controlled pilot intervention using decision tree regression and linear mixed models.
Setting: Community based.
Participants: Seventy-two individuals with spinal cord injury (SCI) were randomized to an intervention group (n = 39) or control group (n = 33). Participants were aged 44.1 ± 13.0 years and 13.1 ± 10.6 years post-injury. Most participants were male (n = 50; 69.4%) and had paraplegia (n = 38; 52.7%). Participants were classified as high versus low SWL at baseline using a cutoff score of 20.
Interventions: The intervention aimed to increase self-efficacy, and in turn, increase engagement in health-promoting behaviors related to SWL. Six 4-hour in-person workshops were conducted over a 3-month period led by experts and peer-mentors who were available for support.
Outcome measure(s): Self-efficacy for health practices, secondary condition severity, health-promoting behaviors, perceived stress, and SWL.
Results: At baseline, participants with low SWL were recently injured (<4.5 years), while persons with high SWL were married and younger (<49 years old). Intervention participants with low SWL at baseline significantly improved SWL over time compared to those with high SWL (P = 0.02).
Conclusion: Certain injury and demographic characteristics were associated with SWL, and intervention participants with low SWL at baseline improved their SWL over 2 years. Healthcare providers should consider time post-injury, marital status, and age in identifying individuals at risk for low SWL that may benefit from wellness interventions.
Keywords: Spinal cord injuries, Quality of life, self-efficacy, Clinical trial, Outcomes assessment, Rehabilitation
Introduction
Satisfaction with life (SWL) generally decreases immediately after spinal cord injury (SCI).1 Individuals with SCI often struggle to learn how to complete daily living tasks following injury.2 High rates of unemployment, low income, and rehospitalizations following injury all reduce independence.3,4 Although increases in SWL typically occur in the years following injury, individuals with SCI overall report lower SWL than the general population.5,6
The Moss-Morris model of adjustment to chronic illness highlights critical factors in psychological, physical, and social adjustments and overall well-being (i.e. affect, distress, and relationships).7 This theory posits that factors outside an individual's control including personal background, illness specific, and background social and environmental factors impact adjustment.7 Further, critical key events and ongoing illness stressors may contribute to negative trajectories of adjustment because they lead to a disruption in an individual's emotional equilibrium and SWL. Demographic factors and injury characteristics fit within these areas of the working model of adjustment and identifying factors that put those at risk for negative adjustment following SCI may be critical to ameliorate trajectories.
Previous studies show mixed findings about the link between personal characteristics and SWL following injury, which hinders provider capability in effectively identifying patients at risk for negative adjustment. Some demographic factors positively associated with SWL include being Caucasian, female, employed, married, and with higher income.6,8–12 Injury characteristics negatively associated with SWL include 1 year or less post-injury, assistive device use, lower functional status, hospitalizations, and secondary conditions.6,9,13,14 However, one study showed that these factors (i.e. injury level or completeness, age, or years post-injury) did not play a meaningful role in reported measures of psychological well-being.15 Other investigations highlighted mixed evidence for other factors such as sex, social integration, and employment which were not associated with SWL.3,16 Therefore, more research is needed to identify personal characteristics that are shared by individuals reporting low SWL.
Wellness interventions for individuals with SCI often target lifestyle behaviors and SWL. These types of interventions can be effective for improving health-related quality of life (HR-QOL), mobility, depression, self-rated health, self-efficacy, well-being, and general QOL.17–21 These interventions cohere within the Moss-Morris model of adjustment by targeting cognitive and behavioral factors that may aid in positive adjustment.7 For example, a 6-month peer led self-management intervention for individuals with SCI versus usual care reported greater SWL, increased service use, and decreased social/role activity limitations among intervention participants.22 However, the results from these interventions often lack statistical significance and instead report “positive trends” and do not account for the impact of demographic and injury characteristics in these changes.
Zemper et al.23 developed a holistic wellness intervention in individuals with SCI called “Well on Wheels” (WOW). The WOW intervention was created using social cognitive theory (SCT) behavior change concepts aimed at improving SWL in individuals with SCI. This intervention targeted behaviors derived from the Stuifbergen's model of QOL in individuals with chronic disabling conditions.24 The preliminary results of this investigation suggested that from baseline to 7-month post-intervention, intervention group participants reported positive trends in improvement in self-efficacy, secondary conditions, and health behaviors, but no significant differences between-group changes.23 However, the role of baseline SWL on longitudinal outcomes in this intervention has not been assessed. Evaluating interventions for understanding who benefits the most, beyond differences in overall group means, is important for refining intervention contents and identifying those most likely to benefit from an intervention. In the case of examining changes in SWL after a wellness intervention, examining baseline SWL may have some value for understanding its role in the potential effectiveness of a wellness intervention.
The current study was a secondary analysis of baseline and longitudinal follow-up data from individuals who participated in the WOW intervention. We first sought to identify subgroups of individuals with high versus low SWL at baseline. It was hypothesized that certain demographic and injury characteristics could correctly identify individuals with low SWL and who may show changes in outcomes following the intervention. Second, we assessed the differential effects of the WOW intervention by baseline SWL group. We expected that individuals in the low SWL group would show larger improvements relative to those in the high SWL group in primary and secondary outcomes at 3 months, 7 months, 1-year post-intervention, and 2-year post-intervention.
Methods
Participants
Individuals were recruited from several locations including an outpatient SCI clinic in the Department of Physical Medicine and Rehabilitation at the University of Michigan Health System, the University of Michigan SCI Model Care System database (SCIMS), and the mailing list for the Center for Independent Living in Ann Arbor. All participants who completed baseline questionnaire data for the WOW intervention were included in this analysis. The WOW intervention was a randomized controlled pilot trial of a holistic wellness intervention for individuals with SCI, as previously described.23 Inclusion criteria for participation included SCI of C5 and below, American Spinal Injury Association (AIS) Impairment Classification Scale A–D, being 18–80 years old, and at least 1-year post-injury. Exclusion criteria included the diagnosis of cognitive deficits such as traumatic brain injury or dementia, medical problems that could impose a health risk (e.g. myocardial infarction), and primary disability not due to SCI. Ninety-eight individuals expressed interest in the study after screening and completed a survey that was returned to the study team. Investigators used surveys to confirm eligibility. Fifteen individuals were deemed ineligible for the study, and 83 individuals were enrolled, however, only 72 provided informed consent, completed the baseline assessment, and were randomized.
Measurements
Demographics variables
Participants self-reported their age, sex, race, education, employment, and marital status.
Injury characteristics
Years post-injury was estimated by subtracting each participant's age at injury from their age at baseline. Participants reported their level of injury as paraplegia or tetraplegia and was confirmed by a physician AIS examination.
Satisfaction with life
The Satisfaction with Life Scale (SWLS) was used to measure global cognitive judgments of satisfaction with one's life.25 The SWLS is a five-item scale, each item rated on a seven-point Likert scale and with scores ranging from 5 to 35. A score of 20 represents the neutral point on the scale and lower scores indicate less satisfaction.26 The SWLS has been used in investigations that included individuals with SCI.6,10,27
Self-efficacy for health practices
The Self-rated Abilities for Health Practice Scale (SAHP) was used to assess self-efficacy to implement health-promoting behaviors.28 The scale includes 28 items rated on a five-point scale from 0 (not at all) to 4 (completely). Total scores range from 0 to 112 with higher scores indicating greater self-efficacy.
Health-promoting behaviors
Personal health-promoting habits were assessed with the Health-Promoting Lifestyle Profile II (HPLP).29 Fifty two items are rated on four-point Likert scales ranging from never (1) to routinely (4). Total scores range from 52 to 108 with higher scores indicating greater health-promoting behaviors.
Secondary condition severity
The Secondary Conditions Scale (SCS) is used to report new problems related to SCI.30 The scale was modified from reporting over the past year to over a 3-month period to be appropriate for the data collection time points. Sixteen common secondary conditions related to SCI were rated on four-point Likert scales ranging from 0 (not a problem) to 3 (significant or chronic problem). Scores were summed to determine a total score that ranged from 0 to 48, with higher scores indicating greater severity of secondary conditions.
Perceived stress
The Perceived Stress Scale (PSS) measures the degree to which situations in one's life are appraised as stressful.31 Ten items are rated on five-point Likert scales ranging from never (0) to very often (4). The total score is obtained by reversing responses to the four positively stated items and then summing across all items, therefore high scores indicate higher stress levels.
Intervention
The WOW intervention included six 4-hour workshops over a 3-month period followed by a 4-month tapering period. Intervention workshops included four modules: lifestyle management (sexual health and stress management), physical activity, nutrition, and preventing secondary conditions. The overall goal of the intervention was to increase self-efficacy, which in turn, would increase engagement in health-promoting behaviors related to increased SWL.24 Didactic and experiential components based on SCT behavior change strategies were utilized to keep participants involved and engaged including experiential exercises, observational learning, self-monitoring, and goal setting.32 Two peers with SCI from local centers for independent living served as moderators whose role was primarily support and guidance. Professionals involved in curriculum modifications taught specific course areas (e.g. exercise modules taught by a physical therapist). Following the six workshop sessions, all intervention participants attended an individual coaching session with facilitators to outline individualized goals for the 4-month tapering period. Two follow-up phone calls were conducted by research assistants during tapering period to discuss individualized goal attainment and barriers. A detailed description of the intervention can be found elsewhere.23
Statistical analyses
Descriptive analyses were used to identify high (SWLS ≥ 20) and low (SWLS < 20) SWL groups based on bimodal distribution of the data, where two latent groups empirically appeared to manifest. The Classification and Regression Tree (CART) method was then used to split data into segments with participants that are as homogenous as possible with respect to SWL status (dependent variable). Based on the previous literature,3,8–14 demographic and injury characteristics associated with SWL were included as the predictor variables of interest (independent variables), including the number of years post-injury, AIS completeness, age, marital status, sex, race, education, and employment. The Gini index was used as the criterion for identifying the target group (low SWL); this method splits the nodes to find variables that are shared with respect to SWL group, aiming to create child nodes that are as homogenous as possible. Criteria were also determined for minimum cases per node; minimum cases in a parent node of ≥30% of the sample (n ≥ 21) and in a child node ≥15% of the sample (n ≥ 10). Results of 10-fold cross-validation were evaluated to avoid overfitting the model.
Linear mixed model analyses were used to examine the relationship between SWL group on primary and secondary outcomes over time. Fixed factors included a full factorial of SWL group and time. The time variable included all five time points with baseline (T1) as the reference. Dependent variables of interest included the primary (SWL and self-efficacy for health practices) and secondary outcomes (health-promoting behaviors, secondary condition severity, and perceived stress). Covariates of interest (i.e. demographic variables and injury characteristics) were included for each outcome based on theoretical associations. Significant covariates were then included in the model as an interaction term (i.e. Covariate × SWL group × Time) to identify any significant differences in groups. None of the covariates (e.g. marital status) assessed for significant interactions terms (e.g. marital status × group) were significant and therefore the unadjusted models were presented. An autoregressive covariance structure was utilized due to assumed correlation among the time points for each participant. P values were obtained by likelihood ratio tests for the model fixed effects.
Results
Descriptive
Table 1 provides sociodemographic and injury characteristics of the 72 participants who enrolled in the WOW intervention. Mean age at baseline was 44.1 ± 13.0 years and time post-injury was 13.1 ± 10.6 years. Sixty-nine percent were male, 52.8% identified as having paraplegia, and 45.8% had complete injuries (AIS-A). The majority of the participants were white (88.9%) and had at least some college education (69.4%). Participants ranged in their employment and marital status with the largest portions being unemployed (45.8%) and married (47.2%).
Table 1. Baseline sociodemographic and injury characteristics of Well on Wheels full study sample, high vs. low SWL group.
| Full sample (N = 72) | High SWL (N = 40) | Low SWL (N = 32) | |
|---|---|---|---|
| Age at enrolment (years) | 44.1 ± 13.0 | 44.3 ± 13.3 | 43.9 ± 12.9 |
| Years post-injury | 13.1 ± 10.6 | 15.2 ± 11.6 | 10.6 ± 8.8 |
| Sex (n (%)) | |||
| Female | 22 (30.6) | 15 (68.2) | 7 (31.8) |
| Male | 50 (69.4) | 25 (50.0) | 25 (50.0) |
| Level of injury† (n (%)) | |||
| Paraplegia | 38 (52.8) | 18 (47.4) | 20 (52.6) |
| Tetraplegia | 30 (41.7) | 20 (66.6) | 10 (33.3) |
| ASIA completeness† (n (%)) | |||
| Complete (A) | 33 (45.8) | 21 (63.6) | 12 (36.4) |
| Incomplete (B–D) | 34 (47.2) | 17 (50.0) | 17 (50.0) |
| Normal (E) | 1 (1.4) | 0 | 1 (100.0) |
| Race (n (%)) | |||
| White | 64 (88.9) | 37 (57.8) | 27 (42.2) |
| Not-White | 8 (11.1) | 3 (37.5) | 5 (62.5) |
| Education† (n (%)) | |||
| High school | 21 (29.2) | 9 (42.9) | 12 (57.1) |
| Some college | 25 (34.7) | 14 (56.0) | 11 (44.0) |
| College degree or more | 25 (34.7) | 16 (64.0) | 9 (36.0) |
| Employment (n (%)) | |||
| Unemployed | 33 (45.8) | 19 (57.6) | 14 (42.4) |
| Employed | 23 (31.9) | 13 (56.5) | 10 (43.5) |
| Retired | 16 (22.2) | 8 (50.0) | 8 (50.0) |
| Marital status (n (%)) | |||
| Single | 27 (37.5) | 12 (44.4) | 15 (55.6) |
| Married | 34 (47.2) | 24 (70.6) | 10 (29.4) |
| Divorced | 11 (15.3) | 4 (36.4) | 7 (63.6) |
| Primary outcome | |||
| SWLS | 20.7 ± 8.0 | 26.9 ± 4.2* | 12.9 ± 3.7* |
SWLS = Satisfaction with Life Scale.
*Significant differences P < 0.05.
†Missing baseline values: Level of injury = 2, ASIA = 2, Education = 1.
Predicting baseline SWL groups
Mean SWLS score at baseline was 20.7 ± 8.0 for the total sample, 26.9 ± 4.2 for high SWL group, and 12.9 ± 3.7 for low SWL group. At baseline, the only significant difference between groups was marital status, with more individuals who were married in the high SWL group (Table 1).
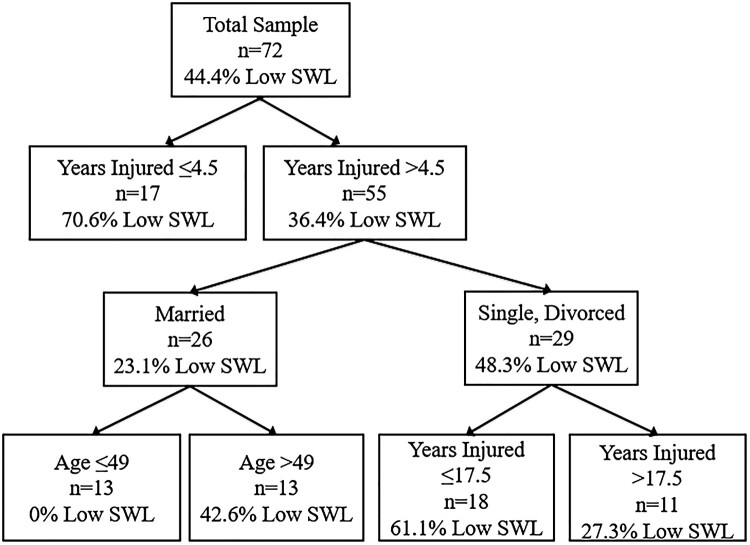
Figure 1 shows the results of the CART decision tree with five terminal nodes predicting baseline SWL group status. Low reported SWL was most likely in participants ≤4.5 years post-injury (70%). Among participants who were >4.5 years post-injury, those who were single or divorced and ≤17.5 years post-injury were most likely to report low SWL (61% vs. 27%). Participants who were >4.5 years post-injury and married reported high SWL (76%). However, among these married participants, age ≤49 years was a significant predictor of high SWL (0% vs. 42%). Calculated risk estimates for the tree were 0.29 ± 0.05 indicating that the SWL group status predicted by the tree was wrong for 29% of the cases. The decision tree model using sociodemographic and injury characteristics correctly predicted 71.9% of participants with low SWL and 70.0% of participants with high SWL.
Figure 1.
Classification and Regression Tree (CART) high and low baseline satisfaction with life (SWL).
Longitudinal intervention group change by SWL status
At baseline, there were significant differences in intervention group participants by SWL group with those with low SWL on average fewer years post-injury and more incomplete injuries. There was a significant SWL group × time interaction (P = 0.02). Individuals with low SWL at baseline showed greater change in SWLS scores over time than those high at baseline (Table 2). There were also significant main effects of both SWL group (P = 0.001) and time (P = 0.01). Potential regression to the mean of low SWL group using the expected difference in the values between baseline and post-intervention scores if no significant changes occurred were evaluated as described in Linden et al., and did not affect the conclusions as the effect was <1.5 points.33
Table 2. Satisfaction with Life Group Primary Outcomes Baseline (T1) to 2-year post-intervention (T5) (N = 39).
| SWLS | 95% CI | SAHP | 95% CI | |||
|---|---|---|---|---|---|---|
| Estimate (SE) | LB | UB | Estimate (SE) | LB | UB | |
| Intercept | 12.06 (1.22)*** | 9.64 | 14.49 | 91.31 (4.16)*** | 83.08 | 99.55 |
| SWL group | 13.68 (1.59)*** | 10.52 | 16.83 | −4.70 (5.42) | −15.43 | 6.02 |
| Time 2 | 3.64 (1.72)* | 0.24 | 7.04 | 3.23 (6.52) | −9.67 | 16.14 |
| Time 3 | 4.71 (1.73)** | 1.29 | 8.12 | −1.45 (7.21) | −15.71 | 12.81 |
| Time 4 | 5.38 (1.74)** | 1.93 | 8.83 | 12.95 (7.96) | −2.81 | 28.70 |
| Time 5 | 6.24 (1.56)*** | 3.14 | 9.34 | −10.37 (8.42) | −27.07 | 6.33 |
| SWL Group × Time | ||||||
| High Time 2 | −4.21 (2.20) | −8.56 | 0.13 | 8.77 (8.37) | −7.78 | 25.32 |
| High Time 3 | −5.16 (2.16)* | −9.44 | −0.88 | 0.04 (9.02) | −17.80 | 17.89 |
| High Time 4 | −6.21 (2.11)** | −10.40 | −2.03 | −8.39 (9.69) | −27.56 | 10.78 |
| High Time 5 | −5.75 (1.89)** | −9.50 | −1.99 | 10.21 (10.34) | −10.31 | 30.72 |
| AR(var) | 23.72 (7.74)** | 17.41 | 32.30 | 277.23 (34.57)** | 217.12 | 353.97 |
| AR(rho) | 0.68 (0.06)** | 0.55 | 0.78 | 0.05 (0.12) | −0.18 | 0.27 |
Referent Low Satisfaction with Life Group and Baseline Time 1.
SWL, Satisfaction with Life; 95% CI, 95% confidence interval; LB, lower bound; UB, upper bound; AR(var), residual variance of dependent variable at each time point; AR(rho), autocorrelation.
*P < 0.05, **P < 0.01, ***P < 0.001.
The other primary outcome of interest was SAHP. There was no significant SWL group × time interaction or main effect for SWL group. There was a significant main effect of time across both groups (P = 0.04), but post hoc analyses showed no significant differences between specific time points (Table 3).
Table 3. Satisfaction with Life group secondary outcomes baseline (T1) to 2-year post-intervention (T5) (N = 39).
| SCS Severity | 95% CI | HPLP | 95% CI | PSS | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate (SE) | LB | UB | Estimate (SE) | LB | UB | Estimate (SE) | LB | UB | |
| Intercept | 19.63 (3.66)*** | 12.39 | 26.86 | 132.75 (5.58)*** | 121.71 | 143.79 | 31.06 (1.37)*** | 28.35 | 33.78 |
| SWL Group | 4.85 (4.76) | −4.57 | 14.28 | −3.31 (7.26) | −17.69 | 11.06 | 1.98 (1.79) | −1.56 | 5.52 |
| Time 2 | −1.90 (5.73) | −13.24 | 9.24 | 0.98 (8.73) | −16.31 | 18.26 | −0.70 (2.15) | −4.95 | 3.56 |
| Time 3 | −4.31 (6.31) | −16.79 | 8.17 | −5.72 (9.64) | −24.80 | 13.36 | 0.81 (2.38) | −3.89 | 5.51 |
| Time 4 | −8.38 (6.94) | −22.11 | 5.35 | 9.10 (10.51) | −11.69 | 29.89 | 0.44 (2.63) | −4.76 | 5.64 |
| Time 5 | −5.43 (7.15) | −19.62 | 8.75 | −16.88 (11.82) | −40.32 | 6.55 | −6.24 (2.81)* | −11.80 | −0.68 |
| SWL Group × Time | |||||||||
| High Time 2 | −6.17 (7.35) | −20.72 | 8.37 | 17.90 (11.02) | −4.27 | 40.08 | −0.01 (2.76) | −5.47 | 5.45 |
| High Time 3 | 2.89 (7.90) | −12.73 | 18.52 | 3.78 (12.07) | −20.11 | 27.68 | −4.48 (2.97) | −10.37 | 1.40 |
| High Time 4 | 2.23 (8.44) | −14.46 | 18.93 | −0.46 (12.77) | −25.73 | 24.81 | −1.49 (3.20) | −7.82 | 4.84 |
| High Time 5 | 2.76 (8.76) | −14.61 | 20.14 | 11.43 (14.63) | −17.58 | 40.44 | 3.93 (3.45) | −2.91 | 10.77 |
| AR(var) | 214.09 (26.97)** | 167.26 | 274.04 | 497.81 (63.62)** | 387.51 | 639.51 | 30.15 (3.75)** | 23.62 | 38.49 |
| AR(rho) | 0.15 (0.11) | −0.06 | 0.35 | −0.20 (0.12) | −0.42 | 0.04 | 0.01 (0.10) | −0.19 | 0.21 |
Referent Low Satisfaction with Life Group and Baseline Time 1.
SWL, Satisfaction with Life; 95% CI, 95% confidence interval; LB, lower bound; UB, upper bound; AR(var), residual variance of dependent variable at each time point; AR(rho), autocorrelation.
*P < 0.05, **P < 0.01, *** P < 0.001.
HPLP was included as a secondary outcome. There was no significant SWL group × time interaction or main effect for SWL group. However, there was a significant main effect of time where HPLP scores decreased over time across both groups (P = 0.04) but post hoc analyses showed no significant differences between specific time points. Similarly, there were no significant SWL group × time interaction or main effects for SWL group or time for SCS and PSS outcomes (Table 3).
Discussion
This study identified years post-injury, marital status, and age as significant factors associated with SWL following SCI. Participants who were recently injured (<4.5 years) were more likely to have low SWL at baseline, while those who were injured longer (>4.5 years) and married reported high SWL. Additionally, participants that were less than 49 years old, married, and at least 4.5 years post-injury all reported high SWL. The demographic and injury factors shared by individuals with low versus high baseline SWL fit well within the Moss-Morris working model of adjustment to chronic illness as important underlying factors associated with positive or negative adjustment.7
Our results are important because individuals with SCI report lower levels of SWL than the general population.34 The first-year post-injury is well documented as a sensitive period during the rehabilitation process in which physiological and psychological factors shift in both positive and negative directions.1 Previous studies report good or excellent QOL in the majority of individuals 20 years or more post-injury and similar levels of SWL compared to same aged peers 10 and 15 years post-injury.15,16 Our findings highlight the importance of further examining individuals not just 1 year post-injury, but up to 4.5 years given the potential risk of low SWL. Individuals in this study tended to report higher SWL more years after injury which may be an opportunity to use interventions to improve SWL sooner after injury.
This investigation identified other factors that were associated with SWL in addition to years post-injury that should be considered in supporting positive adjustment. Marital status was identified as a predictor of SWL at baseline. This finding fits within the Moss-Morris model of adjustment as a social and environmental factor that can impact ongoing illness stressors. Married individuals on average report greater SWL than those who are single or divorced.35 However, the mechanism for the association between marital status and SWL is not well established. Three perspectives highlighted in the literature include selection as well-adjusted individuals may be more likely to get married, social support or social integration, or structural symbolic interactionism perspective based on sociological views of the self.35
Structural symbolic interactionism perspective focuses on unique roles crucial to individual identity (e.g. partner, parent, sibling, etc.) in which a spousal role would be a higher order commitment tied closely to identity and self-esteem.36 The most commonly accepted explanation is social support, having a supportive partner may buffer individuals from stressful life events such as periods of low income, and also emotional benefits of a long-term committed relationship.35 Specifically, for individuals with SCI partners may serve as caregiver support, which can be integral to managing health.37 Further research is needed exploring other mediators that may influence the relationship between SWL and marital status including measures of social support, adjustment and positive affect prior to marriage, and structural symbolic interactionism.
Younger individuals, more than 4.5 years post-injury, who were married were identified as a protected group of individuals with SCI who all reported high SWL. Age is an important personal background factor to consider in the adjustment process as younger individuals with SCI may vary from older individuals. Age is associated with social participation; younger individuals generally reporting more social participation and ease in community reintegration.38 Therefore, in the Moss-Morris working model of adjustment, age may be confounded with background social and environmental factors (i.e. social support and relationships with others) that must be considered in conceptualizing the association between age and SWL. Therefore, this study provides a more comprehensive picture of how marital status, age, and years following injury interact. These interactions provide valuable information to clinicians helping them better identify individuals with SCI most at risk for low SWL in different periods of rehabilitation.6,10,11
Participants from the WOW intervention improved SWL over the 2-year follow-up period. At baseline, mean SWL in this sample was lower than the general population mean.25 Therefore, many individuals in the WOW intervention were at risk for negative physical, social, and psychological adjustments and had the potential to benefit from a wellness intervention. Generally, global SWL is considered a stable construct when measured longitudinally,14,39 however, our study shows that the WOW intervention participants in the low SWL group significantly improved. Participants in the high SWL group on average maintained above average SWL. Strategies from this intervention may provide resources to help improve SWL in individuals with low baseline SWL.
Our findings showed no significant differences in improvements in self-efficacy for health practices, secondary conditions, or health-promoting behaviors by baseline SWL group over a 2-year follow-up period. Time effects for self-efficacy and health-promoting behaviors in this study indicate that these outcomes are variable over time or regress toward the mean.23 Previous findings from the first to third time point in the WOW study showed no significant difference between intervention and control group on self-efficacy for health practices, secondary conditions, or most health-promoting behaviors. Although WOW was based on the Stuifbergen's model of QOL in individuals with chronic disabling conditions,24 change may occur over a longer period of time than initially expected or, as our results suggest, not all individuals change uniformly. If only averages are used, true effects of an intervention like WOW may be missed. This model highlights self-efficacy, secondary conditions, and health-promoting behaviors as the antecedents to QOL in individuals with chronic disabling conditions. These variables may be associated with QOL in individuals with SCI, but the underlying mechanisms and direction of changes may be different. For example, individuals with higher SWL following injury may have more resources to take care of themselves and therefore experience fewer secondary conditions and barriers since greater secondary conditions and barriers are antecedents to SWL.24
Limitations
Limitations in this study include small sample size and homogeneity of certain demographic characteristics (e.g. 89% white). This sample may not be representative of other cohorts of individuals with SCI because they enrolled in a wellness intervention. In light of this, our decision tree model should be tested in larger and more diverse samples. Additionally, SWL was split by distribution to establish high and low groups, which can lead to underestimations of regression to the mean effects as described by Linden et al.33 and it is possible that some participants in the low or high SWL group may have been misclassified based on the baseline measure alone. Future studies should also examine the impact of socioeconomic status as recent findings from Krause et al.40 highlight the moderating effect of socioeconomic status on changes in SWL for individuals with SCI. Parental status is an additional metrics of interest for future research given its impact on social participation and SWL. It is also possible that changes in SWL for this study were primarily due to variability over time or other variables that were not measured such as intervention engagement and the dose of the intervention may have not been sufficient to elicit changes in self-efficacy. Therefore, we suggest further examination, specifically in individuals with SCI, of the causal direction and associations among secondary conditions, self-efficacy, barriers, resources, acceptance, and health-promoting behaviors. More effective interventions to aid adjustment can be developed once the direction of these relationships is better understood.
Conclusion
Overall, practitioners need to consider marital status, years post-injury, and age when working with patients during rehabilitation as individuals with low SWL may share common features that can be identified by collecting demographic information continuously. Individuals who are more recently injured are at risk for low SWL and practitioners have the chance to provide them with important resources such as wellness interventions to aid this process. Individuals should be tracked over time since SWL appears to be amenable to change. Further, individuals who lack a strong support system should be identified as they are most likely to feel isolated and report psychological distress. Our results indicate that marital status is a key background social and environmental factor in adjustment in that having a partner is associated with higher SWL for individuals with SCI.
Acknowledgements
The published material is substantially the product of the first author's dissertation.
Disclaimer statements
Contributors None.
Funding Funding was provided by a grant from the University of Michigan Health Systems (UHMS) Venture Investment Fund; by the UHMS General Clinical Research Center (NIH grant M01-RR00042); and the University of Michigan Spinal Cord Injury Model System Program, funded by NIDLRR grant H133N000009.
Conflicts of interest Authors have no conflicts of interest to declare.
ORCID
Stephanie L. Silveira http://orcid.org/0000-0002-1973-2119
Daniel P. O'Connor http://orcid.org/0000-0001-9750-2864
References
- 1.van Leeuwen CM, Post MW, Hoekstra T, van dar Woude LH, de Groot S, Snoek GJ, et al. Trajectories in the course of life satisfaction after spinal cord injury: identification and predictors. Arch Phys Med Rehabil 2011;92(2):207–13. [DOI] [PubMed] [Google Scholar]
- 2.Boschen KA, Tonack M, Gargaro J.. Long-term adjustment and community reintegration following spinal cord injury. Int J Rehabil Res 2003;26(3):157–64. [DOI] [PubMed] [Google Scholar]
- 3.Dijkers MP. Correlates of life satisfaction among persons with spinal cord injury. Arch Phys Med Rehabil 1999;80(8):867–76. [DOI] [PubMed] [Google Scholar]
- 4.Middleton J, Lim K, Taylor L, Soden R, Rutkowski S.. Patterns of morbidity and rehospitalisation following spinal cord injury. Spinal Cord 2004;42(6):359–67. [DOI] [PubMed] [Google Scholar]
- 5.Krause JS. Life satisfaction after spinal cord injury: a descriptive study. Rehabil Psychol 1992;37(1):61. [Google Scholar]
- 6.Putzke JD, Richards JS, Hicken BL, DeVivo MJ.. Predictors of life satisfaction: a spinal cord injury cohort study. Arch Phys Med Rehabil 2002;83(4):555–61. [DOI] [PubMed] [Google Scholar]
- 7.Moss Morris R. Adjusting to chronic illness: time for a unified theory. Br J Health Psychol 2013;18(4):681–6. [DOI] [PubMed] [Google Scholar]
- 8.Botticello AL, Chen Y, Cao Y, Tulsky DS.. Do communities matter after rehabilitation? The effect of socioeconomic and urban stratification on well-being after spinal cord injury. Arch Phys Med Rehabil 2011;92(3):464–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clayton KS, Chubon RA.. Factors associated with the quality of life of long-term spinal cord injured persons. Arch Phys Med Rehabil 1994;75(6):633–8. [DOI] [PubMed] [Google Scholar]
- 10.Dowler R, Richards JS, Putzke JD, Gordon W, Tate D.. Impact of demographic and medical factors on satisfaction with life after spinal cord injury: a normative study. J Spinal Cord Med 2001;24(2):87–91. [DOI] [PubMed] [Google Scholar]
- 11.Kalpakjian CZ, Houlihan B, Meade MA, Karana-Zebari D, Heinemann AW, Dijkers MP, et al. Marital status, marital transitions, well-being, and spinal cord injury: an examination of the effects of sex and time. Arch Phys Med Rehabil 2011;92(3):433–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krause JS, Dawis RV.. Prediction of life satisfaction after spinal cord injury: a four-year longitudinal approach. Rehabil Psychol 1992;37(1):49. [Google Scholar]
- 13.Jain NB, Sullivan M, Kazis LE, Tun CG, Garshick E.. Factors associated with health-related quality of life in chronic spinal cord injury. Am J Phys Med Rehabil 2007;86(5):387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Koppenhagen CF, Post MW, van der Woude LH, de Groot S, de Witte LP, van Asbeck FW, et al. Recovery of life satisfaction in persons with spinal cord injury during inpatient rehabilitation. Am J Phys Med Rehabil 2009;88(11):887–95. [DOI] [PubMed] [Google Scholar]
- 15.Whiteneck GG, Charlifue SW, Frankel HL, Fraser MH, Gardner BP, Gerhart KA, et al. Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia 1992;30(9):617–30. [DOI] [PubMed] [Google Scholar]
- 16.Cushman LA, Hassett J.. Spinal cord injury: 10 and 15 years after. Paraplegia 1992;30(10):690–6. [DOI] [PubMed] [Google Scholar]
- 17.Block P, Vanner EA, Keys CB, Rimmer JH, Skeels SE.. Project Shake-It-Up: using health promotion, capacity building and a disability studies framework to increase self efficacy. Disabil Rehabil 2010;32(9):741–54. [DOI] [PubMed] [Google Scholar]
- 18.Dicianno BE, Lovelace J, Peele P, Fassinger C, Houck P, Bursic A, et al. Effectiveness of a wellness program for individuals with spina bifida and spinal cord injury within an integrated delivery system. Arch Phys Med Rehabil 2016;97(11):1969–78. [DOI] [PubMed] [Google Scholar]
- 19.Morrison JD, Stuifbergen AK.. Outcome expectations and physical activity in persons with longstanding multiple sclerosis. J Neurosci Nurs 2014;46(3):171–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Phillips VL, Vesmarovich S, Hauber R, Wiggers E, Egner A.. Telehealth: reaching out to newly injured spinal cord patients. Public Health Rep 2001;116 Suppl. 1:94–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Verwer JH, van Leeuwen CM, Bolier L, Post MW.. Feasibility of an online well-being intervention for people with spinal cord injury: a pilot study. Spinal Cord 2016;54(6):473–7. [DOI] [PubMed] [Google Scholar]
- 22.Houlihan BV, Brody M, Everhart-Skeels S, Pernigotti D, Burnett S, Zazula J, et al. Randomized trial of a peer-led, telephone-based empowerment intervention for persons with chronic spinal cord injury improves health self-management. Arch Phys Med Rehabil 2017;98(6):1067–76. [DOI] [PubMed] [Google Scholar]
- 23.Zemper ED, Tate DG, Roller S, Forchheimer M, Chiodo A, Nelson VS, et al. Assessment of a holistic wellness program for persons with spinal cord injury. Am J Phys Med Rehabil 2003;82(12):957–68. [DOI] [PubMed] [Google Scholar]
- 24.Stuifbergen AK, Becker HA.. Predictors of health promoting lifestyles in persons with disabilities. Res Nurs Health 1994;17(1):3–13. [DOI] [PubMed] [Google Scholar]
- 25.Diener E, Emmons RA, Larsen RJ, Griffin S.. The Satisfaction with Life Scale. J Pers Assess 1985;49(1):71–5. [DOI] [PubMed] [Google Scholar]
- 26.Pavot W, Diener E.. The Satisfaction with Life Scale and the emerging construct of life satisfaction. J Posit Psychol. 2008;3(2):137–52. [Google Scholar]
- 27.Chen Y, Cao Y, Allen V, Richards JS.. Weight matters: physical and psychosocial well being of persons with spinal cord injury in relation to body mass index. Arch Phys Med Rehabil 2011;92(3):391–8. [DOI] [PubMed] [Google Scholar]
- 28.Becker H, Stuifbergen A, Oh HS, Hall S.. Self-rated abilities for health practices: a health self-efficacy measure. Health Values 1993;17(5):42–50. [Google Scholar]
- 29.Walker SN, Sechrist KR, Pender NJ.. The Health-Promoting Lifestyle Profile: development and psychometric characteristics. Nurs Res 1987;36(2):76–81. [PubMed] [Google Scholar]
- 30.Seekins T, Smith N, McCleary T, Clay J, Walsh J.. Secondary disability prevention: involving consumers in the development of a public health surveillance instrument. J Disabil Policy Stud 1990;1(3):21–36. [Google Scholar]
- 31.Cohen S. Perceived stress in a probability sample of the United States. 1988.
- 32.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health 1998;13(4):623–49. [Google Scholar]
- 33.Linden A. Assessing regression to the mean effects in health care initiatives. BMC Med Res Methodol 2013;13(1):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dijkers M. Quality of life after spinal cord injury: a meta analysis of the effects of disablement components. Spinal Cord 1997;35(12):829–40. [DOI] [PubMed] [Google Scholar]
- 35.Dush CMK, Amato PR.. Consequences of relationship status and quality for subjective well-being. J Soc Pers Relat 2005;22(5):607–27. [Google Scholar]
- 36.Stryker S, Burke PJ.. The past, present, and future of an identity theory. Soc Psychol Q 2000:284–97. [Google Scholar]
- 37.Sherbourne CD, Hays RD.. Marital status, social support, and health transitions in chronic disease patients. J Health Soc Behav 1990:328–43. [PubMed] [Google Scholar]
- 38.Craig A, Nicholson Perry K, Guest R, Tran Y, Middleton J.. Adjustment following chronic spinal cord injury: determining factors that contribute to social participation. Br J Health Psychol 2015;20(4):807–23. [DOI] [PubMed] [Google Scholar]
- 39.Sakakibara BM, Hitzig SL, Miller WC, Eng JJ.. An evidence-based review on the influence of aging with a spinal cord injury on subjective quality of life. Spinal Cord 2012;50(8):570–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krause JS, Newman JC, Clark JM, Dunn M.. The natural course of spinal cord injury: changes over 40 years among those with exceptional survival. Spinal Cord 2017;55(5):502. [DOI] [PubMed] [Google Scholar]