Abstract
Biological aging occurs concomitantly with chronological aging and is commonly burdened by the development of age-related conditions, such as neurodegenerative, cardiovascular, and a myriad of metabolic diseases. With a current global shift in disease epidemiology associated with aging and the resultant social, economic, and healthcare burdens faced by many countries, the need to achieve successful aging has fueled efforts to address this problem. Aging is a complex biological phenomenon that has confounded much of the historical research effort to understand it, with still limited knowledge of the underlying molecular mechanisms. Interestingly, dietary restriction (DR) is one intervention that produces anti-aging effects from simple organisms to mammals. Research into DR has revealed robust systemic effects that can result in attenuation of age-related diseases via a myriad of molecular mechanisms. Given that numerous age-associated diseases are often polygenic and affect individuals differently, it is possible that they are confounded by interactions between environmental influences and the genome, a process termed ‘epigenetics’. In part one of the review, we summarize the different variants of DR regimens and their corresponding mechanism(s) and resultant effects, as well as in-depth analysis of current knowledge of the epigenetic landscape.
Keywords: dietary restriction, epigenetics, aging, caloric restriction, intermittent fasting, fasting-mimicking diet, DNA methylation, histone modifications, histone remodelling, microRNAs
1.0. Introduction
Over recent decades, human life expectancy has improved significantly due to better medical care, hygiene, food abundance, and lower child mortality rate (Zheng et al., 2014; Brown, 2015; Crimmins, 2015; Lang and Rupprecht, 2019). However, an increase in the length of an individual’s life may not correspondingly result in added quality. Indeed, poor aging occurs when an increase in the number of years of survival is accompanied by the development of age-related conditions, such as cardiovascular, neurodegenerative, as well as metabolic diseases. Such a shift in global disease epidemiology associated with aging is now resulting in an increasing worldwide prevalence of disability, and is a burgeoning concern for many countries facing associated healthcare, social, and economic burdens (Niccoli and Partridge, 2012; Jaul and Barron, 2017; Franceschi et al., 2018; Kehler, 2019). As such, the ideal paradigm of achieving successful aging by reaching old age in good health has fuelled research into new approaches to ameliorate the development and manifestation of age-related diseases (Katz and Calasanti, 2015; Tesch-Römer and Wahl, 2017). Nevertheless, the complexity of the biological process of aging is such that our understanding of the underlying molecular mechanisms remains poor and so interventional strategies to improve lifespan and counter the development of age-associated diseases have been limited.
People around the globe have practiced voluntary abstinence from food since antiquity, including among many religious groups such as Buddhists, Hindus, Jews, Muslims, and Christians, where restriction of food practice is incorporated into traditions and rituals (Ri et al., 2012). Despite such prevalent observation of these practices in these groups, the effects energy restriction has on the human body remains quite poorly understood. It has been recently proposed that energy restriction could exert an evolutionary influence whereby our early ancestors were often challenged with extended periods of food restriction due to famine, and so procurement of food was accompanied by considerable physical activity. Thus, the fundamental needs for survival in terms of physical and mental maintenance without the consumption of food for extended periods may have shaped physiological, behavioural, and cognitive adaptations that have been inherited by modern humans in our genetic framework. Indeed, the current relative abundance of food coupled with our sedentary modern lifestyle, may be poorly compatible with the programmed genetic activity we have inherited. This may disrupt biochemical processes within the body, leading to biochemical derangements and ultimately contributing to the manifestation of a myriad of age-related diseases (Chakravarthy and Booth, 2004; Martin et al., 2010; Bake et al., 2014; Mattson et al., 2014, 2018; Lanktree and Hegele, 2017; Wayhart and Lawson, 2017) (Figure 1a). Indeed, extensive literature has shown unrestricted excessive energy intake provides the impetus for the development of age-related diseases (Uauy and Díaz, 2005). However, it is naïve to posit that starvation is a key to reverse the onset and development of chronic diseases because a balanced diet is critical for the proper maintenance of healthy physiological and metabolic functions, and individuals experiencing undernutrition often suffer from numerous health problems (Andersson and Bryngelsson, 2007; Skerrett and Willett, 2010). Interestingly, adoption of a dietary restriction (DR) regimen has garnered recent popularity, and it is indeed possible to voluntarily abstain from certain or total nutrients without compromising nutritional intake or energy balance. DR can promote beneficial effects on health and longevity, consistent with a potential for attenuation of age-related diseases through various molecular mechanisms (Harvey-Berino, 1999; Koubova and Guarente, 2003; Rogina and Helfand, 2004; Fontana et al., 2004; Guarente and Picard, 2005; Qin et al., 2006; Haigis and Guarente, 2006; John R.Giudicessi, BA.Michael J.Ackerman., 2008; Larson-meyer et al., 2009; Cruzen and Colman, 2009; Qiu et al., 2010b; Duan and A. Ross, 2010; Manzanero et al., 2011; Bake et al., 2014; Colman et al., 2014; Olivo-Marston et al., 2014; Pifferi et al., 2018; Mitchell et al., 2019).
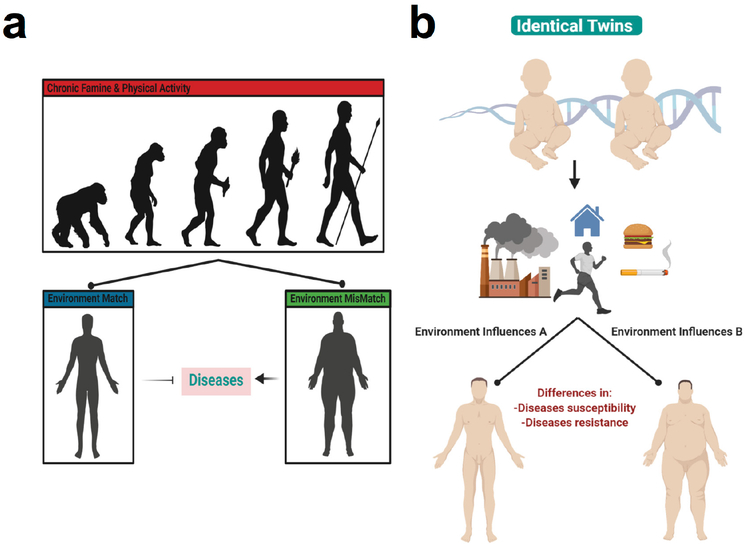
Figure 1.
Environmental Influences and Genetic Framework. (a) As our early ancestors were often challenged with periods of famine. And their procurement of food was accompanied by regular physical activity, they were presumably faced with periods of obligate food restriction and physical activity. The fundamental need for survival in terms of physical and mental maintenance without the consumption of food for extended periods appears to have shaped physiological, behavioural, and cognitive adaptations, and may thus have become inherited by modern humans within our genetic framework. As a result, the relative abundance of food coupled with our sedentary lifestyle today may be less compatible with the activity our evolutionarily programmed genes. As such, our modern lifestyle may disrupt our biochemical processes, and contribute to a myriad of age-related diseases. Thus, perhaps to some extent mimicking the environment of our ancestors may help to ameliorate the onset and development of diseases. (b) Twins possess high similarities in their genetic framework, yet when subjected to different environmental influences may acquire different traits that affect susceptibility to disease.
Epigenetics has gained widespread attention as a means to better understand how an invariant genome can in fact be programmed to adapt to different environmental influences. Twin studies have provided fascinating findings whereby two individuals with almost an identical genome who are subjected to different environmental influences may acquire different traits, which may in turn affect disease susceptibility or resistance (Poulsen et al., 2007; Bell and Spector, 2011; Dempster et al., 2011; Tan et al., 2015) (Figure 1b). Thus, despite our genetic code being ‘hard-wired’, it appears that our genome is not absolutely static but there is instead robust interaction with environmental influences through the heritability of diverse epigenetic marks. As aging is defined as a gradual and progressive decline in normal biological functions (Calvanese et al., 2009; Saldanha and Watanabe, 2015), this phenomenon may coincide with the progressive accumulation of diverse combinations of epigenetic signatures throughout life in response to a myriad of environmental influences. Such a process could underlie the development of diseases and various health outcomes plaguing the global population, especially in people with increasing age. We suggest that it is plausible that many polygenic diseases may be confounded by environmental influences or stochastic variables (Riaz et al., 2016). Indeed, numerous studies provide evidence that epigenetics may play a critical role in influencing biological aging and promoting the onset of age-related diseases (Calvanese et al., 2009; Saldanha and Watanabe, 2015). As a result, a better understanding of the interaction between our genetic framework and our environment using an ‘epigenetics perspective’ may be valuable. Although we cannot control our exposure to many environmental factors, our dietary intake is one factor that can be controlled to a large extent. DR is indeed considered an acceptable intervention by gerontologists and researchers in countering aging (Kirk, 2001; Masoro, 2006; Minor et al., 2010), and it is quite possible that DR acts partly or even substantially via epigenetic mechanisms. In the first part of the review on DR, we will introduce current knowledge of both DR and epigenetic signatures.
2.0. Dietary Restriction
DR is defined as a voluntary abstinence from consumption of a selected or entire nutrient composition without compromising energy balance or inducing malnutrition (Masoro, 1998; Robertson and Mitchell, 2013). As shown in Table 1, variants of DR regimens have emerged over the years, and can be broadly classified as either caloric restriction (CR) or intermittent fasting (IF) (Lee and Longo, 2016), as well as the new ‘fasting mimicking diet’ (FMD) (Wei et al., 2018).
Table 1:
Different Types and Effects of Dietary Restriction Regimens.
| Types of Dietary Restriction Regimens | Description | Effects on Lifespan | Effects on Diseases | References |
|---|---|---|---|---|
| Caloric Restriction |
|
Increase |
|
Bales and Kraus, 2013; Crowelll and Animal, 1935; Heilbronn and Ravussin, 2003; Harvey-Berino, 1999; Colman et al., 2008; Cruzen and Colman, 2009; Marzetti et al., 2009; Devlin et al., 2010; Han and Ren, 2010; Srivastava and Haigis, 2011; Zanto et al., 2011, 2011; Manzanero et al., 2011; O’Flanagan et al., 2017; Prehn et al., 2017; Pifferi et al., 2018; Yousefi et al., 2018; De Lucia et al., 2018; Duszka et al., 2018; Radakovich et al., 2019; Taylor, 2019. |
| Intermittent Fasting |
|
Increase |
|
Ganesan et al., 2018; Gabel et al., 2018; Stekovic et al., 2019;Wijngaarden et al., 2013; Collier, 2013; Fann et al., 2014, 2017; Chausse et al., 2015; Patterson et al., 2015; Wegman et al., 2015; Harvie and Howell, 2017; Anton et al., 2018; Kim et al., 2018; Groot et al., 2019. |
| Fasting Mimicking Diets |
|
No change in lifespan but extend health span |
|
Brandhorst et al., 2015; Wei et al., 2017, 2018; Cheng et al., 2018; Enyati et al., 2019. |
2.1. Caloric Restriction
CR is defined as a sustained eating pattern involving a reduction in day-to-day caloric intake by 15% to 40% as compared to ad libitum (AL). Notably, this method of DR does not result in malnutrition (Bales and Kraus, 2013). The ideology of CR spans many centuries, with notable figures promoting CR including Hippocrates, to whom is ascribed the notion: “Let food be thy medicine and medicine be thy food” (Square, 2002). Experimental studies that began much later first found CR to be able to extend lifespan and improving reproductive performance in CR as opposed to AL rats (CM et al., 1935). These experimental findings drove a renaissance of nutrition research, in which CR was found to positively impact longevity and health across multiple life forms, from simple organisms (such as yeast Saccharomyces cerevisiae, nematode Caenorhabditis elegans, and fruit fly Drosophila melanogaster) to vertebrates (such as mice Mus musculus and primates Macaca mulatta) (Heilbronn and Ravussin, 2003). Besides, CR has been shown to provide protection against numerous diseases, including slowing brain atrophy and preserving cognition, and protecting against neurodegenerative diseases (e.g. Alzheimer and Parkinson’s diseases), intestinal dysfunction, obesity, osteoporosis, arthritis, cardiovascular disorders (e.g. heart and stroke), diabetes, and sarcopenia, as well lowering the risk and progression of cancer (Harvey-Berino, 1999; Luchsinger et al., 2002; Colman et al., 2008; Cruzen and Colman, 2009; Marzetti et al., 2009; Devlin et al., 2010; Han and Ren, 2010; Longo and Luigi Fontana, 2010; Manzanero et al., 2011; Srivastava and C. Haigis, 2011; González et al., 2012; O’Flanagan et al., 2017; Prehn et al., 2017; Pifferi et al., 2018; Yousefi et al., 2018; De Lucia et al., 2018; Duszka et al., 2018; Radakovich et al., 2019; Taylor, 2019).
2.2. Intermittent Fasting
IF involves adjusting the temporal intake of food while maintaining isocaloric consumption overall (Ganesan et al., 2018). IF also has deep historical roots, with observance being reported in many religions for either spiritual reasons or physical benefits (Trepanowski and Bloomer, 2010; Patterson et al., 2015). IF is an umbrella term that encompasses different variants in the frequency of meal consumption. Time-restricted feeding (TRF) and alternate-day fasting (ADF) are examples of IF in which the timing of meals is varied. For TRF, daily meal consumption is restricted to a fixed window (such as a period of four to twelve hours) with nothing consumed outside of this window. ADF, on the other hand, extends the period of no or minimal calorie consumption (25% of energy needs), alternating between 24 hours of fasting and 24 hours of AL consumption. Another popular variant of IF is the 5:2 eating pattern, whereby during a 7 day period, unrestricted eating happens on five days in addition to two non-consecutive days of consumption of no or minimal calories (Gabel et al., 2018; Stekovic et al., 2019). Like CR, IF has been found to induce longevity across many animal models, as well as improving metabolic health. For instance, IF has been reported to influence the circadian clock, intestinal microbiota niche, and metabolic regulation controlling insulin sensitivity, lipid metabolism, hormonal changes, and inflammatory responses. This may lead to an improvement of metabolic function and may explain the development of resistance to cardiovascular diseases (e.g. heart attack and stroke), neurodegenerative diseases (e.g. Alzheimer disease), obesity, type II diabetes mellitus, and cancer (Wijngaarden et al., 2013; Collier, 2013; Fann et al., 2014, 2017; Chausse et al., 2015; Patterson et al., 2015; Wegman et al., 2015; Harvie and Howell, 2017; Anton et al., 2018; Kim et al., 2018; De Groot et al., 2019).
2.3. Fasting Mimicking Diet
Our current social and economic environment typically enables instant gratification from food-seeking to meet hunger, and this “obesogenic” model has made it more difficult for individuals to alter their eating patterns. The recently introduced FMD appears to be a combination of CR and IF, and it has arisen due to the lack of compliance in individuals to adhere to either CR or IF for a prolonged period. FMD is a form of periodic fasting that involves a monthly reduction in caloric intake through low carbohydrate and low protein consumption (~30% of energy needs) for five consecutive days and AL eating for the remaining calendar days, and can be practiced on a monthly or bimonthly basis. Notably, FMD has been shown to promote the extension of health span but not lifespan in rodents. FMD is also effective in enhancing neurocognitive function, and reducing a plethora of aging and disease markers, such as diabetes, cancer, and cardiovascular diseases (Brandhorst et al., 2015; Cheng et al., 2017; Wei et al., 2017, 2018; Rangan et al., 2019).
2.4. Mechanism of Dietary Restriction
From findings in less complex, short-lived organisms through to mammals, it is generally accepted that DR can be an effective non-genetic and non-pharmacological intervention against aging through increased longevity and delayed onset and development of chronic diseases. Those findings from DR studies across diverse organisms suggest an innate evolutionary conservation of either genes or molecular players that respond positively to DR. Indeed, studies that have begun to decipher the mechanisms of DR effects have revealed a plethora of conserved biological pathways and proteins that are modulated in response to a low energy status (Figure 2).
Figure 2.
Mechanism of Dietary Restriction. During DR there is a reduced energy status within the organism, resulting in corresponding decreases in blood glucose, insulin, IGF-1, growth hormones, sex hormones, and T3 thyroid hormones. Also, DR induces a reduction in both oxidative stress and inflammation. Following DR, there are increases in free fatty acids, adiponectin, and cortisol. A lower cellular energy status will lead to reduced mitochondrial activity and aerobic respiration, increasing the AMP:ATP ratio and NAD+ levels. Two major cellular nutrients and energy sensors, AMPK and SIRT1, will be then be activated, respectively. Activated AMPK will inhibit glycogen synthesis, ACC1, ACC2, and HMG-CoA to drive a reduction in fatty acid synthesis, oxidation, and cholesterol synthesis. Activated SIRT1 can enhance ketogenesis and lipolysis, and downregulate glycolysis and glutaminolysis. These effects may be also due to an activation of PPARα, reflecting direct and indirect functions of SIRT1. Activated SIRT1 can also repress the activity of PPARγ to modulate lipid metabolism and enhance fat mobilization in white adipose tissue during DR. Activated SIRT1 can inhibit NF-κB activity, inhibiting the expression of proinflammatory genes. SIRT1 activation is dependent on the increased interaction between FOXO3a and p53 at SIRT1 promoter sites. The physical interaction between FOXO3a and p53, and the subsequent activation of SIRT1, play important roles in repressing cell growth and proliferation. Notably, SIRT1 activation can activate LKB1, which will further activate AMPK, thus creating a positive feedback loop. Reduced levels of insulin, glucose and growth hormone downregulates insulin and IGF-R signaling pathways, inactivating the RAS/MAPK axis, repressing cell growth and proliferation and promoting apoptosis. Repression of IGF-R signaling will include the PI3K pathway, and inhibit downstream mTORC1, promoting autophagy. Inhibition of mTORC1 can also occur via activated AMPK in response to DR. Decreased mTORC1 function can promote ketogenesis and lipolysis, and repress glycolysis and glutaminolysis. Moreover, the corresponding decreased function of mTORC1 also inhibit HIF-1α, which downregulates key biological processes such as glucose metabolism, angiogenesis, and cell cycle progression. The NRF2 pathway is also triggered by DR, which helps to increase production of protective antioxidant enzymes and mitochondrial biogenesis to reduce ROS activity. With lower levels of ROS, there will be reduced DNA damage and a maintained genome stability. Lower energy status will prime cells to low-intensity stress, and this hormetic mechanism will stimulate better management of stress, upregulate DNA repair genes, as well as shifting towards a preferred setting of maintenance and repair (not shown). Overall, DR can act via these mechanisms to counter age-associated diseases and induce longevity.
DR, dietary restriction; IGF-1, insulin growth factor 1; AMP, adenosine monophosphate; ATP, adenosine triphosphate; NAD+, nicotinamide adenine dinucleotide; AMPK, adenosine monophosphate kinase; SIRT1, sirtuin 1 deacetylase; ACC1 and ACC2, acetyl-coenzyme A carboxylase 1 and 2; HMG-CoA, 3-hydroxy-3-methyl-glutaryl-coenzyme A; PPARα and PPARγ, peroxisome proliferator-activated receptor gamma alpha and gamma; NF-κB, nuclear factor kappa-light-chain-enhancer of activated B cells; FOXO3a, forkhead box O3; LKB1, liver kinase B1; IGF-R, insulin growth factor receptor; RAS/MAPK, mitogen-activated protein kinase; PI3K, phosphoinositide 3-kinase; mTORC1, mammalian target of rapamycin complex 1; HIF-1α, hypoxia-inducible factor 1 alpha; NRF2, nuclear factor erythroid 2-related factor 2 ;ROS, reactive oxygen species.
DR exerts pleiotropic cellular effects, inducing a reduced energy status within the organism, and a corresponding decrease in blood glucose, insulin, insulin-like growth factor 1 (IGF-1), growth hormones, sex hormones, and T3 thyroid hormones levels. Also, DR induces a reduction in both oxidative stress and inflammation. Moreover, following DR, an increase in free fatty acids, adiponectin, and cortisol can be observed (Ungvari et al., 2008; Redman et al., 2010; Abedelmalek et al., 2015; Lan et al., 2015; Kapahi et al., 2017).
A reduced cellular energy status will lead to lower mitochondrial activity and thus aerobic respiration, and corresponding increases in the adenosine monophosphate and adenosine triphosphate (AMP:ATP) ratio, and in nicotinamide adenine dinucleotide (NAD+) levels. In turn, two major cellular nutrients and energy sensors, adenosine monophosphate kinase (AMPK) and sirtuin 1 deacetylase (SIRT1), will be activated, respectively (Haigis and Guarente, 2006; Hatori et al., 2012; Marcinko and Steinberg, 2014). Activated AMPK will then inhibit glycogen synthesis, as well as acetyl-coenzyme A carboxylase 1 and 2 (ACC1 and ACC2) and 3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) to reduce fatty acid synthesis, oxidation, and cholesterol synthesis (Motoshima et al., 2006; Thomson and Winder, 2009; Marcinko and Steinberg, 2014; Jeon, 2016; Foretz et al., 2018). Activated SIRT1 can enhance ketogenesis and lipolysis, and downregulate glycolysis and glutaminolysis (Pedersen et al., 2008; Chakrabarti et al., 2011; Chang, Hung-Chun; Guarente, 2012; Zhu et al., 2013). These effects may be also due to an activation of peroxisome proliferator -activated receptor alpha (PPARα), which suggests that SIRT1 can exert both direct and indirect functions. Activated SIRT1 can also repress the activity of peroxisome proliferator-activated receptor gamma (PPARγ), which will in turn modulate lipid metabolism and enhance fat mobilization in white adipose tissue during DR. Depending on the PPAR isoforms, it appears that SIRT1 can exert pleotropic effects on PPAR in response to DR (Purushotham et al., 2009; Hayashida et al., 2010; Picard et al., 2012; Bonzo et al., 2014; Khan et al., 2015). Furthermore, activated SIRT1 can also inhibit the activity of nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), inhibiting the expression of proinflammatory genes (Gillum et al., 2011; Ghisays et al., 2015). SIRT1 activation is dependent on the increased interaction between forkhead box O3 (FOXO3a) and p53 at SIRT1 promoter sites during periods of nutrient deficiency, such as during DR. Thus, SIRT1 activation during DR can be regulated via the NAD+ or the FOXO3a axis. Furthermore, the physical interaction between FOXO3a and p53, as well as the subsequent activation of SIRT1, have been found to play key roles in repressing cell growth and proliferation (Hori et al., 2013; Manuscript, 2013; Zhang et al., 2014). Notably, SIRT1 activation can also activate liver kinase B1 (LKB1), which will further activate AMPK, thus creating a positive feedback loop (Wang et al., 2011; Laboratory, 2012).
When cells detect a corresponding drop in the levels of insulin, glucose, growth hormones, insulin, and insulin-like growth factor receptor (IGF-R) signaling pathways are downregulated (Straus and Takemoto, 1990; Cheng et al., 2014). As a result, DR can also inactivate the mitogen-activated protein kinase (RAS/MAPK) axis, to repress cell growth and proliferation and promote apoptosis (Morikawa et al., 2004; Fuentes et al., 2012). Repression of IGF-R signaling will also repress the phosphoinositide 3-kinase (PI3K) pathway and the downstream mammalian target of rapamycin complex 1 (mTORC1), promoting autophagy. Notably, inhibition of mTORC1 can also occur by activated AMPK in response to DR. Decreased mTORC1 function can promote ketogenesis and lipolysis and inhibit glycolysis and glutaminolysis, as in SIRT1-induced activation of PPARα (De Paula et al., 2017; Sabatini, 2017; Tulsian et al., 2018). Moreover, decreased function of mTORC1 inhibit hypoxia-inducible factor 1 alpha (HIF-1α), which in turn downregulates key biological processes such as glucose metabolism, angiogenesis, and cell cycle progression (Parsons, 2001; Laplante and Sabatini, 2013; Saxton and Sabatini, 2017). The nuclear factor erythroid-2-related factor 2 (NRF2) pathway is also triggered by DR and it contributes to increases in production of protective antioxidant enzymes and mitochondrial biogenesis and reduction of reactive oxygen species (ROS). With reduced ROS levels there will be less DNA damage and improved maintenance of genome stability (Kulkarni et al., 2014). Lower energy status will also prime cells to low-intensity stress, a hormetic mechanism that can facilitate better management of stress, upregulate DNA repair genes, and shift towards a preferred status of maintenance and repair (Kouda and Iki, 2010; Horne BD, Muhlestein JB, 2015).
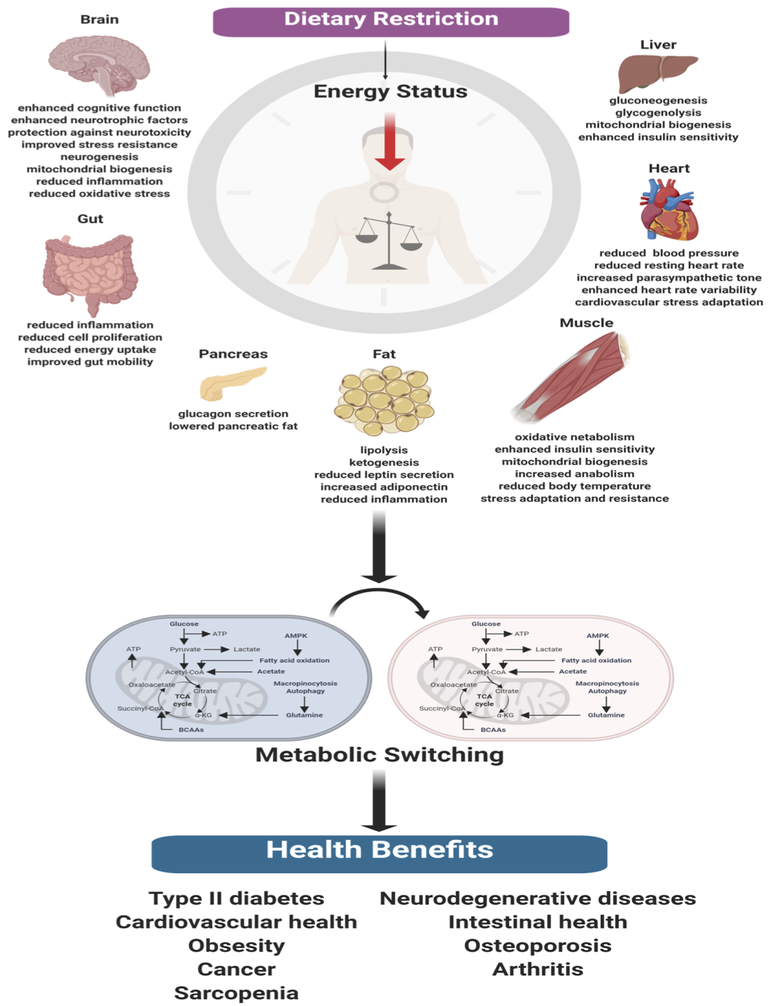
Systemic effects on major organs are also known to occur in response to DR via these molecular and cellular adaptations. In the brain, DR has been reported to enhance cognitive function and neurotrophic factor release, serving to protect against neurotoxicity and improve stress resistance. DR can also promote neurogenesis and mitochondrial biogenesis, and reduce inflammation and oxidative stress within the brain (Qiu et al., 2010; Kynjai et al., 2019). Within the gut, DR promotes gut mobility, and induces a reduction in inflammation, cell proliferation, and energy uptake (Brennan et al., 2011; Ott et al., 2017; Id et al., 2018; Lian et al., 2018). On the other hand, in DR the pancreas comprises less fat and there is promotion of glucagon secretion (Anton et al., 2018; Jiang et al., 2019). Moreover, DR upregulates lipolysis and ketogenesis within adipose tissue, increasing adiponectin synthesis and decreasing leptin secretion (Ding et al., 2012; Rogozina et al., 2012; Fabbiano et al., 2016). In skeletal muscle, oxidative metabolism is shifted preferentially towards increased anabolism, with a corresponding enhancement of insulin sensitivity, mitochondrial biogenesis, reduced body temperature, as well as stress adaptation and resistance in response to DR (Usuki et al., 2004; Hempenstall et al., 2012; Chen et al., 2015; Mitchell et al., 2015; Martins et al., 2018; Faitg et al., 2019). In the heart and vasculature, there is a reduced blood pressure and resting heart rate induced by DR, with increased parasympathetic tone, reduced heart rate variability, and improved cardiovascular stress adaptation (Weiss and Fontana, 2011; Stein et al., 2012; Shinmura, 2013; Nicoll and Henein, 2018). Finally, in response to DR the liver triggers gluconeogenesis, glycogenolysis, mitochondrial biogenesis, and enhanced insulin sensitivity (Hell et al., 1980; Weindruch et al., 1980; Hagopian et al., 2003; Browning et al., 2008; Kirk et al., 2010).
In summary, DR triggers a lower energy status within the organism, which in turn commonly induces robust metabolic switching in major organs (Webster et al., 1972; Millward et al., 1974; Camps et al., 1992; Trayhurn et al., 1995; Mattson and Wan, 2005; Longo and Mattson, 2014; Bujak et al., 2015; Mattson et al., 2017). The resulting systemic changes occur via molecular, cellular, and metabolic adaptations, and may promote longevity and delay the onset and development of many age-associated diseases (Figure 3).
Figure 3.
Effects of Dietary Restriction. DR can induce a myriad of systemic effects. In turn, a robust metabolic switching ensues, which results in molecular, cellular, and metabolic adaptations that delay the onset and development of many age-associated diseases and promote longevity.
3.0. Epigenetics
Epigenetics is an emerging field of knowledge relating to the complex interactions between genome and environment, defined as mitotically and meiotically heritable genetic changes without corresponding changes to the invariant DNA sequence (Panawala et al., 2017; Ng et al., 2018). These epigenetic effects on the genome occur via enzymatic modifications to either the DNA sequence directly or through histone proteins that form part of the hierarchical packing of the chromosomal DNA (Figure 4). Gene expression can then be modulated directly or indirectly via an overall modification towards the chromatin structure and accessibility. The landscape of epigenetic signatures across the genome is termed the ‘epigenome’, with these unique epigenetic tags functioning as distinct microdomains within the nucleus to differentially regulate patterns of gene expression (Qureshi and Mehler, 2010). The overall epigenome status within the nucleus can be also be considered as a ‘tug-of-war’, whereby each epigenetic modification can either promote or inactivate gene expression. The overall direction of gene expression is thereby dependent on the sum of these dynamic interactions. For didactic purposes, these epigenetic modifications can be broadly categorized to comprise DNA methylation, histone protein modifications, histone remodeling complexes, as well as involvement of microRNAs.
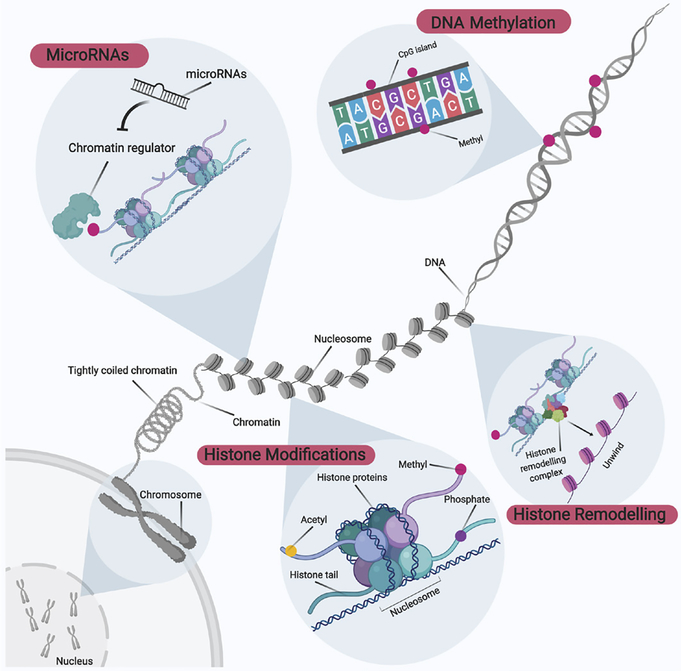
Figure 4.
Overview of Epigenetic Modifications. Epigenetic modifications can be broadly categorized into DNA methylation, histone modifications, histone remodeling, and microRNA involvement. These epigenetic modifications to the genome occur via enzymatic modifications to either the DNA sequence directly or through histone proteins that form part of the hierarchical packing of the chromosomal DNA. In turn, gene expression can be modulated directly or indirectly via an overall modification to chromatin structure and accessibility. The epigenetic signature landscape across the genome is collectively termed the ‘epigenome’, and unique epigenetic tags function as distinct microdomains within the nucleus to regulate differential patterns of gene expression.
3.1. DNA Methylation
DNA methylation is the principal epigenetic modification at the DNA sequence level (Figure 4 and 5). The double helical DNA structure is composed of a combinational sequence of four nucleotide bases; namely thymine, adenine, cytosine, and guanine. DNA methylation involves the principal tagging of a methyl group to carbon position five of the cytosine ring, and this process tends to occur at higher frequency in regions termed CpG dinucleotide islands. CpG islands are genomic regions spanning more than 500-base pairs of DNA and are often located at gene promoter regions which are enriched near the 5’ gene transcript. The characterization of CpG islands falls into two categories; the composition of both cytosine and guanine appears to occupy above 55% in these 500-base pairs region, or CG:GC observed frequency ratio to be at least 0.6. DNA methylation can also occur in other regions called ‘CpG shores’, defined as lower density CpG islands residing downstream by approximately 2 kb (Portela and Esteller, 2010a). Conventionally, DNA methylation was thought to occur only at CpG islands, but recent findings indicate its occurrence in CpG shores shown the complexity underlying this form of regulation. While cytosine nucleotides are scattered across the genome, DNA methylation distribution is asymmetrical and considered to be relatively rare, especially in the mammalian genome, accounting for only 1% of the genome size (Cooper et al., 2010). This is thought to be due to the fact that the addition of a methyl group to cytosine to form 5-methylcytosine is inherently genetically unstable. 5-methylcytosine cannot be excised from the genome or recognized by the DNA repair system. To counter this, 5-methylcytosine undergoes spontaneous deamination to yield a thymine, yet become prone to transition mutations. As a result, CpG islands have evolved to be depleted across the genome and account for very low proportions to decrease the risk of becoming mutational hotspots (Cooper et al., 2010).
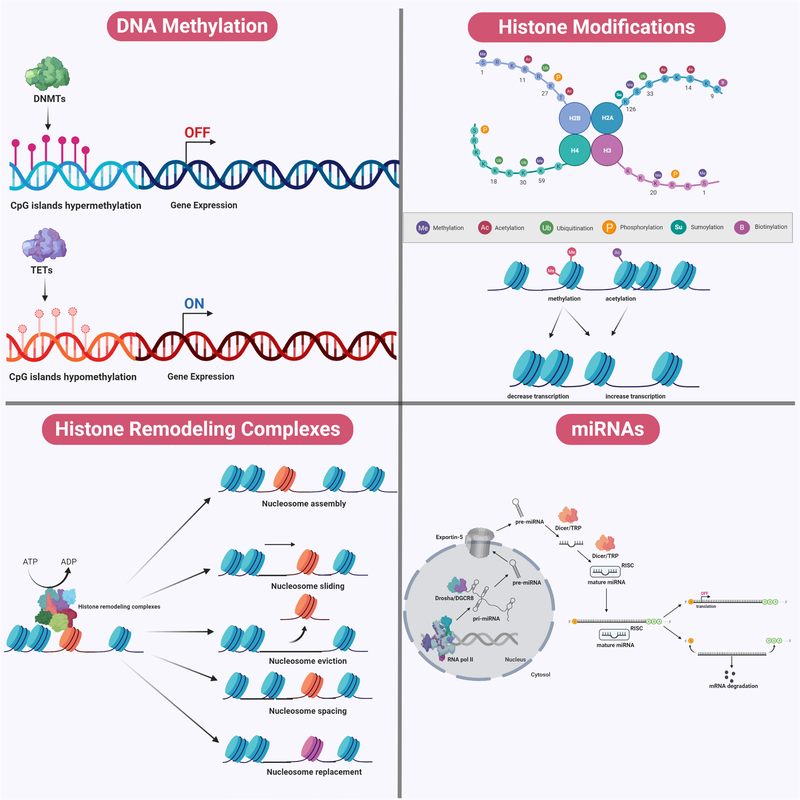
Figure 5.
Mechanisms of Epigenetic Modifications. During DNA methylation, a methyl group is added to carbon position five of the cytosine ring at either CpG dinucleotide islands or CpG shores. DNA methylation is catalyzed by DNMTs, whereas DNA demethylation is catalyzed by TETs. DNA methylation tends to be associated with gene silencing whereas DNA demethylation is associated with transcriptional activation. Chromosomal DNA within the eukaryotic genome is often interlaced with distinct packing and folding, resulting in a distinct organizational structure. At the fundamental level, a nucleosome structural core is first formed through wrapping of a 147 base-pair double helical DNA around an octamer of histone proteins consisting of pairs of H2A-H2B dimers and H3-H4 dimers. Between two nucleosome cores, DNA that is not wrapped around nucleosomes is referred to as ‘linker DNA’, which tends to be associated with H1 histone proteins. A plethora of post-translational modifications (such as acetylation, methylation, phosphorylation, sumoylation, biotinylation, and ubiquitination) can occur on the amino terminal tail protruding from each histone subunit within the nucleosome complex. These histone modifications can affect the relative packing of DNA around these nucleosome cores, and may determine the relative accessibility for the machinery to initiate replication and transcription. Chromatin structure can be modified by ATP-dependent histone remodeling complexes, using the energy from ATP hydrolysis to locally disrupt the interaction between DNA and histones. These remodelers mediate alterations to chromatin structure via nucleosome sliding, eviction, assembly, spacing, histone dimers eviction or replacement, and even entire histone replacement. In addition, miRNAs demonstrate complementary interaction with specific genes and modulate gene expression. Cellular miRNAs are synthesized in a sequential manner and occur in both the nucleus and the cytosol. Within the nucleus, the genome comprises numerous miRNA genes transcribed by RNA polymerase II to form a single large pri-miRNA transcript. Because this pri-miRNAs transcript consists of multiple miRNA loci, it undergoes further processing by a complex called Drosha/DGCR8, a class of RNaseIII enzymatic complex, to generate shorter hairpin-loop structurers termed ‘pre-miRNAs’. This pri-miRNA is exported into the cytosol by Exportin-5 in a RAN-GTP dependent manner. Within the cytosol, another complex belonging to another class of RNaseIII enzymes, termed ‘Dicer/TRBP’ exert its action. Dicer processes the pri-miRNAs into a duplex of mature miRNAs, which undergoes asymmetrical unwinding by the Dicer/TRBP complex to yield a single-stranded mature miRNA. This single-stranded form loads itself into a ribonucleoparticle to yield an RISC, which is the active form of the gene silencing complex. Together, the single-stranded mature miRNAs within the RISC complex will identify the 3’-UTR of targeted mRNAs. The mode of action of gene silencing mediated by miRNAs can occur in two ways, depending on its complementarity with the targeted mRNAs. miRNAs which bind to targeted mRNAs in perfect complementarity induce rapid deadenylation and decapping, leading to mRNA degradation. An imperfect complementarity binding of miRNAs to targeted mRNAs result in translational suppression.
DNMTs, DNA methyltransferase; TETs, ten-eleven translocation; pri-miRNAs, primary miRNA; pre-miRNAs, precursor miRNAs; RISC, RNA-induced silencing complex; 3’-UTR, 3’ untranslated region.
DNA methylation is catalyzed by an important family of enzymes called DNA methyltransferases (DNMT) (Moore et al., 2013). The DNMT family consists of five members, of which only three (DNMT1, DNMT3a, and DMNT3b) possess enzymatic activity. DNMT3a and DNMT3b catalyze de novo methyl group transfer from S-adenosyl methionine to CpG sites, whereas DNMT1 is mostly important for the maintenance of the overall DNA methylation landscape across the genome (Kim et al., 2009; Feng et al., 2010). The conversion and maintenance of methionine and folate to S-adenosyl methionine are mediated by a group of enzymes called methylenetetrahydrofolate reductases (MTHFR). Besides DNA methylation, S-adenosylmethionine also plays important roles in DNA synthesis (Alluri et al., 2005; Daniels et al., 2007; Zhou et al., 2014). On the other hand, the process of DNA demethylation at 5-methylcytosines to 5-hydroxymethylcytosines is mediated by ten-eleven translocation (TET) enzymes in a locus-specific manner. However, these groups of enzymes have only recently become known in the field of epigenetics and understanding of their functions remains poor (Figure 5) (Xu and Wong, 2015).
The effects of DNA methylation have often been linked to transcriptional inactivation via various mechanisms. DNA methylation can directly block the binding of specific DNA binding factors to transcriptional start sites and as a result halt transcription. In another instance, 5-methylcytosines within CpG sites are often recognized by protein families possessing conserved methyl-CpG-binding domains (MBD). Binding of these proteins may in turn recruit a combination of transcriptional corepressors, polycomb proteins, or even chromatin remodeling complexes to bring about transcriptional repression (Huck-Hui and Bird, 1999; Du et al., 2015). Besides playing a conventional role in the area of gene silencing, DNA methylation has been implicated in many biological processes such as genomic imprinting and stability, X chromosome inactivation, differentiation, and development (Moore et al., 2013; Wu and Zhang, 2014).
3.2. Histone Modifications and Remodeling
Chromosomal DNA within the eukaryotic genome is often interlaced with distinct packing and folding, resulting in distinct organizational structure (Figure 4 and 5). At the fundamental level, a nucleosome structural core is first formed through wrapping of a 147 base-pair double helical DNA around an octamer of histone proteins consisting of pairs of H2A-H2B dimers and H3-H4 dimers. This interaction is mediated by the positive charges within the rich pool of lysine and arginine residues in histone proteins, as well as the negatively charged sugar phosphate backbone of DNA. Between two nucleosome cores, DNA that is not wrapped around nucleosomes is referred to as linker DNA. This linker DNA tends to be associated with H1 histone proteins (Zhang and Reinberg, 2001; Boyanapalli and Kong, 2015). The globular structure of histone proteins within nucleosome complexes represents a form of steric hindrance that may impede the accessibility of DNA replication and transcriptional machinery to genomic sites. As a result, the relative packing of DNA around these nucleosome cores may determine the relative accessibility for the machinery to initiate replication and transcription. Therefore, at the genomic level, two defined areas of DNA can be classified depending on the relative packing of DNA; namely euchromatin and heterochromatin. Euchromatin regions are generally characterized by a more spacious chromatin structure which in turn exhibits higher transcriptional rates, whereas heterochromatin regions demonstrate transcriptional silence via tight packing of chromatin (Tamaru, 2010).
The relative transition between these two states is highly dependent on post-translational modifications that can occur on the amino terminal tail protruding from each histone subunit within the nucleosome complex. Histone modifications tend to be short-term and reversible and are readily modulated by external environmental changes (Cedar and Bergman, 2009; Handy et al., 2011; Qureshi, 2011). A myriad of post-translational modifications (such as acetylation, methylation, phosphorylation, sumoylation, biotinylation, and ubiquitination) catalyzed by a plethora of enzymes have been reported to occur at specific amino acid sites within each histone. Each histone modification in turn will determine a critical function, which translates to distinct cellular outcomes (Figure 5). As such, the sum of all histone modifications (termed ‘histone codes’) will determine the overall changes at the cellular level, such as chromatin assembly, transcriptional activation or repression, telomere dynamics, DNA repair, cell cycle, as well as apoptosis (Lennartsson and Ekwall, 2009; Portela and Esteller, 2010). For didactic purposes, two well-studied examples of histone modifications, namely acetylation and methylation, will be discussed to more fully describe the mechanism and complexity underlying histone modifications.
Histone acetylation involves the covalent addition of an acetyl group to a histone tail lysine residue at a conserved epsilon-amino group and is often mediated by a family of enzymes called histone acetyltransferases (HATs). Upon histone acetylation, a synergistic interaction with histone remodeling complexes may be formed with HATs, which in turn weakens the interaction between DNA and histone proteins, thus promoting nucleosome sliding away from DNA, facilitating less packing of chromatin and higher accessibility of transcriptional machinery and activity (Figure 5). By contrast, the removal of acetyl groups from histones is mediated by histone deacetylases (HDACs), which may in turn recruit transcriptional repressors to downregulate transcription via promotion of tighter packing of chromatin (Legube and Trouche, 2003). Histone acetylation and deacetylation at various sites has been reported to be critical for a plethora of biological roles besides transcription, such as histone deposition, chromatin assembly, transcriptional elongation, telomeric silencing, and DNA repair (Tamburini and Tyler, 2005; Zhao et al., 2005; Gong and Miller, 2013; Church and Fleming, 2018).
On the other hand, methylation of histone involves the addition of methyl groups to histone amino terminal tails via the actions of histone methyltransferases (HMTs), with preferential addition to either lysine or arginine residues (Zhang and Reinberg, 2001; Chakravarty et al., 2017). However, effects arising from histone methylation are often diverse and complex, depending on the type or position of amino acid residues that are methylated, and the number of methyl groups added within each specific locus (Figure 5). For instance, at specific lysine residues, methyl groups can be added singly, twice or three times, whereas at specific arginine residues methyl groups can be added either once or twice. This complexity is confounded in that certain methylated residues, such as di-methylated arginine residues, often demonstrate stereo topological layout, either as symmetrical or asymmetrical, which may produce diverse functions (Chen et al., 2012; Chakravarty et al., 2017). Given that enormous complexity occurs as a result of the possible permutations and combinations of histone methylation tags, it is difficult to predict biological effects arising from this post-translational modification. Nevertheless, many studies have shown that histone methylation plays important roles in transcriptional activation and repression, transcriptional elongation, genomic imprinting, checkpoint response, and X chromosome inactivation (Miloucheva, 2002; Chen and Zhu, 2016).
Chromatin structure within the eukaryotic genome can be modified not only by histone enzymatic modifications, but also through the actions of histone remodeling complexes (Figure 4 and 5). These complexes are referred to as ATP-dependent remodeling complexes, using the energy from ATP hydrolysis to locally disrupt the interaction between DNA and histones. The first histone remodeling complex gene was discovered during genetic screening of S. cerevisiae, and subsequently termed switching-defective 2 (SWI2) or sucrose non-fermenting 2 (SNF2). The SWI/SNF2 complex was found to mediate alterations in chromatin structure that led to transcriptional activation (Vignali et al., 2000). Besides the SWI/SNF2 family, three other families of remodelers have now been identified; namely the imitation-switch (ISWI), chromodomain helicase DNA-binding (CHD), and inositol-requiring 80 (INO80). These four identified families of remodelers share a high degree of conservation of an innate ATPase-helicase domain and can function as either a monomer (e.g. CHD1) or as a distinct macromolecular complex (e.g. ISWI). These complexes can be made up of different combinations of subunits, and may be accompanied by distinct microdomains. Depending on their composition, histone remodeling complexes can exert synergistic or antagonistic biochemical and genetic functions (Pillus, 2015). Moreover, these remodelers can mediate alterations in chromatin structure via nucleosome sliding, eviction, assembly, spacing, histone dimers eviction or replacement, and even entire histone replacement (Figure 5). Furthermore, histone modifications and histone remodeling complexes do not only function independently. It has been reported that complexes such as ISWI and CHD1 can also interact with histone modifiers and histone modifications, resulting in diverse functions. As such, the dynamic kinetics of nucleosome positions within the eukaryotic genome will impact key biological processes, such as regulation of gene expression, DNA replication and repair, and homologous recombination events (Vignali et al., 2000; Liu et al., 2012; Narlikar et al., 2013; Pillus, 2015; Tyagi et al., 2016; Zhang et al., 2016; De Castro et al., 2017; Stadler and Richly, 2017).
3.3. MicroRNAs
MicroRNAs (miRNAs) constitute an important class of noncoding RNA and are defined as short (18–25 nucleotides in length), single-strand molecules which exert their actions at the post-transcriptional level (Figure 4 and 5). miRNAs demonstrate complementary interaction with specific genes and can modulate gene expression. Cellular miRNAs are synthesized in a sequential manner and occur in both the nucleus and the cytosol. Within the nucleus, the genome comprises numerous miRNAs genes which will be transcribed to form a single large primary miRNA (pri-miRNAs) transcript by RNA polymerase II. Because this pri-miRNA transcript consists of multiple miRNA loci, it undergoes further processing by a complex called Drosha/DGCR8, a class of RNaseIII enzymatic complex, to generate shorter hairpin-loop structures termed as precursor miRNAs (pre-miRNAs). This pre-miRNA is exported into the cytosol by Exportin-5 in a RAN-GTP dependent manner. Within the cytosol, another complex belonging to another class of RNaseIII enzymes termed ‘Dicer/TRBP’ exerts its action. First, Dicer processes pre-miRNAs into a duplex of mature miRNAs, which undergoes asymmetrical unwinding by the Dicer/TRBP complex to yield a single-stranded mature miRNA. It will then load itself into a ribonucleoparticle to yield an RNA-induced silencing complex (RISC), which is the active form of the gene silencing complex (Figure 5) (Chuang and Jones, 2007; Moutinho and Esteller, 2017; Yao et al., 2019).
Together, the single-stranded mature miRNAs within the RISC complex identify the 3’ untranslated region (3’-UTR) of targeted mRNAs. Gene silencing by miRNAs can occur in two ways, depending on its complementarity with the targeted mRNAs. miRNAs which bind to targeted mRNAs with perfect complementarity induce rapid deadenylation and decapping, which leads to mRNA degradation. On the other hand, an imperfect complementarity binding of miRNAs to targeted mRNAs tends to result in translational suppression. While the activity of miRNAs tends to result in gene downregulation, miRNAs may also promote gene upregulation. For instance, a group of miRNAs can bind to 5’ untranslated region (5’-UTR) of targeted mRNAs to promote ribosomal protein expression, aiding in translation. Interestingly, given that miRNAs are short and can only recognize partial sequences within targeted mRNAs, miRNAs can perform its function simultaneously in a plethora of mRNAs and yet produce diverse outcomes in a cell-dependent manner (Figure 5). Besides modulating the level of gene expression, miRNAs can regulate key epigenetic remodelers such as DNMTs, TETs, HDACs, and HMTs. Notably, this epigenetic regulation by miRNAs is not one-sided, as the expression of miRNAs can be modulated by a myriad of factors, such as DNA methylation, histone modifications, and transcription factors (Figure 4 and 5). Given the complicated mode of action of miRNAs, it is not surprising that miRNAs play diverse roles in many biological processes such as cellular proliferation, differentiation, development, metabolic processes, and apoptosis (Chuang and Jones, 2007; Qureshi, 2011; Udali et al., 2013; Khoshnam et al., 2017; Moutinho and Esteller, 2017; Yao et al., 2019).
4.0. Conclusion
DR has a long historical root and has been practiced by many groups since antiquity. Research on the biological effects of DR and its underlying mechanisms has only become commonplace relatively recently, but has gained enormous interest as a potential ‘holy grail’ for extension of health and lifespan. Supporting evidence has come from studies of many organisms, and have identified a plethora of molecular players and signaling pathways induced or modulated by DR associated with profound metabolic effects that appear capable of counteracting the onset and development of disease. However, the nature of DR-induced effects is complex and often varied and non-translatable between different organisms. Given that DR is a non-pharmacological and non-genetic lifestyle intervention that be readily adopted by many individuals, it is appears that DR represents an environmental stressor that can truly influence an individual’s epigenetic landscape. Hence, it is paramount to also investigate the nature of epigenetic signatures, and the detailed relationship between both DR and epigenetics will be discussed in part two of this review.
Acknowledgments
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The Singapore National Medical Research Council Research Grants (NMRC-CBRG-0102/2016 and NMRC/OFIRG/0036/2017) supported this work.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abedelmalek S, Chtourou H, Souissi N, Tabka Z (2015) Caloric restriction effect on proinflammatory cytokines, growth hormone, and steroid hormone concentrations during exercise in judokas. Oxid Med Cell Longev 2015:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alluri RV, Mohan V, Komandur S, Chawda K, Chaudhuri JR, Hasan Q (2005) MTHFR C677T gene mutation as a risk factor for arterial stroke: A hospital based study. Eur J Neurol 12:40–44. [DOI] [PubMed] [Google Scholar]
- Andersson A, Bryngelsson S (2007) Towards a healthy diet: from nutrition recommendations to dietary advice. Scand J Food Nutr 51:31–40. [Google Scholar]
- Anton SD, Moehl K, Donahoo WT, Marosi K, Lee SA, Mainous AG, Leeuwenburgh C, Mattson MP (2018a) Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity 26:254–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anton SD, Moehl K, Donahoo WT, Marosi K, Lee SA, Mainous AG, Leeuwenburgh C, Mattson MP (2018b) Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity 26:254–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bake T, Morgan DGA, Mercer JG (2014) Feeding and metabolic consequences of scheduled consumption of large, binge-type meals of high fat diet in the Sprague-Dawley rat. Physiol Behav 128:70–79 Available at: 10.1016/j.physbeh.2014.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bales CW, Kraus WE (2013) Caloric restriction: Implications for human cardiometabolic health. J Cardiopulm Rehabil Prev 33:201–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell JT, Spector TD (2011) A twin approach to unraveling epigenetics. Trends Genet 27:116–125 Available at: 10.1016/j.tig.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonzo JA, Brocker C, Jiang C, Wang RH, Deng CX, Gonzalez FJ (2014) Hepatic sirtuin 1 is dispensable for fibrate-induced peroxisome proliferator-activated receptor-α function in vivo. Am J Physiol - Endocrinol Metab 306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyanapalli SSS, Kong ANT (2015) “Curcumin, the King of Spices”: Epigenetic Regulatory Mechanisms in the Prevention of Cancer, Neurological, and Inflammatory Diseases. Curr Pharmacol Reports 1:129–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandhorst S et al. (2015) A Periodic Diet that Mimics Fasting Promotes Multi-System Regeneration, Enhanced Cognitive Performance, and Healthspan. Cell Metab 22:86–99 Available at: 10.1016/j.cmet.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan IM, Seimon RV, Luscombe-marsh ND, Otto B, Horowitz M (2011) Effects of acute dietary restriction on gut motor, hormone and energy intake responses to duodenal fat in obese men. Int J Obes 35:448–456. [DOI] [PubMed] [Google Scholar]
- Brown GC (2015) Living too long: The current focus of medical research on increasing the quantity, rather than the quality, of life is damaging our health and harming the economy. EMBO Rep 16:137–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning JD, Weis B, Davis J, Merritt M, Malloy CR, Burgess SC (2008) Alterations in Hepatic Glucose and Energy Metabolism as a Result of Calorie and Carbohydrate Restriction. Hepatology 48:1487–1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bujak AL, Crane JD, Lally JS, Ford RJ, Kang SJ, Rebalka IA, Green AE, Kemp BE, Hawke TJ, Schertzer JD, Steinberg GR (2015) AMPK activation of muscle autophagy prevents fasting-induced hypoglycemia and myopathy during aging. Cell Metab 21:883–890 Available at: 10.1016/j.cmet.2015.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunney PE, Zink AN, Holm AA, Billington CJ, Kotz CM (2017) Orexin activation counteracts decreases in nonexercise activity thermogenesis (NEAT) caused by high-fat diet. Physiol Behav 176:139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvanese V, Lara E, Kahn A, Fraga MF (2009) The role of epigenetics in aging and age-related diseases. Ageing Res Rev 8:268–276. [DOI] [PubMed] [Google Scholar]
- Camps M, Castello A, Munoz P, Monfar M, Testar X, Palacin M, Zorzano A (1992) Effect of diabetes and fasting on GLUT-4 (muscle/fat) glucose-transporter expression in insulin-sensitive tissues. Heterogeneous response in heart, red and white muscle. Biochem J 282:765–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cedar H, Bergman Y (2009) Linking DNA methylation and histone modification: patterns and paradigms. Nat Genet 10:295–304. [DOI] [PubMed] [Google Scholar]
- Chakrabarti P, English T, Karki S, Qiang L, Tao R, Kim J, Luo Z, Farmer SR, Kandror KV. (2011) SIRT1 controls lipolysis in adipocytes via FOXO1-mediated expression of ATGL. J Lipid Res 52:1693–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakravarthy MV, Booth FW (2004) Eating, exercise, and “thrifty” genotypes: Connecting the dots toward an evolutionary understanding of modern chronic diseases. J Appl Physiol 96:3–10. [DOI] [PubMed] [Google Scholar]
- Chakravarty S, Jhelum P, Bhat UA, Rajan WD, Maitra S, Pathak SS, Patel AB, Kumar A (2017) Insights into the epigenetic mechanisms involving histone lysine methylation and demethylation in ischemia induced damage and repair has therapeutic implication. Biochim Biophys Acta - Mol Basis Dis 1863:152–164 Available at: 10.1016/j.bbadis.2016.09.014. [DOI] [PubMed] [Google Scholar]
- Hung-Chun Chang; Guarente L (2012) SIRT1 and other sirtuins in Metabolism Hung-Chun. 76:211–220. [Google Scholar]
- Chausse B, Vieira-Lara MA, Sanchez AB, Medeiros MHG, Kowaltowski AJ (2015) Intermittent fasting results in tissue-specific changes in bioenergetics and redox state. PLoS One 10:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CNJ, Lin SY, Liao YH, Li ZJ, Wong AMK (2015) Late-onset caloric restriction alters skeletal muscle metabolism by modulating pyruvate metabolism. Am J Physiol - Endocrinol Metab 308:E942–E949. [DOI] [PubMed] [Google Scholar]
- Chen S, Li N, Deb-Chatterji M, Dong Q, Kielstein JT, Weissenborn K, Worthmann H (2012) Asymmetric Dimethyarginine as marker and mediator in Ischemic stroke. Int J Mol Sci 13:15983–16004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Zhu WG (2016) Biological function and regulation of histone and non-histone lysine methylation in response to DNA damage. Acta Biochim Biophys Sin (Shanghai) 48:603–616. [DOI] [PubMed] [Google Scholar]
- Cheng CW, Adams GB, Perin L, Wei M, Zhou X, Lam BS, Da Sacco S, Mirisola M, Quinn DI, Dorff TB, Kopchick JJ, Longo VD (2014) Prolonged fasting reduces IGF-1/PKA to promote hematopoietic-stem-cell- based regeneration and reverse immunosuppression. Cell Stem Cell 14:810–823 Available at: 10.1016/j.stem.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang JC, Jones PA (2007) Epigenetics and microRNAs. Pediatr Res 61:24–29. [DOI] [PubMed] [Google Scholar]
- Church MC, Fleming AB (2018) A role for histone acetylation in regulating transcription elongation. Transcription 9:225–232 Available at: https://www.tandfonline.com/doi/full/10.1080/21541264.2017.1394423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- M CM, C MF, M LA (1935) The effect of retarded growth upon the length of life span and upon the ultimate body size. 1935. Nutrition 5:155–171. [PubMed] [Google Scholar]
- Collier R (2013) Intermittent fasting: the science of going without. CMAJ 185:363–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colman RJ, Beasley TM, Allison DB, Weindruch R (2008) Attenuation of sarcopenia by dietary restriction in rhesus monkeys. Journals Gerontol - Ser A Biol Sci Med Sci 63:556–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colman RJ, Beasley TM, Kemnitz JW, Johnson SC, Weindruch R, Anderson RM (2014) Caloric restriction reduces age-related and all-cause mortality in rhesus monkeys. Nat Commun 5:3557 Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3988801&tool=pmcentrez&rendertype=abstract [Accessed July 12, 2014]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper DN, Mort M, Stenson PD, Ball EV, Chuzhanova NA (2010) Methylation-mediated deamination of 5-methylcytosine appears to give rise to mutations causing human inherited disease in CpNpG trinucleotides, as well as in CpG dinucleotides. Hum Genomics 4:406 Available at: http://humgenomics.biomedcentral.com/articles/10.1186/1479-7364-4-6-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM (2015) Lifespan and healthspan: Past, present, and promise. Gerontologist 55:901–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruzen C, Colman RJ (2009) Effects of Caloric Restriction on Cardiovascular Aging in Non-human Primates and Humans. Clin Geriatr Med 25:733–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels LR, Gladman JR, Altaf N, Moody AR (2007) Heterogeneity of Association Between MTHFR and Stroke Among European Regions: 50. [Google Scholar]
- De Castro RO, Previato L, Goitea V, Felberg A, Guiraldelli MF, Filiberti A, Pezza RJ (2017) The chromatin-remodeling subunit Baf200 promotes homology-directed DNA repair and regulates distinct chromatin-remodeling complexes. J Biol Chem 292:8459–8471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Groot S, Pijl H, Van Der Hoeven JJM, Kroep JR (2019) Effects of short-term fasting on cancer treatment. J Exp Clin Cancer Res 38:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Lucia C, Gambino G, Petraglia L, Elia A, Komici K, Femminella GD, D’Amico ML, Formisano R, Borghetti G, Liccardo D, Nolano M, Houser SR, Leosco D, Ferrara N, Koch WJ, Rengo G (2018) Long-term caloric restriction improves cardiac function, remodeling, adrenergic responsiveness, and sympathetic innervation in a model of postischemic heart failure. Circ Hear Fail 11:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Paula TG, Zanella BTT, De Almeida Fantinatti BE, De Moraes LN, Da Silva Duran BO, De Oliveira CB, Salomäo RAS, Da Silva RN, Padovani CR, Dos Santos VB, Mareco EA, Carvalho RF, Dal-Pai-Silva M (2017) Food restriction increase the expression of mTORC1 complex genes in the skeletal muscle of juvenile pacu (Piaractus mesopotamicus). PLoS One 12:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempster EL, Pidsley R, Schalkwyk LC, Owens S, Georgiades A, Kane F, Kalidindi S, Picchioni M, Kravariti E, Toulopoulou T, Murray RM, Mill J (2011) Disease-associated epigenetic changes in monozygotic twins discordant for schizophrenia and bipolar disorder. Hum Mol Genet 20:4786–4796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devlin MJ, Cloutier AM, Thomas NA, Panus DA, Lotinun S, Pinz I, Baron R, Rosen CJ, Bouxsein ML (2010) Caloric restriction leads to high marrow adiposity and low bone mass in growing mice. J Bone Miner Res 25:2078–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Q, Ash C, Mracek T, Merry B, Bing C (2012) Caloric restriction increases adiponectin expression by adipose tissue and prevents the inhibitory effect of insulin on circulating adiponectin in rats. J Nutr Biochem 23:867–874 Available at: 10.1016/j.jnutbio.2011.04.011. [DOI] [PubMed] [Google Scholar]
- Du Q, Luu PL, Stirzaker C, Clark SJ (2015) Methyl-CpG-binding domain proteins: Readers of the epigenome. Epigenomics 7:1051–1073. [DOI] [PubMed] [Google Scholar]
- Duan W, A. Ross C (2010) Potential Therapeutic Targets for Neurodegenerative Diseases: Lessons Learned from Calorie Restriction. Curr Drug Targets 11:1281–1292 Available at: http://www.eurekaselect.com/openurl/content.php?genre=article&issn=1389-4501&volume=11&issue=10&spage=1281. [DOI] [PubMed] [Google Scholar]
- Duszka K, Ellero-Simatos S, Ow GS, Defernez M, Paramalingam E, Tett A, Ying S, König J, Narbad A, Kuznetsov VA, Guillou H, Wahli W (2018) Complementary intestinal mucosa and microbiota responses to caloric restriction. Sci Rep 8:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabbiano S, Sua N, Veyrat-durebex C, Dokic AS, Colin DJ, Veyrat-durebex C, Dokic AS, Colin DJ, Trajkovski M (2016) Caloric Restriction Leads to Browning of White Adipose Tissue through Type 2 Immune Signaling Article Caloric Restriction Leads to Browning of White Adipose Tissue through Type 2 Immune Signaling. Cell Metab 24:434–446. [DOI] [PubMed] [Google Scholar]
- Faitg J, Leduc-Gaudet JP, Reynaud O, Ferland G, Gaudreau P, Gouspillou G (2019) Effects of aging and caloric restriction on fiber type composition, mitochondrial morphology and dynamics in rat oxidative and glycolytic muscles. Front Physiol 10:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fann DY-W, Ng GYQ, Poh L, Arumugam TV. (2017) Positive effects of intermittent fasting in ischemic stroke. Exp Gerontol 89:93–102 Available at: http://linkinghub.elsevier.com/retrieve/pii/S0531556516304284. [DOI] [PubMed] [Google Scholar]
- Fann DYW, Santro T, Manzanero S, Widiapradja A, Cheng YL, Lee SY, Chunduri P, Jo DG, Stranahan AM, Mattson MP, Arumugam TV. (2014) Intermittent fasting attenuates inflammasome activity in ischemic stroke. Exp Neurol 257:114–119 Available at: 10.1016/j.expneurol.2014.04.017. [DOI] [PubMed] [Google Scholar]
- Feng J, Zhou Y, Campbell SL, Le T, Li E, Sweatt JD, Silva AJ, Fan G (2010) Dnmt1 and Dnmt3a maintain DNA methylation and regulate synaptic function in adult forebrain neurons. Nat Neurosci 13:423–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontana L, Meyer TE, Klein S, Holloszy JO (2004) Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc Natl Acad Sci 101:6659–6663 Available at: http://www.pnas.org/cgi/doi/10.1073/pnas.0308291101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foretz M, Even PC, Viollet B (2018) AMPK activation reduces hepatic lipid content by increasing fat oxidation in vivo. Int J Mol Sci 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franceschi C, Garagnani P, Morsiani C, Conte M, Santoro A, Grignolio A, Monti D, Capri M, Salvioli S (2018) The continuum of aging and age-related diseases: Common mechanisms but different rates. Front Med 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuentes EN, Ruiz P, Valdes JA, Molina A (2012) Catabolic Signaling Pathways, Atrogenes, and Ubiquitinated Proteins Are Regulated by the Nutritional Status in the Muscle of the Fine Flounder. PLoS One 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabel K, Hoddy KK, Haggerty N, Song J, Kroeger CM, Trepanowski JF, Panda S, Varady KA (2018) Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: A pilot study. Nutr Heal Aging 4:345–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganesan K, Habboush Y, Sultan S (2018) Intermittent Fasting: The Choice for a Healthier Lifestyle. Cureus 10:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghisays F, Brace CS, Yackly SM, Kwon HJ, Mills KF, Kashentseva E, Dmitriev IP, Curiel DT, Imai S ichiro, Ellenberger T (2015) The N-Terminal Domain of SIRT1 Is a Positive Regulator of Endogenous SIRT1-Dependent Deacetylation and Transcriptional Outputs. Cell Rep 10:1665–1673 Available at: 10.1016/j.celrep.2015.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillum MP, Erion DM, Shulman GI (2011) Sirtuin-1 regulation of mammalian metabolism. Trends Mol Med 17:8–13 Available at: 10.1016/j.molmed.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong F, Miller KM (2013) Mammalian DNA repair: HATs and HDACs make their mark through histone acetylation. Mutat Res - Fundam Mol Mech Mutagen 750:23–30 Available at: 10.1016/j.mrfmmm.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Guarente L, Picard F (2005) Calorie restriction - The SIR2 connection. Cell 120:473–482. [DOI] [PubMed] [Google Scholar]
- Hagopian K, Ramsey JJ, Weindruch R (2003) Caloric restriction increases gluconeogenic and transaminase enzyme activities in mouse liver. Exp Gerontol 38:267–278. [DOI] [PubMed] [Google Scholar]
- Haigis MC, Guarente LP (2006) Mammalian sirtuins - Emerging roles in physiology, aging, and calorie restriction. Genes Dev 20:2913–2921. [DOI] [PubMed] [Google Scholar]
- Han X, Ren J (2010) Caloric restriction and heart function: Is there a sensible link? Acta Pharmacol Sin 31:1111–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handy D, Castro R, Loscalzo J (2011) Epigenetic Modifications Basic Mechanisms and Role in Cardiovascular Disease. Circulation 123:2145–2156 Available at: http://circ.ahajournals.org/content/123/19/2145.short. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey-Berino J (1999) Calorie restriction is more effective for obesity treatment than dietary fat restriction. Ann Behav Med 21:35–39. [DOI] [PubMed] [Google Scholar]
- Harvie M, Howell A (2017) Potential Benefits and Harms of Intermittent Energy Restriction and Intermittent Fasting Amongst Obese, Overweight and Normal Weight Subjects—A Narrative Review of Human and Animal Evidence. Behav Sci (Basel) 7:4 Available at: http://www.mdpi.com/2076-328X/7/1/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatori M, Vollmers C, Zarrinpar A, DiTacchio L, Bushong EA, Gill S, Leblanc M, Chaix A, Joens M, Fitzpatrick JAJ, Ellisman MH, Panda S (2012) Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab 15:848–860 Available at: 10.1016/j.cmet.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashida S, Arimoto A, Kuramoto Y, Kozako T, Honda SI, Shimeno H, Soeda S (2010) Fasting promotes the expression of SIRT1, an NAD+-dependent protein deacetylase, via activation of PPARα in mice. Mol Cell Biochem 339:285–292. [DOI] [PubMed] [Google Scholar]
- Heilbronn LK, Ravussin E (2003) Calorie restriction and aging: Review of the literature and implications for studies in humans. Am J Clin Nutr 78:361–369. [DOI] [PubMed] [Google Scholar]
- Hell NS, Costa De Oliveira LB, Sterman Dolnikoff M, Scivoletto R, Timo-Iaria C (1980) Changes of carbohydrate metabolism caused by food restriction, as detected by insulin administration. Physiol Behav 24:473–477. [DOI] [PubMed] [Google Scholar]
- Hempenstall S, Page MM, Wallen KR, Selman C (2012) Dietary restriction increases skeletal muscle mitochondrial respiration but not mitochondrial content in C57BL/6 mice. Mech Ageing Dev 133:37–45 Available at: 10.1016/j.mad.2011.12.002. [DOI] [PubMed] [Google Scholar]
- Hori YS, Kuno A, Hosoda R, Horio Y (2013) Regulation of FOXOs and p53 by SIRT1 modulators under oxidative stress. PLoS One 8:13–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne BD, Muhlestein JBAJ (2015) Health effects of intermittent fasting: Hormesis of harm? Am J Clin Nutr 102:464–470. [DOI] [PubMed] [Google Scholar]
- Huck-Hui N, Bird A (1999) DNA methylation and chromatin modification. Curr Opin Genet Dev 9:158–163. [DOI] [PubMed] [Google Scholar]
- Id KA, Id KAW, Katewa SD, Ortega M, Simons J, Id TAH, Kapuria S, Id AS, Id HJ, Id PK (2018) Dietary restriction improves intestinal cellular fitness to enhance gut barrier function and lifespan in D. melanogaster. PLoS Genet 14:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaul E, Barron J (2017) Age-Related Diseases and Clinical and Public Health Implications for the 85 Years Old and Over Population. Front Public Heal 5:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon SM (2016) Regulation and function of AMPK in physiology and diseases. Exp Mol Med 48:e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Y, Spurny M, Schübel R, Nonnenmacher T, Schlett CL, Stackelberg O Von, Ulrich CM, Kaaks R, Kauczor H, Kühn T, Nattenmüller J (2019) Changes in Pancreatic Fat Content Following Diet-Induced Weight Loss. Nutrients 11:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giudicessi, BA John R..Ackerman Michael J.. (2013) Determinants of incomplete penetrance and variable expressivity in heritable cardiac arrhythmia syndromes.161(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapahi P, Kaeberlein M, Hansen M (2017) Dietary restriction and lifespan: Lessons from invertebrate modelslic Access. Ageing Res Rev 39:3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz S, Calasanti T (2015) Critical perspectives on successful aging: Does it “appeal more than it illuminates”? Gerontologist 55:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehler DS (2019) Age-related disease burden as a measure of population ageing. Lancet Public Heal 4:e123–e124 Available at: 10.1016/S2468-2667(19)30026-X. [DOI] [PubMed] [Google Scholar]
- Khan SA, Sathyanarayan A, Mashek MT, Ong KT, Wollaston-Hayden EE, Mashek DG (2015) ATGL-catalyzed lipolysis regulates SIRT1 to control PGC-1α/PPAR-α signaling. Diabetes 64:418–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoshnam SE, Winlow W, Farzaneh M (2017) The interplay of MicroRNAs in the inflammatory mechanisms following ischemic stroke. J Neuropathol Exp Neurol 76:548–561. [DOI] [PubMed] [Google Scholar]
- Kim J et al. (2018) Transcriptome analysis reveals intermittent fasting-induced genetic changes in ischemic stroke. Hum Mol Genet 27:1497–1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K chol, Friso S, Choi SW (2009) DNA methylation, an epigenetic mechanism connecting folate to healthy embryonic development and aging. J Nutr Biochem 20:917–926 Available at: 10.1016/j.jnutbio.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk E, Reeds DN, Finck BN, Mayurranjan MS, Klein S (2010) Sensitivity During Caloric Restriction. Gastroenterology 136:1552–1560 Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2677125/pdf/nihms92461.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk KL (2001) Dietary restriction and aging: Comparative tests of evolutionary hypotheses. Journals Gerontol - Ser A Biol Sci Med Sci 56:123–129. [DOI] [PubMed] [Google Scholar]
- Koubova J, Guarente L (2003) How does calorie restriction work? Genes Dev 17:313–321. [DOI] [PubMed] [Google Scholar]
- Kouda K, Iki M (2010) Beneficial effects of mild stress (Hormetic Effects): Dietary restriction and health. J Physiol Anthropol 29:127–132. [DOI] [PubMed] [Google Scholar]
- Kulkarni SR, Donepudi AC, Xu J, Wei W, Cheng QC, Driscoll MV., Johnson DA, Johnson JA, Li X, Slitt AL (2014) Fasting induces nuclear factor E2-related factor 2 and ATP-binding cassette transporters via protein kinase a and sirtuin-1 in mouse and human. Antioxidants Redox Signal 20:15–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kynjai I, Hadem H, Majaw T, Kharbuli B, Sharma R (2019) Beneficial effects of dietary restriction in aging brain. J Chem Neuroanat 95:123–133 Available at: 10.1016/j.jchemneu.2017.10.001. [DOI] [PubMed] [Google Scholar]
- Laboratory NOand AA and ESR (2012) NOAA/ESRL radiosonde database. Http://WwwEsrlNoaaGov/Raobs/ 15:675–690 Available at: papers3://publication/uuid/1D401301-44F6-4BEE-BB3F-CE3E58AF0F91. [Google Scholar]
- Lan JF, Zhang X, Chen D (2015) Molecular mechanisms of dietary restriction in aging—insights from Caenorhabditis elegans research. Sci China Life Sci 58:352–358. [DOI] [PubMed] [Google Scholar]
- Lang FR, Rupprecht FS (2019) Motivation for Longevity Across the Life Span: An Emerging Issue. Innov Aging 3:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanktree MB, Hegele RA (2017) Metabolic Syndrome. Genomic Precis Med Prim Care Third Ed 365:283–299. [Google Scholar]
- Laplante M, Sabatini DM (2013) Regulation of mTORC1 and its impact on gene expression at a glance. J Cell Sci 126:1713–1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson-meyer DE, Heilbronn LK, Redman LM, Newcomer BR, Frisard MI, Anton S, Smith SR, Maplstat AA, Ravussin E, Team PC (2009) NIH Public Access. 29:1337–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C, Longo V (2016) Dietary restriction with and without caloric restriction for healthy aging. F1000Research 5:1–7 Available at: http://f1000research.com/articles/5-117/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legube G, Trouche D (2003) Regulating histone acetyltransferases and deacetylases. EMBO Rep 4:944–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennartsson A, Ekwall K (2009) Histone modification patterns and epigenetic codes. Biochim Biophys Acta - Gen Subj 1790:863–868. [DOI] [PubMed] [Google Scholar]
- Lian T, Wu Q, Hodge BA, Wilson KA, Yu G, Yang M (2018) Drosophila Gut — A Nexus Between Dietary Restriction and Lifespan. Int J Mol Sci 19:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B, K.H Yip R, Zhou Z(2012) Chromatin Remodeling, DNA Damage Repair and Aging. Curr Genomics 13:533–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longo VD, Fontana Luigi (2010) Calorie restriction and cancer prevention: metabolic and molecular mechanisms. Trends Pharmacol Sci 31:89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longo VD, Mattson MP (2014) Review Fasting: Molecular Mechanisms and Clinical Applications. Cell Metab 19:181–192 Available at: 10.1016/j.cmet.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchsinger JA, Tang MX, Shea S, Mayeux R (2002) Caloric intake and the risk of Alzheimer disease. Arch Neurol 59:1258–1263. [DOI] [PubMed] [Google Scholar]
- Manuscript A (2013) Stress in the Diabetic Milieu: Mechanistic Insights. J Nutr Biochem 23:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manzanero S, Gelderblom M, Magnus T, Arumugam TV. (2011) Calorie restriction and stroke. Exp Transl Stroke Med 3:8 Available at: http://www.etsmjournal.com/content/3/1/8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcinko K, Steinberg GR (2014) The role of AMPK in controlling metabolism and mitochondrial biogenesis during exercise. Exp Physiol 99:1581–1585. [DOI] [PubMed] [Google Scholar]
- Martin B, Ji S, Maudsley S, Mattson MP (2010) “Control” laboratory rodents are metabolically morbid: Why it matters. Proc Natl Acad Sci 107:6127–6133 Available at: http://www.pnas.org/cgi/doi/10.1073/pnas.0912955107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins VF, Tahvilian S, Kang JH, Svensson K, Hetrick B, Chick WS, Schenk S, McCurdy CE (2018) Calorie restriction-induced increase in skeletal muscle insulin sensitivity is not prevented by overexpression of the p55α subunit of phosphoinositide 3-kinase. Front Physiol 9:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzetti E, Lees HA, Wohlgemuth SE, Leeuwenburgh C (2009) Sarcopenia of aging: Underlying cellular mechanisms and protection by calorie restriction. BioFactors 35:28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masoro EJ (1998) Hormesis and the antiaging action of dietary restriction. Exp Gerontol 33:61–66. [DOI] [PubMed] [Google Scholar]
- Masoro EJ (2006) Caloric restriction and aging: Controversial issues. Journals Gerontol - Ser A Biol Sci Med Sci 61:14–19. [DOI] [PubMed] [Google Scholar]
- Mattson MP, Allison DB, Fontana L, Harvie M, Longo VD, Malaisse WJ, Mosley M, Notterpek L, Ravussin E, Scheer FAJL, Seyfried TN, Varady KA, Panda S (2014) Meal frequency and timing in health and disease. Proc Natl Acad Sci 111:16647–16653 Available at: http://www.pnas.org/lookup/doi/10.1073/pnas.1413965111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson MP, Longo VD, Harvie M (2017) Impact of intermittent fasting on health and disease processes. Ageing Res Rev 39:46–58 Available at: 10.1016/j.arr.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson MP, Longo VD, Harvie M, States U, States U, Angeles L, States U, Cancer B, Centre P, Kingdom U (2018) HHS Public Access:46–58. [Google Scholar]
- Mattson MP, Wan R (2005) Beneficial effects of intermittent fasting and caloric restriction on the cardiovascular and cerebrovascular systems. J Nutr Biochem 16:129–137. [DOI] [PubMed] [Google Scholar]
- Millward DJ, Nnanyelugo DO, James WPT, Garlick PJ (1974) Protein metabolism in skeletal muscle: the effect of feeding and fasting on muscle RNA, free amino acids and plasma insulin concentrations. Br J Nutr 32:127–142. [DOI] [PubMed] [Google Scholar]
- Miloucheva I (2002) Traffic_Ngni.Pdf. Nat Rev Genet 13:343–357. [Google Scholar]
- Minor RK, Allard JS, Younts CM, Ward TM, De Cabo R (2010) Dietary interventions to extend life span and health span based on calorie restriction. Journals Gerontol - Ser A Biol Sci Med Sci 65 A:695–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SE, Delville C, Konstantopedos P, Derous D, Green CL, Chen L, Han JDJ, Wang Y, Promislow DEL, Douglas A, Lusseau D, Speakman JR (2015) The effects of graded levels of calorie restriction: III. Impact of short term calorie and protein restriction on mean daily body temperature and torpor use in the C57BL/6 mouse. Oncotarget 6:18314–18337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SJ, Bernier M, Mattison JA, Aon MA, Kaiser TA, Anson RM, Ikeno Y, Anderson RM, Ingram DK, de Cabo R (2019) Daily Fasting Improves Health and Survival in Male Mice Independent of Diet Composition and Calories. Cell Metab 29:221–228.e3 Available at: 10.1016/j.cmet.2018.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore LD, Le T, Fan G (2013) DNA methylation and its basic function. Neuropsychopharmacology 38:23–38 Available at: 10.1038/npp.2012.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morikawa Y, Ueyama E, Senba E (2004) Fasting-induced activation of mitogen-activated protein kinases (ERK/p38) in the mouse hypothalamus. J Neuroendocrinol 16:105–112. [DOI] [PubMed] [Google Scholar]
- Motoshima H, Goldstein BJ, Igata M, Araki E (2006) AMPK and cell proliferation - AMPK as a therapeutic target for atherosclerosis and cancer. J Physiol 574:63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moutinho C, Esteller M (2017) MicroRNAs and Epigenetics, 1st ed. Elsevier Inc. Available at: 10.1016/bs.acr.2017.06.003. [DOI] [PubMed] [Google Scholar]
- Narlikar GJ, Sundaramoorthy R, Owen-Hughes T (2013) Mechanisms and functions of ATP-dependent chromatin-remodeling enzymes. Cell 154:490–503 Available at: 10.1016/j.cell.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng GY-Q, L Yun-An, Sobey Christopher G D T, Fann David Yang-Wei A TV (2018) Epigenetic Regulation of Inflammation in Stroke. Ther Adv Neurol Disord 11:1–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niccoli T, Partridge L (2012) Ageing as a risk factor for disease. Curr Biol 22:R741–R752 Available at: 10.1016/j.cub.2012.07.024. [DOI] [PubMed] [Google Scholar]
- Nicoll R, Henein MY (2018) Caloric restriction and its effect on blood pressure, heart rate variability and arterial stiffness and dilatation: A review of the evidence. Int J Mol Sci 19:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Flanagan CH, Smith LA, McDonell SB, Hursting SD (2017) When less may be more: Calorie restriction and response to cancer therapy. BMC Med 15:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivo-Marston SE, Hursting SD, Perkins SN, Schetter A, Khan M, Croce C, Harris CC, Lavigne J (2014) Effects of calorie restriction and diet-induced obesity on murine colon carcinogenesis, growth and inflammatory factors, and MicroRNA expression. PLoS One 9:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott B, Skurk T, Hastreiter L, Lagkouvardos I, Fischer S, Büttner J, Kellerer T, Clavel T, Rychlik M, Haller D (2017) Effect of caloric restriction on gut permeability, inflammation markers, and fecal microbiota in obese women. Sci Rep 7:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panawala L, Between D, View E, View B, Panawala L (2017) Difference Between Euchromatin and Heterochromatin Difference Between Euchromatin and Heterochromatin Main Difference – Euchromatin vs Heterochromatin Live There with Airbnb. [Google Scholar]
- Parsons J (2001) The GP’s own healthcare. Can we learn to be patients? Aust Fam Physician 30:631. [PubMed] [Google Scholar]
- Patterson RE, Laughlin GA, LaCroix AZ, Hartman SJ, Natarajan L, Senger CM, Martínez ME, Villaseñor A, Sears DD, Marinac CR, Gallo LC (2015a) Intermittent Fasting and Human Metabolic Health. J Acad Nutr Diet 115:1203–1212 Available at: 10.1016/j.jand.2015.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson RE, Laughlin GA, Sears DD, LaCroix AZ, Marinac C, Gallo LC, Hartman SJ, Natarajan L, Senger CM, Martínez ME, Villaseñor A (2015b) INTERMITTENT FASTING AND HUMAN METABOLIC HEALTH Ruth. J Acad Nutr Diet 150:137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen SB, Ølholm J, Paulsen SK, Bennetzen MF, Richelsen B (2008) Low Sirt1 expression, which is upregulated by fasting, in human adipose tissue from obese women. Int J Obes 32:1250–1255. [DOI] [PubMed] [Google Scholar]
- Picard F, Kurtev M, Chung N, Topark-ngarm A, Oliveira RM De, Leid M, Mcburney MW (2012) 2. Gho. 429:1–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pifferi F, Terrien J, Marchal J, Dal-Pan A, Djelti F, Hardy I, Chahory S, Cordonnier N, Desquilbet L, Hurion M, Zahariev A, Chery I, Zizzari P, Perret M, Epelbaum J, Blanc S, Picq J-L, Dhenain M, Aujard F (2018) Caloric restriction increases lifespan but affects brain integrity in grey mouse lemur primates. Commun Biol 1:1–8 Available at: 10.1038/s42003-018-0024-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillus EP and L (2015) Balancing chromatin remodeling and histone modifications in transcription. Trends Genet 29:621–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portela A, Esteller M (2010a) Epigenetic modifications and human disease. Nat Biotechnol 28:1057–1068 Available at: 10.1038/nbt.1685. [DOI] [PubMed] [Google Scholar]
- Portela A, Esteller M (2010b) Epigenetic modifications and human disease. Nat Biotechnol 28:1057–1068. [DOI] [PubMed] [Google Scholar]
- Poulsen P, Esteller M, Vaag A, Fraga MF (2007) The epigenetic basis of twin discordance in age-related diseases. Pediatr Res 61:38–42. [DOI] [PubMed] [Google Scholar]
- Prehn K, Jumpertz von Schwartzenberg R, Mai K, Zeitz U, Witte AV, Hampel D, Szela AM, Fabian S, Grittner U, Spranger J, Flöel A (2017) Caloric Restriction in Older Adults-Differential Effects of Weight Loss and Reduced Weight on Brain Structure and Function. Cereb Cortex 27:1765–1778. [DOI] [PubMed] [Google Scholar]
- Preihs Christian Arambula J, Magda D, Jeong H, Yoo D, Cheon J, Siddik Z, Sessler J (2013) Recent Developments in Texaphyrin Chemistry and Drug Discovery. Inorg Chem 52:12184–12192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purushotham A, Schug TT, Xu Q, Surapureddi S, Guo X, Li X (2009) Hepatocyte-Specific Deletion of SIRT1 Alters Fatty Acid Metabolism and Results in Hepatic Steatosis and Inflammation. Cell Metab 9:327–338 Available at: 10.1016/j.cmet.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin W, Yang T, Ho L, Zhao Z, Wang J, Chen L, Zhao W, Thiyagarajan M, MacGrogan D, Rodgers JT, Puigserver P, Sadoshima J, Deng H, Pedrini S, Gandy S, Sauve AA, Pasinetti GM (2006) Neuronal SIRT1 activation as a novel mechanism underlying the prevention of alzheimer disease amyloid neuropathology by calorie restriction. J Biol Chem 281:21745–21754. [DOI] [PubMed] [Google Scholar]
- Qiu G, Liu S, So K (2010a) Dietary restriction and brain health. Neurosci Bull 26:55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu X, Brown K, Hirschey MD, Verdin E, Chen D (2010b) Calorie restriction reduces oxidative stress by SIRT3-mediated SOD2 activation. Cell Metab 12:662–667 Available at: 10.1016/j.cmet.2010.11.015. [DOI] [PubMed] [Google Scholar]
- Qureshi IA, Mehler MF (2010) Emerging role of epigenetics in stroke: part 1: DNA methylation and chromatin modifications. Arch Neurol 67:1316–1322 Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3685873&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qureshi IMM (2011) The Emerging Role of Epigenetics in Stroke. Neurol Rev 68:294–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radakovich LB, Marolf AJ, Culver LA, Santangelo KS (2019) Calorie restriction with regular chow, but not a high-fat diet, delays onset of spontaneous osteoarthritis in the Hartley guinea pig model. Arthritis Res Ther 21:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rangan P, Choi I, Wei M, Navarrete G, Guen E, Brandhorst S, Enyati N, Pasia G, Maesincee D, Ocon V, Abdulridha M, Longo VD (2019) Fasting-Mimicking Diet Modulates Microbiota and Promotes Intestinal Regeneration to Reduce Inflammatory Bowel Disease Pathology. Cell Rep 26:2704–2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redman LM, Veldhuis JD, Rood J, Smith SR, Williamson D, Ravussin E (2010) The effect of caloric restriction interventions on growth hormone secretion in nonobese men and women. Aging Cell 9:32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ri et al. (2012) NIH Public Access. Tepeapulco, región en Perspect 100:9–10 Available at: 10.1016/j.jand.2015.02.018\nhttp://www.raco.cat/index.php/HojasWarmi/article/view/208552\nhttp://www.raco.cat/index.php/HojasWarmi/article/download/208552/277739\nhttp://www.raco.cat/index.php/HojasWarmi/article/viewArticle/208552/. [DOI] [Google Scholar]
- Riaz N, Wolden SL, Gelblum DY, Eric J (2016) HHS Public Access. 118:6072–6078. [Google Scholar]
- Robertson LT, Mitchell JR (2013) Benefits of short-term dietary restriction in mammals. Exp Gerontol 48:1043–1048 Available at: 10.1016/j.exger.2013.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogina B, Helfand SL (2004) Sir2 mediates longevity in the fly through a pathway related to calorie restriction. Proc Natl Acad Sci 101:15998–16003 Available at: http://www.pnas.org/cgi/doi/10.1073/pnas.0404184101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogozina OP, Bonorden MJL, Seppanen CN, Grande JP, Cleary MP (2012) Effect of Chronic and Intermittent Calorie Restriction on Serum Adiponectin and Leptin and Mammary Tumorigenesis. Cancer Prev Res 4:568–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabatini DM (2017) Twenty-five years of mTOR: Uncovering the link from nutrients to growth. Proc Natl Acad Sci U S A 114:11818–11825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saldanha SN, Watanabe LP (2015) Epigenetics and Aging. Epigenetics and Dermatology 4:379–406. [Google Scholar]
- Saxton RA, Sabatini DM (2017) mTOR Signaling in Growth, Metabolism, and Disease. Cell 168:960–976 Available at: 10.1016/j.cell.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinmura K (2013) Effects of caloric restriction on cardiac oxidative stress and mitochondrial bioenergetics: Potential role of cardiac sirtuins. Oxid Med Cell Longev 2013:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sierra H, Cordova M, Chen CSJ, Rajadhyaksha M (2015) Confocal imaging-guided laser ablation of basal cell carcinomas: An ex vivo study. J Invest Dermatol 135:612–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skerrett PJ, Willett WC (2010) Essentials of healthy eating: A guide. J Midwifery Women’s Heal 55:492–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Square T (2002) This Week in the BMJ. Bmj 324:1185. [Google Scholar]
- Srivastava S, C. Haigis M (2011) Role of Sirtuins and Calorie Restriction in Neuroprotection: Implications in Alzheimers and Parkinsons Diseases. Curr Pharm Des 17:3418–3433. [DOI] [PubMed] [Google Scholar]
- Stadler J, Richly H (2017) Regulation of DNA repair mechanisms: How the chromatin environment regulates the DNA damage response. Int J Mol Sci 18:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein PK, Soare A, Meyer TE, Cangemi R, Holloszy JO, Fontana L (2012) Caloric restriction may reverse age-related autonomic decline in humans. Aging Cell 11:644–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stekovic S et al. (2019) Alternate Day Fasting Improves Physiological and Molecular Markers of Aging in Healthy, Non-obese Humans. Cell Metab 30:462–476. [DOI] [PubMed] [Google Scholar]
- Straus DS, Takemoto CD (1990) Effect of Fasting on Insulin-Like Growth Factor-I (IGF-I) and Growth Hormone Receptor mRNA Levels and IGF-I Gene Transcription in Rat Liver. Mol Endocrinol 4:91–100. [DOI] [PubMed] [Google Scholar]
- Tamaru H (2010) Confining euchromatin/heterochromatin territory: Jumonji crosses the line. Genes Dev 24:1465–1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamburini B a, Tyler JK (2005) Localized Histone Acetylation and Deacetylation Triggered by the Homologous Recombination Pathway of Double-Strand DNA Repair Localized Histone Acetylation and Deacetylation Triggered by the Homologous Recombination Pathway of Double-Strand DNA Repair. 25:4903–4913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan Q, Christiansen L, Von Bornemann Hjelmborg J, Christensen K (2015) Twin methodology in epigenetic studies. J Exp Biol 218:134–139. [DOI] [PubMed] [Google Scholar]
- Taylor R (2019) Calorie restriction for long-term remission of type 2 diabetes. Clin Med J R Coll Physicians London 19:37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tesch-Römer C, Wahl HW (2017) Toward a more comprehensive concept of successful aging: Disability and care needs. Journals Gerontol - Ser B Psychol Sci Soc Sci 72:310–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson DM, Winder WW (2009) AMPK Control of Fat Metabolism in Skeletal Muscle. Acta Physiol (Oxf) 196:147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trayhurn P, Thomas MEA, Duncan JS, Vernon Rayner D (1995) Effects of fasting and refeeding on ob gene expression in white adipose tissue of lean and obese (ob/ob) mice. FEBS Lett 368:488–490. [DOI] [PubMed] [Google Scholar]
- Trepanowski JF, Bloomer RJ (2010) The impact of religious fasting on human health. Nutr J 9:57 Available at: http://www.nutritionj.com/content/9/1/57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tulsian R, Velingkaar N, Kondratov R (2018) Caloric restriction effects on liver mTOR signaling are time-of-day dependent. Aging (Albany NY) 10:1640–1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyagi M, Imam N, Verma K, Patel AK (2016) Chromatin remodelers: We are the drivers!! Nucleus 7:388–404 Available at: 10.1080/19491034.2016.1211217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uauy R, Díaz E (2005) Consequences of food energy excess and positive energy balance. Public Health Nutr 8:1077–1099 Available at: http://www.journals.cambridge.org/abstract_S1368980005001357. [DOI] [PubMed] [Google Scholar]
- Udali S, Guarini P, Moruzzi S, Choi SW, Friso S (2013) Cardiovascular epigenetics: From DNA methylation to microRNAs. Mol Aspects Med 34:883–901 Available at: 10.1016/j.mam.2012.08.001. [DOI] [PubMed] [Google Scholar]
- Ungvari Z, Parrado-Fernandez C, Csiszar A, De Cabo R (2008) Mechanisms underlying caloric restriction and lifespan regulation: Implications for vascular aging. Circ Res 102:519–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usuki F, Yasutake A, Umehara F, Higuchi I (2004) Beneficial effects of mild lifelong dietary restriction on skeletal muscle: Prevention of age-related mitochondrial damage, morphological changes, and vulnerability to a chemical toxin. Acta Neuropathol 108:1–9. [DOI] [PubMed] [Google Scholar]
- Vignali M, Hassan AH, Neely KE, Workman JL (2000) ATP-dependent chromatin-remodeling complexes. Mol Cell Biol 20:1899–1910 Available at: http://www.ncbi.nlm.nih.gov/pubmed/10688638%0Ahttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC110808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Liang Y, Vanhoutte PM (2011) SIRT1 and AMPK in regulating mammalian senescence: A critical review and a working model. FEBS Lett 585:986–994 Available at: 10.1016/j.febslet.2010.11.047. [DOI] [PubMed] [Google Scholar]
- Wayhart JP, Lawson HA (2017) Animal Models of Metabolic Syndrome. Anim Model Study Hum Dis Second Ed:221–243 Available at: 10.1186/s12986-016-0123-9. [DOI] [Google Scholar]
- Webster PD, Singh M, Tucker PC, Black O (1972) Effects of Fasting and Feeding on the Pancreas. Gastroenterology 62:600–605 Available at: 10.1016/S0016-5085(72)80044-1. [DOI] [PubMed] [Google Scholar]
- Wegman MP, Guo MH, Bennion DM, Shankar MN, Chrzanowski SM, Goldberg LA, Xu J, Williams TA, Lu X, Hsu SI, Anton SD, Leeuwenburgh C, Brantly ML (2015) Practicality of Intermittent Fasting in Humans and its Effect on Oxidative Stress and Genes Related to Aging and Metabolism. Rejuvenation Res 18:162–172 Available at: http://online.liebertpub.com/doi/10.1089/rej.2014.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei M, Brandhorst S, Shelehchi M, Mirzaei H, Cheng CW, Budniak J, Groshen S, Mack WJ, Guen E, Di Biase S, Cohen P, Morgan TE, Dorff T, Hong K, Michalsen A, Laviano A, Longo VD (2017) Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease. Sci Transl Med 9:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei S, Han R, Zhao J, Wang S, Huang M, Wang Y, Chen Y (2018) Intermittent administration of a fasting-mimicking diet intervenes in diabetes progression, restores β cells and reconstructs gut microbiota in mice. Nutr Metab 15:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weindruch RH, Cheung MK, Anthony Verity M, Walford RL (1980) Modification of mitochondrial respiration by aging and dietary restriction. Mech Ageing Dev 12:375–392. [DOI] [PubMed] [Google Scholar]
- Weiss EP, Fontana L (2011) Caloric restriction: Powerful protection for the aging heart and vasculature. Am J Physiol - Hear Circ Physiol 301:H1205–H1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijngaarden MA, van der Zon GC, van Dijk KW, Pijl H, Guigas B (2013) Effects of prolonged fasting on AMPK signaling, gene expression, and mitochondrial respiratory chain content in skeletal muscle from lean and obese individuals. AJP Endocrinol Metab 304:E1012–E1021 Available at: http://ajpendo.physiology.org/cgi/doi/10.1152/ajpendo.00008.2013. [DOI] [PubMed] [Google Scholar]
- Wu H, Zhang Y (2014) Reversing DNA methylation: Mechanisms, genomics, and biological functions. Cell 156:45–68 Available at: 10.1016/j.cell.2013.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu GL, Wong J (2015) Oxidative DNA demethylation mediated by Tet enzymes. Natl Sci Rev 2:318–328. [Google Scholar]
- Yao Q, Chen Y, Zhou X (2019) The roles of microRNAs in epigenetic regulation. Curr Opin Chem Biol 51:11–17 Available at: 10.1016/j.cbpa.2019.01.024. [DOI] [PubMed] [Google Scholar]
- Yousefi M, Nakauka-Ddamba A, Berry CT, Li N, Schoenberger J, Simeonov KP, Cedeno RJ, Yu Z, Lengner CJ (2018) Calorie Restriction Governs Intestinal Epithelial Regeneration through Cell-Autonomous Regulation of mTORC1 in Reserve Stem Cells. Stem Cell Reports 10:703–711 Available at: 10.1016/j.stemcr.2018.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang P, Torres K, Liu X, Liu C, E. Pollock R (2016) An Overview of Chromatin-Regulating Proteins in Cells. Curr Protein Pept Sci 17:401–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang P, Tu B, Wang H, Cao Z, Tang M, Zhang C, Gu B, Li Z, Wang L, Yang Y, Zhao Y, Wang H, Luo J, Deng CX, Gao B, Roeder RG, Zhu WG (2014) Tumor suppressor p53 cooperates with SIRT6 to regulate gluconeogenesis by promoting FoxO1 nuclear exclusion. Proc Natl Acad Sci U S A 111:10684–10689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Reinberg D (2001) Transcription regulation by histone methylation: Interplay between different covalent modifications of the core histone tails. Genes Dev 15:2343–2360. [DOI] [PubMed] [Google Scholar]
- Zhao Y, Lu J, Sun H, Chen X, Huang W, Tao D, Huang B (2005) Histone acetylation regulates both transcription initiation and elongation of hsp22 gene in Drosophila. Biochem Biophys Res Commun 326:811–816. [DOI] [PubMed] [Google Scholar]
- Zheng XY, Han YL, Guo C, Zhang L, Qiu Y, Chen G (2014) Progress in research of nutrition and life expectancy. Biomed Environ Sci 27:155–161 Available at: 10.3967/bes2014.036. [DOI] [PubMed] [Google Scholar]
- Zhou BS, Bu GY, Li M, Chang BG, Zhou YP (2014) Tagging SNPs in the MTHFR gene and risk of ischemic stroke in a Chinese population. Int J Mol Sci 15:8931–8940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, Yan Y, Gius DR, Vassilopoulos A (2013) Metabolic regulation of sirtuins upon fasting and the implication for cancer. Curr Opin Oncol 25:630–636. [DOI] [PMC free article] [PubMed] [Google Scholar]