Abstract
Climate variability and change are issues of growing public health importance. Numerous studies have documented risks of extreme heat on human health in different locations around the world. Strategies to prevent heat‐related morbidity and reduce disparities are possible but require improved knowledge of health outcomes during hot days at a small‐scale level as important within‐city variability in local weather conditions, socio‐demographic composition, and access to air conditioning (AC) may exist. We analyzed hospitalization data for three unique climate regions of San Diego County alongside temperature data spanning 14 years to quantify the health impact of ambient air temperature at varying exceedance threshold levels. Within San Diego, coastal residents were more sensitive to heat than inland residents. At the coast, we detected a health impact at lower temperatures compared to inland locations for multiple disease categories including heat illness, dehydration, acute renal failure, and respiratory disease. Within the milder coastal region where access to AC is not prevalent, heat‐related morbidity was higher in the subset of zip codes where AC saturation is lowest. We detected a 14.6% increase (95% confidence interval [4.5%, 24.6%]) in hospitalizations during hot weather in comparison to colder days in coastal locations where AC is less common, while no significant impact was observed in areas with higher AC saturation. Disparities in AC ownership were associated with income, race/ethnicity, and homeownership. Given that heat waves are expected to increase with climate change, understanding health impacts of heat and the role of acclimation is critical for improving outcomes in the future.
Keywords: temperature, heat extremes, health outcomes, disparities, air conditioning, climate zones
Key Points
Analysis of hospitalization data for three climate zones in San Diego County shows disparities in health outcomes during hot weather
Coastal residents are more sensitive to heat than inland residents with significant impacts found for multiple disease categories
Heat sensitivity is reduced through air conditioning access, which is not prevalent at the coast due to generally mild weather
1. Background and Introduction
Heat‐related illnesses are largely preventable, yet extreme heat is the top weather‐related killer in the United States (National Weather Service [NWS], 2017). In California the July 2006 heat wave, which was of an unprecedented magnitude and humidity (Gershunov et al., 2009), was responsible for over 600 excess deaths (Ostro et al., 2009), over 1,200 hospitalizations for cardiovascular and other diseases (Guirguis et al., 2014), and over 16,000 emergency department visits (Knowlton et al., 2009). The strongest health impacts from this and other recent heat waves were manifested at the coast (Gershunov et al., 2011; Guirguis et al., 2014; Knowlton et al., 2009), where residents are used to relatively mild temperatures, are not well acclimated to heat, and may not have air conditioning (AC) in their homes. The associations between hospital and emergency room visits increase with higher temperatures in California during the warm season, with greatest risks found for cardiovascular and renal diseases, some respiratory diseases, diabetes, dehydration, and heat‐related illnesses (Basu et al., 2012). Observed trends and analyses of climate‐model projections have suggested that heat waves in the Southwest United States are becoming more frequent with greater duration and intensity (Gershunov et al., 2009), particularly in coastal areas (Gershunov & Guirguis, 2012). Yet, to our knowledge, no studies have assessed such coastal vulnerability to heat related health impacts within a city.
We know that extreme heat affects public health worldwide, but there is limited understanding regarding how regional impacts vary with acclimatization to the surrounding environment. San Diego County represents a demographically diverse population and spans dramatically different climate zones, where some residents live in desert conditions just inland of coastal populations. Those living near the coast are acclimated to a generally temperate Mediterranean climate, while residents of inland valleys and deserts are more acclimated to heat. Because of the relatively mild average climate, many coastal homes and public facilities (including schools) in San Diego do not have air conditioners, making it less feasible for individuals to cool during prolonged periods of extreme heat. For example, during a recent heat wave in August 2017, students at more than 70 schools in San Diego County were released early because facilities had little or no AC (San Diego Union Tribune, 2017). In homes, the estimated saturation rate for central or room AC for residents within the service area of San Diego Gas and Electric (a local utility company) is 43% and 13%, respectively, as of 2009 (California Energy Commission (2010)). Furthermore, some people cannot afford to use air conditioners, particularly those with lower socioeconomic status, who have other additional risk factors to place them at increased risk. Previous studies focusing on the 2006 California heat wave (Gershunov et al., 2011; Knowlton et al., 2009; Ostro et al., 2009) and several recent heat waves (Guirguis et al., 2014) have shown that although temperatures were hotter inland, the health impacts were stronger along the coast.
Studies have shown that location‐specific assessments are important given that each locality has a specific temperature/health dose response (Curriero et al., 2002; Gasparrini et al., 2015). Other studies of large metropolitan cities have shown important spatial variation in health outcomes during extreme heat at the subcity level (Benmarhnia et al., 2017; Hondula & Barnett, 2014; Vaneckova et al., 2010). While it is typical within a city to use a common temperature threshold for policy purposes, it is likely that within a city, different temperature thresholds are needed to better protect public health during heat episodes (Benmarhnia et al., 2016; Price et al., 2013). In San Diego, heat alerts issued by the NWS are used by local agencies to implement protective measures such as Cool Zones (public/private facilities that voluntarily provide air conditioned spaces for the public to escape the heat) and enhanced staffing for emergency response. Therefore, identifying appropriate temperature thresholds is critical. There is no universal definition of a heat wave (Anderson & Bell, 2011; Chen et al., 2015; Tong et al., 2010). In California, heat‐alert criteria have historically relied on the heat index, which is based on empirical relationships between temperature/humidity thresholds and mortality in a few major U.S. cities. This metric fails to account for local climatology, which is an important limitation. The standard heat index value of 105 used to trigger an alert nationally does not work well in California due to local acclimation and drier climates. Additionally, the associations with health are largely based on mortality, which is a small subset of overall heat risk, and fails to account for increased risk in vulnerable populations such as the elderly or those with preexisting conditions. Recently, the NWS Western Region has developed an improved warning system that accounts for local variation in climatology to issue tiered heat alerts using different temperature thresholds for different locations and for different levels of vulnerability (NWS, https://www.wrh.noaa.gov/wrh/heatrisk/?wfo=sgx). This Heat Risk product aims to identify heat episodes that vary geographically and seasonally in an effort to minimize heat‐related impacts through planning and notification.
In this study, we used patient discharge (PD) data from the California Office of Statewide Health Planning and Development for acute care facilities to determine the impact of high ambient temperatures on hospital admissions in three distinct climate regions of San Diego County and for multiple disease categories that are known to be associated with complications from hot weather (Basu et al., 2012; Bobb et al., 2014). Additionally, we assessed whether access to AC modifies the association between extreme temperatures and morbidity in the coastal zone, and we provided an assessment of disparities in access to AC. Other work has shown that AC use significantly reduces the effect of temperature on health outcomes in California (Medina‐Ramón & Schwartz, 2007; Ostro et al., 2010). This study also focuses on AC use at the subregional level and uses socioeconomic information to address disparities on AC ownership. We hypothesized that during heat waves, hospital admissions in San Diego County would be more concentrated among residents in coastal areas than in inland areas and that such heterogeneity can be explained by differences in climatological acclimation and disparities in AC ownership. Additionally, based on existing epidemiological evidence (Benmarhnia et al., 2015; Gronlund, 2014), we expected that residents would not be affected equally and we assessed if disparities in heat‐related morbidity exist according to age and race/ethnicity. High‐risk groups include the elderly and young children, who may not be able to thermoregulate efficiently; low‐income populations who cannot afford AC; and those with preexisting medical conditions, such as cardiovascular and renal diseases, that render them vulnerable to dehydration (e.g., Basu, 2009; Basu & Malig, 2011; Astrom et al., 2011).
2. Data and Methods
2.1. Climate Zones
We used the building climate zones from the CEC (2015; Figure 1) to define unique climate zones within San Diego County based on similar climate and energy use patterns, as commonly used in epidemiologic studies in California (e.g., Sherbakov et al., 2017). Figure 1 shows the three CEC climate zones used in this study, which have dramatically different climates due to their varying distances from the coast. We refer to these regions as Coastal, Inland, and Desert.
Figure 1.
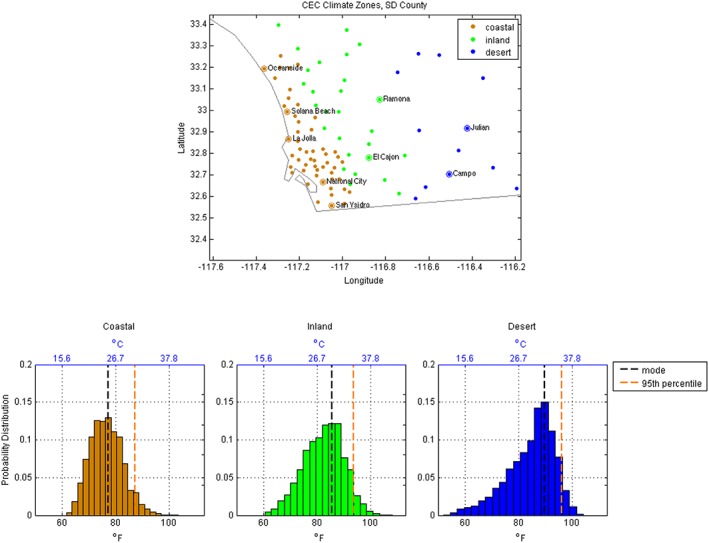
Top panel shows the three climate zones used in this study based on the California Energy Commission (2015) shown here interpolated to zip code. Lower panels show the warm season T max distribution along with the mode and 95th percentile for each climate zone. The black (blue) temperature scales along the lower (upper) horizontal axis give units in °F (°C).
2.2. Temperature Data
Local daily maximum temperatures were collected from Livneh et al. (2013) and aggregated over three regions in San Diego County. This data product is an observationally based gridded data set derived from daily station data interpolated to a 1/16° latitude–longitude grid. The source data are the cooperative observer (COOP) summaries of the day from the National Centers for Environmental Information supplemented by first‐order automated surface observing system observations (National Climatic Data Center, 2009). The Livneh data product is widely used in many scientific studies. It has advantages over station data in regions where stations are sparse. Additionally, it includes data quality measures above and beyond standard NECI practice (Livneh et al., 2013). The gridding uses the synergetic mapping system (SKYMAP, Shepard, 1984) where the temperature value at a grid point is a weighted average from the four nearest stations. Near COOP stations, there is very strong agreement between the station data and the gridded data (Livneh et al., 2013). For example, in San Diego County, we compared three high‐quality stations with long records located at San Diego International Airport, Miramar, and Cuyamaca (a coastal, inland, and desert location, respectively) with the nearest grid point from the Livneh product. The daily temperature correlation was above 0.94 for all locations (0.94, 0.99, and 0.98, respectively) over the period 1950–2013. For our analysis, all calculations were performed on the Fahrenheit temperature scale. Conversions to the Celsius scale are included for reference in the text and figures using °C = (5/9)*(°F − 32).
2.3. Health Outcome Data
Health outcomes and date of hospital admission were provided by the Office of Statewide Health Planning and Development PD data set from May through October 1999–2013, which were aggregated by region for this study. The PD data provided information on hospitalizations at acute care facilities throughout the State. For this study, we considered only unscheduled hospitalizations. The categories for outcomes used in this study included all cardiovascular diseases (ICD‐9 390–459), all respiratory diseases (460–519), acute renal failure (584), mental health (290–319), dehydration (276.5), and heat illness (992). We also used an “all causes” category, which was taken as the sum of the other six categories. The information contained in the PD data set includes zip code of the home address of the patient (not the treatment facility), age, and race/ethnicity. For this analysis, we aggregated the hospitalization data for each region described in section 2.1 (i.e., Coastal, Inland, and Desert). The aggregated PD data were filtered to remove periodic signals (seasonal and weekly cycles), holiday effects, and long‐term trends using the methodology described in Guirguis et al. (2014).
We determined the impact of elevated daily maximum temperatures on hospital admissions in three regions of San Diego County by comparing hospitalizations on days exceeding a given temperature threshold to what was typically observed during the 1999–2013 study period using the risk ratio (RR). The RR is defined in this study as the average number of hospitalizations that occurred on days exceeding a given temperature threshold divided by the average number of hospitalizations occurring overall, independent of any temperature threshold, after removing the influence of both secular and seasonal time trends. A significant health impact is defined using bootstrapping. Specifically, an outcome is significant if the result falls above the 95th percentile of the resampled distribution using 1,000 random samples.
The sample sizes differed between regions with the coastal zone being the most populous (Table 1). The sample size is also affected by the frequency at which a given temperature threshold was exceeded, so the temporal sample size was generally largest (smallest) in the Desert region (Coastal region), since hot temperatures are reached or exceeded there more (less) often (Table 1). While the difference in sample size does affect the sample variance and the width of confidence intervals for our estimates, we do not expect the sample size in one region to affect our inference in other regions. By design, the methodology treats each region separately and uses a self‐comparison approach where we compared health outcomes in one region for different temperature thresholds against a reference value for that same region.
Table 1.
Summary Statistics for Each of the Three Climate Regions Showing the Total Number of Hospitalizations in the Study Period, Average Regional Daily High Temperatures, and the Number of Days Exceeding Different Temperature Thresholds
| Total number of hospitalizations | May–October median daily high temperature | 95th Percentile | Number of days >80 °F (26.6 °C) | Number of days >85 °F (29.4 °C) | Number of days >90 °F (32.2 °C) | Number of days >95 °F (35.0 °C) | |
|---|---|---|---|---|---|---|---|
| Desert | 4,515 | 86.5 °F (30.3 °C) | 96.3 °F (35.7 °C) | 2,008 | 1,564 | 842 | 223 |
| Inland | 156,633 | 83.0 °F (28.3 °C) | 93.8 °F (34.3 °C) | 1,751 | 1,112 | 412 | 94 |
| Coastal | 346,042 | 76.3 °F (24.6 °C) | 87.3 °F (30.7 °C) | 799 | 245 | 60 | 11 |
| Coastal low AC saturation | 196,785 | 75.1 °F (23.9 °C) | 86.0 °F (30.0 °C) | 600 | 179 | 38 | 8 |
| Coastal high AC saturation | 149,257 | 77.5 °F (25.3 °C) | 88.7 °F (31.5 °C) | 995 | 338 | 97 | 18 |
Note. Also provided are summary statistics for the subset of zip codes within the Coastal region that have lower and higher rates of AC saturation (bottom two rows of data). AC = air conditioning.
Table 2.
Summary Statistics Showing the Total Number of Hospitalizations Within the Coastal Region for Different Population Categories During the Study Period
| Population category | Hospitalizations |
|---|---|
| Age | |
| 19–64 | 116,682 |
| 65 up | 216,544 |
| Race/Ethnicity | |
| White | 204,364 |
| Hispanic | 72,440 |
2.4. AC Access
To study local availability of home AC, we used the 2009 California Residential Appliance Saturation Study (CEC, 2010). This data set provided consumer responses to a 2009 questionnaire issued by the CEC, which focused on electric utility use, including AC ownership and use in the home, as well as economic and demographic information. For this study, we aggregated responses for each climate zone for income, race/ethnicity, and homeownership. The race/ethnicity categories were American Indian/Alaska Native, Asian or Pacific Islander, Black/African American, Hispanic/Latino, White/Caucasian, or Other. In this study, we only used information on central AC access and did not include window AC units. The sample size for window units was low with only 13% of Residential Appliance Saturation Study responders reported having window units (CEC, 2010). Previous studies have shown that window units are not effective at reducing negative health impacts due to heat (Ostro et al., 2010).
3. Results
3.1. Diverse Climatology in San Diego County
Local temperatures in San Diego County vary dramatically within relatively short spatial distances (Figure 2, left). The coastal population is used to much cooler conditions than inland residents, due to modulation by the Pacific Ocean that drives cool onshore flow and coastal cloudiness. Because of milder conditions at the coast, coastal residents are much less likely to have AC in their homes, and in fact, the AC saturation rate is very low in coastal San Diego (Figure 2, right). The median May–October temperature for each region is 76.3 °F (24.6 °C), 83.0 °F (28.3 °C), and 86.5 °F (30.3 °C), for the Coastal, Inland, and Desert regions, respectively. The 95th percentile temperature, representing a local threshold for extremely hot temperatures, is 87.3 °F (30.7 °C) for the Coastal region, 93.8 °F (34.4 °C) for the Inland region, and 96.3 °F (35.7 °C) for the Desert region (Table 1).
Figure 2.
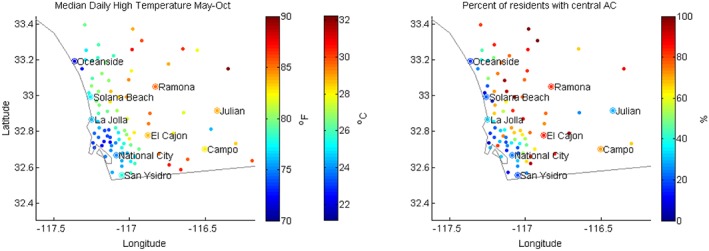
Median daily maximum temperatures during May–October (left) and AC access in San Diego County showing the percent of local residents who reported having central AC in their homes (right).
Although the daily maximum temperatures are generally cooler at the coast, the temperature distribution is strongly skewed with long warm tails (Figure 1, bottom left). This is partly due to the variability of marine layer cloud, which when absent can leave the coast unprotected during an inland heat wave (Clemesha et al., 2017). Additionally, heat waves associated with Santa Ana winds are common during September and October, which can bring very hot temperatures relative to the typical maritime climate. This marked skewness in the summertime T max temperature distribution in the Coastal region indicates the potential for very intense heat waves relative to the mean climate. For example, in the Coastal region, the 95th percentile temperature is 10.0 °F (5.6 °C) hotter than the distribution center (i.e., the mode) whereas in the Desert region the 95th percentile is only 6.4 °F (3.5 °C) hotter than the mode. Since coastal residents are not well acclimated to extreme heat either physiologically (due to the typically mild conditions) or technologically (through AC), we expect the potential for health impacts to be higher here than in other parts of the county.
3.2. Health Outcomes by Climate Zone
The health impacts associated with different temperature thresholds for the three climate regions of San Diego County are shown in Figure 3. We used daily maximum temperatures in the range of 65 °F (18.3 °C) to the regional 95th percentile (see Table 1); therefore, the upper bound varies by region. From Figure 3 (left column) a significant health effect is observed for all three regions for the heat illness category. Within this category, the temperature threshold at which a significant impact is observed emerged at cooler temperatures for the Coastal region than the Inland and Desert regions. In the Coastal region, a significant health impact (RR = 1.31; 95% confidence interval [CI; 1.07, 1.61]) emerged at 73 °F (22.7 °C). In the Inland region, we detected an impact (1.37; 1.07, 1.79) at temperatures at or above 79 °F (26 °C). In the Desert region, the initial impact (2.77; 1.09, 6.55) is seen at 90 °F (32.2 °C). The risk increases with hotter temperatures in all three regions. For the hottest temperatures (above the local 95th percentile), the RR reaches 4.19 (2.68, 6.36) in the Coastal region, RR = 3.79 (2.23, 6.01) in the Inland region, and RR = 8.90 (2.97, 23.74) for the Desert region.
Figure 3.
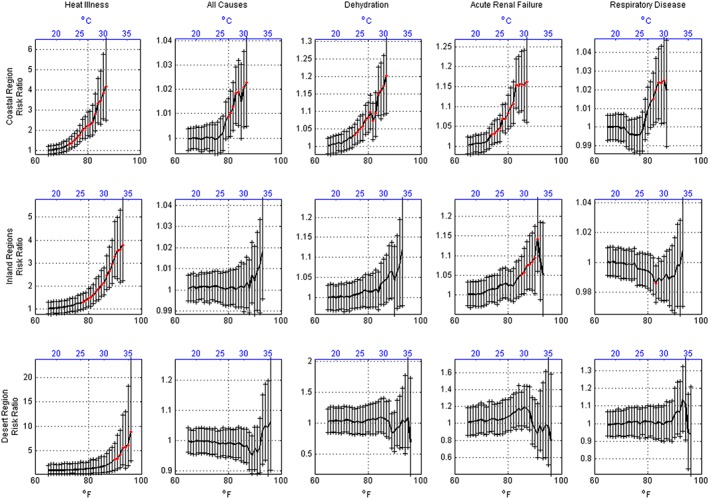
Health impact observed for three regions of San Diego County associated with increasing daily maximum temperature threshold levels. The risk ratio was calculated as the average excess hospitalizations observed on days exceeding a given T max temperature threshold compared to the average observed over the all days, independent of any temperature threshold. Error bars give the 95% confidence interval for the estimate. Red markers indicate statistical significance at the 95% level using Monte Carlo resampling. A significant value means the estimate was found to be above the 95th percentile of the resampled distribution.
Also shown in Figure 3 (columns 2–5), we observed a significant impact in the Coastal region for four other disease categories. At temperatures above 87 °F (30.6 °C), we found elevated risk for all causes (1.02; 1.01, 1.04), dehydration (1.20; 1.11, 1.31), acute renal failure (1.16; 1.06, 1.27), and respiratory disease (1.03; 1.01, 1.04). The health risk emerged at temperatures in the range of 74–81 °F (23–27 °C), depending on disease category.
For dehydration and respiratory disease, we did not find a significant health impact for the Inland and Desert regions. For acute renal failure, we found evidence of a heat impact in the Inland region for temperatures in the range of ~83–93 °F (29–34 °C). We also performed the analysis for cardiovascular disease and mental health and did not observe a significant relationship with temperatures for any region (not shown). For the Inland region and for some categories of the Desert region the risk estimates do not achieve significance, but the effect estimates are still elevated at higher temperatures, which could be due to the lower sample size.
3.3. Effect of AC Access on Health Outcomes in the Coastal Region
To study the effect of AC access on health outcomes during high ambient temperatures, we compared health outcomes for zip codes having different levels of AC saturation within the Coastal region. Specifically, we identified zip codes in the Coastal region where AC access was above or below the median saturation level. Here we focused on the all causes category, representing a more general outcome, which is also the category with the largest sample size. The results suggested a higher risk of heat‐related health impacts for those without AC. From Figure 4 (left), we see an upward shift in the number of hospitalizations at temperatures above 89 °F (31.6 °C), and especially at temperatures above 95 °F (35.0 °C) for the lower AC saturation group. This shift represents a significant change compared to hospitalizations during cooler days (<75 °F or 23.9 °C). At the hottest temperatures (>95 °F or 35 °C) hospital admissions increased by 14.6% (4.5%, 24.6%) compared to the mild‐day reference. From Figure 4 (right), we observed no significant change (α = 0.05) in hospitalizations in the higher AC saturation group.
Figure 4.
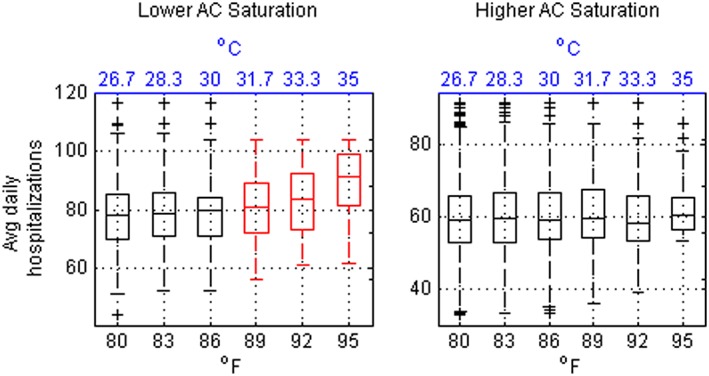
Daily average hospitalizations for zip codes within the Coastal region for days exceeding a given T max temperature threshold. The left plot shows distributions for zip codes with lower AC saturation and the right plot shows distributions for zip codes with higher AC saturation. Boxplots colored in red are significantly different (α = 0.05, t‐test for unequal means) from a reference taken as days cooler than 75 °F. The AC saturation level is defined as below or above the coastal zone median. Results are for the all causes category. Sample size information is provided in Table 1.
3.4. Disparities in AC Access
If, as these results suggest, lack of AC increases health risks on hot days, then it is important to identify those vulnerable populations who lack AC and who may therefore be more vulnerable to heat. We examined information on AC access in San Diego County and found disparities among the population. From Figure 5a, we see that AC access is low in general in the Coastal region. However, access to AC is more likely among those with higher incomes. Residents with incomes above $150,000 are more than three times as likely to have AC in their homes than those in the lowest income brackets. In fact, there is a strong correlation between AC ownership and income level in the Coastal region (r = 0.95). From Figures 5b and 5c, respectively, we see that Hispanics are less likely to have AC than Whites, and renters are less likely to have AC than homeowners. These disparities could affect health outcomes during extreme heat. In fact, other studies have shown that poorer and minority populations are known to be more vulnerable to heat‐related health impacts (e.g., Basu, 2009), and these results suggest that lack of AC access could add to this burden.
Figure 5.
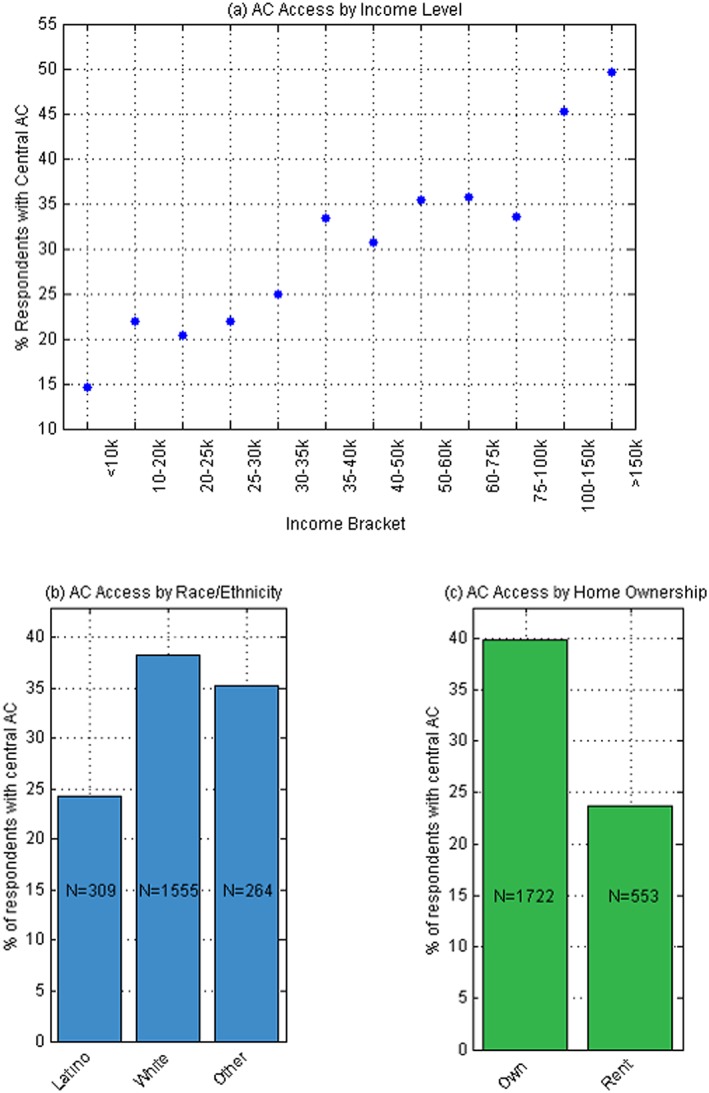
The percent of RASS respondents with central air conditioning in the Coastal region according to income level (a), race/ethnicity (b), and homeownership (c). The race/ethnicity category “Other” refers to American Indians, Asian/Pacific Islanders, and Blacks, which were combined due to small sample size. There were 25,721 RASS respondents in the Coastal region. RASS = Residential Appliance Saturation Study.
3.5. Disparities in Health Outcomes
Figure 6 shows excess hospitalizations for the all causes category for Hispanics and Whites for different temperature thresholds. From this Figure, a significant impact is seen among Whites at temperatures above 95 °F/35 °C (9.3% increase from the mild‐day reference in mean daily hospitalizations, CI [0.3%, 18.2%]) whereas no significant change is seen in hospital admissions for Hispanics. This implies that although Hispanic populations are disadvantaged in terms of AC access, and Hispanics also tend to be disadvantaged socioeconomically in general compared to Whites (e.g., lower rates of health insurance, higher poverty rates, and less education; Centers for Disease Control and Prevention, 2015), their health is less impacted by heat events.
Figure 6.
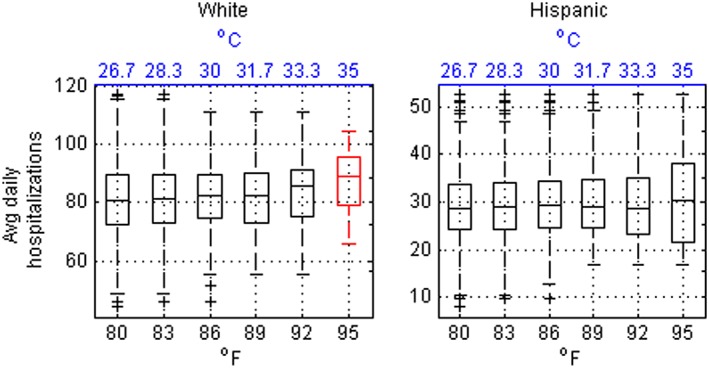
As in Figure 4 but for Whites (left) and Hispanics (right) living in the Coastal region. Sample size information is provided in Tables 1 and 2.
Figure 7 shows results for persons aged 19–64 and 65 and older. In the 65 and older age group, there is a significant increase in hospital admissions relative to the mild‐day reference for temperatures above 83 °F/28.3 °C and for each successive temperature exceedance threshold. At the hottest temperatures (>95 °F/35 °C) daily mean hospital admissions for this group increased 9.9% (CI [2.0%, 17.8%]). For the 19–64 age group, we see no change in hospitalizations with increasing temperature.
Figure 7.
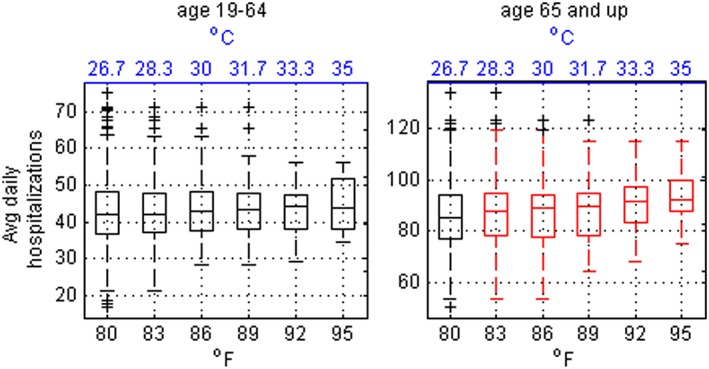
As in Figure 4 but for different age categories within the Coastal region.
4. Conclusions
Our results suggest that coastal San Diegans are more sensitive to heat than inland residents. More specifically, heat‐related health impacts start to be observed at lower temperatures suggesting that specific adaptation strategies are needed. We investigated health outcomes in the form of excess hospitalizations associated with elevated daily maximum temperatures in three different climate zones in the climatologically and demographically diverse region of San Diego County, California. We found that a significant health impact due to heat illness emerged at lower temperatures in the Coastal region compared to the Inland and Desert regions. This is consistent with expectations due to acclimatization to cooler temperatures there.
We also found heightened heat sensitivity in zip codes within the Coastal region, where fewer residents have central AC. Additionally, when we looked at AC access, we found notable disparities related to income level, race/ethnicity, and homeownership. We found that less than half of the coastal population has AC but AC ownership is more likely for coastal residents in higher income brackets. Renters are less likely to have AC than homeowners, and Hispanics are less likely to have AC than Whites. These findings have important implications for climate change as these existing disparities in San Diego County will likely increase as homeowners with higher incomes will be better able to adapt to rising temperatures.
Disparities in AC ownership did not translate to a higher rate of hospitalizations among Hispanics. This finding has also been observed in other epidemiological studies and has been referred to as the Hispanic paradox, which describes research findings showing that in the United States, Hispanics tend to have better health outcomes than Whites even though they have higher poverty rates, less education, and higher rates of being uninsured, all of which are risk factors for poor health outcomes (Centers for Disease Control and Prevention, 2015). Possible explanatory factors cited include lower rates of smoking, higher levels of family support, immigration of healthy individuals to the United States, and return of unhealthy individuals to their birth country (Singh et al., 2013). Other studies have disputed the existence of the paradox citing discrepancies in reporting (Smith & Bradshaw, 2006). In our study, it is possible or even likely that, given lower rates of being insured, Hispanics are less likely to seek medical care or, if they do, are less likely to be admitted to the hospital. Additionally, given the close proximity to the Mexican border, Hispanics living in San Diego might seek medical care across the border where costs are lower. In fact, cross‐border care is quite common in California (Seid et al., 2003; Wallace et al., 2009) and this could result in the underrepresentation of heat‐related illness among Hispanics in our study, which only uses hospitalization data from the U.S. side of the border.
We did observe disparities in health outcomes for different age groups in San Diego County. Analyses of health outcomes for ages 0–5, 19–64, and over 64 years showed a higher health impact for the oldest group, a finding that is consistent with many other epidemiology studies showing the elderly are a high‐risk group for heat‐related health impacts (Basu, 2009; Astrom et al., 2011).
Improved health care, effective heat warnings, public awareness, education, and access to AC can reduce heat‐related health impacts. Heat mortality and morbidity will likely increase without additional adaptation measures and reduction in heat exposures, which could include more green spaces, improved access to cooling centers, targeted outreach to vulnerable individuals, and improved heat warnings and emergency response. For example, based on climate model projections we could see over 500 excess cases of heat‐related mortality in San Diego County per year by 2090 compared to 68 currently (Sheridan et al., 2012). While some acclimatization to changing temperatures is likely, the rate and efficacy of acclimatization is unknown. This study showed that AC can reduce risk during extreme heat. However, other studies of future health impacts due to climate change showed that increases in mortality will be only partly offset by increases in AC ownership (Ostro et al., 2011). Since people tend to adapt to average conditions rather than extremes, increases in AC ownership along the coast are likely to be slow, and it is not practical to expect that all residents will be able to afford the cost of installation or operation. Window units, which are more affordable to purchase than central AC, have been shown to be less effective at reducing heat illness (Ostro et al., 2010), and there is still the cost of operation, which could be prohibitive for low‐income populations. Further, added AC use would increase the energy burden in the region and add to the emissions responsible for climate change.
The varied climatology in San Diego County is likely to play a role in future acclimatization. Research has shown that while average temperatures may increase more slowly in coastal areas due to modulation by the Pacific Ocean, heat wave intensity is expected to increase more strongly at the coast. For example, Gershunov and Guirguis (2012) studied observed and projected heat wave activity over California and found that, along the coast, the hot tail (95th percentile) is increasing at a faster rate than is the median, and this trend is projected to continue. This means that heat waves at the coast are becoming more intense relative to the average climate. Other studies have noted similar patterns in Mediterranean climates (Diffenbaugh et al., 2007). This suggests that coastal Californians may be increasingly vulnerable to heat impacts. Additionally, future behavior of coastal clouds and Santa Ana winds, which are responsible for modulating heat wave activity at the coast, is highly uncertain.
There are some limitations to this study. One limitation is the nature of the AC data, which was obtained from a residential survey. The residents who responded are a small subset of the population, and it is possible that the respondents do not adequately represent the zip code population as a whole. Another limitation is that we do not know where the patient was when they became ill, from our data we only know where they live. Given the high spatial variability of temperatures in the region, it is possible that in some cases the temperature of exposure was much higher than the temperature of residence if an individual traveled only a short distance inland. Additionally, the use of hospitalization data does not provide information on the full spectrum of heat illness. Most people who become ill during heat episodes will be treated and released at emergency or urgent care facilities, or might stay home and self‐treat. Therefore, these results represent only the most severe cases. In addition, there are factors other than high temperatures could contribute to the observed health effects, such as humidity, air pollution, Santa Ana winds, or smoke from wildfires that periodically occur during heat waves in San Diego.
This study contributes to a growing body of research showing the health risks associated with high ambient temperatures. Our results show the importance of climatological acclimatization in determining health outcomes during extreme heat, which highlights the need for location‐specific heat warnings and emergency response strategies. Additionally, our results show that not all individuals respond equally, even if living in the same climate zone. Individuals who are elderly, have preexisting conditions, or lack AC are more vulnerable to heat and would benefit from a tiered alert system that accounts for different levels of risk. Given that heat waves are expected to become more frequent and more intense due to climate change, targeted intervention strategies are needed to reduce illness due to heat exposure.
Conflict of Interest
The authors declare no conflicts of interest relevant to this study.
Acknowledgments
This work was funded by the UCSD Institute for Public Health with additional support from Climate Education Partners through funding by the National Science Foundation under award DUE‐1239797, the University of California Multicampus Research Programs and Initiatives (MRPI), NOAA Coastal and Ocean Climate Applications (COCA) program grant NA15OAR4310114, and by NOAA via the RISA program through the California and Nevada Applications Program grant NA17OAR4310284. The observational temperature data set is freely and publicly available from the University of Washington (ftp://ftp.hydro.washington.edu/pub/blivneh/CONUS/). Health data are distributed by the Office of Statewide Health Planning and Development (https://www.oshpd.ca.gov/HID/Patient-Discharge-Data.html). The Residential Appliance Saturation Study data are from the California Energy Commission (http://www.energy.ca.gov/appliances/rass/). We thank two anonymous reviewers for helpful comments during the evaluation of this paper.
Guirguis, K. , Basu, R. , Al‐Delaimy, W. K. , Benmarhnia, T. , Clemesha, R. E. S. , Corcos, I. , et al. (2018). Heat, disparities, and health outcomes in San Diego County's diverse climate zones. GeoHealth, 2, 212–223. 10.1029/2017GH000127
This article was corrected on 15 JUL 2019. The online version of this article has been modified to include a Conflict of Interest statement.
References
- Anderson, G. B. , & Bell, M. L. (2011). Heat waves in the United States: Mortality risk during heat waves and effect modification by heat wave characteristics in 43 US communities. Environmental Health Perspectives, 119(2), 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astrom, D. O. , Bertil, F. , & Joacim, R. (2011). Heat wave impact on morbidity and mortality in the elderly population: A review of recent studies. Maturitas, 69(2), 99–105. 10.1016/j.maturitas.2011.03.008 [DOI] [PubMed] [Google Scholar]
- Basu, R. (2009). High ambient temperature and mortality: A review of epidemiological studies from 2001 to 2008. Environmental Health, 8(40). 10.1186/1476-069X-8-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu, R. , & Malig, B. (2011). High ambient temperature and mortality in California: Exploring the roles of age, disease, and mortality displacement. Environmental Research, 111, 1286–1292. [DOI] [PubMed] [Google Scholar]
- Basu, R. , Pearson, D. , Malig, B. , Broadwin, R. , & Green, S. (2012). The effect of elevated ambient temperature on emergency room visits. Epidemiology, 23, 813–820. [DOI] [PubMed] [Google Scholar]
- Benmarhnia, T. , Bailey, Z. , Kaiser, D. , Auger, N. , King, N. , & Kaufman, J. S. (2016). A difference‐in‐differences approach to assess the effect of a heat action plan on heat‐related mortality, and differences in effectiveness according to sex, age, and socioeconomic status (Montreal, Quebec). Environmental Health Perspectives, 124(11), 1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benmarhnia, T. , Deguen, S. , Kaufman, J. S. , & Smargiassi, A. (2015). Vulnerability to heat‐related mortality: A systematic review, meta‐analysis, and meta‐regression analysis. Epidemiology, 26(6), 781–793. [DOI] [PubMed] [Google Scholar]
- Benmarhnia, T. , Kihal‐Talantikite, W. , Ragettli, M. S. , & Deguen, S. (2017). Small‐area spatiotemporal analysis of heatwave impacts on elderly mortality in Paris: A cluster analysis approach. Science of the Total Environment, 592, 288–294. [DOI] [PubMed] [Google Scholar]
- Bobb, J. F. , Obermeyer, Z. , Wang, Y. , & Dominici, F. (2014). Cause‐specific risk of hospital admission related to extreme heat in older adults. Journal of the American Medical Association, 312(24), 2659–2667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Energy Commission (2010). California Statewide Residential Appliance Saturation Study: Final report (Report no. CEC‐200‐2010‐004). Sacramento, CA: California Energy Commission; 2010. Retrieved from http://www.energy.ca.gov/appliances/rass/. (Date accessed: March 2, 2018).
- California Energy Commission (2015). California Building Climate Zone Areas. Retrieved from http://www.energy.ca.gov/maps/renewable/building_climate_zones.html
- Centers for Disease Control and Prevention (2015). Vital signs: Leading causes of death, prevalence of diseases and risk factors, and use of health services among Hispanics in the United States—2009‐2013, Morbidity and Mortality Weekly Report, 64(17), 469–478, May 8, 2015. [PMC free article] [PubMed] [Google Scholar]
- Chen, K. , Bi, J. , Chen, J. , Chen, X. , Huang, L. , & Zhou, L. (2015). Influence of heat wave definitions to the added effect of heat waves on daily mortality in Nanjing, China. Science of the Total Environment, 506, 18–25. [DOI] [PubMed] [Google Scholar]
- Clemesha, R. E. S. , Guriguis, K. , Gershunov, A. , Small, I. J. , & Tardy, A. (2017). California heat waves: Their spatial evolution, variation, and coastal modulation by low clouds. Climate Dynamics. 10.1007/s00382-017-3875-7 [DOI] [Google Scholar]
- Curriero, F. C. , Heiner, K. S. , Samet, J. M. , Zeger, S. L. , Strug, L. , & Patz, J. A. (2002). Temperature and mortality in 11 cities of the eastern United States. American Journal of Epidemiology, 155(1), 80–87. [DOI] [PubMed] [Google Scholar]
- Diffenbaugh, N. S. , Pal, J. S. , Giorgi, F. , & Gao, X. (2007). Heat stress intensification in the Mediterranean climate change hotspot. Geophysical Research Letters, 34, L11706 10.1029/2007GL030000 [DOI] [Google Scholar]
- Gasparrini, A. , Guo, Y. , Hashizume, M. , Lavigne, E. , Zanobetti, A. , Schwartz, J. , et al. (2015). Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet, 386(9991), 369–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershunov, A. , Cayan, D. R. , & Iacobellis, S. F. (2009). The great 2006 heat wave over California and Nevada: Signal of an increasing trend. Journal of Climate, 22, 6181–6203. [Google Scholar]
- Gershunov, A. , & Guirguis, K. (2012). California heat waves in the present and future. Geophysical Research Letters, 39, L18710 10.1029/2012GL052979 [DOI] [Google Scholar]
- Gershunov, A. , Johnston, Z. , Margolis, H. , & Guirguis, K. (2011). The California Heat Wave 2006 with Impacts on Statewide Medical Emergency: A space‐time analysis. Geography Research Forum, 31, 53–69. [Google Scholar]
- Gronlund, C. J. (2014). Racial and socioeconomic disparities in heat‐related health effects and their mechanisms: A review. Current Epidemiology Reports, 1(3), 165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guirguis, K. , Gershunov, A. , Tardy, A. , & Basu, R. (2014). The impact of recent heat waves on human health in California. Journal of Applied Meteorology and Climatology, 53, 3–19. [Google Scholar]
- Hondula, D. M. , & Barnett, A. G. (2014). Heat‐related morbidity in Brisbane, Australia: Spatial variation and area‐level predictors. Environmental Health Perspectives, 122, 831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowlton, K. , Rotkin‐Ellman, M. , King, G. , Margolis, H. G. , Smith, D. , Solomon, G. , et al. (2009). The 2006 California heat wave: Impacts on hospitalizations and emergency department visits. Environmental Health Perspectives, 117(1), 61–67. 10.1289/ehp.11594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livneh, B. , Rosenberg, E. A. , Lin, C. , Nijssen, B. , Mishra, V. , Andreadis, K. M. , et al. (2013). A long‐term hydrologically based dataset of land surface fluxes and states for the conterminous United States: Update and extensions. Journal of Climate, 26, 9384–9392. [Google Scholar]
- Medina‐Ramón, M. , & Schwartz, J. (2007). Temperature, temperature extremes, and mortality: A study of acclimatisation and effect modification in 50 US cities. Occupational and Environmental Medicine, 64, 827–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Climatic Data Center (2009). Data documentation for data set 3200 (DSI‐3200): Surface land daily cooperative summary of the day, report, Asheville, NC. Retrieved from https://www1.ncdc.noaa.gov/pub/data/documentlibrary/tddoc/td3200.pdf
- National Weather Service (2017). Natural Hazard Statistics. Retrieved from http://www.nws.noaa.gov/om/hazstats/resources/weather_fatalities.pdf
- Ostro, B. , Rauch, S. , Green, R. , Malig, B. , & Basu, R. (2010). The effects of temperature and use of air conditioning on hospitalizations. American Journal of Epidemiology, 172, 1053–1061. [DOI] [PubMed] [Google Scholar]
- Ostro, B. , Rauch, S. , & Green, S. (2011). Quantifying the health impacts of future changes in temperature in California. Environmental Research, 8, 1258–1264. [DOI] [PubMed] [Google Scholar]
- Ostro, B. D. , Roth, L. A. , Green, B. S. , & Basu, R. (2009). Estimating the mortality effect of the July 2006 California heat wave. Environmental Research, 109(5), 614–619. 10.1016/j.envres.2009.03.010 [DOI] [PubMed] [Google Scholar]
- Price, K. , Perron, S. , & King, N. (2013). Implementation of the Montreal heat response plan during the 2010 heat wave. Canadian Journal of Public Health, 104(2), e96–e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- San Diego Union Tribune (2017). Heat wave causes early school closures Friday.
- Seid, M. , Castañeda, D. , Mize, R. , Zivkovic, M. , & Varni, J. W. (2003). Crossing the border for health care: Access and primary care characteristics for young children of Latino farm workers along the US‐Mexico border, Ambulatory Pediatrics, 3(3), 121‐130. [DOI] [PubMed] [Google Scholar]
- Shepard, D. S. (1984). Computer Mapping: The SYMAP Interpolation Algorithm In Gaile G. L. & Willmott C. J. (Eds.), Spatial Statistics and Models. Theory and Decision Library (An International Series in the Philosophy and Methodology of the Social and Behavioral Sciences) (Vol 40). Dordrecht: Springer. [Google Scholar]
- Sherbakov, T. , Malig, B. , Guirguis, K. , Gershunov, A. , & Basu, R. (2017). Ambient temperature and added heat wave effects on hospitalizations in California from 1999 to 2009. Environmental Research, 160, 83–90. 10.1016/j.envres.2017.08.052 [DOI] [PubMed] [Google Scholar]
- Sheridan, S. C. , Allen, M. , Lee, C. C. , & Kalkstein, L. S. (2012). Future heat vulnerability in California, Part II: Projecting future heat related mortality. Climatic Change, 115, 311–326. [Google Scholar]
- Singh, G. K. , Rodriguez‐Lainz, A. , & Kogan, M. D. (2013). Immigrant health inequalities in the United States: Use of Eight Major National Data Systems. The Scientific World Journal, 21, 512313 10.1155/2013/512313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, D. P. , & Bradshaw, B. S. (2006). Rethinking the Hispanic Paradox: Death rates and life expectancy for US Non‐Hispanic White and Hispanic populations. American Journal of Public Health, 96(9), 1686–1692. 10.2105/AJPH.2003.035378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, S. , Wang, X. Y. , & Barnett, A. G. (2010). Assessment of heat‐related health impacts in Brisbane, Australia: Comparison of different heatwave definitions. PLoS One, 5(8), e12155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaneckova, P. , Beggs, P. J. , & Jacobson, C. R. (2010). Spatial analysis of heat‐related mortality among the elderly between 1993 and 2004 in Sydney, Australia. Social Science & Medicine, 70, 293–304. [DOI] [PubMed] [Google Scholar]
- Wallace, S. P. , Mendez‐Luck, C. , & Castañeda, X. (2009). Heading South: Why Mexican immigrants in California seek health services in Mexico. Medical Care, 47(6), 662–669. 10.1097/MLR.0b013e318190cc95 [DOI] [PMC free article] [PubMed] [Google Scholar]


