Abstract
Climate change threatens human health, but there remains a lack of evidence on the economic toll of climate‐sensitive public health impacts. We characterize human mortality and morbidity costs associated with 10 climate‐sensitive case study events spanning 11 US states in 2012: wildfires in Colorado and Washington, ozone air pollution in Nevada, extreme heat in Wisconsin, infectious disease outbreaks of tick‐borne Lyme disease in Michigan and mosquito‐borne West Nile virus in Texas, extreme weather in Ohio, impacts of Hurricane Sandy in New Jersey and New York, allergenic oak pollen in North Carolina, and harmful algal blooms on the Florida coast. Applying a consistent economic valuation approach to published studies and state estimates, we estimate total health‐related costs from 917 deaths, 20,568 hospitalizations, and 17,857 emergency department visits of $10.0 billion in 2018 dollars, with a sensitivity range of $2.7–24.6 billion. Our estimates indicate that the financial burden of deaths, hospitalizations, emergency department visits, and associated medical care is a key dimension of the overall economic impact of climate‐sensitive events. We found that mortality costs (i.e., the value of a statistical life) of $8.4 billion exceeded morbidity costs and lost wages ($1.6 billion combined). By better characterizing health damages in economic terms, this work helps to shed light on the burden climate‐sensitive events already place on U.S. public health each year. In doing so, we provide a conceptual framework for broader estimation of climate‐sensitive health‐related costs. The high health‐related costs associated with climate‐sensitive events highlight the importance of actions to mitigate climate change and adapt to its unavoidable impacts.
Keywords: climate change, health, valuation, morbidity, mortality, extreme events
Key Points
Climate change threatens human health, but there remains a lack of evidence on the economic toll of the adverse public health impacts of climate‐sensitive events
We estimate $10.0 billion (2018 dollars) in health‐related costs from 10 climate‐sensitive U.S. case study events during 2012
This work helps to shed light on the high burden climate‐sensitive events already place on U.S. public health each year
1. Introduction
Global climate change is underway and accelerating, posing a vast array of direct and indirect threats to human health (Intergovernmental Panel on Climate Change, 2018; U.S. Global Change Research Program, 2016, 2018). Despite growing evidence of the harmful health impacts of climate change and its exacerbation of global inequality (Diffenbaugh & Burke, 2019), there remains a dearth of evidence on the personal and societal economic toll of climate‐sensitive events; numerous studies have called for more investigation on this issue (Diaz & Moore, 2017; Government Accountability Office, 2017; Gropp, 2017; Hutton & Menne, 2014; U.S. Global Change Research Program, 2016).
Cost valuation of climate‐sensitive health impacts is useful for several purposes. First, valuation estimates illuminate a tangible yet understudied impact of climate change and shed light on how this threat is affecting sectors far beyond infrastructure and agriculture (Revesz et al., 2014; Watts, Amann, Arnell, et al., 2018). Some estimates of the economic toll of climate‐sensitive hazards include property and crop damage but limited health data (Bouwer, 2011; Hsiang et al., 2017; Smith & Katz, 2013; U.S. National Oceanic and Atmospheric Administration, 2016), and health impacts (especially human morbidity) are rarely adequately incorporated into economic assessments of climate change impacts (Nordhaus, 1991; Smith & Katz, 2013; U.S. National Oceanic and Atmospheric Administration, 2019) or key measures such as the social cost of carbon, which are central to climate change policy cost‐benefit analyses (Greenstone et al., 2013; Howard, 2014; Marten et al., 2013). Second, such work demonstrates the potential future costs of the continuing increase in global greenhouse gas concentrations: Health‐related cost estimates illuminate how costly future climate‐sensitive events may be, given our understanding of recent climate impacts on health (IPCC, 2018). Third, cost estimations can guide health interventions and help society assess whether investments in climate adaptation measures are achieving their intended benefits (Ebi et al., 2018).
Nationally, public health preparedness for climate‐sensitive health impacts is inadequate, with limited resources designated for strategic resource deployment, public education, and outreach to vulnerable communities (Brown, 2016; Ebi et al., 2016; Eidson et al., 2016; Gilmore & St. Clair, 2018; Grossman et al., 2019; Salas et al., 2018; Sheehan et al., 2017). At the state and local levels, there is considerable variability in public health capacity to respond to climate change (Carr et al., 2012; Roser‐Renouf et al., 2016; Shimamoto & McCormick, 2017). Expanded quantification of the budgetary pressures posed by climate change on the health sector can help decision makers to better engage with the scale of this challenge (Bierbaum et al., 2013; Watts, Amann, Ayeb‐Karlsson, et al., 2018).
A prior study estimated health‐related costs from premature mortality and morbidity in the U.S. from six climate‐sensitive events occurring between 2000 and 2009 (Knowlton et al., 2011), and this research improves upon the methodological approach employed in that work. We consider case studies from one year (2012) to further articulate the potential scope of climate‐sensitive health‐related costs in the U.S. using “publicly‐available” health impact and healthcare utilization data. This study encompasses health impacts not previously included (e.g., hurricane effects on pregnancy complications, carbon monoxide exposures, and mental health, as well as the health implications of harmful algal blooms, allergenic oak pollen, and tick‐borne Lyme disease), and contextualizes health‐related costs relative to 2012 estimates of the broad economic impacts of climate‐sensitive events, such as the billion dollar disaster list compiled annually by the National Oceanic and Atmospheric Administration (NOAA; U.S. National Oceanic and Atmospheric Administration, 2019).
The case studies explored here represent a limited sample of events that occurred within a single year, have been analyzed for estimates of event‐related mortality and specific causes of morbidity, cover a diverse geography of the U.S., and are emblematic of the scope of anticipated future climate‐sensitive health impacts (P. Stott, 2016; Watts, Amann, Arnell, et al., 2018; U.S. Global Change Research Program, 2018). The evidence base for national climate‐sensitive health‐related costs is growing (Balbus et al., 2014; Martinich & Crimmins, 2019; U.S. Global Change Research Program, 2018). Published studies include estimates related to impacts from air pollution (Fann et al., 2015), extreme heat (Lay et al., 2018), wildfires (Fann et al., 2018), allergenic oak pollen (Anenberg et al., 2017), harmful algal blooms (P. Hoagland & Scatasta, 2006; Porter Hoagland et al., 2009), and vector‐borne infectious diseases (Adrion et al., 2015; Shankar et al., 2014). Such studies commonly analyze a single climate‐sensitive exposure category and apply distinct valuation methods. Therefore, synthesis of fragmented health impact and cost estimates using a consistent valuation approach is challenging. Our analysis builds upon prior state‐level climate change valuation research by integrating recent data from state and national health surveillance systems, epidemiologic analyses, and other “publicly‐available” data to consider morbidity and mortality costs across a range of health impacts in a consistent way. In doing so, we demonstrate a conceptual framework for the estimation of other health‐related costs linked to climate‐sensitive events and provide a methodology for broader quantification of these costs.
2. Materials and Methods
2.1. Case Study Selection
To identify climate‐sensitive case studies, we surveyed the peer‐reviewed literature, “publicly‐available” state and federal agency data systems, and online reports for evaluations of the health impacts of 2012 events. We focus our climate‐sensitive health cost estimates on impacts occurring in 2012, when the country experienced some of its then‐warmest weather to date, widespread drought, significant wildfires, an outbreak of West Nile virus, and 10 hurricanes (Climate Central, 2012; U.S. National Oceanic and Atmospheric Administration, 2013a, 2013b). Our review yielded a range of health incidence data for morbidity and mortality associated with 2012 climate‐sensitive events. To select case studies, we prioritized data availability, geographic representativeness, and variation in event type, duration, and intensity. Morbidity data (hospital admissions [HAs] and emergency department visits [EDs]) were included if the information utilized primary case definitions provided by the International Classification of Disease (ICD), Ninth or Tenth Revision (U.S. Centers for Disease Control and Prevention, 2015). For events with multiple published health impact analyses (e.g., Hurricane Sandy), we sought to conservatively capture the documented range of health effects by prioritizing peer‐reviewed studies with statistically significant findings of health impacts and accounting for potential double counting of impacts.
Importantly, only a portion of the 2012 case studies included here consider attribution links to climate change. While research attributing discrete events to climate change has gained precision (Ebi et al., 2017), attribution was not the focus of our case study selection. Rather, these climate‐sensitive case studies encompass varying degrees of certainty about links to climate change (P. A. Stott et al., 2010; U.S. Global Change Research Program, 2018). These case studies are consistent with the long‐term projections for climate change impacts for extreme heat (Christidis et al., 2011; Hansen et al., 2006; Meehl et al., 2007; Vogel et al., 2019; Zwiers et al., 2011), hurricanes (Keellings & Hernández Ayala, 2019), harmful algal blooms (Hilborn et al., 2014; Poh et al., 2019) and other extreme weather (Nilsen et al., 2011; Papalexiou & Montanari, 2019); allergenic pollen (Anenberg et al., 2017; L. H. Ziska et al., 2019), ozone air pollution (Fann et al., 2015; Kinney, 2018), wildfires (Abatzoglou & Williams, 2016; Liu et al., 2016), West Nile virus (Belova et al., 2017; Paull et al., 2017), and Lyme disease (Monaghan et al., 2015).
Our investigation spans 10 climate‐sensitive case study events across 11 U.S. states: wildfires in Colorado and Washington, ozone air pollution in Nevada, heat stress in Wisconsin, infectious disease outbreaks of tick‐borne Lyme disease in Michigan and mosquito‐borne West Nile virus (WNV) in Texas, extreme weather in Ohio, Hurricane Sandy (impacts in New Jersey and New York), allergenic oak pollen in North Carolina, and harmful algal blooms on the Florida coast (Figure 1).
Figure 1.
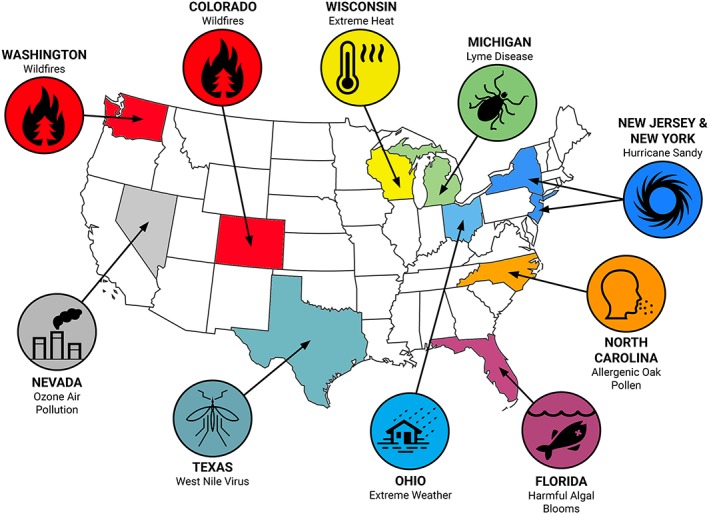
Ten climate‐sensitive case study events from 2012 included in the health‐related cost valuation.
The environmental exposures included in our analysis are each influenced by climate change (to differing degrees) and are expected to increase in frequency, intensity, duration, and/or areal extent in the future (U.S. Global Change Research Program, 2016). We augmented directly reported health incidence information with imputed incidence data from national healthcare utilization statistics (see section 3.2). The amount of available health impact information varied by case study; Table 1 provides an overview of the range of data sources utilized to estimate morbidity and mortality incidence.
Table 1.
Primary Health Effect Incidence Data Sources for Each Climate‐Sensitive Case Study
| State | Case study | Peer‐reviewed literature (number of studies) | State‐collected health data | U.S. Centers for Disease Control and Prevention (CDC) | U.S. Environmental Protection Agency (EPA) | U.S. National Atmospheric and Oceanic Administration (NOAA) | Other data source(s) |
|---|---|---|---|---|---|---|---|
| Michigan | Lyme disease | ✓ (1) | ✓ | ✓ | |||
| Ohio | Extreme weather | ✓ (2) | ✓ | ✓ | ✓ (Ohio Emergency Operations Center) | ||
| Wisconsin | Extreme heat | ✓ (1) | ✓ | ✓ | |||
| North Carolina | Allergenic oak pollen | ✓ (2) | ✓ | ✓ | ✓ (U.S. Census Bureau) | ||
| Nevada | Ozone air pollution | ✓ (2) | ✓ | ||||
| Texas | West Nile virus | ✓ (1) | ✓ | ✓ | |||
| Colorado | Wildfires | ✓ (2) | ✓ | ✓ | ✓ | ✓ (Munich RE) | |
| Washington | Wildfires | ✓ (2) | ✓ | ✓ | ✓ (U.S. National Interagency Fire Center) | ||
| Florida | Harmful algal blooms | ✓ (1) | ✓ | ✓ | |||
| New Jersey | Hurricane Sandy | ✓ (9) | ✓ | ✓ | |||
| New York | ✓ (12) | ✓ | ✓ (U.S. Census Bureau) |
2.2. Health‐Related Cost Valuation Methods
There have been multiple assessments of health‐related costs of specific climate‐sensitive events in recent years, including wildfires (Fann et al., 2018), extreme heat (Lay et al., 2018), air pollution (Carvour et al., 2018; Saari et al., 2017), infectious disease (Adrion et al., 2015), and allergenic oak pollen (Anenberg et al., 2017). These studies employ a range of health cost valuation techniques, including consideration of morbidity via direct healthcare costs (Anenberg et al., 2017) and mortality using willingness‐to‐pay approaches (Saari et al., 2017). These different methodologies help demonstrate distinct approaches toward the valuation of health impacts but make it difficult to aggregate costs in a consistent fashion. This study advances a consistent health‐related cost estimation (utilizing both cost‐of‐illness approach for morbidity and willingness to pay‐derived estimates for the value of a statistical life, VSL) across case study events by linking a defined set of diagnosis codes to cost information from national data sets (Figure 2).
Figure 2.
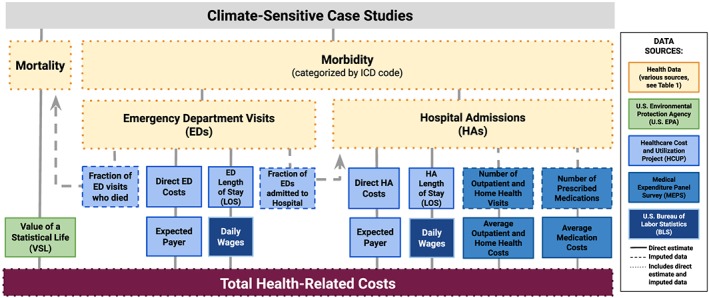
Data sources for health‐related cost estimates for all case studies. Yellow boxes represent health incidence data (various sources; see Table 1), the green box represents the VSL estimate (U.S. Environmental Protection Agency, 2014), light blue boxes represent data from HCUP (U.S. Agency for Healthcare Research and Quality, n.d.‐a), medium blue boxes represent data from MEPS (U.S. Agency for Healthcare Research and Quality, n.d.‐b), and dark blue boxes represent wage data from the BLS (U.S. Bureau of Labor Statistics, 2016). Solid lines are direct estimates, dashed lines are imputed data, and dotted lines denote a combination of direct and imputed data.
Costs were calculated using methods updated from Knowlton et al. (2011), an incidence‐based cost of illness approach that encompasses medical costs from the Healthcare Cost and Utilization Project (HCUP) and estimates of lost worker productivity. The HCUP database is a Federal‐State‐Industry partnership sponsored by the U.S. Agency for Healthcare Research and Quality (AHRQ) that compiles longitudinal hospital care data in the U.S. We accessed national HCUP data using an online tool that displays hospital care data specific to primary ICD diagnosis and expected payer for aggregate annual costs (U.S. Agency for Healthcare Research and Quality, n.d.‐a). The HCUP web tool provided the conversion rate from hospital charges to costs using a combination of state and national hospital accounting data. To supplement this information, we accessed information from the Medical Expenditure Panel Survey (MEPS), an AHRQ‐sponsored survey that compiles health expenditure data from individuals, medical providers, and employers (U.S. Agency for Healthcare Research and Quality, n.d.‐b). MEPS data (in the Household Component Survey) included the average cost per ED visit, annual out‐of‐pocket expenses for ED patients, and outpatient expenses for disease categories.
We also estimated the indirect economic impacts of lost wages during HAs and EDs using length‐of‐stay (LOS) data from HCUP. We calculated lost worker productivity using the median weekly earnings of full‐time employees in 2012 as reported by the U.S. Bureau of Labor Statistics (BLS; U.S. Bureau of Labor Statistics, 2016). For each health outcome with LOS data available in HCUP for the primary ICD diagnosis code, we multiplied the LOS number of days by the average daily earning from BLS for 2012. Health‐related costs were adjusted to 2018 dollars using the Personal Consumption Expenditures Index from the U.S. Bureau of Economic Analysis (Dunn et al., 2018; U.S. Bureau of Economic Analysis, n.d.).
3. Data Sources
3.1. Overview of Health Effect Data
We relied on combinations of available data from distinct sources (e.g., epidemiologic analyses, surveillance data and online reports, published incidence rates, and census‐derived population counts) to estimate health effect incidence (mortality and morbidity) for each case study. In some cases, several health impact studies were conducted on a single case study event (e.g., Hurricane Sandy); we combined nonoverlapping incidence data to more broadly characterize health impacts and associated costs.
3.2. Case Study Information
Below, we describe each of the case studies in detail. For each event, we identify links to climatic conditions and the data sources utilized to estimate morbidity and mortality in each state.
3.2.1. Lyme Disease in Michigan
A changing climate can affect the distribution of infectious diseases including vector‐borne diseases that rely on a nonhuman host for transmission (Beard et al., 2016). Lyme disease is a vector‐borne illness transmitted to humans by infected blacklegged ticks and is the most common tick‐borne disease in the U.S. (Frazier & Douce, 2017). Although rarely fatal, the disease is associated with a number of symptoms, including a skin rash, fever, headache, and fatigue (Ray et al., 2013). A number of nonclimatic factors are linked to increasing incidence of Lyme disease in the U.S. over the past decade (including changes in tick ecology and disease surveillance), but warmer climates have also contributed to an expansion of tick habitat in the U.S. (Monaghan et al., 2015; Ogden et al., 2014).
We estimated the health‐related costs of the total Lyme disease burden in the state of Michigan through treated cases, apportioned to cause‐specific health outcomes consistent with aggregate U.S. Centers for Disease Control and Prevention (CDC) historical data (U.S. Centers for Disease Control and Prevention, 2018a), see supporting information Table S1. CDC does not currently designate Michigan as a high‐incidence state (Schwartz, 2017), but it neighbors high‐incidence states. Moreover, Lyme disease incidence in Michigan increased by a factor of more than 5 between 2000 and 2014, in tandem with an expansion of the tick population (Lantos et al., 2017; U.S. Centers for Disease Control and Prevention, 2018a).
3.2.2. Allergenic Oak Pollen in North Carolina
Allergenic pollen levels are affected by climate, because warmer weather, higher humidity, and heightened levels of carbon dioxide in the atmosphere can stimulate the growth of certain plant species and can extend pollen production season (Neumann et al., 2018; Reid & Gamble, 2009; Sapkota et al., 2019; L. Ziska et al., 2011; L. H. Ziska et al., 2019). Higher pollen levels from specific trees, grasses, and weeds are associated with asthma exacerbations (Sun et al., 2016). We calculated health‐related costs using results from Anenberg et al. (2017), which analyzed national oak tree pollen data for 1994–2010. We estimated total oak pollen‐attributable asthma EDs in North Carolina by applying the southeastern regional incidence rate from that study and 2012 state population data (U.S. Census Bureau, n.d.‐a). To adjust the long‐term average incidence rate for 2012 oak pollen conditions, we linearly scaled the estimate using 2010 and 2012 Wake County oak pollen data published by Sun et al. (2016), which found a significant association between tree pollen levels and asthma ED visits for an analysis spanning 2006–2012 (Sun et al., 2016). We imputed asthma‐related deaths from the ED data (see supporting information Table S1).
3.2.3. Extreme Weather in Ohio
Flooding frequency from heavy precipitation events is expected to increase because of climate change, and heavy precipitation events have increased in both intensity and frequency over the past century (Papalexiou & Montanari, 2019; Rahmstorf & Coumou, 2011; Wuebbles et al., 2017). This effect is important because flooding is already the most common global disaster and the most costly type of disaster in the U.S. (Alderman et al., 2012; Pew Charitable Trusts, 2017).
Brokamp et al. (2017) analyzed the impacts of extreme precipitation events on water infrastructure and human health in Ohio from 2010 to 2014 (Brokamp et al., 2017). Combined sewer systems, which collect sewage and industrial wastewater along with storm water runoff, are the focus of their analysis. Such systems are vulnerable to extreme precipitation events because the systems are designed to release excess flows of untreated wastewater into surface water bodies. These discharges (combined sewer overflows, CSOs) pose risks for human health, including gastrointestinal illness and skin infections from direct exposure to contaminated water and asthma exacerbations due to aerosolized lung irritants and other pathogens (Jagai et al., 2015; Levy et al., 2016; Patz et al., 2014; U.S. Environmental Protection Agency, 1996). For the 2012 health‐related cost analysis, we extracted CSO‐attributable HA data from the overall CSO analysis (Brokamp et al., 2017) and waterborne disease data from CDC (Beer et al., 2015). For flooding‐ and storm‐related mortality data, we relied on data reported to NOAA (U.S. National Oceanic and Atmospheric Administration, n.d.‐b) and to Ohio's Emergency Operations Center for the 29 June storm event (see supporting information Table S1; State of Ohio Emergency Operations Center, 2012).
3.2.4. Extreme Heat in Wisconsin
Extreme heat exposures represent a key climate‐sensitive public health threat as the leading cause of weather‐related mortality in the U.S. over the last 30 years (Luber & McGeehin, 2008; U.S. Centers for Disease Control and Prevention, 2016). In the midwestern U.S., research suggests that climate‐driven heat‐health impacts will grow (Limaye et al., 2018; Lo et al., 2019); national EDs for hyperthermia could triple by 2050 due to climate change (Lay et al., 2018) because of stronger, longer, and more frequent extreme heat events (Greene et al., 2011; Huang et al., 2007; Luber & McGeehin, 2008).
In July 2012, Wisconsin residents experienced record high temperatures over a span of 1 week, causing elevated levels of heat stress, heat stroke, and heat exhaustion (Christenson et al., 2013). Several century‐old daily record maximum temperatures and record high minimum temperatures were tied or broken during this heat wave (U.S. National Oceanic and Atmospheric Administration & U.S. National Oceanic and Atmospheric Administration, n.d.). Extreme July 2012 U.S. temperatures were found to be more consistent with current climate forcing conditions than in a preindustrial forcing scenario (Diffenbaugh & Scherer, 2013). Using heat stress health outcome data collected by Wisconsin's Environmental Public Health Tracking program (Christenson et al., 2013; U.S. Centers for Disease Control and Prevention, n.d.), we imputed HA visits and costs from ED incidence and estimated the total health‐related costs associated with 2012 extreme heat statewide (see supporting information Table S1).
3.2.5. Harmful Algal Blooms in Florida
Higher sea surface temperatures and more acidic seawater, conditions related to climate change, promote the growth of toxic harmful algal blooms (HABs; E. J. Kim, 2016; Moore et al., 2008; Riebesell et al., 2018). These events pose significant risks to human health (particularly respiratory, digestive system, and neurologic effects) because of the range of compounds (toxic and nontoxic) released by certain algae species, which can bioaccumulate in fish and shellfish and cause illness or death in humans (Fleming et al., 2011; Kirkpatrick et al., 2010). Algal blooms are also important threats to coastal fisheries, recreation, and tourism (Hoagland et al., 2014; Larkin & Adams, 2007). The 2012 HAB season in Florida was significant, with intense blooms that persisted from September 2012 into early 2013 (Weisberg et al., 2016). While the degree of climate attribution for the 2012 event has not been quantified, HAB prevalence is expected to increase in the future due to climate change (Hilborn et al., 2014).
We incorporated a recent analysis of the impacts of HABs on morbidity in six Florida counties by Hoagland et al. (2014) and extrapolated HA and ED incidence from that analysis using the published exposure‐response relationship (Hoagland et al., 2014) and 2012 monitoring data for the implicated red tide marine alga (Karenia brevis) from NOAA monitoring documented in the Harmful Algal Blooms Observing System (see supporting information Table S1; U.S. National Oceanic and Atmospheric Administration, n.d.‐a).
3.2.6. Ambient Ozone Air Pollution in Nevada
During the summer of 2012, the state of Nevada experienced some of its then‐hottest and driest weather to date (Hoerling et al., 2013; U.S. National Oceanic and Atmospheric Administration, 2013c), including two heat wave events lasting an average of 5 days each (Bandala et al., 2019). Ozone air pollution (smog) concentrations in the state exceeded the National Ambient Air Quality Standards for monitoring in 2011–2013 according to an analysis by the American Thoracic Society and the Marron Institute (Cromar et al., 2016). Climate change is expected to exacerbate ambient levels of ground‐level ozone because of the temperature‐dependent chemical mechanism of pollution formation in the troposphere (E. J. Kim, 2016). Climate change‐driven warmer temperatures also affect air pollution from fine particles (PM2.5) through direct (Achakulwisut et al., 2019; Mickley, 2004) and indirect mechanisms (Abel et al., 2018); we focus on ozone as a climate‐sensitive air pollutant projected to remain problematic nationally (Fann et al., 2015; Jacob & Winner, 2009; Knowlton et al., 2004; Wu et al., 2008).
We applied state‐specific annual estimates of deaths and cause‐specific morbidity in Nevada due to ozone exposures exceeding the American Thoracic Society‐recommended 8‐hr concentration of 60 parts per billion (ppb; Cromar et al., 2016), as analyzed using the U.S. Environmental Protection Agency Benefits Mapping and Analysis (BenMAP) program (U.S. Environmental Protection Agency, 2017). This level is lower than the corresponding National Ambient Air Quality Standards (70 ppb; U.S. Environmental Protection Agency, 2016) but a threshold at which evidence indicates that significant adverse health impacts are still experienced (Balmes, 2017). For morbidity estimates, we apportioned incidence (asthma, chronic lung disease, and other respiratory problems) using ratios published in a national estimate of ozone impacts on human health (Fann et al., 2012).
3.2.7. West Nile Virus in Texas
During the summer of 2012, the U.S. experienced an unexpected resurgence in the incidence of WNV, a mosquito‐borne disease that first emerged in the country in 1999 and had last peaked in 2003 (Beasley et al., 2013). WNV symptoms include headache, body aches, joint pains, vomiting, diarrhea, or rash; because of its reliance on a mosquito vector, the transmission of WNV is sensitive to both genetic factors and environmental conditions (Poh et al., 2019). An analysis of the 2012 outbreak indicates that environmental factors were key (Nasci et al., 2013). Specifically, elevated case counts during the 2012 WNV outbreak in Texas were attributed to drought, which created stagnant water pools, and elevated temperatures (2 °F warmer than the 2002–2011 average; Nasci et al., 2013), which shorten the extrinsic incubation period of mosquitoes (Roehr, 2012).
Although human cases were reported in each of the 48 contiguous U.S. states, Texas suffered the highest number of WNV deaths nationally (89 of 286 total), with cases concentrated in the Dallas‐Fort Worth Area (Yango et al., 2014). The first treated case of that year in Texas was reported on 25 May and the first death on 5 July. We imputed statewide HA and ED incidence from Dallas County public health morbidity surveillance data (Chung et al., 2013) for residents diagnosed from 30 May to 3 December 2012 and CDC surveillance data on total statewide case counts and used CDC surveillance data for statewide mortality (see supporting information Table S1; U.S. Centers for Disease Control and Prevention, 2013).
3.2.8. Wildfires in Colorado and Washington
Climate change increases the likelihood of more wildfires and longer fire seasons in the U.S. through warmer temperatures, changes in seasonal rainfall patterns, and lower soil moisture (Abatzoglou & Williams, 2016; Liu et al., 2016). We analyzed health‐related costs for impacts of 2012 wildfires in Colorado and Washington documented in three peer‐reviewed studies (Alman et al., 2016; Fann et al., 2018; Gan et al., 2017) and mortality reports from the National Interagency Fire Center and a natural disaster risk management database (Munich RE NatCatSERVICE, 2017; U.S. National Interagency Fire Center, 2012). Fann et al. (2018) examined wildfire smoke‐attributable health impacts nationwide for 2008–2012, combining modeled fine particle (PM2.5) concentrations and a set of exposure response functions using the BenMAP model (U.S. Environmental Protection Agency, 2017).
Alman et al. (2016) and Gan et al. (2017) investigated respiratory and cardiovascular morbidity endpoints during the peak burning periods in each state (from 5 June to 6 July in Colorado and 1 July to 31 October in Washington). Morbidity data were collected by the Colorado and Washington state health agencies for major respiratory ailments (asthma, upper respiratory infection, pneumonia, bronchitis, and chronic obstructive pulmonary disease) and cardiovascular outcomes (e.g., acute myocardial infarction). Health impacts (morbidity and mortality) from wildfire smoke‐attributable PM2.5 exposures were estimated using these studies and 2012 state‐level incidence data from Fann et al. (2018). See supporting information Table S1 for a full listing of case counts.
3.2.9. Hurricane Sandy in New Jersey and New York
Hurricane Sandy struck the coastline of the northeastern U.S. on 29 October 2012, delivering up to 1 ft of rain within 2 days and causing power outages for more than 20 million customers for periods of days to weeks (Kunz et al., 2013). Evidence indicates that sea level rise due to climate change amplified the hurricane's storm surge impacts (N. Lin et al., 2012; U.S. National Oceanic and Atmospheric Administration, 2012; Sweet et al., 2013), and the economic losses associated with hurricanes are growing in ways consistent with the effects of climate change (Estrada et al., 2015). We included a range of health impacts in both New Jersey and New York states. Mortality data were reported by American Red Cross and federal researchers for domestic impacts (Casey‐Lockyer et al., 2013) and later in a systematic study that quantified deaths in the Caribbean and North America (Diakakis et al., 2015).
In our survey of the peer‐reviewed literature on the health impacts of Hurricane Sandy, we found several studies addressing the toll of the storm on human morbidity in terms of HAs and EDs. In New Jersey, impacts included myocardial infarction and stroke (Swerdel et al., 2014), type II diabetes ED visits (Velez‐Valle et al., 2016), kidney disease and dialysis (Kelman et al., 2015), injuries (Marshall et al., 2016, 2018), dehydration (Swerdel et al., 2016), and a combination of health effects observed in the elderly population (McQuade et al., 2018). The mental health consequences of hurricanes are also an increasingly studied health impact, and we incorporated estimates from a study of the elderly population (McQuade et al., 2018) and a cross‐sectional survey quantifying outpatient mental health treatment received for a shoreline community 6 months after the hurricane (Boscarino et al., 2013). One of the studies in New Jersey also reported data for New York, which was incorporated into our analysis (Kelman et al., 2015). Additional health outcomes quantified in the literature for New York included combined hospital visits for Sandy‐related health effects including carbon monoxide exposure (Schnall et al., 2017); pregnancy complications (Xiao et al., 2019); asthma, chronic obstructive pulmonary disease, cardiac chest pain, syncope, and urinary tract infections (Gotanda et al., 2015); dialysis (C. Lin et al., 2014); trauma, musculoskeletal problems, asthma, chronic obstructive pulmonary disease, and syncope (Lee et al., 2016); mental health outcomes including anxiety, substance abuse, and mood disorders (S. Lin et al., 2016); and diseases of the respiratory system (H. Kim et al., 2016). For mental health ED visits, we estimated incidence using the reported morbidity rate and 2012 census population counts for eight counties (see supporting information Table S1; U.S. Census Bureau, n.d.‐a).
3.3. Health‐Related Cost Data
Human mortality costs were based on a VSL approach, as implemented by the U.S. Environmental Protection Agency in regulatory impact analyses (U.S. Environmental Protection Agency, 2015). Each life lost was valued at $9.1 million in 2018 dollars, while a VSL range of $1.0–24.4 million was considered within sensitivity analyses (see supporting information Table S2 for detail on sensitivity methods and results).
Direct morbidity costs for each event include combined expenses from HAs and EDs (new in this analysis, apportioned to expected payers using HCUP data) and costs associated with outpatient visits, home health care costs, and prescribed medications (from MEPS; U.S. Agency for Healthcare Research and Quality, n.d.‐b). Using ratios from HCUP (including the number of ED visits to the number of deaths, HAs, and the number of HAs to outpatient visits and prescriptions; Hess et al., 2014; U.S. Agency for Healthcare Research and Quality, n.d.‐b), we estimated a comprehensive measure of health impacts (see dashed lines in Figure 2). For example, if we only had access to ED data for a certain event, we used the HCUP‐derived ratio of ED visits to HAs for a specific ICD code to extrapolate the number of HA visits and, using HCUP data for the ED‐identified ICD code, related outpatient costs. For a complete listing of ICD codes and directly measured and imputed deaths, EDs, and HAs, see supporting information Table S1.
4. Results
Our analysis yielded results for each climate‐sensitive case study event for both estimated morbidity and mortality incidence and health‐related costs. In Table 2, we identify the range of specific health outcomes identified in the case study data sources.
Table 2.
Health Impacts Included in 2012 Climate‐Sensitive Health Cost Valuation
| State | Case study | Health effects included in valuation |
|---|---|---|
| Michigan | Lyme disease | Arthritis, carditis, erythema migraines rash, facial palsy, meningitis, radiculoneuropathy |
| North Carolina | Extreme weather | Mortality, acute respiratory infection, asthma, gastrointestinal illness, skin and soft tissue infection |
| Ohio | Extreme heat | Mortality, exposure to excessive heat, heat cramps, heat edema, heat exhaustion, heat fatigue, stroke, heat syncope, Sun stroke |
| Wisconsin | Allergenic oak pollen | Mortality, asthma |
| Nevada | Ozone air pollution | Mortality, asthma, chronic lung disease, respiratory problems |
| Texas | West Nile virus | Mortality, acute flaccid paralysis, cranial nerve palsy, encephalitis, fever, meningitis |
| Colorado | Wildfires | Mortality, acute myocardial infarction, asthma, bronchitis, chronic obstructive pulmonary disease, pneumonia, respiratory disease, upper respiratory infection |
| Florida | Harmful algal blooms | Digestive system disease, respiratory disease |
| New Jersey | Hurricane Sandy | Mortality, acute upper respiratory illness, bronchitis, calculus of kidney and ureter, carbon monoxide exposure, contusion, cut/pierce injury, dehydration, dialysis, end‐stage renal disease, falls, fluid imbalance, fracture, functional digestive issue, mental illness, myocardial infarction, open wound, osteoarthritis, other injury, overexertion, sprain, stroke, struck by/against object (unintentional contact) injury, tree‐related injury, Type II diabetes |
| New York | Hurricane Sandy | Mortality, anxiety, carbon monoxide exposure, dialysis, electrolyte abnormality, end‐stage renal disease, external exposure, homelessness, hypertensive kidney disease, hypothermia, legionellosis, mental or mood disorder, myeloproliferative/neoplasm, nonfatal injury, psychosis, pulmonary fibrosis, respiratory problem, substance abuse, suicide counseling, threatened or spontaneous abortion, Type II diabetes, ventilator needed |
| Washington | Wildfires | Mortality, acute myocardial infarction, asthma, bronchitis, cerebrovascular disease, chronic obstructive pulmonary disease, pneumonia, respiratory disease, upper respiratory infection |
Note. For detailed incidence estimates, see Table S1 in the supporting information.
Table 3 summarizes the estimated health impact incidence by case study, in terms of estimated event‐associated mortality and morbidity (HAs and EDs). Cumulatively, the case studies considered encompassed an estimated 917 premature deaths, 20,568 HAs, 17,857 EDs, and 37,425 outpatient encounters (comprised of outpatient visits, home health care visits, and instances in which medications were prescribed).
Table 3.
Estimated Health Impacts in 2012 Climate‐Sensitive Case Studies
| State | Case study | Duration of health effects considered | Mortality | HAs | EDs | Outpatient encounters |
|---|---|---|---|---|---|---|
| Michigan | Lyme disease | Whole year | 0 | 157 | 11 | 2,727 |
| North Carolina | Allergenic oak pollen | Whole year | 4 | 183 | 1,149 | 296 |
| Ohio | Extreme weather | Whole year | 8 | 37 | 343 | 52 |
| Wisconsin | Extreme heat | 16 June to 18 July | 27 | 155 | 1,620 | 57 |
| Nevada | Ozone air pollution | Whole year | 97 | 114 | 194 | 1,989 |
| Texas | West Nile virus | 30 May to 3 December | 89 | 1,628 | 2,680 | 28,303 |
| Colorado | Wildfires | Whole year | 174 | 256 | 1,432 | 35 |
| Florida | Harmful algal blooms | 1 September to 31 December | 0 | 11,066 | 3,857 | 1,473 |
| Washington | Wildfires | Whole year | 245 | 371 | 1,897 | 49 |
| New Jersey | Hurricane Sandy | 28 October to 30 November* | 273* | 5,795 | 2,247 | 2,145 |
| New York | 807 | 2,426 | 299 | |||
| Total | 917 | 20,568 | 17,857 | 37,425 | ||
Note. Outpatient encounters include outpatient visits, home health care visits, and incidents in which medications were prescribed. *Combined Hurricane Sandy mortality estimate for New Jersey and New York also includes deaths reported to CDC from Pennsylvania, West Virginia, Connecticut, Maryland, and deaths not classified by state, and event duration reflects time span for primary mortality data collection (Diakakis et al., 2015). Row and column totals may not equal component sums due to rounding.
Table 4 presents the health‐related costs associated with case study events (in millions of 2018 dollars) sequenced from least to greatest total health‐related costs. The total health‐related cost estimate is $10.0 billion (with a sensitivity analysis range of $2.7–24.6 billion), including impacts from morbidity and mortality. We found that mortality costs (i.e., the value of a statistical life) of $8.4 billion exceeded morbidity costs and lost wages ($1.6 billion combined). In this analysis, the highest absolute costs were associated with Hurricane Sandy ($3.1 billion), followed by wildfires in Washington ($2.3 billion).
Table 4.
Estimated Health‐Related Costs of 2012 Climate‐Sensitive Case Studies (Millions of 2018 Dollars)
| (A) State | (B) Case study | (C) Mortality costs | (D) Morbidity costs (HAs) | (E) Morbidity costs (EDs) | (F) Other health‐related costs (Outpatient, home health care, medications) | (G) Lost wages (HAs and EDs) |
(H) Total health‐related costs (Sensitivity range) |
|---|---|---|---|---|---|---|---|
| (Millions of 2018 dollars) | |||||||
| Michigan | Lyme disease | $0 | $4.5 | $0.3 | $3.0 | $0.1 | $8.0 |
| ($7.9–9.7) | |||||||
| North Carolina | Allergenic oak pollen | $36.5 | $4.3 | $0.6 | $0.9 | $0.7 | $43.0 |
| ($13.6–107.1) | |||||||
| Ohio | Extreme weather | $73.0 | $0.9 | $8.6 | $0.1 | $0.2 | $82.8 |
| ($21.8–208.8) | |||||||
| Wisconsin | Extreme heat | $246.4 | $1.3 | $3.1 | $0.5 | $0.6 | $251.8 |
| ($33.6–664.4) | |||||||
| Florida | Harmful algal blooms | $0 | $398.8 | $146.3 | $0.9 | $11.0 | $557.0 |
| ($236.7–557.0) | |||||||
| Nevada | Ozone air pollution | $886.9 | $4.6 | $4.6 | $1.6 | $0.2 | $897.9 |
| ($105.6–2,376.7) | |||||||
| Texas | West Nile virus | $812.1 | $91.0 | $151.9 | $31.4 | $4.9 | $1,091.3 |
| ($368.6–2,448.2) | |||||||
| Colorado | Wildfires | $1,587.2 | $5.6 | $16.9 | $0.0 | $0.9 | $1,610.5 |
| ($205.2–4,269.7) | |||||||
| Washington | Wildfires | $2,234.9 | $11.2 | $43.4 | $0.0 | $1.4 | $2,290.9 |
| ($311.9–6,035.0) | |||||||
| New Jersey | Hurricane Sandy | $2,490.9* | $439.5 | $80.2 | $17.8 | $6.2 | $3,145.8 |
| New York | $49.5 | $57.2 | $2.5 | $1.9 | ($1,431.3–7,922.4) | ||
| Total | $8,367.7 | $1,011.3 | $513.2 | $58.7 | $28.0 | $9,979.0 | |
| ($2,736.3–24,599.0) | |||||||
Note. Column H (total health‐related costs) equals sum of columns C‐G. Column H (sensitivity range) corresponds to sensitivity analysis (see supporting information Table S2). *Combined Hurricane Sandy mortality estimate for New Jersey and New York also includes deaths reported from Pennsylvania, West Virginia, Connecticut, Maryland, and those not classified by state (Diakakis et al., 2015). Row and column totals may not equal component sums due to rounding.
Figure 3 expands on the morbidity cost estimates presented in Table 4 by detailing the relative proportions of morbidity costs across all case studies (those associated with prescribed medications, home health visits, outpatient care, lost wages from HAs and ED visits, and direct HA and ED costs in each state).
Figure 3.
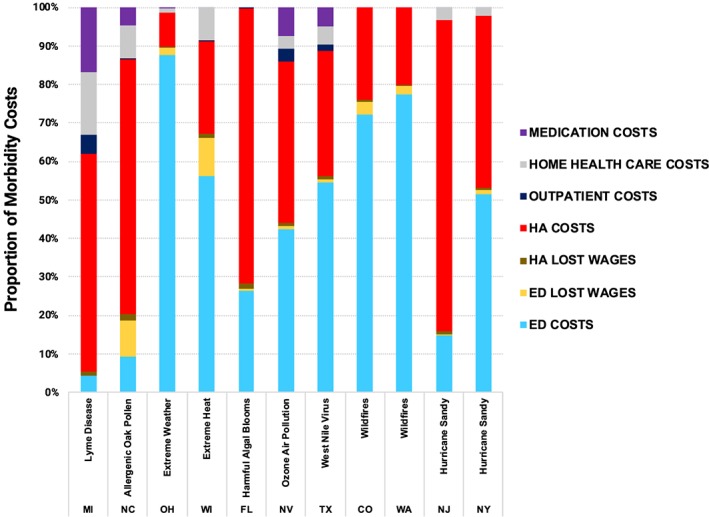
Relative proportions of total estimated morbidity costs for each case study event.
Table 5 stratifies state‐level morbidity costs from HAs and EDs (in millions of 2018 dollars) by expected payer, using HCUP data for primary diagnosis codes within each case study. Overall, Medicare accounts for the largest share of total expected morbidity costs for HAs and EDs, followed by private insurance and Medicaid. The share of expected costs apportioned to these expected payers varies by case study, along with the expected costs incurred by uninsured patients.
Table 5.
Expected Payers of Estimated Health‐Related Costs for Climate‐Sensitive Case Studies (Millions of 2018 Dollars)
| Expected payer from HAs, EDs, and other health‐related costs (outpatient, home health care, medications) | ||||||||
|---|---|---|---|---|---|---|---|---|
| (A) State | (B) Case study | (C) Medicare | (D) Medicaid | (E) Private insurance | (F) Uninsured | (G) Other | (H) Missing data | (I) Expected payer total |
| (Millions of 2018 dollars) | ||||||||
| Michigan | Lyme disease | $3.7 | $1.0 | $2.8 | $0.3 | $0.1 | $0.0 | $7.9 |
| North Carolina | Allergenic oak pollen | $1.6 | $2.1 | $1.4 | $0.6 | $0.1 | $0.0 | $5.8 |
| Ohio | Extreme weather | $1.5 | $3.7 | $2.4 | $1.6 | $0.4 | $0.0 | $9.6 |
| Wisconsin | Extreme heat | $0.9 | $0.7 | $1.7 | $1.0 | $0.6 | $0.0 | $4.9 |
| Florida | Harmful algal blooms | $278.0 | $124.9 | $84.6 | $41.1 | $17.3 | $0.0 | $546.0 |
| Nevada | Ozone air pollution | $2.4 | $3.8 | $2.5 | $1.7 | $0.4 | $0.0 | $10.8 |
| Texas | West Nile virus | $112.7 | $25.7 | $89.1 | $40.2 | $6.5 | $0.0 | $274.3 |
| Colorado | Wildfires | $9.5 | $4.1 | $6.6 | $1.3 | $1.1 | $0.0 | $22.5 |
| Washington | Wildfires | $26.8 | $7.8 | $16.4 | $2.7 | $0.9 | $0.0 | $54.6 |
| New Jersey | Hurricane Sandy | $286.4 | $37.2 | $163.0 | $46.1 | $4.7 | $0.0 | $537.5 |
| New York | $58.2 | $25.4 | $19.8 | $3.7 | $2.1 | $0.0 | $109.2 | |
| Total | $781.7 | $236.5 | $390.4 | $140.3 | $34.2 | $0.1 | $1,583.2 | |
Note. Costs estimated using expected payer HCUP data for primary diagnoses within each case study. Column H reflects missing expected payer data from HCUP. Column I (payer total) equals sum of columns C‐H. Row and column totals may not equal component sums due to rounding.
Costs for ED visits accounted for more than half of total morbidity costs in five of the case studies and were, by proportion of total morbidity costs, highest in Ohio and Washington. The proportional costs of HAs, in contrast, were relatively highest in New Jersey, North Carolina, Florida, and Michigan. The relative proportional costs of medical care were somewhat different in the two Hurricane Sandy states, with HA costs higher in New Jersey and ED costs higher in New York, based on available data.
Comparisons of documented health effects at the state‐level to the corresponding national datasets for 2012 (total Lyme disease cases, allergenic oak pollen‐attributable EDs, and mortality for all other exposures) indicate that the health impacts and related costs studied here are just a fraction of the reported 2012 national burden (Figure 4, see supporting information Table S3 for calculations).
Figure 4.
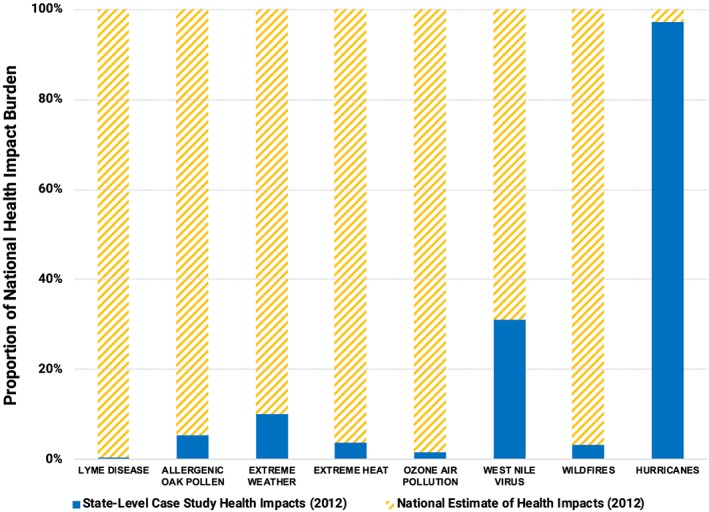
Climate‐sensitive health impacts (total Lyme disease cases, allergenic oak pollen‐attributable EDs, and mortality for all other exposures) included in 2012 state‐level health cost valuation, compared to estimates of the corresponding national annual health impact burden.
For 2012 hurricanes, we estimate that our analysis captured about 97% of total mortality (U.S. National Oceanic and Atmospheric Administration, 2013a). However, the other case studies constitute smaller portions of the 2012 national burden: 31% of mortality recorded for WNV (Poh et al., 2019; U.S. Centers for Disease Control and Prevention, 2013), 10% of extreme weather mortality from thunderstorms and floods (U.S. National Oceanic and Atmospheric Administration, 2016), 5% of allergenic oak pollen EDs, 4% of heat‐related mortality (U.S. Centers for Disease Control and Prevention, n.d.), 3% of smoke‐related wildfire mortality (Fann et al., 2018), 2% of estimated ozone‐related mortality (Cromar et al., 2016), and 0.4% of reported Lyme disease cases (Schwartz, 2017; U.S. Centers for Disease Control and Prevention, 2018b). No national estimates of HAB‐associated health effects were available for 2012.
5. Conclusions
The 10 case studies we analyzed illustrate that climate‐sensitive events impose significant health costs on the United States. While mortality costs ($8.4 billion) dominated, the economic burden of morbidity and lost wages ($1.6 billion combined) is an important and underreported dimension of the overall economic impact of such events. Tables 3 and 4 show that health impacts and costs differed depending on the location, type, duration, and geographic extent of the event.
Our estimated health‐related costs are broadly consistent with other studies investigating different aspects of the national economic impacts of climate‐sensitive events (Balbus et al., 2014; Martinich & Crimmins, 2019). The health‐related costs estimated here are of similar magnitude as the $14.1 billion estimated in the prior analysis encompassing six events from 2000 to 2009, though differing geographies and time horizons preclude a direct cost comparison (Knowlton et al., 2011). At the state level, the estimated morbidity‐related costs of the Texas WNV outbreak ($274.3 million) are consistent with Murray et al. (2013), which reported costs of $15.9–154.2 million (2018 dollars) for acute medical care, outpatient costs, and lost productivity for just 1,028 HAs and EDs (rather than our estimate of 4,308 HAs and EDs; Barber et al., 2010; Murray et al., 2013). Lay et al. (2018) used MEPS data to calculate the economic impact of ED visits for hyperthermia. Using the cost‐per‐ED visit estimate from that study, the Wisconsin ED visits would have cost $2.9 million, compared to our $3.1 million estimate (2018 dollars). Recent studies quantified the national burden of Lyme disease at $786 million to $1.3 billion annually (Adrion et al., 2015; Mac et al., 2019); our estimate for Michigan ($8.0 million) reflects the burden of a single, low‐incidence state. For allergenic oak pollen, our estimate of ED costs in North Carolina ($0.6 million) is consistent with a comparable national estimate ($12.2 million in 2018 dollars; Anenberg et al., 2017). Wildfire impacts in Colorado ($1.6 billion) and Washington ($2.3 billion) correspond with the national economic valuation estimates reported in Fann et al. (2018).
Mortality costs estimated through VSL methods are borne by society as a whole; morbidity costs (Figure 3 and Tables 4 and 5) represent costs borne by individuals, insurance companies, and taxpayer‐funded government health insurance programs (e.g., Medicare and Medicaid). There are substantial differences in expected payers for medical care across these events, due to differences in state demographics and health outcomes across age and income groups. For example, hospital visits for asthma care are more common for children, especially those in low‐income families (Akinbami & Schoendorf, 2002; Moorman et al., 2012), hence the high burden to Medicaid for asthma in North Carolina. Conditions more likely to harm older adults, such as hurricanes and wildfires (Alman et al., 2016; McQuade et al., 2018), have a high burden for Medicare. More than 20% of Florida's population is 65 years or older, so any event there is likely to pose a burden for Medicare (U.S. Census Bureau, n.d.‐b). Overall, about half of the morbidity‐related costs of the events studied were estimated to have been paid for by Medicare (Table 5), despite the fact that Medicare insured only about 16% of Americans in 2012 (Henry J. Kaiser Family Foundation, 2019). The disproportionate share of health‐related costs expected to be paid by Medicare indicates that the health of older adults is highly affected by climate‐sensitive events and further signals the need for targeted health efforts for this vulnerable group (U.S. Global Change Research Program, 2018).
Several limitations impacted our health‐related cost estimates. Despite record‐setting weather conditions across the U.S. in 2012, our analysis was restricted to case studies for which there was adequate documentation of health impacts. We only quantified mental health impacts for Hurricane Sandy, even though other events like wildfires have been shown to adversely affect mental health (Afifi et al., 2012; Reid et al., 2016). In the cases of extreme heat and Lyme disease, routine underreporting of health effects (Luber & McGeehin, 2008; U.S. Centers for Disease Control and Prevention, 2019) could bias estimates downward. Extreme heat can affect cardiovascular and respiratory health (Gronlund et al., 2018; Mora et al., 2017), but these impacts are not included in our analysis. Wildfire impacts were characterized only for PM2.5 exposures, not for wildfire‐linked ozone air pollution (Baker et al., 2016; Wilkins et al., 2018). Other effects on well‐being, such as the toll of displacement and uncertainty stemming from adverse exposures, are difficult to quantify but nonetheless important (Afifi et al., 2012; Berry et al., 2018; Tschakert et al., 2019). As such, the $10.0 billion total we calculated is likely a conservative estimate of the health‐related costs for these case studies.
Our health‐related cost analysis applied HCUP and MEPS data (Figure 2), but at times the precise ICD diagnosis code of health impacts was not made available, or multiple ICD codes were tagged to a single patient, which could bias results upward. Furthermore, we aimed for a conservative approach to health incidence estimates, but reconciling health impact estimates across a patchwork of data sources varying in level of detail and quality was necessarily subjective. Actual lost wages may have exceeded our estimates, in cases when patients missed time from work or other activities after hospital discharge. Expected payer statistics in HCUP are annual ICD‐specific totals, so we were not able to access precise expected payer information linked to the case study exposures. Therefore, our analysis lacks precision in isolating the health endpoints that accounted for morbidity costs and the presumed payer burden.
Beyond these case studies and the specific health impacts identified in Table 2, the U.S. also experienced other significant climate‐sensitive events in 2012 such as drought that affected more than half of the states (Hoerling et al., 2013; Rippey, 2015; U.S. National Oceanic and Atmospheric Administration, 2013a). Drought conditions have been linked with health risks including respiratory illness, mental health issues, and heat stress (Achakulwisut et al., 2019; Hayes et al., 2018; OBrien et al., 2014; Stanke et al., 2013; Vins et al., 2015). Two months before Hurricane Sandy, Hurricane Isaac made landfall over Louisiana, its large storm surge triggering flooding and causing nine deaths (U.S. National Oceanic and Atmospheric Administration, 2013a). Wildfires in 2012 burned 9.2 million acres in total, and caused six immediate deaths outside of Colorado and Washington (U.S. National Oceanic and Atmospheric Administration, 2013a).
Since 2012, many additional weather records have been set across the country (U.S. Global Change Research Program, 2018; U.S. National Oceanic and Atmospheric Administration, 2018). Recently, the U.S. has faced dramatic climate‐sensitive health episodes, including devastating hurricanes (Santos‐Burgoa et al., 2018; van Oldenborgh et al., 2017) and 2018 wildfires in California that were the largest, costliest, and deadliest in the state's history (Smith, 2019). Nationally, ozone levels remain high and climate change threatens to overwhelm historical air quality improvements (American Lung Association, 2019; Cromar et al., 2019). While NOAA tabulated 11 disasters each resulting in at least $1 billion in property and/or infrastructure damages in 2012, the Federal Emergency Management Agency declared a total of 112 disasters that year (Federal Emergency Management Agency, n.d.) and the number of annual billion dollar disasters was exceeded in 2016 (15), 2017 (16), and 2018 (14)—with these years accumulating totals more than double the long‐term average (Smith, 2019; U.S. National Oceanic and Atmospheric Administration, 2019). Therefore, the climate‐sensitive impacts we examined could signal hundreds of billions of dollars in health‐related costs from recent and future exposures nationwide (Figure 4), in line with recent analyses (Martinich & Crimmins, 2019; U.S. Global Change Research Program, 2018).
The impacts of climate change on health are becoming more widely studied, yet the quantification of climate‐sensitive health‐related costs remains limited, in part because of insufficient surveillance and the data linkages necessary to characterize HAs, EDs, and deaths (see Tables 1 and 2). Recent events, such as Hurricane Maria in 2017, have also shown that our collective understanding of such events improves over time—sometimes illuminating health impacts that are significantly higher than initial reports (Kishore et al., 2018; Rappaport & Blanchard, 2016; Santos‐Burgoa et al., 2018). The evidence that does exist suggests that health‐related costs associated with climate‐sensitive events are significant in the context of other damages inflicted by hazardous weather. For example, a NOAA compilation of 2012 damages to property and crops estimated a toll of $38.9 billion nationally (U.S. National Oceanic and Atmospheric Administration, 2016); our estimate of health‐related costs from 10 case study events suggests that the 2012 national economic burden of all extreme weather was, at a minimum, 26% (sensitivity range 7–63%) higher when health‐related costs are considered.
The high health‐related costs associated with climate‐sensitive events highlight the importance of actions to slow the acceleration of climate change and adapt to its unavoidable impacts (U.S. Global Change Research Program, 2018). Prior estimates indicate that global annual climate adaptation costs for the health sector could cost $2–10.7 billion, though the upper limit of this range is likely higher due to the limited documented range of health and economic impacts and the costs of health‐relevant actions in other sectors (Hutton, 2011; Intergovernmental Panel on Climate Change, 2018). Because only a fraction of these interventions would take place in the US, our analysis (and the likelihood of nonlinear increases in future climate change impacts and costs; Intergovernmental Panel on Climate Change, 2018) demonstrates that the health‐related costs of climate‐sensitive events may outweigh the costs of mitigation and adaptation actions that could help society avoid climate‐related triggers of disease and early death (U.S. Environmental Protection Agency, 2019). Estimating the ratio of health‐related benefits to costs is beyond the scope of this study; elsewhere, it has been posited that every dollar spent on preparing for future climate risks saves 6 times as much in avoided infrastructure repair costs (National Institute of Building Sciences, 2017).
The health‐related costs of climate‐sensitive environmental exposures in the U.S. are substantial. By combining estimates of health impacts and the costs of medical treatment for 10 climate‐sensitive case study events that occurred in 2012, we demonstrate multibillion‐dollar economic ramifications within the health sector (Smith & Katz, 2013). Despite the magnitude of costs described in this study, the major economic impacts of climate change on human health are seldom adequately included in measures such as the social cost of carbon, which have a major bearing on the direction of future climate policy. Ambitious actions to mitigate climate change and adapt to its unavoidable impacts can help to avoid unprecedented human suffering and major health‐related costs.
Conflict of Interest
The authors declare no conflicts of interest relevant to this study.
Supporting information
Supporting Information S1
Acknowledgments
Underlying incidence data are available in the supporting information. We thank the authors of the health impact research studies and state public health staff who provided input on case studies and acknowledge the environmental health and health cost databases utilized in this study. We also thank Tina Swanson, Leslie Jones, Kelsey Kane‐Ritsch, Susan Keane, Yukyan Lam, Rob Moore, Joel Scata, and Anna Weber for their reviews of prior manuscript drafts. We acknowledge the artists whose symbols were adapted in Figure 1 under a Creative Commons license: Marco Hernandez (Lyme disease), Corpus Delecti (allergenic oak pollen), Yazmin Alanis (extreme weather), Adrien Coquet (extreme heat), Gemma Evans (harmful algal blooms and ozone air pollution), Yanti Anis (West Nile virus), Tuong Tam (wildfires), and Kirby Wu (hurricane). We also thank the anonymous reviewers whose comments have greatly improved this manuscript. All authors jointly conceived the study approach, conceptual framing, and methods. K. K., J. C., and W. M. consulted with V. L. as he led the analysis. V. L. conducted the literature review, completed data analysis, and led preparation and revision of the manuscript; W. M. directly contributed in drafting the Discussion with V. L.; K. K., J. C., and W. M. reviewed findings, edited and revised the entire manuscript, and approved the final version.
Limaye, V. S. , Max, W. , Constible, J. , & Knowlton, K. (2019). Estimating the health‐related costs of 10 climate‐sensitive U.S. events during 2012. GeoHealth, 3, 245–265. 10.1029/2019GH000202
References
- Abatzoglou, J. T. , & Williams, A. P. (2016). Impact of anthropogenic climate change on wildfire across western U.S. forests. Proceedings of the National Academy of Sciences, 113(42), 11770–11775. 10.1073/pnas.1607171113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abel, D. W. , Holloway, T. , Harkey, M. , Meier, P. , Ahl, D. , Limaye, V. S. , & Patz, J. A. (2018). Air‐quality‐related health impacts from climate change and from adaptation of cooling demand for buildings in the eastern United States: An interdisciplinary modeling study. PLoS Medicine, 15(7), e1002599 10.1371/journal.pmed.1002599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achakulwisut, P. , Anenberg, S. C. , Neumann, J. E. , Penn, S. L. , Weiss, N. , Crimmins, A. , Fann, N. , Martinich, J. , Roman, H. , & Mickley, L. J. (2019). Effects of increasing aridity on ambient dust and public health in the U.S. Southwest under climate change. GeoHealth, 3, 127–144. 10.1029/2019GH000187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adrion, E. R. , Aucott, J. , Lemke, K. W. , & Weiner, J. P. (2015). Health care costs, utilization and patterns of care following Lyme disease. PLoS ONE, 10(2), e0116767 10.1371/journal.pone.0116767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afifi, W. A. , Felix, E. D. , & Afifi, T. D. (2012). The impact of uncertainty and communal coping on mental health following natural disasters. Anxiety, Stress, and Coping, 25(3), 329–347. 10.1080/10615806.2011.603048 [DOI] [PubMed] [Google Scholar]
- Akinbami, L. J. , & Schoendorf, K. C. (2002). Trends in childhood asthma: Prevalence, health care utilization, and mortality. Pediatrics‐English Edition, 110(2), 315–322. [DOI] [PubMed] [Google Scholar]
- Alderman, K. , Turner, L. R. , & Tong, S. (2012). Floods and human health: A systematic review. Environment International, 47, 37–47. 10.1016/j.envint.2012.06.003 [DOI] [PubMed] [Google Scholar]
- Alman, B. L. , Pfister, G. , Hao, H. , Stowell, J. , Hu, X. , Liu, Y. , & Strickland, M. J. (2016). The association of wildfire smoke with respiratory and cardiovascular emergency department visits in Colorado in 2012: A case crossover study. Environmental Health, 15(1). 10.1186/s12940-016-0146-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Lung Association . (2019). State of the Air 2019 (Key Findings). Retrieved from https://www.lung.org/our-initiatives/healthy-air/sota/key-findings/
- Anenberg, S. C. , Weinberger, K. R. , Roman, H. , Neumann, J. E. , Crimmins, A. , Fann, N. , Martinich, J. , & Kinney, P. L. (2017). Impacts of oak pollen on allergic asthma in the United States and potential influence of future climate change: Climate Impacts on Oak Pollen and Health. GeoHealth, 1, 80–92. 10.1002/2017GH000055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker, K. R. , Woody, M. C. , Tonnesen, G. S. , Hutzell, W. , Pye, H. O. T. , Beaver, M. R. , Pouliot, G. , & Pierce, T. (2016). Contribution of regional‐scale fire events to ozone and PM2.5 air quality estimated by photochemical modeling approaches. Atmospheric Environment, 140, 539–554. 10.1016/j.atmosenv.2016.06.032 [DOI] [Google Scholar]
- Balbus, J. M. , Greenblatt, J. B. , Chari, R. , Millstein, D. , & Ebi, K. L. (2014). A wedge‐based approach to estimating health co‐benefits of climate change mitigation activities in the United States. Climatic Change, 127(2), 199–210. 10.1007/s10584-014-1262-5 [DOI] [Google Scholar]
- Balmes, J. R. (2017). EPA's new ozone air quality standard: Why should we care? Annals of the American Thoracic Society, 14(11), 1627–1629. 10.1513/AnnalsATS.201707-557EH [DOI] [PubMed] [Google Scholar]
- Bandala, E. R. , Kebede, K. , Jonsson, N. , Murray, R. , Green, D. , Mejia, J. F. , & Martinez‐Austria, P. F. (2019). Extreme heat and mortality rates in Las Vegas, Nevada: Inter‐annual variations and thresholds. International journal of Environmental Science and Technology. 10.1007/s13762-019-02357-9 [DOI] [Google Scholar]
- Barber, L. M. , Schleier, J. J. III , & Peterson, R. K. (2010). Economic cost analysis of West Nile virus outbreak, Sacramento County, California, USA, 2005. Emerging Infectious Diseases, 16(3), 480–486. 10.3201/eid1603.090667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard, C. B. , Eisen, R. J. , Barker, C. M. , Garofalo, J. F. , Hahn, M. , Hayden, M. , Monaghan, A. J. , Ogden, N. H. , & Schramm, P. J. (2016). Ch. 5: Vectorborne Diseases. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. U.S. Global Change Research Program (pp. 129–156). Washington, DC: US Global Change Research Program; Retrieved from https://health2016.globalchange.gov/vectorborne-diseases, 10.7930/J0765C7V [DOI] [Google Scholar]
- Beasley, D. W. C. , Barrett, A. D. T. , & Tesh, R. B. (2013). Resurgence of West Nile neurologic disease in the United States in 2012: What happened? What needs to be done? Antiviral Research, 99(1), 1–5. 10.1016/j.antiviral.2013.04.015 [DOI] [PubMed] [Google Scholar]
- Beer, K. D. , Gargano, J. W. , Roberts, V. A. , Hill, V. R. , Garrison, L. E. , Kutty, P. K. , Hilborn, E. D. , Wade, T. J. , Fullerton, K. E. , & Yoder, J. S. (2015). Surveillance for waterborne disease outbreaks associated with drinking water—United States, 2011–2012. MMWR. Morbidity and Mortality Weekly Report, 64(31), 842–848. 10.15585/mmwr.mm6431a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belova, A. , Mills, D. , Hall, R. , Juliana, A. S. , Crimmins, A. , Barker, C. , & Jones, R. (2017). Impacts of increasing temperature on the future incidence of West Nile neuroinvasive disease in the United States. American Journal of Climate Change, 06(01), 166–216. 10.4236/ajcc.2017.61010 [DOI] [Google Scholar]
- Berry, H. L. , Waite, T. D. , Dear, K. B. G. , Capon, A. G. , & Murray, V. (2018). The case for systems thinking about climate change and mental health. Nature Climate Change, 8(4), 282–290. 10.1038/s41558-018-0102-4 [DOI] [Google Scholar]
- Bierbaum, R. , Smith, J. B. , Lee, A. , Blair, M. , Carter, L. , Chapin, F. S. , Fleming, P. , Ruffo, S. , Stults, M. , McNeeley, S. , Wasley, E. , & Verduzco, L. (2013). A comprehensive review of climate adaptation in the United States: More than before, but less than needed. Mitigation and Adaptation Strategies for Global Change, 18(3), 361–406. 10.1007/s11027-012-9423-1 [DOI] [Google Scholar]
- Boscarino, J. A. , Hoffman, S. N. , Kirchner, H. L. , Erlich, P. M. , Adams, R. E. , Figley, C. R. , & Solhkhah, R. (2013). Mental health outcomes at the Jersey Shore after Hurricane Sandy. International Journal of Emergency Mental Health, 15(3), 147–158. [PubMed] [Google Scholar]
- Bouwer, L. M. (2011). Have disaster losses increased due to anthropogenic climate change? Bulletin of the American Meteorological Society, 92(1), 39–46. 10.1175/2010BAMS3092.1 [DOI] [Google Scholar]
- Brokamp, C. , Beck, A. F. , Muglia, L. , & Ryan, P. (2017). Combined sewer overflow events and childhood emergency department visits: A case‐crossover study. Science of the Total Environment, 607‐608, 1180–1187. 10.1016/j.scitotenv.2017.07.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, L. (2016). Preparing for the public health challenges of climate change: Perspectives from local public health. Journal of Public Health Management and Practice, 22(1), 102–104. 10.1097/PHH.0000000000000356 [DOI] [PubMed] [Google Scholar]
- Carr, J. L. , Sheffield, P. E. , & Kinney, P. L. (2012). Local preparedness for climate change among local health department officials in New York State: A comparison with national survey results. Journal of Public Health Management and Practice: JPHMP, 18(2), E24–E32. 10.1097/PHH.0b013e31823dea74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvour, M. L. , Hughes, A. E. , Fann, N. , & Haley, R. W. (2018). Estimating the health and economic impacts of changes in local air quality. American Journal of Public Health, 108(S2), S151–S157. 10.2105/AJPH.2017.304252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey‐Lockyer, M. , Heick, R. J. , Mertzlufft, C. E. , Yard, E. E. , Wolkin, A. F. , Noe, R. S. , & Murti, M. (2013). Deaths associated with Hurricane Sandy—October–November 2012. MMWR. Morbidity and Mortality Weekly Report, 62(20), 393–397. [PMC free article] [PubMed] [Google Scholar]
- Christenson, M. L. , Geiger, S. D. , & Anderson, H. A. (2013). Heat‐related fatalities in Wisconsin during the summer of 2012. Wisconsin Medical Journal, 112(5), 6. [PubMed] [Google Scholar]
- Christidis, N. , Stott, P. A. , & Brown, S. J. (2011). The role of human activity in the recent warming of extremely warm daytime temperatures. Journal of Climate, 24(7), 1922–1930. 10.1175/2011JCLI4150.1 [DOI] [Google Scholar]
- Chung, W. M. , Buseman, C. M. , Joyner, S. N. , Hughes, S. M. , Fomby, T. B. , Luby, J. P. , & Haley, R. W. (2013). The 2012 West Nile encephalitis epidemic in Dallas, Texas. JAMA, 310(3), 297–307. 10.1001/jama.2013.8267 [DOI] [PubMed] [Google Scholar]
- Climate Central . (2012). 2012 Record temperatures: Which states led the nation. Retrieved June 26, 2019, from https://www.climatecentral.org/news/2012-record-temperatures-which-states-led-the-nation-14951
- Cromar, K. R. , Gladson, L. A. , & Ewart, G. (2019). Trends in excess morbidity and mortality associated with air pollution above ATS—Recommended standards, 2008 to 2017. Annals of the American Thoracic Society, 16(7), 836–845. 10.1513/AnnalsATS.201812-914OC [DOI] [PubMed] [Google Scholar]
- Cromar, K. R. , Gladson, L. A. , Perlmutt, L. D. , Ghazipura, M. , & Ewart, G. W. (2016). American Thoracic Society and Marron Institute Report. Estimated excess morbidity and mortality caused by air pollution above American Thoracic Society–Recommended standards, 2011–2013. Annals of the American Thoracic Society, 13(8), 1195–1201. 10.1513/AnnalsATS.201602-103AR [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diakakis, M. , Deligiannakis, G. , Katsetsiadou, K. , & Lekkas, E. (2015). Hurricane Sandy mortality in the Caribbean and continental North America. Disaster Prevention and Management: An International Journal, 24(1), 132–148. 10.1108/DPM-05-2014-0082 [DOI] [Google Scholar]
- Diaz, D. , & Moore, F. (2017). Quantifying the economic risks of climate change. Nature Climate Change, 7(11), 774–782. 10.1038/nclimate3411 [DOI] [Google Scholar]
- Diffenbaugh, N. S. , & Burke, M. (2019). Global warming has increased global economic inequality. Proceedings of the National Academy of Sciences, 201816020 10.1073/pnas.1816020116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diffenbaugh, N. S. , & Scherer, M. (2013). Likelihood of July 2012 U.S. temperatures in preindustrial and current forcing regimes. Bulletin of the American Meteorological Society, 94(9), S6–S9. [Google Scholar]
- Dunn, A. , Grosse, S. D. , & Zuvekas, S. H. (2018). Adjusting health expenditures for inflation: A review of measures for health services research in the United States. Health Services Research, 53(1), 175–196. 10.1111/1475-6773.12612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebi, K. L. , Boyer, C. , Bowen, K. J. , Frumkin, H. , & Hess, J. (2018). Monitoring and evaluation indicators for climate change‐related health impacts, risks, adaptation, and resilience. International Journal of Environmental Research and Public Health, 15(9), 1943 10.3390/ijerph15091943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebi, K. L. , Ogden, N. H. , Semenza, J. C. , & Woodward, A. (2017). Detecting and attributing health burdens to climate change. Environmental Health Perspectives, 125(8), 085004 10.1289/EHP1509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebi, K. L. , Semenza, J. C. , & Rocklöv, J. (2016). Current medical research funding and frameworks are insufficient to address the health risks of global environmental change. Environmental Health, 15(1). 10.1186/s12940-016-0183-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eidson, M. , Clancy, K. , & Birkhead, G. (2016). Public health climate change adaptation planning using stakeholder feedback. Journal of Public Health Management and Practice, 22(1), E11–E19. 10.1097/PHH.0000000000000243 [DOI] [PubMed] [Google Scholar]
- Estrada, F. , Botzen, W. W. , & Tol, R. S. (2015). Economic losses from U.S. hurricanes consistent with an influence from climate change. Nature Geoscience, 8(11), 880–884. 10.1038/ngeo2560 [DOI] [Google Scholar]
- Fann, N. , Alman, B. , Broome, R. A. , Morgan, G. G. , Johnston, F. H. , Pouliot, G. , & Rappold, A. G. (2018). The health impacts and economic value of wildland fire episodes in the U.S.: 2008–2012. Science of the Total Environment, 610‐611, 802–809. 10.1016/j.scitotenv.2017.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fann, N. , Lamson, A. D. , Anenberg, S. C. , Wesson, K. , Risley, D. , & Hubbell, B. J. (2012). Estimating the national public health burden associated with exposure to ambient PM2.5 and ozone: U.S. public health burden of PM2.5 and ozone. Risk Analysis, 32(1), 81–95. 10.1111/j.1539-6924.2011.01630.x [DOI] [PubMed] [Google Scholar]
- Fann, N. , Nolte, C. G. , Dolwick, P. , Spero, T. L. , Brown, A. C. , Phillips, S. , & Anenberg, S. (2015). The geographic distribution and economic value of climate change‐related ozone health impacts in the United States in 2030. Journal of the Air & Waste Management Association, 65(5), 570–580. 10.1080/10962247.2014.996270 [DOI] [PubMed] [Google Scholar]
- Federal Emergency Management Agency . (n.d.). Disaster declarations by year|FEMA.gov. Retrieved March 3, 2019, from https://www.fema.gov/disasters/year/2012?field_dv2_declaration_type_value=All
- Fleming, L. E. , Kirkpatrick, B. , Backer, L. C. , Walsh, C. J. , Nierenberg, K. , Clark, J. , Reich, A. , Hollenbeck, J. , Benson, J. , Cheng, Y. S. , Naar, J. , Pierce, R. , Bourdelais, A. J. , Abraham, W. M. , Kirkpatrick, G. , Zaias, J. , Wanner, A. , Mendes, E. , Shalat, S. , Hoagland, P. , Stephan, W. , Bean, J. , Watkins, S. , Clarke, T. , Byrne, M. , & Baden, D. G. (2011). Review of Florida red tide and human health effects. Harmful Algae, 10(2), 224–233. 10.1016/j.hal.2010.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier, N. M. , & Douce, R. W. (2017). First reported case of Lyme carditis in Southwest Michigan. Spartan Medical Research Journal, 1(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan, R. W. , Ford, B. , Lassman, W. , Pfister, G. , Vaidyanathan, A. , Fischer, E. , Volckens, J. , Pierce, J. R. , & Magzamen, S. (2017). Comparison of wildfire smoke estimation methods and associations with cardiopulmonary‐related hospital admissions: Estimates of smoke and health outcomes. GeoHealth, 1, 122–136. 10.1002/2017GH000073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore, E. A. , & St. Clair, T. (2018). Budgeting for climate change: Obstacles and opportunities at the U.S. state level. Climate Policy, 18(6), 729–741. 10.1080/14693062.2017.1366891 [DOI] [Google Scholar]
- Gotanda, H. , Fogel, J. , Husk, G. , Levine, J. M. , Peterson, M. , Baumlin, K. , & Habboushe, J. (2015). Hurricane Sandy: Impact on emergency department and hospital utilization by older adults in Lower Manhattan, New York (USA). Prehospital and Disaster Medicine, 30(5), 496–502. 10.1017/S1049023X15005087 [DOI] [PubMed] [Google Scholar]
- Government Accountability Office . (2017). Climate change: Information on potential economic effects could help guide federal efforts to reduce fiscal exposure (No. GAO‐17‐720). Retrieved from https://www.gao.gov/products/GAO-17-720
- Greene, S. , Kalkstein, L. S. , Mills, D. M. , & Samenow, J. (2011). An examination of climate change on extreme heat events and climate–mortality relationships in large U.S. cities. Weather, Climate, and Society, 3(4), 281–292. 10.1175/WCAS-D-11-00055.1 [DOI] [Google Scholar]
- Greenstone, M. , Kopits, E. , & Wolverton, A. (2013). Developing a social cost of carbon for U.S. regulatory analysis: A methodology and interpretation. Review of Environmental Economics and Policy, 7(1), 23–46. 10.1093/reep/res015 [DOI] [Google Scholar]
- Gronlund, C. J. , Sheppard, L. , Adar, S. D. , O'Neill, M. S. , Auchincloss, A. , Madrigano, J. , Kaufman, J. , & Diez Roux, A. V. (2018). Vulnerability to the cardiovascular effects of ambient heat in six U.S. cities: Results from the Multi‐Ethnic Study of Atherosclerosis (MESA). Epidemiology, 29(6), 756–764. 10.1097/EDE.0000000000000910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gropp, R. E. (2017). The cost of ignoring environmental trends. BioScience, 67(12), 1015–1015. 10.1093/biosci/bix139 [DOI] [Google Scholar]
- Grossman, E. , Hathaway, M. , Bush, K. , Cahillane, M. , English, D. , Holmes, T. , Moran, C. E. , Uejio, C. K. , York, E. A. , & Dorevitch, S. (2019). Minigrants to local health departments: An opportunity to promote climate change preparedness. Journal of Public Health Management and Practice, 25(2), 113–120. 10.1097/PHH.0000000000000826 [DOI] [PubMed] [Google Scholar]
- Hansen, J. , Sato, M. , Ruedy, R. , Lo, K. , Lea, D. W. , & Medina‐Elizade, M. (2006). Global temperature change. Proceedings of the National Academy of Sciences, 103(39), 14288–14293. 10.1073/pnas.0606291103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, K. , Blashki, G. , Wiseman, J. , Burke, S. , & Reifels, L. (2018). Climate change and mental health: Risks, impacts and priority actions. International Journal of Mental Health Systems, 12(1), 28 10.1186/s13033-018-0210-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess, J. J. , Saha, S. , & Luber, G. (2014). Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: Analysis of a nationally representative sample. Environmental Health Perspectives, 122(11), 1209–1215. 10.1289/ehp.1306796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilborn, E. D. , Roberts, V. A. , Backer, L. , DeConno, E. , Egan, J. S. , Hyde, J. B. , Nicholas, D. C. , Wiegert, E. J. , Billing, L. M. , DiOrio, M. , Mohr, M. C. , Hardy, F. J. , Wade, T. J. , Yoder, J. S. , & Hlavsa, M. C. (2014). Algal bloom‐associated disease outbreaks among users of freshwater lakes—United States, 2009–2010. New York, 63(1), 5. [PMC free article] [PubMed] [Google Scholar]
- Hoagland, P. , Jin, D. , Beet, A. , Kirkpatrick, B. , Reich, A. , Ullmann, S. , Fleming, L. E. , & Kirkpatrick, G. (2014). The human health effects of Florida Red Tide (FRT) blooms: An expanded analysis. Environment International, 68, 144–153. 10.1016/j.envint.2014.03.016 [DOI] [PubMed] [Google Scholar]
- Hoagland, P. , & Scatasta, S. (2006). The economic effects of harmful algal blooms In Granéli E., & Turner J. T. (Eds.), Ecology of Harmful Algae, (Vol. 189, pp. 391–402). Berlin Heidelberg: Springer; 10.1007/978-3-540-32210-8_30 [DOI] [Google Scholar]
- Hoagland, P. , Jin, D. , Polansky, L. Y. , Kirkpatrick, B. , Kirkpatrick, G. , Fleming, L. E. , Reich, A. , Watkins, S. M. , Ullmann, S. G. , & Backer, L. C. (2009). The costs of respiratory illnesses arising from Florida Gulf Coast Karenia brevis blooms. Environmental Health Perspectives, 117(8), 1239–1243. 10.1289/ehp.0900645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IPCC (2018). Impacts of 1.5 °C global warming on natural and human systems In Masson‐Delmotte V., Zhai P., Pörtner H.‐O., Roberts D., Skea J., Shukla P. R., Pirani A., Moufouma‐Okia W., Péan C., Pidcock R., Connors S., Matthews J. B. R., Chen Y., Zhou X., Gomis M. I., Lonnoy E., Maycock T., Tignor M., & Waterfield T. (Eds.), Global Warming of 1.5°C. An IPCC Special Report on the impacts of global warming of 1.5°C above pre‐industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty (Chap. 3, pp. 240–241). Geneva, Switzerland. [Google Scholar]
- Hoerling, M. , Schubert, S. , & Mo, K. (2013). An interpretation of the origins of the 2012 central Great Plains drought. NOAA Drought Task Force/National Integrated Drought Information System (NIDIS). Retrieved from https://www.esrl.noaa.gov/psd/csi/factsheets/pdf/noaa-gp-drought-assessment-report.pdf
- Howard, P . (2014). Omitted damages: What's missing from the social cost of carbon. Retrieved from https://costofcarbon.org/files/Omitted_Damages_Whats_Missing_From_the_Social_Cost_of_Carbon.pdf
- Hsiang, S. , Kopp, R. , Jina, A. , Rising, J. , Delgado, M. , Mohan, S. , Rasmussen, D. J. , Muir‐Wood, R. , Wilson, P. , Oppenheimer, M. , Larsen, K. , & Houser, T. (2017). Estimating economic damage from climate change in the United States. Science, 356(6345), 1362–1369. 10.1126/science.aal4369 [DOI] [PubMed] [Google Scholar]
- Huang, M.‐Y. , Alavalapati, J. R. R. , Carter, D. R. , & Langholtz, M. H. (2007). Is the choice of renewable portfolio standards random? Energy Policy, 35(11), 5571–5575. 10.1016/j.enpol.2007.06.010 [DOI] [Google Scholar]
- Hutton, G. (2011). The economics of health and climate change: Key evidence for decision making. Globalization and Health, 7(1), 18 10.1186/1744-8603-7-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton, G. , & Menne, B. (2014). Economic evidence on the health impacts of climate change in Europe. Environmental Health Insights, 8, EHI.S16486 10.4137/EHI.S16486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intergovernmental Panel on Climate Change . (2018). Global warming of 1.5 °C: Summary for policymakers (No. IPCC SR1.5) (p. 33). Geneva, Switzerland: Intergovernmental Panel on Climate Change; Retrieved from https://www.ipcc.ch/sr15/chapter/summary-for-policy-makers/ [Google Scholar]
- Jacob, D. J. , & Winner, D. A. (2009). Effect of climate change on air quality. Atmospheric Environment, 43(1), 51–63. 10.1016/j.atmosenv.2008.09.051 [DOI] [Google Scholar]
- Jagai, J. S. , Li, Q. , Wang, S. , Messier, K. P. , Wade, T. J. , & Hilborn, E. D. (2015). Extreme precipitation and emergency room visits for gastrointestinal illness in areas with and without combined sewer systems: An analysis of Massachusetts data, 2003–2007. Environmental Health Perspectives, 123(9), 873–879. 10.1289/ehp.1408971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Henry J. Family Foundation . (2019). Medicare beneficiaries as a percent of total population. Retrieved June 18, 2019, from https://www.kff.org/medicare/state-indicator/medicare-beneficiaries-as-of-total-pop/
- Keellings, D. , & Hernández Ayala, J. J. (2019). Extreme rainfall associated with Hurricane Maria over Puerto Rico and its connections to climate variability and change. Geophysical Research Letters, 46, 2964–2973. 10.1029/2019GL082077 [DOI] [Google Scholar]
- Kelman, J. , Finne, K. , Bogdanov, A. , Worrall, C. , Margolis, G. , Rising, K. , MaCurdy, T. E. , & Lurie, N. (2015). Dialysis care and death following Hurricane Sandy. American Journal of Kidney Diseases, 65(1), 109–115. 10.1053/j.ajkd.2014.07.005 [DOI] [PubMed] [Google Scholar]
- Kim, E. J. (2016). The impacts of climate change on human health in the United States: A scientific assessment, by U.S. Global Change Research Program. Journal of the American Planning Association, 82(4), 418–419. 10.1080/01944363.2016.1218736 [DOI] [Google Scholar]
- Kim, H. , Schwartz, R. M. , Hirsch, J. , Silverman, R. , Liu, B. , & Taioli, E. (2016). Effect of Hurricane Sandy on Long Island emergency departments visits. Disaster Medicine and Public Health Preparedness, 10(3), 344–350. 10.1017/dmp.2015.189 [DOI] [PubMed] [Google Scholar]
- Kinney, P. L. (2018). Interactions of climate change, air pollution, and human health. Current Environmental Health Reports, 5(1), 179–186. 10.1007/s40572-018-0188-x [DOI] [PubMed] [Google Scholar]
- Kirkpatrick, B. , Bean, J. A. , Fleming, L. E. , Kirkpatrick, G. , Grief, L. , Nierenberg, K. , Reich, A. , Watkins, S. , & Naar, J. (2010). Gastrointestinal emergency room admissions and Florida red tide blooms. Harmful Algae, 9(1), 82–86. 10.1016/j.hal.2009.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishore, N. , Marqués, D. , Mahmud, A. , Kiang, M. V. , Rodriguez, I. , Fuller, A. , Ebner, P. , Sorensen, C. , Racy, F. , Lemery, J. , Maas, L. , Leaning, J. , Irizarry, R. A. , Balsari, S. , & Buckee, C. O. (2018). Mortality in Puerto Rico after Hurricane Maria. New England Journal of Medicine, 379(2), 162–170. 10.1056/NEJMsa1803972 [DOI] [PubMed] [Google Scholar]
- Knowlton, K. , Rosenthal, J. E. , Hogrefe, C. , Lynn, B. , Gaffin, S. , Goldberg, R. , Rosenzweig, C. , Civerolo, K. , Ku, J. Y. , & Kinney, P. L. (2004). Assessing ozone‐related health impacts under a changing climate. Environmental Health Perspectives, 112(15), 1557–1563. 10.1289/ehp.7163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowlton, K. , Rotkin‐Ellman, M. , Geballe, L. , Max, W. , & Solomon, G. M. (2011). Six climate change‐related events in the United States accounted for about $14 billion in lost lives and health costs. Health Affairs, 30(11), 2167–2176. 10.1377/hlthaff.2011.0229 [DOI] [PubMed] [Google Scholar]
- Kunz, M. , Mühr, B. , Kunz‐Plapp, T. , Daniell, J. , Khazai, B. , Wenzel, F. , Vannieuwenhuyse, M. , Comes, T. , Elmer, F. , Schröter, K. , Fohringer, J. , Münzberg, T. , Lucas, C. , & Zschau, J. (2013). Investigation of superstorm Sandy 2012 in a multi‐disciplinary approach. Natural Hazards and Earth System Sciences, 13(10), 2579–2598. 10.5194/nhess-13-2579-2013 [DOI] [Google Scholar]
- Lantos, P. M. , Tsao, J. , Nigrovic, L. E. , Auwaerter, P. G. , Fowler, V. , Ruffin, F. , Foster, E. , & Hickling, G. (2017). Geographic expansion of Lyme disease in Michigan, 2000‐2014. Open Forum Infectious Diseases, ofw269 10.1093/ofid/ofw269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larkin, S. L. , & Adams, C. M. (2007). Harmful algal blooms and coastal business: Economic consequences in Florida. Society & Natural Resources, 20(9), 849–859. 10.1080/08941920601171683 [DOI] [Google Scholar]
- Lay, C. R. , Mills, D. , Belova, A. , Sarofim, M. C. , Kinney, P. L. , Vaidyanathan, A. , Jones, R. , Hall, R. , & Saha, S. (2018). Emergency department visits and ambient temperature: Evaluating the connection and projecting future outcomes. GeoHealth, 2(6), 182–194. 10.1002/2018GH000129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, D. C. , Gupta, V. K. , Carr, B. G. , Malik, S. , Ferguson, B. , Wall, S. P. , Smith, S. W. , & Goldfrank, L. R. (2016). Acute post‐disaster medical needs of patients with diabetes: Emergency department use in New York City by diabetic adults after Hurricane Sandy. BMJ Open Diabetes Research & Care, 4(1), e000248 10.1136/bmjdrc-2016-000248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy, K. , Woster, A. P. , Goldstein, R. S. , & Carlton, E. J. (2016). Untangling the impacts of climate change on waterborne diseases: A systematic review of relationships between diarrheal diseases and temperature, rainfall, flooding, and drought. Environmental Science & Technology, 50(10), 4905–4922. 10.1021/acs.est.5b06186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limaye, V. S. , Vargo, J. , Harkey, M. , Holloway, T. , & Patz, J. A. (2018). Climate change and heat‐related excess mortality in the eastern USA. EcoHealth, 15(3), 485–496. 10.1007/s10393-018-1363-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C. , Pierce, L. C. , Roblin, P. M. , & Arquilla, B. (2014). Impact of Hurricane Sandy on hospital emergency and dialysis services: A retrospective survey. Prehospital and Disaster Medicine, 29(4), 374–379. 10.1017/S1049023X14000715 [DOI] [PubMed] [Google Scholar]
- Lin, N. , Emanuel, K. , Oppenheimer, M. , & Vanmarcke, E. (2012). Physically based assessment of hurricane surge threat under climate change. Nature Climate Change, 2(6), 462–467. 10.1038/nclimate1389 [DOI] [Google Scholar]
- Lin, S. , Lu, Y. , Justino, J. , Dong, G. , & Lauper, U. (2016). What happened to our environment and mental health as a result of Hurricane Sandy? Disaster Medicine and Public Health Preparedness, 10(3), 314–319. 10.1017/dmp.2016.51 [DOI] [PubMed] [Google Scholar]
- Liu, J. C. , Mickley, L. J. , Sulprizio, M. P. , Yue, X. , Peng, R. D. , Dominici, F. , & Bell, M. L. (2016). Future respiratory hospital admissions from wildfire smoke under climate change in the western U.S. Environmental Research Letters, 11(12), 124018 10.1088/1748-9326/11/12/124018 [DOI] [Google Scholar]
- Lo, Y. T. E. , Mitchell, D. M. , Gasparrini, A. , Vicedo‐Cabrera, A. M. , Ebi, K. L. , Frumhoff, P. C. , Millar, R. J. , Roberts, W. , Sera, F. , Sparrow, S. , Uhe, P. , & Williams, G. (2019). Increasing mitigation ambition to meet the Paris Agreement's temperature goal avoids substantial heat‐related mortality in U.S. cities. Science Advances, 5(6). 10.1126/sciadv.aau4373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luber, G. , & McGeehin, M. (2008). Climate change and extreme heat events. American Journal of Preventive Medicine, 35(5), 429–435. 10.1016/j.amepre.2008.08.021 [DOI] [PubMed] [Google Scholar]
- Mac, S. , da Silva, S. R. , & Sander, B. (2019). The economic burden of Lyme disease and the cost‐effectiveness of Lyme disease interventions: A scoping review. PLoS ONE, 14(1), e0210280 10.1371/journal.pone.0210280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall, E. G. , Lu, S.‐E. , Shi, Z. , Swerdel, J. , Borjan, M. , & Lumia, M. E. (2016). Work‐related unintentional injuries associated with Hurricane Sandy in New Jersey. Disaster Medicine and Public Health Preparedness, 10(3), 394–404. 10.1017/dmp.2016.47 [DOI] [PubMed] [Google Scholar]
- Marshall, E. G. , Lu, S.‐E. , Williams, A. O. , Lefkowitz, D. , & Borjan, M. (2018). Tree‐related injuries associated with response and recovery from Hurricane Sandy, New Jersey, 2011‐2014. Public Health Reports, 133(3), 266–273. 10.1177/0033354918766871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marten, A. L. , Kopp, R. E. , Shouse, K. C. , Griffiths, C. W. , Hodson, E. L. , Kopits, E. , Mignone, B. K. , Moore, C. , Newbold, S. C. , Waldhoff, S. , & Wolverton, A. (2013). Improving the assessment and valuation of climate change impacts for policy and regulatory analysis. Climatic Change, 117(3), 433–438. 10.1007/s10584-012-0608-0 [DOI] [Google Scholar]
- Martinich, J. , & Crimmins, A. (2019). Climate damages and adaptation potential across diverse sectors of the United States. Nature Climate Change, 9(5), 397–404. 10.1038/s41558-019-0444-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuade, L. , Merriman, B. , Lyford, M. , Nadler, B. , Desai, S. , Miller, R. , & Mallette, S. (2018). Emergency department and inpatient health care services utilization by the elderly population: Hurricane Sandy in the State of New Jersey. Disaster Medicine and Public Health Preparedness, 12(6), 730–738. 10.1017/dmp.2018.1 [DOI] [PubMed] [Google Scholar]
- Meehl, G. A. , Arblaster, J. M. , & Tebaldi, C. (2007). Contributions of natural and anthropogenic forcing to changes in temperature extremes over the United States. Geophysical Research Letters, 34, L19709 10.1029/2007GL030948 [DOI] [Google Scholar]
- Mickley, L. J. (2004). Effects of future climate change on regional air pollution episodes in the United States. Geophysical Research Letters, 31, L24103 10.1029/2004GL021216 [DOI] [Google Scholar]
- Monaghan, A. J. , Moore, S. M. , Sampson, K. M. , Beard, C. B. , & Eisen, R. J. (2015). Climate change influences on the annual onset of Lyme disease in the United States. Ticks and Tick‐Borne Diseases, 6(5), 615–622. 10.1016/j.ttbdis.2015.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, S. K. , Trainer, V. L. , Mantua, N. J. , Parker, M. S. , Laws, E. A. , Backer, L. C. , & Fleming, L. E. (2008). Impacts of climate variability and future climate change on harmful algal blooms and human health. Environmental Health, 7(Suppl 2), S4 10.1186/1476-069X-7-S2-S4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorman, J. E. , Akinbami, L. J. , Bailey, C. , Zahran, H. , King, M. , Johnson, C. , & Liu, X. (2012). National surveillance of asthma: United States, 2001‐2010. Vital & Health Statistics. Series 3, Analytical and Epidemiological Studies, 35, 1–58. [PubMed] [Google Scholar]
- Mora, C. , Counsell, C. W. W. , Bielecki, C. R. , & Louis, L. V. (2017). Twenty‐seven ways a heat wave can kill you: Deadly heat in the era of climate change. Circulation. Cardiovascular Quality and Outcomes, 10(11). 10.1161/CIRCOUTCOMES.117.004233 [DOI] [PubMed] [Google Scholar]
- Munich RE NatCatSERVICE . (2017). Heatwave/wildfire events in the United States 2011–2016. Retrieved January 22, 2019, from https://natcatservice.munichre.com/
- Murray, K. O. , Ruktanonchai, D. , Hesalroad, D. , Fonken, E. , & Nolan, M. S. (2013). West Nile virus, Texas, USA, 2012. Emerging Infectious Diseases, 19(11). 10.3201/eid1911.130768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasci, R. , Xiang, J. , D'Anton, M. , Duggal, N. K. , Day, J. , Seiferth, R. , & Brault, A. C. (2013). Sequence analyses of 2012 West Nile virus isolates from Texas fail to associate viral genetic factors with outbreak magnitude. The American Journal of Tropical Medicine and Hygiene, 89(2), 205–210. 10.4269/ajtmh.13-0140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Building Sciences . (2017). Natural hazard mitigation saves study. Washington D.C., USA: National Institute of Building Sciences; Retrieved from https://www.nibs.org/page/mitigationsaves [Google Scholar]
- Neumann, J. E. , Anenberg, S. C. , Weinberger, K. R. , Amend, M. , Gulati, S. , Crimmins, A. , Roman, H. , Fann, N. , & Kinney, P. L. (2018). Estimates of present and future asthma emergency department visits associated with exposure to oak, birch, and grass pollen in the United States. GeoHealth, 3, 11–27. 10.1029/2018GH000153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsen, V. , Lier, J. A. , Bjerkholt, J. T. , & Lindholm, O. G. (2011). Analysing urban floods and combined sewer overflows in a changing climate. Journal of Water and Climate Change, 2(4), 260–271. 10.2166/wcc.2011.042 [DOI] [Google Scholar]
- Nordhaus, W. D. (1991). The cost of slowing climate change: A survey. The Energy Journal, 37–65. [Google Scholar]
- OBrien, L. V. , Berry, H. L. , Coleman, C. , & Hanigan, I. C. (2014). Drought as a mental health exposure. Environmental Research, 131, 181–187. 10.1016/j.envres.2014.03.014 [DOI] [PubMed] [Google Scholar]
- Ogden, N. H. , Radojević, M. , Wu, X. , Duvvuri, V. R. , Leighton, P. A. , & Wu, J. (2014). Estimated effects of projected climate change on the basic reproductive number of the Lyme disease vector ixodes scapularis. Environmental Health Perspectives, 122(6), 631–638. 10.1289/ehp.1307799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papalexiou, S. M. , & Montanari, A. (2019). Global and regional increase of precipitation extremes under global warming. Water Resources Research, 55, 4901–4914. 10.1029/2018WR024067 [DOI] [Google Scholar]
- Patz, J. A. , Grabow, M. L. , & Limaye, V. S. (2014). When it rains, it pours: Future climate extremes and health. Annals of Global Health, 80(4), 332–344. 10.1016/j.aogh.2014.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paull, S. H. , Horton, D. E. , Ashfaq, M. , Rastogi, D. , Kramer, L. D. , Diffenbaugh, N. S. , & Kilpatrick, A. M. (2017). Drought and immunity determine the intensity of West Nile virus epidemics and climate change impacts. Proceedings of the Royal Society B: Biological Sciences, 284(1848), 20162078 10.1098/rspb.2016.2078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Charitable Trusts . (2017). Flooding disasters cost billions in 2016. Retrieved June 26, 2019, from http://pew.org/2kh102n
- Poh, K. C. , Chaves, L. F. , Reyna‐Nava, M. , Roberts, C. M. , Fredregill, C. , Bueno, R. , Debboun, M. , & Hamer, G. L. (2019). The influence of weather and weather variability on mosquito abundance and infection with West Nile virus in Harris County, Texas, USA. Science of the Total Environment, 675, 260–272. 10.1016/j.scitotenv.2019.04.109 [DOI] [PubMed] [Google Scholar]
- Rahmstorf, S. , & Coumou, D. (2011). Increase of extreme events in a warming world. Proceedings of the National Academy of Sciences, 108(44), 17905–17909. 10.1073/pnas.1101766108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappaport, E. N. , & Blanchard, B. W. (2016). Fatalities in the United States indirectly associated with Atlantic tropical cyclones. Bulletin of the American Meteorological Society, 97(7), 1139–1148. 10.1175/BAMS-D-15-00042.1 [DOI] [Google Scholar]
- Ray, G. , Schulz, T. , Daniels, W. , Daly, E. R. , Andrew, T. A. , Brown, C. M. , Cummings, P. , Nelson, R. , Cartter, M. L. , Backenson, P. B. , White, J. L. , Kurpiel, P. M. , Rockwell, R. , Rotans, A. S. , Hertzog, C. , Squires, L. S. , Linden, J. V. , Prial, M. , House, J. , Pontones, P. , Batten, B. , Blau, D. , DeLeon‐Carnes, M. , Muehlenbachs, A. , Ritter, J. , Sanders, J. , Zaki, S. R. , Mead, P. , Hinckley, A. , Nelson, C. , Perea, A. , Schriefer, M. , Molins, C. , & Forrester, J. D. (2013). Three sudden cardiac deaths associated with Lyme carditis—United States, November 2012–July 2013. MMWR. Morbidity and Mortality Weekly Report, 62(49), 993–996. [PMC free article] [PubMed] [Google Scholar]
- Reid, C. E. , Brauer, M. , Johnston, F. H. , Jerrett, M. , Balmes, J. R. , & Elliott, C. T. (2016). Critical review of health impacts of wildfire smoke exposure. Environmental Health Perspectives, 124(9), 1334–1343. 10.1289/ehp.1409277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid, C. E. , & Gamble, J. L. (2009). Aeroallergens, allergic disease, and climate change: Impacts and adaptation. EcoHealth, 6(3), 458–470. 10.1007/s10393-009-0261-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Revesz, R. L. , Howard, P. H. , Arrow, K. , Goulder, L. H. , Kopp, R. E. , Livermore, M. A. , Oppenheimer, M. , & Sterner, T. (2014). Global warming: Improve economic models of climate change. Nature News, 508(7495), 173–175. 10.1038/508173a [DOI] [PubMed] [Google Scholar]
- Riebesell, U. , Aberle‐Malzahn, N. , Achterberg, E. P. , Algueró‐Muñiz, M. , Alvarez‐Fernandez, S. , Arístegui, J. , Bach, L. T. , Boersma, M. , Boxhammer, T. , Guan, W. , Haunost, M. , Horn, H. G. , Löscher, C. R. , Ludwig, A. , Spisla, C. , Sswat, M. , Stange, P. , & Taucher, J. (2018). Toxic algal bloom induced by ocean acidification disrupts the pelagic food web. Nature Climate Change, 8(12), 1082–1086. 10.1038/s41558-018-0344-1 [DOI] [Google Scholar]
- Rippey, B. R. (2015). The U.S. drought of 2012. Weather and Climate Extremes, 10, 57–64. 10.1016/j.wace.2015.10.004 [DOI] [Google Scholar]
- Roehr, B. (2012). U.S. hit by massive West Nile virus outbreak centred around Texas. BMJ, 345(aug21 2), e5633–e5633. 10.1136/bmj.e5633 [DOI] [PubMed] [Google Scholar]
- Roser‐Renouf, C. , Maibach, E. W. , & Li, J. (2016). Adapting to the changing climate: An assessment of local health department preparations for climate change‐related health threats, 2008‐2012. PLoS ONE, 11(3), e0151558 10.1371/journal.pone.0151558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saari, R. K. , Thompson, T. M. , & Selin, N. E. (2017). Human health and economic impacts of ozone reductions by income group. Environmental Science & Technology, 51(4), 1953–1961. 10.1021/acs.est.6b04708 [DOI] [PubMed] [Google Scholar]
- Salas, R. , Knappenberger, P. , & Hess, J. (2018). 2018 Lancet countdown on health and climate change, Brief for the United States of America. Retrieved from http://www.lancetcountdown.org/media/1426/2018-lancet-countdown-policy-brief-usa.pdf
- Santos‐Burgoa, C. , Sandberg, J. , Suárez, E. , Goldman‐Hawes, A. , Zeger, S. , Garcia‐Meza, A. , Pérez C. M., Estrada‐Merly N., Colón‐Ramos U., Nazario C. M., Andrade E., Roess A., Goldman L. (2018). Differential and persistent risk of excess mortality from Hurricane Maria in Puerto Rico: A time‐series analysis. The Lancet Planetary Health, 2(11), e478–e488. 10.1016/S2542-5196(18)30209‐2 [DOI] [PubMed] [Google Scholar]
- Sapkota, A. , Murtugudde, R. , Curriero, F. C. , Upperman, C. R. , Ziska, L. , & Jiang, C. (2019). Associations between alteration in plant phenology and hay fever prevalence among U.S. adults: Implication for changing climate. PLoS ONE, 14(3), e0212010 10.1371/journal.pone.0212010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnall, A. , Law, R. , Heinzerling, A. , Sircar, K. , Damon, S. , Yip, F. , Schier, J. , Bayleyegn, T. , & Wolkin, A. (2017). Characterization of carbon monoxide exposure during Hurricane Sandy and subsequent Nor'easter. Disaster Medicine and Public Health Preparedness, 11(5), 562–567. 10.1017/dmp.2016.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz, A. M. (2017). Surveillance for Lyme disease—United States, 2008–2015. MMWR Surveillance Summaries, 66(22), 1–12. 10.15585/mmwr.ss6622a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar, M. B. , Staples, J. E. , Fischer, M. , Meltzer, M. I. , & Sejvar, J. J. (2014). Initial and long‐term costs of patients hospitalized with West Nile virus disease. The American Journal of Tropical Medicine and Hygiene, 90(3), 402–409. 10.4269/ajtmh.13-0206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan, M. C. , Fox, M. A. , Kaye, C. , & Resnick, B. (2017). Integrating health into local climate response: Lessons from the U.S. CDC climate‐ready states and cities initiative. Environmental Health Perspectives, 125(9), 094501 10.1289/EHP1838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimamoto, M. M. , & McCormick, S. (2017). The role of health in urban climate adaptation: An analysis of six U.S. cities. Weather, Climate, and Society, 9(4), 777–785. 10.1175/WCAS-D-16-0142.1 [DOI] [Google Scholar]
- Smith, A. B. (2019). 2018's billion dollar disasters in context|NOAA Climate.gov. Retrieved June 18, 2019, from https://www.climate.gov/news-features/blogs/beyond-data/2018s-billion-dollar-disasters-context
- Smith, A. B. , & Katz, R. W. (2013). U.S. billion‐dollar weather and climate disasters: Data sources, trends, accuracy and biases. Natural Hazards, 67(2), 387–410. 10.1007/s11069-013-0566-5 [DOI] [Google Scholar]
- Stanke, C. , Kerac, M. , Prudhomme, C. , Medlock, J. , & Murray, V. (2013). Health effects of drought: A systematic review of the evidence. PLoS Currents. 10.1371/currents.dis.7a2cee9e980f91ad7697b570bcc4b004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- State of Ohio Emergency Operations Center . (2012). Situation report (Statewide Severe Weather – June 29, 2012). Retrieved from https://www.ema.ohio.gov/Documents/SituationReports/Statewide%20Severe%20Weather%20-%20June%202012/Statewide%20Severe%20Weather%20-June%2029%202012%20-%20SitRep%2020120707.pdf
- Stott, P. (2016). How climate change affects extreme weather events. Science, 352(6293), 1517–1518. 10.1126/science.aaf7271 [DOI] [PubMed] [Google Scholar]
- Stott, P. A. , Gillett, N. P. , Hegerl, G. C. , Karoly, D. J. , Stone, D. A. , Zhang, X. , & Zwiers, F. (2010). Detection and attribution of climate change: A regional perspective—Detection and attribution of climate change. Wiley Interdisciplinary Reviews: Climate Change, 1(2), 192–211. 10.1002/wcc.34 [DOI] [Google Scholar]
- Sun, X. , Waller, A. , Yeatts, K. B. , & Thie, L. (2016). Pollen concentration and asthma exacerbations in Wake County, North Carolina, 2006–2012. Science of the Total Environment, 544, 185–191. 10.1016/j.scitotenv.2015.11.100 [DOI] [PubMed] [Google Scholar]
- Sweet, W. , Zervas, C. , Gill, S. , & Park, J. (2013). Hurricane Sandy inundation probabilities today and tomorrow. Bulletin of the American Meteorological Society, 94(9), S17–S20. [Google Scholar]
- Swerdel, J. N. , Janevic, T. M. , Cosgrove, N. M. , Kostis, J. B. , & the Myocardial Infarction Data Acquisition System (MIDAS 24) Study Group (2014). The effect of Hurricane Sandy on cardiovascular events in New Jersey. Journal of the American Heart Association, 3(6), e001354 10.1161/JAHA.114.001354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swerdel, J. N. , Rhoads, G. G. , Cosgrove, N. M. , Kostis, J. B. , & for the Myocardial Infarction Data Acquisition System (MIDAS 25) Study Group (2016). Rates of hospitalization for dehydration following Hurricane Sandy in New Jersey. Disaster Medicine and Public Health Preparedness, 10(2), 188–192. 10.1017/dmp.2015.169 [DOI] [PubMed] [Google Scholar]
- Tschakert, P. , Ellis, N. R. , Anderson, C. , Kelly, A. , & Obeng, J. (2019). One thousand ways to experience loss: A systematic analysis of climate‐related intangible harm from around the world. Global Environmental Change, 55, 58–72. 10.1016/j.gloenvcha.2018.11.006 [DOI] [Google Scholar]
- U.S. Agency for Healthcare Research and Quality . (n.d.‐a). HCUPnet, Healthcare Cost and Utilization Project. Retrieved June 21, 2019, from https://hcupnet.ahrq.gov/
- U.S. Agency for Healthcare Research and Quality . (n.d.‐b). Medical expenditure panel survey household component overview. Retrieved June 26, 2019, from https://meps.ahrq.gov/mepsweb/survey_comp/household.jsp
- U.S. Bureau of Economic Analysis . (n.d.). Personal consumption expenditures: Chain‐type price index. Retrieved June 26, 2019, from https://fred.stlouisfed.org/series/PCEPI
- U.S. Bureau of Labor Statistics . (2016). Employment and wages, Annual Averages 2012. Retrieved June 26, 2019, from https://www.bls.gov/cew/cewbultn12.htm
- U.S. Census Bureau . (n.d.‐a). American FactFinder—Results. Retrieved June 20, 2019, from https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk
- U.S. Census Bureau . (n.d.‐b). U.S. Census Bureau QuickFacts: Florida; United States. Retrieved June 28, 2019, from https://www.census.gov/quickfacts/fact/table/FL,US/AGE775218
- U.S. Centers for Disease Control and Prevention . (2013). West Nile virus disease cases and presumptive viremic blood donors reported to ArboNET, United States. Retrieved June 9, 2017, from https://www.cdc.gov/westnile/resources/pdfs/data/2012WNVHumanInfectionsbyState.pdf
- U.S. Centers for Disease Control and Prevention . (2015). ICD‐9 (International Classification of Diseases, Ninth Revision). Retrieved June 25, 2019, from https://www.cdc.gov/nchs/icd/icd9.htm
- U.S. Centers for Disease Control and Prevention . (2016). Extreme heat. Retrieved June 20, 2019, from https://ephtracking.cdc.gov/showClimateChangeExtremeHeat.action
- U.S. Centers for Disease Control and Prevention . (2018a). Lyme disease charts and figures: Historical data. Retrieved June 19, 2019, from https://www.cdc.gov/lyme/stats/graphs.html
- U.S. Centers for Disease Control and Prevention . (2018b). Lyme disease data tables: Historical data. Retrieved June 21, 2019, from https://www.cdc.gov/lyme/stats/tables.html
- U.S. Centers for Disease Control and Prevention . (2019). Data and surveillance (Lyme disease). Retrieved June 20, 2019, from https://www.cdc.gov/lyme/datasurveillance/index.html
- U.S. Centers for Disease Control and Prevention . (n.d.). National environmental public health tracking. Retrieved June 20, 2019, from https://www.cdc.gov/nceh/tracking/default.htm
- U.S. Environmental Protection Agency . (1996). Sanitary sewer overflows. Retrieved from https://www3.epa.gov/npdes/pubs/ssodesc.pdf
- U.S. Environmental Protection Agency . (2014). Mortality risk valuation [Overviews and Factsheets]. Retrieved June 25, 2019, from https://www.epa.gov/environmental-economics/mortality-risk-valuation
- U.S. Environmental Protection Agency . (2015). Regulatory impact analysis for the clean power plan final rule (No. EPA‐452/R‐15‐003). Retrieved from https://www3.epa.gov/ttnecas1/docs/ria/utilities_ria_final-clean-power-plan-existing-units_2015-08.pdf
- U.S. Environmental Protection Agency . (2016). National ambient air quality standards (table). Retrieved June 25, 2019, from https://www.epa.gov/criteria-air-pollutants/naaqs-table
- U.S. Environmental Protection Agency (2017). Environmental benefits mapping and analysis program—Community Edition (BenMAP‐CE) [Collections and Lists]. Retrieved June 25, 2019, from. https://www.epa.gov/benmap
- U.S. Environmental Protection Agency . (2019). Planning for natural disaster debris (No. EPA 530‐F‐19‐003) (p. 150). Retrieved from https://www.epa.gov/sites/production/files/2019-05/documents/final_pndd_guidance_0.pdf
- U.S. Global Change Research Program . (2016). The impacts of climate change on human health in the United States: A scientific assessment. Washington D.C., U.S.A. Retrieved from https://health2016.globalchange.gov/downloads
- U.S. Global Change Research Program . (2018). Fourth National Climate Assessment, Volume II: Impacts, risks, and adaptation in the United States (p. 1515). Washington, D.C: US Global Change Research Program; Retrieved from https://nca2018.globalchange.gov/ [Google Scholar]
- U.S. National Interagency Fire Center . (2012). Wildland fire fatalities by Year, 1910‐2017. Retrieved February 1, 2019, from https://www.nifc.gov/safety/safety_documents/Fatalities-by-Year.pdf
- U.S. National Oceanic and Atmospheric Administration . (2012). Superstorm Sandy and sea level rise. Retrieved June 25, 2019, from https://www.climate.gov/news-features/features/superstorm-sandy-and-sea-level-rise
- U.S. National Oceanic and Atmospheric Administration . (2013a). Billion‐dollar weather and climate disasters: Table of events. Retrieved June 18, 2019, from https://www.ncdc.noaa.gov/billions/events/US/2012
- U.S. National Oceanic and Atmospheric Administration . (2013b). Hurricanes and tropical storms (Annual 2012). Retrieved June 19, 2019, from https://www.ncdc.noaa.gov/sotc/tropical-cyclones/201213
- U.S. National Oceanic and Atmospheric Administration . (2013c). National climate report—Annual 2012. Retrieved June 26, 2019, from https://www.ncdc.noaa.gov/sotc/national/2012/13/supplemental/page-8/
- U.S. National Oceanic and Atmospheric Administration . (2016). Summary of natural hazard statistics for 2012 in the United States. Retrieved from https://www.nws.noaa.gov/om/hazstats/sum12.pdf
- U.S. National Oceanic and Atmospheric Administration . (2018). Reporting on the state of the climate in 2017. Retrieved August 1, 2018, from http://www.ncei.noaa.gov/news/reporting-state-climate-2017
- U.S. National Oceanic and Atmospheric Administration . (2019). Billion‐dollar weather and climate disasters: Overview. Retrieved June 25, 2019, from https://www.ncdc.noaa.gov/billions/
- U.S. National Oceanic and Atmospheric Administration . (n.d.‐a). Harmful algal blooms observing system—HABSOS [Document]. Retrieved June 26, 2019, from https://catalog.data.gov/dataset/physical-and-biological-data-collected-along-the-texas-mississippi-and-florida-gulf-coasts-in-t
- U.S. National Oceanic and Atmospheric Administration . (n.d.‐b). Natural Hazard Statistics (HazStat). Retrieved June 26, 2019, from https://www.nws.noaa.gov/om/hazstats.shtml
- U.S. National Oceanic and Atmospheric Administration , & U.S. National Oceanic and Atmospheric Administration . (n.d.). July 1‐7, 2012 Wisconsin heat wave. Retrieved June 19, 2019, from https://www.weather.gov/mkx/070112-WisconsinHeatWave
- van Oldenborgh, G. J. , van der Wiel, K. , Sebastian, A. , Singh, R. , Arrighi, J. , Otto, F. , Haustein, K. , Li, S. , Vecchi, G. , & Cullen, H. (2017). Attribution of extreme rainfall from Hurricane Harvey, August 2017. Environmental Research Letters, 12(12), 124009 10.1088/1748-9326/aa9ef2 [DOI] [Google Scholar]
- Velez‐Valle, E. M. , Shendell, D. , Echeverria, S. , & Santorelli, M. (2016). Type II diabetes emergency room visits associated with Hurricane Sandy in New Jersey: Implications for preparedness. Journal of Environmental Health, 79(2), 9. [PubMed] [Google Scholar]
- Vins, H. , Bell, J. , Saha, S. , & Hess, J. (2015). The mental health outcomes of drought: A systematic review and causal process diagram. International Journal of Environmental Research and Public Health, 12(10), 13251–13275. 10.3390/ijerph121013251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel, M. M. , Zscheischler, J. , Wartenburger, R. , Dee, D. , & Seneviratne, S. I. (2019). Concurrent 2018 hot extremes across Northern Hemisphere due to human‐induced climate change. Earth's Future, 7, 692–703. 10.1029/2019EF001189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts, N. , Amann, M. , Arnell, N. , Ayeb‐Karlsson, S. , Belesova, K. , Berry, H. , Bouley, T. , Boykoff, M. , Byass, P. , Cai, W. , Campbell‐Lendrum, D. , Chambers, J. , Daly, M. , Dasandi, N. , Davies, M. , Depoux, A. , Dominguez‐Salas, P. , Drummond, P. , Ebi, K. L. , Ekins, P. , Montoya, L. F. , Fischer, H. , Georgeson, L. , Grace, D. , Graham, H. , Hamilton, I. , Hartinger, S. , Hess, J. , Kelman, I. , Kiesewetter, G. , Kjellstrom, T. , Kniveton, D. , Lemke, B. , Liang, L. , Lott, M. , Lowe, R. , Sewe, M. O. , Martinez‐Urtaza, J. , Maslin, M. , McAllister, L. , Mikhaylov, S. J. , Milner, J. , Moradi‐Lakeh, M. , Morrissey, K. , Murray, K. , Nilsson, M. , Neville, T. , Oreszczyn, T. , Owfi, F. , Pearman, O. , Pencheon, D. , Pye, S. , Rabbaniha, M. , Robinson, E. , Rocklöv, J. , Saxer, O. , Schütte, S. , Semenza, J. C. , Shumake‐Guillemot, J. , Steinbach, R. , Tabatabaei, M. , Tomei, J. , Trinanes, J. , Wheeler, N. , Wilkinson, P. , Gong, P. , Montgomery, H. , & Costello, A. (2018). The 2018 report of the Lancet Countdown on health and climate change: Shaping the health of nations for centuries to come. The Lancet, 392(10163), 2479–2514. 10.1016/S0140-6736(18)32594-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts, N. , Amann, M. , Ayeb‐Karlsson, S. , Belesova, K. , Bouley, T. , Boykoff, M. , Byass, P. , Cai, W. , Campbell‐Lendrum, D. , Chambers, J. , Cox, P. M. , Daly, M. , Dasandi, N. , Davies, M. , Depledge, M. , Depoux, A. , Dominguez‐Salas, P. , Drummond, P. , Ekins, P. , Flahault, A. , Frumkin, H. , Georgeson, L. , Ghanei, M. , Grace, D. , Graham, H. , Grojsman, R. , Haines, A. , Hamilton, I. , Hartinger, S. , Johnson, A. , Kelman, I. , Kiesewetter, G. , Kniveton, D. , Liang, L. , Lott, M. , Lowe, R. , Mace, G. , Odhiambo Sewe, M. , Maslin, M. , Mikhaylov, S. , Milner, J. , Latifi, A. M. , Moradi‐Lakeh, M. , Morrissey, K. , Murray, K. , Neville, T. , Nilsson, M. , Oreszczyn, T. , Owfi, F. , Pencheon, D. , Pye, S. , Rabbaniha, M. , Robinson, E. , Rocklöv, J. , Schütte, S. , Shumake‐Guillemot, J. , Steinbach, R. , Tabatabaei, M. , Wheeler, N. , Wilkinson, P. , Gong, P. , Montgomery, H. , & Costello, A. (2018). The Lancet Countdown on health and climate change: From 25 years of inaction to a global transformation for public health. The Lancet, 391(10120), 581–630. 10.1016/S0140-6736(17)32464-9 [DOI] [PubMed] [Google Scholar]
- Weisberg, R. H. , Zheng, L. , Liu, Y. , Corcoran, A. A. , Lembke, C. , Hu, C. , Lenes, J. M. , & Walsh, J. J. (2016). Karenia brevis blooms on the West Florida Shelf: A comparative study of the robust 2012 bloom and the nearly null 2013 event. Continental Shelf Research, 120, 106–121. 10.1016/j.csr.2016.03.011 [DOI] [Google Scholar]
- Wilkins, J. L. , Pouliot, G. , Foley, K. , Appel, W. , & Pierce, T. (2018). The impact of U.S. wildland fires on ozone and particulate matter: A comparison of measurements and CMAQ model predictions from 2008 to 2012. International Journal of Wildland Fire, 27(10), 684 10.1071/WF18053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, S. , Mickley, L. J. , Leibensperger, E. M. , Jacob, D. J. , Rind, D. , & Streets, D. G. (2008). Effects of 2000–2050 global change on ozone air quality in the United States. Journal of Geophysical Research, 113(D6). 10.1029/2007JD008917 [DOI] [Google Scholar]
- Wuebbles, D. J. , Fahey, D. W. , & Hibbard, K. A. (2017). Climate science special report: Fourth National Climate Assessment, Volume I. Retrieved from https://repository.library.noaa.gov/view/noaa/19486/noaa_19486_DS1.pdf
- Xiao, J. , Huang, M. , Zhang, W. , Rosenblum, A. , Ma, W. , Meng, X. , & Lin, S. (2019). The immediate and lasting impact of Hurricane Sandy on pregnancy complications in eight affected counties of New York State. Science of the Total Environment, 678, 755–760. 10.1016/j.scitotenv.2019.04.436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yango, A. F. , Fischbach, B. V. , Levy, M. , Chandrakantan, A. , Tan, V. , Spak, C. , Melton, L. , Rice, K. , Barri, Y. , Rajagopal, A. , & Klintmalm, G. (2014). West Nile virus infection in kidney and pancreas transplant recipients in the Dallas‐Fort Worth Metroplex during the 2012. Texas epidemic: Transplantation, 1 10.1097/01.tp.0000438621.81686.ab [DOI] [PubMed] [Google Scholar]
- Ziska, L. , Knowlton, K. , Rogers, C. , Dalan, D. , Tierney, N. , Elder, M. A. , Filley, W. , Shropshire, J. , Ford, L. B. , Hedberg, C. , Fleetwood, P. , Hovanky, K. T. , Kavanaugh, T. , Fulford, G. , Vrtis, R. F. , Patz, J. A. , Portnoy, J. , Coates, F. , Bielory, L. , & Frenz, D. (2011). Recent warming by latitude associated with increased length of ragweed pollen season in central North America. Proceedings of the National Academy of Sciences, 108(10), 4248–4251. 10.1073/pnas.1014107108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziska, L. H. , Makra, L. , Harry, S. K. , Bruffaerts, N. , Hendrickx, M. , Coates, F. , Saarto, A. , Thibaudon, M. , Oliver, G. , Damialis, A. , Charalampopoulos, A. , Vokou, D. , Heiđmarsson, S. , Guđjohnsen, E. , Bonini, M. , Oh, J. W. , Sullivan, K. , Ford, L. , Brooks, G. D. , Myszkowska, D. , Severova, E. , Gehrig, R. , Ramón, G. D. , Beggs, P. J. , Knowlton, K. , & Crimmins, A. R. (2019). Temperature‐related changes in airborne allergenic pollen abundance and seasonality across the northern hemisphere: A retrospective data analysis. The Lancet Planetary Health, 3(3), e124–e131. 10.1016/S2542-5196(19)30015-4 [DOI] [PubMed] [Google Scholar]
- Zwiers, F. W. , Zhang, X. , & Feng, Y. (2011). Anthropogenic influence on long return period daily temperature extremes at regional scales. Journal of Climate, 24(3), 881–892. 10.1175/2010JCLI3908.1 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1


