Abstract
College students are prone to stress, making them vulnerable to cardiovascular disease (CVD). Harmful health behaviors, such as tobacco or alcohol use, further predispose students to hypertension (HTN). African-Americans (AA) experience increased blood pressure reactivity, and weathering, due to race-related stressors. This interplay makes AA college students good targets for strategies to prevent stress and HTN disease risk. This project examined the relationship between mindfulness, perceived stress and blood pressure among a group of AA college students enrolled in an HBCU healthy heart course. Participants’ systolic and diastolic blood pressure averaged 122 mmHg and 76 mmHg, respectively. The Spearman correlation revealed a negative strong relationship between mindfulness and perceived stress (rs = −0.61, p = 0.004). The coefficient of determination indicated that 37% of the variance in mindfulness was explained by perceived stress. College health practitioners should consider integrating mindfulness into course activities and expanding its treatment modality.
Keywords: African-Americans, cardiovascular disease, college students, HBCU, hypertension, mindfulness, perceived stress
INTRODUCTION
Research shows higher prevalence of stress among college students today compared to fifteen years ago (Rizer, Fagan, Kilmon, & Rath, 2016; Saleh, Camart, & Romo, 2017). According to the American College Health Association (ACHA, 2013), the majority of students complain of feeling overwhelmed by the responsibilities of college life. In response to the 2013 National College Health Assessment, one-third of US college students reported experiencing psychological distress within a one-year period (Novotney, 2014). While research suggests stress is common among college students (Baghurst & Kelley, 2014), not all share the same stressors.
For instance, African-American college students face additional stressors uniquely related to their racial and ethnic background (Greer, Ricks, & Baylor, 2015). Compared to Caucasian students, they are more prone to stress that stems from racism, discrimination, and negative life events (Gebre & Taylor, 2017; Greer et al., 2015). These factors can affect their mental and physical health, making them vulnerable to cardiovascular disease (CVD) (Bell, 2015; Greer et al., 2015). Researchers imply that African-Americans are facing a growing health crisis evidenced by increased blood pressure reactivity, and weathering, caused by race-related stressors (Beatty Moody et al., 2016).
Prolonged stress among African-American college students based on racial discrimination is identified as a chronic stressor, corroding individual protective barriers and increasing vulnerability to physical illness (Clark, Perkins, Carson, Boyd, & Jefferson, 2015). Physical and psychological stressors stimulate regions of the nervous system eliciting a response in the hypothalamic-pituitary-adrenal (HPA) axis and autonomic nervous system that results in the stress response, or fight-or-flight response. Necessary in emergencies or brief endangerment, constant release of stress hormones (cortisol and catecholamine) and related unhealthy behaviors can have adverse cardiovascular effects. Elevated stress hormone levels result in platelet hyperactivity, vascular inflammation, vasoconstriction, oxidative stress, endothelial dysfunction, elevated blood pressure, and elevated heart rate. Additionally, college students affected by stress may engage in unhealthy behaviors, such as overeating, inactivity, smoking, and drinking alcohol (American Heart Association [AHA], 2015; Golbidi, Frisbee, & Laher, 2015). Physiologic responses coupled with harmful health behaviors can predispose students to CVD development.
Cardiovascular disease is the leading cause of death for adults in the United States (Melnyk, Panza, Zaleski, & Taylor, 2015), and the fifth leading cause of death among young adults 15 to 34 years of age in North Carolina (Lai, Ward, & Bolin, 2015). Moreover, CVD remains one of the leading causes of death among African-Americans (Centers for Disease Control and Prevention [CDC], 2018; Holland, Carthron, Duren-Winfield, & Lawrence, 2014). Each year CVD is responsible for an estimated 17.5 million deaths, accounting for 31 percent of all deaths globally (World Health Organization [WHO], 2018). Researchers are certain that the number of deaths can be reduced by modifying the risk factors that lead to CVD (Barnes, Kapuku, & Treiber, 2012).
The most common risk factor for CVD is HTN (Grant, Hobkirk, Persons, Hwang, & Danoff-Burg, 2013), and HTN prevalence among Africn-Americans is the highest in the world (AHA, 2015). Approximately 70 million adults in America have HTN, which results in an average total healthcare cost of $48.6 billion annually (CDC, 2016). Researchers suggest that the disproportionate prevalence of HTN among African-Americans is due to stress, a known aggravating risk factor (Coulon et al., 2016; Woods-Giscombé & Gaylord, 2014).
Younger populations are not spared from the risk factors leading to this disease, indicating increased morbidity and decreased productivity in future generations (Nyombi et al., 2016). Current reports indicate that HTN prevalence among college-aged populations is higher than reported clinically (Egan & Moreno, 2011; Jain & Verma, 2016). More than half of adults aged 18 to 24 years have at least one CVD risk factor that surfaced in their adolescent years (Arts, Fernandez, & Lofgren, 2014). Despite these findings, their CVD risk is underestimated. Young college students are at a critical juncture, when understanding their risk and making sound lifestyle choices can improve their lifelong cardiovascular health (Holland et al., 2014). Scholars have suggested that health professionals on college campuses consider CVD risk assessments, such as HTN screening for students (Arts et al., 2014).
African-American college students are at increased risk of HTN given their race, ethnicity, common co-morbidities, and family history, all of which are linked to CVD. They also encounter unique combination of financial, academic, and social challenges that increase their stress level and may increase incidence of HTN (Bell, 2015; Coulon et al., 2016; Imes & Lewis, 2014; Woods-Giscombé & Gaylord, 2014). This interplay makes them prime targets for intervention strategies to prevent and reduce stress and HTN disease risk (Bell, 2015).
Mindfulness is an inexpensive, non-pharmacological, and convenient intervention. It increases attention and awareness, which has shown to decrease stress and lower blood pressure (Bell, 2015; Shearer, Hunt, Chowdhury, & Nicol, 2016). It has been used in studies similar to this project, which include a randomized controlled trial conducted by Bell (2015) to show its benefit for the physical and mental health of African-American urban residents and college students at an HBCU. It was found to reduce participants’ stress-related hypertension. Loucks et al. (2015) linked the overall ratio of high mindfulness scores to better cardiovascular health. Participants in a study by Woods-Giscombé and Gaylord (2014) reported that mindfulness helped with stress and healing management and improved relaxation and perceived health outcomes. An RCT conducted by Hughes et al. (2013) examined the effect of mindfulness on blood pressure and found that participants with the highest baseline blood pressure had the greatest reductions.
The correlation between stress and HTN among college students is clear (Shearer et al., 2016), but non-pharmacological interventions are lacking (Bell, 2015). African-American college students need ways to manage stress and decrease their risk of developing pre-HTN or HTN and other manifestations of CVD. Evidence shows that mindfulness meditation improved stress and lowered blood pressure. The purpose of this project was to examine the relationship between mindfulness, perceived stress, and blood pressure among a group of African-American college students enrolled in a healthy heart course at an HBCU.
This project was guided by Betty Neuman’s Health-Care Systems Model. This framework acknowledges the relationship between the stressed students and their ability to recover from stress (Ahmadi & Sadeghi, 2017). It addressed participants as a core system with unique variables, such as genetic, organ health, cognitive ability, and physical strength (Neuman & Young, 1972; Reed, 1993). It posits three concentric rings around an individual that are flexible lines of defense. These lines may be threatened during a stressful encounter in individuals with lower levels of mindfulness, who may then experience higher levels of stress.
METHODS
Design
The project used a cross-sectional, descriptive, correlational design to evaluate the correlations among mindfulness, perceived stress, and blood pressure among a group of African-American college students enrolled in a healthy heart course at an HBCU. The study was approved by University’s Institutional Review Board and fully supported by the course instructor.
Sample and Setting
The project was conducted on the campus of a Southeastern US HBCU. Participants included a convenience sample of African-American male and female undergraduate students (n = 20) enrolled in a healthy heart education course designed to teach students how to calculate CVD risk factors and understand how lifestyle behaviors contribute to chronic disease risk. At a designated class session, the instructor notified students of the option to participate. They were recruited using an in-class flyer, email, and the learning management system. The principal investigator was available during a designated class session to answer questions, obtain informed consent, and complete assessment measures.
Students who self-reported to be of African-American race, aged 18–25 years, and enrolled as a student in the health education course were included. Self-identified non African-American students were offered the opportunity to engage to avoid any perception of partiality, yet their data was excluded from analysis. The exclusion criteria were self-reported cognitive impairment consistent with the scientific reasoning that self-administered tasks are complex undertakings (Taylor, DeMers, Vig, & Borson, 2012).
Recruitment
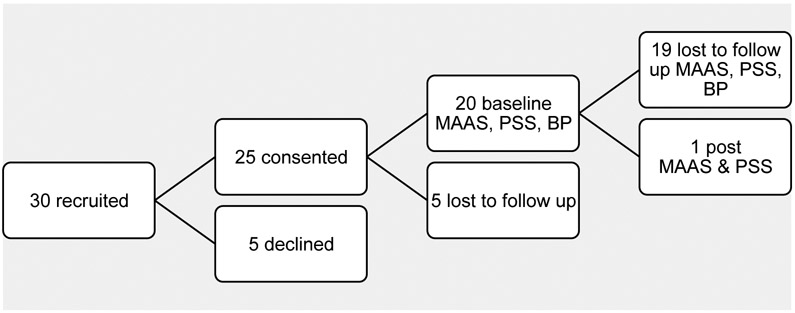
A total of 30 students were invited to participate using a recruitment flyer shared electronically by the course instructor. Of the 30 students, 25 consented either in class or online, and 20 completed the assessment measures. Participants were given a mindfulness meditation script that provided step-by-step instructions on how to perform self-directed mindfulness. It is available at no cost from the Mindful Awareness Research Center at the University of California. Participants were encouraged to practice mindfulness five minutes daily, but the opportunity to assess MAAS, PSS, and blood pressure at a later date was constrained due to attrition (see Figure 1).
Figure 1.
Flow Chart of the Participants’ Recruitment
Outcome Measures
Mindfulness was assessed using the Mindful Attention Awareness Scale (MAAS), evaluating 15 items according to a six-point Likert scale from “1” meaning almost always to “6” meaning almost never. MAAS is specifically designed to assess open or receptive awareness, which is a core characteristic of dispositional mindfulness (Brown & Ryan, 2003). The internal consistency levels (Cronbach’s alpha) range from 0.80 to 0.90 (Brown & Ryan, 2003); its test-retest reliability is 0.81 (Park, Reilly-Spong, & Gross, 2013). The scale is scored by computing a mean average of the 15 items; higher scores reflect higher levels of mindfulness (Brown & Ryan, 2003).
Perceived stress was captured using the Perceived Stress Scale (PSS). The 10-item questionnaire measures of the degree to which life situations are appraised as stressful (Cohen, Kamark, & Mermelstein, 1983). Scores range from low (0 – 13) to moderate (14 – 26) to high (27 – 40). This tool has a Cronbach’s alpha = 0.84 when assessed in college students (Cohen et al., 1983).
Systolic and diastolic blood pressures were measured using a sphygmomanometer and stethoscope to obtain a manual reading. Readings were obtained by gently palpating the anterior aspect of the elbow to position the sphygmomanometer cuff. The bell of the stethoscope was placed over the brachial artery using light pressure to assure a good seal. The 2014 Eighth Joint National Committee classifications accepted by the American Heart Association (AHA, 2015) were used as a reference point at the time of assessment. Normal blood pressure are lower than 120/80 mmHg; pre-hypertension is a blood pressure consistently ranging from 120–139/80–89 mmHg; stage-1 hypertension consistently ranges from 140–159/90–99 mmHg; and stage 2 hypertension consistently ranges above 160/100 mmHg. Hypertensive crisis is a blood pressure above 180/110 mmHg.
Data Collection and Analysis
Students completed a demographic survey capturing data on social demographics, their own medical history, their parents’ medical history, and lifestyle-related cardiovascular risks such as tobacco and alcohol use. They then completed the MAAS and PSS. All forms and surveys were completed either in class or online using a survey software tool. The course instructor posted a link to the online items using a web-based learning management system and also emailed the web link to students. Hard copies of the forms were provided during a scheduled class session that coincided with the date the electronic items were posted and emailed. Data were collected during or within one day of the class session. The one-day window accommodated students who were absent during the initial class session but otherwise eligible to participate. Blood pressure measured in class, and students were given results and interpretation.
Primary data analysis used descriptive statistics for the following outcome variables: categorical variables (e.g., gender, risk history, and family risk history), reporting frequencies and percentages, and continuous variables (e.g., age, SBP, and DBP) reporting the mean, standard deviation, minimum, and maximum. The MAAS questionnaire responses were scored using six-point Likert-type scale, and the PSS, a four-point Likert scale. Subanalyses for the PSS and MAAS were conducted to understand how students respond to questions using the Likert scale, with frequencies and percentages reported. MAAS and PSS scores were reported as mean, standard deviation, minimum, and maximum. Bivariate correlation analysis (Spearman correlation) was used to examine the relationship between MAAS and PSS, MAAS and SBP, and MAAS and DBP to understand its strength and direction and the contribution of the variance (coefficient of determination) to the outcome (MAAS) by PSS, SBP, and DBP. All data analysis was conducted using SPSS version 24.0 (IBM Corp., 2016) with a statistical significance set at p < 0.05.
RESULTS
Demographics
Demographic characteristics of study participants reflected the overall composition of the health education course. In total, the undergraduate African-American sample was n = 20. All participants self-identified as non-Hispanic African-American ethnicity; 14 (59%) were women, and 6 men. The mean age was 19.8 years; the minimum reported age was 18 and the maximum 21 years.
Tobacco/Alcohol Use
Of the total, 1 of 20 reported tobacco use and 5 of 20 reported alcohol use. Four reported parental use of tobacco, and 7, parental alcohol use.
Medical History
The majority did not report medical history, but one reported hypertension. In terms of parental medical history, 4 cited hyperlipidemia; 6 diabetes; and 10, hypertension. Of this entire sample, 8 self-reported co-morbidities among their parents.
Blood Pressure
SBP values ranged from 108 to 142 (M = 124 mmHg, SD = 2.48), and DBPs ranged from 60 – 115 (M = 77 mmHg, SD = 2.69). In terms of classification frequency, 7 students fell within normal range; 9 within the pre-hypertensive stage; 3 within the stage 1 HTN category; no students were classified as stage 2; but 1 fell within the hypertensive crisis category.
Mindfulness
The overall mean and standard deviation for MAAS score of the total sample were (M = 3.62, SD = 1.69; see Table 1). Most (n = 9; 45%) reported “almost never“ to the statement “I drive places on automatic pilot, and then wonder why I went there.” Seven (35%) responded “very infrequently” to the questions, “I tend not to notice feelings of physical tension or discomfort until they really grab my attention” and “It seems I am running on automatic, without much awareness of what I’m doing.”
Table 1.
Mindfulness Attention Awareness Scale, n = 20
| AA * | VF * | SF * | SI * | VI * | AN * | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Questions | n | % | n | % | N | % | n | % | n | % | n | % | Mean | SD |
| I could be experiencing some emotion and not be conscious of it until sometime later | 1 | 5 | 1 | 5 | 2 | 10 | 7 | 35 | 5 | 25 | 4 | 20 | 4.3 | 1.34 |
| I break or spill things because of carelessness, not paying attention, or thinking of something else | 2 | 10 | 0 | 0 | 1 | 5 | 3 | 15 | 8 | 40 | 6 | 30 | 4.65 | 1.5 |
| I find it difficult to stay focused on what’s happening in the present | 2 | 10 | 2 | 10 | 5 | 25 | 4 | 20 | 3 | 15 | 4 | 20 | 3.8 | 1.61 |
| I tend to walk quickly to get where I’m going without paying attention to what I experience along the way | 4 | 20 | 4 | 20 | 5 | 25 | 2 | 10 | 3 | 15 | 2 | 10 | 3.1 | 1.65 |
| I tend not to notice feelings of physical tension or discomfort until they really grab my attention | 4 | 20 | 1 | 5 | 1 | 5 | 4 | 20 | 7 | 35 | 3 | 15 | 3.9 | 1.77 |
| I forget a person’s name almost as soon as I’ve been told it for the first time | 4 | 20 | 2 | 10 | 4 | 20 | 3 | 15 | 2 | 10 | 5 | 25 | 3.6 | 1.88 |
| It seems I am running on automatic, without much awareness of what I’m doing | 4 | 20 | 2 | 10 | 1 | 5 | 3 | 15 | 7 | 35 | 3 | 15 | 3.8 | 1.82 |
| I rush through activities without being really attentive to them | 4 | 20 | 1 | 5 | 3 | 15 | 4 | 20 | 6 | 30 | 2 | 10 | 3.65 | 1.69 |
| I get so focused on the goal I want to achieve that I lose touch with what I’m doing right now to get there | 5 | 25 | 1 | 5 | 7 | 35 | 2 | 10 | 4 | 20 | 1 | 5 | 3.1 | 1.59 |
| I do jobs or tasks automatically, without being aware of what I’m doing | 6 | 30 | 3 | 15 | 3 | 15 | 3 | 15 | 3 | 15 | 2 | 10 | 3 | 1.78 |
| I find myself listening to someone with one ear, doing something else at the same time | 6 | 30 | 4 | 20 | 3 | 15 | 4 | 20 | 2 | 10 | 1 | 5 | 2.75 | 1.59 |
| I drive places on automatic pilot and then wonder why I went there | 5 | 25 | 1 | 5 | 0 | 0 | 3 | 15 | 2 | 10 | 9 | 45 | 4.15 | 2.13 |
| I find myself preoccupied with the future or the past | 4 | 20 | 2 | 10 | 7 | 35 | 5 | 25 | 1 | 5 | 1 | 5 | 3 | 1.38 |
| I find myself doing things without paying attention | 4 | 20 | 2 | 10 | 3 | 15 | 4 | 20 | 4 | 20 | 3 | 15 | 3.55 | 1.76 |
| I snack without being aware that I’m eating | 5 | 25 | 0 | 0 | 2 | 10 | 4 | 20 | 4 | 20 | 5 | 25 | 3.85 | 1.93 |
| Overall Mindfulness | 3.62 | 1.69 |
AA: Almost Always, VF: Very Frequently, SF: Somewhat Frequently, SI: Somewhat Infrequently, VI: Very Infrequently, AN: Almost Never
Perceived Stress
The mean and SD for the total sample in this study were M = 2.03, SD = 1.1 (see Table 2). The majority (n = 13; 65%) reported “sometimes” to, “In the last month, how often have you felt that things were going your way?” Eleven (55%) reported “sometimes” to, “In the last month, how often have you found that you could not cope with all the things that you had to do?” and “In the last month, how often have you felt that you were on top of things?”
Table 2.
Perceived Stress Scale, n = 20
| Never |
Almost
Never |
Sometimes |
Fairly
Often |
Very Often |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Questions | n | % | n | % | n | % | n | % | n | % | Mean | SD |
| In the last month, how often have you been upset because of something that happened unexpectedly? | 1 | 5 | 2 | 10 | 7 | 35 | 6 | 30 | 4 | 20 | 2.50 | 1.1 |
| In the last month, how often have you felt that you were unable to control the important things in your life? | 2 | 10 | 4 | 20 | 6 | 30 | 3 | 15 | 5 | 25 | 2.25 | 1.33 |
| In the last month, how often have you felt nervous and “stressed”? | 1 | 5 | 2 | 10 | 3 | 15 | 6 | 30 | 8 | 40 | 2.90 | 1.21 |
| In the last month, how often have you felt confident about your ability to handle your personal problems? | 3 | 15 | 9 | 45 | 7 | 35 | 0 | 0 | 1 | 5 | 1.35 | 0.93 |
| In the last month, how often have you felt that things were going your way? | 0 | 0 | 3 | 15 | 13 | 65 | 3 | 15 | 1 | 5 | 2.10 | 0.72 |
| In the last month, how often have you found that you could not cope with all the things that you had to do? | 2 | 10 | 2 | 10 | 11 | 55 | 3 | 15 | 2 | 10 | 2.05 | 1.05 |
| In the last month, how often have you been able to control irritations in your life? | 3 | 15 | 6 | 30 | 8 | 40 | 1 | 5 | 2 | 10 | 1.65 | 1.14 |
| In the last month, how often have you felt that you were on top of things | 3 | 15 | 4 | 20 | 11 | 55 | 1 | 5 | 1 | 5 | 1.65 | 1 |
| In the last month, how often have you been angered because of things that were outside of your control? | 1 | 5 | 5 | 25 | 5 | 25 | 5 | 25 | 4 | 20 | 2.30 | 1.22 |
| In the last month, how often have you felt difficulties were piling up so high that you could not overcome them? | 3 | 15 | 3 | 15 | 8 | 40 | 2 | 10 | 4 | 20 | 2.05 | 1.32 |
| Overall Perceived Stress | 2.03 | 1.1 | ||||||||||
Correlation of Mindfulness, Perceived Stress, and Blood Pressure
Spearman correlation analysis was used for nonparametric data and revealed a strong negative relationship between MAAS scores and PSS scores (rs = −0.61, p = 0.004). The coefficient of determination indicated that 37% of the variance in mindfulness attention awareness is explained by perceived stress. There was a very weak negative relationship between the MAAS with SBP scores (rs = −0.049) and a moderate positive relationship between the MAAS and DBP scores (r = 0.42); neither relationship was significant. Both the very weak negative relationship between PSS and SBP (rs= −0.08) and PSS and DBP (rs = −0.075) were significant (see Table 3).
Table 3.
Spearman Correlation for Perceived Stress Scale, Mindfulness Attention Awareness Scale, Systolic Blood Pressure, and Diastolic Blood Pressure, n = 20
|
Perceived
Stress Scale |
Mindfulness
Attention Awareness Scale |
Systolic
Blood Pressure |
Diastolic
Blood Pressure |
|||
|---|---|---|---|---|---|---|
| Spearman’s | Perceived | Correlation | 1 | −0.61** | −0.08 | −0.075 |
| rho | Stress Scale | Coefficient | ||||
| Sig. (2-tailed) | . | 0.004 | 0.738 | 0.753 | ||
| Mindfulness | Correlation | - | 1 | −0.049 | 0.42 | |
| Attention | Coefficient | |||||
| Awareness | Sig. (2-tailed) | - | . | 0.839 | 0.062 | |
| Scale | ||||||
| Systolic | Correlation | - | ||||
| Blood | Coefficient | |||||
| Pressure | Sig. (2-tailed) | - | - | 1 | 0.282 | |
| - | - | . | 0.229 | |||
| Diastolic | Correlation | - | - | - | 1 | |
| Blood | Coefficient | |||||
| Pressure | Sig. (2-tailed) | - | - | - | . | |
| - | - | - | . |
Correlation is significant at the 0.01 level (2-tailed)
DISCUSSION
Results reinforce the need for innovative strategies to decrease CVD risk among African-American college students. Nonmodifiable risk factors were similar to those in other studies: race, ethnicity, medical history and co-morbidities. Recent studies (Bell, 2015; Coulon et al., 2016; Woods-Giscombé & Gaylord, 2014) continue to identify these risks as contributing factors for the disproportionate prevalence of CVD affecting African-Americans. Familial history of CVD is a well-documented, nonmodifiable genetic predisposition.
Modifiable risk factors found in this sample are comparable to those reported in the literature (Greer et al., 2015; Holland et al., 2014) and include alcohol use, tobacco use, and elevated blood pressure. The stress of college life likely results in poor behavior choices, such as overeating and inactivity, which further increase CVD risk (Bell, 2015; Lee, Corneille, Hall, Yancu, & Myers, 2016). With the updated 2017 blood pressure guidelines, more students are now classified in a higher risk category, and more would be assigned to the stage 2 category (American College of Cardiology, 2017).
Hence, nonmodifiable risks were significant, but modifiable lifestyle behaviors played a key role in the sample’s CVD risk. The highest self-reported modifiable risk among the students and their parents was alcohol use; oddly, a higher percentage of female students reported alcohol use. Still, the overall study population was in good health. Only one student reported a history of HTN, though half of the total sample reported that their parents had HTN. The self-reported hypertensive participant was a woman, and in similar findings (Lai et al., 2015), African-American women were at higher risk for elevated blood pressure. On the other hand, both female and male students had either systolic or diastolic blood pressure results that fall within the hypertensive ranges and also reported a parental history of two or more CVD risks. This finding is consistent with previous studies (Bell, 2015; Coulon et al., 2016; Imes & Lewis, 2014; Woods-Giscombé & Gaylord, 2014) that report a relationship between a family history of CVD and CVD risk.
The most important project outcome demonstrated a significant, strong, negative relationship between MAAS and PSS scores. The coefficient of determination indicated that 37% of the variance in mindfulness attention awareness in college students is explained by perceived stress. Higher levels of mindfulness were associated with lower levels of perceived stress. A similar study conducted by Shearer, Hunt, Chowdhury, and Nicol (2016) reported a significant relationship between mindfulness and stress responses, reinforcing the great benefits of mindfulness for relieving stress.
In contrast, a very weak, negative, nonsignificant relationship was found between mindfulness and SBP, while a moderate positive relationship between mindfulness and DBP, was still not significant. This finding differs from a study by Bell (2015) that looked at similar variables and found a significant relationship between mindfulness and DBP. A pre-post analysis is needed to fully evaluate the outcome variables. The relationship between PSS scores and both SBP and DBP were negative, very weak, and not significant, consistent with a study by Coulon et al. (2016).
The purpose of this project was to examine the relationship between mindfulness, perceived stress, and blood pressure among a group of African-American college students in a healthy heart course at an HBCU. Although, none of the participants fell in the low stress category, those who fell in the moderate stress category had higher mindfulness awareness scores than those in the high stress category. Higher mindfulness levels serve as lines of resistance to perceived stress and align with Neuman’s theoretical model. Mindfulness, as primary and secondary intervention to prevent stress and blood pressure elevation, may serve as a line of defense and resistance.
Limitations
The main limitations of the project were the use of convenience sampling and the small sample size. Participants were chosen through convenience sampling and not randomly selected, creating opportunity for sample bias and an inability to generalize the findings. Also, the small sample size may have limited the ability to compare the group differences among male and female participants. In terms of strengths, the project was very cost-effective and used technology for convenient survey and form completion. As a possible intervention, mindfulness does not require special training and can be self-administered.
Recommendations and Implications
Future research should be conducted at the beginning of the semester, when students are not so burdened with end-of-semester deadlines. This approach might increase student participation and completion of postassessments. Conducting the project at the beginning of the semester would also allow the researcher to examine the outcome variables over a longer period of time. Other recommendations are to allot more class time to conducting pre- and post-blood pressure assessments. Further evaluation of blood pressure classification shifts might warrant more recommendations for lifestyle modification and medication therapies. Assessing whether the subjects have prior experience with meditation or are participating in other stress intervention program prior to initial data collection would also be wise. Additionally, a survey to identify the source of student stress would be valuable.
The study has many practice and policy implications. Student health center providers (doctors, nurse practitioners, nurses, counselors, and psychologists) should screen students for perceived stress levels and offer mindfulness as a technique to relieve stress, anxiety, and stress-related health conditions like HTN. At orientation, first-year students could be invited to discuss college-related stress and management solutions that include mindfulness. Moreover, enlisting faculty to incorporate brief mindfulness meditation sessions into course activities before tests might offer an additional coping measure. Lastly, project findings may help to garner support to expand use of mindfulness as a stress management technique in primary care settings.
CONCLUSION
This study demonstrates a relationship between higher levels of mindfulness and lower levels of perceived stress, suggesting mindfulness sessions may be beneficial. It is important to encourage college students to explore mindfulness practices that may yield significant health benefits. This project contributes new information on the interplay of mindfulness, stress, and blood pressure in African-American college students. Given their CVD risk profile, effective and complimentary innovations to improve physical and mental health are sorely needed. Mindfulness may be a sensible, culturally relevant, and cost-effective strategy to manage stress in African-American college students. However, it should be embedded in an appropriate course near the start of the semester, not the end, when students are overburdened.
ACKNOWLEDGMENTS
The authors would like to acknowledge the study participants from the health-education course, whose support was critical to the success of this project.
This project was funded by a grant from the National Institutes of Health (Grant Number: R15MD010194; Vanessa Duren-Winfield, PhD, MS and Amanda Alise Price, PhD, Principal Investigators).
REFERENCES
- Ahmadi Z, & Sadeghi T (2017). Application of the Betty Neuman systems model in the nursing care of patients/clients with multiple sclerosis. Multiple Sclerosis Journal - Experimental, Translational and Clinical, 3(3), 2055217317726798. doi: 10.1177/2055217317726798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Cardiology. (2017). New ACC/AHA high blood pressure guidelines lower definition of hypertension. Retrieved from https://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017
- American College Health Association [ACHA]. (2013). American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2013. Hanover, MD: American College Health Association. Retrieved from http://www.acha-ncha.org/docs/acha-ncha-ii_referencegroup_executivesummary_spring2013.pdf [Google Scholar]
- American Heart Association. (2015). African Americans and heart disease, stroke. Retrieved from http://www.heart.org/HEARTORG/Conditions/More/MyHeartandStrokeNews/AfricanAmericans-and-Heart-Disease_UCM_444863_Article.jsp#.WbivpNGQzIU
- Arts J, Fernandez ML, & Lofgren IE (2014). Coronary heart disease risk factors in college students. Advances in Nutrition, 5(2), 177–187. doi: 10.3945/an.113.005447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baghurst T, & Kelley BC (2014). An examination of stress in college students over the course of a semester. Health Promotion Practice, 15(3), 438–447. doi: 10.1177/1524839913510316 [DOI] [PubMed] [Google Scholar]
- Barnes VA, Kapuku GK, & Treiber FA (2012). Impact of transcendental meditation on left ventricular mass in African American adolescents. Evidence-Based Complementary and Alternative Medicine (eCAM), 2012, 923153. doi: 10.1155/2012/923153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beatty Moody DL, Waldstein SR, Tobin JN, Cassells A, Schwartz JC, & Brondolo E (2016). Lifetime racial/ethnic discrimination and ambulatory blood pressure: The moderating effect of age. Health Psychology, 35(4), 333–342. doi: 10.1037/hea0000270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell TP (2015). Meditative practice cultivates mindfulness and reduces anxiety, depression, blood pressure, and heart rate in a diverse sample. Journal of Cognitive Psychotherapy, 29(4), 343–355. doi: 10.1891/0889-8391.29.4.343 [DOI] [PubMed] [Google Scholar]
- Brown KW, & Ryan RM (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. doi: 10.1037/0022-3514.84.4.822 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control [CDC]. (2016). High blood pressure fact sheet. Retrieved from https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_bloodpressure.htm
- Centers for Disease Control [CDC]. (2018). Heart disease and stroke. Retrieved from http.www.cdc.gov/chronicdisease/resources/publications/aag/heart-disease-stroke.htm
- Clark VR, Perkins P, Carson BL, Boyd K, & Jefferson TM (2015). Fasting serum glucose and cholesterol as predictors of cardiovascular reactivity to acute stress in a sample of African American college students. Ethnicity & Disease, 25(2), 175–179. [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. doi: 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Coulon SM, Wilson DK, Van Horn ML, Hand GA, & Kresovich S (2016). The association of neighborhood gene-environment susceptibility with cortisol and blood pressure in African-Americans adults. Annals of Behavioral Medicine, 50(1), 98–107. doi: 10.1007/s12160-015-9737-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan KG, & Moreno MA (2011). Prevalence of stress references on college freshmen Facebook profiles. CIN: Computers, Informatics, Nursing, 29(10), 586–592. doi: 10.1097/NCN.0b013e3182160663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebre A, & Taylor RD (2017). Association of poor kin relations, college adjustment and psychological well-being among African American undergraduates. Journal of Child and Family Studies, 26(1), 217–224. doi: 10.1007/s10826-016-0539-x [DOI] [Google Scholar]
- Golbidi S, Frisbee JC, & Laher I (2015). Chronic stress impacts the cardiovascular system: Animal models and clinical outcomes. American Journal of Physiology, 308(12), H1476–H1498. doi: 10.1152/ajpheart.00859.2014 [DOI] [PubMed] [Google Scholar]
- Grant C, Hobkirk A, Persons E, Hwang V, & Danoff-Burg S (2013). Cardiovascular reactivity to and recovery from stressful tasks following a mindfulness analog in college students with a family history of hypertension. The Journal of Alternative and Complementary Medicine, 19(4), 341–346. doi: 10.1089/acm.2011.0880 [DOI] [PubMed] [Google Scholar]
- Greer TM, Ricks J, & Baylor AA (2015). The moderating role of coping strategies in understanding the effects of intragroup race-related stressors on academic performance and overall levels of perceived stress for African American students. Journal of Black Psychology, 41 (6), 565–585. doi: 10.1177/0095798414560018 [DOI] [Google Scholar]
- Holland C, Carthron DL, Duren-Winfield V, & Lawrence W (2014). An experiential cardiovascular health education program for African American college students. ABNF Journal, 25(2), 52–56. [PubMed] [Google Scholar]
- Hughes JW, Fresco DM, Myerscough R, van Dulmen M, Carlson LE, & Josephson R (2013). Randomized controlled trial of mindfulness-based stress reduction for prehypertension. Psychosomatic Medicine, 75(8), 721–728. doi: 10.1097/PSY.0b013e3182a3e4e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imes CC, & Lewis FM (2014). Family history of cardiovascular disease, perceived cardiovascular disease risk, and health-related behavior: A review of the literature. The Journal of Cardiovascular Nursing, 29(2), 108–129. doi: 10.1097/JCN.0b013e31827db5eb [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0 Armonk, NY: IBM Corp. [Google Scholar]
- Jain A, & Verma S (2016). Prevalence of stress and coping strategies among college students. Journal of Advanced Medical and Dental Sciences Research, 4(6), 95–99. doi: 10.21276/jamdsr.2016.4.6.21 [DOI] [Google Scholar]
- Lai HL, Ward R, & Bolin P (2015). Cardiovascular health of North Carolina undergraduates. North Carolina Medical Journal, 76(5), 286–292. doi: 10.18043/ncm.76.5.286 [DOI] [PubMed] [Google Scholar]
- Lee AK, Corneille MA, Hall NM, Yancu CN, & Myers M (2016). The stressors of being young and Black: Cardiovascular health and Black young adults. Psychology & Health, 31(5), 578–591. doi: 10.1080/08870446.2015.1127373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loucks EB, Schuman-Olivier Z, Britton WB, Fresco DM, Desbordes G, Brewer JA, & Fulwiler C (2015). Mindfulness and cardiovascular disease risk: State of the evidence, plausible mechanisms, and theoretical framework. Current Cardiology Reports, 17(12), 112. doi: 10.1007/s11886-015-0668-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnyk JA, Panza G, Zaleski A, & Taylor B (2015). Awareness and knowledge of cardiovascular risk through blood pressure and cholesterol testing in college freshmen. American Journal of Health Education, 46(3), 138–143. doi: 10.1080/19325037.2015.1023474 [DOI] [Google Scholar]
- Neuman BM, & Young RJ (1972). A model for teaching total person approach to patient problems. Nursing Research, 21(3), 264–269. doi: 10.1097/00006199-197205000-00015 [DOI] [PubMed] [Google Scholar]
- Novotney A (2014). Students under pressure: College and university counseling centers are examining how best to serve the growing number of students seeking their services. APA Monitor, 45(8), 36. Retrieved from http://www.apa.org/monitor/2014/09/cover-pressure.aspx [Google Scholar]
- Nyombi KV, Kizito S, Mukunya D, Nabukalu A, Bukama M, Lunyera J, … Kalyesubula R (2016). High prevalence of hypertension and cardiovascular disease risk factors among medical students at Makerere University College of Health Sciences, Kampala, Uganda. BMC Research Notes, 9, 110. doi: 10.1186/s13104-016-1924-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park T, Reilly-Spong M, & Gross CR (2013). Mindfulness: A systematic review of instruments to measure an emergent patient-reported outcome (PRO). Quality of Life Research, 22(10), 2639–2659. doi: 10.1007/s11136-013-0395-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed KS (1993). The Neuman systems model: Assumptions and concepts. In Reed KS (Ed.), Betty Neuman: The Neuman systems model (pp. 7–21). Newbury Park, CA: SAGE Publications, Inc. [Google Scholar]
- Rizer CA, Fagan MH, Kilmon C, & Rath L (2016). The role of perceived stress and health beliefs on college students’ intentions to practice mindfulness meditation. American Journal of Health Education, 47(1), 24–31. doi: 10.1080/19325037.2015.1111176 [DOI] [Google Scholar]
- Saleh D, Camart N, & Romo L (2017). Predictors of stress in college students. Frontiers in Psychology, 8, 19. doi: 10.3389/fpsyg.2017.00019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shearer A, Hunt M, Chowdhury M, & Nicol L (2016). Effects of a brief mindfulness meditation intervention on student stress and heart rate variability. International Journal of Stress Management, 23(2), 232–254. doi: 10.1037/a0039814 [DOI] [Google Scholar]
- Taylor JS, DeMers SM, Vig EK, & Borson S (2012). The disappearing subject: Exclusion of people with cognitive impairment and dementia from geriatrics research. Journal of the American Geriatrics Society, 60(3), 413–419. doi: 10.1111/j.1532-5415.2011.03847.x [DOI] [PubMed] [Google Scholar]
- Woods-Giscombé CL, & Gaylord SA (2014). The cultural relevance of mindfulness meditation as a health intervention for African Americans: Implications for reducing stress-related health disparities. Journal of Holistic Nursing, 32(3), 147–160. doi: 10.1177/0898010113519010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization [WHO]. (2018). Cardiovascular disease. Retrieved from http://www.who.int/cardiovascular_diseases/en/