Abstract
Breastfeeding provides optimal nutrition for infants, including short- and longterm health benefits for baby and mother. Maternity care practices supporting breastfeeding after delivery increase the likelihood of exclusive breastfeeding. This study explores trends in early infant feeding practices by maternal race and other characteristics in Hawai‘i. Data from a linked 2008–2015 Hawai‘i Newborn Metabolic Screening and Birth Certificate file for 128 399 singleton term infants were analyzed. Early infant feeding occurring 24–48 hours after delivery and before discharge was categorized: Early formula feeding; early mixed feeding; and early exclusive breastfeeding. Differences were assessed over time by maternal race and other socio-demographic characteristics. Further assessment of maternal race included a generalized logit model adjusting for maternal age, marital status, county of residence, type of birth attendant, and birth year. Statewide, early exclusive breastfeeding increased from 58.8% in 2008 to 79.1% in 2015 (relative increase=+35%); early mixed feeding declined from 31.1% to 16.0% (relative decrease=−49%) and early formula feeding declined from 10.1% to 4.9% (relative decrease=−51%). Most maternal race subgroups experienced increases in early exclusive breastfeeding and decreases in mixed and formula. Japanese mothers were 2.15 (95%CI=1.90–2.42) and Korean mothers were 1.73 (95%CI=1.37–2.18) times more likely to practice early exclusive breastfeeding compared with white mothers. Several subgroups were less likely to practice early exclusive breastfeeding compared with white mothers. Substantial increases in early exclusive breastfeeding in Hawai‘i occurred across all subgroups. Development of culturally appropriate hospital practices, particularly in those with persistently lower estimates, could help improve early exclusive breastfeeding.
Keywords: early infant feeding, breastmilk, disparities, exclusive breastfeeding, Native Hawaiian, Other Pacific Islanders, Asians, Hawai‘i
Background
Breastfeeding is cost-effective and provides medical, nutritional, developmental, psychological, social, economic, and environmental advantages for the health of both mother and child.1 In contrast, formula-fed children may require more doctor visits and are at higher risk for childhood obesity, diabetes, asthma, and other health issues.2–4 To increase the uptake of breastfeeding, several organizations endorse its benefits. For example, the American Academy of Pediatrics, American College of Obstetricians and Gynecologists, and the American Academy of Family Physicians promote exclusive breastfeeding for approximately the first 6 months after delivery, followed by continued breastfeeding with complementary foods introduction, and ongoing support of breastfeeding for at least one year or as long as mutually desired by mother and child.5–7
The Ten-Steps to Successful Breastfeeding (Ten-Steps) is accepted as the standard of care for maternity care in hospitals in establishing and promoting breastfeeding.8–11 These steps are a set of evidence-based practices that improve the maternity care provided to patients in the hospital that support optimal breastfeeding outcomes and include: written policies; ensure appropriate training of staff; inform all pregnant women on the benefits and management of breastfeeding; timely initiation of breastfeeding; ensure women are educated on maintaining lactation; ensure no food or drink other than breast milk are provided to infants unless medically indicated; practice rooming in (sharing a bedroom with the infant); encourage breastfeeding on demand; no use of teats or pacifiers; and foster breastfeeding support groups that women can access upon discharge.9
In 2010, the Hawai‘i State Department of Health developed an initiative to promote breastfeeding using the Ten-Steps through the Baby-Friendly Hawai‘i Project. This project improves maternity care practices in the critical early postpartum period by supporting health systems through staff training and on-going technical assistance to all birthing hospitals in the State.12 In 2011 the US Surgeon General Call to Action outlined many barriers to breastfeeding. The report included a lack of maternal knowledge on the benefits of breastfeeding, social norms favorable toward formula feeding, embarrassment, lactation problems, poor family and social support, lack of supportive environments at work, and health services-related barriers.1 Health services related barriers included the early hospital experience of breastfeeding. The Call to Action included the Ten-Steps to Successful Breastfeeding (Ten-Steps) in the final recommendations.1
There are about 18 000 births annually amongst a population of nearly 1.4 million people in Hawai‘i. Hawai‘i is composed of a diverse population that may have differences in early infant feeding. Analysis of data collected in the state of Hawai‘i offers an opportunity to understand differences in breastfeeding initiation or early experience of feeding among a wide variety of racial and ethnic subgroups including Asian and Native Hawaiian or Other Pacific Islander (NHOPI) subgroups. Asians and NHOPI are a diverse population consisting of several distinct subgroups with different characteristics that include language, occupations, culture, and length of residence in the United States.13–14
A Hawai‘i Pregnancy Risk Assessment Monitoring System (PRAMS) study based on 2004–2008 data, prior to implementation of the Baby-Friendly Hawai‘i Project, highlighted that Asian and NHOPI subgroups were less likely to exclusively breastfeed at least 8 weeks compared to white mothers.15 The study highlighted differences among the Asian and NHOPI subgroups at 8 weeks. However, it is unknown whether there are differences in early infant feeding experience in the hospital at the population level among the diverse race groups in Hawai‘i.
An overall increase occurred statewide in early exclusive breastfeeding, indicated by Newborn Metabolic Screening data in Hawai‘i between 2009 and 2014, covering the time since the Baby-Friendly Hawai‘i Project started.12 However, it is unclear if these improvements were seen across various maternal race and other characteristic subgroups. The aims of this paper are to report the trends in early infant feeding practices by maternal race and other characteristics in Hawai‘i and to explore further some differences in early infant feeding practices in maternal race compared with white mothers accounting for the other characteristics.
Methods
This is a retrospective, cross-sectional descriptive secondary analysis of de-identified linked data provided to the researcher after the linkage was completed. The analysis was considered as exempt from Institutional Review Board approval by the Hawai‘i State Department of Health.
The Hawai‘i Newborn Metabolic Screening Program collects information and a blood spot specimen to identify 33 rare metabolic conditions early for appropriate counseling and referral to treatment among families with affected newborns. The Hawai‘i State Department of Health Office of Health Status and Monitoring (OHSM) collects vital statistics for the state on all births. Linkage of birth certificate and metabolic screening data based on patient identifiers (eg, names, dates, weight, times, institution) using a combination of 3–4 variables per each of 15 iterations was done by staff at OHSM. For the time period included in this manuscript, the linkage rate between the two sources was 99.4% (n=963 not linked). A de-identified analytic file covering data collected for births from 2008–2015 was provided to the researchers for analysis. A total of 150 589 births were identified in the linked data set. Information on early infant feeding was obtained from the Newborn Metabolic Screening program data while maternal race, other socio-demographic, and some clinical based information such as gestational age, birthweight, delivery method, and maternal factors complicating delivery were included in the linked OHSM birth certificate file. Analysis was limited to term singleton deliveries (gestational age ≥ 37 weeks) to minimize concerns about a multiple gestation or preterm infants having medical concerns that could influence early infant feeding. The potential samples of 132 867 were available for analysis.
The protocol for the Newborn Metabolic Screening test is to collect the blood spot specimen and other information between 24 and 48 hours post-delivery for both hospital and out of hospital births. Infant feeding information is based on an assessment of the last 24 hours at time of newborn metabolic testing. If an infant is discharged less than 24 hours after delivery, the specimen and other information is collected at time of discharge. Infant feeding practices were based on reporting at discharge. The information on infant feeding was categorized into three mutually exclusive categories used for analysis in this paper: Early exclusive breastfeeding (ie, received only human milk in the last 24 hours), early mixed feeding (ie received both human milk and formula, though not necessarily at the same time, during the last 24 hours), and early formula feeding (ie, received only infant formula in the last 24 hours). There were 4 468 excluded records with a feeding status of “Other,” Nil per Os (“NPO”) or nothing by mouth, “Tube Feeding,” or missing, resulting in the final study sample of 128 399 observations.
The Hawai‘i birth certificate collects information on all reported race groups at delivery for both parents. This information is converted to 1 of 22 single race groups by an algorithm implemented by OHSM.16 The algorithm prioritizes Hawaiian for those that list multiple race groups, followed by the first non- Caucasian race reported. Thus, those that report being Hawaiian in combination with another race group would be considered part-Hawaiian. All other multiple race groups without Hawaiian listed are coded to a single race group in the algorithm. For consistency with race reporting in Hawai‘i, this analysis combines part-Hawaiian and Hawaiian single race groups together, referred to as Native Hawaiian. The 22 maternal single race groups provided by OHSM were categorized into 9 total race groups for this analysis which reflected those commonly reported in Hawai‘i, and to ensure sufficient sample size for reliable estimates: white (Caucasian), black, Native Hawaiian (Hawaiian and part-Hawaiian), Samoan, Filipino, Japanese, Chinese, Korean, and all others (including Vietnamese, Asian Indian, Other Asian, Guamanian/Chamorro, other Pacific Islander, Puerto Rican, Portuguese, Cuban, Mexican, American Indian/Alaskan Native, all others). Maternal race was used for this analysis to be consistent with general reporting of birth outcomes by race.
Maternal age, calculated by mother's age upon birth of the infant, was categorized into the following 5 year age groups other than at tails which included commonly used categories and ensured at least 10% in the youngest group: Under 20, 20–24, 25–29, 30–34, and 35 or more years. Marital status was considered married or unmarried as reported at time of delivery on the birth certificate. Birth attendant was categorized as physician, midwife, or other. The other group may include out of hospital deliveries attended by bystanders, non-licensed providers, or where the attendant is unknown, but that specific level of detail was not available in analytic data set. Resident zip code, as collected in the birth certificate data, was used to categorize into the four counties of residence in the State.
Annual estimates for the prevalence of each feeding type and bivariate associations with maternal race, maternal age, marital status, type of birth attendant, and county of residence were calculated. Relative changes from 2008 to 2015 were calculated for each feeding type overall and among all maternal race and other subgroups. The Cochran-Armitage Trend test assesses unadjusted trends in prevalence over time for each outcome (ie, early exclusive breastfeeding, early mixed feeding, and early formula feeding) overall and among all subgroups.
To assess trends over time in each maternal race subgroup while accounting for other factors, individual generalized logit modeling determined crude and adjusted odd ratios for early exclusive breastfeeding and early mixed feeding compared with the reference group of early formula feeding for each maternal race subgroup. The models for each maternal race subgroup were performed with birth year as a primary predictor (categorical with comparison from 2015 to 2008) with adjustment for maternal age, marital status, birth attendant, and county of residence. The factors were selected based on their availability in the database and review of the general literature as possible predictors of infant feeding. For simplicity, only the results of the birth year odds ratios stratified by maternal race for early exclusive breastfeeding compared with formula feeding are shown in the manuscript.
To assess differences among maternal race subgroups for the entire time period of the study while accounting for the influence of these other factors, a generalized logit model was developed with maternal race subgroup as the primary predictor and adjustment for the other factors noted previously for the trend model along with using birth year as a categorical variable. SAS version 9.4 (SAS Institute, Inc., Cary, North Carolina) was used for analysis with a two-tailed P-value of <.05 considered statistically significant.
Results
Within the final analytic sample (N=128,399), nearly two-thirds of births were to mothers who identified within the three following race groups: Native Hawaiian (26.8%), white (23.7%), and Filipino (16.9%; Table 1). Over half the births were to mothers who were 25–29 (28.1%) or 30–34 (25.3%) years of age. Nearly two-thirds of the births were to married (62.7%) mothers and nearly all births were delivered by a physician (89.6%). Nearly three-quarters of the births in the sample were to mothers residing in Honolulu County (71.9%).
Table 1.
Maternal Race and Other Characteristics, 2008–2015 (N=128 399)
| Characteristic | n | % |
|---|---|---|
| Maternal Race | ||
| white | 30 370 | 23.7 |
| black | 3 503 | 2.7 |
| Native Hawaiian | 34 326 | 26.8 |
| Samoan | 3 325 | 2.6 |
| Filipino | 21 683 | 16.9 |
| Japanese | 12 031 | 9.4 |
| Chinese | 5 486 | 4.3 |
| Korean | 2 377 | 1.9 |
| All othersa | 15 048 | 11.7 |
| Missing | 250 | |
| Maternal Age | ||
| <20 years | 12 810 | 10.0 |
| 20–24 years | 24 607 | 19.2 |
| 25–29 years | 36 046 | 28.1 |
| 30–34 years | 32 499 | 25.3 |
| 35 years and older | 22 330 | 17.4 |
| Missing | 107 | |
| Marital Status | ||
| Married | 80 518 | 62.7 |
| Unmarried | 47 878 | 37.3 |
| Missing | 3 | |
| County of Residence | ||
| Hawai‘i | 16 281 | 12.9 |
| Honolulu | 90 605 | 71.9 |
| Kaua‘i | 5 634 | 4.5 |
| Maui | 13 528 | 10.7 |
| Missing | 2 351 | |
Notes: Data source is the Newborn Metabolic Screening-Linked Birth Certificate File. Individual subgroup column totals may not sum to overall total due to missing/unknown data and row percentages may not sum to 100% due to rounding.
All others include Vietnamese, Asian Indian, other Asian, Guamanian/Chamorro, other Pacific Islander, Puerto Rican, Portuguese, Cuban, Mexican, American Indian/Alaskan Native, and all others.
Statewide, the prevalence of early exclusive breastfeeding increased from 58.8% in 2008 to 79.1% in 2015 (a relative increase of +35%; Table 2). Early exclusive breastfeeding increased among all maternal race groups with Samoan mothers having the largest relative increase (+71%), followed by all others (+54%), Filipino (+49%), and Native Hawaiian (+44%) mothers (Table 2 and Figure 1). Increases in early exclusive breastfeeding were also seen across all characteristic subgroups categorized by maternal age, marital status, birth attendant, and county of residence (Table 2).
Table 2.
Relative Changes in Early Infant Feedinga by Maternal Race and Other Characteristics, 2008–2015
| Characteristic | Early Exclusive Breastfeeding | Early Mixed Feeding | Early Formula Feeding | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2008 % |
2015 % |
Relative Changeb |
Trend P−valuec |
2008 % |
2015 % |
Relative Change |
Trend P−value |
2008 % |
2015 % |
Relative Change |
Trend P−value |
|
| Maternal Race | ||||||||||||
| white | 75.9 | 87.7 | 16% | <.001 | 16.1 | 8.8 | −45% | <.001 | 7.9 | 3.5 | −56% | <.001 |
| black | 59.6 | 72.9 | 22% | <.001 | 25.5 | 19.4 | −24% | .019 | 15.0 | 7.7 | −49% | <.001 |
| Native Hawaiian | 52.6 | 76.0 | 44% | <.001 | 33.9 | 17.5 | −48% | <.001 | 13.5 | 6.6 | −51% | <.001 |
| Samoan | 37.1 | 63.4 | 71% | <.001 | 41.1 | 26.2 | −36% | <.001 | 21.8 | 10.4 | −52% | <.001 |
| Filipino | 52.0 | 77.4 | 49% | <.001 | 38.3 | 18.0 | −53% | <.001 | 9.7 | 4.6 | −53% | <.001 |
| Japanese | 67.1 | 87.4 | 30% | <.001 | 28.3 | 11.0 | −61% | <.001 | 4.6 | 1.6 | −65% | <.001 |
| Chinese | 63.1 | 74.5 | 18% | <.001 | 28.8 | 20.7 | −28% | <.001 | 8.1 | 4.9 | −40% | <.001 |
| Korean | 66.1 | 83.9 | 27% | <.001 | 29.6 | 14.2 | −52% | <.001 | 4.3 | 1.8 | −58% | .128 |
| All othersd | 45.8 | 70.7 | 54% | <.001 | 45.2 | 24.2 | −46% | <.001 | 9.1 | 5.1 | −44% | <.001 |
| Maternal Age | ||||||||||||
| <20 years | 51.1 | 77.2 | 51% | <.001 | 37.5 | 16.2 | −57% | <.001 | 11.3 | 6.7 | −41% | <.001 |
| 20–24 years | 55.4 | 77.4 | 40% | <.001 | 32.4 | 17.0 | −48% | <.001 | 12.2 | 5.6 | −54% | <.001 |
| 25–29 years | 59.9 | 78.7 | 31% | <.001 | 29.8 | 16.5 | −45% | <.001 | 10.3 | 4.8 | −53% | <.001 |
| 30–34 years | 62.7 | 81.3 | 30% | <.001 | 28.2 | 14.6 | −48% | <.001 | 9.1 | 4.1 | −55% | <.001 |
| 35 years and older | 61.4 | 79.2 | 29% | <.001 | 31.0 | 16.3 | −47% | <.001 | 7.7 | 4.5 | −42% | <.001 |
| Marital Status | ||||||||||||
| Married | 64.2 | 81.6 | 27% | <.001 | 27.6 | 14.6 | −47% | <.001 | 8.2 | 3.8 | −54% | <.001 |
| Unmarried | 49.7 | 74.9 | 51% | <.001 | 37.0 | 18.4 | −50% | <.001 | 13.3 | 6.7 | −50% | <.001 |
| Birth Attendant | ||||||||||||
| Physician | 57.7 | 77.5 | 34% | <.001 | 32.0 | 17.4 | −46% | <.001 | 10.3 | 5.2 | −50% | <.001 |
| Midwife | 70.6 | 90.5 | 28% | <.001 | 21.8 | 6.7 | −69% | <.001 | 7.6 | 2.8 | −63% | <.001 |
| Other | 69.7 | 88.2 | 27% | .008 | 15.2 | 8.8 | −42% | .440 | 15.2 | 2.9 | −81% | .002 |
| County of Residence | ||||||||||||
| Hawai‘i | 59.1 | 71.5 | 21% | <.001 | 30.0 | 21.5 | −28% | <.001 | 10.8 | 7.1 | −34% | <.001 |
| Honolulu | 58.2 | 79.4 | 36% | <.001 | 31.5 | 15.6 | −50% | <.001 | 10.3 | 5.0 | −51% | <.001 |
| Kauai | 80.3 | 92.5 | 15% | <.001 | 12.5 | 4.0 | −68% | <.001 | 7.2 | 3.5 | −51% | <.001 |
| Maui | 52.7 | 81.1 | 54% | <.001 | 38.3 | 17.2 | −55% | <.001 | 9.0 | 1.8 | −80% | <.001 |
| Overall | 58.8 | 79.1 | 35% | <.001 | 31.1 | 16.0 | −49% | <.001 | 10.1 | 4.9 | −51% | <.001 |
Notes: Data source is the Newborn Metabolic Screening-Linked Birth Certificate File. Individual subgroup column totals may not sum to overall total due to missing/unknown data and row percentages may not sum to 100% due to rounding.
Early is based on time of newborn metabolic screening test, less than 48 hours from discharge.
Relative Change is defined by: (Prevalence in 2015 – Prevalence in 2008) / (Prevalence in 2008)
Trend p-value based on Cochrane-Armitage Trend Test
All others include Vietnamese, Asian Indian, other Asian, Guamanian/Chamorro, other Pacific Islander, Puerto Rican, Portuguese, Cuban, Mexican, American Indian/Alaskan Native, and all others.
Figure 1.
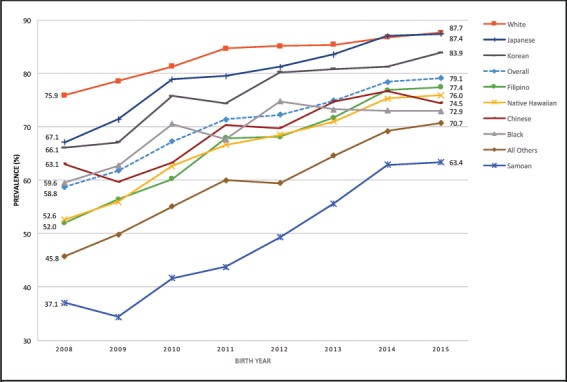
Early Exclusive Breastfeeding by Maternal Race, Hawai‘i Newborn Metabolic Screening-Linked Birth Certificate, File, 2008–2015
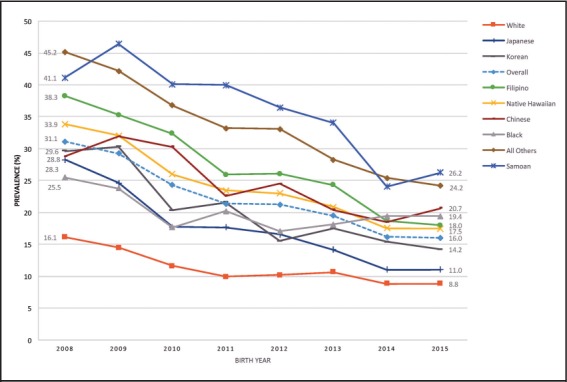
Conversely, the prevalence of early mixed feeding decreased from 31.1% in 2008 to 16.0% in 2015 (a relative decrease of −49%; Table 2). Early mixed feeding declined among all maternal race groups with Japanese mothers having the largest relative decrease (−61%), followed by Filipino (−53%), Korean (−52%), and Native Hawaiian (−48%) mothers (Table 2 and Figure 2). Declines in early mixed feeding were also seen across all characteristic subgroups categorized by maternal age, marital status, birth attendant (except other birth attendant), and county of residence (Table 2).
Figure 2.
Early Formula Feeding by Maternal Race, Hawai‘i Newborn Metabolic Screening-Linked Birth Certificate File, 2008–2015
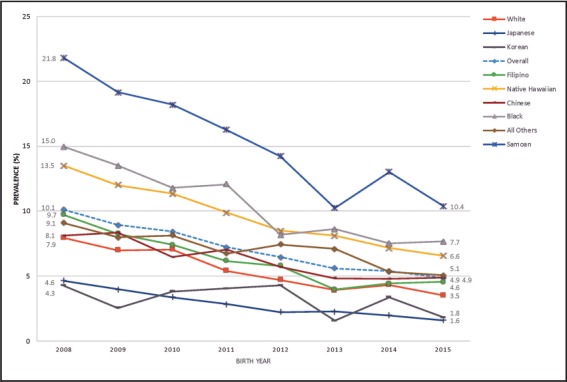
Statewide, the prevalence of early formula feeding decreased from 10.1% in 2008 to 4.9% in 2015 (a relative decrease of -51%; Table 2). Early formula feeding declined among all maternal race groups (except Korean mothers) with Japanese mothers having the largest relative decrease (−65%; Table 2 and Figure 3). Declines in early formula feeding were also seen across all characteristic subgroups categorized by maternal age, marital status, birth attendant, and county of residence (Table 2).
Figure 3.
Early Mixed Feeding by Maternal Race, Hawai‘i Newborn Metabolic Screening-Linked Birth Certificate File, 2008–2015
Overall, there was a 2.78 times greater odds of early exclusive breastfeeding versus early formula feeding in 2015 compared to 2008 after adjustment for maternal race, maternal age, marital status, birth attendant, and county of residence (Table 3). Additionally, within each maternal race subgroup, adjusted odds ratios indicated women who delivered in 2015 were more likely to practice early exclusive breastfeeding than early formula feeding compared with women who delivered in 2008 (Table 3).
Table 3.
Overall and Individual Maternal Race Subgroups Logistic Regression Models of Early Exclusive Infant Feeding for Birth year 2015 compared with 2008, 2008–2015
| Maternal Race | Crude OR (95% CIa) | Adjusted ORb (95% CI) |
|---|---|---|
| white | 2.60 (2.11 – 3.21) | 2.41 (1.95 – 2.99) |
| black | 2.40 (1.54 – 3.72) | 2.11 (1.35 – 3.32) |
| Native Hawaiian | 2.97 (2.55 – 3.46) | 3.05 (2.60 – 3.56) |
| Samoan | 3.59 (2.35 – 5.49) | 3.48 (2.23 – 5.44) |
| Filipino | 3.17 (2.53 – 3.97) | 3.29 (2.62 – 4.13) |
| Japanese | 3.79 (2.34 – 6.13) | 3.80 (2.29 – 6.31) |
| Chinese | 1.97 (1.26 – 3.10) | 2.20 (1.39 – 3.46) |
| Korean | 2.98 (1.04 – 8.49) | 2.68 (0.93 – 7.74) |
| All othersc | 2.77 (2.12 – 3.62) | 2.97 (2.26 – 3.89) |
| Overall | 2.80 (2.56 – 3.06) | 2.78 (2.54 – 3.05) |
Note: Data source is the Newborn Metabolic Screening-Linked Birth Certificate File. Individual models for each Maternal Race group and overall were used to assess trend difference between 2015 and 2008.
CI denotes Confidence interval around the odds ratio estimate
Individual models were adjusted for maternal age, marital status, birth attendant, and county of residence
All others include Vietnamese, Asian Indian, other Asian, Guamanian/Chamorro, other Pacific Islander, Puerto Rican, Portuguese, Cuban, Mexican, American Indian/Alaskan Native, and all others.
In the generalized logit model to compare differences by maternal race subgroups, Japanese and Korean mothers were more likely to practice early exclusive breastfeeding (reference=early formula feeding) compared with white mothers after adjusting for maternal age, marital status, birth attendant, county of residence, and birth year (Table 4). However, Samoan, Black, Native Hawaiian, Filipino, Chinese, and all others were all less likely to practice early exclusive breastfeeding compared with white mothers. In the adjusted analysis for early mixed feeding (reference=early formula feeding), Japanese, Korean, Filipino, Chinese, Native Hawaiian, Samoan, and all others were more likely to practice early mixed feeding compared with white mothers.
Table 4.
Maternal Race Generalized Logit Model of Early Exclusive Breastfeeding and Early Mixed Feeding,a 2008–2015
| Early Exclusive Breastfeeding | Early Mixed Feeding | |||
|---|---|---|---|---|
| Maternal Race | Crude OR (95% CIb) | Adjusted ORc (95% CI) | Crude OR (95% CI) | Adjusted OR (95% CI) |
| white | ref ref | ref ref | ref ref | ref ref |
| black | 0.44 (0.39–0.50) | 0.48 (0.42–0.54) | 0.94 (0.82–1.08) | 1.00 (0.87–1.15) |
| Native Hawaiian | 0.44 (0.42–0.47) | 0.57 (0.53–0.61) | 1.22 (1.14–1.31) | 1.33 (1.23–1.43) |
| Samoan | 0.20 (0.18–0.23) | 0.25 (0.23–0.28) | 1.13 (1.01–1.28) | 1.26 (1.11–1.42) |
| Filipino | 0.68 (0.63–0.73) | 0.80 (0.74–0.86) | 2.10 (1.93–2.28) | 2.22 (2.03–2.41) |
| Japanese | 1.77 (1.58–1.99) | 2.15 (1.90–2.42) | 2.98 (2.62–3.38) | 3.10 (2.72–3.54) |
| Chinese | 0.74 (0.66–0.84) | 0.83 (0.73–0.94) | 1.93 (1.69–2.20) | 2.03 (1.77–2.32) |
| Korean | 1.54 (1.22–1.94) | 1.73 (1.37–2.18) | 3.07 (2.40–3.93) | 3.07 (2.39–3.94) |
| All othersd | 0.55 (0.51–0.59) | 0.65 (0.60–0.71) | 2.28 (2.09–2.49) | 2.43 (2.22–2.67) |
Note: Data source is the Newborn Metabolic Screening-Linked Birth Certificate File.
Formula Feeding is the referent comparison group for each outcome.
Early is based on time of newborn metabolic screening test.
CI denotes Confidence interval around the odds ratio estimate.
Adjusted for maternal age, marital status, birth attendant, county of residence, and birth year.
All others include Vietnamese, Asian Indian, other Asian, Guamanian/Chamorro, other Pacific Islander, Puerto Rican, Portuguese, Cuban, Mexican, American Indian/Alaskan Native, and all others.
Discussion
These findings highlight early infant feeding patterns among a diverse subgroup of maternal races not previously described in the general literature. There was an overall improvement in early exclusive breastfeeding and declines in early mixed feeding and in early formula feeding among almost all maternal race subgroups in Hawai‘i from 2008–2015. Further evaluation identified some persistent differences in maternal race subgroups. Additionally, there were improvements in early exclusive breastfeeding for other socio-demographic characteristics in the unadjusted analysis.
There are likely several factors contributing to the noted improvements in early infant feeding patterns seen among maternal race subgroups. In 2010, the Baby Friendly Hawai‘i Project started promoting breastfeeding support in hospitals, through maternity care practices without giving specific attention to high-risk populations.12 The study results, showing improvement in all maternal race and other subgroups, support the premise that this system level change helped improve early infant feeding rates for all women. Additionally, other system level factors including the establishment of Joint Commission measures in 2010 for breastfeeding at hospitals or other smaller scale interventions may have contributed to this large-scale improvement.14,17 The increasing awareness of the benefits of breastfeeding in society over time also likely contributed to the improvement. The descriptive nature of this study does not allow further exploration but are briefly mentioned here. For example, breastfeeding is promoted though legislative laws to protect the ability of women to breastfeed in the workplace and in public. The Hawai‘i Special Supplemental Nutrition Program for Women Infants and Children (WIC) provides education on infant feeding to nearly half the mothers in the state on breastfeeding and supports policy and workplace efforts across the state.18
Despite the overall significant improvement noted, some notable differences remain in early infant feeding patterns, among maternal race subgroups. Understanding the reasons for these differences could help inform the development of programs to address disparities. Rates of breastfeeding change as immigrant populations become acculturated to living in the United States.19–26 Other key factors including employment where breastfeeding is not supported and general societal expectations are also important for breastfeeding.19,20 Finally, other factors including health literacy may also be related to early infant feeding as it has been associated with other perinatal outcomes in Hawai‘i including low birth weight, cesarean delivery, obstetric trauma, medical decision making, and vaginal birth after cesarean27–32 and in other settings for breastfeeding.33,34 Understanding and learning from differences within the diverse race groups in Hawai‘i is challenging but clarifying the influence due to immigration, acculturation, health literacy, employment, and cultural factors through both quantitative and qualitative approaches could be helpful in developing targeted interventions among these particular subgroups.
The accuracy of the feeding pattern reported on the Newborn Metabolic Screening data and the quality of the data collection may vary from hospital to hospital and for births outside a hospital potentially influencing our results. Additionally, the analysis is based on the feeding pattern noted within the first 24–48 hours of life only, but this is a critical time period that is predictive of future breastfeeding patterns.35–38 This analysis was limited to term newborns to minimize concerns about medical conditions associated with prematurity that could influence early breastfeeding, but overall results without this exclusion demonstrated very similar patterns and rates (data not shown). Moreover, race was based on the maternal single race provided by OHSM, which limits the ability to generalize these results to all Asian and NHOPI subgroups particularly due to the inability to separate out those women who were of more than 1 race. Additionally, the number of births among some of the other smaller Asian or NHOPI subgroups were too small (ie, Vietnamese, Micronesian) to be analyzed and may result in different patterns. Moreover, race is a social construct that is not even homogenous within a population and thus there are limitations on its use to characterize populations. Further, the ability to look at the combination of mother and father race or of proportions of various race groups for those that were multirace were not possible with the data provided. Other limitations include the lack of ability to look at other social determinants (ie, income, household federal poverty level, and insurance status) and cultural practices that likely influence infant feeding patterns. The data did not include a woman's past experience with breastfeeding or familial support of breastfeeding, which are both important predictors for breastfeeding experience and continuation.20,39,40 Finally, this study was based on a diverse population in Hawai‘i and although many of these same populations live in communities across the country, these results may not be generalizable to those populations due to acculturation and cultural differences from those found outside Hawai‘i. However, these results may provide insight into early infant feeding patterns in these subgroups, and it will be important to validate these results in other states.
Conclusions
There was substantial improvement in early exclusive breastfeeding in the state of Hawai‘i, coinciding with systemic changes implemented by hospitals. However, some persistent disparities exist among maternal race groups. Further understanding of reasons why certain maternal race subgroups continue to have lower while others have high estimates of early exclusive breastfeeding may help in the development of culturally appropriate hospital practices to address disparities in early infant feeding in Hawai‘i.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Hawai‘i State Department of Health.
Acknowledgements
BFHP was funded by Cooperative Agreement CDC-RFA-DP09- 90101ARRA09, from the Centers for Disease Control and Prevention Communities Putting Prevention to Work (CPPW) and the Healthy Hawai‘i Initiative Tobacco Settlement Special Fund. We would like to thank the Hawai‘i State Department of Health, Newborn Metabolic Screening Program for providing the Newborn Metabolic Screening data that we used in this manuscript and the Hawai‘i State Department of Health, Office of Health Status and Monitoring for conducting the linkage and providing the information from the birth certificate used in this analysis. The authors would like to thank Ms. Meghan McGurk form the University of Hawai‘i, Office of Public Health Studies for her contribution in providing critical input throughout the development of the manuscript. The authors also appreciate the assistance from the Maternal and Child Health Epidemiology Team, Division of Reproductive Health and the Division of Nutrition and Physical Activity and Obesity at the Centers for Disease Control and Prevention who assisted in oversight and review of the analysis.
Abbreviations/Acronyms
- NHOPI
Native Hawaiian or Other Pacific Islander
- OHSM
Office of Health Status and Monitoring
- PRAMS
Pregnancy Risk Assessment Monitoring System
- WIC
Special Supplemental Nutrition Program for Women, Infant, and Children
Contributor Information
Donald K. Hayes, Centers for Disease Control and Prevention, Division of Reproductive Health, Atlanta, GA (DKH); Hawai‘i State Department of Health, Family Health Services Division, Honolulu, HI(DKH).
Ellen O. Boundy, Centers for Disease Control and Prevention, Epidemic Intelligence Service, Atlanta, GA (EOB); Centers for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity,Atlanta, GA (EOB).
Conflict of Interest
None of the authors identify a conflict of interest.
Disclosure
Donald Hayes initiated his work on the reported research while affiliated with the Hawai‘i State Department of Health. Currently, he is affiliated with the Centers for Disease Control and Prevention's Division for Heart Disease and Stroke Prevention. The research in this manuscript was completed and submitted outside of the official duties of his current position.
References
- 1.United States. Public Health Service. Office of the Surgeon General., Centers for Disease Control and Prevention (U.S.) United States. Department of Health and Human Services. Office on Women's Health The surgeon general's call to action to support breastfeeding. 2011. http://www.ncbi.nlm.nih.gov/books/NBK52682. Accessed March 14, 2019.
- 2.Chantry CJ, Eglash A, Labbok M. The Academy of Breastfeeding Medicine Position on Breastfeeding-Revised 2015. Breastfeeding Medicine. 2015;10((9)):407–411. doi: 10.1089/bfm.2015.29012.cha. [DOI] [PubMed] [Google Scholar]
- 3.Eidelman AI. The Relative Value of Breastfeeding Versus the Feeding of Breastmilk. Breastfeeing Medicine. 2016;11((6)):269–.. doi: 10.1089/bfm.2016.29015.aie. [DOI] [PubMed] [Google Scholar]
- 4.Ip S, Chung M, Raman G, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evidince Report/Technology Assessment. 2007;((153)):1–186. [PMC free article] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012;129((3)):e827–841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- 6.American College of Obstetricians and Gynecologists ACOG committee opinion: Optimizing Support for Breastfeeding as Part of Obstetric Practice. 2016. https://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Optimizing-Supportfor-Breastfeeding-as-Part-of-Obstetric-Practice. Accessed March 14, 2019.
- 7.American Academy of Family Physicians Breastfeeding Policy Statement. http://www.aafp.org/about/policies/all/breastfeeding.html. Updated April 2017. Accessed March 14, 2019.
- 8.World Health Organization . Geneva: World Health Organization; Division of Child Health and Development. Evidence of the Ten Steps to Successful Breastfeding. http://www.who.int/nutrition/publications/evidence_ten_step_eng.pdf. Accessed March 14, 2019. [Google Scholar]
- 9.Pound CM, Unger SL, Canadian Paediatric Society, Hospital Paediatrics Section, Nutrition and Gastroenterology Committee The Baby-Friendly Initiative: Protecting, promoting and supporting breastfeeding. Paediatrica and Child Health. 2012;17((6)):317–327. [PMC free article] [PubMed] [Google Scholar]
- 10.Pérez-Escamilla R, Martinez JL, Segura-Pérez S. Impact of the Baby-friendly Hospital Initiative on breastfeeding and child health outcomes: a systematic review. Maternal Child Nutrition. 2016;12((3)):402–417. doi: 10.1111/mcn.12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salera-Vieira J, Zembo CT. Trends in Baby-Friendly® Care in the United States: Historical Influences on Contemporary Care. Journal of Perinatal and Neonatal Nursing. 2016;30((3)):243–248. doi: 10.1097/JPN.0000000000000176. [DOI] [PubMed] [Google Scholar]
- 12.Kahin SA, McGurk M, Hansen-Smith H, West M, Li R, Melcher CL. Key Program Findings and Insights From the Baby-Friendly Hawaii Project. Journal of Human Lactation. 2017;33((2)):409–414. doi: 10.1177/0890334416683675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lai EY, Arguelles D. The new face of Asian Pacific America: numbers, diversity, & change in the 21st century. San Francisco, CA: UCLA's Asian American Studies Center Press; 2003. in cooperation with the Organization of Chinese Americans and the National Coalition for Asian Pacific American Community Development. [Google Scholar]
- 14.Reeves TJ, Bennett CE. The Asian and Pacific Islander Population in the United States: March 2002. Current Population Reports. 2003:P20–540. [Google Scholar]
- 15.Hayes DK, Mitchell KM, Donohoe-Mather C, Zaha RL, Melcher C, Fuddy LJ. Predictors of exclusive breastfeeding at least 8 weeks among Asian and Native Hawaiian or other Pacific Islander race subgroups in Hawaii, 2004-2008. Maternal and Child Health Journal. 2014;18((5)):1215–1223. doi: 10.1007/s10995-013-1355-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sorenson C, Wood B, Prince E. Race & ethnicity data: Developing a common language for public health surveillance in Hawaii. Californian Journal of Health Promotion (Special Issue: Hawaii) 2003:91–104. [Google Scholar]
- 17.Feldman-Winter L, Douglass-Bright A, Bartick MC, Matranga J. The new mandate from the joint commission on the perinatal care core measure of exclusive breast milk feeding: implications for practice and implementation in the United States. Journal of Human Lactation. 2013;29((3)):291–295. doi: 10.1177/0890334413485641. [DOI] [PubMed] [Google Scholar]
- 18. Hawaii State Department of Health, Family Health Services Division, Women Infant and Children Branch. 2018. http://health.hawaii.gov/wic/. Accessed December 14, 2018.
- 19.Bai DL, Fong DY, Tarrant M. Factors associated with breastfeeding duration and exclusivity in mothers returning to paid employment postpartum. Maternal and Child Health Journal. 2015;19((5)):990–999. doi: 10.1007/s10995-014-1596-7. [DOI] [PubMed] [Google Scholar]
- 20.McKinney CO, Hahn-Holbrook J, Chase-Lansdale PL, et al. Community Child Health Research Network. Racial and Ethnic Differences in Breastfeeding. Pediatrics. 2016;138((2)):2015–2388. doi: 10.1542/peds.2015-2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Babington L, Patel B. Understanding child feeding practices of Vietnamese mothers. MCN The American Journal of Maternal/Child Nursing. 2008;33((6)):376–381. doi: 10.1097/01.NMC.0000341259.03298.26. [DOI] [PubMed] [Google Scholar]
- 22.Barcelona de Mendoza V, Harville E, Theall K, Buekens P, Chasan-Taber L. Acculturation and Intention to Breastfeed among a Population of Predominantly Puerto Rican Women. Birth. 2016;43((1)):78–85. doi: 10.1111/birt.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cartagena D, Ameringer SW, McGrath JM, Masho SW, Jallo N, Myers BJ. Factors contributing to infant overfeeding in low-income immigrant Latina mothers. Applied Nursing Research. 2015;28((4)):316–321. doi: 10.1016/j.apnr.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Choudhry K, Wallace LM. ‘Breast is not always best’: South Asian women's experiences of infant feeding in the UK within an acculturation framework. Maternal and Child Nutrition. 2012;8((1)):72–87. doi: 10.1111/j.1740-8709.2010.00253.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Donaldson H, Kratzer J, Okutoro-Ketter S, Tung P. Breastfeeding among Chinese immigrants in the United States. Journal of Midwifery Womens Health. 2010;55((3)):277–281. doi: 10.1016/j.jmwh.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 26.Hohl S, Thompson B, Escareño M, Duggan C. Cultural Norms in Conflict: Breastfeeding Among Hispanic Immigrants in Rural Washington State. Maternal and Child Health Journal. 2016;20((7)):1549–1557. doi: 10.1007/s10995-016-1954-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chang AL, Hurwitz E, Miyamura J, Kaneshiro B, Sentell T. Maternal risk factors and perinatal outcomes among pacific islander groups in Hawaii: a retrospective cohort study using statewide hospital data. BMC Pregnancy Childbirth. 2015;15:239. doi: 10.1186/s12884-015-0671-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davis CM, Guo M, Miyamura J, Chang A, Nelson-Hurwitz DC, Sentell T. Key Factors in Obstetric Delivery Decision-Making among Asian and Pacific Islander Women by English Proficiency. Hawaii Journal of Medicine and Public Health. 2017;76((10)):279–286. [PMC free article] [PubMed] [Google Scholar]
- 29.Sentell T, Baker KK, Onaka A, Braun K. Low health literacy and poor health status in Asian Americans and Pacific Islanders in Hawai’i. Journal of Health Communication. 2011;16(Suppl 3):279–294. doi: 10.1080/10810730.2011.604390. [DOI] [PubMed] [Google Scholar]
- 30.Sentell T, Braun KL, Davis J, Davis T. Health literacy and meeting breast and cervical cancer screening guidelines among Asians and whites in California. Springerplus. 2015;4:432. doi: 10.1186/s40064-015-1225-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sentell T, Chang A, Cheng Y, Miyamura J. Maternal quality and safety outcomes for Asians and Pacific Islanders in Hawaii: an observational study from five years of statewide data. BMC Pregnancy Childbirth. 2014;14:298. doi: 10.1186/1471-2393-14-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sentell T, Dela Cruz MR, Heo HH, Braun KL. Health literacy, health communication challenges, and cancer screening among rural native Hawaiian and Filipino women. Journal of Cancer Education. 2013;28((2)):325–334. doi: 10.1007/s13187-013-0471-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kilfoyle KA, Vitko M, O'Conor R, Bailey SC. Health Literacy and Women's Reproductive Health: A Systematic Review. Journal of Womens Health (Larchmt) 2016;25((12)):1237–1255. doi: 10.1089/jwh.2016.5810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Poorman E, Gazmararian J, Elon L, Parker R. Is health literacy related to health behaviors and cell phone usage patterns among the text4baby target population? Archives of Public Health. 2014;72((1)):13–.. doi: 10.1186/2049-3258-72-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Declercq E, Labbok MH, Sakala C, O'Hara M. Hospital practices and women's likelihood of fulfilling their intention to exclusively breastfeed. American Journal of Public Health. 2009;99((5)):929–935. doi: 10.2105/AJPH.2008.135236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DiGirolamo AM, Grummer-Strawn LM, Fein SB. Effect of maternity-care practices on breastfeeding. Pediatrics. 2008;122((Suppl 2)):S43–49. doi: 10.1542/peds.2008-1315e. [DOI] [PubMed] [Google Scholar]
- 37.Hawkins SS, Stern AD, Baum CF, Gillman MW. Evaluating the impact of the Baby-Friendly Hospital Initiative on breast-feeding rates: a multi-state analysis. Public Health Nutrition. 2015;18((2)):189–197. doi: 10.1017/S1368980014000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Murray EK, Ricketts S, Dellaport J. Hospital practices that increase breastfeeding duration: results from a population-based study. Birth. 2007;34((3)):202–211. doi: 10.1111/j.1523-536X.2007.00172.x. [DOI] [PubMed] [Google Scholar]
- 39.Mitchell-Box KM, Braun KL. Impact of male-partner-focused interventions on breastfeeding initiation, exclusivity, and continuation. Journal of Human Lactation. 2013;29((4)):473–479. doi: 10.1177/0890334413491833. [DOI] [PubMed] [Google Scholar]
- 40.Rempel LA, Rempel JK, Moore KC. Relationships between types of father breastfeeding support and breastfeeding outcomes. Maternal Child Nutrition. 2017;13((3)):e12337. doi: 10.1111/mcn.12337. [DOI] [PMC free article] [PubMed] [Google Scholar]


