Abstract
BACKGROUND
Women diagnosed with polycystic ovary syndrome (PCOS) suffer from an unfavorable cardiometabolic risk profile, which is already established by child-bearing age.
OBJECTIVE AND RATIONALE
The aim of this systematic review along with an individual participant data meta-analysis is to evaluate whether cardiometabolic features in the offspring (females and males aged 1–18 years) of women with PCOS (OPCOS) are less favorable compared to the offspring of healthy controls.
SEARCH METHODS
PubMed, Embase and gray literature databases were searched by three authors independently (M.N.G., M.A.W and J.C.) (last updated on 1 February 2018). Relevant key terms such as ‘offspring’ and ‘PCOS’ were combined. Outcomes were age-specific standardized scores of various cardiometabolic parameters: BMI, blood pressure, glucose, insulin, lipid profile and the sum scores of various cardiometabolic features (metabolic sum score). Linear mixed models were used for analyses with standardized beta (β) as outcome.
OUTCOMES
Nine relevant observational studies could be identified, which jointly included 1367 children: OPCOS and controls, originating from the Netherlands, Chile and the USA. After excluding neonates, duplicate records and follow-up screenings, a total of 885 subjects remained. In adjusted analyses, we observed that OPCOS (n = 298) exhibited increased plasma levels of fasting insulin (β = 0.21(95%CI: 0.01–0.41), P = 0.05), insulin-resistance (β = 0.21(95%CI: 0.01–0.42), P = 0.04), triglycerides (β = 0.19(95%CI: 0.02–0.36), P = 0.03) and high-density lipoprotein (HDL)-cholesterol concentrations (β = 0.31(95%CI: 0.08–0.54), P < 0.01), but a reduced birthweight (β = −116(95%CI: −195 to 38), P < 0.01) compared to controls (n = 587). After correction for multiple testing, however, differences in insulin and triglycerides lost their statistical significance. Interaction tests for sex revealed differences between males and females when comparing OPCOS versus controls. A higher 2-hour fasting insulin was observed among female OPCOS versus female controls (estimated difference for females (βf) = 0.45(95%CI: 0.07 to 0.83)) compared to the estimated difference between males ((βm) = −0.20(95%CI: −0.58 to 0.19)), with interaction-test: P = 0.03. Low-density lipoprotein–cholesterol differences in OPCOS versus controls were lower among females (βf = −0.39(95%CI: −0.62 to 0.16)), but comparable between male OPCOS and male controls (βm = 0.27(95%CI: −0.03 to 0.57)), with interaction-test: P < 0.01. Total cholesterol differences in OPCOS versus controls were also lower in females compared to the difference in male OPCOS and male controls (βf = −0.31(95%CI: −0.57 to 0.06), βm = 0.28(95%CI: −0.01 to 0.56), interaction-test: P = 0.01). The difference in HDL-cholesterol among female OPCOS versus controls (βf = 0.53(95%CI: 0.18–0.88)) was larger compared to the estimated mean difference among OPCOS males and the male controls (βm = 0.13(95%CI: −0.05−0.31), interaction-test: P < 0.01). Interaction test in metabolic sum score revealed a significant difference between females (OPCOS versus controls) and males (OPCOS versus controls); however, sub analyses performed in both sexes separately did not reveal a difference among females (OPCOS versus controls: βf = −0.14(95%CI: −1.05 to 0.77)) or males (OPCOS versus controls: βm = 0.85(95%CI: −0.10 to 1.79)), with P-value < 0.01.
WIDER IMPLICATIONS
We observed subtle signs of altered cardiometabolic health in OPCOS. Therefore, the unfavorable cardiovascular profile of women with PCOS at childbearing age may—next to a genetic predisposition—influence the health of their offspring. Sensitivity analyses revealed that these differences were predominantly observed among female offspring aged between 1 and 18 years. Moreover, studies with minimal risk of bias should elucidate the influence of a PCOS diagnosis in mothers on both sexes during fetal development and subsequently during childhood.
Keywords: PCOS, preconception, periconception, offspring, children, cardiovascular health, metabolic health, cardiometabolic health, sex differences
Introduction
Polycystic ovary syndrome (PCOS) represents a heterogeneous condition often including ovulatory dysfunction, hyperandrogenemia and characteristic alterations in ovarian morphology, and is present in 6–15% of all women of reproductive age (Fauser et al., 2012; Williams et al., 2016). Obesity, insulin resistance, dyslipidemia and type 2 diabetes mellitus are all features frequently associated with PCOS (Moran et al., 2010; Fauser et al., 2012). In addition, PCOS often runs in families (Legro et al., 1998; Kahsar-Miller et al., 2001), suggesting a genetic component (Carey et al., 1993; Urbanek et al., 1999; Day et al., 2018).
PCOS is often diagnosed in women who wish to conceive. Recent research revealed that even during singleton pregnancies, women with PCOS present with increased pregnancy complication rates, such as gestational diabetes mellitus, pregnancy induced hypertension and pre-eclampsia (Boomsma et al., 2006). Moreover, neonates born from women with PCOS present with increased neonatal complication rates, especially resulting from preterm birth (Boomsma et al., 2006; Palomba et al., 2015; Christ et al., 2019).
The Barker hypothesis implies that the health and development of children is directly affected by the intrauterine environment (Barker et al., 1989; Kermack et al., 2015; Paauw et al., 2017). An association between maternal health and offspring health has been convincingly demonstrated in the general population (Reynolds et al., 2007; Yu et al., 2013; Gaillard et al., 2014). The maternal influence is hypothesized to be exerted via fetal programming, which occurs in utero during critical development stages in early embryonic and fetal life (Kwon and Kim, 2017). Fetal programming may affect male and female fetuses differently in the intrauterine environment. Animal studies, for example, report on higher offspring blood pressure in males compared to females in response to maternal pharmacological glucocorticoid administration during gestation (Dodic et al., 1998, 2002). However, in human studies concerning adiposity in offspring, female offspring appear to be more sensitive to increased maternal glucose levels (Regnault et al., 2013).
Currently, limited information is available regarding health of the offspring of women with PCOS (OPCOS). The sample size of the studies in OPCOS is rather small and the possibility to adjust for confounding factors is therefore limited. The majority of human studies in PCOS predominantly report on female offspring. Moreover, existing literature concerning metabolic outcomes in OPCOS is inconsistent. For example, the increased insulin concentrations found in the American and Chilean OPCOS (Sir-Petermann et al., 2007; Kent et al., 2008; Legro et al., 2017) were not observed in Dutch children from mothers with PCOS (Wilde et al., 2018). Cardiometabolic derailments in childhood are often subtle, but may still have distinct implications for cardiovascular health in adulthood (Daniels, 2001; Baker et al., 2007; Singh et al., 2008). In two studies including both female and male offspring, no sex differences were observed in anthropometrics, lipid profile or glucose and insulin concentrations in serum (Kent et al., 2008; Wilde et al., 2018).
Therefore, the primary purpose of the current systematic review and individual participant data (IPD) meta-analysis was to compare cardiometabolic health in the children of women previously diagnosed with PCOS to healthy controls. Second, we aim to explore whether any differences in metabolic and other factors in female and male OPCOS exist. An IPD meta-analysis was conducted to increase the power to detect potential differences. We hypothesize that OPCOS exhibit worse increased insulin concentrations compared to healthy controls.
Methods
We conducted our systematic review according to PRISMA guidelines (Moher et al., 2009). A systematic search in the PubMed and EMBASE was performed on 1 June 2016 and last updated on 1 February 2018. Relevant key terms such as ‘offspring’ and ‘polycystic ovarian syndrome’ and serum hormones such as ‘glucose’ and ‘insulin’ were combined in a search syntax with the use of database specific subject headings (e.g. MeSH-terms in PubMed). There was no methodological search term (e.g. ‘cohort’ or ‘case-control’) added to the search syntax, because we expected little added value in the completeness of the articles retrieved by our search (Supplementary Table S1). We also conducted an online gray literature search. Duplicates were removed electronically and manually by using Mendeley software. The full search terms are listed in the Supplementary Table SI. The study protocol is registered at PROSPERO with number: CRD42019117798 (http://www.crd.york.ac.uk/PROSPERO/).
Study selection
We selected studies on children of women with PCOS. PCOS diagnosis must be performed by a physician in a standardized fashion in all mothers of the included children. We included studies with children between 1 and 18 years of age, regardless of sex. Studies reporting on children in the neonatal period were excluded because they mainly focused on pregnancy and perinatal outcomes (Anderson et al., 2010). We intended to focus on features potentially relevant for prediction of long-term health outcomes: BMI, blood pressure, fasting and post-load (after oral glucose administration) levels of serum glucose and insulin, and lipid profile. Only human studies with original data were eligible for inclusion. All English, Dutch, German, French and Spanish publications were included. Commentaries, opinion papers, case reports, small case series (n < 10) and systematic reviews were not eligible for inclusion. We used similar criteria for title and abstract screening as for the full text screening. Authors who independently performed the screening (M.N.G., M.A.W. and J.P.C.) endorsed the final selection of articles. A fourth author (B.C.J.M.F.) was available when consensus on final article selection was not achieved. The final step in study selection was performing a thorough check of the reference lists of all relevant articles, regardless of design, in the search (cross reference checking) (Fig. 1).
Figure 1.
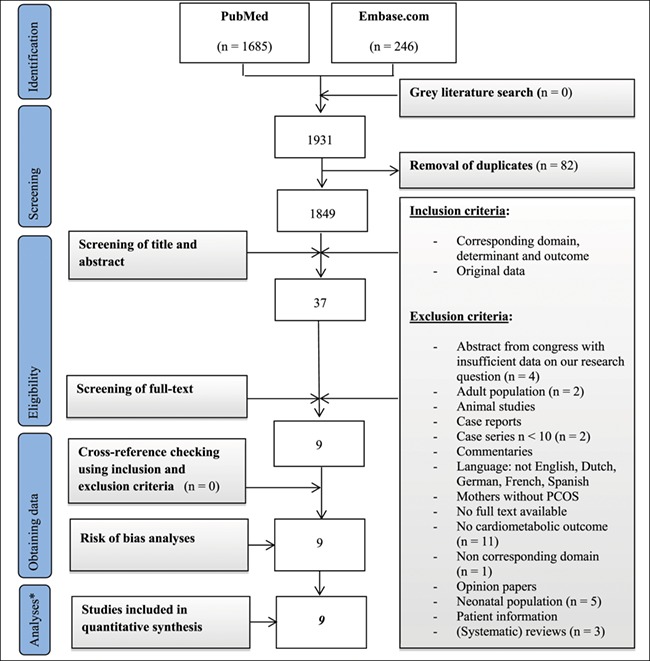
Flowchart of the search, according to PRISMA guidelines. * = all data in this step were available obtained and analyzed, n = number. All numbers (n) mentioned in the exclusion criteria were extracted in the ‘screening on full-text’ step (Figure adjusted from the PRISMA group (Moher 2009).
Risk of bias assessment
Internal validity of the individual studies was assessed using the Newcastle Ottawa Quality Assessment Scale (NOS). The NOS is recommended for observational studies, which was the expected study design for our research question (Wells et al., 2014). The three main categories of the NOS are: selection of patients and controls, comparability of patients and controls and exposure of both groups. The NOS has the possibility to add study specific elements to its criteria. Considering our hypothesis, we chose to specifically assess the adjustment for age, sex and socio-economic status. Each study separately received a risk of bias level: high (1–3 stars), medium (4–6 stars) or low (7–9 stars) (Supplementary Table SII).
Data collection
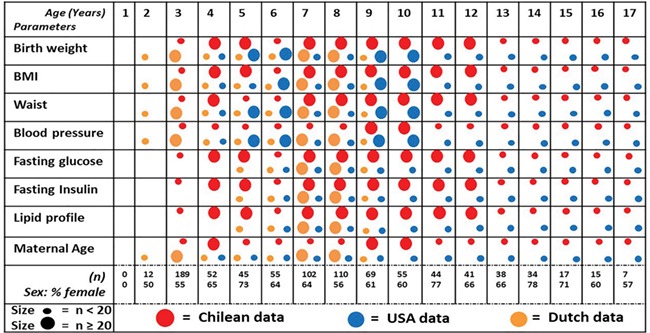
Authors of studies eligible for inclusion in our IPD meta-analysis were invited to join our study and share their data. As previously published, the research groups received approval for the individual studies from the local medical ethics committee. Requested data comprised continuous data on maternal characteristics, birthweight of their offspring and data on the cardiometabolic status of the offspring. An exception was dichotomous data on sex, gestation (multiple/singleton) and presence of siblings in the dataset. Received data were uniformly coded and harmonized in one dataset (Figs 2 and 3). We converted all serum concentrations into similar units of measure. The Dutch data on glucose and lipid profiles were converted from millimole per liter (mmol/L) to milligram per deciliter (mg/dL) (Haney et al., 2007). No further harmonization issues had to be encountered.
Figure 2. Flowchart of the study: from systematic search results to IPD dataset. This flowchart represents the four steps (four columns’ from left to right), which were undertaken to collect our final data for the IPD meta-analysis. Column (1) Participants (n) per study. Our screening resulted in nine publications from three research groups with (n) participants per article (cases and controls together). Column (2) Received data. Each research group shared one file with all offspring of women with PCOS (OPCOS) and all healthy controls (n), which showed that some subjects participated in more than one publication. Column (3) Extraction <1 yr (year) and duplicates. In the third step, we excluded all children below 1 year old and all duplicate children (children who were screened multiple times). Column (4) IPD analysis n = 885. In the fourth step, a dataset remained with 885 unique children aged 1–18 years (OPCOS and controls), on which we conducted our IPD meta-analyses.
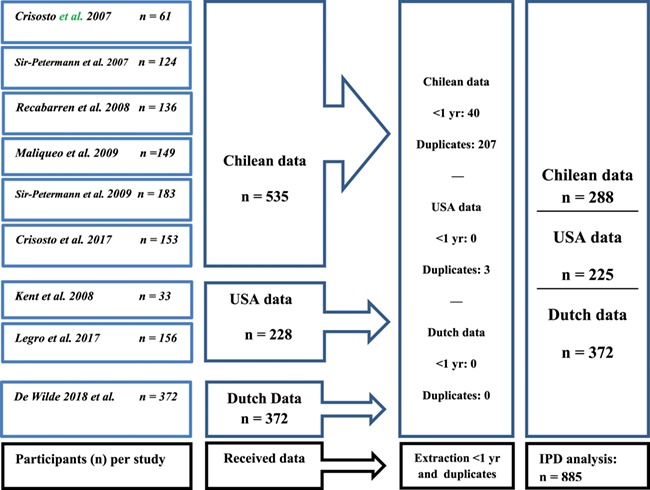
Figure 3. Parameters measured per age category in all included centers. Total number of included children on their first visit is 885: for two children their age and sex is missing. (n) = number of children in which the parameter is available.
The outcomes were parameters of the cardiometabolic profile of offspring: age- and sex-corrected BMI and systolic blood pressure (SBP), and age-corrected fasting and post-load insulin and glucose concentrations, homeostatic model assessment for insulin resistance (HOMA-IR), total-cholesterol, triglycerides, low/high-density lipoprotein-cholesterol (LDL/HDL-c) concentrations and composites of the aforementioned offspring parameters: the metabolic sum scores. We calculated HOMA-IR levels if not yet present in the received datasets, which is a measure for insulin resistance (HOMA-IR = [fasting insulin (μU/ml)*fasting glucose (mmol/liter)]/405) (Matthews et al., 1985). Due to the lack of consensus on how to define the metabolic syndrome in children, we calculated two different metabolic sum scores, a summation of multiple standardized scores (SDS) (Eisenmann, 2008). First, we calculated metabolic sum score-1, a composite of BMI, SBP, fasting insulin, triglycerides and HDL-c. Second, we calculated metabolic sum score-2, a composite of waist-to-height ratio, SBP, glucose, triglycerides and HDL-c. Metabolic sum score-2 was previously used in a large Dutch cohort study (Oostvogels et al., 2014).
Statistical analysis
Continuous normally distributed data were summarized with a mean and SD, and if non-normally distributes a median and interquartile range (IQR) were used. Categorical variables were summarized by number and percentage. We used the square root of fasting and post-load insulin concentrations and HOMA-IR, since these variables were non-normally distributed.
For missing baseline characteristics, multiple imputations (n = 5) following the predictive mean matching principal was used. We calculated age-specific SDS based on the control population for all metabolic parameters. We used the World Health Organization (WHO) reference standards of 2007 to calculate the BMI SDS for each child using a WHO tool: WHO Anthro version 3.2.2, January 2011 (WHO, 2006, 2011). The BMI SDS accounts for the age and sex of the child and is universally applicable. We also calculated age- and sex-dependent SBP percentiles according to The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents (National Institutes of Health, 2004). Percentiles were transformed to SDS, which were used for analyses.
Conversion of metabolic markers, as described previously, took place before pooling all data (Haney et al., 2007).
Heterogeneity among studies was assessed by constructing Forest plots and performing a Chi2-test. We also evaluated potential publication bias by constructing Funnel plots. For both plots, we used the metabolic sum score-1 (composite SDS of: BMI, SBP, fasting insulin, triglycerides and HDL-c) of the first visits of all children and the total number of visits of the children separately. The software utilized was Review Manager, version 5 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
To answer our research question on cardiometabolic outcomes in OPCOS versus controls, we used a one-step approach and constructed a linear mixed model with a random effect for the country or research group the children originated from. By correcting for country of origin, we take international differences, such as anthropometric and assay differences, into account.
In the first analyses, we analyzed differences between OPCOS and controls, regardless of sex, in a basic (models 1, 3, 5 and 7) and an adjusted model (models 2, 4, 6 and 8).
For birthweight, we adjusted in a basic model only for gestational age and the country (USA, Chile or The Netherlands) from which the children originated (model 1). In the adjusted model, we additionally corrected birthweight for sex, parity, multiple gestation and presence of siblings in this study (model 2).
In two variables, we calculated SDS using external reference populations: WHO-based BMI SDS and the Centers for disease control and prevention (CDC)-based SBP SDS. In the WHO-based BMI SDS, the age and sex of the child are already taken into account and in the basic model and we additionally corrected for the country from which children originated (model 3). In the adjusted model, we also adjusted for parity, multiple gestation and presence of siblings in this study (model 4). In the CDC-based SBP SDS, sex, height and age were already taken into account and we additionally adjusted for the country from which children originated (model 5). In the adjusted model, we added similar factors as for the adjusted model with BMI SDS, with addition of the weight of the offspring (model 6). For all other outcomes, in the basic model, we adjusted for age of the child and the country from which the children originated (model 7). In the adjusted model, we additionally corrected for sex of the child, parity of the mother, multiple gestation and whether children had any siblings in the IPD meta-analysis included (model 8).
Second, we added interaction terms to the additionally adjusted mixed models (models 2, 4, 6 and 8) to evaluate whether sex was an effect modifier in the association between the exposure variable (a mother with or without PCOS diagnosis) and the dependent variables (the cardiometabolic outcomes). The P-values presented are the results of the interaction test. We provided estimated mean differences with a 95% CI of OPCOS versus controls, and of the male and female children separately, without P-values. All data were analyzed using SPSS Statistics, version 25.0 (IBM SPSS Inc., Chicago, IL, USA). Owing to the number of statistical tests we performed, a Bonferroni correction for multiple testing (Chen et al., 2017) was applied. Three independent cardiometabolic outcomes were tested: anthropometrics, insulin resistance and lipid profile: outcomes were divided in these three clusters. Therefore, the significance level P = 0.05 was divided by three, which provides a significance level corrected for multiple testing: P = 0.017.
Results
Search results
The systematic search identified a total of 1931 articles, of which nine articles were selected for internal validity assessment (Fig. 1, Supplementary Table SIII). Risk of bias assessment using the NOS revealed six articles with a medium risk of bias and three articles with low risk of bias (Table I).
Table I. Internal validity of included studies using the NOS for assessing the quality of observational studiesa.
| Study | Selection | Comparability of cases and controls |
Exposure | Total risk of bias (number of stars) |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Adequate case definition? |
Representative cases? | Selection of controls |
Definition of controls |
Ascertainment of exposure? |
Similar method of ascertainment in both groups |
Non-response rate |
|||
| Crisosto et al. 2007 | * | * | NR | * | * * | * | * | NR | 7 |
| Sir-Petermann et al. 2007 | * | * | NR | * | * | * | * | NR | 6 |
| Recabarren et al. 2008 | * | * | NR | * | * * | * | * | NR | 7 |
| Maliqueo 2009 | * | * | NR | * | - | * | * | NR | 5 |
| Sir-Petermann et al. 2009 | * | - | NR | * | * | * | * | NR | 5 |
| Kent et al. 2008 | * | - | * | * | * | * | * | NR | 6 |
| Legro et al. 2017 | * | NR | NR | * | * * | * | * | NR | 6 |
| Crisosto et al. 2017 | * | * | NR | * | * | * | * | NR | 6 |
| De Wilde et al. 2018 | * | - | * | * | * * | * | - | * | 7 |
See also Supplementary Table SII.
- = study did not receive a star for this item, * = study receives a star for this item, total risk of bias: 1–3 stars = high, 4–6 stars = medium, 7–9 stars = low; NR = not reported.
Baseline characteristics
A total of 1367 children participated in the identified studies eligible for this IPD meta-analysis. Multiple children participated several times during their childhood. However, we chose to use only the first visit of all children to avoid any possible inclusion bias, i.e. an over presentation of children with an unfavorable measurement outcomes. Therefore, only 885 cardiovascular screenings of unique children OPCOS = 298 (female n = 196, male n = 102), controls n = 587 (female: n = 354, male: n = 233) were used for the current mixed model analysis (Fig. 2).
Mean age of the OPCOS group was 8.1 years old (SD 3.7) and of the healthy controls 7.9 years old (SD 3.7). Mean BMI was 18.8 kg/m2 (SD 4.5) in OPCOS and for the control group 18.1 kg/m2 (SD 3.8). Mean age and BMI among mothers with PCOS was 35.7 years old (SD 6.0) and 32.4 kg/m2 (SD 8.6) and among the controls 38.1 years old (SD 5.3) and 24.8 kg/m2 (SD 4.2), respectively. The Tanner stages were reported by the American research group: (Kent et al., 2008) and the Chilean research group, presented in Table II (Sir-Petermann et al., 2009). The Chi2-tests for heterogeneity of our study population was not significant (P = 0.42) and accompanied by a non-significant effect on the metabolic sum score-1 status between OPCOS and healthy controls (P = 0.55). The Funnel plot reported no clear sign of publication bias (Supplementary Figs SI and SII).
Table II. Baseline characteristics of all 885 first visits of offspring of women with PCOS and controls in this IPD analysis.
| Sir-Peterman et al. – Chilean data |
Legro et al. – USA data |
De Wilde et al. – Dutch data |
||||
|---|---|---|---|---|---|---|
| n = 288 | n = 225 | n = 372 | ||||
| PCOS | Controls | PCOS | Controls | PCOS | Controls | |
| n = 119 | n = 169 | n = 105 | n = 120 | n = 74 | n = 298 | |
| Baseline at birth | ||||||
| Sex (% girls) | 70 (59) | 80 (47) | 90 (86) | 103 (86) | 36 (48.6) | 171 (57.4) |
| Gestational age (weeks), median (IQR) | 39.0 (38.0–40.0) | 39.0 (38.0–40.0) | 40.0 (39.0–40.0) | 40.0 (40.0–40.0) | 39.1 (38.2–40.4) | 39.6 (39.0–40.6) |
| Birthweight (grams), mean (±) | 3287 ± 589 | 3323 ± 515 | 3726 ± 637 | 3806 ± 637 | 3304 ± 648 | 3569 ± 488 |
| Multiple gestation (%) | 0 (0%) | 0 (0%) | 2 twin pairs (1%) | 1 twin pair (2%) | 2 twin pairs (5%) | 4 twin pairs (3%) |
| Screening during childhood | ||||||
| Age at screening (year), mean (±) | 9.1 ± 3.6 | 10.4 ± 3.1 | 9.2 ± 3.5 | 10.2 ± 3.6 | 4.9 ± 2.0 | 5.6 ± 2.2 |
| BMI (kg/m2), median (IQR) | 19.3 (16.7–22.4) | 20.1 (17.4–22.8) | 19.8 (15.8–22.4) | 19.6 (16.1–21.9) | 15.6 ± 1.6 | 16.1 ± 1.5 |
| Waist (cm), median (IQR) | 62 (56–72) | 66 (60–73) | 62 (55–74) | 66 (56–75) | 52 (50–55) | 55 (52–58) |
| Waist to height ratio, mean (±) | 0.49 ± 0.1 | 0.47 ± 0.1 | 0.48 ± 0.1 | 0.47 ± 0.1 | 0.48 ± 0.1 | 0.48 ± 0.1 |
| SBP (mm Hg), mean (±) | 91 ± 11 | 93 ± 13 | 106 ± 14 | 107 ± 11 | 98 ± 8 | 99 ± 9 |
| DBP (mm Hg), mean (±) | 56 ± 9 | 57 ± 10 | 65 ± 8 | 65 ± 8 | 51 ± 7 | 52 ± 6 |
| Fasting glucose (mg/dL), mean (±) | 83 ± 10 | 83 ± 9 | 78 ± 10 | 78 ± 12 | 84 ± 6 | 82 ± 11 |
| Fasting 2-hour glucose (mg/dL), mean (±) |
99 ± 24 | 95 ± 17 | 86 ± 20 | 82 ± 17 | NA | NA |
| Fasting insulin (μU/ml), median (IQR) | 8 (5–14) | 10 (6–14) | 15 (6–21) | 13 (7–15) | 4 (2–5) | 5 (4–7) |
| Fasting 2-hour insulin (μU/ml), median (IQR) | 33 (13–63) | 32 (18–51) | 52 (31–86) | 49 (28–67) | NA | NA |
| HOMA-IR, median (IQR), median (IQR) | 2.3 (1.1–2.8) | 2.0 (1.2–2.8) | 3.3 (1.2–4.1) | 2.5 (1.3–2.0) | 0.9 (0.5–1.2) | 1.1 (0.7–1.4) |
| LDL-cholesterol (mg/dL), mean (±) | 93 ± 31 | 90 ± 35 | 58 ± 25 | 55 ± 21 | 120 ± 48 | 106 ± 24 |
| Total cholesterol (mg/dL), mean (±) | 157 ± 30 | 167 ± 31 | 150 ± 29 | 145 ± 12 | 189 ± 51 | 170 ± 27 |
| HDL-cholesterol (mg/dL), mean (±) | 44 ± 13 | 42 ± 10 | 84 ± 53 | 69 ± 32 | 56 ± 12 | 56 ± 10 |
| Triglycerides (mg/dL), mean (±) | 114 ± 45 | 116 ± 36 | 85 ± 27 | 82 ± 30 | 62 ± 21 | 42 ± 18 |
| Metabolic sum score-1 (SDS), mean (±) | 1.5 ± 2.9 | 1.0 ± 2.7 | 0.5 ± 4.0 | 1.6 ± 2.2 | −0.9 ± 1.2 | −1.3 ± 2.0 |
| Metabolic sum score-2 (SDS), mean (±) | 0.2 ± 2.6 | 0.1 ± 2.4 | −1.4 ± 4.3 | −0.3 ± 1.9 | −0.9 ± 1.1 | −1.6 ± 1.8 |
| Tanner stage: pubic hair | NA | NA | 1 (1–2) | 1 (1–3) | NA | NA |
| Tanner stage: breasts | 2 (1–4) | 2 (1–4) | 1 (1–3) | 1 (1–4) | NA | NA |
| Tanner stage: testis | 2 (1–3) | 2 (1–4) | 2 (0–4) | 1 (0–2) | NA | NA |
| Maternal age during screening child (years), mean (±) | 34.6 ± 7.2 | 37.9 ± 6.8 | 35.6 ± 5.8 | NA | 37.0 ± 4.4 | 38.2 ± 4.6 |
PCOS: polycystic ovary syndrome, SBP/DBP = systolic/diastolic blood pressure, NA = not available data, SDS = standardized deviation score, WHO = World Health Organization. Baseline characteristics in: n (%), mean (±: SD) or median with interquartile range (IQR): 25–75th percentile.
Outcomes in all children
The basic model revealed a lower birth weight in OPCOS versus controls (β = −129 (95%CI:−208—51), P < 0.01). Furthermore, a higher fasting insulin (β = 0.21(95%CI:0.03–0.40), P = 0.03) and 2 hour post-load insulin (β = 0.27(0.01–0.53), P = 0.04), HOMA-IR (β = 0.23(0.03–0.44), P = 0.02), triglycerides (β = 0.21(0.05–0.38), P = 0.01) and HDL-cholesterol (β = 0.31(0.09–0.54), P < 0.01) were identified in the OPCOS group (Table III). However, after correction for multiple testing only birthweight, triglycerides and HDL-cholesterol remained significant.
Table III. Cardiometabolic profile parameters recorded at all 885 first visits (229 males, 550 females), analyzed by using mixed model analysis unstratified for sex of the offspring.
| Outcomes | PCOS: n = 298 | Controls: n = 587 |
Basic model – Estimated difference: PCOS versus controls (95%CI) |
P | Adjusted model – Estimated difference: PCOS versus controls (95%CI) | Adjusted P |
|---|---|---|---|---|---|---|
| Mean (±) | ||||||
| Anthropometrics | ||||||
| Birth weight (g) | 3446(653) | 3555(554) | −129(−208 to −51) | <0.01*** | −116(−195 to −38) | <0.01*** |
| BMI SDS (WHO references) | 0.84(1.25) | 0.64(1.13) | 0.03(−0.05 to 0.12) | 0.68 | 0.03(−0.14 to 0.19) | 0.74 |
| Waist to height ratio (WtHR) | 0.08(1.21) | 0.08(1.01) | 0.03(−0.13 to 0.19) | 0.70 | 0.03(−0.13 to 0.18) | 0.73 |
| Waist SDS | 0.21(3.39) | 0.00(1.01) | 0.02(−0.14 to 0.18) | 0.81 | 0.01(−0.15 to 0.18) | 0.87 |
| SBP SDS | −0.15(1.25) | −0.16(1.16) | 0.12(−0.04 to 0.29) | 0.15 | 0.14(−0.03 to 0.31) | 0.11 |
| Endocrine markers | ||||||
| Fasting glucose SDS | −0.03(0.96) | −0.04(0.99) | 0.04(−0.14 to 0.22) | 0.68 | 0.04(−0.14 to 0.22) | 0.68 |
| Fasting insulin* SDS | 0.39(1.0) | −0.03(1.00) | 0.21(0.03 to 0.40) | 0.03 | 0.21(0.01 to 0.41) | 0.05 |
| HOMA-IR* SDS | 0.39(1.28) | −0.03(1.00) | 0.23(0.03 to 0.44) | 0.02 | 0.21(0.01 to 0.42) | 0.04 |
| Fasting 2 hour glucose SDS | −0.69(0.54) | −0.68(0.58) | −0.03(−0.13 to 0.08) | 0.64 | −0.02(−0.13 to 0.09) | 0.72 |
| Fasting 2 hour insulin* SDS | 0.29(1.29) | 0.02(1.04) | 0.27(0.01 to 0.53) | 0.04 | 0.20(−0.09 to 0.49) | 0.18 |
| Lipid profile | ||||||
| LDL-cholesterol SDS | −0.26(1.11) | −0.04(1.00) | −0.07(−0.26 to 0.11) | 0.46 | −0.09(−0.28 to 0.10) | 0.37 |
| Total cholesterol SDS | −0.10(1.03) | −0.01(0.99) | −0.01(−0.21 to 0.20) | 0.96 | −0.05(−0.25 to 0.15) | 0.66 |
| HDL-cholesterol SDS | 0.34(1.87) | 0.08(1.02) | 0.31(0.09 to 0.54) | <0.01*** | 0.31(0.08 to 0.54) | <0.01*** |
| Triglycerides (TG) SDS | 0.35(1.03) | −0.08(0.98) | 0.21(0.05 to 0.38) | 0.01*** | 0.19(0.02 to 0.36) | 0.03 |
| Cardiometabolic health | ||||||
| Metabolic sum score-1: BMI + SBP + INSULIN + TG ± HDL | 0.89(3.27) | −0.14(2.65) | 0.29(−0.40 to 0.61) | 0.38 | 0.30(−0.36 to 0.95) | 0.38 |
| Metabolic sum score-2: WtHR + SBP + Glucose + TG + −HDL | −0.52(3.33) | −0.82(2.24) | 0.08(−0.52 to 0.68) | 0.80 | 0.18(−0.43 to 0.80) | 0.56 |
* = square root of fasting insulin and HOMA-IR, ** = in the Methods section the rationale was postulated for the models used, *** = P-value remained significant after correction for multiple testing, Bold text = P-values below 0.05, HOMA-IR = ([fasting insulin (μU/ml)*fasting glucose (mmol/liter)]/405) (Matthews 1985)], SDS = z-score.
Outcomes are presented in standardized (except for birthweight) mean estimated differences with a 95%CI and P-value: offspring of women with PCOS versus controls. We tested a basic and an adjusted model, as follows.
Models used**: In the basic model (model 1), birthweight was adjusted for gestational age and country from which the children originated (USA, Chile or The Netherlands). And in the adjusted model (model 2), we additionally adjusted for sex, parity, multiple gestation and presence of siblings in this study.
In two variables, we calculated SDS using an external reference population: WHO-based BMI SDS and the CDC-based SBP. In the WHO-based BMI SDS, the age and sex of the child are taken into account in the basic model (model 3) and we additionally adjusted for country from which children originated. In the adjusted model (model 4), we also adjusted for parity, multiple gestation and presence of siblings in this study. In the CDC-based SBP SDS: sex, height and age were taken into account and we additionally adjusted for country from which children originated (model 5). In the adjusted model (model 6), we added similar factors as in BMI SDS, with the addition of the offspring weight.
For all other outcomes: in the basic model (model 7), we adjusted for: age of the child and the country from which the children originated (USA, Chile or The Netherlands). In the adjusted model (model 8), we additionally corrected for sex of the child, parity of the mother, multiple gestation and whether children had any siblings in the IPD included.
In all variables, with exception for birthweight, SDS was used.
P-value <0.017 was considered significant, as we had to correct our analysis for multiple testing (P-value of 0.017 was calculated as: 0.05 divided by 3).
Analysis with the adjusted model revealed that OPCOS (n = 298) exhibited increased plasma levels of fasting insulin (β = 0.21(95%CI:0.01–0.41), P = 0.05), insulin-resistance (β = 0.21(95%CI:0.01–0.42), P = 0.04), triglycerides (β = 0.19(95%CI:0.02–0.36), P = 0.03) and HDL-cholesterol concentrations (β = 0.31(95%CI: 0.08–0.54), P < 0.01), but reduced birthweight (β = −116(95%CI: −195 to 38), P < 0.01) compared to controls (n = 587). After correcting for multiple testing, only the differences in HDL-cholesterol and birthweight remained significant (Table III).
Effect modification by sex in metabolic profile in offspring of women with or without PCOS
We also investigated in the adjusted models whether effect modification by sex of the child played a role in the association between offspring status (PCOS mother or mother without PCOS) and cardiometabolic outcome. This was the case for 2 hour post-load insulin, LDL-cholesterol, total cholesterol, HDL-cholesterol and both metabolic sum scores (Table IV). However, after correction for multiple testing, only the interaction test for LDL-cholesterol, total cholesterol, HDL-cholesterol and metabolic sum score-1 remained significant. In brief, female OPCOS presented with lower LDL-cholesterol, lower total cholesterol and lower metabolic sum score-1 compared to female controls, compared to the mean difference among males. HDL-cholesterol differences were slightly larger in female OPCOS versus controls, compared to the difference among males (Table IV).
Table IV. Cardiometabolic profile parameters of all 885 first visits stratified for sex of the offspring and assessed by mixed model analysis.
| Outcomes | Male PCOS offspring versus controls: Estimated difference (95%CI) |
Female PCOS offspring versus controls: Estimate difference (95%CI) |
Interaction term for sex difference: PCOS versus controls P-value |
|---|---|---|---|
| Anthropometrics | |||
| Birthweight (grams) | −69(−174 to 35) | −126(−232 to 21) | 0.68 |
| BMI SDS: WHO reference | −0.10(−0.37 to 0.18) | 0.11(−0.21 to 0.59) | 0.45 |
| WtHR SDS | 0.03(−0.20 to 0.26) | 0.03(−0.18 to 0.24) | 0.73 |
| Waist SDS | −0.03(−0.28 to 0.21) | 0.05(−0.16 to 0.25) | 0.71 |
| SBP SDS | 0.30(−0.01 to 0.62) | 0.04(−0.16 to 0.25) | 0.09 |
| Endocrine markers | |||
| Fasting glucose SDS | 0.03(−0.20 to 0.27) | −0.01(−0.27 to 0.27) | 0.98 |
| Fasting insulin SDS | 0.11(−0.16 to 0.38) | 0.21(−0.08 to 0.49) | 0.88 |
| HOMA-IR SDS | 0.11(−0.16 to 0.37) | 0.22(−0.07 to 0.51) | 0.75 |
| Fasting 2 hour glucose SDS | −0.03(−0.16 to 0.10) | −0.02(−0.18 to 0.13) | 0.75 |
| Fasting 2 hour *insulin SDS | −0.20(−0.58 to 0.19) | 0.45(0.07 to 0.83) | 0.03 |
| Lipid profile | |||
| LDL-cholesterol SDS | 0.27(−0.03 to 0.57) | −0.39(−0.62 to −0.16) | <0.01*** |
| Total cholesterol SDS | 0.28(−0.01 to 0.56) | −0.31(−0.57 to −0.06) | 0.01*** |
| HDL-cholesterol SDS | 0.13(−0.05 to 0.31) | 0.53(0.18 to 0.88) | <0.01*** |
| TG SDS | 0.12(−0.11 to 0.34) | 0.26(0.01 to 0.51) | 0.52 |
| Cardiometabolic health | |||
| Metabolic sum score-1 BMI + SBP + INSULINE + TG + HDL | 0.85(−0.10 to 1.79) | −0.14(−1.05 to 0.77) | <0.01 * * * |
| Metabolic sum score-2: WtHR+SBP + Glucose + TG + HDL | 0.64(−0.17 to 1.45) | −0.19(−1.12 to 0.74) | 0.02 |
Outcomes are presented in mean estimated differences with a 95%CI: PCOS offspring versus controls. We tested whether sex of the child was a significant mediator, when comparing PCOS offspring versus controls.
* = square root of insulin, *** = P-value remained significant after correction for multiple testing. Bold text = P-values below 0.05.
Models used: In birthweight, we adjusted for country from which the children originated, gestational age, siblings in the dataset and multiple gestation.
In SBP, we adjusted for: country from which the children originated, gestational age, multiple gestation, siblings in the dataset, age of the child and BMI of the child. In all remaining parameters, we adjusted for country from which the children originated, gestational age, multiple gestation, siblings in the dataset and age of the child.
P-value < 0.017 was considered significant, as we had to correct our analysis for multiple testing (P-value of 0.017 was calculated as: 0.05 divided by 3). The P-value was the result of the interaction test for sex; we did not report mean estimated differences for the interaction test. The estimated differences (95%CI) presented in this table for males and females separately are the differences in male PCOS offspring versus male controls, and female PCOS offspring versus female controls. We refrained from the reporting of P-values for these secondary analyses.
Discussion
The current systematic review of the literature and subsequent IPD meta-analysis was designed to assess whether OPCOS present with less favorable cardiometabolic features compared to offspring of healthy controls. First, the adjusted IPD analyses of all initial offspring screenings (n = 885) demonstrated that OPCOS (n = 298) exhibited significantly increased fasting insulin and insulin resistance, HDL-cholesterol and triglyceride concentrations, but lower birthweight compared to controls (n = 587). However, after correction for multiple testing, only the mean differences in birthweight and HDL-cholesterol remained significant. Second, we identified significant effect modification by sex in 2 hour post-load insulin, LDL-cholesterol, total cholesterol, HDL-cholesterol and both metabolic sum scores. After correction for multiple testing, effect modification by sex was only statistically significant in LDL-cholesterol, total cholesterol, HDL-cholesterol and metabolic sum score-1. Only in the female offspring did we observe estimated differences (95%CI) that did not contain the neutral value; female OPCOS have a higher insulin concentration and HDL-cholesterol, but a lower LDL-cholesterol and total cholesterol compared to female controls.
This study demonstrates that PCOS and its associated features in the mothers have implications for offspring health, with potential sex-dependent alterations in metabolic profiles in childhood. These conclusions were based on data of individual studies of level IV evidence (data of case-control studies), which reflects the need for high-validity studies on the metabolic health of children from mothers with PCOS (Sackett, 1989).
In the current study, we also investigated whether birthweight differed between OPCOS and controls. Birthweight is of interest due to its direct link with cardiovascular disease (CVD) later in life and in adulthood (Ibanez et al., 2011). Conditions of the intra-uterine environment are partially reflected in birthweight (Barker et al., 1989). The lower birthweight observed in OPCOS compared to controls is in agreement with a meta-analysis conducted earlier by our research group involving both high- and low-quality studies (Boomsma et al., 2006). This effect could be mediated to some extent by an increased incidence of pre-eclampsia next to maternal metabolic dysfunction (Boomsma et al., 2006; Christ et al., 2018). The definition of low birthweight according to WHO is a birthweight below 2500 g, independent of gestational age. Only 3.6% of all infants in our study had a low birthweight; 5.1% in the OPCOS and 2.9% in the controls. This difference was not statistically significant. Therefore, we do not expect the cardiovascular profiles to deviate solely because of differences in birthweight, in this study (WHO, 2012).
BMI, waist-to-height-ratio, waist circumference and blood pressure in OPCOS were comparable to the measurements in controls, despite the well-known increased incidence of obesity among adult women diagnosed with PCOS (Teede et al., 2013). Only one of the included Chilean studies reported that BMI of OPCOS was significantly higher compared to the BMI of controls (Recabarren et al., 2008). Waist circumference in Dutch children participating in the current study was smaller compared to the American and Chilean offspring, and blood pressure was systematically higher in Dutch and American compared to Chilean offspring. Differences in BMI and blood pressure between studies potentially reflect the influence of intercontinental differences in the IPD meta-analysis, which were considered in our analyses by correcting for the continent the offspring originated from. The reference data we used for BMI from WHO were based on a multi-ethnic dataset with children from Brazil, Ghana, India, Norway, Oman and the USA. We believe that since North-America, South-America and North-Europe were represented in this reference data, generalizability of the reference data to the IPD meta-analysis study population was warranted (WHO, 2006, 2011). The CDC data, which were used as reference data for blood pressure, were retrieved from a multi-ethnic American population, in which all races were represented (National Institutes of Health, 2004). Therefore, we also expect reasonable generalizability of this reference data to our IPD meta-analysis study population.
After correction for multiple testing, we could not confirm a difference in insulin resistance in the total OPCOS population versus the controls. However, the increased 2 hour post-load insulin concentrations in female OPCOS might have implications later in life. For instance, the association between insulin concentrations during childhood and later life onset of type 2 diabetes mellitus has been investigated repeatedly (Morrison et al., 2011) and gave rise to conflicting results regarding the age at which such an association could be identified. Nonetheless, a significant association of increased insulin concentrations during childhood and later life type 2 diabetes mellitus, has been demonstrated regardless of BMI (Nguyen et al., 2010; Morrison et al., 2011; Sabin et al., 2015).
The higher triglyceride concentrations observed in OPCOS may seem unfavorable. Nevertheless, increased lipid levels during childhood do not appear to predict unfavorable lipid profiles in adulthood (Lozano et al., 2016). We observed lower LDL-cholesterol and total cholesterol concentrations in female OPCOS in comparison with female controls. HDL-cholesterol concentrations in female OPCOS seem higher in daughters of women with PCOS compared to controls. The higher HDL-cholesterol in OPCOS might seem contradictory, since HDL-cholesterol may play a protective role in developing CVD in later life (Assmann and Gotto, 2004). A Scandinavian study, however, suggests that the adults with the highest ranges of HDL-cholesterol actually may have an increased chance for CVD (Madsen et al., 2017). This is a potential explanation for our finding. But caution is warranted, since our study does not provide sufficient data to predict lipid profiles of OPCOS in adulthood. It also should be noted that there may be a sexual dimorphism regarding the expression of both insulin and lipids in the offspring of women diagnosed with PCOS, with an early appearance of hyperlipidemia and hyperinsulinemia in girls and a normal insulin and lipid profile in boys. This sexual dimorphism in both insulin and lipids has been reported earlier in normal adolescent girls compared to boys (Barja et al., 2013). Thus, biomarkers in daughters and sons of women with PCOS seem to be modulated in part by the naturally occurring biological differences related to sex (Kirchengast and Marosi, 2008; Marceau et al., 2011; Dearden et al., 2018). Sex differences in physical activity could also influence cardiometabolic outcome in offspring (Andersen et al., 2006). Supporting for this presumed sexual dimorphism comes from the higher 2 hour post-load insulin in OPCOS females compared to male OPCOS (Supplementary Table SIV).
It has been hypothesized that offspring health is determined by an interplay between genetic and environmental factors (Horwitz and Neiderhiser, 2011). The Barker hypothesis proposes that early genetic adaptation to suboptimal conditions in utero may translate into adverse health later in life (Baker et al., 2007). The onset of CVD has been observed in childhood. For instance, a post-mortem study in human adolescents and young adults who died from external injury, revealed the existence of manifest atherosclerosis early in life (PDAY Research Group, 1993). In contrast to these findings, we were unable to observe an increased metabolic sum score during childhood in OPCOS compared to controls. Our sample size may still be too small to detect subtle differences. We used a composite outcome: two variants of the metabolic sum score (arbitrarily defined as the sum of BMI or waist-to-height ratio, SBP, fasting and post-load insulin or glucose, triglycerides and HDL-cholesterol (metabolic sum score-1), or the sum of waist-to-height ratio, SBP, glucose, triglycerides, and HDL-cholesterol (metabolic sum score-2)) to mimic the multifactorial origin of CVD, as previously described ((Poulter, 1999), personal communication). Both vascular and metabolic factors contribute to the onset of CVD ((Poulter, 1999), personal communication).
The mechanisms underlying potential differences between OPCOS and healthy controls are diverse and incompletely understood (Homburg et al., 2017). Maternal overweight induces the transport of glucose, free fatty acids and amino acids to the fetus (Whitaker and Dietz, 1998). Metabolic and adipocyte function could thereby be altered and influence the development of offspring (de Ferranti and Mozaffarian, 2008). Conflicting theories have been put forward regarding the role of maternal androgens. It is suggested that hyperandrogenemia of the mother has a limited influence on the fetus due to the placental aromatase activity, which converts maternal androgens to estrogens (Simpson, 2002). However, the changing activities of placental enzymes diminish the conversion of androgens to estrogens, which could in theory lead to an increased testosterone supply from the placenta. This theory was not confirmed in two studies in which cord-blood testosterone was measured with liquid chromatography–tandem mass spectrometry assays (Caanen et al., 2016; Daan et al., 2017). Studies in women with PCOS revealed macroscopic and microscopic alterations of the placenta, suggesting a deviant intrauterine environment compared to healthy controls (Maliqueo et al., 2013; Palomba et al., 2013). A small study of PCOS suggested that amniotic fluid androgen concentrations were elevated (Palomba et al., 2012). This was only observed in women pregnant of a female fetus, again suggesting potential sexual dimorphism (Palomba et al., 2012). Unfortunately, our data do not allow the elucidation of any causal mechanism for the alterations in OPCOS.
Owing to the age criteria applied in this IPD meta-analysis, puberty does play a role in this study. It is well known that puberty affects serum markers and, specifically, an early onset of puberty could influence the cardiometabolic profile (Ibanez et al., 2014). Of the included studies, we know that the Chilean research group excluded girls with precocious pubarche. Data on puberty of the offspring were recorded in the American and Chilean offspring only and reported in our baseline table (Table II). Tanner stages across studies appeared to be quite similar. Dutch OPCOS were included at 2.5–4 and 6–8 years of age, therefore, we refrained from recording there pubertal status. We did not use Tanner stages in our analyses due to the selective reporting and missing values in the Tanner data in the included studies. Another reason for this was the inconsistent data on age at menarche in women with PCOS themselves. A recent large Scandinavian cohort study does not confirm a lower age at menarche in women with PCOS compared to controls, as often suggested (Welt and Carmina, 2013; Koivuaho et al., 2019).
To the best of our knowledge, the current study represents the first IPD meta-analysis concerning cardiometabolic health in OPCOS. Rigorous methodology was applied when analyzing the data. Presumably due to the large sample size we were able to detect distinct sex-differences, while previous individual studies among OPCOS mainly focused on females, with often limited sample size (Sir-Petermann et al., 2007, 2009; Kent et al., 2008; Wilde et al., 2018).
Several limitations should also be considered when interpreting our study results. In the current study, we used international external reference sources to calculate sex- and age-dependent SDS for BMI and SBP, which represents both strength and a limitation. The additional correction for sex by using interaction terms and stratification methods may have resulted in an underestimation of differences between males and females. On the other hand, the external reference sources do increase the external validity to other study populations.
The stratified analyses in male and female offspring suggest that females are influenced more compared to males by having mothers with PCOS. It could also be the cases that we did not observe any differences among males because of a lower number of male offspring in our dataset.
Another limitation is the limited data obtained on the mode of conception, precluding the assessment of a possible influence of infertility treatment per se. The Chilean study group reported that only children who were conceived naturally were eligible for participation in the follow-up study (Recabarren et al., 2008).
Further details on pregnancies and parental health were not available. Therefore, we were not able to detect differences in familial or genetic predisposition for CVD between OPCOS and controls. It is plausible that a compromised familial history on CVD does encourage participation in an offspring follow-up study and introduces a selection bias.
Last, we must emphasize that we were not able to rule out any influence of sampling time differences and inter-assay variability on serum markers. We were not able to analyze one similar sample in every participating laboratory and with the same assay used in all the studies. We minimized the effect of different assay use by applying a mixed effect model, in which we added a random effect for country of origin of the child.
In conclusion, we observed in the current IPD meta-analysis of children born from women diagnosed with PCOS subtle signs of a compromised cardiometabolic health, predominantly in female offspring. The unfavorable cardiovascular profile of women with PCOS at childbearing age may—next to a genetic predisposition—influence health of their offspring.
It appears crucial to be able to make a distinction between the effects of a genetic predisposition and suboptimal conditions during pregnancy when aiming to improve the future health of OPCOS (Colilla et al., 2001; Franks, 2002). To achieve this, more high validity follow-up studies on OPCOS are necessary with clearly defined endpoints on cardiometabolic health.
Acknowledgements
We would like to thank Dr Barbara Echiburu of the departments of Endocrinology and Metabolism and the Unit of Endocrinology of the University of Chile, for her outstanding work in the offspring follow-up studies of which the data were used in this IPD meta-analysis. We thank Dr Paulien Wiersma information and collection specialist of the Utrecht University Library for her expertise in co-designing the systematic search string. Last, we thank Dr Suzanne Veltman-Verhulst who was involved in the design of the follow-up study on Dutch OPCOS.
Authors’ roles
M.N.G., B.C.J.M.F., B.B.v.R. and C.S.P.M.U. were involved in the design of the study. M.N.G., J.P.C. and M.A.d.W. performed the article selection and quality assessment of the retrieved articles. B.F. was involved in the article selection procedure when consensus on final article selection was not achieved. M.N.G., C.S.P.M.U, T.S-P, N.C., M.A.d.W., A.R.K. and R.S.L. were involved in retrieving the original data and data management. M.N.G., B.C.J.M.F., W.d.J. and M.J.C.E. were involved in data analyses and interpretation of the data. M.N.G., B.C.J.M.F. and N.C. were involved in drafting the article. M.N.G., T.S.-P., N.C., B.v.R. M.A.d.W., J.P.C., C.S.P.M.U. W.d.J. M.J.C.E. A.R.K. R.S.L. and B.C.J.M.F. revised the manuscript critically for important intellectual content. All authors were involved in the writing of the article and approved its final version.
Funding
This study was funded by the UMC Utrecht (strategic impulse child health), and the Dutch Heart Foundation (grant number 2013T083).
Conflict of interest
Dr Gunning reports personal fees (congress travel funding) from Merck, personal fees (congress travel funding) from Gedeon Richter, research grants from Dutch heart foundation, outside the submitted work. Dr W. de Jager is employee of Luminex. B.V. Mr Kunselman reports stock ownership in Merck. Prof. Legro received consulting fees and grant support from AbbVie, Bayer, Endocrine Society, Euroscreen/Ogeda, Ferring, Fractyl, Guerbet, Kindex, Milendo and the National Institutes of Health. During the most recent 5-year period Prof. Fauser received fees and grant support from the following entities (in alphabetic order); Abbott, Controversies in Obstetrics & Gynecology (COGI), Dutch Heart Foundation (Hartstichting), Dutch Medical Research Council (ZonMW), Euroscreen/Ogeda, Ferring, London Womens Clinic (LWC), Menogenix, Myovant, OvaScience, Pantharei Bioscience, PregLem/Gedeon Richter, Reproductive Biomedicine Online (RBMO), Teva/Theramex, World Health Organisation (WHO). Prof. Sir-Petermann, Dr N. Crisosto, Dr M.A. de Wilde, Dr C.S.P.M. Uiterwaal and Prof. Eijkemans have no disclosures to report.
Supplementary Material
References
- Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, Anderssen SA. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (the European youth heart study). Lancet (London, England) 2006;368:299–304. [DOI] [PubMed] [Google Scholar]
- Anderson H, Fogel N, Grebe SK, Singh RJ, Taylor RL, Dunaif A. Infants of women with polycystic ovary syndrome have lower cord blood androstenedione and estradiol levels. J Clin Endocrinol Metab 2010;95:2180–2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assmann G, Gotto AMJ. HDL cholesterol and protective factors in atherosclerosis. Circulation 2004;109:III8–III14. [DOI] [PubMed] [Google Scholar]
- Baker JL, Olsen LW, Sorensen TIA. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med 2007;357:2329–2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barja S, Barrios X, Arnaiz P, Dominguez A, Villarroel L, Castillo O, Farias M, Ferreccio C, Mardones F. Blood lipids in Chilean children 10-14 years of age. Nutr Hosp 2013;28:719–725. [DOI] [PubMed] [Google Scholar]
- Barker DJ, Osmond C, Golding J, Kuh D, Wadsworth ME. Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ 1989;298:564–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boomsma CM, Eijkemans MJC, Hughes EG, Visser GHA, Fauser BCJM. Macklon NS. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum Reprod Update 2006;12:673–683. [DOI] [PubMed] [Google Scholar]
- Caanen M, Kuijper E, Hompes P, Kushnir M, Rockwood A, Meikle W, Homburg R, Lambalk C. Mass spectrometry methods measured androgen and estrogen concentrations during pregnancy and in newborns of mothers with polycystic ovary syndrome. Eur J Endocrinol 2016;174:25–32. [DOI] [PubMed] [Google Scholar]
- Carey AH, Chan KL, Short F, White D, Williamson R, Franks S. Evidence for a single gene effect causing polycystic ovaries and male pattern baldness. Clin Endocrinol (Oxf) 1993;38:653–658. [DOI] [PubMed] [Google Scholar]
- Chen S-Y, Feng Z, Yi X. A general introduction to adjustment for multiple comparisons. J Thorac Dis 2017;9:1725–1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christ JP, Gunning MN, Meun C, Eijkemans MJC, van Rijn BB, Bonsel GJ, Laven JSE, Fauser BCJM. Pre-conception characteristics predict obstetrical and neonatal outcomes in women with polycystic ovary syndrome. J Clin Endocrinol Metab 2019;104:809–818. [DOI] [PubMed] [Google Scholar]
- Christ JP, Gunning MN, Meun C, Eijkemans MJC, Van Rijn BB, Bonsel GJ, Laven JSE, Fauser BCJM. Pre-conception characteristics predict obstetrical and neonatal outcomes in women with polycystic ovary syndrome. J Clin Endocrinol Metab 2018;104. [DOI] [PubMed] [Google Scholar]
- Colilla S, Cox N, Ehrmann D. Heritability of insulin secretion and insulin action in women with polycystic ovary syndrome and their first degree relatives. J Clin Endocrinol Metab 2001;86:2027–2031. [DOI] [PubMed] [Google Scholar]
- Crisosto N, Codner E, Maliqueo M, Echiburú B, Sánchez F, Cassorla F, Sir-Petermann T. Anti-Müllerian hormone levels in peripubertal daughters of women with polycystic ovary syndrome. J Clin Endocrinol Metab 2007;92:2739–2743. [DOI] [PubMed] [Google Scholar]
- Daan NMP, Koster MPH, Steegers-Theunissen RP, Eijkemans MJC, Fauser BCJM. Endocrine and cardiometabolic cord blood characteristics of offspring born to mothers with and without polycystic ovary syndrome. Fertil Steril 2017;107:261–268.e3. [DOI] [PubMed] [Google Scholar]
- Daniels SR. Cardiovascular disease risk factors and atherosclerosis in children and adolescents. Curr Atheroscler Rep 2001;3:479–485. [DOI] [PubMed] [Google Scholar]
- Day F, Karaderi T, Jones MR, Meun C, He C, Drong A, Kraft P, Lin N, Huang H, Broer L et al. . Large-scale genome-wide meta-analysis of polycystic ovary syndrome suggests shared genetic architecture for different diagnosis criteria. PLoS Genet 2018;14:e1007813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Ferranti S, Mozaffarian D. The perfect storm: obesity, adipocyte dysfunction, and metabolic consequences. Clin Chem 2008;54:945–955. [DOI] [PubMed] [Google Scholar]
- de Wilde MA, Eising JB, Gunning MN, Koster MPH, Evelein AMV, Dalmeijer GW, Uiterwaal CSPM, Eijkemans MJC, van der Ent CK, Meijboom FJ et al. . Cardiovascular and metabolic health of 74 children from women previously diagnosed with polycystic ovary syndrome in comparison with a population-based reference cohort. Reprod Sci 2018;25:1492–1500. [DOI] [PubMed] [Google Scholar]
- Dearden L, Bouret SG, Ozanne SE. Sex and gender differences in developmental programming of metabolism. Mol Metab 2018;15:8–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodic M, Abouantoun T, O’Connor A, Wintour EM, Moritz KM. Programming effects of short prenatal exposure to dexamethasone in sheep. Hypertens (Dallas, Tex 1979) 2002;40:729–734. [DOI] [PubMed] [Google Scholar]
- Dodic M, May CN, Wintour EM, Coghlan JP. An early prenatal exposure to excess glucocorticoid leads to hypertensive offspring in sheep. Clin Sci (Lond) 1998;94:149–155. [DOI] [PubMed] [Google Scholar]
- Eisenmann JC. On the use of a continuous metabolic syndrome score in pediatric research. Cardiovasc Diabetol 2008;7:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauser BCJM, Tarlatzis BC, Rebar RW, Legro RS, Balen AH, Lobo R, Carmina E, Chang J, Yildiz BO, Laven JSE, et al. Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-sponsored 3rd PCOS consensus workshop group. Fertil Steril 2012;97:28–38.e25. [DOI] [PubMed] [Google Scholar]
- Franks S. Adult polycystic ovary syndrome begins in childhood. Best Pract Res Clin Endocrinol Metab 2002;16:263–272. [DOI] [PubMed] [Google Scholar]
- Gaillard R, Steegers EAP, Duijts L, Felix JF, Hofman A, Franco OH, Jaddoe VWV. Childhood cardiometabolic outcomes of maternal obesity during pregnancy: the generation R study. Hypertens (Dallas, Tex 1979) 2014;63:683–691. [DOI] [PubMed] [Google Scholar]
- Haney EM, Huffman LH, Bougatsos C, Freeman M, Steiner RD, Nelson HD. Screening and treatment for lipid disorders in children and adolescents: systematic evidence review for the US preventive services task force. Pediatrics 2007;120:e189–e214. [DOI] [PubMed] [Google Scholar]
- Homburg R, Gudi A, Shah A, Layton M. A novel method to demonstrate that pregnant women with polycystic ovary syndrome hyper-expose their fetus to androgens as a possible stepping stone for the developmental theory of PCOS. A pilot study. Reprod Biol Endocrinol 2017;15:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz BN, Neiderhiser JM. Gene - environment interplay, family relationships, and child adjustment. J Marriage Fam 2011;73:804–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibanez L, Lopez-Bermejo A, Diaz M, Marcos MV. Endocrinology and gynecology of girls and women with low birth weight. Fetal Diagn Ther 2011;30:243–249. [DOI] [PubMed] [Google Scholar]
- Ibanez L, Ong KK, Lopez-Bermejo A, Dunger DB, de Zegher F. Hyperinsulinaemic androgen excess in adolescent girls. Nat Rev Endocrinol 2014;10:499–508. [DOI] [PubMed] [Google Scholar]
- Kahsar-Miller MD, Nixon C, Boots LR, Go RC, Azziz R. Prevalence of polycystic ovary syndrome (PCOS) in first-degree relatives of patients with PCOS. Fertil Steril 2001;75:53–58. [DOI] [PubMed] [Google Scholar]
- Kent SC, Gnatuk CL, Kunselman AR, Demers LM, Lee PA, Legro RS. Hyperandrogenism and hyperinsulinism in children of women with polycystic ovary syndrome: a controlled study. J Clin Endocrinol Metab 2008;93:1662–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kermack AJ, Van Rijn BB, Houghton FD, Calder PC, Cameron IT, Macklon NS. The “developmental origins” hypothesis: relevance to the obstetrician and gynecologist. J Dev Orig Health Dis 2015;6:415–424. [DOI] [PubMed] [Google Scholar]
- Kirchengast S, Marosi A. Gender differences in body composition, physical activity, eating behavior and body image among normal weight adolescents--an evolutionary approach. Coll Antropol 2008;32:1079–1086. [PubMed] [Google Scholar]
- Koivuaho E, Laru J, Ojaniemi M, Puukka K, Kettunen J, Tapanainen JS, Franks S, Jarvelin M-R, Morin-Papunen L, Sebert S et al. . Age at adiposity rebound in childhood is associated with PCOS diagnosis and obesity in adulthood-longitudinal analysis of BMI data from birth to age 46 in cases of PCOS. Int J Obes (Lond) 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon EJ, Kim YJ. What is fetal programming? A lifetime health is under the control of in utero health. Obstet Gynecol Sci 2017;60:506–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legro RS, Driscoll D, Strauss JF 3rd, Fox J, Dunaif A. Evidence for a genetic basis for hyperandrogenemia in polycystic ovary syndrome. Proc Natl Acad Sci U S A 1998;95:14956–14960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legro RS, Kunselman AR, Stetter CM, Gnatuk CL, Estes SJ, Brindle E, Vesper HW, Botelho JC, Lee PA, Dodson WC. Normal pubertal development in daughters of women with PCOS: a controlled study. J Clin Endocrinol Metab 2017;102:122–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano P, Henrikson NB, Morrison CC, Dunn J, Nguyen M, Blasi PR, Whitlock EP. Lipid screening in childhood and adolescence for detection of multifactorial dyslipidemia: evidence report and systematic review for the US preventive services task force. JAMA 2016;316:634–644. [DOI] [PubMed] [Google Scholar]
- Madsen CM, Varbo A, Nordestgaard BG. Extreme high high-density lipoprotein cholesterol is paradoxically associated with high mortality in men and women: two prospective cohort studies. Eur Heart J 2017;38:2478–2486. [DOI] [PubMed] [Google Scholar]
- Maliqueo M, Sir-Petermann T, Perez V, Echiburu B, Ladron de Guevara A, Galvez C, Crisosto N, Azziz A. Adrenal Function during Childhood and Puberty in Daughters of Women with Polycystic Ovary Syndrome. J Clin Endocrinol Metab September 2009;94:3282–3288. [DOI] [PubMed] [Google Scholar]
- Maliqueo M, Lara HE, Sanchez F, Echiburu B, Crisosto N, Sir-Petermann T. Placental steroidogenesis in pregnant women with polycystic ovary syndrome. Eur J Obstet Gynecol Reprod Biol 2013;166:151–155. [DOI] [PubMed] [Google Scholar]
- Marceau K, Ram N, Houts RM, Grimm KJ, Susman EJ. Individual differences in boys’ and girls’ timing and tempo of puberty: modeling development with nonlinear growth models. Dev Psychol 2011;47:1389–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–419. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DJ. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;21:6–e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran LJ, Misso ML, Wild RA, Norman RJ. Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update 2010;16:347–363. [DOI] [PubMed] [Google Scholar]
- Morrison JA, Glueck CJ, Daniels S, Wang P, Stroop D. Adolescent oligomenorrhea in a biracial schoolgirl cohort: a simple clinical parameter predicting impaired fasting glucose plus type 2 diabetes mellitus, insulin, glucose, insulin resistance, and centripetal obesity from age 19 to 25 years. Metabolism 2011;60:1285–1293. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health National Heart Lung and blood institute. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114:555–576. [PubMed] [Google Scholar]
- Natural history of aortic and coronary atherosclerotic lesions in youth. Findings from the PDAY Study Pathobiological determinants of atherosclerosis in youth (PDAY) research group. Arterioscler Thromb J Vasc Biol 1993;13:1291–1298. [DOI] [PubMed] [Google Scholar]
- Nguyen QM, Srinivasan SR, Xu J-H, Chen W, Kieltyka L, Berenson GS. Utility of childhood glucose homeostasis variables in predicting adult diabetes and related cardiometabolic risk factors: the Bogalusa heart study. Diabetes Care 2010;33:670–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oostvogels AJJM, Stronks K, Roseboom TJ, van der Post JAM, van Eijsden M, Vrijkotte TGM. Maternal prepregnancy BMI, offspring’s early postnatal growth, and metabolic profile at age 5–6 years: the ABCD study. J Clin Endocrinol Metab 2014;99:3845–3854. [DOI] [PubMed] [Google Scholar]
- Paauw ND, van Rijn BB, Lely AT, Joles JA. Pregnancy as a critical window for blood pressure regulation in mother and child: programming and reprogramming. Acta Physiol (Oxf) 2017;219:241–259. [DOI] [PubMed] [Google Scholar]
- Palomba S, de Wilde MA, Falbo A, Koster MPH, La Sala GB, Fauser BCJM. Pregnancy complications in women with polycystic ovary syndrome. Hum Reprod Update 2015;21:575–592. [DOI] [PubMed] [Google Scholar]
- Palomba S, Marotta R, Di Cello A, Russo T, Falbo A, Orio F, Tolino A, Zullo F, Esposito R, La Sala GB. Pervasive developmental disorders in children of hyperandrogenic women with polycystic ovary syndrome: a longitudinal case-control study. Clin Endocrinol (Oxf) 2012;77:898–904. [DOI] [PubMed] [Google Scholar]
- Palomba S, Russo T, Falbo A, Di Cello A, Tolino A, Tucci L, La Sala GB, Zullo F. Macroscopic and microscopic findings of the placenta in women with polycystic ovary syndrome. Hum Reprod 2013;28:2838–2847. [DOI] [PubMed] [Google Scholar]
- Poulter N. Coronary heart disease is a multifactorial disease. Am J Hypertens 1999;12:92S–95S. [DOI] [PubMed] [Google Scholar]
- Recabarren SE, Sir-Petermann T, Rios R, Maliqueo M, Echiburu B, Smith R, Rojas-Garcia P, Recabarren M, Rey RA. Pituitary and testicular function in sons of women with polycystic ovary syndrome from infancy to adulthood. J Clin Endocrinol Metab 2008;93:3318–3324. [DOI] [PubMed] [Google Scholar]
- Regnault N, Gillman MW, Rifas-Shiman SL, Eggleston E, Oken E. Sex-specific associations of gestational glucose tolerance with childhood body composition. Diabetes Care 2013;36:3045–3053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Review Manager, version 5 Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. Available at: https://community.cochrane.org/sites/default/files/uploads/inline-files/RevMan_5.3_User_Guide.pdf. [Google Scholar]
- Reynolds MF, Sisk EC, Rasgon NL. Valproate and neuroendocrine changes in relation to women treated for epilepsy and bipolar disorder: a review. Curr Med Chem 2007;14:2799–2812. [DOI] [PubMed] [Google Scholar]
- Sabin MA, Magnussen CG, Juonala M, Shield JPH, Kahonen M, Lehtimaki T, Ronnemaa T, Koskinen J, Loo B-M, Knip M et al. . Insulin and BMI as predictors of adult type 2 diabetes mellitus. Pediatrics 2015;135:e144–e151. [DOI] [PubMed] [Google Scholar]
- Sackett DL. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest 1989;95:2S–4S. [PubMed] [Google Scholar]
- Simpson ER. Aromatization of androgens in women: current concepts and findings. Fertil Steril 2002;77:S6–S10. [DOI] [PubMed] [Google Scholar]
- Singh AS, Mulder C, Twisk JWR, van Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008;9:474–488. [DOI] [PubMed] [Google Scholar]
- Sir-Petermann T, Codner E, Perez V, Echiburu B, Maliqueo M, Ladron de Guevara A, Preisler J, Crisosto N, Sanchez F, Cassorla F et al. . Metabolic and reproductive features before and during puberty in daughters of women with polycystic ovary syndrome. J Clin Endocrinol Metab 2009;94:1923–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sir-Petermann T, Maliqueo M, Codner E, Echiburu B, Crisosto N, Perez V, Perez-Bravo F, Cassorla F, S-P T, M M et al. . Early metabolic derangements in daughters of women with polycystic ovary syndrome. J Clin Endocrinol Metab 2007;92:4637–4642. [DOI] [PubMed] [Google Scholar]
- Teede HJ, Joham AE, Paul E, Moran LJ, Loxton D, Jolley D, Lombard C. Longitudinal weight gain in women identified with polycystic ovary syndrome: results of an observational study in young women. Obesity (Silver Spring) 2013;21:1526–1532. [DOI] [PubMed] [Google Scholar]
- Urbanek M, Legro RS, Driscoll DA, Azziz R, Ehrmann DA, Norman RJ, Strauss JF 3rd, Spielman RS, Dunaif A. Thirty-seven candidate genes for polycystic ovary syndrome: strongest evidence for linkage is with follistatin. Proc Natl Acad Sci U S A 1999;96:8573–8578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells G, O’Connell S, Petersen J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Canada: Department of Epidemiology and Community Medicine, University of Ottawa; 2014. Available at:http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. [Google Scholar]
- Welt CK, Carmina E. Clinical review: lifecycle of polycystic ovary syndrome (PCOS): from in utero to menopause. J Clin Endocrinol Metab 2013;98:4629–4638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitaker RC, Dietz WH. Role of the prenatal environment in the development of obesity. J Pediatr 1998;132:768–776. [DOI] [PubMed] [Google Scholar]
- WHO WHO Anthro Version 3.2.2. Child Growth Standards. 2011. Available at: https://www.who.int/childgrowth/software/en/.
- WHO Multicentre Growth Reference Study. WHO Child Growth Standards. Length, Height for-Age, Weightfor-Age, Weight-for-Length and Body Mass Index-for Age. Methods and Development. Geneva: World Health Organization; 2006. Available at: https://www.who.int/childgrowth/standards/Technical_report.pdf. [Google Scholar]
- WHO. Resolution WHA65.6. Comprehensive implementation plan on maternal, infant and young child nutrition In: Sixty-fifth World Health Assembly Geneva, 21–26 May 2012. Resolutions and decisions, annexes. Geneva: World Health Organization; 2012:12–13. [Google Scholar]
- Williams T, Mortada R, Diagnosis PS. Treatment of polycystic ovary syndrome. Am Fam Physician 2016;94:106–113. [PubMed] [Google Scholar]
- Yu Z, Han S, Zhu J, Sun X, Ji C, Guo X. Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS One 2013;8:e61627. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


