Abstract
E-cig use is continuing to increase, particularly among youth never-smokers, and is used by some smokers to quit. The acute and chronic toxicity of e-cig use is unclear generally in the context of increasing reports of inflammatory-type pneumonia in some e-cig users. To assess lung effects of e-cigs without nicotine or flavors, we conducted a pilot study with serial bronchoscopies over 4 weeks in 30 never-smokers, randomized either to a four-week intervention with the use of e-cigs containing only 50% propylene glycol (PG) and 50% vegetable glycerine (VG) or to a no-use control group. Compliance to the e-cig intervention was assessed by participants sending daily puff counts and by urinary propylene glycol (PG). Inflammatory cell counts and cytokines were determined in bronchoalveolar lavage (BAL) fluids. Genome-wide expression, microRNA, and mRNA were determined from bronchial epithelial cells. There were no significant differences in changes of BAL inflammatory cell counts or cytokines between baseline and follow-up, comparing the control and e-cig groups. However, in the intervention but not the control group, change in urinary PG as a marker of e-cig use and inhalation, was significantly correlated with change in cell counts (cell concentrations, macrophages, and lymphocytes) and cytokines (IL-8, IL-13, and TNF-α), although the absolute magnitude of changes was small. There were no significant changes in mRNA or microRNA gene expression. Although limited by study size and duration, this is the first experimental demonstration of an impact of e-cig use on inflammation in the human lung among never-smokers.
Trial registry
ClinicalTrials.gov; No.: ; URL: www.clinicaltrials.gov.
Keywords: Electronic cigarettes, inflammation, clinical trial, gene expression, lung
INTRODUCTION
Use of electronic cigarettes (e-cigs) is increasingly popular among both smokers and never-smokers (1). Among youth in particular, use is sharply increasing. From 2017 to 2018, current e-cig use increased 78% (from 11.7 to 20.8%) and 48% (from 3.3% to 4.9%) by high- and middle-school students respectively (2). Overall, about 67% of current e-cig adult users are current smokers and about 60% of smokers have tried e-cigs (3,4). However, possible e-cig toxicity is not well understood. Constituents of e-liquids, including propylene glycol (PG) and vegetable glycerine (VG) as solvent carriers for flavors and nicotine in e-liquids are “generally regarded as safe” by the Food and Drug Administration (FDA) when used in foods and cosmetics. It is not known what effects they have, if any, when heated and inhaled from e-cigs.
The acute and chronic health effects of e-cig use is unclear, and there are an increasing and alarming reports of inflammatory-type pneumonias in e-cig users (5–7). E-aerosols from PG and VG contain more than 100 volatile organic compounds, including propylene oxide, acrolein, acetaldehyde, and formaldehyde with varied toxic properties. (8) There is in vitro evidence that e-cig aerosol exposure can lead to increased inflammatory cytokine production (9), oxidative stress response (10), neutrophil inflammatory response (11), DNA damage (12) and altered gene expression (13). In experimental animal studies, unheated PG or VG have minimal lung toxicity. (14) However, when delivered from e-cigs, there are measurable increases in lung inflammatory infiltrates, cytokines, infections, reactive oxygen species and gene expression (9,15,16). Because of increasing use of e-cigs by never smokers, there is a critical need to understand their biological effects on the lung in this group. To date, there has been only one clinical trial examining human lung biomarkers for e-cig use in healthy never smokers. Exposure to 20 puffs during approximately one hour resulted in changes in gene expression (17). Human data regarding e-cig effects for longer use are needed. To better understand health effects of e-cigs, focusing on the solvent carriers e-liquid constituents, we conducted a pilot clinical trial of never-smokers randomized to nicotine- and flavor-free e-cigs, examining lung inflammation and gene expression.
MATERIALS AND METHODS
The overview of the study design is shown in Supplementary Figure 1.
Study Participants
This study underwent concept-review by the National Cancer Institute, the Food and Drug Administration, and peer review through Ohio State University Intramural Research Program. The OSU Clinical Scientific Research Committee and the Institutional Review Board approved the study protocol (ClinicalTrials.gov: ). All procedures and data were followed by ethical guidelines and monitored by an external Data Safety and Monitoring Board.
Full inclusion and exclusion criteria are described in Supplementary Methods. Briefly, subjects, age 21–30, were healthy never-smokers (n=30) (had smoked less than 100 cigarettes in their lifetime) and had not used an e-cig or cigarette in the past year. Participants were excluded if they had a history of significant medical problems including lung disease, general anesthesia or bronchoscopy within the previous year, recent drug use, use of other combustible tobacco within the past year, pregnancy, or any other medical disorder that would affect their bronchoscopy risk (e.g., BMI>40) or would affect the biomarkers.
Procedures
Participants were recruited between 2015 and 2017 from local print and television media, the OSU Study Search website, the Research Match website, the OSU Tobacco Centers of Regulatory Science Participant Registry, and Craigslist. After an orientation session, eligibility evaluation, informed written consent and medical evaluation, a bronchoscopy was performed. Lung samples were collected by bronchial alveolar lavage (BAL) for inflammatory cells and cytokines, and bronchial brushings from normal appearing epithelium for gene expression assays. Bronchoscopies were performed consistent with current standards of care at OSU. Subjects were randomized to receive the BAL and brushing on the right or left side; follow-up bronchoscopy sampled the opposite side. Procedures were done under light intravenous sedation. A spot urine was collected. Product use began 1 week after the baseline bronchoscopy. The second bronchoscopy occurred 5 weeks following the first bronchoscopy (after 4 weeks of product use). Subjects received $37 for the orientation visit and $200 for each bronchoscopy.
Study Design for the Intervention
Study subjects (n=30) were randomized to either e-cig use or no use controls. For the intervention participants, one week after bronchoscopy, e-cigs were provided with an Innokin iTaste VV 4.0 refillable tank device (https://www.innokin.com/vaporizers/itaste-vv4/) and e-liquids that contained 50% PG and 50% VG (http://www.ecblendflavors.com/flavorless-eliquid/), without nicotine or flavors. Although no single device is representative of many or most devices on the market, we chose this device because it is commonly used, has a refillable tank system so that we can use nicotine- and flavor-free e-cigs, and had a method to record puff number. Subjects attended a training session and demonstrated their ability to inhale the e-cig and use the device. They were instructed to use the device at least twice per day, 20 puffs over 60 minutes each time. The device included an LED screen with a puff-counter. Participants received daily text messages reminding them to use the device and to send us the photo of the display showing puff counts; intervention group subjects sent daily photos of the LED screen to indicate usage.
Biweekly visits and product use
Subjects randomized to the e-cig intervention returned after 2 weeks of use for evaluation of compliance based on their daily reports and the e-liquid remaining in their bottles and tanks. Subjects were queried about any adverse events, and any change in their medical history and overall health. They were provided $7 for transportation and parking, and $20 for each visit, contingent on demonstrating use via the LED photos. Subjects using e-cigs who consented to follow-up after the trial (n=10) were contacted 3 months later; none reported any e-cig use.
Assays
BAL Cell Counts
Total cell counts were measured by 1:1 dilution in trypan blue and instillation into disposable Countess™ cell counting chamber slides. Automated cell counts were evaluated by the Countess® Automated Cell Counter (Invitrogen, Carlsbad, CA), according to manufacturer’s instruction. Differential cell counting was performed by a clinical histopathologist blinded to intervention status using Diff-Quik stained cytospins (Dade Behring-Switzerland) and light microscopy, counting at least 200 cells according to standard morphologic criteria.
BAL Inflammatory Cytokines
Following centrifugation, cell-free lavage fluid was assayed using a Meso Scale Discovery Sector Imager™ 2400A (Meso Scale Discovery, Rockville, MD) with a V-PLEX Plus Proinflam Combo 10 panel that includes tobacco smoking associated pro-inflammatory cytokines including IFN-γ, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12p70, IL-13, and TNF-α. The CVs for 10 cytokines were below 7% for intra-run and below 15% for inter-run which fell within expected CVs by the manufacturer.
Urinary Propylene Glycol (1,2-propanediol) Analysis(18)
Detailed methods are provided in Supplementary Methods. Briefly, using deuterated glycerol-d8 [Sigma. 447498] and 6 (±)-1,2-propanediol-d8 [CDN, D-1656]) as an internal standard, samples were analyzed by LCMS/MS (Agilent 1290 Infinity II UPLC system with Agilent Zorbax Eclipse Plus C18 column; Santa Clara, CA). Eluted compounds were further separated and quantified through the coupled Agilent 6495 Triple Quadrupole equipped with an electrospray ion (ESI) source. The coefficient of variation for PG from 14-blinded repeat samples was 15.4%.
Gene Expression
Total RNA was extracted from bronchial brushings using an Allprep DNA/RNA kit (Qiagen) and assayed for gene expression using the GeneChip® Human Transcriptome Array 2.0 (Affymetrix Inc, Santa Clara, CA) on the Affymetrix GeneChip Scanner 3000 7G. MicroRNA (miRNA) was assayed by the Affymetrix GeneChip miRNA Array v.4.0 (Affymetrix Inc, Santa Clara, CA). Raw data sets were normalized using the Expression Console Affymetrix with the robust multi-array average method (19) algorithmically based on microarrays spiked-in for standard normalization. The CEL files were imported into the Partek Genomics Suite™ 6.6 (St. Louis, MO) for log2 transformation and quantile normalization. Analysis of covariance (ANOVA) was used to remove potential batch effects. The expression data was deposited to under NCBI’s Gene Expression Omnibus database (GEO 138326).
Statistical Analysis
Statistical analyses were performed in JMP 10 (SAS Institute, Cary, NC) and Partek software. Data considered Guassian were summarized as mean (standard deviation) while non-normal data summarized as median (range). The Wilcoxon rank-sum test was used to test for an association between age and treatment group, and Fisher’s exact tests were used for gender and race comparisons to treatment group.
To compare baseline and follow-up for cell counts and cytokine levels, Wilcoxon Signed Rank tests with counts and paired t-tests (log10 transformed levels) were performed, respectively. For mRNA and miRNA expression, paired t-tests were used with log2 transformed expression levels. Absolute changes over a month for PG, cells, cytokines, mRNAs, and miRNAs were calculated by subtracting the raw baseline level from raw follow-up level. Correlations for the changes over a month between PG and cells, cytokines, mRNAs, and miRNAs were assessed by Spearman rank correlation. To determine expression signal clustering of the samples, unsupervised Principal Component Analysis (PCA)(20) was performed. False discovery rate (FDR)(21) adjusted q<0.1 was considered statistically significant. FDR was calculated separately for cell counts, cytokines, mRNA and miRNA expression.
RESULTS
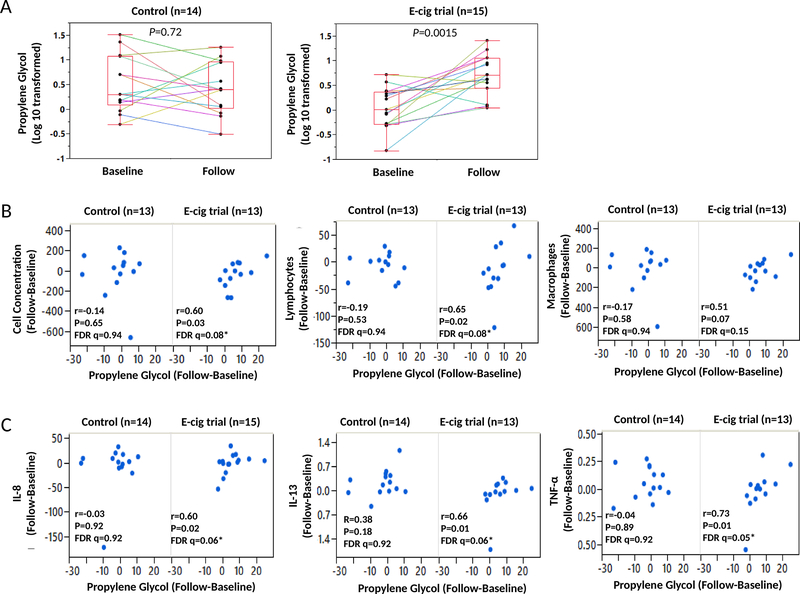
Thirty-four never-smokers, age 21–30, were randomized to using flavor- and nicotine-free e-cigs or to a control group of no-use. Subjects (n=30) underwent bronchoscopies both at baseline and 5 weeks later (Supplementary Figure 1). Four subjects did not have a second bronchoscopy, three due to new medical conditions (two respiratory tract infections and an unstable mental health issue) unrelated to the study that might affect safety or study results, and one lost to follow-up. Control and intervention groups were similar with respect to age (P=0.54), gender (P=0.71), and race (P=0.18) (Supplementary Table 1). Compliance to the e-cig intervention was assessed by daily LED readouts of puff number transmitted via cell phone and the measurement for increases in urinary PG (Figure 1A). PG was significantly increased in the intervention (P=0.0015), but not the control group (P=0.72).
Figure 1. Urine propylene glycol (PG) inflammation over one month intervention.
(A) Log10 transformed levels for PG in urine samples at baseline and follow-up for the control (left) and e-cig intervention (right) groups. Each dot represents one subject and paired assays for baseline and after the intervention are connected by a line. The box plot uses the median and the lower and upper quartiles (25th and 75th). (B-C) Spearman correlations of change (follow up-baseline) between PG and cell concentration, macrophages, and lymphocytes (B), and between PG and cytokines including IL-8, IL-13, and TNF-α (C) are shown in the control (left) and e-cig trial (right) groups. Significant False Positive Rate (FDR) q-values at the 0.1 level indicated by asterisks. Changes in PG and on the x-axis and change in cells (B) and cytokines (C) are on the y-axis. Note: One subject with very high baseline and follow-up PG level (likely a dietary source) was removed for analyses for changes of cells and cytokines. Subjects with red blood cell contamination were removed from the cell count analysis. In the e-cig use group, IL-13 and TNF-α were not detected at follow-up in two subjects.
There were no significant differences in cell counts or cytokines between the control and e-cig groups, whether measured by absolute number at the end of the trial, change in level, or fold-change (Table 1). However, changes for these markers were correlated with changes in urinary PG level as a marker of e-cig inhalation and compliance. For the intervention group, we found statistically significant positive correlations of PG change with changes in total cell concentration (r=0.60, raw P=0.03, FDR q=0.08) and lymphocyte counts (r=0.65, raw P=0.02, FDR q=0.08), and a borderline significant correlation with macrophage counts (r=0.51, raw P=0.07, FDR q=0.15)(Figure 1B). For controls, correlations were not statistically significant. Similarly, change in PG was significantly correlated with changes in IL-8 (r=0.60, raw P=0.02, FDR q=0.06), IL-13 (r=0.66, raw P=0.01, FDR q=0.06), and TNF-α (r=0.73, raw P=0.01, FDR q=0.05) for the intervention, but not the control group (Figure 1C). One outlier subject was removed with very high baseline and follow-up PG level (likely a dietary source).
Table 1.
Inflammatory cell counts and cytokines in bronchoalveolar lavage fluids: Randomized trial of never smokers
| Clinical Trials | Control (n=14) | E-cig use (n=13) | Control (n=14) | E-cig use (n=13) | |||||||||
| Cell counts1 | Baseline | Follow-up | Baseline | Follow-up | Absolute Difference | Absolute Difference | |||||||
| Median | (Range) | Media n | (Range) | P2 value | Median | (Range) | Median | (Range) | P2 value | Follow-Baseline Median | Follow-Baseline Median | P3 value | |
| Recovery (mL) | 56 | (41–71) | 58 | (40–72) | 0.7 | 55 | (47–65) | 54 | (37–63) | 0.23 | −0.5 | 0 | 0.26 |
| (% of instilled volume) | 55 | (41–71) | 56 | (40–72) | 0.73 | 55 | (40–65) | 54 | (37–63) | 0.25 | 0.5 | 0 | 0.30 |
| Total cell yield (× 106) | 14 | (8–34) | 15 | (6–23) | 0.92 | 13 | (9–29) | 10 | (8–19) | 0.33 | 1.5 | −3 | 0.18 |
| Cell concentration (×106/L) | 243 | (141–763) | 268 | (98–396) | 0.95 | 236 | (156–521) | 194 | (141–518) | 0.33 | 10 | −20 | 0.51 |
| Macrophages (×106/L) | 203 | (125–694) | 231 | (96–350) | 1.00 | 196 | (152–459) | 176 | (95–486) | 0.89 | 29 | −31 | 0.51 |
| (%) | 88 | (68–98) | 89 | (70–98) | 0.53 | 87 | (61–100) | 92 | (58–100) | 0.11 | 0 | 6 | 0.54 |
| Lymphocytes (×106/L) | 28 | (3–83) | 25 | (1–88) | 0.46 | 32 | (0–159) | 15 | (0–111) | 0.50 | 0.5 | −13 | 0.45 |
| (%) | 10 | (2–28) | 9 | (1–27) | 0.5 | 11 | (0–37) | 5 | (0–41) | 0.11 | 0 | −6 | 0.37 |
| Neutrophils (×106/L) | 5 | (0–31) | 3 | (0–19) | 0.77 | 3 | (0–14) | 2 | (0–12) | 0.58 | 1.5 | −1 | 0.48 |
| (%) | 2 | (0–6) | 1 | (0–6) | 0.67 | 1 | (0–6) | 1 | (0–4) | 0.52 | 0.5 | 0 | 0.75 |
| Eosinophils (×106/L) | 0 | (0–8) | 0 | (0–6) | 0.63 | 0 | (0–5) | 0 | (0–6) | 0.69 | 0 | 0 | 0.79 |
| (%) | 0 | (0–1) | 0 | (0–2) | 0.63 | 0 | (0–2) | 0 | (0–3) | 0.08 | 0 | 0 | 0.33 |
| Control (n=15) | E-cig use (n=15) | Control (n=15) | E-cig use (n=15) | ||||||||||
| Cytokines | Baseline | Follow-up | Baseline | Follow-up | Absolute Difference | Absolute Difference | |||||||
| Mean | (SD) | Mean | (SD) | P4 value | Mean | (SD) | Mean | (SD) | P4 value | Follow-Baseline Median | Follow-Baseline Median | P3 value | |
| IL-1β | 0.66 | (0.36) | 1.30 | (1.38) | 0.04 | 0.77 | (0.27) | 1.22 | (0.31) | 0.33 | 0.28 | 0.06 | 0.30 |
| IL-2 | 0.34 | (0.14) | 0.41 | (0.16) | 0.02 | 0.43 | (0.12) | 0.40 | (0.12) | 0.33 | 0.03 | 0.00 | 0.09 |
| IL-4 | 0.04 | (0.01) | 0.04 | (0.01) | 0.68 | 0.04 | (0.01) | 0.04 | (0.02) | 0.13 | 0.00 | 0.00 | 0.28 |
| IL-6 | 0.87 | (0.54) | 0.96 | (0.47) | 0.57 | 1.06 | (0.59) | 1.03 | (0.61) | 0.39 | 0.04 | 0.03 | 0.68 |
| IL-8 | 35.12 | (59.56) | 26.64 | (17.39) | 0.74 | 24.38 | (16.97) | 22.62 | (15.29) | 0.42 | 1.30 | 1.86 | 0.97 |
| IL-10 | 0.09 | (0.02) | 0.10 | (0.03) | 0.05 | 0.09 | (0.02) | 0.10 | (0.02) | 0.64 | 0.01 | 0.00 | 0.36 |
| IL-12p70 | 0.13 | (0.05) | 0.15 | (0.06) | 0.04 | 0.15 | (0.04) | 0.14 | (0.04) | 0.58 | 0.02 | 0.00 | 0.09 |
| IL-13 | 2.06 | (2.7) | 2.24 | (2.93) | 0.09 | 1.66 | (0.92) | 1.55 | (0.59) | 0.69 | 0.16 | −0.03 | 0.11 |
| IFN-γ | 0.91 | (0.32) | 0.91 | (0.35) | 0.88 | 0.89 | (0.23) | 0.78 | (0.28) | 0.16 | 0.06 | −0.01 | 0.25 |
| TNF-α | 0.41 | (0.15) | 0.46 | (0.15) | 0.36 | 0.50 | (0.23) | 0.51 | (0.17) | 0.95 | 0.01 | 0.00 | 0.58 |
BAL with red blood cell contamination were removed for cell count.
Wilcoxon Signed Rank tests
Wilcoxon Rank Sums
Paired t-tests using log10 transformed data. None of the cell counts and cytokines reached significant if controlling FDR at 0.1.
Note: In the e-cig use group, IL-10, IL-13, IL-12p70, and TNF-α were not detected in two subjects and INF-γ was not detected in one subject.
Median, range, mean, and standard deviation (SD) were presented as raw values.
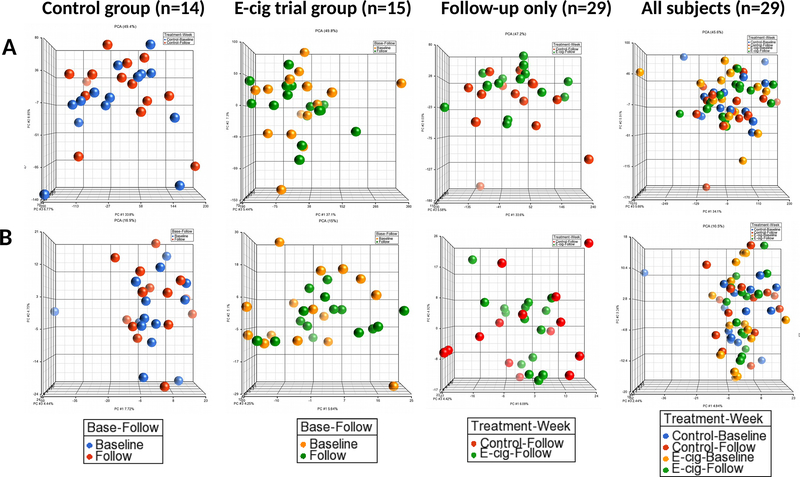
There were no significant changes in gene expression from lung epithelial cell brushings for either group and no differences between the intervention and controls groups (Figure 2A for mRNAs and 2B for miRNAs) (the lowest FDR q=0.99 for both mRNAs and miRNAs). Spearman correlations for changes in expression with changes in PG among the e-cig group were not significant (the lowest FDR q=0.99 for mRNA and FDR q=0.24 for miRNA).
Figure 2. Principal Component Analysis (PCA) of mRNAs (A and B) and miRNAs (C) for transcripts before and after the trial for control and intervention groups.
The PCA was generated using (A) entire 33,494 mRNA transcripts analyzed, and (B) entire 2,578 miRNA transcripts analyzed. Dots represent each individual for baseline controls (blue), follow-up controls (red), baseline intervention (orange), and follow-up intervention (green).
DISCUSSION
In this pilot trial of healthy, never-smokers randomized to use of a nicotine- and flavor-free e-cig containing only PG/VG or to a no-use control, we found that e-cig use induced lung inflammation correlated with change in PG exposure, albeit to a relatively low extent; inflammatory markers in the e-cig users after the intervention remained within the range of never-smokers’ (17,22,23).
In this study, e-cigs containing only PG and VG were assessed; possible effects of nicotine were not evaluated. Nicotine is highly bioactive and depending on the laboratory assessment method, can have both pro- and anti-inflammatory effects (8). In some experimental animal studies, the presence of nicotine in e-aerosols increases inflammation, while in those studies PG and VG have less effect (9,14,16,24). Future studies may evaluate e-cigs with and without nicotine to provide some understanding for the effects of nicotine on the lung.
In this study, the use of the nicotine- and flavor-free e-cigs did not affect gene expression, including expression commonly associated with cigarette smoking. The lack of change in gene expression in our study was not likely due to a short duration of exposure, given that Staudt, et al. observed changes in expression in never-smokers after just one session of less than an hour of e-cig use with and without nicotine (17). Further, in experimental studies in mice exposed to PG and VG over 2 weeks, there were changes in gene expression (25). In cultured normal human bronchial epithelial cells exposed for 2 hours to commercial e-aerosols without nicotine, but with flavors, there were also changes induced in gene expression (13). The reasons why our e-cig intervention did not cause changes in gene expression are unclear, especially given the observed changes in inflammation. These findings support the hypothesis that large magnitude changes in expression are likely not to occur from inhaling PG and VG, at least after one month of use.
There are several limitations to the findings of this randomized trial. The results here might not be generalizable to the general population of e-cig users given the health and age restrictions. However, this age group is the adult demographic that most commonly uses e-cigs and is a group with high use among never smokers. Further, while there were some observed effects on inflammation and none on gene expression, a one-month duration of use may not be sufficient to fully characterize effects of chronic use. As discussed above, and in other studies, brief duration of exposure in humans and laboratory studies (as short as 2 hour exposures) cause cell and cytokine increases, DNA damage, changes in gene expression and other toxicities in bronchial lung cell culture (13,14,16,26). In our study, we examined only e-liquid that included both PG and VG in equal concentrations. The relative contribution of each could not be assessed; the two compounds may have differential effects on the lung. Exposures to different relative concentrations of PG and VG might also have different impact.
This also study has important strengths, particularly the randomized trial design of an e-cig intervention among never-smokers, providing data specific to e-liquid solvent carriers. Such data are critical to an understanding of the impact of e-cig use constituents that can be regulated by the FDA. Future studies are needed regarding effects of varying the relative proportions of VG and PG to identify if there are different effects on lung toxicity. Because this study used bronchoscopic biomarkers, it allows for a direct examination of lung cancer and COPD mechanisms in the lung as the target organ. Our findings of a dose-response in inflammation markers relative to PG have important implications for understanding effects of e-cig use. Further, we investigated multiple biomarkers of effect to understand biological and mechanistic changes, using sampling methods to capture BAL and brushings, to provide a comprehensive picture of the impact of e-cig use. The changes in urinary PG that were positively correlated with changes of cell counts and cytokines, indicating a dose-response, strengthens the biological plausibility of a real effect.
The FDA’s Center for Tobacco Products has recently deemed regulatory authority for e-cig and e-liquid product design, as well as marketing and messaging to consumers. To make sound policy, regulators need data about e-cig toxicity in humans whether they are never-smokers (e.g., youth who experiment with e-cigs and/or become regular users) or smokers switching to e-cigs as a smoking cessation aid. The data from this study provide direct safety information regarding the e-cig solvent carriers, PG and VG. We found small changes in inflammation correlated with change in PG exposure but no difference between the intervention and the control groups in expression. Future studies are needed to better understand the clinical significance for the magnitude of the effect by PG and VG, varying ratios of the two and longer duration of use as well as effects of flavors.
Supplementary Material
ACKNOWLEDGMENTS
Research reported in this publication was supported by funding from the National Cancer Institute of the National Institutes of Health (NIH) (P30 CA016058), the Food and Drug Administration Center for Tobacco Products (CTP) (P50CA180908 and R21HL147401), the National Center For Advancing Translational Sciences (UL1TR001070) and from the Pelotonia Intramural Research Funds, and the Prevent Cancer Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA. We thank the Genomics Shared Resource for performing the GeneChip® Human Transcriptome Array 2.0, Center for Clinical and Translational Science for measuring the inflammatory cytokines, and Department of Pathology for BAL differential cell counts at The Ohio State University (Columbus, OH). We acknowledge the support of the Bioinformatics Shared Resource and the Biostatistics Shared Resource at The Ohio State University (Columbus, OH). We also thank the study participants, the staff and nurses of the OSU Clinical Research Center, and Mrs. Sahar Kamel for assisting in recruiting participants.
Abbreviations list
- E-cigs
electronic cigarettes
- PG
propylene glycol
- BAL
bronchoalveolar lavage
- VG
vegetable glycerine
- FDA
Food and Drug Administration
- miRNA
microRNA
- ANOVA
Analysis of covariance
- PCA
Principal Component Analysis
Footnotes
CONFLICTS OF INTEREST
PGS has served as an expert witness and consultant in tobacco company litigation on behalf of plaintiffs. The other authors declare that they have no potential conflicts of interest.
References
- 1.Singh T, Arrazola RA, Corey CG, Husten CG, Neff LJ, Homa DM, et al. Tobacco Use Among Middle and High School Students--United States, 2011–2015. MMWR Morbidity and mortality weekly report 2016;65(14):361–7 doi 10.15585/mmwr.mm6514a1. [DOI] [PubMed] [Google Scholar]
- 2.Cullen KAAB, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the Field: Use of Electronic Cigarettes and Any Tobacco Product Among Middle and High School Students — United States. MMWR Morbidity and mortality weekly report 2018;67:1276–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Academies of Sciences E, and Medicine. Public health consequences of e-cigarettes. Washington, DC: The National Academies Press; 2018. doi 10.17226/24952. [DOI] [PubMed] [Google Scholar]
- 4.Coleman B, Rostron B, Johnson SE, Persoskie A, Pearson J, Stanton C, et al. Transitions in electronic cigarette use among adults in the Population Assessment of Tobacco and Health (PATH) Study, Waves 1 and 2 (2013–2015). Tob Control 2018. doi 10.1136/tobaccocontrol-2017-054174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Viswam D, Trotter S, Burge PS, Walters GI. Respiratory failure caused by lipoid pneumonia from vaping e-cigarettes. BMJ Case Rep 2018;2018 doi 10.1136/bcr-2018-224350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sommerfeld CG, Weiner DJ, Nowalk A, Larkin A. Hypersensitivity Pneumonitis and Acute Respiratory Distress Syndrome From E-Cigarette Use. Pediatrics 2018;141(6) doi 10.1542/peds.2016-3927. [DOI] [PubMed] [Google Scholar]
- 7.Itoh M, Aoshiba K, Herai Y, Nakamura H, Takemura T. Lung injury associated with electronic cigarettes inhalation diagnosed by transbronchial lung biopsy. Respirol Case Rep 2018;6(1):e00282 doi 10.1002/rcr2.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shields PG, Berman M, Brasky TM, Freudenheim JL, Mathe E, McElroy JP, et al. A Review of Pulmonary Toxicity of Electronic Cigarettes in the Context of Smoking: A Focus on Inflammation. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology 2017;26(8):1175–91 doi 10.1158/1055-9965.EPI-17-0358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Husari A, Shihadeh A, Talih S, Hashem Y, El Sabban M, Zaatari G. Acute Exposure to Electronic and Combustible Cigarette Aerosols: Effects in an Animal Model and in Human Alveolar Cells. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco 2016;18(5):613–9 doi 10.1093/ntr/ntv169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scheffler S, Dieken H, Krischenowski O, Forster C, Branscheid D, Aufderheide M. Evaluation of E-cigarette liquid vapor and mainstream cigarette smoke after direct exposure of primary human bronchial epithelial cells. Int J Environ Res Public Health 2015;12(4):3915–25 doi 10.3390/ijerph120403915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higham A, Rattray NJ, Dewhurst JA, Trivedi DK, Fowler SJ, Goodacre R, et al. Electronic cigarette exposure triggers neutrophil inflammatory responses. Respiratory research 2016;17(1):56 doi 10.1186/s12931-016-0368-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu V, Rahimy M, Korrapati A, Xuan Y, Zou AE, Krishnan AR, et al. Electronic cigarettes induce DNA strand breaks and cell death independently of nicotine in cell lines. Oral oncology 2016;52:58–65 doi 10.1016/j.oraloncology.2015.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shen Y, Wolkowicz MJ, Kotova T, Fan L, Timko MP. Transcriptome sequencing reveals e-cigarette vapor and mainstream-smoke from tobacco cigarettes activate different gene expression profiles in human bronchial epithelial cells. Scientific reports 2016;6:23984 doi 10.1038/srep23984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glynos C, Bibli SI, Katsaounou P, Pavlidou A, Magkou C, Karavana V, et al. Comparison of the effects of e-cigarette vapor with cigarette smoke on lung function and inflammation in mice. Am J Physiol Lung Cell Mol Physiol 2018. doi 10.1152/ajplung.00389.2017. [DOI] [PubMed] [Google Scholar]
- 15.Garcia-Arcos I, Geraghty P, Baumlin N, Campos M, Dabo AJ, Jundi B, et al. Chronic electronic cigarette exposure in mice induces features of COPD in a nicotine-dependent manner. Thorax 2016. doi 10.1136/thoraxjnl-2015-208039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lerner CA, Sundar IK, Yao H, Gerloff J, Ossip DJ, McIntosh S, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PloS one 2015;10(2):e0116732 doi 10.1371/journal.pone.0116732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Staudt MR, Salit J, Kaner RJ, Hollmann C, Crystal RG. Altered lung biology of healthy never smokers following acute inhalation of E-cigarettes. Respir Res 2018;19(1):78 doi 10.1186/s12931-018-0778-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li H, Dong J, Chen W, Wang S, Guo H, Man Y, et al. Measurement of serum total glycerides and free glycerol by high-performance liquid chromatography. J Lipid Res 2006;47(9):2089–96 doi 10.1194/jlr.D600009-JLR200. [DOI] [PubMed] [Google Scholar]
- 19.Irizarry RA, Hobbs B, Collin F, Beazer-Barclay YD, Antonellis KJ, Scherf U, et al. Exploration, normalization, and summaries of high density oligonucleotide array probe level data. Biostatistics 2003;4(2):249–64 doi 10.1093/biostatistics/4.2.249. [DOI] [PubMed] [Google Scholar]
- 20.Williams HAaLJ. Principal component analysis. Wiley Interdisciplinary Reviews: Computational Statistics 2010;2(4):433–59. [Google Scholar]
- 21.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B 1995;57:289–300. [Google Scholar]
- 22.Song MA, Jo FL, Brasky TM, McElroy JP, Nickerson QA, Reisinger SA, et al. Electronic Cigarette Use and Lung Toxicity. Cross reference. [Google Scholar]
- 23.Ghosh A, Coakley RC, Mascenik T, Rowell TR, Davis ES, Rogers K, et al. Chronic E-Cigarette Exposure Alters the Human Bronchial Epithelial Proteome. Am J Respir Crit Care Med 2018;198(1):67–76 doi 10.1164/rccm.201710-2033OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garcia-Arcos I, Geraghty P, Baumlin N, Campos M, Dabo AJ, Jundi B, et al. Chronic electronic cigarette exposure in mice induces features of COPD in a nicotine-dependent manner. Thorax 2016;71(12):1119–29 doi 10.1136/thoraxjnl-2015-208039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lechasseur A, Jubinville E, Routhier J, Berube JC, Hamel-Auger M, Talbot M, et al. Exposure to electronic cigarette vapors affects pulmonary and systemic expression of circadian molecular clock genes. Physiol Rep 2017;5(19) doi 10.14814/phy2.13440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen J, Higby R, Tian D, Tan D, Johnson MD, Xiao Y, et al. Toxicological analysis of low-nicotine and nicotine-free cigarettes. Toxicology 2008;249(2–3):194–203 doi 10.1016/j.tox.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.