Abstract
Objective
The purpose of this study was to examine the associations of sleep duration and socioecological protective factors with patterns of adolescent risk behaviors in Fairfax County, VA - one of the largest public-school districts in the United States.
Methods
A total of 21,360 and 20,330 students in 10th and 12th grades who completed the youth risk behavior survey were included in this cross-sectional analysis. Sleep duration was measured by self-report of the average number of hours of sleep on a school night. Ten socioecological protective factors included individual-peer, family, school, and community domains. Latent class analysis was used to classify 7 risk behaviors (alcohol use, cigarette use, illicit drug use, inappropriate prescription drug use, risky sexual behavior, deviant behavior, and academic failure) into 4 class-memberships (Low, Some, Moderate, and High). Multinomial regression models were adjusted for age, gender, and race.
Results
Adolescents who reported sleeping the recommended 8–9 hours were significantly less likely to belong to the class-memberships of greater risk behaviors compared to those who reported short and longer sleep duration after controlling for age, gender, race, and survey year. There was a significant inverse relationship between the number of socioecological protective factors and risk behaviors for both 10th and 12th graders. Potential risks of age, sex, and race on risky behaviors were observed. No significant interaction between sleep duration and protective factors was found in both grades.
Conclusions
This study highlights the significant associations between sleep duration and risk behaviors in adolescents with diverse socioecological protective factors. Prioritization of prevention-focused resources should consider sleep duration in addition to the socioecological protective factors commonly cited in the literature when addressing adolescent risk behaviors.
Introduction
Adolescent risk behaviors, including engagement in behaviors such as delinquency, substance use, alcohol use, and risky sexual behavior pose a threat to healthy development and significantly increase morbidity and mortality in this population.1,2 Although rates of some adolescent risk behaviors such as alcohol use and sexual activity have declined in the United States over the past two decades, the rates remain high at over 30% and 40% respectively.3 Additionally, reported rates of marijuana use among adolescents have remained steady at around 22%.3 Because of the association between risk behaviors and adverse outcomes4,5 such as motor vehicle crashes, other unintentional injuries, homicide and suicide – the four causes of over 70% of all deaths among persons 10–24 years according to the most recent data6 - risky behaviors in adolescents are considered to be a major public health threat.7 Thus, investment in enhancing protective factors in order to prevent adolescent risk behaviors has the potential to improve survival rates and well-being.8
Because adolescent risk behaviors occur within the context of complex interactions between socioecological risk and protective factors,9 primary prevention efforts must consider all socioecological levels - individual, interpersonal, community, and societal - to reduce risk and enhance protective factors.10 Previous studies have found a wide range of protective factors, including parental expectations and monitoring, positive peer influences, supportive school environment, and positive perception of their community to provide protection against engagement in adolescent risk behaviors,11 including cigarette, alcohol, and drug use among high school students.12 Despite these insights, identifying primary prevention approaches to reduce adolescent risk behaviors remains one of both critical importance and ongoing study.12–14
The search for additional protective factors beyond those described above has led to consideration of the role of sleep duration in mitigating adolescent risk behaviors.15–17 It is recommended that adolescents sleep 8–10 hours per day to meet their overall health and developmental needs;18 however, only about 30% of adolescents in the U.S. achieve this goal.19 Furthermore, there is a substantial body of evidence supporting an association between insufficient sleep in adolescents and an increased risk of motor vehicle accidents,20 sports injuries,21 work-related injuries,22 and adverse mental health outcomes,16 as well as engagement in smoking, sexual activity, alcohol use, and illicit drug use.23 The association between insufficient sleep and poor academic performance24 is also of concern considering the link between academic achievement and human health and capital.25 In a large socioeconomically diverse school-based sample of 10,718 and 11,240 eighth-grade students in 2010 and 2012, respectively, we previously reported that insufficient sleep, specifically, a sleep duration ≤7 hours, was associated with increased risk behaviors.17
Previous epidemiological studies predominantly examined sleep duration as a risk factor in the context of adolescent risk behaviors, but there are merits to examining sleep duration as a protective factor. Sleep duration is a low cost, modifiable factor that may be important in the development and implementation of primary prevention interventions to address adolescent risk behaviors. The leading advocates for children’s health such as the American Academy of Pediatrics, and the American Academy of Sleep Medicine (AASM) endorsed protective effects of the recommended amount of sleep on a regular basis to promote optimal health.18 For adolescents with access to fewer socioecological protective factors, it is expected that the association between sleep duration and risk behaviors could be complex. However, the combination or interactive effect of sleep duration and socioecological protective factors on adolescent risk behaviors remain unclear, and worth further exploration for the planning of cost-effective and tailored prevention and intervention strategies.
Because different forms of adolescent risk behaviors often co-occur, use of latent class analysis (LCA) as a statistical method to identify subgroups/classes within a population is increasingly used in studies involving adolescent risk behaviors.26–28 However, we are unaware of any studies that examined multiple adolescent risks simultaneously, in relation to protective factors and sleep duration.
Considering the emerging interest in the effects of sleep on adolescent risk behaviors and the existing body of literature on socioeconomic protective factors and adolescent risk behaviors, the purpose of this study was to examine the associations between sleep duration and socioecological protective factors (independently and combined) and patterns of adolescent risk behaviors in one of the largest and diverse public-school districts in the United States. Our study used LCA to identify latent classes among 7 adolescent risk behaviors, including Alcohol Use, Cigarette Use, Use of illicit drugs, Inappropriate Use of Prescription/Over the Counter Medications (Rx/OTC), Weapon carrying, Risky Sexual Activity, and Academic Failure. We hypothesized that there is an association between sleep duration and socioecological protective factors and the latent class of risk behaviors engaged in by adolescents. In addition, we hypothesized that healthy sleep duration would be associated with fewer risk behaviors among adolescents. Considering the importance of socioecological protective factors in buffering youth against the trajectory of risk29 and adverse childhood experiences,30 the role of sleep health may provide an important focus for policy and intervention development.
Methods
Participants
The publicly available archival data used in this study includes 41,690 10th and 12th grade students responding to surveys conducted in 2012 and 2014 within the Fairfax County Public Schools in Virginia, one of the largest school districts in the United States. Beginning in the fall of 2015, the Fairfax County Schools changed the school start times in an effort to provide additional sleep opportunity for the children, therefore data from 2016 were not included due the potential for historical bias. We were not able to determine how many 10th graders in 2012 were 12th graders in the 2014 because the data were deidentified, therefore analyses were performed separately by grade level and we did not perform statistical test for differences between grades. The 2012 and 2014 surveys were combined since the data were collected within the same school system and there were no differences in the study variables between the two years. Because the data were publicly available and de-identified by the Fairfax County Public, this research received an exemption from IRB review. Permission to conduct this study was provided by Fairfax County Public.
Measures
Demographics
Sex and race/ethnicity characteristics were included in our analyses as covariates following previous studies.16,17 The students were asked two questions about their race and ethnicity, and these data were re-coded by the school system as white and non-white for de-identification purposes. Due to the variability of age within the 10th and 12th grades, we also controlled for age in our analyses. We also controlled for cluster correlation within each school.
Youth Survey
The Youth Survey used in this study was adapted from the Centers for Disease Control and Prevention (CDC) Youth Risk Behavior Survey (YRBS) that has been conducted nationally since 1991. The YRBS provides a unique opportunity to examine the relationships between socio-demographic and socioecological factors, including sleep duration, protective factors, and multiple adolescent risk behaviors. The 210-question survey is administered every two years to all consenting adolescents in 10th and 12th grades in every public high school in the district. Completion of the survey is voluntary and parents may opt out of allowing their child to complete it. All responses are confidential and all data de-identified. A total of 89.6% and 86.7% of students enrolled in Fairfax County Public Schools (excluding alternative schools) in 2012 and 2014, respectfully, participated in the survey. Less than 1% of families opted out,17 but information on the reasons why other students did not complete the survey (e.g. those who were absent on the day of the survey) was not available to the authors. Due to the limited number of students attending alternative schools and the desire to analyze data by grade, gender, and race/ethnicity, alternative schools were not included in the publicly available dataset provided to the authors.
Sleep duration
Sleep duration was assessed by a single question on the survey, “On an average school night, how many hours of sleep do you get?” Students self-reported that they received on average either, “4 hours or less”, “5 hours”, “6 hours”, “7 hours”, “8 hours”, “9 hours”, or “10 hours or more”. Because the data were not continuous, we re-coded sleep duration to less than recommended amount of sleep (1= 7 hours or less), recommended amount of sleep (2= 8 or 9 hours), and more than the recommended amount of sleep (3= 10 hours or more) to align with the recommendations for adolescent sleep duration by the American Academy of Sleep Medicine 18.
Protective factors
The survey included 114 questions from the Communities That Care Youth Survey from the U.S. Substance Abuse and Mental Health Services Administration to examine 18 risk and 10 protective factors that fall under four domains: community, school, family, and peer-individual. We focused on the protective factors for this study, something that to our knowledge has not previously been examined. Associations between the 18 risk factors (of note, risk factors are different variables from risk behaviors) and sleep duration were previously reported by several of the co-authors.17. The 10 protective factors included: two community scales (opportunity and rewards for involvement); three family scales (attachment scale, opportunities, and rewards for involvement); two school scales (opportunity for involvement and rewards for prosocial involvement); and three peer-individual scales (religiosity, social skills, and belief in moral order). There were 3–5 questions within each subscale. Each subscale score was compared to a national standard established by the Social Development Research Group at the University of Washington, based on a database of over 310,000 surveys. The students’ scores were dichotomized according to national cut-offs established for 10th and 12th grades.32 Students who fell above the cut-off score were considered to have high protection (coded as 1) in that subscale and those who fell below the cut-off were considered to have low protection (coded as 0) in that subscale. The 10 subscale scores were then added to create a total number of protective factors (0–10) that were considered to provide “high protection” to establish a cumulative protective factor score. To ensure the validity and reliability of the information, the Fairfax County Youth Survey used items from the nationally-validated survey, Communities That Care. The Cronbach’s alpha values for the 10 protective factors scales in the 2012 survey ranged from 0.42 to 0.83, and in 2014 survey ranged from 0.43 to 0.844 (two of the 10 subscales had a Cronbach’s alpha below 0.6: social skills (α=0.54) and community opportunities for prosocial involvement (α=0.43).
Outcome: Risk behaviors
The seven risk behaviors included in this study were: alcohol use, cigarette use, drug use (illicit and inappropriate prescription use), risky sexual behavior, carrying a weapon, and academic failure. The prevalence of each risk behavior was calculated based on frequency distribution of the student’s answers to 1–5 questions about each risk behavior. The list of risk behavior questions is provided in the Supplemental Digital Content 1. The responses were dichotomized to a score of zero indicating that the student did not endorse engaging in a particular risk behavior and a score of one if the student reported answering at least one of the questions from each risk behavior category affirmatively. For example, students who reported using beer, wine, or hard liquor in the past 30 days were scored a one and those who did not report drinking alcohol were scored a zero. Similarly, students were asked about using an illicit drug (marijuana, methamphetamine, steroids, heroin, ecstasy). If they endorsed using any of these five illicit drugs then they were scored as one and those who denied any drug use were scored a zero. Any use of cigarettes was scored a one. Questions about prescription drug abuse included use of painkillers without a doctor’s order, use of other prescription drug other than painkiller without a doctor’s order, and use of OTC to get high. Risk related to carrying a weapon included handgun and non-handgun weapon use. Risky sexual behavior was determined by endorsement of sexual intercourse, oral sex, and unprotected sexual intercourse. Academic failure was determined by endorsement of academic grades that were mostly D’s and F’s, skipping school, or coming to class unprepared. These risk behaviors were chosen based on Jessor’s problem behavior theory wherein psychosocial determinants of adolescent health include a range of health-compromising behaviors.33 Because adolescents commonly engage in multiple or clusters of risk behaviors, we used latent class analysis described below to empirically identify subgroups that represent the range of co-occurring risk behaviors among the adolescents.
Statistical analysis
Descriptive analysis was performed with means (standard deviation) and frequency of demographic characteristics, sleep duration, cumulative protective factors, and risk behaviors between 10th and 12th grade. Latent class analysis (LCA) was performed to identify class-memberships of the seven risk behaviors with separate samples of 10th and 12th grade due to the potential dependence from identical individuals between two grade groups. Examining the sample separately by grade insured that class-memberships were not the same between two grades. Because we could not match students from 2012 to 2014, we did not perform any statistical analysis for grade difference. LCA was performed using SAS/STAT ® version 9.4 with PROC LCA, which used the EM algorithm (Expectation-maximization).34 Missing data on risk behaviors was handled by the EM algorithm with an assumption of missing at random. The number of latent class-memberships was determined based on goodness-of-fit criteria, including the likelihood-ratio G2 statistics, Akaike’s Information Criterion (AIC), consistent AIC, Bayesian Information Criterion (BIC), and adjusted BIC. The LCA produced a categorical variable (i.e., class-membership) characterized by the patterns (i.e., response probability) of risk-behaviors within class-membership. We estimated odds ratios (OR) of risky-behavior class-memberships for potential risk factors including total sleep time (short: ≤7h, recommended: 8–9h, and long: 10+h), the cumulative protective factors, age, sex, race (white vs. non-white), and survey years using multinomial regression model, separately, in 10th and 12th grades. Lastly, we examined the moderation effect of total sleep time using the multinomial models with an interaction between total sleep time and cumulative protective factors in each grade.
Results
Descriptive statistics
A total of 20,787 in 2012 and 20,903 in 2014 students in 10th and 12th grades combined participated in the Youth Survey. Upon data cleaning, 91.3% and 93.5% of the questionnaires were included in the final dataset in 2012 and 2014, respectively.35 Table 1 provides a descriptive comparison of the sample. Among 10th grade students, only 22.5% reported obtaining 8–9 hours of sleep (recommended amount) whereas 76.3% reported sleeping ≤7 hours (insufficient/short sleep duration) in 2012 and 2014. Similarly, only 14% of 12th graders reported sleeping 8–9 hours, with the majority (85%) reporting 7 hours or less of sleep per night. Only a very small percentage of 10th and 12th graders reported sleeping 10 or more hours (1.1% and 0.9%, respectively). These results indicated that 10th and 12th graders reported somewhat higher rates of insufficient sleep than the national rates reported by the Centers for Disease Control and Prevention based on 2014 Youth Risk Behavior Survey data. According to National data, 67.4% and 76.6%, reported <8 hours of sleep in 10th and 12th grade, respectfully compared to 76.3% and 85% in this study.36
Table 1.
Sample characteristics
| Grade 10 | Grade 12 | |||||
|---|---|---|---|---|---|---|
| Samples in 2014 (N=10,784) | Samples in 2012 (N=10,576) | Overall (N=21,360) | Samples in 2014 (N=10,119) | Samples in 2012 (N=10,211) | Overall (N=20,330) | |
| Age, Mean (SD) | 15.3 (0.5) | 15.2 (0.5) | 15.2 (0.5) | 17.2 (0.5) | 17.2 (0.5) | 17.2 (0.5) |
| Sex, N(%) | ||||||
| Male | 5,289 (49.3%) | 5,139 (48.8%) | 10,428 (49.1%) | 5,000 (49.7%) | 4,990 (49.1%) | 9,990 (49.4%) |
| Female | 5,437 (50.7%) | 5,389 (51.2%) | 10, 826 (50.9%) | 5,062 (50.3%) | 5,170 (50.9%) | 10,232 (50.6%) |
| Race, N(%) | ||||||
| White Race | 4,589 (43.0%) | 4,591 (43.8%) | 9,180 (43.4%) | 4,480 (44.6%) | 4,646 (45.9%) | 9,126 (45.2%) |
| Non-White Race | 6,077 (57.0%) | 5,884 (56.2%) | 11,961 (56.6%) | 5,564 (55.4%) | 5,487 (54.1%) | 11,051 (54.85) |
| Protective factors, Mean (SD) | 6.08 (2.62) | 5.92 (2.65) | 6.00 (2.63) | 5.90 (2.61) | 5.86 (2.58) | 5.88 (2.60) |
| Community opportunities prosocial involvement | 5072 (49.02%) | 4838 47.64% | 9910 (48.34%) | 4318 (44.79%) | 4221 (43.59%) | 8539 (44.19%) |
| Community rewards for prosocial involvement | 5731 (54.86%) | 5625 (54.87%) | 11356 (54.87%) | 5158 (53.08%) | 5248 (53.54%) | 10406 (53.31%) |
| Family attachment | 5422 (53.19%) | 4801 (47.94%) | 10223 (50.58%) | 5429 (57.20%) | 5394 (56.37%) | 10823 (56.78%) |
| Family opportunities for prosocial involvement | 6138 (59.05%) | 5584 (54.98%) | 11723 (57.04%) | 5372 (55.81%) | 5229 (53.67%) | 10601 (54.73%) |
| Family rewards for prosocial involvement | 6073 (58.58%) | 5688 (56.14%) | 11762 (57.38%) | 5249 (54.59%) | 5123 (52.79%) | 10372 (53.69%) |
| School opportunities for prosocial involvement | 7376 (69.10%) | 7315 (69.69%) | 14692 (69.40%) | 7252 (72.25%) | 7153 (70.58%) | 14405 (71.41%) |
| School rewards for prosocial involvement | 6922 (64.58%) | 6919 (65.81) | 13842 (65.19%) | 5185 (51.66%) | 5315 (52.37%) | 10500 (52.02%) |
| Religiosity | 4755 (45.56%) | 4872 (47.69%) | 9628 (46.62%) | 6678 (69.02%) | 7078 (72.48%) | 13756 (70.76%) |
| Belief in moral order | 8291 (77.41%) | 7751 (73.71%) | 16043 (75.57%) | 5275 (52.63%) | 5366 (52.99%) | 10641 (52.81%) |
| Social skills | 7752 (73.19%) | 7279 (69.89%) | 15032 (71.55%) | 7473 (75.59%) | 7376 (74.08%) | 14849 (74.83%) |
| Sleep duration, N(%)1 | ||||||
| Short sleep (≤7 hours) | 8,152 (77.6%) | 7,727 (75.0%) | 15,879 (76.3%) | 8,376 (85.6%) | 8,343 (84.5%) | 16,719 (85.0%) |
| Recommended Sleep (8–9 hours) | 2,249 (21.4%) | 2,241 (23.7%) | 4,690 (22.5%) | 1,329 (13.6%) | 1,425 (14.4%) | 2,754 (14.0%) |
| Health risk behaviors, N(%) | ||||||
| Alcohol Use | 1,827 (17.4%) | 1,979 (19.0%) | 3,806 (18.2%) | 3,487 (35.6%) | 3,480 (34.9%) | 6,967 (35.3%) |
| Cigarette Use | 1,333 (12.5%) | 1,570 (15.0%) | 2,903 (13.8%) | 2,364 (23.8%) | 2,734 (27.3%) | 5,098 (25.6%) |
| Use of illicit drugs | 183 (1.7%) | 252 (2.4%) | 435 (2.1%) | 264 (2.7%) | 322 (3.3%) | 586 (3.0%) |
| Inappropriate Use of Rx/OTC | 774 (7.3%) | 848 (8.2%) | 1,622 (7.8%) | 1,133 (11.5%) | 991 (10.0%) | 2,124 (10.8%) |
| Weapon carrying | 1,183 (11.1%) | 1,294 (12.4%) | 2,477 (11.7%) | 1,119 (11.3%) | 1,197 (11.9%) | 2,316 (11.6%) |
| Risky Sexual Activity | 2,349 (22.6%) | 2,709 (26.5%) | 5,058 (24.5%) | 4,378 (45.2%) | 4,596 (47.2%) | 8,974 (46.2%) |
| Academic Failure | 2,544 (24.2%) | 2,547 (24.6%) | 5,091 (24.4%) | 4,061 (41.2%) | 3,816 (38.4%) | 7,877 (39.8%) |
Only a very small percentage of 10th and 12th graders reported sleeping 10 or more hours (1.1% and 0.9%, respectively).
On average, students reported an average cumulative protective factor score of 6 (Table 1). The means and standard deviations for the cumulative protective factors) were similar between 10th and 12th grade, ranging from 5.86 (SD=2.58) to 6.08 (SD=2.62).
From the least to most prevalent, rates of risk behaviors in 10th graders ranged from 2.1% (use of illicit drugs) to 24.4% (academic failure). Students in 12th grade also reported the use of illicit drugs at the lowest rate (3%), and risky sexual activity was the most prevalent risk behavior (46.2%). Four distinct levels of risk behaviors were identified using LCA in both 10th and 12th grade students (Table 2). The criteria for model selection are shown in Table 4 and the criteria are rapidly decreased from 2 and 3 class-models and slightly decreased after then. The cAIC, BIC, and adj. BIC were minimized at 5 class-models. We reviewed the response probabilities for 3, 4, and 5-class models and decided that a 4 class-model included the largest response probabilities for all health risk behaviors and was clinically relevant. These classes were labeled Low-Risk behaviors (I, N=15,746, 73.7%), Some-Risk behaviors (II, N=477, 2.2%), Moderate-Risk behaviors (III, N=4,458, 20.9%), and High-Risk behaviors (IV, N=671, 3.1%) within 10th graders. The same labels for the four classes were used for the 12th graders but the size of each class differed from the 10th graders: Low-Risk behaviors (I, N=11,196, 55.1%), Some-Risk behaviors (II, N=1,661, 8.2%), Moderate-Risk behaviors (III, N=6,143, 30.3%), and High Risk behaviors (IV, N=1,309, 6.5%). Risk behaviors within each class had similar response probabilities between 10th and 12th except within Class II: Some-Risk behaviors included high risk of alcohol use and risky sexual activity only at 12th grade.
Table 2.
Parameter estimates for LCA with four class-memberships of health risk behaviors in 10th and 12th grade
| LCA in 10th grade Students | ||||
| Class I | Class II | Class III | Class IV | |
| Class-membership Probability* N (%) |
.6723 N=15,746 (73.7%) |
.0595 N=477 (2.2%) |
0.2254 N=4,458 (20.9%) |
0.0428 N=671 (3.1%) |
| Response Probability | ||||
| Alcohol Use | 0.0515 | 0.2391 | 0.4359 | 0.8467 |
| Cigarette Use | 0.0207 | 0.1572 | 0.3695 | 0.7415 |
| Use of illicit drugs | 0.0000 | 0.0248 | 0.0241 | 0.3340 |
| Inappropriate use of Rx/OTC | 0.0134 | 0.2256 | 0.1151 | 0.7030 |
| Weapon carrying | 0.0341 | 0.3085 | 0.2296 | 0.5751 |
| Risky sexual activity | 0.0793 | 0.0002 | 0.6896 | 0.8919 |
| Academic failure | 0.1242 | 0.5099 | 0.4384 | 0.7510 |
| LCA in 12th grade Students | ||||
| Class I | Class II | Class III | Class IV | |
| Class-membership Probability* | 0.5490 N=11,196 (55.1%) |
0.0978 N=1,661 (8.2%) |
0.2795 N=6,143 (30.3%) |
0.0737 N=1,309 (6.5%) |
| Response Probability | ||||
| Alcohol Use | 0.1002 | 0.7082 | 0.5771 | 0.9342 |
| Cigarette Use | 0.0427 | 0.3338 | 0.4979 | 0.8306 |
| Use of illicit drugs | 0.0017 | 0.0000 | 0.0181 | 0.3281 |
| Inappropriate use of Rx/OTC | 0.0168 | 0.0168 | 0.1338 | 0.7467 |
| Weapon carrying | 0.0406 | 0.0406 | 0.1977 | 0.4640 |
| Risky sexual activity | 0.1749 | 0.9972 | 0.7119 | 0.9514 |
| Academic failure | 0.2427 | 0.2296 | 0.6588 | 0.7963 |
Note. Class-membership (Class I=low risk; Class II=some risk; Class III=moderate risk; Class IV=high risk) probability is the estimated probability of belonging to each class-membership and N (%) is the actual number and proportions of students who were classified to each class-membership.
Table 4.
Model Selection for LCA in 10th and 12th grade adolescents
| Model Selection in 10th grade | |||||
| No. of class-memberships | G2 | AIC | cAIC | BIC | Adj. BIC |
| 2 | 1006.6 | 1036.6 | 1171.2 | 1156.2 | 1108.5 |
| 3 | 339.8 | 385.8 | 592.0 | 569.0 | 496.0 |
| 4 | 249.1 | 311.1 | 589.2 | 558.2 | 459.6 |
| 5 | 160.0 | 238.0 | 587.8 | 548.8 | 424.9 |
| 6 | 111.2 | 205.2 | 626.8 | 579.8 | 430.4 |
| Model Selection in 12th grade | |||||
| No. of class-memberships | G2 | AIC | cAIC | BIC | Adj. BIC |
| 2 | 1705.2 | 1735.2 | 1869.0 | 1854.0 | 1806.4 |
| 3 | 428.8 | 474.8 | 679.9 | 656.9 | 583.8 |
| 4 | 286.8 | 348.8 | 625.2 | 594.2 | 495.7 |
| 5 | 180.0 | 258.0 | 605.8 | 566.8 | 442.9 |
| 6 | 139.4 | 233.4 | 652.6 | 605.6 | 456.2 |
Note. cAIC and Adj. BIC are representing consistent AIC and adjusted BIC, respectively
Associations among sleep duration, protective factors and risk behaviors in bivariate analysis
Table 3 shows the odds ratios of Class II, III, and IV for total sleep time and cumulative protective factors after adjusting for age, sex, race, and survey year. Male students were more likely to belong to higher risky behavior classes (Class II, III, and IV) compared to class I among both 10th and 12th grade students. White students were more likely to belong to higher risky behavior Classes III and IV compared to class I among both 10th and 12th grade students. While there were no significant race differences in belonging to Class II versus I among 10th graders, white adolescents in 12th grade were three times more likely to belong to group II versus group I. Older age adolescents in 10th grade were more likely to belong to classes II-IV compared to Class I.
Table 3.
Odds Ratio of class-memberships with high risky behaviors (Class II, III, IV) compared to low risky behaviors (Class I) for total sleep time, protective factor, age, gender, race, and survey year at 10th and 12th grades
| Odds Ratio (OR) of high risky behaviors at 10th grade | ||||
| Class II OR (95% CI) |
Class III OR (95% CI) |
Class IV OR (95% CI) |
p-value | |
| Total Sleep Time | ||||
| Short (<8h) vs. Recommended (8–9h) | 1.38 (1.06, 1.80)* | 1.16 (1.05, 1.27) * | 1.26 (0.99, 1.61) | .0001 |
| Long (≥10h) vs. Recommended (8–9h) | 1.02 (0.32, 3.29) | 1.83 (1.31, 2.57) * | 2.65 (1.33, 5.28) * | |
| Protective Factor | 0.75 (0.72, 0.78) * | 0.74 (0.73, 0.75) * | 0.57 (0.54, 0.59) * | <.0001 |
| Age | 1.28 (1.06, 1.55) * | 1.56 (1.45, 1.68) * | 2.09 (1.80, 2.42) * | <.0001 |
| Sex (Male vs. Female) | 1.59 (1.30, 1.94)* | 1.34 (1.24, 1.44) * | 1.36 (1.14, 1.62) * | <.0001 |
| Race (White vs. Non-white) | 1.19 (0.97, 1.45) | 1.19 (1.10, 1.28) * | 1.33 (1.11, 1.59) * | <.0001 |
| Survey year (2014 vs. 2012) | 0.98 (0.80, 1.19) | 0.89 (0.82, 0.95) * | 0.74 (0.62, 0.88) * | .0003 |
| Odds Ratio (OR) of high risky behaviors at 12th grade | ||||
| Class II OR (95% CI) |
Class III OR (95% CI) |
Class IV OR (95% CI) |
p-value | |
| Total Sleep Time | ||||
| Short (<8h) vs. Recommended (8–9h) | 0.89 (0.77, 1.04) | 1.04 (0.94, 1.15) | 0.90 (0.74, 1.08) | .2212 |
| Long (≥10h) vs. Recommended (8–9h) | 0.59 (0.28, 1.24) | 1.05 (0.72, 1.53) | 1.28 (0.72, 2.27) | |
| Protective Factor | 0.89 (0.87, 0.91) * | 0.78 (0.77, 0.80) * | 0.64 (0.62, 0.66) * | <.0001 |
| Age | 1.13 (0.99, 1.28) | 1.34 (1.24, 1.44) * | 1.22 (1.06, 1.40) * | <.0001 |
| Sex (Male vs. Female) | 0.80 (0.72, 0.89) | 1.12 (1.04, 1.20) * | 1.32 (1.16, 1.51) * | <.0001 |
| Race (White vs. Non-white) | 3.02 (2.69, 3.39) * | 1.34 (1.25, 1.44) * | 2.20 (1.93, 2.51) * | <.0001 |
| Survey year (2014 vs. 2012) | 0.98 (0.88, 1.09) | 0.99 (0.92, 1.06) | 1.13 (0.99, 1.28) | .2397 |
Note. Odds ratios and 95% confidence intervals were estimated from multinomial regression models. Class I=low risk; Class II=some risk; Class III=moderate risk; Class IV=high risk
indicates significant OR
Sleep duration and risk behaviors
Among 10th grade students, those reporting ≤7 hours versus the recommended 8–9 hours of sleep had a significantly higher odds of class membership in Class II (OR 1.38 CI=1.06, 1.80) and III (OR 1.16, CI 1.05, 1.27), and marginally significant in Class IV (OR 1.26, CI .99, 1.61) levels of risk behaviors compared to low level of risk behavior (Class I) (Table 3). Regarding those reporting >10 hours of sleep, students in 10th grade were significantly more likely than those students who slept the recommended duration to be in Class III (OR 1.83, CI 1.31, 2.57), and IV (OR 2.65, CI 1.33, 5.28) levels of risk behaviors behavior compared to low level of risky behavior (Class I). Among 12th graders, the relationship between classes of risk behaviors and sleep duration was not significant, despite having higher incidence of risk behaviors.
Protective factors and risk behaviors
The associations between cumulative (0–10) protective factors and risk behaviors after adjusting for the covariates are shown in Table 3. Students with greater cumulative protective factors were less likely to belong to a class-membership of higher risk behaviors rather than low risk behavior class membership in both 10th and 12th grades. The odds ratios for greater cumulative protective factors are significantly less than 1 in 10th grade (Class II (OR= .75 CI = .72, .78), Class III (OR .74, CI=.73, .75), Class IV (OR .57 CI=.54, 59) as well as 12th grade (Class II (OR .89 CI=.98, 91), Class III (OR .78 CI=.77, 80), and Class IV (OR .64. CI=.62, 66)).
Interaction between sleep and protective factors on risk behaviors
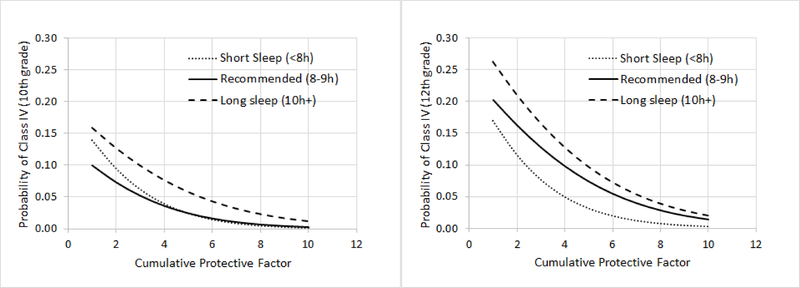
Upon determining that healthy sleep duration and protective factors were uniquely associated with lower risk behavior class-membership, we examined the interaction of sleep and protective factors. We did not find significant interaction between sleep duration and cumulative protective factors on the healthy risk behavior class-memberships in either group. Figure 1 shows the estimated probabilities of belonging to the highest risk class-membership of healthy behaviors (Class IV) in short sleep (<8h), recommended sleep (8–9h), and long sleep (10h+) duration across cumulative protective factors in 10th and 12th grade samples. The graph shows less likelihood of the most risky class of health behaviors in the healthy sleep durations compared to short and long duration when the cumulative protective factor was zero in 10th grade. While the probability of risk behaviors was higher among 12th graders who reported fewer protective factors, healthy sleep did not provide additional protection.
Figure 1.
Predicted probability of high risky behavior class-membership (Class IV) across cumulative protective factor with different sleep time
Note. The estimated probabilities were obtained from multinomial regression model with protective factor, total sleep time, and their interaction at 10th and 12th grade separately.
Discussion
Previous studies have examined the role of sleep as a risk factor for adolescent risk behaviors17,37 The unique contribution of our results is the focus on sleep as a protective factor for similar risk behaviors. Our findings indicate that when younger adolescents (10th graders) obtain the recommended amount of sleep, adolescent risk behaviors are attenuated, specifically in those adolescents who report fewer socioecological protective factors. Exploration of healthy sleep duration as a potential buffering factor in combination with socioecological protective factors among younger adolescents is warranted. Considering that children will spend 40% of their lives sleeping by the time they are 18 years old, primary care pediatric providers play an important role in messaging about sleep health. However, a recent review of the literature found that sleep is not commonly addressed in pediatric primary care visits; there are even lower rates of identification of sleep problems and interventions to address sleep health.38 Future studies using a longitudinal design to expand and replicate our findings could have important implications for increasing attention on sleep health in primary care and developing tailored, cost-effective interventions for adolescents in low resource communities or who otherwise report a low connection with their peers, families, school and/or communities.
Further implications for this study include evidence to provide more sleep opportunity for adolescents. Researchers have linked early school start times, which limit the opportunity for sleep and are in direct conflict with natural circadian rhythms, to many negative consequences, including depression symptoms and suicidal ideation, substance use,16 increased sports-related injuries in student athletes,21 and an increased risk of drowsy driving and motor vehicle crashes,20 as well as other injury-related risk behaviors such as not wearing a seatbelt and texting while driving.39 This is further compounded by “social jet lag” that results from the common practice of extending sleep on weekends.40 Conversely, there is growing evidence that later school start times are associated with less depression41,42 and fewer car crashes43–45 as well as improved academic achievement, higher standardized test scores, reduced absenteeism, and higher graduation rates.46 There has been considerable discussion about which students would benefit most from later start times, and our study may help inform these decisions. For example, we found that 10th graders who achieved the recommended hours of sleep participate in less risky behaviors; this same association was not found in 12th graders, suggesting that in terms of risk behaviors, younger teens may benefit most from delayed start times. Results from this study suggest that sleep is a protective factor in reducing adolescent risk taking behaviors, thus providing an argument for increased sleep opportunity resulting from later school start times.
The use of LCA allowed us to cluster adolescent risk behaviors and simultaneously examine the association of these clusters with socioecological protective factors and sleep duration. In this way we focused on sleep duration as a protective factor, arguably one that may be more easily modifiable that the socioecological protective factors. Our results validate the well-established literature on the high prevalence of poor sleep duration among adolescents.39,47,48 Hence, much more work is needed to help meet the goal rate of 33% of adolescents who receive 8 or more hours of sleep as highlighted by the Healthy People 2020 sleep initiatives.19
Consistent with previous studies, adolescents in this study reported concurrent risk behaviors. An increasing number of studies examine risk factors in clusters, and just as described in a recent systematic review,49 our findings indicate that sexual risk behavior clustered together with alcohol and cigarette use. An understanding of how adolescents’ risk behaviors are clustered has important implications for the development and tailoring of interventions.50 The consensus of the research on clustering of adolescent risk behaviors is to approach prevention by identifying when to optimally intervene and focus on promoting healthy lifestyles.49,50
Protective factors operate within the socioecological levels of individual, interpersonal (family and friends), organization (school), and community.51 While there is strong evidence to support the role of protective factors in reducing rates of adolescent risk behaviors, morbidity and mortality rates related to risk behaviors remain high.14,52–54 Identifying additional ways to reduce adolescent risk behaviors remains one of both critical importance and ongoing study.12–14 Thus, our findings that sleep is associated with fewer risk behaviors has important clinical and policy implications. For example, a recent MMWR publication highlighted the development of coordinated school health models such as the Whole School, Whole Community, Whole Child model to provide safe, supportive environments and increase engagement from the community and families (i.e. protective factors) in order to reduce the risk of academic failure among high school students, a known risk for poorer future health.55 The significant negative association between sleep and protective factors with risk taking behaviors in our study suggests that, at the organization level, coordinated school health models might include sleep as a key variable in future programming.
Our hypothesis that sleep duration would be associated with fewer risk behaviors was less robustly supported among 12th graders and is worth further exploration. One possible explanation could be the maturity in logical reasoning abilities. Logical reasoning abilities reach adult levels by age 16 (typically 11th grade) and therefore could have exerted a stronger influence on risk behaviors than the combination of sleep duration and protective factors among the 12th graders.56 However, understanding the link between neuromaturational processes (many of which extend well into the third decade of life) and real-world behaviors is not well understood and is the focus of many current studies.57 For example, the prefrontal cortex is one of the last areas of the brain to mature and it is the center for judgment making when faced with difficult situations.58 This may be exacerbated by chronic sleep loss. Chronic sleep loss can change behavioral, cognitive, and emotional control centers, located primarily in the prefrontal cortex, that alter thought processes about taking risks.59 Notably, the 12th graders in this study reported very low rates of recommended sleep duration, 14% - much lower than 10th graders. The cross-sectional design of this study and deidentified data set limited our ability to test whether sleep loss persisted or worsened in individuals from 10th to 12th grade.
There are several strengths and limitations in this study. The strength of a large sample size in this study must be balanced with the reliance on self-reported sleep duration data rather than objective sleep data that could be obtained with actigraphy or polysomnography and cross-sectional design. In addition, the adolescent report of sleep duration was limited to nighttime sleep during the school week and therefore did not capture the amount of sleep on the weekends or daytime nap periods. Previous studies have noted that a weekday-weekend sleep discrepancy can lead to functional impairment (“social jet lag”) that may lead to increased risk behaviors.60 Furthermore, due to the limitations of the sleep data, we were not able to explore the possible role of circadian factors, specifically, an “evening chronotype” or circadian-based preference for later bedtimes and wake times, which has been shown to be associated with both deficits in self-regulation48 and increased risk behavior in adolescents.61 While the study sample was large and socio-culturally diverse, the fact that students were from a single school district may limit the generalizability. Finally, we did not have access to survey data regarding students’ race and ethnicity (beyond white versus non-white) or socioeconomic status, therefore limiting more granularity on the potential influence of student background on the variables of interest. Student background, health, and environment (e.g. mental illness, trauma exposure, socioeconomic status, etc.) may have provided additional confounders to understand the context in which adolescents sleep >10 hours a night and report limited protective factors.
Conclusion
Our aims for this study were to extend what is known about the unique influences of protective factors and sleep duration on adolescent risk behaviors and provide population-level data on their associations with adolescent risk behaviors that threaten adolescents’ morbidity and mortality. Considering that more than two-thirds of adolescents sleep less than what is recommended by the American Academy of Sleep Medicine and the American Academy of Pediatrics, the negative associations between sleep and adolescent risk taking in the presence of fewer protective factors reported in this paper provides support for programs that support adolescents in obtaining the recommended hours of sleep to supplement the mitigating effects of protective factors on adolescent risk behaviors. The findings that 12th grade students reported receiving adequate sleep at lower rates than 10th grade students suggest that sleep deprivation may be worse among older adolescents. Future work should include longitudinal matched data to examine the patterns of sleep deprivation with risk taking. The potential for such chronic sleep deprivation to negatively affect the prefrontal cortex, the cornerstone for emotion and behavior regulation, has great policy and practice implications to develop interventions to support sleep health earlier in childhood.
Supplementary Material
Acknowledgements
We would like to thank Dr. Maggie Holland and Dr. Fen Ren for their statistical consultation. We are also very grateful to the Fairfax County Public Schools for providing the deidentified data for our analyses and reviewing this manuscript. Monica Ordway is supported by NIH/NINR (K23NR16277). Guanghai Wang was supported by National Natural Science Foundation of China (81601162), Shanghai Municipal Commission of Health and Family Planning (20164Y0001), Shanghai Children’s Medical Center Foundation (YJY-SCMC2016-5), Project of Shanghai Children’s Health Service Capacity Construction (GDEK201708), and Fundamental Research Funds for the Central Universities from the Key Laboratory of Child Development and Learning Science (Southeast University) and the Ministry of Education (CDLS-2018-03)
Financial Support
Monica Ordway is supported by NIH/NINR (K23NR16277) Guanghai Wang was supported by the National Natural Science Foundation of China (81601162, 81773443, 81602868, 81602870), Shanghai Municipal Commission of Health and Family Planning (20164Y0001, 20164Y0095), Shanghai Science and Technology Commission (19QA1405800, 19411968800, 17XD1402800, 14441904004, 17411965300, 18JC1420305, 18JC1420305), Shanghai Pudong District Technology Development Funds (PKJ2018-Y45), Shanghai Jiao Tong University School of Medicine Innovation Team on Pediatric Research Funds, Shanghai Jiao Tong University School of Medicine Child Developing Brian Research Center Construction Funds, Project of Shanghai Children’s Health Service Capacity Construction (GDEK201708), and Fundamental Research Funds for the Central Universities from the Key Laboratory of Child Development and Learning Science (Southeast University) and the Ministry of Education (CDLS-2018-03).
Footnotes
Author Disclosure
All authors report no conflicts of interest to disclose.
Note: The inclusion of Fairfax County Public School’s name in this publication does not imply its support, endorsement or approval of the findings, conclusions, or other contents of this work.
References
- 1.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance - United States, 2009. MMWR Surveill Summ. 2010;59(5):1–142. [PubMed] [Google Scholar]
- 2.Blum RW. Young people: not as healthy as they seem. Lancet. 2009;374(9693):853–854. [DOI] [PubMed] [Google Scholar]
- 3.Kann Laura, Tim McManus William A. Harris, et al. Youth Risk Behavior Surveillance — United States, 2015. In: Summary MS, ed. Vol 65(No. SS-6). https://www.cdc.gov/mmwr/volumes/65/ss/ss6506a1.htm#suggestedcitation2016:1-74. [DOI] [PubMed] [Google Scholar]
- 4.Garrison CZ, McKeown RE, Valois RF, et al. Aggression, substance use, and suicidal behaviors in high school students. Am J Public Health. 1993;83(2):179–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hingson RW, Zha W. Age of drinking onset, alcohol use disorders, frequent heavy drinking, and unintentionally injuring oneself and others after drinking. Pediatrics. 2009;123(6):1477–1484. [DOI] [PubMed] [Google Scholar]
- 6.Heron M Death: Leading causes for 2014 In: U.S. Department of Health and Human Services CfDCaP, National Center for Health Statistics, National Vital Statistics System, ed. Vol 65 Washington, DC: Public Health Service; 2016. [Google Scholar]
- 7.Steinberg L How to Improve the Health of American Adolescents. Perspect Psychol Sci. 2015;10(6):711–715. [DOI] [PubMed] [Google Scholar]
- 8.Laski L Realising the health and wellbeing of adolescents. BMJ : British Medical Journal. 2015;351. [DOI] [PubMed] [Google Scholar]
- 9.Jessor R Risk behavior in adolescence: A psychosocial framework for understanding and action. J Adolesc Health. 1991;12(8):597–605. [DOI] [PubMed] [Google Scholar]
- 10.Leather NC. Risk-taking behaviour in adolescence: a literature review. Journal of Child Health Care. 2009;13(3):295–304. [DOI] [PubMed] [Google Scholar]
- 11.Coley RL, Votruba-Drzal E, Schindler HS. Fathers’ and Mothers’ Parenting Predicting and Responding to Adolescent Sexual Risk Behaviors. Child Dev. 2009;80(3):808–827. [DOI] [PubMed] [Google Scholar]
- 12.Resnick MD, Bearman PS, Blum RW, et al. Protecting adolescent’s from harm: Findings from the national longitudinal study on adolescent health. J Am Med Assoc. 1997;278(10):823–832. [DOI] [PubMed] [Google Scholar]
- 13.Jessor R, Van Den Bos J, Vanderryn J, et al. Protective Factors in Adolescent Problem Behavior: Moderator Effects and Developmental Change. Dev Psychol. 1995;31(6):923–933. [Google Scholar]
- 14.Arthur MW, Hawkins JD, Pollard JA, et al. Measuring Risk and Protective Factors for Use, Delinquency, and Other Adolescent Problem Behaviors. Evaluation Review. 2002;26(6):575–601. [DOI] [PubMed] [Google Scholar]
- 15.Owens J, Au R, Carskadon M, et al. Insufficient Sleep in Adolescents and Young Adults: An Update on Causes and Consequences. Pediatrics. 2014;134(3):e921–e932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Winsler A, Deutsch A, Vorona RD, et al. Sleepless in Fairfax: the difference one more hour of sleep can make for teen hopelessness, suicidal ideation, and substance use. J Youth Adolesc. 2015;44(2):362–378. [DOI] [PubMed] [Google Scholar]
- 17.Owens J, Wang G, Lewin D, et al. Association between short sleep duration and risk behavior factors in middle school students. Sleep. 2017;40(1). [DOI] [PubMed] [Google Scholar]
- 18.Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016;12(6):785–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.HealthyPeople.gov. Sleep Health. https://www.healthypeople.gov/2020/topics-objectives/topic/sleep-health/objectives2015. Accessed February 5, 2015.
- 20.Martiniuk AL, Senserrick T, Lo S, et al. Sleep-deprived young drivers and the risk for crash: the DRIVE prospective cohort study. JAMA Pediatr. 2013;167(7):647–655. [DOI] [PubMed] [Google Scholar]
- 21.Milewski MD, Skaggs DL, Bishop GA, et al. Chronic lack of sleep is associated with increased sports injuries in adolescent athletes. J Pediatr Orthop. 2014;34(2):129–133. [DOI] [PubMed] [Google Scholar]
- 22.Graves JM, Miller ME. Reduced sleep duration and history of work-related injuries among Washington State adolescents with a history of working. Am J Ind Med. 2015;58(4):464–471. [DOI] [PubMed] [Google Scholar]
- 23.McKnight-Eily LR, Eaton DK, Lowry R, et al. Relationships between hours of sleep and health-risk behaviors in US adolescent students. Prev Med. 2011;53(4–5):271–273. [DOI] [PubMed] [Google Scholar]
- 24.Dewald JF, Meijer AM, Oort FJ, et al. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med Rev. 2010;14(3):179–189. [DOI] [PubMed] [Google Scholar]
- 25.Miller SR. Shortcut: High School Grades As a Signal of Human Capital. Educational Evaluation and Policy Analysis. 1998;20(4):299–311. [Google Scholar]
- 26.Pena JB, Matthieu MM, Zayas LH, et al. Co-occurring risk behaviors among White, Black, and Hispanic US high school adolescents with suicide attempts requiring medical attention, 1999–2007: Implications for future prevention initiatives. Soc Psychiatry Psychiatr Epidemiol. 2012;47(1):29–42. [DOI] [PubMed] [Google Scholar]
- 27.Rivera PM, Bray BC, Guastaferro K, et al. Linking Patterns of Substance Use With Sexual Risk-Taking Among Female Adolescents With and Without Histories of Maltreatment. J Adolesc Health. 2018;62(5):556–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sullivan CJ, Childs KK, O’Connell D. Adolescent risk behavior subgroups: An empirical assessment. J Youth Adolesc. 2010;39(5):541–562. [DOI] [PubMed] [Google Scholar]
- 29.Foster CE, Horwitz A, Thomas A, et al. Connectedness to family, school, peers, and community in socially vulnerable adolescents. Children and Youth Services Review. 2017;81:321–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moses JO, Villodas MT. The Potential Protective Role of Peer Relationships on School Engagement in At-Risk Adolescents. J Youth Adolesc. 2017;46(11):2255–2272. [DOI] [PubMed] [Google Scholar]
- 31.Lewin DS, Wang G, Chen YI, et al. Variable School Start Times and Middle School Student’s Sleep Health and Academic Performance. J Adolesc Health. 2017;61(2):205–211. [DOI] [PubMed] [Google Scholar]
- 32.Briney JS, Brown EC, Hawkins JD, et al. Predictive Validity of Established Cut Points for Risk and Protective Factor Scales from the Communities That Care Youth Survey. The Journal of Primary Prevention. 2012;33(5):249–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jessor R Problem Behavior Theory and Adolescent Health: The Collected Works of Richard Jessor. Vol 2: Springer International Publishing; 2017. [Google Scholar]
- 34.Lanza ST, Collins LM. A New SAS Procedure for Latent Transition Analysis: Transitions in Dating and Sexual Risk Behavior. Dev Psychol 2008;44(2):446–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fairfax County Youth Survey School Year 2014–2015. http://www.fairfaxcounty.gov/demogrph/youth_survey/pdfs/sy2014_15_youth_survey_report.pdf Fall, 2015 2015.
- 36.Centers for Disease Control and Prevention. Short Sleep Duration Among US Adults. 2014; https://www.cdc.gov/sleep/data_statistics.html. Accessed January 12, 2019.
- 37.Traube DE, James S, Zhang J, et al. A national study of risk and protective factors for substance use among youth in the child welfare system. Addict Behav. 2012;37(5):641–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Honaker SM, Meltzer LJ. Sleep in pediatric primary care: A review of the literature. Sleep Med Rev. 2016;25(Supplement C):31–39. [DOI] [PubMed] [Google Scholar]
- 39.Wheaton AG, Olsen EO, Miller GF, et al. Sleep Duration and Injury-Related Risk Behaviors Among High School Students--United States, 2007–2013. MMWR Morb Mortal Wkly Rep. 2016;65(13):337–341. [DOI] [PubMed] [Google Scholar]
- 40.Crowley SJ, Carskadon MA. MODIFICATIONS TO WEEKEND RECOVERY SLEEP DELAY CIRCADIAN PHASE IN OLDER ADOLESCENTS. Chronobiol Int. 2010;27(7):1469–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wheaton AG, Ferro GA, Croft JB. School Start Times for Middle School and High School Students - United States, 2011–12 School Year. MMWR Morb Mortal Wkly Rep. 2015;64(30):809–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Minges KE, Redeker NS. Delayed school start times and adolescent sleep: A systematic review of the experimental evidence. Sleep Med Rev. 2016;28:86–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Danner F, Phillips B. Adolescent Sleep, School Start Times, and Teen Motor Vehicle Crashes. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine. 2008;4(6):533–535. [PMC free article] [PubMed] [Google Scholar]
- 44.Vorona RD, Szklo-Coxe M, Wu A, et al. Dissimilar teen crash rates in two neighboring southeastern Virginia cities with different high school start times. J Clin Sleep Med. 2011;7(2):145–151. [PMC free article] [PubMed] [Google Scholar]
- 45.Vorona RD, Szklo-Coxe M, Lamichhane R, et al. Adolescent Crash Rates and School Start Times in Two Central Virginia Counties, 2009–2011: A Follow-up Study to a Southeastern Virginia Study, 2007–2008. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine. 2014;10(11):1169–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wahlstrom K, Dretzke B, M. G, et al. Examining the Impact of Later School Start Times on the Health and Academic Performance of High School Students: A Multi-Site Study. St. Paul, MN: University of Minnesota;2014. [Google Scholar]
- 47.Malone SK, Zemel BS, Compher C, et al. Characteristics associated with Sleep Duration, Chronotype, and Social jet lag in Adolescents. The Journal of school nursing : the official publication of the National Association of School Nurses. 2016;32(2):120–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Owens JA, Dearth-Wesley T, Lewin D, et al. Self-Regulation and Sleep Duration, Sleepiness, and Chronotype in Adolescents. Pediatrics. 2016;138(6). [DOI] [PubMed] [Google Scholar]
- 49.Meader N, King K, Moe-Byrne T, et al. A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health. 2016;16:657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Champion KE, Mather M, Spring B, et al. Clustering of Multiple Risk Behaviors Among a Sample of 18-Year-Old Australians and Associations With Mental Health Outcomes: A Latent Class Analysis. Frontiers in Public Health. 2018;6(135). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: a foundation for future health. The Lancet. 2012;379(9826):1630–1640. [DOI] [PubMed] [Google Scholar]
- 52.DiIorio C, Dudley WN, Soet JE, et al. Sexual possibility situations and sexual behaviors among young adolescents: The moderating role of protective factors. J Adolesc Health. 2004;35(6). [DOI] [PubMed] [Google Scholar]
- 53.Cleveland MJ, Feinberg ME, Bontempo DE, et al. The Role of Risk and Protective Factors in Substance Use across Adolescence. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2008;43(2):157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Whittle S, Simmons JG, Dennison M, et al. Positive parenting predicts the development of adolescent brain structure: A longitudinal study. Dev Cogn Neurosci. 2014;8:7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rasberry C, Tiu G, Kann L, et al. Health-Related Behaviors and Academic Achievement Among High School Students — United States, 2015. 2017;66:921–927. Accessed September 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Steinberg L Risk Taking in Adolescence. Curr Dir Psychol Sci. 2007;16(2):55–59. [Google Scholar]
- 57.Johnson SB, Blum RW, Giedd JN. Adolescent Maturity and the Brain: The Promise and Pitfalls of Neuroscience Research in Adolescent Health Policy. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2009;45(3):216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Giedd JN. Structural magnetic resonance imaging of the adolescent brain. Ann N Y Acad Sci. 2004;1021(1):77–85. [DOI] [PubMed] [Google Scholar]
- 59.Killgore W Sleep Deprivation and Behavioral Risk-Taking. 2015.
- 60.Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31(6):175–184. [DOI] [PubMed] [Google Scholar]
- 61.Wang L, Chartrand TL. Morningness-eveningness and risk taking. J Psychol. 2015;149(3–4):394–411. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.