Abstract
Introduction:
Most important in the evaluation of thyroid thyroid disease is to differentiate a disease that is treated medically from a disease that requires surgical treatment. In preoperative differentiation of a malignant from a benign lesion are used different diagnostic methods (US, scintigraphy, FNAC, MRI).
Aim:
The aim of the study was to determine the diagnostic value of fine needle aspiration cytology (FNAC) and serum thyroglobulin antibodies (TgAb) values in individual cytological categories.
Methods:
The prospective study included 100 patients with scintigraphic cold thyroid nodules divided into two groups. The first group consisted of 50 patients with histopathological verified benign nodules and the second group of 50 patients with histopathological verified benign nodules. Demographic datas, FNAC findings, TgAb levels and final histopathological findings were recorded. FNAC with ultrasound (US) guidance was performed by the so-called Free hand technique. TgAtb values were estimated by the radio-immunity assay (RIA) method.
Results:
In patients with histopathological findings of a benign nodule, 20 patients had a cytological finding of a colloidal nodule, 18 patients had a cellular nodule, 12 had a finding of follicular neoplasm. In patients with a histopathological finding of the malignant nodule, 9 patients had a cytological finding of a colloidal nodule, 8 had a cellular nodule, 21 follicular neoplasm and 12 patients had cancer. FNAC had a sensitivity of 66%, specificity of 76%, a positive predictive value of 73%, a negative predictive value of 69%. The highest preoperative serum TgAb values were in patients with cytologic findings of cancer, and the lowest in the cellular nodule.
Conclusion:
The finding of FNAC together with serum TgAb values contributes to better diagnosis and selection of patients requiring surgery.
Keywords: FNAC, thyroid nodule, thyroid malignancy, thyroglobulin antibodies
1. INTRODUCTION
Most important in the evaluation of thyroid thyroid disease is to differentiate a disease that is treated medically from a disease that requires surgical treatment. In preoperative differentiation of a malignant from a benign lesion are used different diagnostic methods (US, scintigraphy, FNAC, MRI). However, none of the above diagnostic methods has 100% accuracy (1, 2, 3). FNAC with US guidance is the most important method in the evaluation of thyroid nodules because of its high diagnostic reliability and low risk of complications. The introduction of this method has reduced the number of unnecessary operations of thyroid gland. FNAC contributed that the highest number of thyroidectomies are performed in patients with malignant thyroid nodules (4, 5). Although most thyroid lesions are easily recognized by this method, there are still difficulties in distinguishing between follicular adenoma, well-differentiated follicular cancer, and follicular variants of papillary carcinoma. Due to the nature of the method itself, FNAC of the thyroid gland cannot distinguish follicular cancer from follicular adenoma. They differ in tumor invasion of the capsule (6, 7).
Some studies investigated the role of TgAb in the preoperative prediction of thyroid malignancy (8, 9, 10). FNAC and determination of preoperative TgAb values can contribute to better diagnosis of scintigraphically cold thyroid nodles and to the selection of patients who require surgery.
2. AIM
The aim of the study was to determine the diagnostic value of fine needle aspiration cytology (FNAC) and serum thyroglobulin antibodies (TgAb) values in individual cytological categories.
3. METHODS
The prospective study included 100 patients with scintigraphically cold thyroid nodules treated at the Department for Thyroid Gland Diseases, Radiology and Nuclear Medicine Clinic and at the Department for Ear, Nose and Throat (ENT) Diseases of the University Clinical Center Tuzla. The patients included in the study were both sexes divided into two groups based on final histopathological report. The first group consisted of 50 patients with histopathologically verified malignant nodules. The second group consisted of 50 patients with histopathologically verified benign nodeules. The subjects of this study were patients who had preoperative clinical examination, thyroid hormone finding and serum TSH, US, FNAC, TgAb, scintigraphically cold nodule (solitary, or multiples) and which had a orderly functional state of the thyroid gland. Patients with scintigraphically warm and hot nodules were excluded from the study. The study also excluded patients with functional thyroid disorders and those who did not have the complete medical records provided by the diagnostic protocol. The following datas were analyzed: age, sex, scintigraphic finding of cold nodules, FNAC fiding, serum TgAb values in malignant and benign thyroid nodules and in separate cytological categories. FNAC with US guidance was performed with 21-22 gauge needles attached to 10-20ml plastic syrings, by “free-hand technique”. Each punctured node is localized exactly, its size and echostructure is indicated, so that it can be compared with the cytological finding. Immediately after puncture, the aspirates were smeared on slides, sprayed with fixation spray and allowed to dry at room temperature and then stained using the Pappanicolau method. Subsequently, the dried preparations were analyzed microscopically at the Department of Pathological Anatomy of the University Clinical Center Tuzla. Based on cytological analysis, the findings were classified into three categories: benign, suspected malignant and malignant lesion. The benign lesion is represented by a cytologic finding of the colloidal and cellular thyroid nodule. A suspected malignant lesion was a cytologic finding of a follicular neoplasm. A malignant lesion is a cytologic finding that, according to cytomorphological criteria, indicates to a malignant tumor of the thyroid gland. After surgery, the surgical material was examined at the Department of Pathology at the University Clinical Center Tuzla. Slices were taken from the nodule for microscopic analysis, and after fixation in formalin and paraffin molding, they were cut to a thickness of up to 5 microns. They were then stained with the standard hemalaun-eosin method (HE).
Thyroglobulin antibodies (TgAb) were determined by radioimmunoassay in the serum of the patients. TgAb reference values in UCC Tuzla laboratory are <60 IU / mL. The surgery was performed at the ENT Clinic in General Endotracheal Anesthesia. Indications for the surgery of benign thyroid lesions included the size of nodules (due to compressive syndrome) or retrosternal node extension as well as cosmetic reasons (at the patient’s request). A conventional method and the operation with an ultrasonic blade were applied. For statistical data processing for comparison of continuous variables, the T test of independent samples was used, or the Mann-Whitney test, depending on the symmetry of the data distribution. Sensitivity, specificity value were calculated by diagnostic tests. Specificity was the presence of benign lesions identified by FNAC (negative report); sensitivity was the presence of malignant lesions identified cytologically (positive for malignancy) and accuracy was percentage of total lesions (benign or malignant) identified correctly. The data was statistically analyzed using MedCalc Software, Mariakerke, Belgium. P values <0,05 were considered statistically significant.
4. RESULTS
The average age of the subjects was 46 ± 13 years. There were 12 men and 88 women. The mean age in the groups with benign and malignant nodes was 46 ± 12 and 47 ± 15 years, (p> 0.05), and the sex distribution was identical, with 6 males and 44 females in both groups (p> 0.05 ).
Table 1 shows the relationship between individual cytological categories and histopathological findings.
Table 1. Relationship between individual cytological categories and histopathological findings.
| Histopathology | FNAC | Total | |||
|---|---|---|---|---|---|
| colloidal nodus | cellular nodus | follicular neoplasm | cancer | ||
| Benign lesions | 20 | 18 | 12 | 0 | 50 |
| Malignant lesions | 9 | 8 | 21 | 12 | 50 |
| Total | 29 | 26 | 33 | 12 | 100 |
| p | <0,0001 | ||||
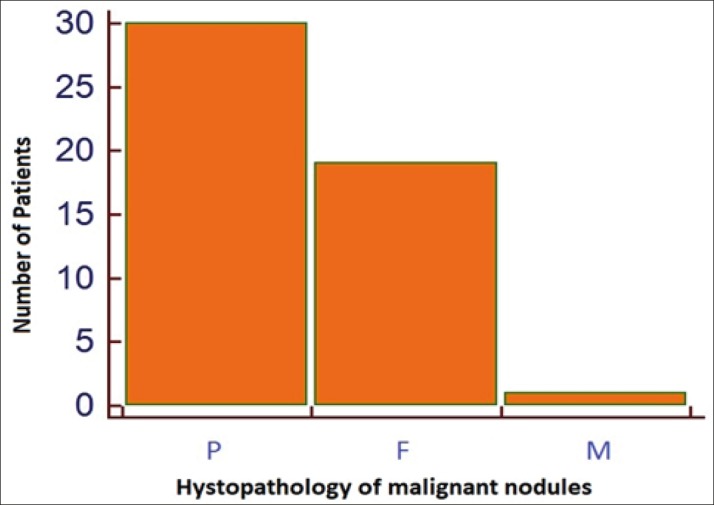
Of the 50 patients with a histopathological diagnosis of a malignant lesion, 30 patients were diagnosed with papillary carcinoma, 19 patients with follicular cancer, and 1 patient with a finding of medullary cancer (Figure 1).
Figure 1. Distribution types of carcinoma in the total number of malignant lesions (P-papillary; F-follicular; M-medullary).
The cytological findings of cold nodes are shown in Table 2. The diagnostic value of FNAC in the detection of thyroid cancer is shown in Table 3. Table 3 shows that FNAC had a sensitivity of 66%, specificity of 76%, a positive predictive value of 73%, a negative predictive value of 69%. If cancer is present, FNAC will detect it in 66% of cases. The diagnostic accuracy of FNAC was 71% in our patients.
Table 2. Comparison of cytological findings with pathohistological findings.
| FNAC finding | Histopathology | ||
|---|---|---|---|
| Malignant (n=50) | Benign (n=50) | Total (n=100) | |
| Malignant Benign | 33(66%) 17(34%) | 12(24%) 38(76%) | 45 55 |
| Total | 50 (100 %) | 50 (100%) | 100 |
Table 3. Diagnostic Accuracy of FNAC in detection of thyroid cancer.
| Test Validity | |
|---|---|
| Sensitivity Specificity Positive predictive value Negative predictive value Diagnostic Accuracy of malignancy |
66% 76% 73% 69% 71% |
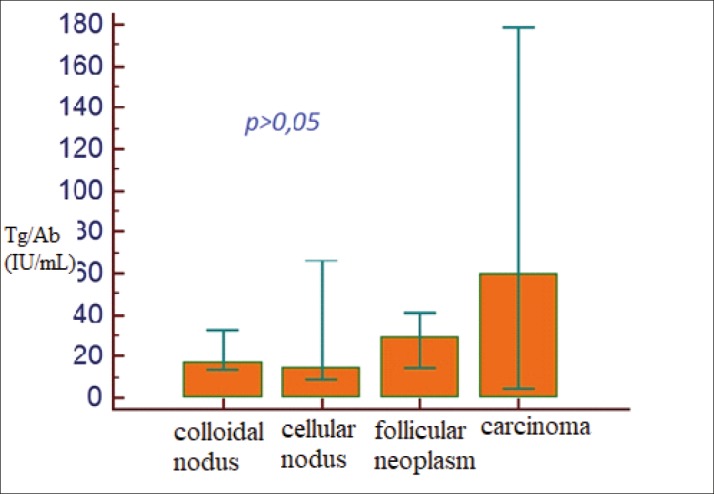
TgAb values in the groups with colloidal nodus, cellular nodus, follicular neoplasm, and cancer were 17, 14, 29, or 59 ng / ml, (Figure 2). The highest TgAb values were observed in the cytological categories of cancer and follicular neoplasm. There was no statistically significant difference between individual cytological categories (p> 0.05)).
Figure 2. Distribution of TgAb values according to the FNAC finding.
5. DISCUSSION
Most important in the evaluation of thyroid nodose disease is to differentiate a disease that is treated medically from a disease that requires surgical treatment. Preoperative differentiation of a malignant from a benign lesion uses different diagnostic methods (US, scintigraphy, FNAC, MRI). However, none of the above diagnostic methods has 100% accuracy (3, 4). FNAC with US guidance is the most significant method in the evaluation of thyroid nodules because of its high diagnostic reliability and low risk of complications. The introduction of this method has reduced the number of unnecessary thyroid gland operettas.
In our study, FNAC had a sensitivity of 66%, specificity of 76%, a positive predictive value of 73%, a negative predictive value of 69%, a diagnostic accuracy of 71%. The results are partially comparable to other published data, which reports a sensitivity ranging from 65% to 98%, specificity from 72% to 100%, and an overall accuracy of 75% to 90%. (11) Other studies on solitary thyroid nodule FNAC have shown sensitivity and specificity of 68.1% and 100% (12), 75% and 100% (13), 89.4% and 99.2% (14),, 78.1% and 76.5 % (15). In a study from Mistry et al. in a sample of 67 patients, the sensitivity was 55.3 patients with a false-negative rate of 44.7%. The sensitivity in their study was also lower than the sensitivity in recent literature (16). In a study by Georgescu et al. FNAC sensitivity was 76.47%, specificity 83.1%, positive predictive value was 35.1%, negative predictive value was 96.7%, false positive rate 16,%, false negative rate 23%, accuracy was 82.3%. (17).
Recent studies have reported the diagnostic value of TgAb in the preoperative prediction of thyroid malignancy (8, 9, 10). In our study, the highest TgAb values were observed in the cytological categories of cancer and follicular neoplasm.
Boi et al. in a retrospective study on an unselected consecutive sample of 590 patients with thyroid nodules compared the FNAC US guidance findings with serum anti-thyroid antibody (ATA) values. Their results show that ATAs were positive in 197 patients, while the remaining patients (393) did not have elevated serum ATAs. Based on this, these authors found a high prevalence of malignant and suspected malignant cytologic findings in patients with positive ATA versus patients with negative ATA. They had a low prevalence of positive ATA with cytologic findings, which they identified as a benign lesion. The operated patients who were diagnosed with histopathologically with thyroid cancer (among which papillary was the most prevalent) belonged to the group of patients in whom ATA was positive. Therefore, these authors recommend further research to demonstrate the association between thyroid autoimmunity and cancer (18).
The results of our study are similar to the results of the study conducted by Boi et al. We had the highest TgAb values in patients with a cytologic diagnosis of cancer, followed by patients with a suspected malignant cytologic finding (follicular neoplasm). The major problem in diagnosis is the cytologic finding of the follicular neoplasm, which belongs to the category of suspected malignant cytological findings. Based on cytological finding, it is not possible to conclude with certainty whether it is a follicular adenoma or a cancer. Only on the basis of the capsule invasion can it be concluded that this is a cancer, and this can only be seen on the histopathological findings. As we found in our sample the highest serum TgAb values in patients who had a cytologic finding of cancer, and in the second place in the cytological finding follicular neoplasm, this data could be used in further studies on a larger sample.
6. CONCLUSION
Although FNAC is of great importance in the preoperative diagnosis of thyroid malignancy, in some cases it is not sufficient for the accuracy of preoperative diagnosis, especially in doubtful cytological findings (follicular neoplasm). Increased TgAb values in patients with indeterminate cytologic findings according to our study could help in more accurate preoperative selection of patients with suspected thyroid malignancy.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent forms
Author’s contribution:
A.B, M.P.G., A.B and M.A.P gave substantial contributions to the conception or design of the work in acquisition, analysis, or interpretation of data for the work. A.P and I.M. had a part in article preparing for drafting or revising it critically for important intellectual content, and I.M. gave final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflicts of interest:
There are no conflicts of interest.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Camargo R, Corigliano S, Friguglietti C, Gauna A, Harach R, Munizaga F, et al. Latin American Thyroid Society recommendations for management of thyroid nodules. Arq Bras Endocrinol Metab. 2009;53(9):1167–1175. doi: 10.1590/s0004-27302009000900014. [DOI] [PubMed] [Google Scholar]
- 2.Harach HR, Ceballos GA. Thyroid cancer, thyroiditis and dietary iodine: a review based on the Salta, Argentina model. Endocr Pathol. 2008;19(4):209–220. doi: 10.1007/s12022-008-9038-y. [DOI] [PubMed] [Google Scholar]
- 3.Castro MR, Gharib H. Thyroid nodules and cancer. When to wait and watch, when to refer. Postgrad Med. 2000;107(1):113–116. 119–120, 123–124. doi: 10.3810/pgm.2000.01.808. [DOI] [PubMed] [Google Scholar]
- 4.Lansford C. Evaluation of Thyroid Nodule. Carle Selected Paper. 2011;52(1):12–22. [Google Scholar]
- 5.Sidawy MK, Del Vecchio DM, Knoll SM. Fine needle aspiration of thyroid nodules: correlation between cytology and histology and evaluation of discrepant cases. Cancer. 1997;81(4):253–259. doi: 10.1002/(sici)1097-0142(19970825)81:4<253::aid-cncr7>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 6.Bomeli SR, LeBeau SO, Ferris RL. Evaluation of a thyroid nodule. Otolaryngol Clin North Am. 2010;43(2):229–238. doi: 10.1016/j.otc.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baloch ZW, LiVolsi VA, Asa SL, Rosai J, Merino MJ, Randolph G, et al. Diagnostic terinology and morphologic criteria for cytologic diagnosis of thyroid lesions: a synopsis of the National Cancer Institute Thyroid Fine-Needle Aspiration State o the Science Conference. Diagn Cytopathol. 2008;36(6):425–437. doi: 10.1002/dc.20830. [DOI] [PubMed] [Google Scholar]
- 8.Kim ES, Lim DJ, Baek KH, Lee JM, Kim MK, Kwon HS, Song KH, Kang MI, Cha BY, Lee KW, Son HY. Thyroglobulin antibody is associated with increased cancer risk in thyroid nodules. Thyroid. 2010;20(8):885–891. doi: 10.1089/thy.2009.0384. [DOI] [PubMed] [Google Scholar]
- 9.Hosseini S, Payne RJ, Zawawi F, et al. Can preoperative thyroglobulin antibody levels be used as a marker for well differentiated thyroid cancer? Journal of Otolaryngology - Head & Neck Surgery. 2016;45:31. doi: 10.1186/s40463-016-0143-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qin Jing, Yu Zhenqian, Guan Haixia, et al. High Thyroglobulin Antibody Levels Increase the Risk of Differentiated Thyroid Carcinoma. Disease Markers. 2015 doi: 10.1155/2015/648670. Article ID 648670, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Musani MA, Khan FA, Malik S, Khambaty Y. Fine needle aspiration cytology: sensitivity and specificity in thyroid lesions. J Ayub Med Coll Abbottabad. 2011 Jan-Mar;23(1):34–36. [PubMed] [Google Scholar]
- 12.Aggarwal SK, Jayaram G, Kakar A, Guel GD, Prakash R, Pant CS. Fine needle aspiration cytologic diagnosis of the solitary cold thyroid nodule - comparison with ultrasonography, radionuclide perfusion and xeroradiography. Acta Cytol. 1989;33(1):41, 7–20. [PubMed] [Google Scholar]
- 13.Bapat RD, Shah SH, Relekar RG, Pandit A, Bhandarkar SD. Analyis of 105 uninodulargoitres. J Postgrad Med. 1992;38:60–1. 21. [PubMed] [Google Scholar]
- 14.Gupta M, Gupta S, Gupta VB. Correlation of fine needle aspiration cytology with histopathology in the diagnosis of solitary thyroid nodule. J Thyroid Res. 2010;3 doi: 10.4061/2010/379051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duek SD, Goldenberg D, Linn S, Krausz MM, Hershko DD. The role of fine-needle aspiration and intraoperative frozen section in the surgical management of solitary thyroid nodules. Surg Today. 2002;32(10):857–861. doi: 10.1007/s005950200167. [DOI] [PubMed] [Google Scholar]
- 16.Mistry SG, Mani N, Murthy P. Investigating the value of fine needle aspiration cytology in thyroid cancer. J Cytol. 2011 Oct;28(4):185–190. doi: 10.4103/0970-9371.86345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Georgescu R, Oprea A, Contra A, et al. The Sensitivity and Specificity of Fine-Needle Aspiration in Thyroid Neoplasia. Journal of Interdisciplinary Medicine. 2017;2(2):127–131. doi: 10.1515/jim-2017-0047. Retrieved 10 Dec. 2019. [DOI] [Google Scholar]
- 18.Boi F, Lai M L, Marziani B, Minerba L, Faa G, Mariotti S. High prevalence of suspicious cytology in thyroid nodules associated with positive thyroid autoantibodies. European Journal of Endocrinology. 2005;153:637–642. doi: 10.1530/eje.1.02020. [DOI] [PubMed] [Google Scholar]


