Abstract
Background:
Gorham-Stout disease (GSD) is a rare skeletal disorder characterized by massive osteolysis of a bony area in the body. When it hits the shoulder, the patient is faced with a debilitating limitation in terms of motion, stability and quality of life. GSD etiology and pathology are unknown and, as a result, therapeutic modalities remain unclear. The aim of this paper is to explore and offer medical insight into the possible etiologies, pathologies and therapeutic modalities of GSD in the shoulder.
Methods:
We explored PubMed/Medline for GSD cases in the shoulder. The search involved all articles published from database inception until February 1, 2019. Only articles published in English were included. Demographics and clinical information extrapolated from the reported cases were analyzed to deduce patterns and infer conclusions.
Results:
Only 32 studies met our criteria, with a total of 37 cases (n=37). Males predominated in 21 cases (57%). Twelve cases (32%) were younger than 18 years, and 18 cases (49%) were aged between 18 and 65 years. Shoulder pain was the predominant reporting symptom. The humerus was the most common shoulder site affected (54%), followed by the scapula (35%) and the clavicle (30%). Almost half of the cases affected the right shoulder (51%), the left shoulder was affected in 16 cases (43%). Conservative treatment was opted in 17 cases (46%), while surgery was performed in 13 cases (35%). Good outcomes were reported in 28 cases (76%), while death occurred twice (5%).
Conclusion:
Understanding the demographics and clinical characteristics of GSD in the shoulder region will help in formulating better therapeutic interventions and preventive health policies.
Key Words: one loss, Gorham-stout disease, steolysis, houlder
Introduction
Gorham-Stout disease (GSD), also known as primary bone lymphangioma, hemangiomatosis with massive osteolysis, or vanishing bone disease, is a rare skeletal disorder that is characterized by massive osteolysis of a bone or a contiguous group of bones in the body (1). Bone loss occurs due to the replacement of normal intramedullary fat tissue and bone marrow with proliferating lymphatic vessels (2-6). Gradually, non-neoplastic fibrovascular tissues enclose the affected bone and lead to bone resorption (6). GSD is often included in a group of massively osteolytic diseases like Winchester syndrome and hereditary and non-hereditary multicentric osteolysis. There has been no consensus regarding the etiology or pathology of GSD. As such, therapeutic modalities remain under question (7).
GSD affects bony areas in the body that form via intramembranous ossification like the spine, the ribs, the shoulders, the pelvis and the skull (8-12). GSD in the shoulder joint is especially incapacitating, knowing that the shoulder is the joint with the most motion in the human body. As a result, the spontaneous onset of GSD in the shoulder joint presents a huge limitation to the patient in terms of movement, general stability and quality of life (13).
Given the rarity of this disease, few cases of GSD in the shoulder area exist in the medical literature. This work aims to explore the demographics and clinical characteristics of patients with GSD, describe the possible pathologies of GSD in the shoulder region and extrapolate effective therapeutic modalities based on a systematic review of the literature.
Materials and Methods
Search Strategy and Selection Criteria
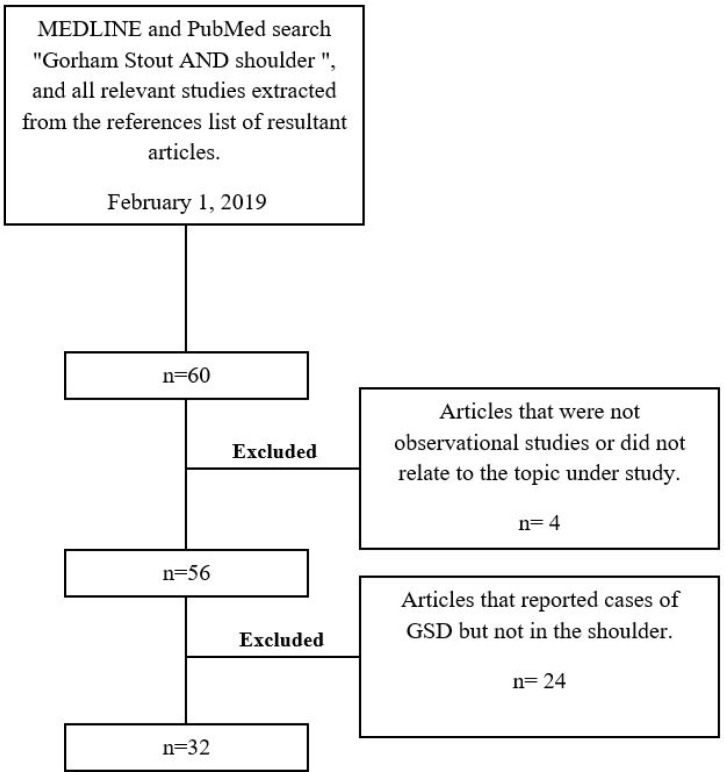
To explore the different cases of GSD in the shoulder reported in the literature, sources were identified by searching MEDLINE and PubMed for English language articles published from database inception until February 1, 2019. We used the following search terms: “Gorham Stout” and “shoulder”, and the boolean operator “AND” was utilized to combine both search terms. Additional studies were identified from the reference lists of retrieved articles. Only observational studies, interventional trials and case reports were included [Figure 1].
Figure 1.
Article selection process
Data Collection
The articles were reviewed critically by authors and included as appropriate to provide readers with a current overview on the etiologies, pathologies, and presentations of GSD in the shoulder. Information was acquired from the final data set on GSD presentation, diagnosis and treatment. In addition, demographics and clinical characteristics including age, sex, site of disease and medical history were also collected.
Results
Only 32 studies met our criteria [Table 1] (5, 12, 14-43). These studies reported a total of 37 cases of GSD in the shoulder region (n=37). The demographics and clinical characteristics of the cases reported were assessed and analyzed [Table 2]. Out of the 37 cases reported in the literature, 21 cases (57%) affected males, while 16 cases affected females (43%). Twelve cases (32%) were younger than 18 years, 18 cases (49%) were aged between 18 and 65 years, and seven cases were older than 65 years (19%).
Table 1.
Documented cases of Gorham-Stout Disease of the shoulder in the medical literature. n/a – non-available
| Author | Year | Case Description | Clinical Findings | Prognosis |
|---|---|---|---|---|
| Gorham et al. (14) | 1954 | 16-year-old male presented with pain and deformation of his right clavicle. The affected clavicle was fractured six months prior. | X-ray revealed total absence of the clavicle and osteolysis of the acromion and the scapula. Radiological and histological findings revealed massive osteolysis. | The patient suffered severe complications, and treatment options failed. The patient died 2 years and 5 months after fracturing his clavicle. |
| 44-year-old male presented with right shoulder pain of six months duration and no history of trauma. | Radiographic and histological examination revealed osteolysis of the clavicle, yet no diagnosis could be determined. | Due to the lack of a definite diagnosis, no surgical treatment was taken. The patient acquired an abscess on his triceps that was drained and had an uneventful recovery afterwards. | ||
| Jacobs (15) | 1964 | 31-year-old male presents with an injured right shoulder due to a car accident. | There was a subluxation of the right acromioclavicular joint. He was unable to resume heavy work and felt weakness for months. Radiographic imaging revealed tapering of the bone. | n/a |
| 28-year-old male presents with an injured shoulder after playing Rugby. He complained of severe shoulder pain for months. | Radiographic Imagining revealed bone loss in the shoulder area of the patient. | |||
| Feigl et al. (16) | 1981 | 26-year-old female presented with shortness of breath. She had previously fell and contused her right shoulder. | A roentgenogram revealed a lytic process of the distal third of the lateral right clavicle. Further imaging reveals bilateral pleural effusion. Surgical exploration of the right clavicle revealed complete osteolysis. An ill-defined highly vascularized mass replaced the missing bone. | The vascularized mass was removed and repeated thoracocentesis was done to eliminate the excess fluid. Talcum was instilled into each pleural cavity twice before the accumulation of fluid ceased. Follow-up after 2 years showed normal chest roentgenogram and no signs of additional bone resorption. |
| Hugo and Schmidt (17) | 1989 | Onset of massive Osteolysis in the shoulder due to Gorham Stout disease | n/a | n/a |
| Damron et al. (18) | 1993 | 36-year-old male presented with limited motion in the shoulder region | Osteolysis of normal scapular landmarks in the absence of any palpable soft tissue mass. Magnetic Resonance Imaging (MRI) helped assess the extent of the disease. | Open biopsy was performed of the remaining acromion. After the wound healed, the patient underwent physical therapy to increase shoulder strength control and motion and was kept under close monitoring. |
| Canil et al. (19) | 1994 | 12-year-old male, previously healthy, presents with a 2 week history of dyspnea, left shoulder pain, and chest swelling. | Chest X-ray showed moth-eaten lytic lesions in the ribs, scapula, and clavicle. Computed Tomography (CT) scan showed massive pleural effusion. Histological examination revealed lymphangiomatosis. | A left thoracotomy was performed, and the pleural cavity was evacuated from fluid. The patient was ventilated postoperatively to keep the lungs expanded. At 8 month follow-up, the patient was in a stable condition. |
| Sato et al. (20) | 1995 | 15-year-old boy presents to the hospital with concerns regarding delay of union of humeral fracture. He had previously suffered immense pain around the left shoulder while playing sports, and without any traumatic incident. | Surgery was done and the humerus was fixed with plate and screws. Three months later, no signs of healing were evident under radiological imaging. The shoulder was atrophied and immobilized. Further radiological imaging failed to detect any abnormality. A temporary diagnosis of GSD was made, later confirmed using histological sections. | After attempts at stopping the osteolysis failed, surgical treatment was chosen. The physicians resected the left humeral head and the proximal quarter of the humerus, performed thorough curettage in the distal humerus, and fixed an intramedullary artificial humeral head. The symptoms later subsided, and the patient’s condition became stable. |
| Pans et al. (21) | 1999 | 72-year-old male presenting with increasing pain in right shoulder along with loss of function. | Radiographs suggested massive osteolysis of proximal humerus and destruction of glenoid fossa. | After radiotherapy failed to solve the problem, arthroscopic debridement was carried out. This limited further osteolysis in the region |
| Moller et al. (22) | 1999 | 83-year-old female presented with massive osteolysis of the right proximal humerus, with no history of trauma or other events. | Histological examination revealed bone fragments resorbed by osteoclasts and vascular fibrous tissue. | n/a |
| 56-year-old female presented with increasing pain in her right shoulder of eight weeks duration. | Radiographs showed destruction of the head of the right humerus. Biopsy revealed vascular fibrous tissue, active osteoclasts, and destruction of the spongiosa. | A shoulder arthroplasty was done and the patient made an uneventful recovery. Follow-up 2 months later show no complications. | ||
| Hofbauer et al. (12) | 1999 | 8-year-old male present with weakness in his right dominant arm. | Affected shoulder was significantly lower than the healthy one. Scapula and clavicle were absent upon palpation. There was decreased radiodensity of humerus. MRI confirmed bone destruction. | Bone biopsy was not performed due to concerns of reactive osteolysis. After 6-12 months of gradual bone resorption, stability incurred, and no further damage took place. |
| Mochizuki et al. (23) | 2000 | 14-year-old male presented with a of pain in the right shoulder that started 5 months ago while throwing. Physical examination showed that the contour of the right scapula was smaller than that of the left. The right shoulder also witnessed some limitation in movement. | Radiographic imaging revealed a lytic lesion in the lower part of the right scapula. CT scan revealed a bone defect without a periosteal reaction. Histology revealed hemangiomatosis associated with a few osteoclasts and endothelial-like cells. Massive osteolysis, also known as Gorham Stout disease, was diagnosed. | Radiation therapy failed to stop the osteolysis. Additional therapy was needed to stabilize the scapula and interrupt the osteolysis. The patient reported improvements in mobility and performing daily activities. |
| Rao et al. (24) | 2001 | 40-year-old male manual laborer presented with a 5 month history of shoulder swelling and 5 week history of not being able to lift heavy objects. | Roentgenographic examinations showed rapid destruction of the humeral head. MRI confirmed the osteolysis. Due to the lack of any clinical evidence supporting neurological cause, Gorham Stout disease was the strongest possibility. | Given the fact that the patient presented late, and that the osteolysis had already ceased, the patient did not undergo any treatment. |
| Bode-Lesniewska et al. (5) | 2002 | 65-year-old female with a history of pain in the left shoulder and cervico-thoracic regions. She attributed the case to a traumatic dislocation of her humerus 2 years prior to presentation. | Left arm mobility was impaired, and profound tenderness was found at the cervico-thoracic region. Radiographs and MRI showed bone resorption in multiple areas of the shoulder and the affected vertebra. | Conservative therapy failed to stop progression. Massive osteolysis hindered further medical procedures, and consequently, the patient became bedridden. Post-radiation esophagitis and severe depression developed, and the patient died 15 months after clinical investigation. |
| Vrettos et al. (25) | 2004 | 17-year-old male presented with a history of sudden onset of severe right shoulder pain after lifting himself out of a swimming pool. | Radiographic imaging revealed a pathologic fracture involving the shoulder girdle region. The muscles in that region were significantly atrophied when compared to the contralateral side. Biopsy of the blade and scapula confirmed Gorham-Stout disease. | A total scapular replacement was performed. The patient then made an uneventful recovery. On 6-year follow-up, the patient reported improvements in pain and strength. |
| Underwood et al. (26) | 2006 | 47-year-old male with a previously fractured right clavicle, presents to the hospital with extreme dyspnea. | After conventional therapy failed to heal the clavicular fracture, autodigestion led to the disappearance of the patient’s right clavicle. This led to chylothorax and the patient’s respiratory symptoms. After further examination, Gorham-Stout disease was diagnosed. | The patient underwent surgery to drain the chyle from the right pleural cavity. The right thoracic duct was excised and the patient was given neostigmine and glycopyrrolate. After the surgical procedure, the patient became stable and no further complications were reported. |
| Jangid et al. (27) | 2006 | 8-year-old female presented with a one and a half year pain and swelling in the left arm. There was a history of a fracture at the level of the humerus three years prior. There was a massive swelling in the area, and shoulder and elbow motion was markedly lost. | Radiologic examination revealed massive osteolysis in the humeral shaft and the proximal end of the humerus. An open biopsy of the lesion established a diagnosis of Gorham Stout disease. | A left sided forequarter amputation was performed. |
| Sestan and Miletic (28) | 2006 | 58-year-old male presented with swelling and weakness of the right shoulder of six months duration. No history of trauma was recorded. | Radiological imaging revealed osteolysis of humeral head and lateral clavicle. Gorham Stout disease was diagnosed. | No intervention was done since the osteolysis had already stopped and the disease had already stabilized. |
| Malik et al. (29) | 2008 | 8-year-old female presents with a complaint of swelling extending from the tip of the left arm near the shoulder to just above elbow. The swelling was hard and painful upon deep palpation. | X-ray findings showed multicystic expansile lytic areas with loss of cortical definition, and suggested Gorham Stout disease. Histological evidence of cystic angiomatosis confirmed the diagnosis. | n/a |
| Buerfeind et al. (30) | 2010 | 46-year-old business economist suffered an inadequate trauma to the humerus and subsequently developed self-limited idiopathic osteolysis of the left humeral head. | Histopathological findings confirmed Gorham Stout syndrome of the shoulder. | Treatment was indicated operatively by means of inverted shoulder joint endoprosthesis. |
| De Smet et al. (31) | 2010 | 8-year-old male patient presented with dyspnea and tachypnea of recent onset. | CT Scans and chest radiographs revealed massive chylothorax with mediastinal shift. Later imaging with 3D rendering revealed massive bone loss of rib, clavicle, and shoulder regions. | A biopsy of the left scapula confirmed Gorham Stout syndrome associated with chylothorax. The patient was treated with interferon alfa-2b and intravenous bisphosphonate with calcium supplements. Months later, chyle production diminished and eventually stopped. |
| Garbers et al. (32) | 2011 | 77-year-old female patient with rest pain in both shoulders after suffering minor trauma 8 weeks prior to presentation. | X-rays of both shoulders revealed osteolysis of both humoral heads, glenoids, and lateral clavicles. | Bisphosphonate treatment, calcium, and calcitonin administration was able to stop osteolysis in the left shoulder. However, and after recurrence of osteolysis in the right shoulder, reconstruction using prosthesis on that side was executed. |
| Busilacchi et al. (33) | 2012 | 36-year-old male dockworker presented with a dislocated shoulder after being hit by a heavy piece of equipment during work. The dislocation was immediately reduced. The shoulder was immobilized in a splint for 4 weeks. | The patient presented for a follow-up after 2 months. He complained of a painful clunk during flexion and adduction. Physical examination showed positive apprehension, posterior stress, and posterior shift and load tests. The symptoms were clearly due to capsulolabral deficiency. However, Radiographs showed small osteolytic areas. | An Arthroscopic posterior capsulorrhaphy was executed as a treatment. However, the patient was readmitted after a month with his shoulder swollen and painful. After multiple tests failed to show the cause of the osteolysis, a shoulder replacement procedure was performed. 12 months later, osteolysis stopped. Histopathological findings later revealed Gorham Stout syndrome. |
| Zheng et al. (34) | 2012 | 5-year-old female patient presented with back pain of 3 month history. Diagnosis was that of tuberculous pleuritis. However, anti-tuberculous therapy was not successful. 50 days afterwards, a soft mass appeared at her upper leg. | X-rays revealed massive osteolysis of the bilateral clavicle, bilateral scapula, multiple ribs, multiple vertebra, and other bony structures of her body. Histopathological, clinical, and radiographic findings later confirmed Gorham Stout disease. | The patient was given oral anti-osteoclastic medication containing bisphosphonates. No evidence of osteolysis was found 3 years later. |
| El-Kouba et al. (35) | 2015 | 8-year-old male patient presented with a history of 3 traumatic fractures of his left clavicle in a span of 2 years. Weeks after the third traumatic incident, radiographs showed that part of the bone was missing. | ACT, MRI, and biopsy were requested. The MRI showed no impairment of soft tissue, and the biopsy suggested bone angioma. Due to the patient’s history and examination, Gorham Stout disease was the reached diagnosis. | After 3 years of medical follow-up, osteolysis stabilized. Treatment constituted of physical therapy and hydrotherapy to strengthen the muscles. Bisphosphonate and calcitonin were administered to prevent reabsorption. |
| Liu et al. (36) | 2016 | 37-year-old female presented with bone pain that affected the right scapula and clavicle. | Examination revealed GSD of the right shoulder | The patient was started on Pamidronate and remained stable afterwards. |
| Brunner et al. (37) | 2016 | 84-year-old female presented with pain, swelling, and hematoma of the left upper arm with no history of trauma. | Clinical, radiological, and histopathological findings revealed Gorham Stout syndrome of the shoulder. | Clinical and radiological follow-up examinations were conducted every year for four years following initial presentation. |
| 92-year-old female presented with minor left shoulder pain due to a contusion. | Clinical examination revealed an unstable shoulder. MRI revealed destruction of the humeral head. Biopsy of the joint capsule confirmed Gorham Stout disease. | Clinical and radiological follow-up were conducted every three months for four years following initial presentation. | ||
| 77-year-old female presented with pain in the right shoulder with no history of trauma. | Radiographic and histological examination revealed Gorham Stout disease. | Patient underwent a reverse shoulder arthroplasty, and recovered without complications. | ||
| Brance et al. (38) | 2017 | 70-year-old man presented with a history of pain and limited motion in the left shoulder with normal X-ray. A pathological fracture of the humerus occurred 6 months later. | MRI showed severe osteolysis and disorganization in the affected area. After ruling out other diagnoses, and executing further tests, Gorham Stout disease was diagnosed. | The patient was treated using intravenous zoledronic acid. A good response was reported after the first infusion. |
| Papadakis et al. (39) | 2017 | 44-year-old male presents with pain and movement limitation in right shoulder. | X-ray revealed absence of largest portion of the scapula. Further examination revealed Gorham Stout disease. | n/a |
| Stevens et al. (40) | 2018 | 44-year-old female, previously healthy, presented with a history of increasing pain and reduced range of motion in right shoulder. | MRI revealed an infiltrative lesion in the proximal humerus, with cortical thinning and soft tissue involvement. Subsequent radiological findings revealed intramedullary and subcortical radiolucent foci. Gorham Stout disease was diagnosed. | n/a |
| Suranigi et al. (41) | 2018 | 37-year-old female with presented with a 3-month history of discomfort in her left shoulder and difficulty in using her left arm. | Radiological imaging revealed significant osteolysis and the absence of the humeral head. Gorham Stout disease was suspected. Nevertheless, and due to the fact that the patient only had minimal disability, she was not willing to biopsy or undergo surgical treatment. | The patient underwent physical therapy to strengthen the muscles of the area and to increase range of motion. After 2 years, the patient stated that the disability did not worsen and hence refused further hospital visits. |
| Li et al. (42) | 2018 | 26-year-old male presented with pain in left shoulder after colliding with other players while playing basketball. | Radiographs revealed osteolysis of the left scapula and the 7th-9th left ribs. Further pathological examinations revealed Gorham Stout disease. | In an aim to preserve shoulder function, the patient was treated conservatively. Radiotherapy and bisphosphonate treatment was administered for 6 months, and the patient showed marked improvement. |
| Wang and Li (43) | 2018 | 3-year-old female presents with dyspnea of one week duration and a firm, violaceous and depressed lesion on her right chest, shoulder, and upper arm. | Chest radiograph revealed major osteolysis of the right humerus, scapula, and most of the clavicle. This was complicated by a right-sided pleural effusion. These findings suggested Gorham Stout disease. | The patient was started on sirolimus therapy, and within 13 months, her status showed marked umprovement. |
Table 2.
Demographic and clinical characteristics of the cases under study
| N | Percent (%) | ||
|---|---|---|---|
| Sex | Male | 21 | 57 |
| Female | 16 | 43 | |
| Age | >18 | 12 | 32 |
| 18-65 | 18 | 49 | |
| 65< | 7 | 19 | |
| Side | Right | 19 | 51 |
| Left | 16 | 43 | |
| Bilateral | 2 | 6 | |
| History | Traumatic | 13 | 35 |
| Non-traumatic | 14 | 38 | |
| n/a | 10 | 27 | |
| Treatment | Surgical | 13 | 35 |
| Non-surgical | 17 | 46 | |
| n/a | 7 | 19 | |
| Location (more than one anatomical location in the shoulder can be involved in one case) | Humerus | 20 | 54 |
| Scapula | 13 | 35 | |
| Clavicle | 11 | 30 | |
| Other | 5 | 15 | |
All cases reported pain or discomfort in the shoulder area. The anatomical location most prone to GSD in the shoulder seemed to be the humerus, since it was affected in 20 of the cases reported (54%). The scapula and the clavicle followed as they were affected in 13 cases (35%) and 11 (30%) cases, respectively. In addition, 16 cases (43%) affected the left side, 19 cases (51%) affected the right side and two cases (6%) were bilateral.
Moreover, 14 cases (38%) reported no history of trauma prior to GSD, 13 cases (35%) reported a traumatic incident that led to GSD, and nine cases (27%) did not report whether the onset of GSD was traumatic or not.
Therapeutic options were surgical or non-surgical. Conservative treatment was opted in 17 cases (46%), while surgery was performed in 13 (35%). Seven cases (19%) did not report the therapeutic modality used for treatment. Outcomes were reported stable and positive in 28 cases (76%). Death occurred in two cases (5%), whereas seven cases (19%) did not report any outcome.
Discussion
GSD is an idiopathic, rare and debilitating condition of bone lysis that can affect the shoulder. Our study shows that males and females are almost equally affected, and that the condition is common among young adults. Pain is the predominating presenting symptom and the humerus is the most common site of disease. Understanding the demographics and clinical characteristics of GSD in the shoulder region will help in formulating better therapeutic interventions and public health policies.
Shoulder Joint
The shoulder provides the largest extent of motion in the body using a complex of static and dynamic elements (44-47). The bony elements that are prone to GSD in the shoulder girdle region are the humerus, the glenoid, the scapula, the acromion, the clavicle, and the coracoid. The large mobility of the shoulder joint is sacrificed with decreased stability. This stability is maintained using functional muscular groups, the glenoid labrum, articular cartilage, glenohumeral ligaments and the shoulder joint capsule (45). Together, the stabilizers and the bony components provide a balanced network that is involved in many of our daily movements and functions (46). Hence, any disability in this area would cause a significant impairment in a patient’s life. Osteolysis in the shoulder region compromises both its stability and its mobility, and thus, renders the patient incapacitated. Moreover, the severe damage in the affected region causes weakness and progressively loss of function, along with significant pain (21). Patients often suffer from a decreased quality of life due to the inactivity, and may even develop depression due to chronic pain (5, 47-50).
Presentation and Diagnosis
Upon the first visit, patients usually present with a history of trauma or dislocation to the shoulder area (15, 33). Pain persists for long durations and is often accompanied with loss of function and swelling (29). While histology may confirm the presence of lymphatic infiltration and angiomatosis, it is radiographic examination that confirms the massive osteolysis involved in the shoulder area.
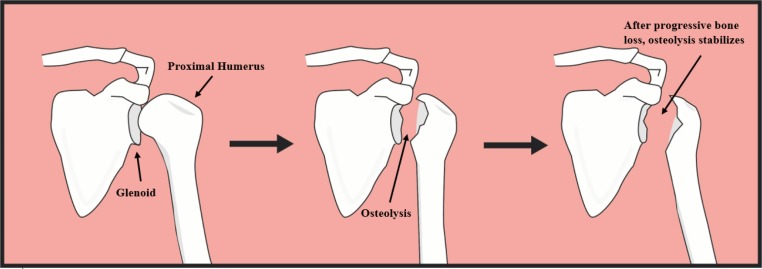
The initial radiologic sign that may suggest GSD can appear on Magnetic Resonance Imaging (MRI) or computed tomography (CT), and constitute lucent changes in the foci of intramedullary and subcortical regions, similar to osteoporosis (51, 52). Concentric reduction of the bone leads to tapering, which often results in bone that resembles a “stick of candy.” Complete disappearance and resorption of the affected bone follows, suggesting the term ‘Vanishing Bone Disease’ [Figure 2] (51).
Figure 2.
An example of progressive bone loss in Gorham-Stout Disease affecting the proximal humerus and glenoid region. Osteolytic patterns are unpredictable, and progress erratically before reaching a stable state and subsiding
GSD can occur in both sexes, in any age group, and can affect either sides of the body (54). The scapula and proximal end of the humerus are the most frequent sites for massive osteolysis. GSD in the shoulder area, as well as in other areas like the ribs or the thoracic vertebrae, can cause further complications that include chylothorax and nerve root compression, leading to a poorer prognosis (55). Chylothorax is usually fatal since it is associated with malnutrition and immunosuppression involving lymphocytopenia (55). Moreover, subsequent respiratory failures due to incapacitation can lead to death (55). Several differential diagnoses exist for GSD. These include osteomyelitis, hereditary multicentric osteolysis, rheumatoid arthritis, osteolysis due to intraosseous malignacies, neuroarothropathic shoulder, hyperparathyroidism and eosinophilic granuloma (24, 56, 57).
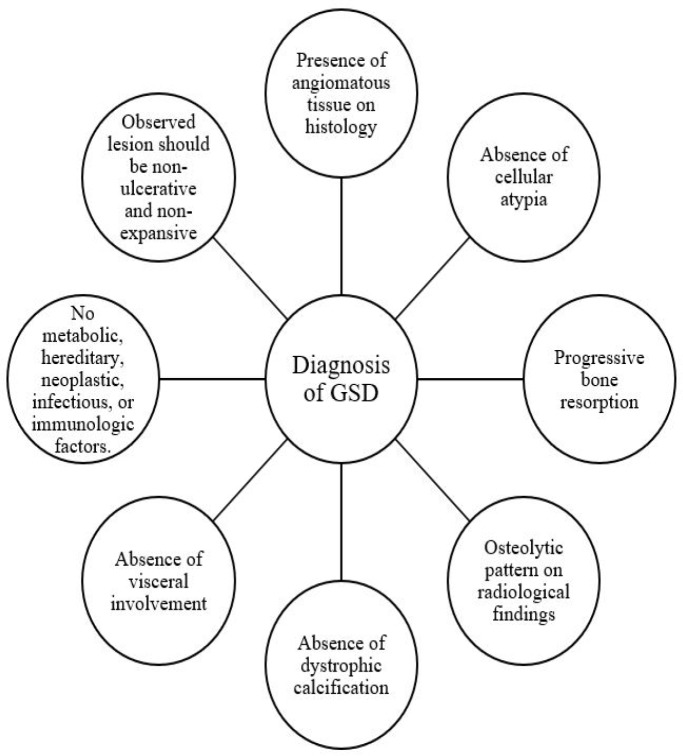
Due to the controversy behind its etiology, GSD is often diagnosed late and by elimination. Several criteria should be met for a definitive diagnosis of GSD in the shoulder, and these involve several examinations [Figure 3] (58). The first criterion depends on the histological findings of the patient; presence of angiomatous tissue in the affected shoulder area must be noted. Absence of cellular atypia that may predict malignancy must be noted as well (58). There should also be evidence of progressive bone resorption in the shoulder area and an osteolytic radiographic pattern which is typically visualized using a MRI, X-ray or CT scan (59, 60). Absence of dystrophic calcification and visceral involvement should be noted as well, and the observed lesion should be non-ulcerative and non-expansive (58). Finally, metabolic, hereditary, neoplastic, infectious, or immunologic factors should be eliminated. Once all these criteria are met, a diagnosis of GSD in the shoulder can be confirmed.
Figure 3.
The different criteria needed to diagnose Gorham-Stout disease. These include the presence of angiomatous tissue, evidence of progressive bone resorption and an osteolytic radiographic pattern. Moreover, absence of cellular atypia, dystrophic calcification, and visceral involvement should be noted as well, and the observed lesion should be non-ulcerative and non-expansive. Finally, to confirm the diagnosis, one must eliminate any metabolic, hereditary, neoplastic, infectious, or immunologic factors
Etiology
Even though active osteolysis signifies GSD, its etiology remains under question. Several modalities have been proposed to help describe how the disease progresses. In 1955, Gorham and Stout concluded that GSD is associated with angiomatosis of the blood and the lymph, and is pathologically distinct from hemangiomas of the bones (61). Usually, GSD occurs in a specific area, but it can be generalized and associated with multiple cutaneous hemangiomas (62). Several other conditions have been associated with GSD, and these include growth of unrestricted granulation tissue, posttraumatic hyperemia, hemangiomatosis, and lymphangiomatosis (55).
In GSD patients, angiomatosis is often present in the affected bones or the adjacent soft tissue, and consequently, osteolysis of the affected area is often associated with angiomatosis of the lymphatic tissues and the blood (55). Multiple approaches have been debated with regards to the etiology of GSD. One approach suggests that this angiomatosis changes the environment of the affected area causing increased hypoxia and acidosis which may induce chelation of calcium ions and activation of hydrolytic enzymes. This, in turn, can cause osteolysis and resorption of the bone in the affected region, suggesting that GSD is mainly due to irregular lymphangiogenesis and angiomatosis. Another approach describes an error in the cellular and humoral machineries of osteoclast formation (63-65). Osteoclasts are activated by Interleukin-6 (IL-6) and this leads to bone resorption. Monocyte cultures show increased IL-6 concentrations in the serum of GSD patients (37, 63). This increase in IL-6 causes a rise in osteoclast sensitivity to humoral elements which leads to massive bone resorption, leading to a state of osteolysis (65, 66).
The etiology of the disease has also been attributed to the unrestricted growth of granulation tissue in the affected area, which can exert pressure and lead to bone resorption, similar to what happens in enlarged aneurysms (67).
The possibility of agenesis of thyroid C cells which secrete calcitonin has also been suggested as a possible contributor to GSD (68). Calcitonin serves as an inhibitor of bone resorption, and therefore, the lack of development of thyroid C cells would greatly diminish the amount of calcitonin in the body. This in fact can cause, or at least contribute to, the massive osteolysis found in GSD (68).
Therapeutic Modalities
Even though GSD is generally a benign condition with spontaneous remission, the extent of damage and limitation it inflicts on the life of a patient highlights the need for proper therapeutic modalities. Given the mysterious nature of this disease, its unclear pathology and unpredictable prognosis, treatment options remain a challenge and are often catered specifically to the individual case (35, 57). Differences in general health conditions, comorbidities, and extent of loss of functions entail different therapeutic approaches (35).
GSD in the shoulder treatment usually consists of three parts: conservative therapy and medication, radiotherapy, and surgery (69). Conservative therapy often includes physical therapy to strengthen the muscles of the shoulder and provide support to the affected area, in an aim to restore some of its function and stability (34). As for medication, bisphosphonates have shown promising results, and are the first-line treatment for GSD; their anti-osteolytic activity limits bone resorption. Other possible medications include vitamin D, calcium, adrenal extracts, androgens and interferon alpha-2b (70-74).
In cases of severe symptomatology, radiotherapy and surgical intervention are considered (75). Radiotherapy have proven to be adequate in moderate doses but has been shown to cause some serious long-term complications in high doses (76). These include secondary malignancies, and growth restrictions in children and adolescents (75). Surgical intervention includes surgical resection of the affected area in the shoulder, and often involves a replacement of the shoulder joint via arthroplasty (37).
GSD is a rare disease of unknown etiology and unpredictable prognosis that causes spontaneous massive osteolysis in the body. The shoulder girdle is the most common site for GSD. Therapeutic regimens have not been fully established and validated. Given the substantial involvement of the shoulder in our daily lives, it is of pivotal importance to raise awareness on this condition in an aim to provide a correct diagnosis and delegate proper therapeutic modalities.
Limitations
We focused on studies and reports that explored patients with GSD in the shoulder, exclusively. We took ample precautions to avoid any bias or improper analyses by having two authors (M.Y.F. and J.F.) revise all studies identified and the selection steps. Some information might be missing and/or without follow-up. Nevertheless, this analysis is distinctive and imperative as it provides a wholistic perspective on the current state of GSD in the shoulder and offers researchers and clinicians the opportunity to reflect upon future prospective and observational studies on GSD.
References
- 1.Dong Q, Zhang Y, Sun C, Guo J. Gorham-Stout syndrome affecting the left mandible: a case report. Exp Ther Med. 2013;5(1):162–4. doi: 10.3892/etm.2012.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang W, Wang H, Zhou X, Li X, Sun W, Dellinger M, et al. Lymphatic endothelial cells produce M-CSF, causing massive bone loss in mice. J Bone Miner Res. 2017;32(5):939–50. doi: 10.1002/jbmr.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manisali M, Ozaksoy D. Gorham disease: correlation of MR findings with histopathologic changes. Eur Radiol. 1998;8(9):1647–50. doi: 10.1007/s003300050603. [DOI] [PubMed] [Google Scholar]
- 4.van der Linden-van der Zwaag H, Onvlee GJ. Massive osteolysis (Gorham’s disease) affecting the femur. Acta Orthop Belg. 2006;72(3):261–8. [PubMed] [Google Scholar]
- 5.Bode-Lesniewska B, Von Hochstetter A, Exner G, Hodler J. Gorham-stout disease of the shoulder girdle and cervico-thoracic spine: fatal course in a 65-year-old woman. Skeletal Radiol. 2002;31(12):724–9. doi: 10.1007/s00256-002-0568-y. [DOI] [PubMed] [Google Scholar]
- 6.Yoo SY, Hong SH, Chung HW, Choi JA, Kim CJ, Kang HS. MRI of Gorham’s disease: findings in two cases. Skeletal Radiol. 2002;31(5):301–6. doi: 10.1007/s00256-002-0487-y. [DOI] [PubMed] [Google Scholar]
- 7.Mavrogenis AF, Zambirinis CP, Dimitriadis PA, Tsakanikas A, Papagelopoulos PJ. Gorham-Stout disease. J Surg Orthop Adv. 2010;19(2):85–90. [PubMed] [Google Scholar]
- 8.Maillot C, Cloche T, Le Huec JC. Thoracic osteotomy for Gorham-stout disease of the spine: a case report and literature review. Eur Spine J. 2018;27(9):2285–90. doi: 10.1007/s00586-014-3613-3. [DOI] [PubMed] [Google Scholar]
- 9.Möller G, Priemel M, Amling M, Werner M, Kuhlmey AS, Delling G. The Gorham-stout syndrome (Gorham’s massive osteolysis) A report of six cases with histopathological findings. J Bone Joint Surg Br. 1999;81(3):501–6. doi: 10.1302/0301-620x.81b3.9468. [DOI] [PubMed] [Google Scholar]
- 10.Kulenkampff HA, Richter GM, Hasse WE, Adler CP. Massive pelvic osteolysis in the Gorham-Stout syndrome. Int Orthop. 1990;14(4):361–6. doi: 10.1007/BF00182645. [DOI] [PubMed] [Google Scholar]
- 11.Lee S, Finn L, Sze RW, Perkins JA, Sie KC. Gorham stout syndrome (disappearing bone disease): two additional case reports and a review of the literature. Arch Otolaryngol Head Neck Surg. 2003;129(12):1340–3. doi: 10.1001/archotol.129.12.1340. [DOI] [PubMed] [Google Scholar]
- 12.Hofbauer LC, Klassen RA, Khosla S. Gorham-Stout disease (phantom bone) of the shoulder girdle. Rheumatology. 1999;38(9):904–5. doi: 10.1093/rheumatology/38.9.904. [DOI] [PubMed] [Google Scholar]
- 13.Bedi G. Shoulder injury in athletes. J Clin Orthop Trauma. 2011;2(2):85–92. [Google Scholar]
- 14.Gorham LW, Wright AW, Shultz HH, Maxon FC Jr. Disappearing bones: a rare form of massive osteolysis: report of two cases, one with autopsy findings. Am J Med. 1954;17(5):674–82. doi: 10.1016/0002-9343(54)90027-3. [DOI] [PubMed] [Google Scholar]
- 15.Jacobs P. Post-traumatic osteolysis of the outer end of the clavicle. J Bone Joint Surg Br. 1964;46(4):705–7. [PubMed] [Google Scholar]
- 16.Feigl D, Seidel L, Marmor A. Gorham’s disease of the clavicle with bilateral pleural effusions. Chest. 1981;79(2):242–4. doi: 10.1378/chest.79.2.242. [DOI] [PubMed] [Google Scholar]
- 17.Hugo B, Schmidt M. Pseudo-tumour of the shoulder after massive osteolysis (Gorham-Stout) Rofo. 1989;150(1):108–10. doi: 10.1055/s-2008-1046988. [DOI] [PubMed] [Google Scholar]
- 18.Damron TA, Brodke DS, Heiner JP, Swan JS, DeSouky S. Case report 803. Skeletal Radiol. 1993;22(6):464–7. doi: 10.1007/BF00538454. [DOI] [PubMed] [Google Scholar]
- 19.Canil K, Fitzgerald P, Lau G. Massive chylothorax associated with lymphangiomatosis of the bone. J Pediatr Surg. 1994;29(9):1186–8. doi: 10.1016/0022-3468(94)90796-x. [DOI] [PubMed] [Google Scholar]
- 20.Sato K, Sugiura H, Yamamura S, Mieno T, Nagasaka T, Nakashima N. Gorham massive osteolysis. Arch Orthop Trauma Surg. 1997;116(8):510–3. doi: 10.1007/BF00387590. [DOI] [PubMed] [Google Scholar]
- 21.Pans S, Simon JP, Dierickx C. Massive osteolysis of the shoulder (Gorham-stout syndrome) J Shoulder Elbow Surg. 1999;8(3):281–3. doi: 10.1016/s1058-2746(99)90144-1. [DOI] [PubMed] [Google Scholar]
- 22.Möller G, Priemel M, Amling M, Werner M, Kuhlmey AS, Delling G. The Gorham-Stout syndrome (Gorham’s massive osteolysis) A report of six cases with histopathological findings. J Bone Joint Surg Br. 1999;81(3):501–6. doi: 10.1302/0301-620x.81b3.9468. [DOI] [PubMed] [Google Scholar]
- 23.Mochizuki K, Koyama S, Ishii Y. Seventeen-year follow-up of massive osteolysis of the scapula. J Orthop Sci. 2000;5(6):618–21. doi: 10.1007/s007760070016. [DOI] [PubMed] [Google Scholar]
- 24.Rao P, Kotwal PP, Goel S. Painless destruction of the shoulder joint: a case report. Clin Rheumatol. 2001;20(2):143–6. doi: 10.1007/pl00011194. [DOI] [PubMed] [Google Scholar]
- 25.Vrettos BC, Wallace WA, Neumann L, Frostick SP. Total scapular replacement: medium-term follow-up. J Shoulder Elbow Surg. 2004;13(4):472–5. doi: 10.1016/j.jse.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 26.Underwood J, Buckley J, Manning B. Gorham disease: an intraoperative case study. AANA J. 2006;74(1):45–8. [PubMed] [Google Scholar]
- 27.Jangid S, Mittal R, Sharma V, Das AK. Progressive massive osteolysis of the humerus. J Shoulder Elbow Surg. 2006;15(3):386–90. doi: 10.1016/j.jse.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 28.Sestan B, Miletic D. Rapid idiopathic osteolysis of the humeral head and clavicle. West Indian Med J. 2006;55(5):354–7. doi: 10.1590/s0043-31442006000500013. [DOI] [PubMed] [Google Scholar]
- 29.Malik R, Malik R, Tandon S, Tandon P. Skeletal angiomatosis-rare cause of bone destruction: a case report with review of literature. Indian J Pathol Microbiol. 2008;51(4):515–8. doi: 10.4103/0377-4929.43745. [DOI] [PubMed] [Google Scholar]
- 30.Buerfeind A, Bürger H, Schlüter-Brust K, Eysel P, Delank KS. Gorham-Stout syndrome (GSS) with fulminant aseptic osteonecrosis of the shoulder. Orthopade. 2010;39(10):1003–8. doi: 10.1007/s00132-010-1638-9. [DOI] [PubMed] [Google Scholar]
- 31.De Smet K, De Maeseneer M, Huijssen-Huisman E, Van Gorp V, Hachimi-Idrissi S, Ernst C. A rare cause of dyspnea due to chylothorax. Emerg Radiol. 2010;17(6):503–5. doi: 10.1007/s10140-010-0898-3. [DOI] [PubMed] [Google Scholar]
- 32.Garbers E, Reuther F, Delling G. Report of a rare case of Gorham-stout disease of both shoulders: bisphosphonate treatment and shoulder replacement. Case Rep Rheumatol. 2011;2011:565142. doi: 10.1155/2011/565142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Busilacchi A, Ramazzotti D, Ulisse S, Gigante A. Gorham-Stout disease as a complication of posterior shoulder capsulorrhaphy. J Shoulder Elbow Surg. 2012;21(9):e1–7. doi: 10.1016/j.jse.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 34.Zheng MW, Yang M, Qiu JX, Nan XP, Huang LY, Zhang WD, et al. Gorham-Stout syndrome presenting in a 5-year-old girl with a successful bisphosphonate therapeutic effect. Exp Ther Med. 2012;4(3):449–51. doi: 10.3892/etm.2012.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El-Kouba G, de Araujo Santos R, Pilluski PC, Severo A, Lech O. Gorham-stout syndrome: phantom bone disease. Rev Bras Ortop. 2015;45(6):618–22. doi: 10.1016/S2255-4971(15)30313-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu Y, Zhong DR, Zhou PR, Lv F, Ma DD, Xia WB, et al. Gorham-stout disease: radiological, histological, and clinical features of 12 cases and review of literature. Clin Rheumatol. 2016;35(3):813–23. doi: 10.1007/s10067-014-2780-2. [DOI] [PubMed] [Google Scholar]
- 37.Brunner U, Rückl K, Konrads C, Rudert M, Plumhoff P. Gorham-stout syndrome of the shoulder. SICOT J. 2016;2(1) doi: 10.1051/sicotj/2016015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brance ML, Castiglioni A, Cóccaro N, Palatnik M. Two cases of Gorham-stout disease with good response to zoledronic acid treatment. Clin Cases Miner Bone Metab. 2017;14(2):250–3. doi: 10.11138/ccmbm/2017.14.2.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Papadakis GZ, Millo C, Bagci U, Blau J, Collins MT. 18F-NaF and 18F-FDG PET/CT in Gorham-Stout disease. Clin Nucl Med. 2016;41(11):884–5. doi: 10.1097/RLU.0000000000001369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stevens J, Flower H, Patton JT. What does vanishing bone disease look like? BMJ Case Rep. 2018;2018:bcr–2017. doi: 10.1136/bcr-2017-224061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Suranigi SM, Kerketta AH, Palaniappan P, Najimudeen SP. An interesting case of vanishing shoulder. BMJ Case Rep. 2018;2018:bcr–2018. doi: 10.1136/bcr-2018-226768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li MH, Zhang HQ, Lu YJ, Gao P, Huang H, Hu YC, et al. Successful management of gorham–stout disease in scapula and ribs: a case report and literature review. Orthop Surg. 2018;10(3):276–80. doi: 10.1111/os.12390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang Z, Li K. A girl with Gorham–stout disease. J Pediatr. 2018;203(1):456. doi: 10.1016/j.jpeds.2018.07.076. [DOI] [PubMed] [Google Scholar]
- 44.Wilk KE, Obma P, Simpson CD, Cain EL, Dugas J, Andrews JR. Shoulder injuries in the overhead athlete. J Orthop Sports Phys Ther. 2009;39(2):38–54. doi: 10.2519/jospt.2009.2929. [DOI] [PubMed] [Google Scholar]
- 45.Fares MY, Salhab HA, Khachfe HH, Kane L, Fares Y, Fares J, et al. Upper limb injuries in major league baseball. Phys Ther Sport. 2020;41:49–54. doi: 10.1016/j.ptsp.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 46.Fares MY, Fares J, Baydoun H, Fares Y. Prevalence and patterns of shoulder injuries in major league baseball. Phys Sportsmed. 2019;17(1):1–5. doi: 10.1080/00913847.2019.1629705. [DOI] [PubMed] [Google Scholar]
- 47.Fares MY, Fares J, Fares Y, Abboud JA. Musculoskeletal and head injuries in the Ultimate Fighting Championship (UFC) Phys Sportsmed. 2019;47(2):205–11. doi: 10.1080/00913847.2018.1546108. [DOI] [PubMed] [Google Scholar]
- 48.Fares J, Fares MY, Fares Y. Musculoskeletal neck pain in children and adolescents: risk factors and complications. Surg Neurol Int. 2017;8(1):72. doi: 10.4103/sni.sni_445_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fares MY, Dimassi Z, Baydoun H, Musharrafieh U. Slipping rib syndrome: solving the mystery of the shooting pain. Am J Med Sci. 2018;357(2):168–73. doi: 10.1016/j.amjms.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 50.Fares MY, Fares J, Baydoun H, Fares Y. Sport and exercise medicine research activity in the Arab world: a 15-year bibliometric analysis. BMJ Open Sport Exerc Med. 2017;3(1):e000292. doi: 10.1136/bmjsem-2017-000292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnson PM, McClure JG. Observations on massive osteolysis: a review of the literature and report of a case. Radiology. 1958;71(1):28–42. doi: 10.1148/71.1.28. [DOI] [PubMed] [Google Scholar]
- 52.Vinée P, Tanyü MO, Hauenstein KH, Sigmund G, Stöver B, Adler CP. CT and MRI of Gorham syndrome. J Comput Assist Tomogr. 1994;18(6):985–9. doi: 10.1097/00004728-199411000-00028. [DOI] [PubMed] [Google Scholar]
- 53.Malik R, Malik R, Tandon S, Tandon P. Skeletal angiomatosis-rare cause of bone destruction: a case report with review of literature. Indian J Pathol Microbiol. 2008;51(4):515–8. doi: 10.4103/0377-4929.43745. [DOI] [PubMed] [Google Scholar]
- 54.Sage MR, Allen PW. Massive osteolysis Report of a case. J Bone Joint Surg Br. 1974;56(1):130–5. [PubMed] [Google Scholar]
- 55.Liu M, Liu W, Qiao C, Han B. Mandibular Gorham–stout disease: a case report and literature review. Medicine. 2017;96(42):e8184. doi: 10.1097/MD.0000000000008184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ozbayrak M, Yilmaz MH, Kantarci F, Ozer H, Harmanci K, Babacan M, et al. A case of an idiopathic massive osteolysis with skip lesions. Korean J Radiol. 2013;14(6):946–50. doi: 10.3348/kjr.2013.14.6.946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nikolaou VS, Chytas D, Korres D, Efstathopoulos N. Vanishing bone disease (Gorham-stout syndrome): a review of a rare entity. World J Orthop. 2014;5(5):694–8. doi: 10.5312/wjo.v5.i5.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Heffez L, Doku HC, Carter BL, Feeney JE. Perspectives on massive osteolysis: report of a case and review of the literature. Oral Surg Oral Med Oral Pathol. 1983;55(4):331–43. doi: 10.1016/0030-4220(83)90185-8. [DOI] [PubMed] [Google Scholar]
- 59.Marymont JV. Comparative imaging: massive osteolysis (Gorham’s syndrome, disappearing bone disease) Clin Nucl Med. 1987;12(2):153–4. [PubMed] [Google Scholar]
- 60.Assoun J, Richardi G, Railhac JJ, Le Guennec P, Caulier M, Dromer C, et al. CT and MRI of massive osteolysis of Gorham. J Comput Assist Tomogr. 1994;18(6):981–4. doi: 10.1097/00004728-199411000-00027. [DOI] [PubMed] [Google Scholar]
- 61.Gorham LW, Stout AP. Massive osteolysis (acute spontaneous absorption of bone, phantom bone, disappearing bone): its relation to hemangiomatosis. J Bone Joint Surg Am. 1955;37(5):985–1004. [PubMed] [Google Scholar]
- 62.Fornasier VL. Haemangiomatosis with massive osteolysis. J Bone Joint Surg Br. 1970;52(3):444–51. [PubMed] [Google Scholar]
- 63.Nisbet JA, Helliwell S, Nordin BE. Relation of lactic and citric acid metabolism to bone resorption in tissue culture. Clin Orthop Relat Res. 1970;70(1):220–30. [PubMed] [Google Scholar]
- 64.Heyden G, Kindblom LG, Nielsen JM. Disappearing bone disease A clinical and histological study. J Bone Joint Surg Am. 1977;59(1):57–61. [PubMed] [Google Scholar]
- 65.Dellinger MT, Garg N, Olsen BR. Viewpoints on vessels and vanishing bones in Gorham-Stout disease. Bone. 2014;63(1):47–52. doi: 10.1016/j.bone.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 66.Devlin RD, Bone HG 3rd, Roodman GD. Interleukin-6: a potential mediator of the massive osteolysis in patients with Gorham-Stout disease. J Clin Endocrinol Metab. 1996;81(5):1893–7. doi: 10.1210/jcem.81.5.8626854. [DOI] [PubMed] [Google Scholar]
- 67.Thompson JS, Schurman DJ. Massive osteolysis: case report and review of literature. Clin Orthop Relat Res. 1974;103(1):206–11. [PubMed] [Google Scholar]
- 68.Koršić M, Jelašić D, Potočki K, Giljević Z, Aganović I. Massive osteolysis in a girl with agenesis of thyroid C cells. Skeletal Radiol. 1998;27(9):525–8. doi: 10.1007/s002560050433. [DOI] [PubMed] [Google Scholar]
- 69.Hu P, Yuan XG, Hu XY, Shen FR, Wang JA. Gorham-stout syndrome in mainland China: a case series of 67 patients and review of the literature. J Zhejiang Univ Sci B. 2013;14(8):729–35. doi: 10.1631/jzus.B1200308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hammer F, Kenn W, Wesselmann U, Hofbauer LC, Delling G, Allolio B, et al. Gorham-stout disease--stabilization during bisphosphonate treatment. J Bone Miner Res. 2005;20(2):350–3. doi: 10.1359/JBMR.041113. [DOI] [PubMed] [Google Scholar]
- 71.Bruch-Gerharz D, Gerharz CD, Stege H, Krutmann J, Pohl M, Koester R, et al. Cutaneous lymphatic malformations in disappearing bone (Gorham-stout) disease: a novel clue to the pathogenesis of a rare syndrome. J Am Acad Dermatol. 2007;56(2 Suppl):S21–5. doi: 10.1016/j.jaad.2006.01.063. [DOI] [PubMed] [Google Scholar]
- 72.Radhakrishnan K, Rockson SG. Gorham’s disease. Ann N Y Acad Sci. 2008;1131(1):203–5. doi: 10.1196/annals.1413.022. [DOI] [PubMed] [Google Scholar]
- 73.Binder H, Weber PC, Siess W. Separation of inositol phosphates and glycerophosphoinositol phosphates by high-performance liquid chromatography. Anal Biochem. 1985;148(1):220–7. doi: 10.1016/0003-2697(85)90649-9. [DOI] [PubMed] [Google Scholar]
- 74.Aizawa T, Sato T, Kokubun S. Gorham disease of the spine: a case report and treatment strategies for this enigmatic bone disease. Tohoku J Exp Med. 2005;205(2):187–96. doi: 10.1620/tjem.205.187. [DOI] [PubMed] [Google Scholar]
- 75.Patel DV. Gorham’s disease or massive osteolysis. Clin Med Res. 2005;3(2):65–74. doi: 10.3121/cmr.3.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dunbar SF, Rosenberg A, Mankin H, Rosenthal D, Suit HD. Gorham’s massive osteolysis: the role of radiation therapy and a review of the literature. Int J Radiat Oncol Biol Phys. 1993;26(3):491–7. doi: 10.1016/0360-3016(93)90968-2. [DOI] [PubMed] [Google Scholar]